Assessment Tools for Health Literacy among the General Population: A Systematic Review
Abstract
1. Introduction
Aims
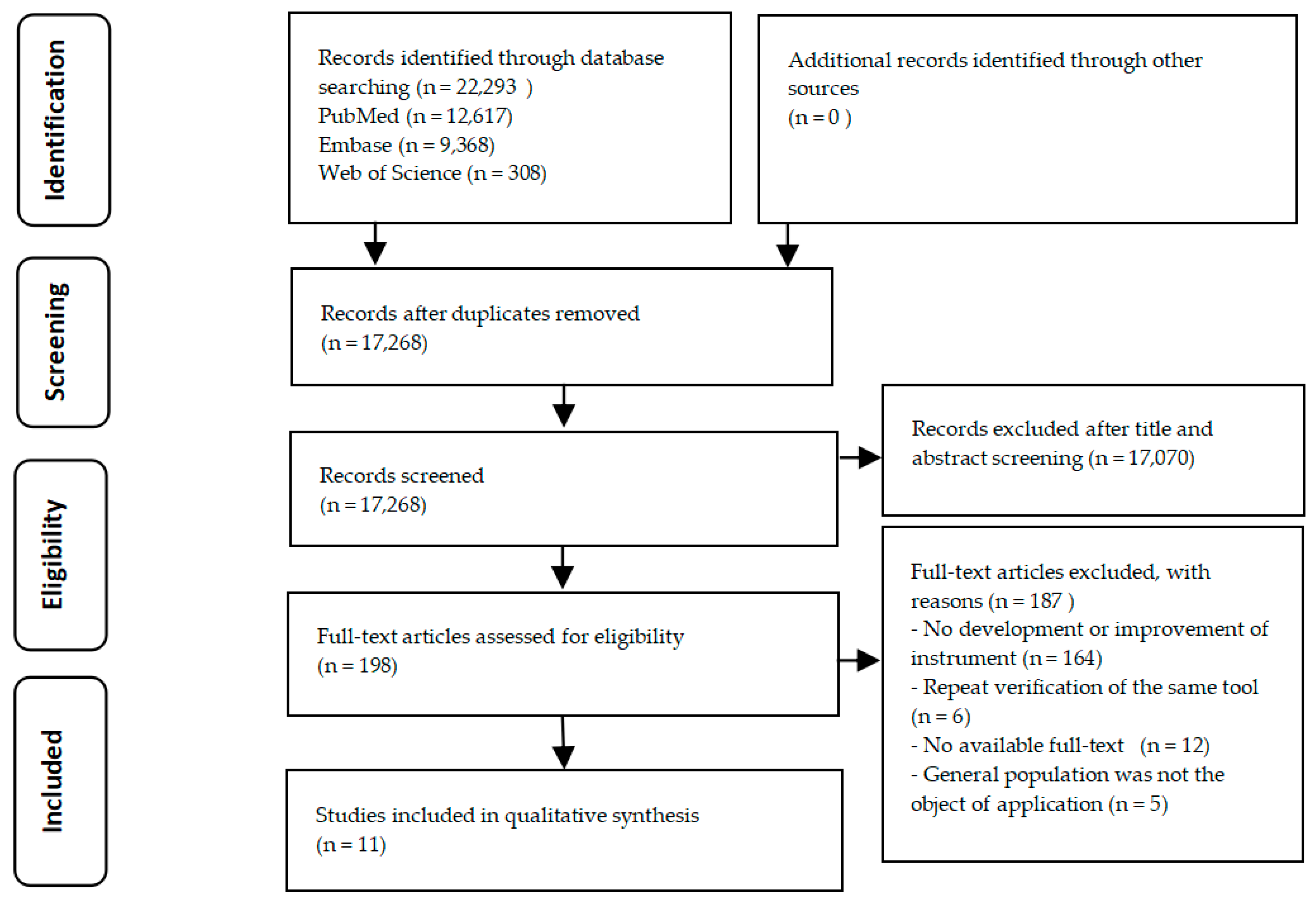
2. Materials and Methods
2.1. Retrieval Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Literature Screening, Quality Assessment, and Data Extraction
3. Results
3.1. Main Instrument Characteristics
3.2. S Measurement Modes Based on Health-Related Fields
3.3. Measurement Modes Based on Health-Related Abilities
3.4. Combination of Both Measurement Modes
3.5. Quality Assessment of Health Literacy Instrument Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Shanghai Declaration on Promoting Health in the 2030 Agenda for Sustainable Development. Available online: http://www.who.int/healthpromotion/conferences/9gchp/shanghai-declaration.pdf?ua=1 (accessed on 3 April 2018).
- World Health Organization. Health Promotion Glossary. 1998. Available online: http://www.who.int/healthpromotion/about/HPR%20Glossary%201998.pdf?ua=1 (accessed on 3 April 2018).
- The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy, September 2006. U.S. Dept. of Education, National Center for Education Statistics. Available online: https://nces.ed.gov/pubs2006/2006483_1.pdf (accessed on 3 April 2018).
- Health Literacy, Australia. 2006; Australian Bureau of Statistics. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/4233.0Main%20Features22006?opendocument&tabname=Summary&prodno=4233.0&issue=2006&num=&view= (accessed on 3 April 2018).
- Li, Y.; Mao, Q.; Shi, Q.; Tao, M.; Nie, X.; Li, L.; Huang, X.; Shi, M. Health literacy monitoring results of Chinese residents in 2012. Health Educ. China 2015, 31, 99–103. [Google Scholar]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Consortium. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Guidance on Strengthening Health Promotion and Education. National Health Commission of the People’s Republic of China. Available online: http://www.nhfpc.gov.cn/xcs/s7846/201611/05cd17fa96614ea5a9f02bd3f7b44 a25.shtml (accessed on 8 April 2018).
- Kilfoyle, K.A.; Vitko, M.; O’Conor, R.; Bailey, S.C. Health Literacy and Women’s Reproductive Health: A Systematic Review. J. Womens Health 2016, 25, 1237–1255. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.M.; Fraser, S.D.S.; Bradley, J.A.; Bradley, C.; Draper, H.; Metcalfe, W.; Oniscu, G.C.; Tomson, C.R.V.; Ravanan, R.; Roderick, P.J.; et al. A Systematic Review of the Prevalence and Associations of Limited Health Literacy in CKD. Clin. J. Am. Soc. Nephrol. 2017, 12, 1070–1084. [Google Scholar] [CrossRef] [PubMed]
- Shum, J.; Poureslami, I.; Wiebe, D.; Doyle-Waters, MM.; Nimmon, L.; FitzGerald, JM.; Canadian Airways Health Literacy Study Group. Airway diseases and health literacy (HL) measurement tools: A systematic review to inform respiratory research and practice. Patient Educ. Couns. 2018, 101, 596–618. [Google Scholar] [CrossRef] [PubMed]
- Perazzo, J.; Reyes, D.; Webel, A.A. Systematic Review of Health Literacy Interventions for People Living with HIV. AIDS Behav. 2017, 21, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Ogi, H.; Nakamura, D.; Ogawa, M.; Nakamura, T.; Izawa, K.P. Associations between Parents’ Health Literacy and Sleeping Hours in Children: A Cross-Sectional Study. Healthcare 2018, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Mandate for Health Literacy. Available online: http://www.who.int/healthpromotion/conferences/9gchp/health-literacy/en/ (accessed on 3 April 2018).
- World Health Organization. Moving Forward: A Plan for the Next Fifteen Years. Available online: http://www.who.int/healthpromotion/conferences/9gchp/health-literacy-moving-forward/en/ (accessed on 3 April 2018).
- Yang, S.J.; Chee, Y.K. Development and psychometric testing of the Health Literacy Index for Female Marriage Immigrants (HLI-FMI) in Korea. Women Health 2017, 57, 1007–1030. [Google Scholar] [CrossRef] [PubMed]
- Vaart, R.; Drossaert, C. Development of the Digital Health Literacy Instrument: Measuring a Broad Spectrum of Health 1.0 and Health 2.0 Skills. J. Med. Internet Res. 2017, 19, e27. [Google Scholar] [CrossRef] [PubMed]
- Peralta, L.; Rowling, L.; Samdal, O.; Hipkins, R.; Dudley, D. Conceptualising a new approach to adolescent health literacy. Health Educ. J. 2017, 76, 787–801. [Google Scholar] [CrossRef]
- Mounsey, A.; Sexton, B. Health Literacy Tools in the Outpatient Setting. Am. Fam. Physician 2017, 96, 252. [Google Scholar] [PubMed]
- Mafutha, N.G.; Mogotlane, S.; De Swardt, H. Development of a Hypertension Health Literacy Assessment Tool for use in primary healthcare clinics in South Africa, Gauteng. Afr. J. Prim. Health Care Fam. Med. 2017, 9, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Bennett, C.; Khangura, S.; Brehaut, J.C.; Graham, I.D.; Moher, D.; Potter, B.K.; Grimshaw, J.M. Reporting guidelines for survey research: An analysis of published guidance and reporting practices. PLoS Med. 2010, 8, e1001069. [Google Scholar] [CrossRef] [PubMed]
- Rivero-Méndez, M.; Suárez, E.; Solís-Báez, S.S.; Hernández, G.; Cordero, W.; Vázquez, I.; Medina, Z.; Padilla, R.; Flores, A.; Bonilla, J.L.; Holzemer, W.L. Internal consistency of the Spanish health literacy test (TOFHLA-SPR) for Puerto Rico. P. R. Health Sci. J. 2010, 29, 49–53. [Google Scholar] [PubMed]
- Helitzer, D.; Hollis, C.; Sanders, M.; Roybal, S. Addressing the “other” health literacy competencies—Knowledge, dispositions, and oral/aural communication: Development of TALKDOC, an intervention assessment tool. J. Health Commun. 2012, 17 (Suppl. S3), 160–175. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, G.; Khazaezadeh, N.; Oteng-Ntim, E.; Seed, P.; Barr, S.; Weiss, B.D. Development and validation of a measure of health literacy in the UK: The newest vital sign. BMC Public Health 2013, 13, 116. [Google Scholar] [CrossRef] [PubMed]
- Elsworth, G.R.; Beauchamp, A.; Osborne, R.H. Measuring health literacy in community agencies: A Bayesian study of the factor structure and measurement invariance of the health literacy questionnaire (HLQ). BMC Health Serv. Res. 2016, 16, 508. [Google Scholar] [CrossRef] [PubMed]
- Stagliano, V.; Wallace, L.S. Brief health literacy screening items predict newest vital sign scores. JABFM 2013, 26, 558–565. [Google Scholar] [CrossRef] [PubMed]
- Ko, Y.; Lee, J.Y.; Toh, M.P.; Tang, W.E.; Tan, A.S. Development and validation of a general health literacy test in Singapore. Health Promot. Int. 2012, 27, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Fadda, M.; Kanj, M.; Kabakian-Khasholian, T.; Johannes Schulz, P. Validation of three Arabic health literacy assessment tools in Lebanon. Health Promot. Int. 2018, 33, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Gerich, J.; Moosbrugger, R. Subjective Estimation of Health Literacy-What Is Measured by the HLS-EU Scale and How Is It Linked to Empowerment? Health Commun. 2018, 33, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Heide, I.; Uiters, E.; Sørensen, K.; Röthlin, F.; Pelikan, J.; Rademakers, J.; Boshuizen, H.; EPHORT Consortium. Health literacy in Europe: The development and validation of health literacy prediction models. Eur. J. Public Health 2016, 26, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, D.; Berens, E.M.; Vogt, D. Health Literacy in the German Population. Dtsch. Arztebl. Int. 2017, 114, 53–60. [Google Scholar] [PubMed]
- Pleasant, A.; Kuruvilla, S. A tale of two health literacies: Public health and clinical approaches to health literacy. Health Promot. Int. 2008, 23, 152–159. [Google Scholar] [CrossRef] [PubMed]
- McCormack, L.; Bann, C.; Squiers, L.; Berkman, N.D.; Squire, C.; Schillinger, D.; Ohene-Frempong, J.; Hibbard, J. Measuring health literacy: A pilot study of a new skills-based instrument. J. Health Commun. 2010, 15 (Suppl. S2), 51–71. [Google Scholar] [CrossRef]
- Tsai, T.I.; Lee, S.Y.; Tsai, Y.W.; Kuo, K.N. Methodology and validation of health literacy scale development in Taiwan. J. Health Commun. 2011, 16, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Chinn, D.; McCarthy, C. All Aspects of Health Literacy Scale (AAHLS): Developing a tool to measure functional, communicative and critical health literacy in primary healthcare settings. Patient Educ. Couns. 2013, 90, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Jordan, J.E.; Buchbinder, R.; Briggs, A.M.; Elsworth, G.R.; Busija, L.; Batterham, R.; Osborne, R.H. The health literacy management scale (HeLMS): A measure of an individual’s capacity to seek, understand and use health information within the healthcare setting. Patient Educ. Couns. 2013, 91, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Van, D.; Broucke, S.; Pelikan, J.M.; Fullam, J.; Doyle, G.; Slonska, Z.; Kondilis, B.; Stoffels, V.; Osborne, R.H.; et al. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health 2013, 13, 948. [Google Scholar]
- Suka, M.; Odajima, T.; Kasai, M.; Igarashi, A.; Ishikawa, H.; Kusama, M.; Nakayama, T.; Sumitani, M.; Sugimori, H. The 14-item health literacy scale for Japanese adults (HLS-14). Environ. Health Prev. Med. 2013, 18, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Haghdoost, A.A.; Rakhshani, F.; Aarabi, M.; Montazeri, A.; Tavousi, M.; Solimanian, A.; Sarbandi, F.; Namdar, H.; Iranpour, A. Iranian Health Literacy Questionnaire (IHLQ): An Instrument for Measuring Health Literacy in Iran. Iran. Red Crescent Med. J. 2015, 17, e25831. [Google Scholar] [CrossRef]
- O’Connor, M.; Casey, L. The Mental Health Literacy Scale (MHLS): A new scale-based measure of mental health literacy. Psychiatry Res. 2015, 229, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Intarakamhang, U.; Kwanchuen, Y. The development and application of the ABCDE-health literacy scale for Thais. Asian Biomed. 2016, 10, 587–594. [Google Scholar]
- Schrauben, S.J.; Wiebe, D.J. Health literacy assessment in developing countries: A case study in Zambia. Health Promot. Int. 2017, 32, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Pleasant, A.; McKinney, J. Coming to consensus on health literacy measurement: An online discussion and consensus-gauging process. Nurs. Outlook 2011, 59, 95–106. [Google Scholar] [CrossRef] [PubMed]
- Stein, L.; Pettersen, K.S.; Bergdahl, M.; Bergdahl, J. Development and validation of an instrument to assess oral health literacy in Norwegian adult dental patients. Acta Odontol. Scand. 2015, 73, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Jordan, J.E.; Buchbinder, R.; Osborne, R.H. Conceptualising health literacy from the patient perspective. Patient Educ. Couns. 2010, 79, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Yuen, E.Y.; Dodson, S.; Batterham, R.W.; Knight, T.; Chirgwin, J.; Livingston, P.M. Development of a conceptual model of cancer caregiver health literacy. Eur. J. Cancer Care 2016, 25, 294–306. [Google Scholar] [CrossRef] [PubMed]
- Oldfield, S.R.; Dreher, H.M. The concept of health literacy within the older adult population. Holist. Nurs. Pract. 2010, 24, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Altin, S.V.; Finke, I.; Kautz-Freimuth, S.; Stock, S. The evolution of health literacy assessment tools: A systematic review. BMC Public Health 2014, 14, 1207. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, J.M. Assessment and measurement of health literacy: An integrative review of the literature. Nurs. Health Sci. 2009, 11, 77–89. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Scale Names | Nation | Theoretical Basis | Methods | Sample | Domains, Items (#) | Feasibility; Reliability; Validity | Domains |
|---|---|---|---|---|---|---|---|---|
| Measurement modes based on health-related fields | ||||||||
| Pleasant, A., 2008 [32] | The public health literacy knowledge scale | The United States | Thirteen essential Facts for Life messages | Expert consultation; participant feedback; Flesch–Kinkaid readability assessment | 829 public (Mexico = 200, China = 220, Ghana = 204, India = 205) | 13, 17 | 75% response rate; Cronbach’s alpha = 0.797; the public health knowledge scale and the science literacy scale = 0.391 | Timing of births; safe motherhood; child development and early learning; breastfeeding, nutrition and growth; immunization; diarrhea; coughs, colds and more serious illnesses; hygiene; malaria; HIV/AIDS; injury prevention; disasters and emergencies |
| O’Connor, M., 2015 [33] | The mental health literacy scale | Australia | Mental health literacy consists of seven attributes; Diagnostic and Statistical Manual of Mental Disorders IV TR criteria | Developed using an iterative process; a consensus by the clinical panel; feedback | 372 participants | 7, 35 | /; Cronbach’s alpha = 0.797; / | Ability to recognize disorders; knowledge of where to seek information; knowledge of risk factors and causes; knowledge of self-treatment; knowledge of professional help available; attitudes that promote recognition or appropriate help-seeking behavior |
| Measurement modes based on health-related abilities | ||||||||
| Schrauben, S.J., 2017 [34] | Zambia’s health literacy scale | Zambia | The Institute of Medicine’s (IOM) definition of health literacy | Cross-sectional questionnaire; factor analysis methods | 13,646 participants between the ages of 15 and 49 | 4, 15 | /; Cronbach’s alpha = 0.68; good content validity | Capacity to interpret; capacity to obtain; capacity to understand; make appropriate health decisions |
| Jordan, J.E., 2013 [35] | The health literacy management scale | Australia | / | Develop conceptual framework of health literacy (in-depth interviews, concept mapping workshops); cognitive interviews; scale score and test–retest reliability calculation | 542 participants | 8, 29 | 61% response rate; Cronbach’s alpha > 0.82; / | Patient attitudes towards their health; understanding health information; social support; socioeconomic considerations; accessing general medical practitioner (GP) healthcare services; communication with health professionals; being proactive; using health information |
| McCormack, L, 2010 [36] | Health Literacy Skills Instrument | The United States | / | Real-world health-related stimuli (print (prose, document, or quantitative), Internet-based information seeking), cognitive interviews | 1559 Knowledge Network panelists aged 18 or over | 5, 25 | Completion rate = 71%, took 45 min; Cronbach’s alpha = 0.86; item-total correlations of 0.40 or higher item response theory (IRT) discrimination parameters of 1.00 or higher | Identifying and understanding health-related text; interpreting information and/or data in the form of tables, charts, pictures, symbols, maps, and videos; completing computations; making inferences based on the information presented or applying information to a specific scenario; utilizing the Internet/computer to obtain health information |
| Haghdoost, A.A., 2015 [37] | The Iranian Health Literacy Questionnaire | Iran | Priorities in accordance with Iranian health policies and culture sensitivity | Comprehensive review of the literature; expert consultation (health educator, an epidemiologist, and two specialists in oral health and community medicine) | 1080 participants aged 18 to 60 years | 10, 36 | 91% response rate; Cronbach’s alpha = 0.71–0.96; Kaiser–Meyer–Olkin (KMO) = 0.95, Bartlett’s test = 3.017 | Reading/comprehension skills; individual empowerment (first aid skills); communication/decision making skills; assessment skills of health information in virtual media; accurate assessment/judgment skills; social empowerment; individual empowerment (household medical equipment use); health information access; health information use; health knowledge |
| Chinn, D., 2013 [38] | All Aspects of Health Literacy Scale | The UK | Nutbeam’s health literacy theory (functional, communicative, and critical health literacy) | Undertook a review of published research on health literacy definitions and concepts, and on its measurement; drew up a list of potential items; the course of a local consultation exercise | 146 participants | 3, 14 | Took approximately 7 min on average; Cronbach’s alpha = 0.75; functional health literacy and communicative health literacy = 0.393, functional health literacy and critical health literacy = 0.59, communicative health literacy and critical health literacy = 0.186 | Functional health literacy; communicative health literacy; critical health literacy |
| Suka, M., 2013 [39] | The 14-item health literacy scale | Japan | Ishikawa and colleagues’ health literacy scale specific to diabetes patients | Questionnaire | 1507 eligible respondents aged 30–69 years | 3, 14 | 96.4%–99.5% response rate; Cronbach’s alpha = 0.83; Acceptable fit of the three-factor model (comparative fit index = 0.912, normed fit index = 0.905, root mean square error of approximation = 0.082) | Functional health literacy; communicative health literacy; critical health literacy |
| The combination of both measurement modes | ||||||||
| Tsai, T.I., 2011 [40] | The Mandarin Health Literacy Scale | China (Taiwan) | The Institute of Medicine’s definition of health literacy (four kinds of abilities); an individual often encounters six main types of health information and health services in a health care system; three domains of literacy skills | Semi-structured in-depth interviews of health care consumers; consultation with health care, education, and psychometrics experts; generation of an item pool; selection of items for inclusion in the Mandarin Health Literacy Scale; evaluation of readability | 323 Taiwanese adults | 5, 50 | 72.1% response rate; Cronbach’s alpha = 0.97; an item-total correlation equal to or greater than 0.40 | Years of schooling; reading habit; health status; health knowledge; reading assistance |
| Sørensen, K., 2013 [41] | The European Health Literacy Survey Questionnaire | Netherlands | A conceptual model and definition | Item development, pre-testing, field-testing, external consultation, plain language check, and translation from English to Bulgarian, Dutch, German, Greek, Polish, and Spanish | 19 focus group sample, 99 pre-test sample | 12, 47 | Less than 95% response rate took 20–30 min; Cronbach’s alpha = 0.51–0.91; / | The three domains: healthcare; disease prevention; health promotion four-component structure: accessing; understanding; appraising and applying health related information |
| Intarakamhang, U., 2016 [42] | ABCDE (alcohol, baccy, coping, diet, and exercise)-health literacy scale | Thailand | The concepts of ABCDE behavior; the principles of promoting diet, managed exercise, reducing alcohol consumption, and ceasing smoking | Qualitative research methods focused on theoretical publications; expert consultation; focus groups; the causal models for measuring health literacy | 4401 participants aged >15 years | 8, 64 | 97.8% response rate; Cronbach’s alpha = 0.611–0.912; / | Needed health knowledge and understanding; accessing information and services; communicating with professionals; managing their health condition; getting media and information literacy; making appropriate health decisions to good practice; participating in social health literacy; maintaining healthy behavior |
| Reporting Item | Described | Not described | ||
|---|---|---|---|---|
| N | % | N | % | |
| Background | ||||
| Background literature review | 10 | 90.9 | 1 | 9.1 |
| Explicit research question | 9 | 81.8 | 2 | 18.2 |
| Clear study objectives * | 11 | 100 | 0 | 0.0 |
| Methods | ||||
| Description of methods of data analysis * | 11 | 100 | 0 | 0.0 |
| Method of questionnaire administration | 1 | 9.1 | 10 | 90.9 |
| Location of data collection * | 11 | 100 | 0 | 0.0 |
| Dates of data collection | 5 | 45.5 | 6 | 54.5 |
| Description of methods for replication | 9 | 81.8 | 2 | 18.2 |
| Methods for data entry | 2 | 18.2 | 9 | 81.8 |
| Sample selection | ||||
| Sample size calculation | 0 | 0.0 | 11 | 100.0 |
| Representativeness of the sample | 2 | 18.2 | 9 | 81.8 |
| Method of sample selection | 7 | 63.6 | 4 | 36.4 |
| Population and sample frame | 10 | 90.9 | 1 | 9.1 |
| Research tool | ||||
| Description of the research tool * | 11 | 100 | 0 | 0.0 |
| Development of research tool * | 11 | 100 | 0 | 0.0 |
| Instrument pretesting * | 11 | 100 | 0 | 0.0 |
| Instrument reliability and/or validity * | 11 | 100 | 0 | 0.0 |
| Scoring methods | 7 | 63.6 | 4 | 36.4 |
| Results | ||||
| Results of research presented * | 11 | 100 | 0 | 0.0 |
| Results address objectives * | 11 | 100 | 0 | 0.0 |
| Generalizability | 5 | 45.5 | 6 | 54.5 |
| Response rates | ||||
| Response rate stated | 10 | 90.9 | 1 | 9.1 |
| Response rate calculated | 4 | 36.4 | 7 | 63.6 |
| Discussion of nonresponse bias | 3 | 27.3 | 8 | 72.7 |
| Missing data | 4 | 36.4 | 7 | 63.6 |
| Interpretation and discussion | ||||
| Interpret and discuss findings * | 11 | 100 | 0 | 0.0 |
| Conclusions and recommendations * | 11 | 100 | 0 | 0.0 |
| Limitations | 7 | 63.6 | 4 | 36.4 |
| Ethics and disclosure | ||||
| Consent | 6 | 54.5 | 5 | 45.5 |
| Sponsorship | 6 | 54.5 | 5 | 45.5 |
| Mean reporting frequency | 66.3 | 33.7 | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.; Zeng, H.; Shen, Y.; Zhang, F.; Sharma, M.; Lai, W.; Zhao, Y.; Tao, G.; Yuan, J.; Zhao, Y. Assessment Tools for Health Literacy among the General Population: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 1711. https://doi.org/10.3390/ijerph15081711
Liu H, Zeng H, Shen Y, Zhang F, Sharma M, Lai W, Zhao Y, Tao G, Yuan J, Zhao Y. Assessment Tools for Health Literacy among the General Population: A Systematic Review. International Journal of Environmental Research and Public Health. 2018; 15(8):1711. https://doi.org/10.3390/ijerph15081711
Chicago/Turabian StyleLiu, Hongyan, Huan Zeng, Yang Shen, Fan Zhang, Manoj Sharma, Weiyun Lai, Yu Zhao, Genhui Tao, Jun Yuan, and Yong Zhao. 2018. "Assessment Tools for Health Literacy among the General Population: A Systematic Review" International Journal of Environmental Research and Public Health 15, no. 8: 1711. https://doi.org/10.3390/ijerph15081711
APA StyleLiu, H., Zeng, H., Shen, Y., Zhang, F., Sharma, M., Lai, W., Zhao, Y., Tao, G., Yuan, J., & Zhao, Y. (2018). Assessment Tools for Health Literacy among the General Population: A Systematic Review. International Journal of Environmental Research and Public Health, 15(8), 1711. https://doi.org/10.3390/ijerph15081711






