Association of Self-Perceived Oral Health and Function with Clinically Determined Oral Health Status among Adults Aged 35–54 Years: A Cross-Sectional Study
Abstract
:1. Introduction
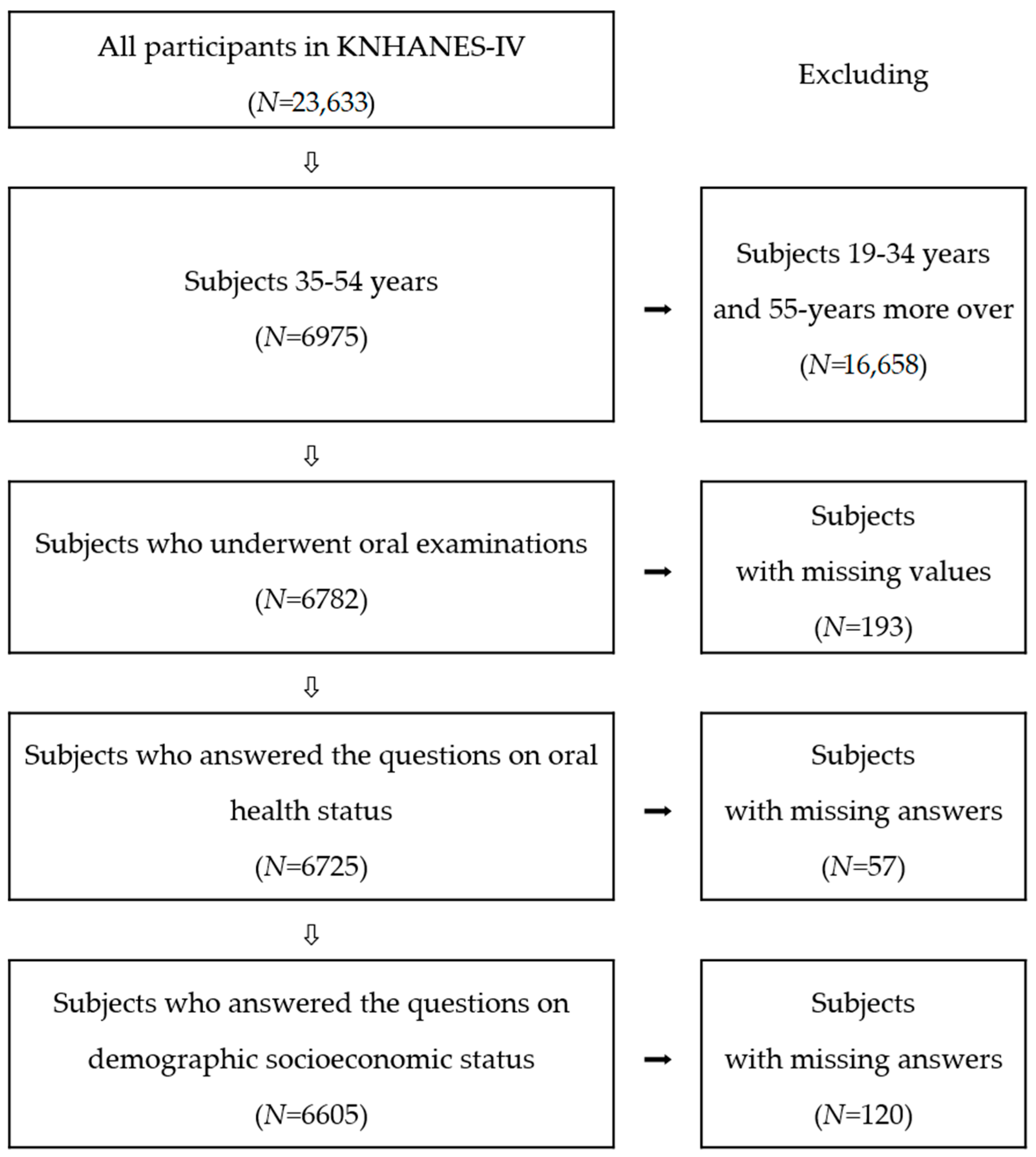
2. Materials and Methods
2.1. Data Sources
2.2. Variables
2.3. Statistical Analysis
2.4. Ethics Approval and Consent to Participate
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Petersen, P.E. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century—The approach of the WHO Global Oral Health Programme. Commun. Dent. Oral Epidemiol. 2003, 31, 3–23. [Google Scholar] [CrossRef]
- Griffin, S.O.; Jones, J.A.; Brunson, D.; Griffin, P.M.; Bailey, W.D. Burden of oral disease among older adults and implications for public health priorities. Am. J. Public Health 2012, 102, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Medina-Solís, C.E.; Pontigo-Loyola, A.P.; Pérez-Campos, E.; Hernández-Cruz, P.; De la Rosa-Santillana, R.; Navarete-Hernández Jde, J.; Maupomé, G. Principal reasons for extraction of permanent tooth in a sample of Mexicans adults. Rev. Invest. Clin. 2013, 65, 141–149. [Google Scholar] [PubMed]
- Shigli, K.; Hebbal, M.; Angadi, G.S. Relative contribution of caries and periodontal disease in adult tooth loss among patients reporting to the Institute of Dental Sciences, Belgaum, India. Gerodontology 2009, 26, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Castrejón-Pérez, R.C.; Borges-Yáñez, S.A.; Gutiérrez-Robledo, L.M.; Ávila-Funes, J.A. Oral health conditions and frailty in Mexican community-dwelling elderly: A cross sectional analysis. BMC Public Health 2012, 12, 773. [Google Scholar] [CrossRef] [PubMed]
- Walls, A.; Steele, J. The relationship between oral health and nutrition in older people. Mech. Ageing Dev. 2004, 125, 853–857. [Google Scholar] [CrossRef] [PubMed]
- Emami, E.; de Souza, R.F.; Kabawat, M.; Feine, J.S. The impact of edentulism on oral and general health. Int. J. Dent. 2013, 2013, 498305. [Google Scholar] [CrossRef] [PubMed]
- Fontijn-Tekamp, F.; Slagter, A.; Van Der Bilt, A.; Van’T Hof, M.; Witter, D.; Kalk, W.; Jansen, J.A. Biting and chewing in overdentures, full dentures, and natural dentitions. J. Dent. Res. 2000, 79, 1519–1524. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Divaris, K.; Baker, A.D.; Rozier, R.G.; Vann Jr, W.F. The relationship of oral health literacy and self-efficacy with oral health status and dental neglect. Am. J. Public Health 2012, 102, 923–929. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Logan, H.L.; Dodd, V.J.; Muller, K.E.; Marks, J.G.; Riley III, J.L. Health literacy: A pathway to better oral health. Am. J. Public Health 2014, 104, e85–e91. [Google Scholar] [CrossRef] [PubMed]
- Watt, R.G. Social determinants of oral health inequalities: Implications for action. Commun. Dent. Oral Epidemiol. 2012, 40, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Pattussi, M.P.; Peres, K.G.; Boing, A.F.; Peres, M.A.; Da Costa, J.S.D. Self-rated oral health and associated factors in Brazilian elders. Commun. Dent. Oral Epidemiol. 2010, 38, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Parker, E.; Jamieson, L. Access, literacy and behavioural correlates of poor self-rated oral health amongst an Indigenous South Australian population. Commun. Dent. Health 2014, 31, 167–171. [Google Scholar]
- Matthias, R.E.; Atchison, K.A.; Schweitzer, S.O.; Lubben, J.E.; Mayer-Oakes, A.; Jong, F.D. Comparisons between dentist ratings and self-ratings of dental appearance in an elderly population. Spec. Care Dentist. 1993, 13, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Atchison, K.A.; Matthias, R.E.; Dolan, T.A.; Lubben, J.E.; Jong, F.; Schweitzer, S.O.; Mayer-Oakes, S.A. Comparison of oral health ratings by dentists and dentate elders. J. Public Health Dent. 1993, 53, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.N.; Kwon, H.K.; Chung, W.G.; Cho, Y.S.; Choi, Y.H. The association of perceived oral health with oral epidemiological indicators in Korean adults. J. Korean Acad. Dent. Health 2005, 29, 250–260. [Google Scholar]
- Kim, J.H.; Lee, M.H. Comparative analysis of self-perceived oral health and actual oral examination. J. Koeran Dent. Hyg. 2011, 13, 311–323. [Google Scholar]
- Gotfredsen, K.; Walls, A.W. What dentition assures oral function? Clin. Oral Implants Res. 2008, 19, 326–328. [Google Scholar]
- Kim, H.N.; Ha, T.G.; Kim, M.J.; Jun, E.J.; Jeong, S.H.; Kim, J.B. Factors related to number of present teeth in Korean elderly adults aged 55–84 years. Int. J. Dent. Hyg. 2016, 14, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Dembowska, E.; Jakubowska-Kocór, U.; Samulak-Zielińska, R.; Sosińska, K.; Czuryszkiewicz-Cyranal, J.; Suwała, M. Periodontal status of Szczecin citizens aged 35–44 years according to the Community Periodontal Index. Pomeranian J. Life Sci. 2015, 61, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Korea Center for Disease Control and Prevention. Korean National Health and Examination Surveys: The 4th Surveys; Korea Center for Disease Control and Prevention: Cheongwongun, Korea, 2008. [Google Scholar]
- Korea Center for Disease Control and Prevention. Standardization for Oral Health Survey in KNHANES (2009); Korea Center for Disease Control and Prevention: Cheongwongun, Korea, 2010. [Google Scholar]
- Kojima, A.; Ekuni, D.; Mizutani, S.; Furuta, M.; Irie, K.; Azuma, T.; Tomofuji, T.; Iwasaki, Y.; Morita, M. Relationships between self-rated oral health, subjective symptoms, oral health behavior and clinical conditions in Japanese university students: A cross-sectional survey at Okayama University. BMC Oral Health 2013, 13, 62. [Google Scholar] [CrossRef] [PubMed]
- Olusile, A.O.; Adeniyi, A.A.; Orebanjo, O. Self-rated oral health status, oral health service utilization, and oral hygiene practices among adult Nigerians. BMC Oral Health 2014, 14, 140. [Google Scholar] [CrossRef] [PubMed]
- Bordin, D.; Fadel, CB.; Santos, C.B.D.; Garbin, C.A.S.; Moimaz, S.A.S.; Saliba, N.A. Determinants of oral self-care in the Brazilian adult population: a national cross-sectional study. Braz. Oral Res. 2017, 31, e115. [Google Scholar] [CrossRef] [PubMed]
- Marcenes, W.; Kassebaum, N.J.; Bernabé, E.; Flaxman, A.; Naghavi, M.; Lopez, A.; Murray, C.J. Global burden of oral conditions in 1990–2010: A systematic analysis. J. Dent. Res. 2013, 92, 592–597. [Google Scholar] [CrossRef] [PubMed]
- N Gom, P.I.; Woda, A. Influence of impaired mastication on nutrition. J. Prosthet. Dent. 2002, 87, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Gift, H.; Atchison, K.; Drury, T. Perceptions of the natural dentition in the context of multiple variables. J. Dent. Res. 1998, 77, 1529–1538. [Google Scholar] [CrossRef] [PubMed]
- Watt, R.; Sheiham, A. Inequalities in oral health: A review of the evidence and recommendations for action. Br. Dent. J. 1999, 187, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Locker, D. Deprivation and oral health: A review. Commun. Dent. Oral Epidemiol. 2000, 28, 161–169. [Google Scholar] [CrossRef]
- Guarnizo-Herreño, C.C.; Watt, R.G.; Fuller, E.; Steele, J.G.; Shen, J.; Morris, S.; Wildman, J.; Tsakos, G. Socioeconomic position and subjective oral health: Findings for the adult population in England, Wales and Northern Ireland. BMC Public Health 2014, 14, 827. [Google Scholar] [CrossRef] [PubMed]
- Locker, D.; Miller, Y. Evaluation of subjective oral health status indicators. J. Public Health Dent. 1994, 54, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Blizniuk, A.; Ueno, M.; Zaitsu, T.; Kawaguchi, Y. Association between self-reported and clinical oral health status in Belarusian adults. J. Investig. Clin. Dent. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H.; Kim, H.D.; Han, D.H.; Jin, B.H.; Paik, D.I. Relationship between perceived oral symptoms and perceived oral health status among the elderly in welfare institutions in Seoul. J. Korean Acad. Dent. Health 2006, 30, 141–150. [Google Scholar]
- Jang, Y.J.; Kim, N.S. Relationship of oral health behavior to subjective oral health status and the DMFT index in Korean adults. J. Korean Soc. Dent. Hyg. 2011, 11, 499–509. [Google Scholar]
| Age Group (Years) | Total | Men | Women | ||
|---|---|---|---|---|---|
| N | Estimate % | N | Estimate % | ||
| All | 6605 | 2828 | 50.9 | 3777 | 49.1 |
| 35–44 | 3467 | 1487 | 51.2 | 1980 | 48.8 |
| 45–54 | 3138 | 1341 | 50.6 | 1797 | 49.4 |
| Variables | Very Good/Very CFT † | Good/CFT † | Fair | Poor/UnCFT ‡ | Very Poor/Very UnCFT ‡ | p-Value * |
|---|---|---|---|---|---|---|
| Self-perceived oral health | ||||||
| Sex | <0.001 | |||||
| Men | 1.2 | 12.2 | 37.9 | 39.2 | 9.6 | |
| Women | 0.5 | 10.8 | 41.7 | 40.3 | 6.7 | |
| Age group (years) | <0.001 | |||||
| 35–44 | 0.7 | 10.7 | 42.5 | 38.7 | 7.4 | |
| 45–54 | 1.0 | 12.3 | 36.8 | 40.8 | 9.1 | |
| Education | <0.001 | |||||
| ≤Junior high school | 0.8 | 10.5 | 35.3 | 42.4 | 11.1 | |
| High school | 0.8 | 10.2 | 41.9 | 39.4 | 7.8 | |
| ≥College | 1.0 | 14.0 | 40.2 | 38.2 | 6.7 | |
| Household income § | 0.003 | |||||
| Low | 1.6 | 10.5 | 36.1 | 41.4 | 10.4 | |
| Middle | 0.7 | 10.9 | 39.4 | 40.0 | 9.1 | |
| High | 0.8 | 12.7 | 41.2 | 38.9 | 6.4 | |
| Chewing ability | ||||||
| Sex | 0.142 | |||||
| Men | 31.4 | 24.1 | 17.8 | 21.5 | 5.3 | |
| Women | 33.0 | 25.5 | 17.6 | 19.4 | 4.5 | |
| Age group (years) | <0.001 | |||||
| 35–44 | 35.1 | 27.5 | 18.0 | 16.8 | 2.6 | |
| 45–54 | 29.0 | 21.9 | 17.3 | 24.5 | 7.4 | |
| Education | <0.001 | |||||
| ≤Junior high school | 27.0 | 18.6 | 16.3 | 27.7 | 10.4 | |
| High school | 33.1 | 25.3 | 18.3 | 19.8 | 3.5 | |
| ≥College | 34.6 | 28.5 | 17.9 | 16.2 | 2.8 | |
| Household income § | <0.001 | |||||
| Low | 28.9 | 18.5 | 19.1 | 23.6 | 10.0 | |
| Middle | 31.2 | 23.0 | 18.3 | 22.1 | 5.4 | |
| High | 34.4 | 29.0 | 16.4 | 17.2 | 3.0 | |
| Speaking ability | ||||||
| Sex | 0.116 | |||||
| Men | 64.6 | 21.6 | 7.9 | 4.9 | 1.0 | |
| Women | 66.4 | 19.3 | 7.5 | 6.0 | 0.9 | |
| Age group (years) | <0.001 | |||||
| 35–44 | 70.9 | 18.8 | 6.0 | 3.8 | 0.5 | |
| 45–54 | 59.6 | 22.2 | 9.5 | 7.2 | 1.4 | |
| Education | <0.001 | |||||
| ≤Junior high school | 54.8 | 23.3 | 10.1 | 9.3 | 2.6 | |
| High school | 66.5 | 19.6 | 7.8 | 5.6 | 0.5 | |
| ≥College | 71.8 | 19.4 | 5.9 | 2.5 | 0.3 | |
| Household income § | <0.001 | |||||
| Low | 56.5 | 19.5 | 9.6 | 11.4 | 2.9 | |
| Middle | 64.3 | 20.8 | 8.2 | 5.7 | 1.0 | |
| High | 69.3 | 20.1 | 6.5 | 3.8 | 0.4 | |
| Variables | DT † | DMFT ‡ | Prosthesis Scores (0–10) § | Periodontal Scores (0–4) ∥ | p-Value * | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | ||
| Self-perceived oral health | <0.001 | ||||||||
| Very good | 0.32 a | 0.10 | 2.55 a | 0.50 | 0.15 a | 0.07 | 0.93 a | 0.11 | |
| Good | 0.40 a | 0.04 | 3.48 a | 0.15 | 0.38 b | 0.04 | 0.88 a | 0.04 | |
| Fair | 0.52 b | 0.03 | 4.98 b | 0.09 | 0.43 b | 0.02 | 0.95 a | 0.03 | |
| Poor | 0.83 c | 0.04 | 6.16 c | 0.09 | 0.82 c | 0.03 | 1.21 b | 0.03 | |
| Very poor | 1.70 d | 0.12 | 7.43 d | 0.23 | 1.32 d | 0.09 | 1.63 c | 0.05 | |
| Chewing ability | <0.001 | ||||||||
| Very comfortable | 0.52 a | 0.03 | 4.51 a | 0.09 | 0.40 a | 0.02 | 0.97 a | 0.03 | |
| Comfortable | 0.60 a | 0.04 | 5.62 b | 0.12 | 0.60 b | 0.03 | 0.96 a | 0.03 | |
| Fair | 0.71 a | 0.04 | 5.75 b | 0.12 | 0.63 b | 0.04 | 1.07 b | 0.03 | |
| Uncomfortable | 0.98 b | 0.05 | 6.21 c | 0.13 | 0.96 c | 0.05 | 1.34 c | 0.03 | |
| Very uncomfortable | 1.65 c | 0.14 | 6.59 c | 0.28 | 1.25 d | 0.11 | 1.75 d | 0.08 | |
| Speaking ability | <0.001 | ||||||||
| Very comfortable | 0.64 a | 0.02 | 5.17 a | 0.07 | 0.47 a | 0.02 | 1.03 a | 0.02 | |
| Comfortable | 0.86 b | 0.05 | 5.80 b | 0.13 | 0.79 b | 0.04 | 1.18 b | 0.04 | |
| Fair | 0.81 b | 0.07 | 6.03 b | 0.19 | 1.13 c | 0.09 | 1.22 b | 0.05 | |
| Uncomfortable | 0.95 b | 0.11 | 6.59 b | 0.29 | 1.40 c | 0.12 | 1.39 c | 0.07 | |
| Very uncomfortable | 1.47 b | 0.27 | 6.55 b | 0.73 | 1.54 c | 0.31 | 1.86 d | 0.19 | |
| Age Group (Years) | Self-Perceived Oral Health * (p § = 0.004) | Self-Perceived Oral Functions† | Self-Perceived Oral Health Status and Oral Functions ‡ (p § < 0.001) | |||||
|---|---|---|---|---|---|---|---|---|
| Chewing Ability (p § < 0.001) | Speaking Ability (p § < 0.001) | |||||||
| M ∥ | SE | M ∥ | SE | M ∥ | SE | M ∥ | SE | |
| All | 3.43 | 0.01 | 2.41 | 0.02 | 1.56 | 0.01 | 7.73 | 0.07 |
| 35–44 | 3.46 | 0.02 | 2.30 | 0.02 | 1.49 | 0.02 | 7.33 | 0.08 |
| 45–54 | 3.40 | 0.02 | 2.54 | 0.03 | 1.64 | 0.02 | 8.15 | 0.10 |
| Variables | Self-Perceived Oral Health Status and Subjective Oral Functions * | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 (R2 = 0.127) | Model 2 (R2 = 0.136) a | Model 3 (R2 = 0.148) b | |||||||
| B | SE | p† | B | SE | p† | B | SE | p† | |
| (intercept) | 5.309 | 0.13 | <0.001 | 1.684 | 0.51 | 0.001 | 5.038 | 0.66 | <0.001 |
| Age | 0.086 | 0.01 | <0.001 | 0.064 | 0.01 | <0.001 | |||
| Sex ‡ | −0.048 | 0.13 | 0.701 | −0.245 | 0.13 | 0.058 | |||
| Household income § | −0.521 | 0.11 | <0.001 | ||||||
| Education ∥ | −0.492 | 0.10 | <0.001 | ||||||
| DT ¶ | 0.424 | 0.05 | <0.001 | 0.452 | 0.05 | <0.001 | 0.405 | 0.05 | <0.001 |
| DMFT ** | 0.110 | 0.02 | <0.001 | 0.112 | 0.02 | <0.001 | 0.126 | 0.02 | <0.001 |
| Prosthesis scores (0–10) *** | 0.822 | 0.07 | <0.001 | 0.731 | 0.07 | <0.001 | 0.691 | 0.07 | <0.001 |
| Mean periodontal scores (0-4) **** | 0.883 | 0.09 | <0.001 | 0.783 | 0.09 | <0.001 | 0.700 | 0.09 | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-Y.; Kim, J.-E.; Kim, H.-N.; Jun, E.-J.; Lee, J.-H.; Kim, J.-S.; Kim, J.-B. Association of Self-Perceived Oral Health and Function with Clinically Determined Oral Health Status among Adults Aged 35–54 Years: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2018, 15, 1681. https://doi.org/10.3390/ijerph15081681
Kim S-Y, Kim J-E, Kim H-N, Jun E-J, Lee J-H, Kim J-S, Kim J-B. Association of Self-Perceived Oral Health and Function with Clinically Determined Oral Health Status among Adults Aged 35–54 Years: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2018; 15(8):1681. https://doi.org/10.3390/ijerph15081681
Chicago/Turabian StyleKim, Se-Yeon, Ji-Eun Kim, Han-Na Kim, Eun-Joo Jun, Jung-Ha Lee, Ji-Soo Kim, and Jin-Bom Kim. 2018. "Association of Self-Perceived Oral Health and Function with Clinically Determined Oral Health Status among Adults Aged 35–54 Years: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 15, no. 8: 1681. https://doi.org/10.3390/ijerph15081681
APA StyleKim, S.-Y., Kim, J.-E., Kim, H.-N., Jun, E.-J., Lee, J.-H., Kim, J.-S., & Kim, J.-B. (2018). Association of Self-Perceived Oral Health and Function with Clinically Determined Oral Health Status among Adults Aged 35–54 Years: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 15(8), 1681. https://doi.org/10.3390/ijerph15081681





