Key Dimensions for the Prevention and Control of Communicable Diseases in Institutional Settings: A Scoping Review to Guide the Development of a Tool to Strengthen Preparedness at Migrant Holding Centres in the EU/EEA
Abstract
1. Introduction
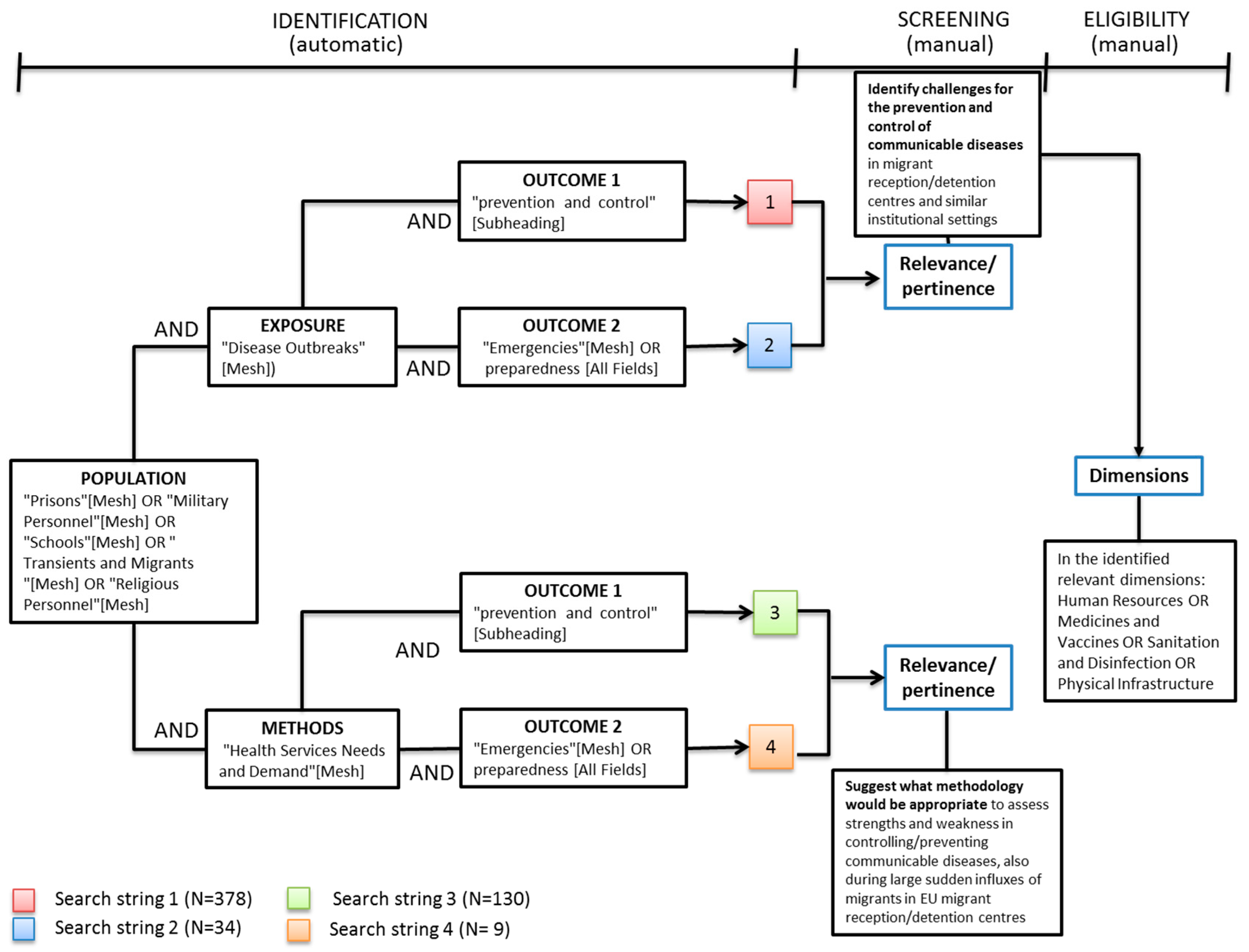
2. Materials and Methods
- (i)
- they were published between January 2000 and October 2015 in English, French, or Italian;
- (ii)
- they referred to institutional settings (i.e., institutions hosting “closed” or “semi-open” communities);
- (iii)
- they described types of disease transmission in these settings, and which dimensions were more frequently critical for transmission prevention/outbreak control (so as to address objective 1);
- (iv)
- they described existing assessment tools or prior assessments (so as to address objective 2).
3. Results
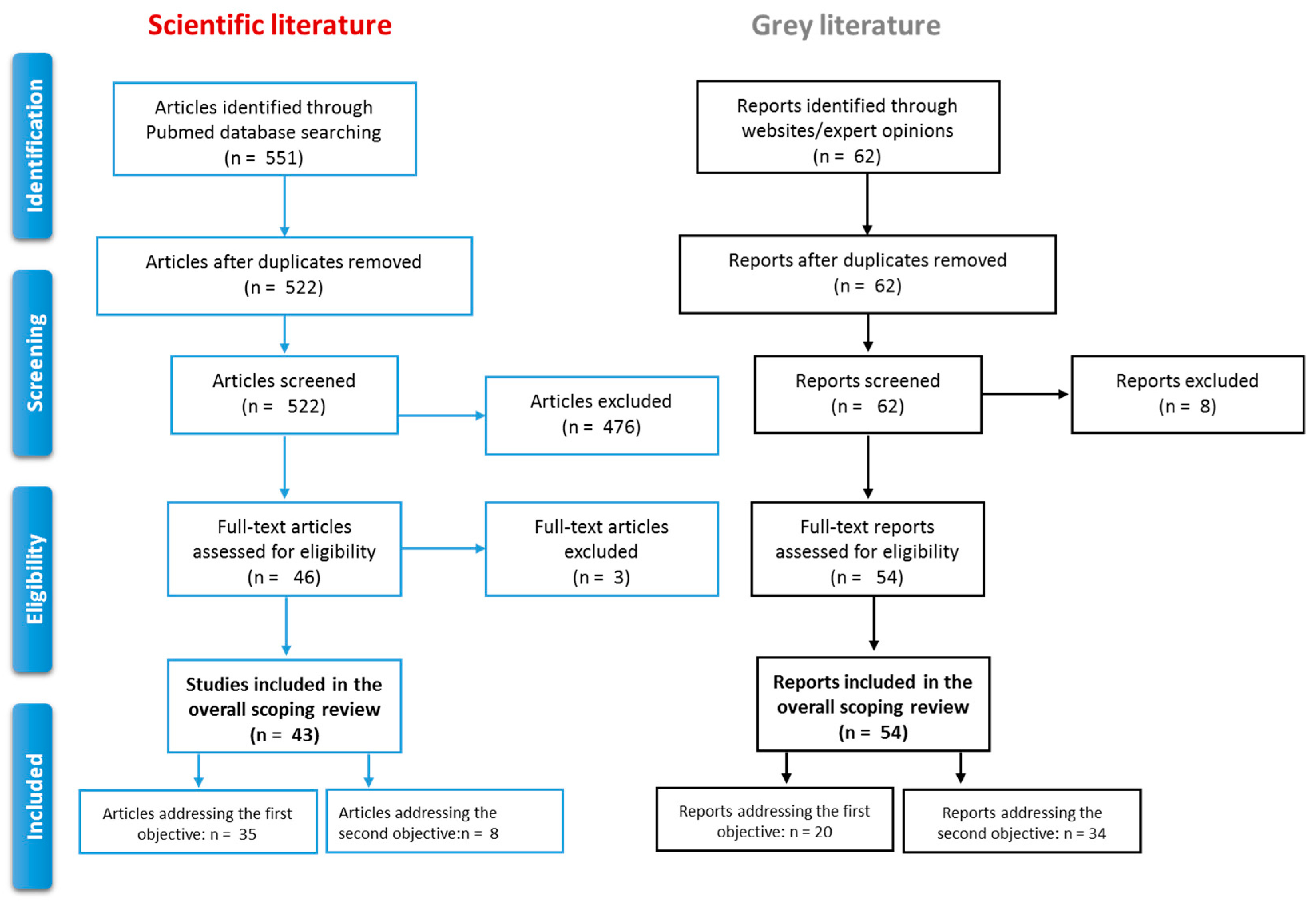
3.1. Selection Process
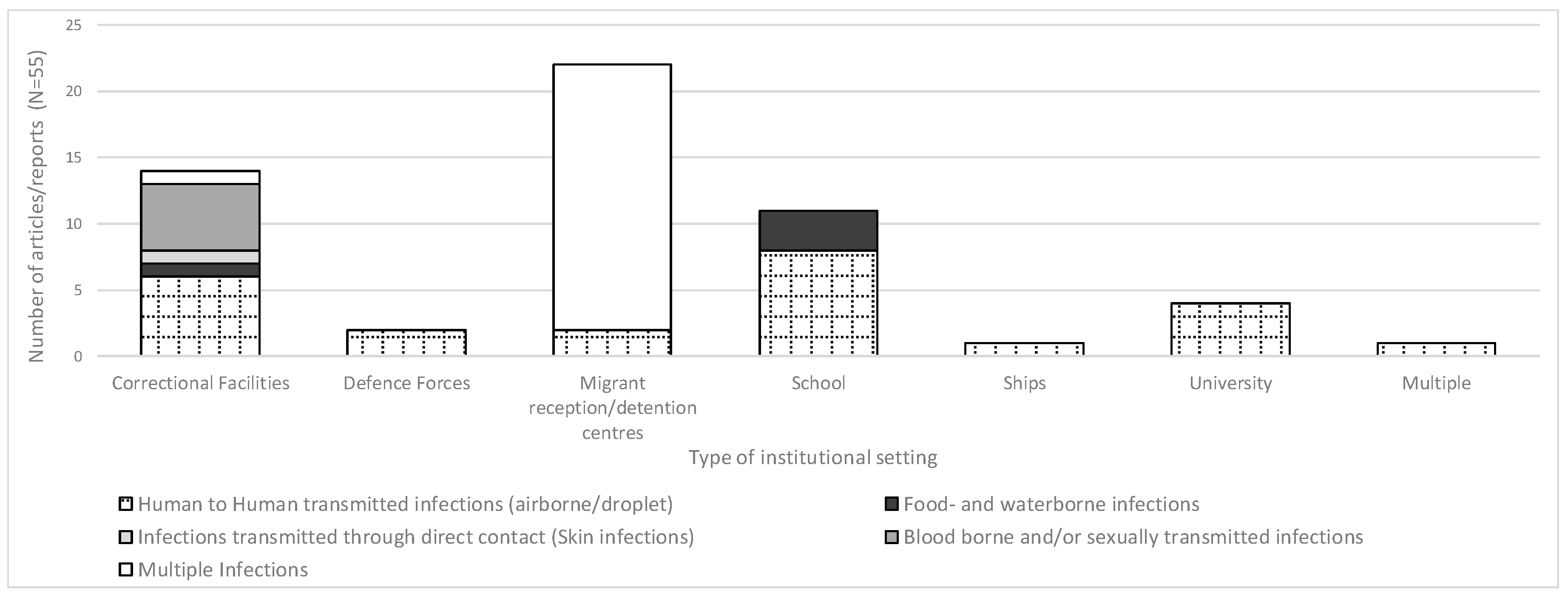
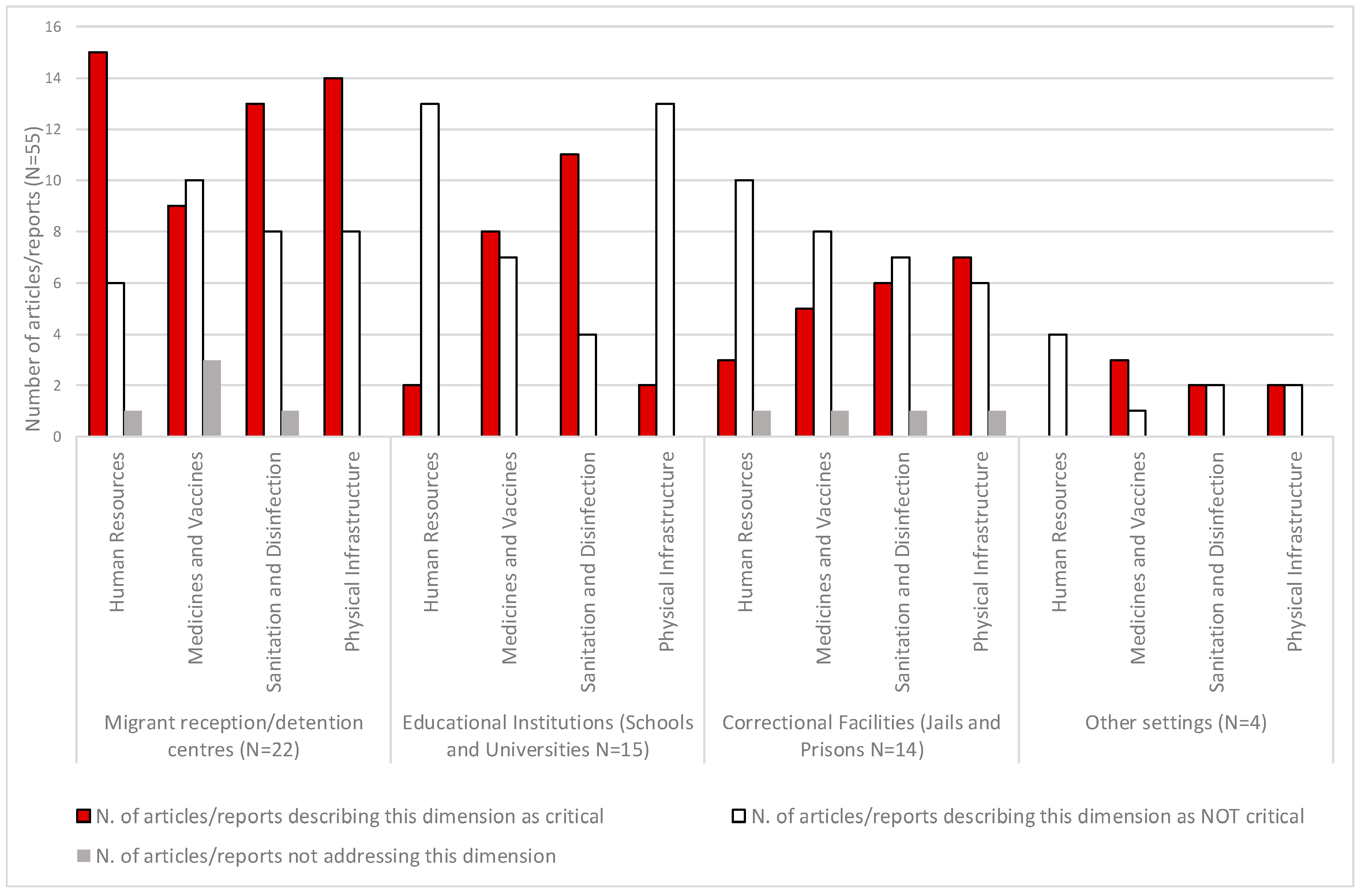
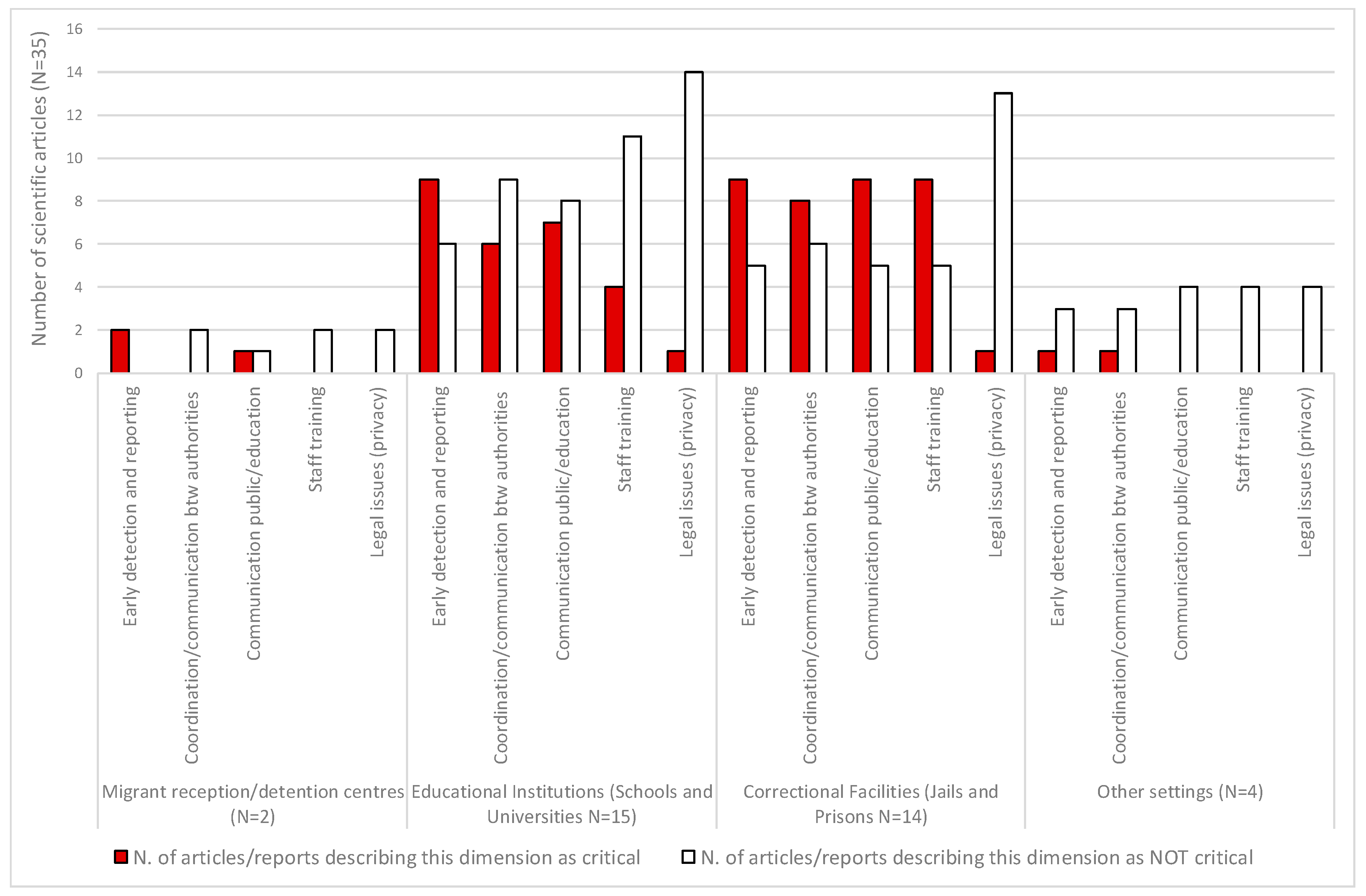
3.2. Challenges for the Prevention and Control of Communicable Diseases in Migrant Centres and Similar Institutional Settings
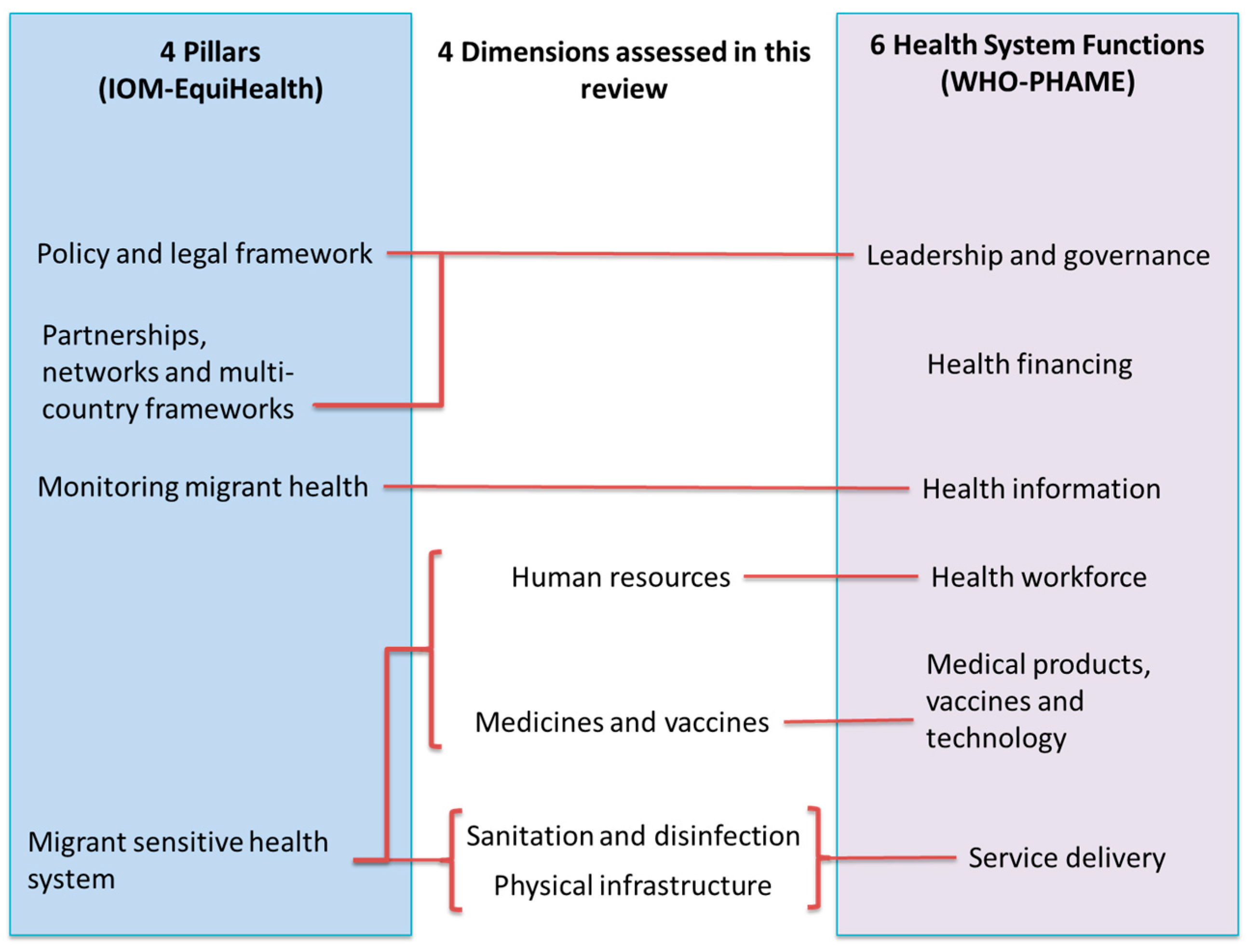
3.3. Suitable Approaches for Assessing Strengths and Weaknesses in Controlling/Preventing Communicable Diseases
4. Discussion
- Outbreak prevention (covering communicable disease prevention, rapid case detection, and case management)
- Outbreak control (covering outbreak detection and control in the reception/detention centre being assessed)
- Outbreak management during a large sudden influx of migrants (communicable disease prevention, detection, and control during a large sudden influx of refugee migrants at the reception/detention centre being assessed.
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Riccardo, F.; Dente, M.G.; Kärki, T.; Fabiani, M.; Napoli, C.; Chiarenza, A.; Giorgi Rossi, P.; Munoz, C.V.; Noori, T.; Declich, S. Towards a European Framework to Monitor Infectious Diseases among Migrant Populations: Design and Applicability. Int. J. Environ. Res. Public Health 2015, 12, 11640–11661. [Google Scholar] [CrossRef] [PubMed]
- Migration Policy Debates © OECD May 2014. Available online: https://www.oecd.org/migration/OECD%20Migration%20Policy%20Debates%20Numero%202.pdf (accessed on 11 May 2017).
- Horton, R. Offline: Migration and health—From aspiration to desperation. Lancet 2016, 388, 2071. [Google Scholar] [CrossRef]
- Riccardo, F.; Giorgi Rossi, P.; Chiarenza, A.; Noori, T.; Declich, S. Letter to the editor: Responding to a call for action—Where are we now? Eurosurveillance 2015, 20, 30096. [Google Scholar] [CrossRef] [PubMed]
- Eurostat. Asylum in the EU Member States: Record Number of over 1.2 Million First Time Asylum Seekers Registered in 2015. Available online: http://ec.europa.eu/eurostat/web/products-press-releases/-/3-04032016-AP (accessed on 11 May 2017).
- Van Loenen, T.; van den Muijsenbergh, M.; Hofmeester, M.; Dowrick, C.; van Ginneken, N.; Mechili, E.A.; Angelaki, A.; Ajdukovic, D.; Bakic, H.; Pavlic, D.R.; et al. Primary care for refugees and newly arrived migrants in Europe: A qualitative study on health needs, barriers and wishes. Eur. J. Public Health 2018, 28, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Kärki, T.; Napoli, C.; Riccardo, F.; Fabiani, M.; Dente, M.G.; Carballo, M.; Noori, T.; Declich, S. Screening for infectious diseases among newly arrived migrants in EU/EEA countries—Varying practices but consensus on the utility of screening. Int. J. Environ. Res. Public Health 2014, 11, 11004–11014. [Google Scholar] [CrossRef] [PubMed]
- Basu, S.; Stuckler, D.; McKee, M. Addressing institutional amplifiers in the dynamics and control of tuberculosis epidemics. Am. J. Trop. Med. Hyg. 2011, 84, 30–37. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Handbook on Using the ECDC Preparedness Checklist Tool to Strengthen Preparedness against Communicable Disease Outbreaks at Migrant Reception/Detention Centres; ECDC: Stockholm, Sweden, 2016.
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Haas, E.J.; Dukhan, L.; Goldstein, L.; Lyandres, M.; Gdalevich, M. Use of vaccination in a large outbreak of primary varicella in a detention setting for African immigrants. Int. Health 2014, 6, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Valin, N.; Antoun, F.; Chouaïd, C.; Renard, M.; Dautzenberg, B.; Lalande, V.; Ayache, B.; Morin, P.; Sougakoff, W.; Thiolet, J.M.; et al. Outbreak of tuberculosis in a migrants’ shelter, Paris, France. Int. J. Tuberc. Lung Dis. 2002, 9, 528–533. [Google Scholar]
- World Health Organization Office for Europe. Migrant Health in the European Region. Available online: http://www.euro.who.int/en/health-topics/health-determinants/migration-and-health/migrant-health-in-the-european-region (accessed on 26 May 2016).
- International Organization for Migration. EquiHealth Project. Available online: http://equi-health.eea.iom.int/ (accessed on 26 May 2016).
- European Centre for Disease Prevention and Control. Expert Opinion on the Public Health Needs of Irregular Migrants, Refugees or Asylum Seekers Across the EU’s Southern and Southeastern Borders; ECDC: Stockholm, Sweden, 2015.
- United Nations Interagency Health-Needs-Assessment Mission. Southern Turkey, 4–5 December 2012. Available online: http://www.euro.who.int/__data/assets/pdf_file/0006/189213/United-Nations-interagency-health-needs-assessment-mission-final.pdf?ua=1 (accessed on 11 May 2017).
- WHO Regional Office for Europe. Health Needs Assessment, Malta. 2012. Available online: http://www.euro.who.int/__data/assets/pdf_file/0011/144011/Malta_report.pdf?ua=1 (accessed on 11 May 2017).
- IOM EquiHealth Assessment Report: The Health Situation at EU Southern Borders Migrant Health, Occupational Health and Public Health Malta. 2013. Available online: http://equi-health.eea.iom.int/images/SAR_Malta_Final.pdf (accessed on 11 May 2017).
- Medicins Sans Frontieres, Italy. Al di la del muro Viaggio nei Centri per Migrant in Italia. 2010. Available online: http://www.asgi.it/wp-content/uploads/public/al.di.la.del.muro.viaggio.nei.centri.per.migranti.in.italia.pdf (accessed on 11 May 2017).
- Medici Senza Frontiere. Rapporto sulle Condizioni di Accoglienza nel CPSA Pozzallo. November 2015. Available online: http://archivio.medicisenzafrontiere.it/pdf/Rapporto_CPI_CPSA_Pozzallo_final.pdf (accessed on 11 May 2017).
- WHO Regional Office for Europe. Increased Influx of Migrants in Lampedusa, Italy. Joint Report from the Ministry of Health, Italy and the WHO Regional Office for Europe Mission of 28–29 March 2011. Available online: http://www.euro.who.int/__data/assets/pdf_file/0004/182137/e96761.pdf?ua=1 (accessed on 11 May 2017).
- WHO Regional Office for Europe. Second Assessment of Migrant Health Needs Lampedusa and Linosa, Italy. Joint Report on a Mission of the Ministry of Health of Italy, the Regional Health Authority of Sicily and the WHO Regional Office for Europe, 16–19 May 2012. Available online: http://www.euro.who.int/__data/assets/pdf_file/0010/184465/e96796.pdf?ua=1 (accessed on 11 May 2017).
- WHO Regional Office for Europe. Sicily, Italy: Assessing Health-System Capacity to Manage Sudden Large Influxes of Migrants Joint Report on a Mission of the Ministry of Health of Italy, the Regional Health Authority of Sicily and the WHO Regional Office for Europe. 2014. Available online: http://www.euro.who.int/__data/assets/pdf_file/0007/262519/Sicily-Italy-Assessing-health-system-capacity-manage-sudden-large-influxes-migrantsEng.pdf?ua=1 (accessed on 11 May 2017).
- IOM EquiHealth Assessment Report: The Health Situation at EU Southern Borders Migrant Health, Occupational Health and Public Health Italy. 2013. Available online: http://equi-health.eea.iom.int/images/SAR_Italy_Final.pdf (accessed on 11 May 2017).
- WHO Regional Office for Europe. Cyprus: Assessing Health-System Capacity to Manage Sudden Large Influxes of Migrants. Joint Report on a Mission of the Ministry of Health of Cyprus, the International Centre for Migration, Health and Development and the WHO Regional Office for Europe. 2015. Available online: http://www.euro.who.int/__data/assets/pdf_file/0020/293330/Cyprus-Assessment-Report-en.pdf?ua=1 (accessed on 11 May 2017).
- IOM EquiHealth Assessment Report: The Health Situation at EU Southern Borders Migrant Health, Occupational Health and Public Health Croatia. 2014. Available online: http://equi-health.eea.iom.int/images/SAR_Croatia_Final.pdf (accessed on 11 May 2017).
- WHO Regional Office for Europe. Serbia: Assessing Health-System Capacity to Manage Sudden Large Influxes of Migrants. Joint Report on a Mission of the Ministry of Health of Serbia and the WHO Regional Office for Europe with the Collaboration of the International Organization for Migration. 2015. Available online: http://www.euro.who.int/__data/assets/pdf_file/0010/293329/Serbia-Assessment-Report-en.pdf?ua=1 (accessed on 11 May 2017).
- WHO Regional Office for Europe. Assessing Health-System Capacity to Manage Sudden Large Influxes of Migrants Bulgaria. Joint Report on a Mission of the Ministry of Health of Bulgaria and the WHO Regional Office for Europe. 2015. Available online: http://www.euro.who.int/__data/assets/pdf_file/0009/300402/Bulgaria-Assessment-Report-en.pdf (accessed on 11 May 2017).
- IOM EquiHealth Assessment Report: The Health Situation at EU Southern Borders Migrant Health, Occupational Health and Public Health Bulgaria. 2014–2015. Available online: http://equi-health.eea.iom.int/images/SAR_Bulgaria_Final.pdf (accessed on 11 May 2017).
- WHO Regional Office for Europe. Portugal: Assessing Health-System Capacity to Manage Sudden Large Influxes of Migrants Joint Report on a Mission of the Ministry of Health of Portugal, the International Centre for Migration, Health and Development and the WHO Regional Office for Europe. 2014. Available online: http://www.euro.who.int/__data/assets/pdf_file/0016/265012/Portugal-assessing-health-system-capacity-to-manage-sudden-large-influxes-of-migrants.pdf?ua=1 (accessed on 11 May 2017).
- European Centre for Disease Prevention and Control and WHO Regional Office for Europe. Joint ECDC/WHO Regional Office for Europe Mission Report: Increased Influx of Migrants at the Greek–Turkish Border. Greece, 4–8 April 2011. Stockholm: ECDC. 2011. Available online: http://www.euro.who.int/__data/assets/pdf_file/0012/144012/Greece_mission_rep_2011.pdf?ua=1 (accessed on 11 May 2017).
- WHO Regional Office for Europe. Greece: Assessing Health-System Capacity to Manage Sudden Large Influxes of Migrants. Joint Report on a Mission of the Ministry of Health of Greece, Hellenic Centre for Disease Control and Prevention and WHO Regional Office for Europe. 2015. Available online: http://www.euro.who.int/__data/assets/pdf_file/0007/300400/Greece-Assessment-Report-en.pdf?ua=1 (accessed on 11 May 2017).
- IOM EquiHealth Assessment Report: The Health Situation at EU Southern Borders Migrant Health, Occupational Health and Public Health Greece. 2013. Available online: http://equi-health.eea.iom.int/images/SAR_Greece_Final.pdf (accessed on 11 May 2017).
- IOM EquiHealth Assessment Report: The Health Situation at EU Southern Borders Migrant Health, Occupational Health and Public Health Spain. 2013. Available online: http://equi-health.eea.iom.int/images/SAR_Spain_Final.pdf (accessed on 11 May 2017).
- Lee, M.B.; Greig, J.D. A review of gastrointestinal outbreaks in schools: Effective infection control interventions. J. Sch. Health 2010, 80, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Greig, J.D.; Lee, M.B.; Harris, J.E. Review of enteric outbreaks in prisons: Effective infection control interventions. Public Health 2011, 125, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Tsalik, E.L.; Cunningham, C.K.; Cunningham, H.M.; Lopez-Marti, M.G.; Sangvai, D.G.; Purdy, W.K.; Anderson, D.J.; Thompson, J.R.; Brown, M.; Woods, C.W.; et al. An Infection Control Program for a 2009 influenza A H1N1 outbreak in a university-based summer camp. J. Am Coll. Health 2011, 59, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Leung, J.; Lopez, A.S.; Tootell, E.; Baumrind, N.; Mohle-Boetani, J.; Leistikow, B.; Harriman, K.H.; Preas, C.P.; Cosentino, G.; Bialek, S.R.; et al. Challenges with controlling varicella in prison settings: Experience of California, 2010 to 2011. J. Correct. Health Care 2014, 20, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Jongcherdchootrakul, K.; Henderson, A.K.; Iamsirithaworn, S.; Modchang, C.; Siriarayapon, P. First pandemic A (H1N1) pdm09 outbreak in a private school, Bangkok, Thailand, June 2009. J. Med. Assoc. Thai 2014, 97 (Suppl. 2), S145–S152. [Google Scholar] [PubMed]
- Guthrie, J.A.; Lokuge, K.M.; Levy, M.H. Influenza control can be achieved in a custodial setting: Pandemic (H1N1) 2009 and 2011 in an Australian prison. Public Health 2012, 126, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Kadlubowski, M.; Wasko, I.; Klarowicz, A.; Hryniewicz, W. Invasive meningococcal disease at a military base in Warsaw, January 2007. Wkly. Releases 2007, 12, 3147. [Google Scholar] [CrossRef]
- Matthews, E.; Armstrong, G.; Spencer, T. Pertussis infection in a baccalaureate nursing program: Clinical implications, emerging issues, and recommendations. J. Contin. Educ. Nurs. 2008, 39, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Bonačić Marinović, A.A.; Swaan, C.; Wichmann, O.; van Steenbergen, J.; Kretzschmar, M. Effectiveness and timing of vaccination during school measles outbreak. Emerg. Infect. Dis. 2012, 18, 1405–1413. [Google Scholar] [CrossRef] [PubMed]
- Kay, D.; Roche, M.; Atkinson, J.; Lamden, K.; Vivancos, R. Mumps outbreaks in four universities in the North West of England: Prevention, detection and response. Vaccine 2011, 29, 3883–3887. [Google Scholar] [CrossRef] [PubMed]
- Crum, N.F.; Wallace, M.R.; Lamb, C.R.; Conlin, A.M.; Amundson, D.E.; Olson, P.E.; Ryan, M.A.; Robinson, T.J.; Gray, G.C.; Earhart, K.C. Halting a pneumococcal pneumonia outbreak among United States Marine Corps trainees. Am. J. Prev. Med. 2003, 25, 107–111. [Google Scholar] [CrossRef]
- Elias, A.F.; Chaussee, M.S.; McDowell, E.J.; Huntington, M.K. Community-based intervention to manage an outbreak of MRSA skin infections in a county jail. J. Correct. Health Care 2010, 16, 205–215. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wolfe, M.I.; Xu, F.; Patel, P.; O’Cain, M.; Schillinger, J.A.; St Louis, M.E.; Finelli, L. An outbreak of syphilis in Alabama prisons: Correctional health policy and communicable disease control. Am. J. Public Health 2001, 91, 1220–1225. [Google Scholar] [CrossRef] [PubMed]
- Hellard, M.E.; Aitken, C.K. HIV in prison: What are the risks and what can be done? Sex Health 2004, 1, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Wohl, D.A.; Rosen, D.; Kaplan, A.H. HIV and incarceration: Dual epidemics. AIDS Read. 2006, 16, 247–250, 257–260. [Google Scholar] [PubMed]
- Ehrmann, T. Community-based organizations and HIV prevention for incarcerated populations: Three HIV prevention program models. AIDS Educ. Prev. 2002, 14 (Suppl. 5), 75–84. [Google Scholar] [CrossRef] [PubMed]
- Zalumas, J.C.; Rose, C.D. Hepatitis C and HIV in incarcerated populations: Fights, bites, searches, and syringes! J. Assoc. Nurses AIDS Care 2003, 14 (Suppl. 5), 108S–115S. [Google Scholar] [CrossRef] [PubMed]
- Van’t Hoff, G.; Fedosejeva, R.; Mihailescu, L. Prisons’ preparedness for pandemic flu and the ethical issues. Public Health 2009, 123, 422–425. [Google Scholar] [CrossRef] [PubMed]
- Arinaminpathy, N.; Raphaely, N.; Saldana, L.; Hodgekiss, C.; Dandridge, J.; Knox, K.; McCarthy, N.D. Transmission and control in an institutional pandemic influenza A(H1N1) 2009 outbreak. Epidemiol. Infect. 2012, 140, 1102–1110. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schwartz, R.D. The impact of correctional institutions on public health during a pandemic or emerging infection disaster. Am. J. Disaster Med. 2008, 3, 165–170. [Google Scholar] [PubMed]
- Levy, M.H.; Quilty, S.; Young, L.C.; Hunt, W.; Matthews, R.; Robertson, P.W. Pox in the docks: Varicella outbreak in an Australian prison system. Public Health 2003, 117, 446–451. [Google Scholar] [CrossRef]
- WHO Regional Office for Europe. Large Influxes of Refugees and Migrants. Toolkit for Assessing Health System Capacity to Manage Large Influxes of Refugees and Migrants in the Acute Phase. 2015. Available online: https://www.escap.eu/bestanden/Care%20(38)/Refugees/toolkit_assessing_hs_capacity_manage_large_influxes_refugees_asylum_seekers_migrants.pdf (accessed on 11 May 2017).
- World Health Organization. International Health Regulations (2005): Assessment Tool for Core Capacity Requirements at Designated Airports, Ports and Ground Crossings; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- OSCE. Self-Assessment Tool for Nations to Increase Preparedness for Cross-Border Implications of Crises; OSCE Secretariat Transnational Threats Department Borders Unit: Vienna, Austria, 2013. [Google Scholar]
- WHO Regional Office for Europe. Strengthening Health-System Emergency Preparedness. Toolkit for Assessing Health-System Capacity for Crisis Management. Part 1. User Manual; World Health Organization: Copenhagen, Denmark, 2012. [Google Scholar]
- WHO Regional Office for Europe. Hospital Emergency Response Checklist. An All-Hazards Tool for Hospital Administrators and Emergency Managers; World Health Organization: Copenhagen, Denmark, 2011. [Google Scholar]
- Brown, V.W.; Moren, A.; Paquet, C. Rapid Health Assessment of Refugee and Displaced Populations, 3rd ed.; Médecins Sans Frontières: Paris, France, 2006. [Google Scholar]
- Council of Europe Visiting Immigration Detention Centres. A Guide for Parliamentarians. 2013. Available online: http://www.apt.ch/content/files_res/guide-for-parliamentarians-visiting-detention-centres-en.pdf (accessed on 11 May 2017).
- Public Health England. Health and Justice Health Needs Assessment Template: Adult Prisons. 2014. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/331628/Health_Needs_Assessment_Toolkit_for_Prescribed_Places_of_Detention_Part_2.pdf (accessed on 11 May 2017).
- United Nations Office on Drugs and Crime. HIV in Prisons: Situation and Needs Assessment Toolkit. 2010. Available online: http://www.unodc.org/documents/hiv-aids/publications/HIV_in_prisons_situation_and_needs_assessment_document.pdf (accessed on 11 May 2017).
- International Health Regulations 2005 (second edition) World Health Organization 2008. Available online: http://apps.who.int/iris/bitstream/10665/43883/1/9789241580410_eng.pdf (accessed on 11 May 2017).
- Medecins Sans Frontiers. Refugee Health. An Approach to Emergency Situations. Available online: http://refbooks.msf.org/msf_docs/en/refugee_health/rh.pdf (accessed on 11 May 2017).
- World Health Organization. Communicable Disease Control in Emergencies; World Health Organization: Copenhagen, Denmark, 2005. [Google Scholar]
- United Nations High Commissioner for Refugees. UNHCR Handbook for Emergencies, 3rd ed.; UNHCR: Geneva, Switzerland, 2007. [Google Scholar]
- European Centre for Disease Prevention and Control. Outline for Initial Migrant Health Assessment at Point of Entry to the European Union; European Centre for Disease Prevention and Control: Solna, Sweden, 2011.
- United Nations High Commissioner for Refugees. Shelter Needs Assessment. Available online: https://emergency.unhcr.org/entry/60439/shelter-needs-assessment (accessed on 11 May 2017).
- Inter-Agency Standing Committee (IASC) (2012) Multi-Cluster/Sector Initial Rapid Assessment (MIRA). Available online: https://docs.unocha.org/sites/dms/Documents/mira_final_version2012.pdf (accessed on 11 May 2017).
- The Sphere Project (2011) Humanitarian Charter and Minimum Standards in Humanitarian Response. Available online: http://www.spherehandbook.org/en/how-to-use-this-chapter-2/ (accessed on 11 May 2017).
- United Nations Refugee Agency. A Guidance for UNHCR Field Operations on Water and Sanitation Services; United Nations Refugee Agency: Geneva, Switzerland, 2008. [Google Scholar]
- Pacifici, L.E.; Riccardo, F. Manuale di Buone Pratiche. Esperienze da un Centro di Accoglienza per Richiedenti Asilo. Italian Red Cross. 2010. Available online: https://www.cri.it/flex/cm/pages/ServeAttachment.php/L/IT/D/D.5385afb5b4bd69f22d63/P/BLOB%3AID%3D4983/E/pdf (accessed on 11 May 2017).
- Platform for European Red Cross Cooperation on Refugees, Asylum Seekers and Migrants (PERCO). Guidelines on the Reception of Asylum Seekers for National Red Cross and Red Crescent Societies. Available online: http://www.justice.ie/en/JELR/Irish%20Red%20Cross.pdf/Files/Irish%20Red%20Cross.pdf (accessed on 11 May 2017).
- Regione del Veneto. Direzione Attuazione Programmazione Sanitaria. Settore Promozione e Sviluppo Igiene e Sanità Pubblica. Protocollo Operativo per il Controllo delle Malattie Infettive e la Profilassi Immunitaria in Relazione All’afflusso di Immigrati. 2 Ottobre 2014. Available online: http://repository.regione.veneto.it/public/2ab9a9def3c4c2ce6140dd9404517dd6.php?dl=true (accessed on 26 July 2017).
- Napoli, C.; Riccardo, F.; Declich, S.; Dente, M.G.; Pompa, M.G.; Rizzo, C.; Rota, M.C.; Bella, A.; National Working Group. An early warning system based on syndromic surveillance to detect potential health emergencies among migrants: Results of a two-year experience in Italy. Int. J. Environ. Res. Public Health 2014, 11, 8529–8541. [Google Scholar] [CrossRef] [PubMed]
- Riccardo, F.; Napoli, C.; Bella, A.; Rizzo, C.; Rota, M.C.; Dente, M.G.; De Santis, S.; Declich, S. Syndromic surveillance of epidemic-prone diseases in response to an influx of migrants from North Africa to Italy, May to October 2011. Eurosurveillance 2011, 16, 20016. [Google Scholar] [CrossRef]
- Rojek, A.M.; Gkolfinopoulou, K.; Veizis, A.; Lambrou, A.; Castle, L.; Georgakopoulou, T.; Blanchet, K.; Panagiotopoulos, T.; Horby, P.W.; The Epidemic Diseases Research Group field team. Clinical assessment is a neglected component of outbreak preparedness: Evidence from refugee camps in Greece. BMC Med. 2018, 16, 43. [Google Scholar] [CrossRef] [PubMed]
- Veneti, L.; Theocharopoulos, G.; Gkolfinopoulou, K.; Baka, A.; Lytras, T.; Triantafillou, E.; Lambrou, A.; Tsiodras, S.; Georgakopoulou, T.; Mellou, K.; et al. Implementation of infectious disease syndromic surveillance in points of care for refugees/migrants, Greece, April–July 2016. In ESCAIDE Conference Paper; European Centre for Disease Prevention and Control (ECDC): Stockholm, Sweden, 2016. [Google Scholar]
- Bradby, H.; Humphris, R.; Newall, D.; Phillimore, J. Public Health Aspects of Migrant Health: A Review of the Evidence on Health Status for Refugees and Asylum Seekers in the European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- European Centre for Disease Prevention and Control. Handbook on Implementing Syndromic Surveillance in Migrant Reception/Detention Centres and other Refugee Settings; ECDC: Stockholm, Sweden, 2016.
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. Theory Pract. 2005, 8, 19–32. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riccardo, F.; Suk, J.E.; Espinosa, L.; Bella, A.; Giambi, C.; Del Manso, M.; Napoli, C.; Dente, M.G.; Nacca, G.; Declich, S. Key Dimensions for the Prevention and Control of Communicable Diseases in Institutional Settings: A Scoping Review to Guide the Development of a Tool to Strengthen Preparedness at Migrant Holding Centres in the EU/EEA. Int. J. Environ. Res. Public Health 2018, 15, 1120. https://doi.org/10.3390/ijerph15061120
Riccardo F, Suk JE, Espinosa L, Bella A, Giambi C, Del Manso M, Napoli C, Dente MG, Nacca G, Declich S. Key Dimensions for the Prevention and Control of Communicable Diseases in Institutional Settings: A Scoping Review to Guide the Development of a Tool to Strengthen Preparedness at Migrant Holding Centres in the EU/EEA. International Journal of Environmental Research and Public Health. 2018; 15(6):1120. https://doi.org/10.3390/ijerph15061120
Chicago/Turabian StyleRiccardo, Flavia, Jonathan E. Suk, Laura Espinosa, Antonino Bella, Cristina Giambi, Martina Del Manso, Christian Napoli, Maria Grazia Dente, Gloria Nacca, and Silvia Declich. 2018. "Key Dimensions for the Prevention and Control of Communicable Diseases in Institutional Settings: A Scoping Review to Guide the Development of a Tool to Strengthen Preparedness at Migrant Holding Centres in the EU/EEA" International Journal of Environmental Research and Public Health 15, no. 6: 1120. https://doi.org/10.3390/ijerph15061120
APA StyleRiccardo, F., Suk, J. E., Espinosa, L., Bella, A., Giambi, C., Del Manso, M., Napoli, C., Dente, M. G., Nacca, G., & Declich, S. (2018). Key Dimensions for the Prevention and Control of Communicable Diseases in Institutional Settings: A Scoping Review to Guide the Development of a Tool to Strengthen Preparedness at Migrant Holding Centres in the EU/EEA. International Journal of Environmental Research and Public Health, 15(6), 1120. https://doi.org/10.3390/ijerph15061120






