Comparative Evaluation of Arabin Pessary and Cervical Cerclage for the Prevention of Preterm Labor in Asymptomatic Women with High Risk Factors
Abstract
1. Introduction
2. Materials and Methods
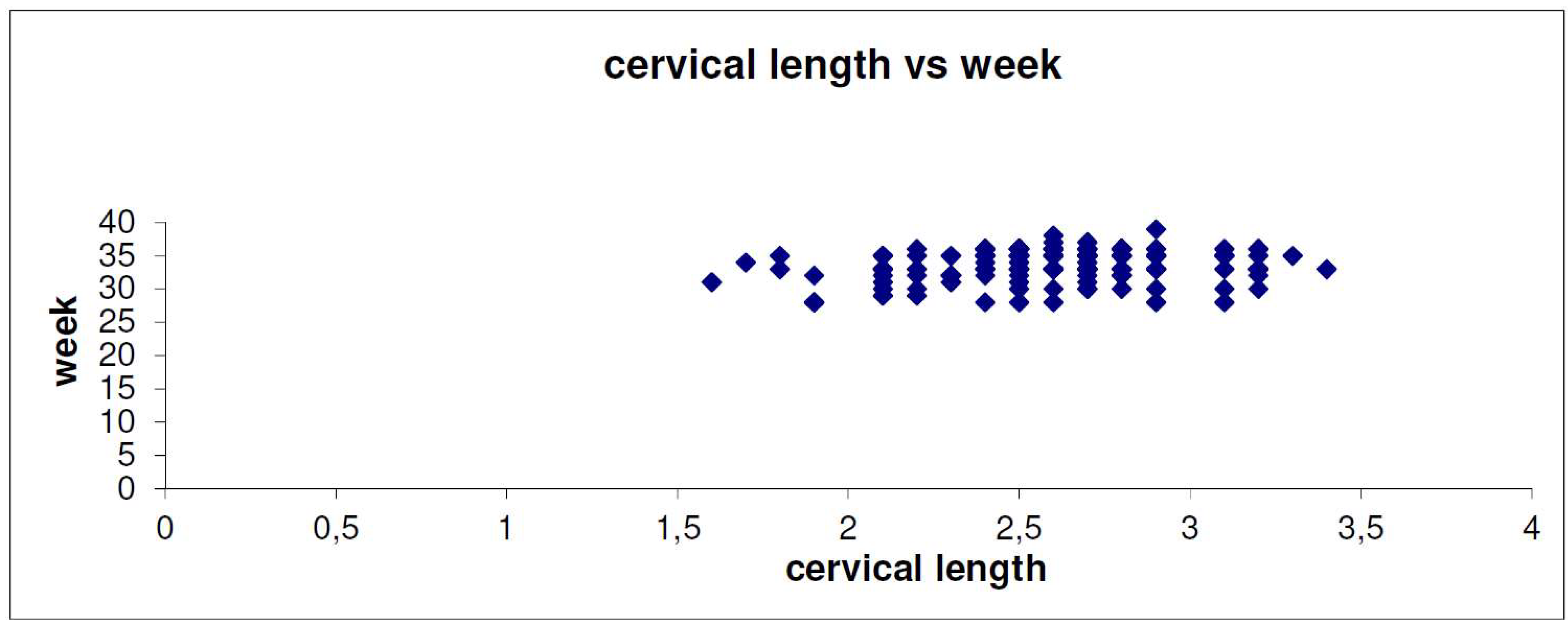
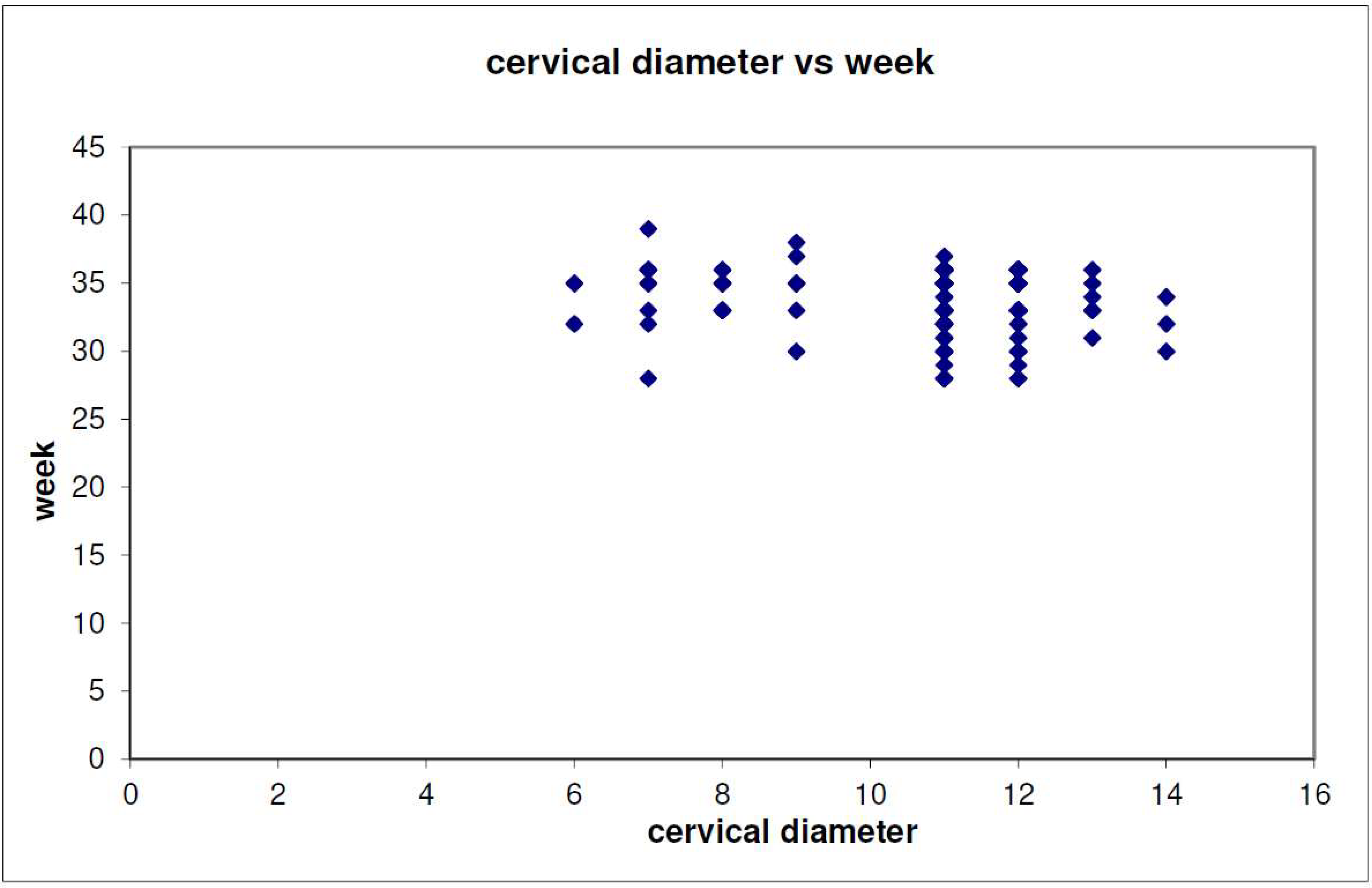
3. Results
4. Discussion
Prevention of Preterm Birth
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Wise, J. NICE guideline aims to cut premature birth rates. BMJ 2015, 351, h6253. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.; Butt, K.; Crane, J.M. SOGC Clinical Practice Guideline. Ultrasonographic cervical length assessment in predicting preterm birth in singleton pregnancies. J. Obstet. Gynaecol. Can. 2011, 33, 486–499. [Google Scholar] [CrossRef]
- Slattery, M.M.; Morrison, J.J. Preterm delivery. Lancet 2002, 360, 1489–1497. [Google Scholar] [CrossRef]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Chang, H.H.; Larson, J.; Blencowe, H.; Spong, C.Y.; Howson, C.P.; Cairns-Smith, S.; Lackritz, E.M.; Lee, S.K.; Mason, E.; Serazin, A.C.; et al. Born Too Soon Preterm prevention analysis group. Preventing preterm births: Analysis of trends and potential reductions with interventions in 39 countries with very high human development index. Lancet 2013, 381, 223–234. [Google Scholar] [CrossRef]
- Blencowe, H.; Cousens, S.; Oestergaard, M.Z.; Chou, D.; Moller, A.B.; Narwal, R.; Adler, A.; Vera Garcia, C.; Rohde, S.; Say, L.; et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. Lancet 2012, 379, 2162–2172. [Google Scholar] [CrossRef]
- Finnström, O.; Olausson, P.O.; Sedin, G.; Serenius, F.; Svenningsen, N.; Thiringer, K.; Tunell, R.; Wennergren, M.; Wesström, G. The Swedish national prospective study on extremely low birthweight (ELBW) infants. Incidence, mortality, morbidity and survival in relation to level of care. Acta Paediatr. 1997, 86, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Papageorghiou, A.T.; Knight, H.E.; Gravett, M.G.; Iams, J.; Waller, S.A.; Kramer, M.; Culhane, J.F.; Barros, F.C.; Conde-Agudelo, A.; et al. The preterm birth syndrome: A prototype phenotypic classification. Am. J. Obstet. Gynecol. 2012, 206, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, R.L.; Gravett, M.G.; Iams, J.; Papageorghiou, A.T.; Waller, S.A.; Kramer, M.; Culhane, J.; Barros, F.; Conde-Agudelo, A.; Bhutta, Z.A.; et al. The preterm birth syndrome: Issues to consider in creating a classification system. Am. J. Obstet. Gynecol. 2012, 206, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Berghella, V.; Tolosa, J.E.; Kuhlman, K.; Weiner, S.; Bolognese, R.J.; Wapner, R.J. Cervical ultrasonography compared with manual examination as a predictor of preterm delivery. Am. J. Obstet. Gynecol. 1997, 177, 723–730. [Google Scholar] [CrossRef]
- Berghella, V.; Kuhlman, K.; Weiner, S.; Texeira, L.; Wapner, R.J. Cervical funneling: Sonographic criteria predictive of preterm delivery. Ultrasound Obstet. Gynecol. 1997, 10, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Owen, J.; Yost, N.; Berghella, V.; MacPherson, C.; Swain, M.; Dildy, G.A., 3rd; Miodovnik, M.; Langer, O.; Sibai, B. Maternal-Fetal Medicine Units Network. Can shortened midtrimester cervical length predict very early spontaneous preterm birth? Am. J. Obstet. Gynecol. 2004, 191, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Drakeley, A.J.; Roberts, D.; Alfirevic, Z. Cervical cerclage for prevention of preterm delivery: Meta-analysis of randomized trials. Obstet. Gynecol. 2003, 102, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Arabin, B.; Halbesma, J.R.; Vork, F.; Hübener, M.; van Eyck, J. Is treatment with vaginal pessaries an option in patients with a sonographically detected short cervix? J. Perinat. Med. 2003, 31, 122–133. [Google Scholar] [CrossRef] [PubMed]
- Iams, J.D. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network What have we learned about uterine contractions and preterm birth? The HUAM Prediction Study. Semin Perinatol. 2003, 27, 204–211. [Google Scholar] [CrossRef]
- Miller, E.S.; Tita, A.T.; Grobman, W.A. Second-Trimester Cervical Length Screening Among Asymptomatic Women: An Evaluation of Risk-Based Strategies. Obstet. Gynecol. 2015, 126, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Shennan, A.; Jones, B. The cervix and prematurity: Aetiology, prediction and prevention. Semin. Fetal Neonatal Med. 2004, 9, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Westergren-Thorsson, G.; Norman, M.; Björnsson, S.; Endrésen, U.; Stjernholm, Y.; Ekman, G.; Malmström, A. Differential expressions of mRNA for proteoglycans, collagens and transforming growth factor-beta in the human cervix during pregnancy and involution. Biochim. Biophys. Acta 1998, 1406, 203–213. [Google Scholar] [CrossRef]
- Iwahashi, M.; Muragaki, Y.; Ooshima, A.; Umesaki, N. Decreased type I collagen expression in human uterine cervix during pregnancy. J. Clin. Endocrinol. Metab. 2003, 88, 2231–2235. [Google Scholar] [CrossRef] [PubMed]
- Törnblom, S.A.; Klimaviciute, A.; Byström, B.; Chromek, M.; Brauner, A.; Ekman-Ordeberg, G. Non-infected preterm parturition is related to increased concentrations of IL-6, IL-8 and MCP-1 in human cervix. Reprod. Biol. Endocrinol. 2005, 3, 39. [Google Scholar] [CrossRef] [PubMed]
- Törnblom, S.A.; Maul, H.; Klimaviciute, A.; Garfield, R.E.; Byström, B.; Malmström, A.; Ekman-Ordeberg, G. mRNA expression and localization of bNOS, eNOS and iNOS in human cervix at preterm and term labour. Reprod. Biol. Endocrinol. 2005, 3, 33. [Google Scholar] [CrossRef] [PubMed]
- Honest, H.; Bachmann, L.M.; Coomarasamy, A.; Gupta, J.K.; Kleijnen, J.; Khan, K.S. Accuracy of cervical transvaginal sonography in predicting preterm birth: A systematic review. Ultrasound Obstet. Gynecol. 2003, 22, 305–322. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Reeves, M.; Owen, J.; Keith, L.G. Precocious cervical ripening as a screening target to predict spontaneous preterm delivery among asymptomatic singleton pregnancies: A systematic review. Am. J. Obstet. Gynecol. 2015, 212, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Spong, C.Y. Prediction and prevention of recurrent spontaneous preterm birth. Obstet. Gynecol. 2007, 110, 405–415. [Google Scholar] [CrossRef] [PubMed]
- Owen, J.; Yost, N.; Berghella, V.; Thom, E.; Swain, M.; Dildy, G.A., 3rd; Miodovnik, M.; Langer, O.; Sibai, B.; McNellis, D. National Institute of Child Health and Human Development, Maternal-Fetal Medicine Units Network. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA 2001, 286, 1340–1348. [Google Scholar] [CrossRef] [PubMed]
- Owen, J.; Szychowski, J.M.; Hankins, G.; Iams, J.D.; Sheffield, J.S.; Perez-Delboy, A.; Berghella, V.; Wing, D.A.; Guzman, E.R.; Vaginal Ultrasound Trial Consortium. Does midtrimester cervical length ≥25 mm predict preterm birth in high-risk women? Am. J. Obstet. Gynecol. 2010, 203, 393e1–393e5. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, R.L.; Iams, J.D.; Miodovnik, M.; Van Dorsten, J.P.; Thurnau, G.; Bottoms, S.; Mercer, B.M.; Meis, P.J.; Moawad, A.H.; Das, A.; et al. The preterm prediction study: Risk factors in twin gestations. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am. J. Obstet. Gynecol. 1996, 175, 1047–1053. [Google Scholar] [CrossRef]
- To, M.S.; Skentou, C.; Cicero, S.; Liao, A.W.; Nicolaides, K.H. Cervical length at 23 weeks in triplets: Prediction of spontaneous preterm delivery. Ultrasound Obstet. Gynecol. 2000, 16, 515–518. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, M.S.; Szychowski, J.M.; Owen, J.; Hankins, G.; Iams, J.D.; Sheffield, J.S.; Perez-Delboy, A.; Berghella, V.; Wing, D.A.; Guzman, E.R.; et al. Cervical funneling: Effect on gestational length and ultrasound-indicated cerclage in high-risk women. Am. J. Obstet. Gynecol. 2010, 203, 259e1–259e5. [Google Scholar] [CrossRef] [PubMed]
- Tsikouras, P.; Galazios, G.; Zalvanos, A.; Bouzaki, A.; Athanasiadis, A. Transvaginal sonographic assessment of the cervix and preterm labor. Clin. Exp. Obstet. Gynecol. 2007, 34, 159–162. [Google Scholar] [PubMed]
- Mella, M.T.; Mackeen, A.D.; Gache, D.; Baxter, J.K.; Berghella, V. The utility of screening for historical risk factors for preterm birth in women with known second trimester cervical length. J. Matern. Fetal Neonatal Med. 2013, 26, 710–715. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, A.; Harper, L.M.; Szychowski, J.M.; Owen, J. Predictive Value of Initial Cervical Length for Subsequent Cervical Length Shortening in Women with a Prior Preterm Birth. Am. J. Perinatol. 2016, 33, 350–355. [Google Scholar] [PubMed]
- Orzechowski, K.M.; Boelig, R.; Nicholas, S.S.; Baxter, J.; Berghella, V. Is universal cervical length screening indicated in women with prior term birth? Am. J. Obstet. Gynecol. 2015, 212, 234e1–234e5. [Google Scholar] [CrossRef] [PubMed]
- Geitona, M.; Hatzikou, M.; Hatzistamatiou, Z.; Anastasiadou, A.; Theodoratou, T.D. The economic burden of treating neonates in Intensive Care Units (ICUs) in Greece. Cost Eff. Resour. Alloc. 2007, 5, 9. [Google Scholar] [CrossRef] [PubMed]
- Boelig, R.C.; Orzechowski, K.M.; Berghella, V. Cervical length, risk factors, and delivery outcomes among women with spontaneous preterm birth. J. Matern. Fetal Neonatal Med. 2016, 29, 2840–2844. [Google Scholar] [CrossRef] [PubMed]
- Kuusela, P.; Jacobsson, B.; Söderlund, M.; Bejlum, C.; Almström, E.; Ladfors, L.; Hagberg, H.; Wennerholm, U.B. Transvaginal sonographic evaluation of cervical length in the second trimester of asymptomatic singleton pregnancies, and the risk of preterm delivery. Acta Obstet. Gynecol. Scand. 2015, 94, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Szychowski, J.M.; Owen, J.; Hankins, G.; Iams, J.D.; Sheffield, J.S.; Perez-Delboy, A.; Berghella, V.; Wing, D.A.; Guzman, E.R. Vaginal Ultrasound Trial Consortium Can the optimal cervical length for placing ultrasound-indicated cerclage be identified? Ultrasound Obstet. Gynecol. 2016, 48, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Chandiramani, M.; Shennan, A. Preterm labour: Update on prediction and prevention strategies. Curr. Opin. Obstet. Gynecol. 2006, 18, 618–624. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, E.B.; Celik, E.; Parra, M.; Singh, M.; Nicolaides, K.H. Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N. Engl. J. Med. 2007, 357, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Kyvernitakis, I.; Khatib, R.; Stricker, N.; Arabin, B. Is Early Treatment with a Cervical Pessary an Option in Patients with a History of Surgical Conisation and a Short Cervix? Geburtshilfe Frauenheilkd. 2014, 74, 1003–1008. [Google Scholar] [CrossRef] [PubMed]
- Goya, M.; Pratcorona, L.; Merced, C.; Rodó, C.; Valle, L.; Romero, A.; Juan, M.; Rodríguez, A.; Muñoz, B.; Santacruz, B.; et al. Pesario Cervical para Evitar Prematuridad (PECEP) Trial GroupCervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet 2012, 379, 1800–1806. [Google Scholar] [CrossRef]
- Liem, S.; Schuit, E.; Hegeman, M.; Bais, J.; de Boer, K.; Bloemenkamp, K.; Brons, J.; Duvekot, H.; Bijvank, B.N.; Franssen, M.; et al. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): A multicentre, open-label randomised controlled trial. Lancet 2013, 382, 1341–1349. [Google Scholar] [CrossRef]
- Barinov, S.V.; Shamina, I.V.; Lazareva, O.V.; Tirskaya, Y.I.; Ralko, V.V.; Shkabarnya, L.L.; Dikke, G.B.; Kochev, D.M.; Klementyeva, L.L. Comparative assessment of arabin pessary, cervical cerclage and medical management for preterm birth prevention in high-risk pregnancies. J. Matern. Fetal Neonatal Med. 2017, 30, 1841–1846. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, M.; Goya, M.; Gascón, A.; Pratcorona, L.; Merced, C.; Rodó, C.; Valle, L.; Romero, A.; Juan, M.; Rodríguez, A.; et al. Modification of cervical length after cervical pessary insertion: Correlation weeks of gestation. J. Matern. Fetal Neonatal Med. 2017, 30, 1596–1601. [Google Scholar] [CrossRef] [PubMed]
- Mateus, J. Clinical management of the short cervix. Obstet. Gynecol. Clin. N. Am. 2011, 38, 367–385. [Google Scholar] [CrossRef] [PubMed]
- Nam, K.H.; Kwon, J.Y.; Kim, Y.H.; Park, Y.W. Pregnancy outcome after cervical conization: Risk factors for preterm delivery and the efficacy of prophylactic cerclage. J. Gynecol. Oncol. 2010, 21, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Berghella, V.; Ciardulli, A.; Rust, O.A.; To, M.; Otsuki, K.; Althuisius, S.; Nicolaides, K.; Roman, A.; Saccone, G. Cerclage for Short Cervix on Ultrasound in Singleton Gestations without Prior Spontaneous Preterm Birth: A Systematic Review and Meta-analysis of Trials using individual patient-level data. Ultrasound Obstet. Gynecol. 2017, 50, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Norman, J.E. Preterm labour. Cervical function and prematurity. Best Pract. Res. Clin. Obstet. Gynaecol. 2007, 21, 791–806. [Google Scholar] [CrossRef] [PubMed]
| # of Women | % | ||
|---|---|---|---|
| Cervical length <2.7 cm | 95 | 57.2 | |
| Dilatation of internal cervical os ≥10 mm | 138 | 83.1 | |
| Cervical funneling | 51 | 30.7 | |
| Cervical cerclage | 20 | 12 | |
| Pessary | 124 | 74 | |
| Preterm labor <33 weeks | 39 | 23.5 | |
| Mode of delivery | Normal vaginal delivery | 61 | 36.7 |
| Vacuum extraction | 9 | 5.4 | |
| Cesarean section | 96 | 57.8 | |
| Cervical Characteristics | # of Women | % | p | |
|---|---|---|---|---|
| Cervical length | <2.7 cm | 24 | 25.6 | 0.534 |
| ≥2.7 cm | 15 | 21.12 | ||
| Dilatation of internal cervical os | >10 mm | 35 | 25.3 | 0.210 |
| ≤10 mm | 4 | 14.2 | ||
| Cervical funneling | No | 19 | 19.8 | <0.001 |
| Yes | 20 | 39.2 |
| Caption | # of Women | % | p | |
|---|---|---|---|---|
| Cervical cerclage | No | 29 | 19.6 | 0.003 |
| Yes | 10 | 50 | ||
| Pessary | No | 9 | 21.4 | 0.717 |
| Yes | 30 | 24.2 |
| Cervical characteristics | OR | CI | p |
|---|---|---|---|
| Cervical length <2.7 cm | 0.792 | 0.38–1.651 | 0.537 |
| Dilatation of internal cervical os >10 cm | 2.039 | 0.665–6.285 | 0.215 |
| Funneling | 3.260 | 1.544–6.881 | 0.002 |
| Cervical cerclage | 4.034 | 1.535–10.603 | 0.005 |
| Pessary | 1.170 | 0.503–2.721 | 0.715 |
| Pessary | Cerclage | # of Women | # of Early Preterm Labor Women | p |
|---|---|---|---|---|
| No | No | 40 | 8 | <0.05 |
| Yes | No | 106 | 21 | 0.139 |
| No | Yes | 2 | 1 | 0.401 |
| Yes | Yes | 18 | 9 | <0.05 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsikouras, P.; Anastasopoulos, G.; Maroulis, V.; Bothou, A.; Chalkidou, A.; Deuteraiou, D.; Anthoulaki, X.; Tsatsaris, G.; Bourazan, A.H.; Iatrakis, G.; et al. Comparative Evaluation of Arabin Pessary and Cervical Cerclage for the Prevention of Preterm Labor in Asymptomatic Women with High Risk Factors. Int. J. Environ. Res. Public Health 2018, 15, 791. https://doi.org/10.3390/ijerph15040791
Tsikouras P, Anastasopoulos G, Maroulis V, Bothou A, Chalkidou A, Deuteraiou D, Anthoulaki X, Tsatsaris G, Bourazan AH, Iatrakis G, et al. Comparative Evaluation of Arabin Pessary and Cervical Cerclage for the Prevention of Preterm Labor in Asymptomatic Women with High Risk Factors. International Journal of Environmental Research and Public Health. 2018; 15(4):791. https://doi.org/10.3390/ijerph15040791
Chicago/Turabian StyleTsikouras, Panagiotis, George Anastasopoulos, Vasileios Maroulis, Anastasia Bothou, Anna Chalkidou, Dorelia Deuteraiou, Xanthoula Anthoulaki, Georgios Tsatsaris, Arzou Halil Bourazan, George Iatrakis, and et al. 2018. "Comparative Evaluation of Arabin Pessary and Cervical Cerclage for the Prevention of Preterm Labor in Asymptomatic Women with High Risk Factors" International Journal of Environmental Research and Public Health 15, no. 4: 791. https://doi.org/10.3390/ijerph15040791
APA StyleTsikouras, P., Anastasopoulos, G., Maroulis, V., Bothou, A., Chalkidou, A., Deuteraiou, D., Anthoulaki, X., Tsatsaris, G., Bourazan, A. H., Iatrakis, G., Zervoudis, S., Galazios, G., Inagamova, L.-K., Csorba, R., & Teichmann, A.-T. (2018). Comparative Evaluation of Arabin Pessary and Cervical Cerclage for the Prevention of Preterm Labor in Asymptomatic Women with High Risk Factors. International Journal of Environmental Research and Public Health, 15(4), 791. https://doi.org/10.3390/ijerph15040791








