Perinatal Mortality in South Asia: Systematic Review of Observational Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Outcome Measure
2.2. Search Strategy
- [“perinatal mortality*” or “Perinatal death*”]
- AND
- [risk* or “risk factor*” or predictor* or determinant* or socioeconomic* or sociodemographic* or factor*]
- AND
- [“South Asia*” or “Southern Asia*” or Afghan* or Bangladesh* or Bhutan* or India* or Maldives or Nepal* or Pakistan* or Sri Lanka*]
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Quality Assessment
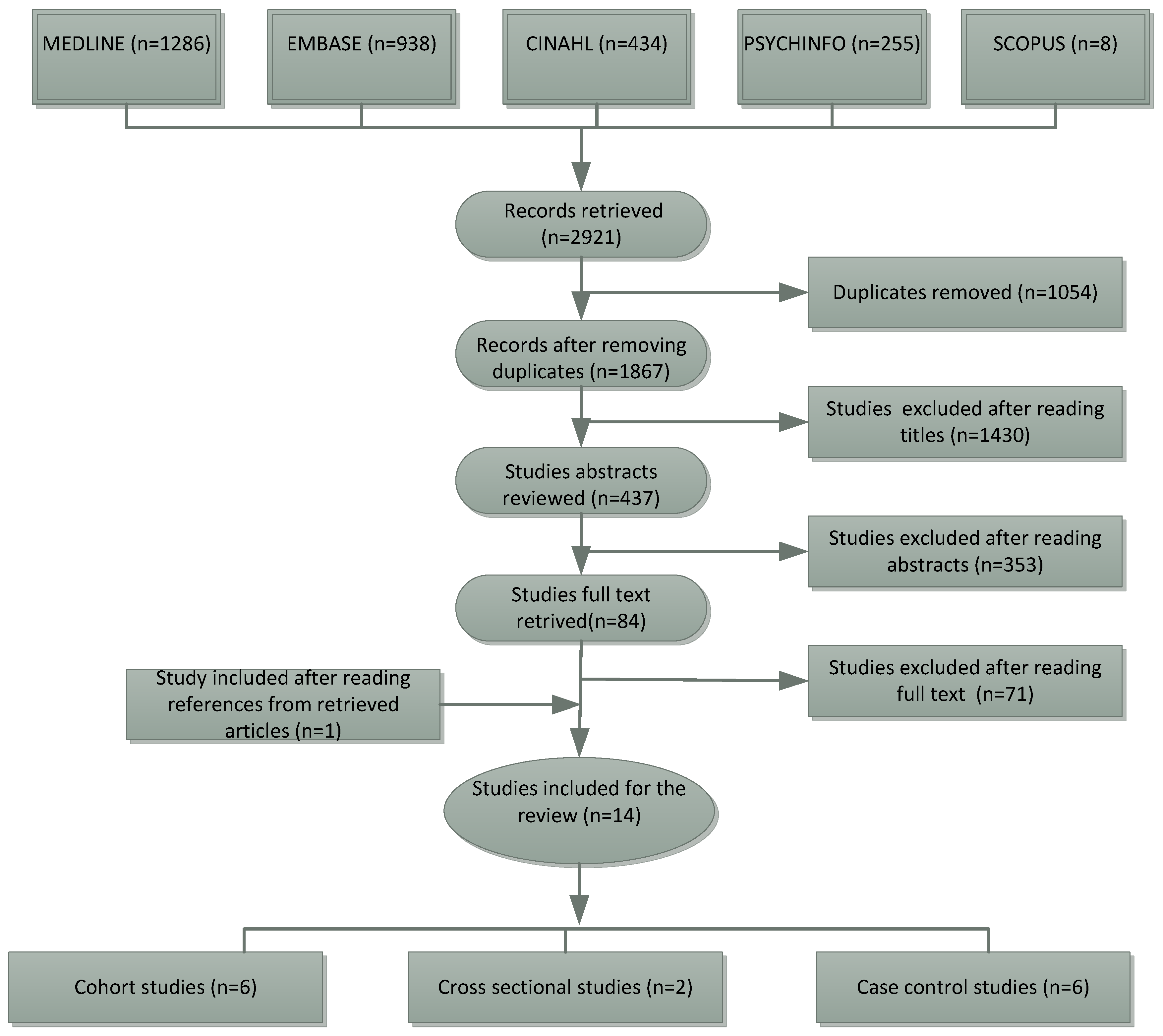
3. Results
3.1. Characteristics of Selected Studies
3.2. Summary of Reviewed Studies
4. Discussion
4.1. Strengths and Limitations
4.2. Policy Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Neonatal and Perinatal Mortality: Country, Regional and Global Estimates; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Opportunities for Africas Newborns: Practical Data Policy and Programmatic Support for Newborn Care in Africa. Available online: http://www.who.int/pmnch/media/publications/oanfullreport.pdf (accessed on 3 July 2017).
- Paul, V.K.; Sachdev, H.S.; Mavalankar, D.; Ramachandran, P.; Sankar, M.J.; Bhandari, N.; Sreenivas, V.; Sundararaman, T.; Govil, D.; Osrin, D.; et al. Reproductive health, and child health and nutrition in India: Meeting the challenge. Lancet 2011, 377, 332–349. [Google Scholar] [CrossRef]
- Fink, G.; Günther, I.; Hill, K. The effect of water and sanitation on child health: Evidence from the demographic and health surveys 1986–2007. Int. J. Epidemiol. 2011, 40, 1196–1204. [Google Scholar] [CrossRef] [PubMed]
- Lehtonen, L.; Gimeno, A.; Parra-Llorca, A.; Vento, M. Early neonatal death: A challenge worldwide. Semin. Fetal Neonatal Med. 2017, 22, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Mason, E.; McDougall, L.; Lawn, J.E.; Gupta, A.; Claeson, M.; Pillay, Y.; Presern, C.; Lukong, M.B.; Mann, G.; Wijnroks, M. From evidence to action to deliver a healthy start for the next generation. Lancet 2014, 384, 455–467. [Google Scholar] [CrossRef]
- Shah, R.; Sharma, B.; Khanal, V.; Pandey, U.K.; Vishwokarma, A.; Malla, D.K. Factors associated with neonatal deaths in Chitwan district of Nepal. BMC Res. Notes 2015, 8, 818. [Google Scholar] [CrossRef] [PubMed]
- Lawn, J.E.; Cousens, S.; Zupan, J. Lancet Neonatal Survival Steering Team. 4 million neonatal deaths: When? Where? Why? Lancet 2005, 365, 891–900. [Google Scholar] [CrossRef]
- Wang, H.; Bhutta, Z.A.; Coates, M.M.; Coggeshall, M.; Dandona, L.; Diallo, K.; Franca, E.B.; Fraser, M.; Fullman, N.; Gething, P.W. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1725–1774. [Google Scholar] [CrossRef]
- United Nations Inter-Agency Group for Child Mortality Estimation (UN IGME). Levels & Trends in Child Mortality: Report 2017, Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation; United Nations Children’s Fund: New York, NY, USA, 2017. [Google Scholar]
- Hogan, M.C.; Foreman, K.J.; Naghavi, M.; Ahn, S.Y.; Wang, M.; Makela, S.M.; Lopez, A.D.; Lozano, R.; Murray, C.J.L. Maternal mortality for 181 countries, 1980–2008: A systematic analysis of progress towards Millennium Development Goal 5. Lancet 2010, 375, 1609–1623. [Google Scholar] [CrossRef]
- Lawn, J.E.; Blencowe, H.; Waiswa, P.; Amouzou, A.; Mathers, C.; Hogan, D.; Flenady, V.; Frøen, J.F.; Qureshi, Z.U.; Calderwood, C.; et al. Stillbirths: Rates, risk factors, and acceleration towards 2030. Lancet 2016, 387, 587–603. [Google Scholar] [CrossRef]
- Darmstadt, G.L.; Kinney, M.V.; Chopra, M.; Cousens, S.; Kak, L.; Paul, V.K.; Martines, J.; Bhutta, Z.A.; Lawn, J.E. The Lancet Every Newborn Study Group. Who has been caring for the baby? Lancet 2014, 384, 174–188. [Google Scholar] [CrossRef]
- Lawn, J.E.; Blencowe, H.; Oza, S.; You, D.; Lee, A.C.; Waiswa, P.; Lalli, M.; Bhutta, Z.; Barros, A.J.; Christian, P.; et al. Every Newborn: Progress, priorities, and potential beyond survival. Lancet 2014, 384, 189–205. [Google Scholar] [CrossRef]
- World Halth Organization. Every Newborn: An Action Plan to End Preventable Deaths; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Kusiako, T.; Ronsmans, C.; Van der Paal, L. Perinatal mortality attributable to complications of childbirth in Matlab, Bangladesh. Bull. World Health Organ. 2000, 78, 621–627. [Google Scholar] [PubMed]
- Ahmed, S.; Koenig, M.A.; Stephenson, R. Effects of domestic violence on perinatal and early-childhood mortality: Evidence from north India. Am. J. Public Health 2006, 96, 1423–1428. [Google Scholar] [CrossRef] [PubMed]
- Shah, D.; Shroff, S.; Ganla, K. Factors affecting perinatal mortality in India (perinatal audit). Prenat. Neonatal Med. 2000, 5, 288–302. [Google Scholar]
- Khan, M.N.; Rahman, M.M.; Shariff, A.A.; Rahman, M.M.; Rahman, M.S.; Rahman, M.A. Maternal undernutrition and excessive body weight and risk of birth and health outcomes. Arch. Public Health 2017, 75, 12. [Google Scholar] [CrossRef] [PubMed]
- Tarique, A.; Khan, M.; Ahmed, L. Perinatal Mortality (PNM): A discussion of social myths, socioeconomic taboos and psychosocial stress. Med. Channel 2013, 19, 8–12. [Google Scholar]
- Bhutta, Z.A.; Das, J.K.; Bahl, R.; Lawn, J.E.; Salam, R.A.; Paul, V.K.; Sankar, M.J.; Blencowe, H.; Rizvi, A.; Chou, V.B. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014, 384, 347–370. [Google Scholar] [CrossRef]
- World Health Organization. WHO Recommended Interventions for Improving Maternal and Newborn Health: Integrated Management of Pregnancy and Childbirth; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Perveen, S.; Soomro, T.K. Sideropaenic anaemia: Impact on perinatal outcome at tertiary care hospital. J. Pak. Med. Assoc. 2016, 66, 952–956. [Google Scholar] [PubMed]
- Rahman, M.M.; Abe, S.K.; Rahman, M.S.; Kanda, M.; Narita, S.; Bilano, V.; Ota, E.; Gilmour, S.; Shibuya, K. Maternal anemia and risk of adverse birth and health outcomes in low-and middle-income countries: Systematic review and meta-analysis. Am. J. Clin. Nutr. 2016, 103, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Chinkhumba, J.; De Allegri, M.; Muula, A.S.; Robberstad, B. Maternal and perinatal mortality by place of delivery in sub-Saharan Africa: A meta-analysis of population-based cohort studies. BMC Public Health 2014, 14, 1014. [Google Scholar] [CrossRef] [PubMed]
- Merali, H.S.; Lipsitz, S.; Hevelone, N.; Gawande, A.A.; Lashoher, A.; Agrawal, P.; Spector, J. Audit-identified avoidable factors in maternal and perinatal deaths in low resource settings: A systematic review. BMC Pregnancy Childbirth 2014, 14, 280. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- United Nations International Children’s Fund. The State of the World’s Children 2014 in Numbers: Every Child Counts. Revealing Disparities, Advancing Children’s Rights; United Nations International Children’s Fund: New York, NY, USA, 2014. [Google Scholar]
- Bari, W.; Chowdhury, R.I.; Islam, M.; Chakraborty, N.; Akhter, H. The differentials and determinants of perinatal mortality in rural Bangladesh. Eur. J. Contracept. Reprod. Health Care 2002, 7, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Guidotti, R.J.; Kandasamy, T.; Betrán, A.P.; Merialdi, M.; Hakimi, F.; Van Look, P.; Kakar, F. Monitoring perinatal outcomes in hospitals in Kabul, Afghanistan: The first step of a quality assurance process. J. Matern. Fetal Neonatal Med. 2009, 22, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.; Majid, A.; Khan, H.A.; Muhammad, Z. Perinatal mortality and its related obstetrics risk factors. J. Med. Sci. 2014, 22, 76–79. [Google Scholar]
- Sachar, R.; Soni, R. Brief report. Perinatal mortality in rural Punjab—A population based study. J. Trop. Pediatr. 2000, 46, 43–45. [Google Scholar] [CrossRef] [PubMed]
- Shabbir, S.; Zahid, M.; Qazi, A. To detect outcome of pregnancy in advanced maternal age among Pakistani women. Pak. J. Med. Sci. 2014, 1, 709–712. [Google Scholar]
- Siddalingappa, H.; Nrayana Murthy, M.; Kulkarni, P.; Ashok, N. Prevalence and factors influencing perinatal mortality in rural Mysore, India. J. Clin. Diagn. Res. 2013, 7, 2796. [Google Scholar] [CrossRef] [PubMed]
- Wassan, K.; Rani, S.; Haider, G. Perinatal mortality-A hazardous dilemma. Rawal Med. J. 2009, 34, 195–198. [Google Scholar]
- Khanam, R.; Ahmed, S.; Creanga, A.A.; Begum, N.; Koffi, A.K.; Mahmud, A.; Rosen, H.; Baqui, A.H. Antepartum complications and perinatal mortality in rural Bangladesh. BMC Pregnancy Childbirth 2017, 17, 81. [Google Scholar] [CrossRef] [PubMed]
- Short, V.L.; Geller, S.E.; Moore, J.L.; McClure, E.M.; Goudar, S.S.; Dhaded, S.M.; Kodkany, B.S.; Saleem, S.; Naqvi, F.; Pasha, O.; et al. The Relationship between Body Mass Index in Pregnancy and Adverse Maternal, Perinatal, and Neonatal Outcomes in Rural India and Pakistan. Am. J. Perinatol. 2018. [Google Scholar] [CrossRef]
- Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 13 January 2018).
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- McDermott, J.; Steketee, R.; Wirima, J. Perinatal mortality in rural Malawi. Bull. World Health Organ. 1996, 74, 165–171. [Google Scholar] [PubMed]
- Nkwo, P.O.; Lawani, L.O.; Ezugwu, E.C.; Iyoke, C.A.; Ubesie, A.C.; Onoh, R.C. Correlates of poor perinatal outcomes in non-hospital births in the context of weak health system: The Nigerian experience. BMC Pregnancy Childbirth 2014, 14, 341. [Google Scholar] [CrossRef] [PubMed]
- Flenady, V.; Koopmans, L.; Middleton, P.; Frøen, J.F.; Smith, G.C.; Gibbons, K.; Coory, M.; Gordon, A.; Ellwood, D.; McIntyre, H.D. Major risk factors for stillbirth in high-income countries: A systematic review and meta-analysis. Lancet 2011, 377, 1331–1340. [Google Scholar] [CrossRef]
- Pal, S. Impact of hospital delivery on child mortality: An analysis of adolescent mothers in Bangladesh. Soc. Sci. Med. 2015, 143, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.; Raynes-Greenow, C.; McGeechan, K.; Morris, J.; Jeffery, H. Risk factors for antepartum stillbirth and the influence of maternal age in New South Wales Australia: A population based study. BMC Pregnancy Childbirth 2013, 13, 12. [Google Scholar] [CrossRef] [PubMed]
- Karkee, R.; Lee, A.H.; Khanal, V. Need factors for utilisation of institutional delivery services in Nepal: An analysis from Nepal Demographic and Health Survey, 2011. BMJ Open 2014, 4, e004372. [Google Scholar] [CrossRef] [PubMed]
- Joshi, C.; Torvaldsen, S.; Hodgson, R.; Hayen, A. Factors associated with the use and quality of antenatal care in Nepal: A population-based study using the demographic and health survey data. BMC Pregnancy Childbirth 2014, 14, 94. [Google Scholar] [CrossRef] [PubMed]
- Jehan, K.; Sidney, K.; Smith, H.; de Costa, A. Improving access to maternity services: An overview of cash transfer and voucher schemes in South Asia. Repord. Health Matters 2012, 20, 142–154. [Google Scholar] [CrossRef]
- Shah, N.M.; Shah, M.A.; Khalaf, A.A.; Mustafa, M.M.; Al-Sayed, A. Searching for socioeconomic risk factors in perinatal mortality in Kuwait: A case control study. Soc. Sci. Med. 2000, 51, 539–550. [Google Scholar] [CrossRef]
- Haththotuwa, R.; Senanayake, L.; Senarath, U.; Attygalle, D. Models of care that have reduced maternal mortality and morbidity in Sri Lanka. Int. J. Gynaecol. Obstet. 2012, 119, S45–S49. [Google Scholar] [CrossRef] [PubMed]
- Lawn, J.E.; Kerber, K.; Enweronu-Laryea, C.; Cousens, S. 3.6 Million Neonatal Deaths—What Is Progressing and What Is Not? Semin. Perinatol. 2010, 34, 371–386. [CrossRef] [PubMed]
- Lawn, J.E.; Blencowe, H.; Pattinson, R.; Cousens, S.; Kumar, R.; Ibiebele, I.; Gardosi, J.; Day, L.T.; Stanton, C. The Lancet’s Stillbirths Series Steering Committee. Stillbirths: Where? When? Why? How to make the data count? Lancet 2011, 377, 1448–1463. [Google Scholar] [CrossRef]
- Vogel, J.; Souza, J.; Mori, R.; Morisaki, N.; Lumbiganon, P.; Laopaiboon, M.; Ortiz-Panozo, E.; Hernandez, B.; Pérez-Cuevas, R.; Roy, M.; et al. Maternal complications and perinatal mortality: Findings of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG 2014, 121, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Kerber, K.J.; de Graft-Johnson, J.E.; Bhutta, Z.A.; Okong, P.; Starrs, A.; Lawn, J.E. Continuum of care for maternal, newborn, and child health: From slogan to service delivery. Lancet 2007, 370, 1358–1369. [Google Scholar] [CrossRef]
- Darmstadt, G.L.; Bhutta, Z.A.; Cousens, S.; Adam, T.; Walker, N.; De Bernis, L. Lancet Neonatal Survival Steering Team. Evidence-based, cost-effective interventions: How many newborn babies can we save? Lancet 2005, 365, 977–988. [Google Scholar] [CrossRef]
- Randive, B.; Diwan, V.; De Costa, A. India’s Conditional Cash Transfer Programme (the JSY) to Promote Institutional Birth: Is There an Association between Institutional Birth Proportion and Maternal Mortality? PLoS ONE 2013, 8, e67452. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Paudel, M.; Javanparast, S.; Dasvarma, G.; Newman, L. Religio-cultural factors contributing to perinatal mortality and morbidity in mountain villages of Nepal: Implications for future healthcare provision. PLoS ONE 2018, 13, e0194328. [Google Scholar] [CrossRef] [PubMed]
| Author [Ref.] Year Country | Study Design | Pregnancy Outcome (N) | Factors Associated with Perinatal Mortality | Study Limitations | Quality Assessment Score |
|---|---|---|---|---|---|
| Ahmed et al. [17] 2006 India | Cross-sectional study | 2199 | Domestic violence, first birth, lack of maternal education, poor socioeconomic status. | Underreporting of violence because of the involvement of perpetrators for obtaining data, no direct question to justify if the violence occurred during pregnancy, and underreport of pregnancy and death due to a retrospective study. | 7/14 (Fair) |
| Bari et al. [29] 2002 Bangladesh | Cohort study | 965 | Five or more pregnancy prior to index pregnancy, assisted delivery, poor economic status, anemia prevalence. | All study variables used in the analysis are not defined. | 10/14 (Good) |
| Guidotti et al. [30] 2009 Afghanistan | Cross-sectional study | 53,524 | Mode of delivery, medical risk factors. | Data were obtained from hospital records that are not primarily designed for research purpose; and this has limited study findings for the adjustment of other important confounding factors. | 4/14 (Poor) |
| Iqbal et al. [31] 2014 Pakistan | Cohort study | 11,260 | Antepartum hemorrhage, hypertensive disorders, mechanical problems, congenital anomalies, neonatal problems, maternal medical problems. | Small sample size. | 2/14 (Poor) |
| Khan et al. [19] 2017 Bangladesh | Cross-sectional study | 6584 | Maternal overweight and obesity. | Pregnancy outcomes reported in this study are based on based on maternal recall in five years preceding the survey that may inaccurately capture the total number of perinatal death. | 7/14 (Fair) |
| Perveen et al. [23] 2016 Pakistan | Cohort study | 234 | Sideropaenic anemia. | Small sample size, hospital-based study and it has the limitation of generalization of the finding into wider community level. | 5/14 (Fair) |
| Sachar et al. [32] 2000 India | Case-control study | 2424 | Lower maternal weight and height, BMI, literacy, pregnancy interval, prematurity, home delivery. | The study is based on rural setting, and findings from this study cannot be generalized to make a programmatic response to urban women. The risk variables used in the study are poorly defined. | 6/12 (Fair) |
| Shabbir et al. [33] 2014 Pakistan | Cohort study | 2010 | Multiparous, advanced maternal age. | Limitation of ascertainment bias. | 7/14 (Fair) |
| Shah et al. [18] 2000 India | Case-control study | 10,715 | Antenatal care, socioeconomic status, maternal education, tobacco consumption, parity, history of abortion, history of stillbirth, history of neonatal death, history of infant death, pregnancy spacing, maternal medical problems, obstetric problems, weeks of gestation, birth weight, type of labor, rupture of membranes, type of presentation, mode of delivery, anesthesia, intrapartum medical problems, Apgar score, state of amniotic fluid, resuscitation of the newborn, placenta and cord abnormalities, congenital defects. | Data collection was not regionally homogeneous limiting to apply study findings across the country. | 9/12 (Fair) |
| Siddalingappa et al. [34] 2013 India | Cross-sectional study | 314 | The intrapartum complication, intrauterine complication, small gestational size at birth, the time taken for a first cry, multiple pregnancies. | Limited sample size, limited scope for generalization. | 5/14 (Fair) |
| Wassan et al. [35] 2009 Pakistan | Cohort study | 2778 | Antenatal care, birth weight, gestational age, fetal causes, types of residence, maternal risk factors. | Hospital-based study and the study lacks generalizability of findings to a wider population. The study has lacked statistical measure to examine factors associate with perinatal mortality. | 4/14 (Poor) |
| Kusiako et al. [16] 2000 Bangladesh | Cross-sectional study | 3865 | Maternal age, poor obstetric history, antenatal nutritional marker, signs and symptoms of pregnancy, length of gestation, complications during labor. | As the data was collected by midwives, and lack of verbal autopsy may increase classification bias for perinatal mortality. | 6/14 (Fair) |
| Khanam et al. [36] 2017 Bangladesh | Cross-sectional study | 6285 | Antepartum hemorrhage, pregnancy-induced hypertension, probable infection. | The use of cross-sectional data lacks establishment of a temporal relationship between pregnancy complication and perinatal mortality. Selective recall bias as mothers who experienced perinatal deaths were more likely to recall antepartum complications compared with those who did not experience a complication. | 8/14 (Fair) |
| Short et al. [37] 2018 India and Pakistan | Cohort study | 41,778 | Obesity and overweight during pregnancy. | The findings are limited to reflect the whole of the cohort as almost 60% women who measured their weight after 12 weeks of pregnancy were excluded from the analysis. | 8/14 (Fair) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghimire, P.R.; Agho, K.E.; Akombi, B.J.; Wali, N.; Dibley, M.; Raynes-Greenow, C.; Renzaho, A.M.N. Perinatal Mortality in South Asia: Systematic Review of Observational Studies. Int. J. Environ. Res. Public Health 2018, 15, 1428. https://doi.org/10.3390/ijerph15071428
Ghimire PR, Agho KE, Akombi BJ, Wali N, Dibley M, Raynes-Greenow C, Renzaho AMN. Perinatal Mortality in South Asia: Systematic Review of Observational Studies. International Journal of Environmental Research and Public Health. 2018; 15(7):1428. https://doi.org/10.3390/ijerph15071428
Chicago/Turabian StyleGhimire, Pramesh Raj, Kingsley E. Agho, Blessing J. Akombi, Nidhi Wali, Michael Dibley, Camille Raynes-Greenow, and Andre M. N. Renzaho. 2018. "Perinatal Mortality in South Asia: Systematic Review of Observational Studies" International Journal of Environmental Research and Public Health 15, no. 7: 1428. https://doi.org/10.3390/ijerph15071428
APA StyleGhimire, P. R., Agho, K. E., Akombi, B. J., Wali, N., Dibley, M., Raynes-Greenow, C., & Renzaho, A. M. N. (2018). Perinatal Mortality in South Asia: Systematic Review of Observational Studies. International Journal of Environmental Research and Public Health, 15(7), 1428. https://doi.org/10.3390/ijerph15071428







