Condom and Substance Use at Last Sex: Differences between MSMO and MSWO High School Youth
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Analytic Sample
2.3. Measures
2.4. Statistical Analysis
3. Results
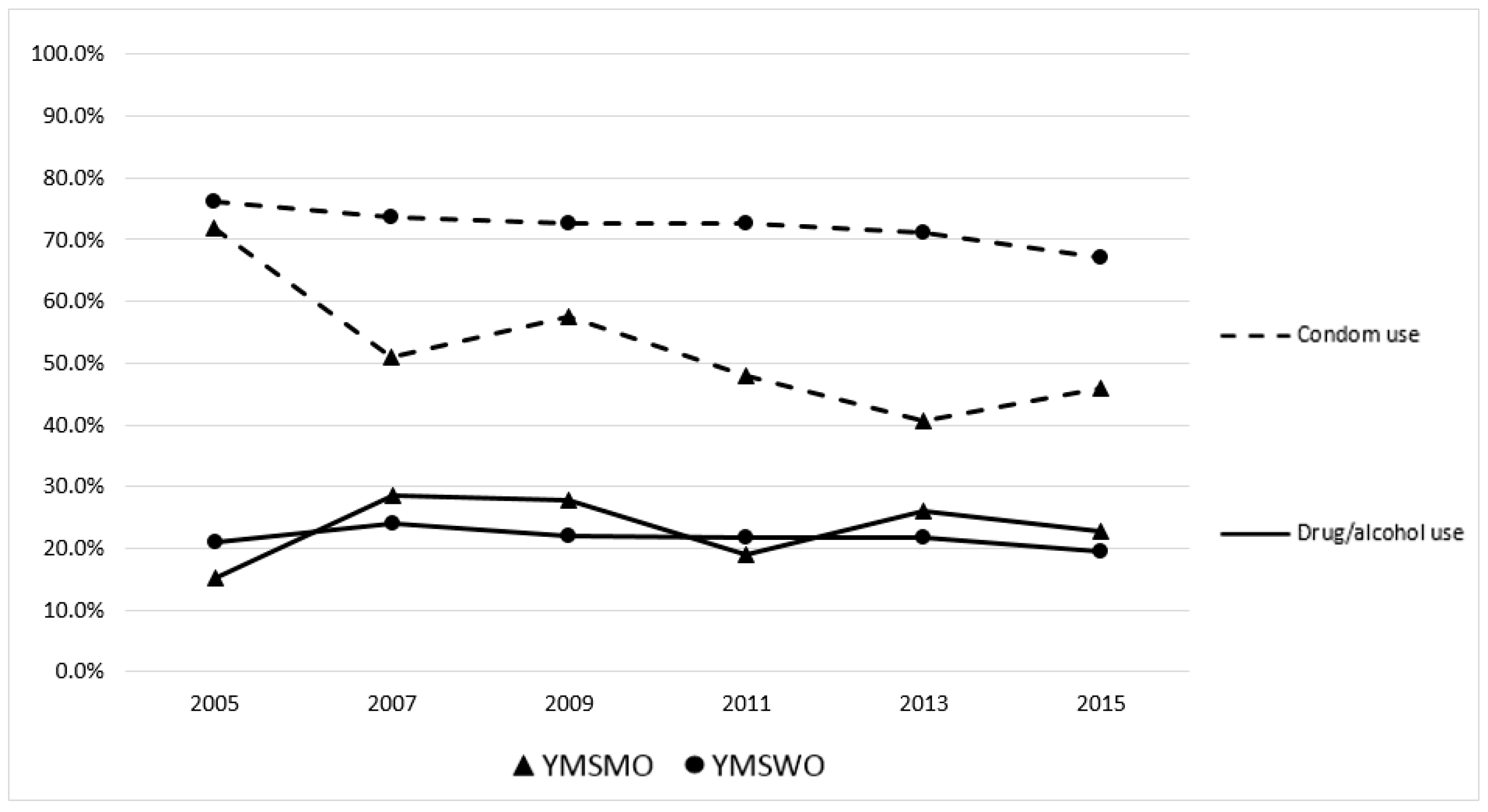
3.1. Condom Use/Substance Use at Last Sex
3.2. Associations with Sex of Partner
3.3. Longitudinal Associations
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC). HIV Surveillance Report, 2016; CDC: Atlanta, GA, USA, 2017; Volume 28. [Google Scholar]
- Prejean, J.; Song, R.; Hernandez, A.; Ziebell, R.; Green, T.; Walker, F.; Lin, L.S.; An, Q.; Mermin, J.; Lansky, A.; et al. Estimated HIV incidence in the United States, 2006–2009. PLoS ONE 2011, 6, e17502. [Google Scholar] [CrossRef] [PubMed]
- CDC. CDC Fact Sheet: HIV among Gay and Bisexual Men; CDC: Atlanta, GA, USA, 2017. [Google Scholar]
- Shlay, J.C.; McClung, M.W.; Patnaik, J.L.; Douglas, J.M., Jr. Comparison of sexually transmitted disease prevalence by reported condom use: Errors among consistent condom users seen at an urban sexually transmitted disease clinic. Sex. Transm. Dis. 2004, 31, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Pathela, P.; Braunstein, S.L.; Schillinger, J.A.; Shepard, C.; Sweeney, M.; Blank, S. Men who have sex with men have a 140-fold higher risk for newly diagnosed HIV and syphilis compared with heterosexual men in New York City. J. Acquir. Immune Defic. Syndr. 2011, 58, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Reece, M.; Herbenick, D.; Schick, V.; Sanders, S.A.; Dodge, B.; Fortenberry, J.D. Condom use rates in a national probability sample of males and females ages 14 to 94 in the United States. J. Sex. Med. 2010, 7, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Friedman, M.R.; Wei, C.; Klem, M.L.; Silvestre, A.J.; Markovic, N.; Stall, R. HIV Infection and Sexual Risk among Men Who Have Sex with Men and Women (MSMW): A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e87139. [Google Scholar] [CrossRef] [PubMed]
- Gorbach, P.M.; Murphy, R.; Weiss, R.E.; Hucks-Ortiz, C.; Shoptaw, S. Bridging sexual boundaries: Men who have sex with men and women in a street-based sample in Los Angeles. J. Urban Health 2009, 86, 63–76. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pathela, P.; Schillinger, J.A. Sexual behaviors and sexual violence: Adolescents with opposite-, same-, or both-sex partners. Pediatrics 2010, 126, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Hess, K.L.; Chavez, P.R.; Kanny, D.; DiNenno, E.; Lansky, A.; Paz-Bailey, G.; Group, N.S. Binge drinking and risky sexual behavior among HIV-negative and unknown HIV status men who have sex with men, 20 US cities. Drug Alcohol Depend. 2015, 147, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Irwin, T.W.; Morgenstern, J.; Parsons, J.T.; Wainberg, M.; Labouvie, E. Alcohol and sexual HIV risk behavior among problem drinking men who have sex with men: An event level analysis of timeline followback data. AIDS Behav. 2006, 10, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Jones-Webb, R.; Smolenski, D.; Brady, S.; Wilkerson, M.; Rosser, B.R. Drinking settings, alcohol consumption, and sexual risk behavior among gay men. Addict. Behav. 2013, 38, 1824–1830. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Temple, M.T.; Leigh, B.C.; Schafer, J. Unsafe Sexual-Behavior and Alcohol-Use at the Event Level—Results of a National Survey. J. Acquir. Immune Defic. Syndr. 1993, 6, 393–401. [Google Scholar] [PubMed]
- Shuper, P.A.; Joharchi, N.; Irving, H.; Rehm, J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: Review and meta-analysis. AIDS Behav. 2009, 13, 1021–1036. [Google Scholar] [CrossRef] [PubMed]
- Conner, M.; Sutherland, E.; Kennedy, F.; Grearly, C.; Berry, C. Impact of alcohol on sexual decision making: Intentions to have unprotected sex. Psychol. Health 2008, 23, 909–934. [Google Scholar] [CrossRef] [PubMed]
- Dir, A.L.; Gilmore, A.K.; Moreland, A.D.; Davidson, T.M.; Borkman, A.L.; Rheingold, A.A.; Danielson, C.K. What’s the harm? Alcohol and marijuana use and perceived risks of unprotected sex among adolescents and young adults. Addict. Behav. 2018, 76, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Hingson, R.W.; Strunin, L.; Berlin, B.M.; Heeren, T. Beliefs about AIDS, use of alcohol and drugs, and unprotected sex among Massachusetts adolescents. Am. J. Public Health 1990, 80, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Kingree, J.B.; Braithwaite, R.; Woodring, T. Unprotected sex as a function of alcohol and marijuana use among adolescent detainees. J. Adolesc. Health 2000, 27, 179–185. [Google Scholar] [CrossRef]
- Newcomb, M.E.; Mustanski, B. Developmental change in the relationship between alcohol and drug use before sex and sexual risk behavior in young men who have sex with men. AIDS Behav. 2014, 18, 1981–1990. [Google Scholar] [CrossRef] [PubMed]
- Newcomb, M.E. Moderating effect of age on the association between alcohol use and sexual risk in MSM: Evidence for elevated risk among younger MSM. AIDS Behav. 2013, 17, 1746–1754. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kerr, D.C.R.; Washburn, I.J.; Morris, M.K.; Lewis, K.A.G.; Tiberio, S.S. Event-Level Associations of Marijuana and Heavy Alcohol Use With Intercourse and Condom Use. J. Stud. Alcohol Drugs 2015, 76, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Kahler, C.W.; Wray, T.B.; Pantalone, D.W.; Kruis, R.D.; Mastroleo, N.R.; Monti, P.M.; Mayer, K.H. Daily associations between alcohol use and unprotected anal sex among heavy drinking HIV-positive men who have sex with men. AIDS Behav. 2015, 19, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Leigh, B.C. Alcohol and condom use—A meta-analysis of event-level studies. Sex. Transm. Dis. 2002, 29, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Rendina, H.J.; Moody, R.L.; Ventuneac, A.; Grov, C.; Parsons, J.T. Aggregate and event-level associations between substance use and sexual behavior among gay and bisexual men: Comparing retrospective and prospective data. Drug Alcohol Depend. 2015, 154, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Feinstein, B.A.; Newcomb, M.E. Event-Level Associations Among Drinking Motives, Alcohol Consumption, and Condomless Anal Sex in a Sample of Young Men Who Have Sex With Men. AIDS Behav. 2017, 21, 1904–1913. [Google Scholar] [CrossRef] [PubMed]
- Wells, B.E.; Rendina, H.J.; Kelly, B.C.; Golub, S.A.; Parsons, J.T. Demographic Predictors of Event-Level Associations between Alcohol Consumption and Sexual Behavior. J. Urban Health Bull. N. Y. Acad. Med. 2016, 93, 155–169. [Google Scholar] [CrossRef] [PubMed]
- CDC. Trends in the Prevalence of Sexual Behaviors and HIV Testing. NationalYrbs: 1991–2011; CDC: Atlanta, GA, USA, 2011. [Google Scholar]
- Brener, N.D.; Kann, L.; Shanklin, S.; Kinchen, S.; Eaton, D.K.; Hawkins, J.; Flint, K.H. Methodology of the youth risk behavior surveillance system—2013. MMWR Recomm. Rep. 2013, 62, 1–20. [Google Scholar] [PubMed]
- Kann, L. Sexual Identity, Sex of Sexual Contacts, and Health-Related Behaviors Among Students in Grades 9–12—United States and Selected Sites, 2015. MMWR Surveill. Summ. 2016, 65, 1–202. [Google Scholar] [CrossRef] [PubMed]
- Esser, M.B. Current and Binge Drinking Among High School Students—United States, 1991–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 474. [Google Scholar] [CrossRef] [PubMed]
- Troiden, R.R. Homosexual identity development. J. Adolesc. Health Care 1988, 9, 105–113. [Google Scholar] [CrossRef]
- Abara, W.E.; Oraka, E.; Jeffries, W.L.; Chavez, P.; Nasrullah, M.; DiNenno, E. Prevalence and correlates of condom use among sexually active men who have sex with men in the United States: Findings from the National Survey of Family Growth, 2002, 2006–2010 and 2011–2013. Sex. Health 2017, 14, 363–371. [Google Scholar] [PubMed]
- Lindley, L.L.; Walsemann, K.M. Sexual Orientation and Risk of Pregnancy among New York City High-School Students. Am. J. Public Health 2015, 105, 1379–1386. [Google Scholar] [CrossRef] [PubMed]
- Kiene, S.M.; Barta, W.D.; Tennen, H.; Armeli, S. Alcohol, helping young adults to have unprotected sex with casual partners: Findings from a daily diary study of alcohol use and sexual behavior. J. Adolesc. Health 2009, 44, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Farchi, S.; Molino, N.; Giorgi Rossi, P.; Borgia, P.; Krzyzanowski, M.; Dalbokova, D.; Kim, R. Health risk behaviors among adolescents who do and do not attend school—United States, 1992. MMWR Morb. Mortal. Wkly. Rep. 1994, 43, 129–132. [Google Scholar]
- Gowen, L.K.; Winges-Yanez, N. Lesbian, gay, bisexual, transgender, queer, and questioning youths’ perspectives of inclusive school-based sexuality education. J. Sex. Res. 2014, 51, 788–800. [Google Scholar] [CrossRef] [PubMed]
- Boyce, K.S.; Travers, M.; Rothbart, B.; Santiago, V.; Bedell, J. Adapting Evidence-Based Teen Pregnancy Programs to Be LGBT-Inclusive: Lessons Learned. Health Promot. Pract. 2018. [Google Scholar] [CrossRef] [PubMed]
- Raifman, J.; Beyrer, C.; Arrington-Sanders, R. HIV Education and Sexual Risk Behaviors Among Young Men Who Have Sex with Men. LGBT Health 2018, 5, 131–138. [Google Scholar] [CrossRef] [PubMed]
| n | % ** | |
|---|---|---|
| Sex of Partner | ||
| Male | 2207 | 3.3 |
| Female | 61,631 | 96.7 |
| Condom Use at Last Sex | ||
| Yes | 45,339 | 70.0 |
| No | 18,499 | 30.0 |
| Drug/Alcohol Use at Last Sex | ||
| Yes | 13,573 | 21.3 |
| No | 50,265 | 78.7 |
| Condom & Drug/Alcohol Use at Last Sex | ||
| Condom use & no drug/alcohol use | 36,554 | 56.5 |
| Condom use & drug/alcohol use | 8785 | 13.5 |
| No condom use & no drug/alcohol use | 13,711 | 22.2 |
| No condom use & drug/alcohol use | 4788 | 7.8 |
| Grade | ||
| 9th | 11,442 | 17.6 |
| 10th | 15,044 | 22.5 |
| 11th | 18,140 | 26.9 |
| 12th | 19,212 | 33.1 |
| Race/Ethnicity | ||
| White | 26,548 | 48.7 |
| Black | 13,053 | 20.3 |
| Hispanic/Latino | 16,853 | 24.7 |
| Other Race | 7384 | 6.3 |
| β | SE | p-Value | OR | 95% CI | |
|---|---|---|---|---|---|
| Race/Ethnicity | |||||
| White | REF | ||||
| Black | 0.24 | 0.11 | 0.046 | 1.26 | (1.00, 1.59) |
| Hispanic | 0.16 | 0.16 | 0.309 | 1.18 | (0.86, 1.61) |
| Other | 0.41 | 0.14 | 0.005 | 1.50 | (1.13, 1.99) |
| Grade | |||||
| 9th | -0.18 | 0.14 | 0.209 | 0.84 | (0.63, 1.10) |
| 10th | -0.25 | 0.13 | 0.056 | 0.78 | (0.60, 1.01) |
| 11th | 0.04 | 0.13 | 0.735 | 1.05 | (0.81, 1.35) |
| 12th | REF | ||||
| M1: No Interaction | M2: Interaction Model | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | p-Value | OR | 95% CI | β | SE | p-Value | OR | 95% CI | |
| Condom Use at Last Sex | ||||||||||
| Yes | −0.95 | 0.08 | <0.001 | 0.39 | (0.33, 0.46) | −0.97 | 0.09 | <0.001 | 0.38 | (0.32, 0.45) |
| No | REF | |||||||||
| Drug/Alcohol Use at Last Sex | ||||||||||
| Yes | 0.05 | 0.12 | 0.650 | 1.06 | (0.84, 1.33) | 0.00 | 0.15 | 0.980 | 1.00 | (0.75, 1.35) |
| No | REF | |||||||||
| Grade | ||||||||||
| 9th | −0.15 | 0.15 | 0.318 | 0.86 | (0.65, 1.15) | −0.15 | 0.15 | 0.323 | 0.86 | (0.65, 1.15) |
| 10th | −0.19 | 0.14 | 0.162 | 0.83 | (0.63, 1.08) | −0.19 | 0.14 | 0.164 | 0.83 | (0.63, 1.08) |
| 11th | 0.08 | 0.14 | 0.558 | 1.08 | (0.83, 1.41) | 0.08 | 0.14 | 0.556 | 1.08 | (0.83, 1.41) |
| 12th | REF | |||||||||
| Race/Ethnicity | ||||||||||
| White | REF | |||||||||
| Black | 0.33 | 0.12 | 0.007 | 1.39 | (1.10, 1.77) | 0.33 | 0.12 | 0.007 | 1.39 | (1.10, 1.77) |
| Hispanic | 0.16 | 0.17 | 0.352 | 1.17 | (0.84, 1.64) | 0.16 | 0.17 | 0.352 | 1.17 | (0.84, 1.64) |
| Other | 0.42 | 0.15 | 0.004 | 1.53 | (1.14, 2.05) | 0.43 | 0.15 | 0.004 | 1.53 | (1.14, 2.05) |
| Condom Use × Drug/Alcohol Use | 0.11 | 0.2 | 0.580 | 1.12 | (0.75, 1.66) | |||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Phillips, G.; Kalmin, M.M.; Turner, B.; Felt, D.; Marro, R.; Salamanca, P.; Beach, L.B. Condom and Substance Use at Last Sex: Differences between MSMO and MSWO High School Youth. Int. J. Environ. Res. Public Health 2018, 15, 995. https://doi.org/10.3390/ijerph15050995
Phillips G, Kalmin MM, Turner B, Felt D, Marro R, Salamanca P, Beach LB. Condom and Substance Use at Last Sex: Differences between MSMO and MSWO High School Youth. International Journal of Environmental Research and Public Health. 2018; 15(5):995. https://doi.org/10.3390/ijerph15050995
Chicago/Turabian StylePhillips, Gregory, Mariah M. Kalmin, Blair Turner, Dylan Felt, Rachel Marro, Paul Salamanca, and Lauren B. Beach. 2018. "Condom and Substance Use at Last Sex: Differences between MSMO and MSWO High School Youth" International Journal of Environmental Research and Public Health 15, no. 5: 995. https://doi.org/10.3390/ijerph15050995
APA StylePhillips, G., Kalmin, M. M., Turner, B., Felt, D., Marro, R., Salamanca, P., & Beach, L. B. (2018). Condom and Substance Use at Last Sex: Differences between MSMO and MSWO High School Youth. International Journal of Environmental Research and Public Health, 15(5), 995. https://doi.org/10.3390/ijerph15050995





