From Content Knowledge to Community Change: A Review of Representations of Environmental Health Literacy
Abstract
:1. Introduction
2. Methods
2.1. Definitions and Search Methods
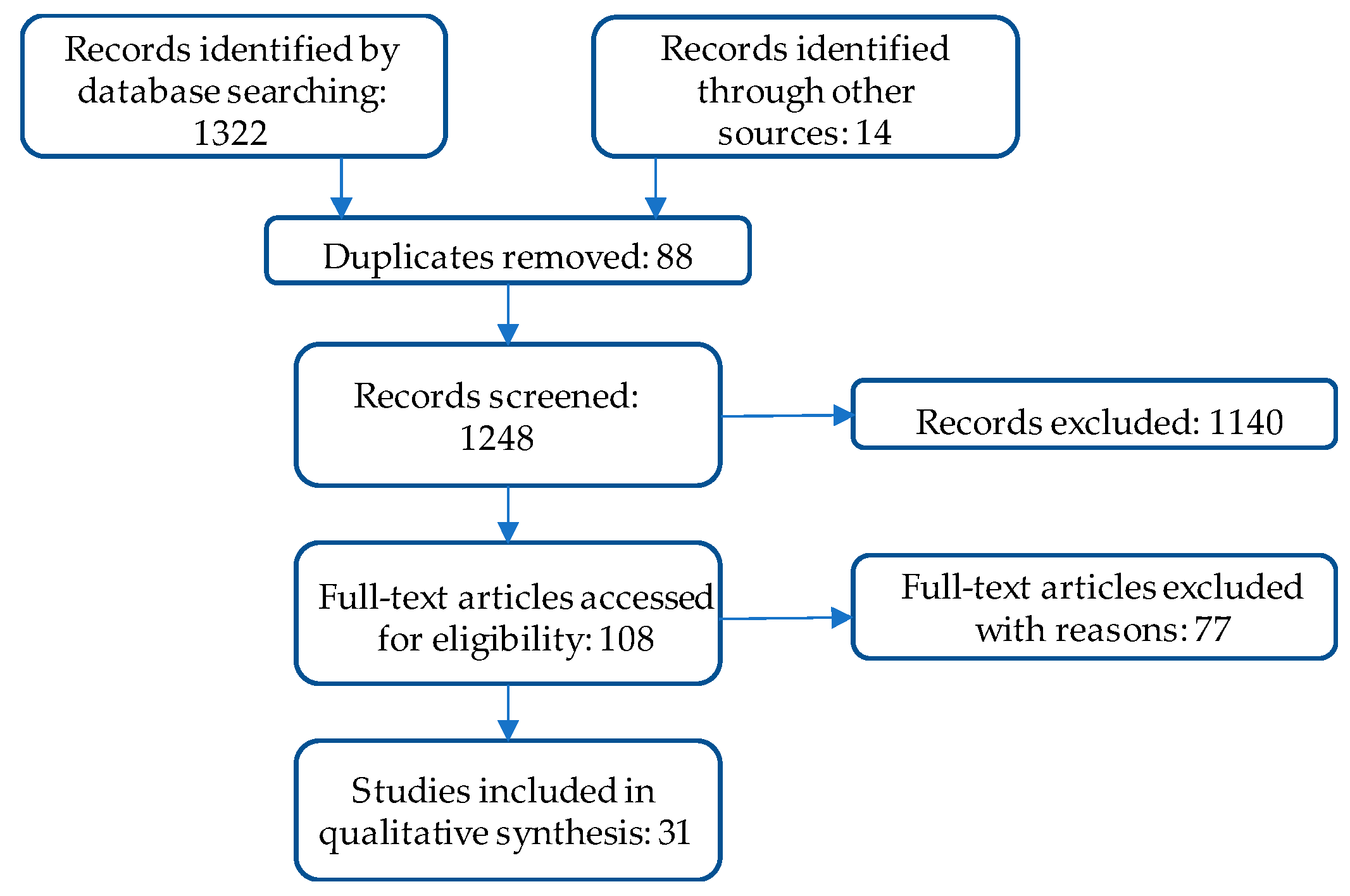
2.2. Screening Methods
3. Results
- Individual-level EHL was described as: (a) understanding the connection between environmental exposures and health; (b) representations of content knowledge, such as a score on a survey of environmental health knowledge or gains in content knowledge demonstrated with pre/post-assessments; and, (c) behavior changes reported in response to environmental exposures.
- EHL that spanned individual and community levels appeared in biomonitoring studies that emphasized “report-back” of individual and community-wide results to participants.
- Community-level EHL was represented as community change or collective action reported in response to environmental exposures.
3.1. Individual Level EHL: Understanding the Connection between Environmental Exposures and Health
3.2. Individual Level EHL: Representations of Content Knowledge
3.2.1. Community Settings
3.2.2. Formal Educational Settings
3.3. Individual Level EHL: Behavior Change in Response to Environmental Exposures
The Role of Community Health Workers
3.4. Spanning Individual and Community-Level EHL: Participation in Report-Back Studies
3.5. Community Level EHL: Community Changes or Collective Action in Response to Environmental Exposure
4. Discussion
- Awareness and understanding: This dimension incorporates the broad recognition that environmental exposures and socio-cultural dynamics influence health. Such awareness may occur in the context of a specific environmental exposure (such as arsenic in groundwater); and, an individual may have varying levels of awareness across different exposures, as represented by Finn and O’Fallon [1]. Alternately, this awareness may reflect a more general understanding that environmental exposures interact with biological processes to cause negative health outcomes. Presumably, either type of understanding would incorporate some recognition of the limits of current science and uncertainty in scientific research.
- Skills that enable health protective decision-making and self-efficacy associated with those skills: This dimension incorporates social cognitive theory by focusing on an individual’s self-efficacy for reducing harmful environmental exposures as well as beliefs about her/his potential to influence a specific outcome. Mastery of relevant skills is an important component of this dimension; and such skills may be general in nature (e.g., the ability to find and understand scientific information or the ability to participate in community decision-making) or exposure-specific (e.g., the ability to take steps to reduce environmental asthma triggers in a home).
- Community change or collective action to reduce or remove harmful environmental exposures: In this dimension, both individuals and groups apply their knowledge and skills, in the context of self-efficacy for the desired behavior change, to reduce harmful environmental exposures and improve health. This review suggests that community change outcomes may require an overarching theoretical framework that engages participants throughout the research process and taps into their funds of knowledge and self-efficacy.
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- Finn, S.; O’Fallon, L. The emergence of environmental health literacy—From its roots to is future potential. Environ. Health Perspect. 2017, 125, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Society for Public Health Education. What Is Environmental Health Literacy? Available online: http://www.sophe.org/environmentalhealth/key_ehl.asp (accessed on 4 May 2017).
- Zarcadoolas, C.; Timm, E.; Bibeault, L. Brownfields: A case study in partnering with residents to develop an easy-to-read print guide. J. Environ. Health 2001, 64, 15–20. [Google Scholar] [PubMed]
- National Academies of Sciences, Engineering, and Medicine. Science Literacy: Concepts, Contexts, and Consequences; Snow, C.E., Dibner, K.A., Eds.; National Academies Press: Washington, DC, USA, 2016. [Google Scholar]
- American Association for the Advancement of Science (AAAS). Science for All Americans; Oxford University: New York, NY, USA, 1990; Available online: http://www.project2061.org/publications/sfaa/online/sfaatoc.htm (accessed on 4 May 2017).
- Laugksch, R.C. Scientific literacy: A conceptual overview. Sci. Educ. 2000, 84, 71–94. [Google Scholar] [CrossRef]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Committee on Health Literacy. Health Literacy: A Prescription to End Confusion; Nielsen-Bohlman, L., Panzer, A.M., Kindig, D.A., Eds.; The National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- Freedman, D.A.; Bess, K.D.; Tucker, H.A.; Boyd, D.L.; Tuchman, A.M.; Wallston, K.A. Public health literacy defined. Am. J. Prev. Med. 2009, 36, 446–451. [Google Scholar] [CrossRef] [PubMed]
- North American Association for Environmental Education. Developing a Framework for Assessing Environmental Literacy: Executive Summary. Available online: https://naaee.org/sites/default/files/envliteracyexesummary.pdf (accessed on 15 December 2017).
- Cole, A.G. Expanding the field: Revisiting environmental education principles through multidisciplinary frameworks. J. Environ. Educ. 2007, 38, 35–44. [Google Scholar] [CrossRef]
- Hoover, A.G. Connecting Disciplines to Inform and Develop the Emerging Field of Environmental Health Literacy. Available online: https://www.niehs.nih.gov/research/supported/assets/docs/a_c/connecting_disciplines_to_inform_and_develop_the_emerging_field_of_environmental_health_literacy_508.pdf (accessed on 24 June 2014).
- Marsili, D. A cross-disciplinary approach to global environmental health: The case of contaminated sites. Annali Instituto Superiore Sanita 2016, 52, 516–523. [Google Scholar]
- Chan, L.M.; Chalupka, S.M.; Barrett, R. Female college student awareness of exposures to environmental toxins in personal care products and their effect on preconception health. Workplace Health Saf. 2015, 63, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Barrett, E.S.; Velez, M.; Conn, K.; Heinert, S.; Qiu, X. Using the Health Belief Model to illustrate factors that influence risk assessment during pregnancy and implications for prenatal education about endocrine disruptors. Policy Futures Educ. 2014, 12, 961–974. [Google Scholar] [CrossRef]
- Barrett, E.S.; Sathyanarayana, S.; Janssen, S.; Redmon, J.B.; Nguyen, R.H.; Kobrosly, R.; Swan, S.H. Environmental health attitudes and behaviors: Findings from a large pregnancy cohort study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 176, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Bogar, S.; Szabo, A.; Woodruff, S.; Johnson, S. Urban youth knowledge and attitudes regarding lead poisoning. J. Community Health 2017, 42, 1255–1266. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.K.; Lopez, A.; Malloy, N.; Morello-Frosch, R. Surveying for environmental health justice: Community organizing applications of community-based participatory research. Environ. Justice 2014, 9, 129–136. [Google Scholar] [CrossRef]
- Schure, M.B.; Kile, M.L.; Harding, A.; Harper, B.; Harris, S.; Uesugi, S.; Goins, R.T. Perceptions of the environment and health among members of the Confederated Tribes of the Umatilla Indian Reservation. Environ. Justice 2013, 6, 115–120. [Google Scholar] [CrossRef] [PubMed]
- White, B.M.; Hall, E.; Johnson, C. Environmental health literacy in support of social action: An environmental justice perspective. J. Environ. Health 2014, 77, 24–29. [Google Scholar] [PubMed]
- Dixon, J.K.; Hendrickson, K.C.; Ercolano, E.; Quackenbush, R.; Dickson, J.P. The Environmental Health Engagement Profile: What people think and do about environmental health. Public Health Nurs. 2009, 26, 460–473. [Google Scholar] [CrossRef] [PubMed]
- Ratnapradipa, D.; Wodika, A.B.; Brown, S.L.; Preihs, K. What does the public know about environmental health? A qualitative approach to refining an environmental health awareness instrument. J. Environ. Health 2015, 77, 22–28. [Google Scholar] [PubMed]
- Brenner, B.; Evans, S.; Miller, K.; Weinberg, L.; Rothenberg, A.; Martinez, C.; Jandorf, L. Breast cancer and the environment: Reaching multicultural communities; Advocates mentoring advocates. Environ. Justice 2015, 8, 117–125. [Google Scholar] [CrossRef]
- Cohen, A.K.; Waters, A.; Brown, P. Place-based environmental health justice education: A community-university-government-middle school partnership. Environ. Justice 2012, 5, 188–197. [Google Scholar] [CrossRef]
- Ferguson, A.; Kavouras, I.; Ulmer, R.; Harris, K.; Helm, R.; Bursac, Z. Environmental health education for teachers: Results of pre- and post-surveys from a pilot study addressing chemical use reduction and integrated pest management in homes. J. Community Med. Health Educ. 2014, 4, 318. [Google Scholar] [CrossRef]
- LePrevost, C.E.; Storm, J.F.; Asuaje, C.R.; Arellano, C.; Cope, W.G. Assessing the effectiveness of the Pesticides and Farmworker Health Toolkit: A curriculum for enhancing farmworkers’ understanding of pesticide safety concepts. J. Agromed. 2014, 19, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.D.; Valenti, M.; Schettler, T.; Tencza, B. A multimedia e-book—A story of health: Filling a gap in environmental health literacy for health professionals. Environ. Health Perspect. 2016, 124, A133–A136. [Google Scholar] [CrossRef] [PubMed]
- Ramos, I.N.; He, O.; Ramos, K.S. Improvements in environmental health literacy along the Texas-Mexico border following community-wide health education. Environ. Justice 2012, 5, 32–37. [Google Scholar] [CrossRef]
- Rosas, L.G.; Trujillo, C.; Camacho, J.; Madrigal, D.; Bradman, A.; Eskenazi, B. Acceptability of health information technology aimed at environmental health education in a prenatal clinic. Patient Educ. Couns. 2014, 97, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Butterfield, P.G.; Hill, W.; Postma, J.; Butterfield, P.W.; Odom-Maryon, T. Effectiveness of a household environmental health intervention delivered by rural public health nurses. Am. J. Public Health 2011, 101, S262–S270. [Google Scholar] [CrossRef] [PubMed]
- Derrick, C.G.; Miller, J.S.A.; Andrews, J.M. A fish consumption study of anglers in an at-risk community: A community-based participatory approach to risk reduction. Public Health Nurs. 2008, 25, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Korfmacher, K.S.; Kuholski, K. Rochester’s healthy home: A community-based innovation to promote environmental health action. Environ. Pract. 2008, 10, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Mankikar, D.; Campbell, C.; Greenberg, R. Evaluation of a home-based environmental and educational intervention to improve health in vulnerable households: Southeastern Pennsylvania lead and healthy homes program. Int. J. Environ. Res. Public Health 2016, 13, 900. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.P.; Rigrod, P.; Wingate, S.; Borsuk, M.E. A community-driven intervention in Tuftonboro, New Hampshire, succeeds in altering water testing behavior. J. Environ. Health 2015, 78, 30–39. [Google Scholar] [PubMed]
- Quandt, S.A.; Grzywacz, J.G.; Talton, J.W.; Trejo, G.; Tapia, J.; D’Agostino, R.B.; Arcury, T.A. Evaluating the effectiveness of a lay health promoter-led, community-based participatory pesticide safety intervention with farmworker families. Health Promot. Pract. 2013, 14, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Zierold, K.M.; Sears, C.G.; Brock, G.N. Exposure-reducing behaviors among residents living near a coal ash storage site. Health Educ. Behav. 2016, 43, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Adams, C.; Brown, P.; Morello-Frosch, R.; Brody, J.G.; Rudel, R.A.; Zota, A.; Patton, S. Disentangling the exposure experience: The roles of community context and report-back of environmental exposure data. J. Health Soc. Behav. 2011, 52, 180–196. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.; Brody, J.G.; Morello-Frosch, R.; Tovar, J.; Zota, A.R.; Rudel, R.A. Measuring the success of community science: The northern California Household Exposure Study. Environ. Health Perspect. 2012, 120, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Haynes, E.N.; Elam, S.; Burns, R.; Spencer, A.; Yancey, E.; Kuhnell, P.; Dietrich, K.N. Community engagement and data disclosure in environmental health research. Environ. Health Perspect. 2016, 124, A24–A27. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, D.S.; Minkler, M.; Parra, K.L.; Mundo, C.; Gonzalez, J.E.; Jimenez, R.; Harley, K.G. Improving Latino youths’ environmental health literacy and leadership skills through participatory research on chemical exposures in cosmetics: The HERMOSA Study. Int. Quart. Community Health Educ. 2016, 36, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Andreotta, M.D.; Brody, J.G.; Lothrop, N.; Loh, W.; Beamer, P.I.; Brown, P. Improving environmental health literacy and justice through environmental exposure results communication. Int. J. Environ. Res. Public Health 2016, 13, 690. [Google Scholar] [CrossRef] [PubMed]
- Emmett, E.A.; Zhang, H.; Shofer, F.S.; Rodway, N.; Desai, C.; Freeman, D.; Hufford, M. Development and successful application of a “Community-First” communication model for community-based environmental health research. J. Occup. Environ. Med. 2009, 5, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Andreotta, M.D.; Brusseau, M.L.; Artiola, J.; Maier, R.M.; Gandolfi, A.J. Building a co-created citizen science program with gardeners neighboring a Superfund site: The Gardenroots case study. Int. Public Health J. 2015, 7, 13. [Google Scholar] [PubMed]
- Ramirez-Andreotta, M.D.; Lothrop, N.; Wilkinson, S.T.; Root, R.A.; Artiola, J.F.; Klimecki, W.; Loh, W. Analyzing patterns of community interest at a legacy mining waste site to assess and inform environmental health literacy efforts. J. Environ. Stud. Sci. 2016, 6, 543–555. [Google Scholar] [CrossRef] [PubMed]
- Ratnapradipa, D.; Brown, S.L.; Middleton, W.K.; Wodika, A.B. Measuring environmental health perception among college students. Health Educ. 2011, 43, 13–20. [Google Scholar]
- Ratnapradipa, D.; Rhodes, D.L.; Brown, S.L. Evaluating pre-service teacher workforce: Environmental health knowledge, attitude and behavior. Online J. Workforce Educ. Dev. 2011, 5, 1–18. [Google Scholar]
- Bandura, A. Health promotion from the perspective of social cognitive theory. Psychol. Health 1998, 13, 623–649. [Google Scholar] [CrossRef]
- O’Fallon, L.; Dearry, A. Community-based participatory research as a tool to advance environmental health sciences. Environ. Health Perspect. 2002, 110, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Vygotsky, L. Interaction between learning and development. In Reading on the Development of Children; Gauvain, M., Cole, M., Eds.; Scientific American Books: New York, NY, USA, 1978; pp. 34–40. [Google Scholar]
- Champion, V.L.; Skinner, C.S. The Health Belief Model. In Health Behavior and Health Education: Theory, Research, and Practice, 4th ed.; Glanz, K., Rimer, B.K., Lewis, F.M., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Freudenberg, N.; Pastor, M.; Israel, B. Strengthening community capacity to participate in making decisions to reduce disproportionate environmental exposures. Am. J. Public Health 2011, 101, S123–S130. [Google Scholar] [CrossRef] [PubMed]

| Author & Date | Journal | Study Participants | Environmental Exposure | Methods | Theoretical Framework | Funding Source |
|---|---|---|---|---|---|---|
| Individual Understanding of Connection between Environmental Exposures and Health | ||||||
| Barrett et al. (2014) [16] | Eur. J. Obs. Gynecol. Reprod. Biol. | 894 pregnant women | Environmental chemicals in personal care products | Questionnaires | Not specified | National Institute of Environmental Health Sciences (NIEHS) |
| Bogar, S., Szabo, A., Woodruff, S., & Johnson, S. (2017) [17] | J. Community Health | 169 urban youth | Lead poisoning and community-identified environmental health (EH) issues | Survey, focus groups | Community-based participatory research (CBPR) | Medical College of Wisconsin, Purple Door Ice Cream |
| Chan, L.M., Chalupka, S.M., & Barrett, R. (2015) [14] | Workplace Health Saf. | 72 female college students | Endocrine disrupting chemicals (EDCs) in personal care products | Survey | Integrated Model for Environmental Health Research | Worcester State Foundation |
| Chen, S., Barrett, E.S., Velez, M., Conn, K., Heinert, S., & Qiu, X. (2014) [15] | Policy Futures Educ. | 124 women | EDC exposure during pregnancy | Semi-structured interviews, survey | Health Belief Model | NIEHS |
| Cohen, A.K., Lopez, A., Malloy, N., & Morello-Frosch, R. (2014) [18] | Environ. Justice | 188 residents of environmental justice (EJ) community in California | Local environmental pollution (e.g., petrochemical industry) & neighborhood stressors | Community health survey | CBPR | Avon Foundation |
| Schure, M.B. et al. (2013) [19] | Environ. Justice | 27 members of the Confederated Tribes of the Umatilla Indian Reservation | Air pollution, water pollution, toxic chemicals | Focus group | Not specified | NIEHS |
| White, B.M., Hall, E.S., & Johnson, C. (2014) [20] | J. Environ. Health | 42 adult residents of Chicago public housing | Environmental hazards in community (air, land & water) | Focus groups, surveys | Not specified | Univ. of Minnesota School of Public Health |
| Representation of Content Knowledge | ||||||
| Scores and Other Representations of Environmental Health Knowledge | ||||||
| Dixon, J.K., Hendrickson, K.C., Ercolano, E., Quackenbush, R., & Dixon, J.P. (2009) [21] | Public Health Nurs. | 433 urban residents in Northeastern state | Varied sources of pollution linked with health effects | Focus groups, in-person and phone interviews | Not specified | NIEHS |
| Ratnapradipa, D., Middleton, W.K., Wodika, A.B., Brown, S., & Priehs, K. (2015) [22] | J. Environ. Health | 32 individuals in 4 states | Range of exposures including air, water, radiation, waste | Focus groups | Not specified | Southern Illinois University |
| Knowledge Gains on Pre/Post-Assessments | ||||||
| Brenner, B., Evans, S., Miller, K., Weinberg, L., Rothenberg, A., Martinez, C., & Jandorf, L. (2015) [23] | Environ. Justice | 12 volunteer educators, 103 workshop participants | EDCs in personal care products and chemicals in cleaners, plastics and pesticides | Focus group, post-workshop evaluation | Not specified | National Cancer Institute (NCI), NIEHS |
| Cohen, A.K., Waters, A., & Brown, P. (2012) [24] | Environ. Justice | Middle school students | Dioxin | Pre/post-surveys, student reflections, writing & discussion | CBPR principles, EJ | NIEHS, Brown Univ. Teaching & Research Award |
| Ferguson, A., Kavouras, I., Ulmer, R., Harris, K., Helm, R., & Bursac, Z. (2014) [25] | J. Community Med. Health Educ. | 35 teachers | Pesticides and other chemicals used in homes | Pre/post-surveys | Cooperative learning | Not specified |
| LePrevost, C.E., Storm, J.F., Asuaje, C.R., Arellano, C., & Cope, W.G. (2014) [26] | J. Agromed. | 20 farmworkers | Pesticides | Pre/post-assessments | Not specified | NC Dept. of Agriculture & Consumer Services |
| Miller, M.D., Valenti, M., Schettler, T., & Tencza, B. (2016) [27] | Environ. Health Perspect. | 304 health professionals | Factors in natural, built chemical, food, economic & social environments | Embedded questions in online course | Not specified | Agency for Toxic Substances and Disease Registry (ATSDR), US Environmental Protection Agency (USEPA) |
| Ramos, I.N., He, Q., & Ramos, K.S. (2012) [28] | Environ. Justice | 498 households in community on Texas-Mexico border | Pesticides, environmental tobacco smoke (ETS), water pollution | Pre/post surveys administered in-person | Not specified | NIEHS |
| Rosas, L.G., Trujillo, C., Camacho, J., Madrigal, D., Bradman, A., & Eskenazi, B. (2014) [29] | Patient Educ. Couns. | 152 pregnant, Spanish-speaking patients | Pesticides, metals, toxic household products, ETS, allergens, indoor & outdoor air pollution | Electronic waiting room kiosk, pre/post-questionnaires | Not specified | California Wellness Foundation, NIEHS, USEPA |
| Individual Behavior Change in Response to Environmental Exposure | ||||||
| Butterfield, P.G., Hill, W., Postma, J., Butterfield, P.W., & Odom-Mayon, T. (2011) [30] | Am. J. Public Health | 235 families in rural areas of two Northwestern states | EH hazards in homes (carbon monoxide (CO), drinking water contaminants, mold, radon) | Pre/post surveys | Translational environmental research in rural areas (TERRA), Social Cognitive Theory, Weinstein’s Precaution Adoption Model | National Institute of Nursing Research (NINR) |
| Derrick, C.G., Miller, J.S., & Andrews, J.M. (2008) [31] | Public Health Nurs. | 23 African-American subsistence anglers residing in public housing | Mercury in fish | Pre/post-surveys | Social cognitive theory | Sigma Theta Tau |
| Korfmacher, K.S. & Kuholski, K. (2008) [32] | Environ. Pract. | 32 visitors to healthy home exhibit | EH hazards in homes (asbestos, CO, ETS, lead, mold, pesticides, radon) | Written surveys on-site, follow-up interviews | Not specified | NIEHS |
| Mankikar, D., Campbell, C. & Greenberg, R. (2016) [33] | Int. J. Environ. Res. Public Health | 150 families participating in healthy homes program | Environmental health hazards in homes (CO, lead, mold, pests) | Pre/post-questionnaires, observations | Not specified | Health Resources & Services Admin. Block Grant |
| Paul, M.P., Rigrod, P., Wingate, S., & Borsuk, M.E. (2015) [34] | J. Environ. Health | 285 well owners | Arsenic in well water | Number of wells sampled | Not specified | NIEHS |
| Quandt et al. (2013) [35] | Health Promot. Pract. | 610 family members of farmworkers | Pesticides | Pre/post-questionnaires | Health Belief Model | National Institute of Occupational Safety and Health (NIOSH) |
| Zierold, K.M., Sears C.G., & Brock, G.N. (2016) [36] | Health Educ. Behav. | 257 residents of community with large coal ash storage site | Coal ash (particulate matter, metals) | Focus groups, survey | Not specified | None |
| Participation in Report-Back Studies | ||||||
| Adams, C. et al. (2011) [37] | J. Health Soc. Behav. | 50 residents of two California communities, one bordering an oil refinery, one comparison | EDCs, pollutants associated with oil refining | Interviews, individual & community meetings | Exposure experience, health social movements, public engagement with science | Not specified |
| Brown, P., Brody, J.G., Morello-Frosch, R., Tovar, J., Zota, A.R., & Rudel, R.A. (2012) [38] | Environ. Health Perspect. | 50 residents of two California communities, one bordering an oil refinery, one comparison | EDCs, polybrominated diphenyl ethers (PBDEs) | Multi-faceted evaluation of ongoing CBPR project | CBPR | NIEHS, National Science Foundation (NSF) |
| Haynes et al. (2016) [39] | Environ. Health Perspect. | 30 participants in exposure study | Airborne manganese | Community input, surveys | Not specified | NIEHS, NINR |
| Madrigal, D.S. et al. (2016) [40] | Int. Q. Community Health Educ. | 15 members of Youth Community Council | EDCs in cosmetics | Written reflections, questionnaires, participant observation | EHL, CBPR | CA Breast Cancer Research Program, NIEHS, USEPA |
| Ramirez-Andreotta, M.D., Brody, J.G., Lothrop, N., Loh, M., Beamer, P.I., & Brown, P. (2016) [41] | Int. J. Environ. Res. Public Health | 17 parents who participated in MESH study | Arsenic | Interviews | EHL, EJ, contextual model of learning | NIEHS |
| Community Change or Collective Action in Response to an Environmental Exposure | ||||||
| Emmett, E.A., Zhang, H., Shofer, F.S., Rodway, N., Desai, C., Freeman, D., & Hufford, M. (2009) [42] | J. Occup. Environ. Med. | Residents of rural Appalachian town in Ohio | Perfluorooctanoate (PFOA) | Participatory research design, community meetings, follow-up surveys | CBPR, EJ | NIEHS |
| Ramirez-Andreotta, M.D., Brusseau, M.L., Artiola, J., Maier, R.M., & Gandolfi, A.J. (2015) [43] | Int. Public Health J. | 18 participants in Gardenroots training | Arsenic | Survey | CBPR, public participation in scientific research (PPSR) | NASA, NIEHS, USEPA, Alfred P Sloan Foundation, Univ. of Arizona |
| Ramirez-Andreotta, M.D., Lothrop, N., Wilkinson, S.T., Root, R.A., Artiola, J.F., Klimecki, W., & Loh, M. (2016) [44] | J. Environ. Stud. Sci. | Residents of Dewey-Humboldt, Arizona who participated in community involvement (CI) activities | Arsenic | Review of interviews, community meetings and other CI activities | CBPR, EHL, EJ, risk communication, | NIEHS |
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gray, K.M. From Content Knowledge to Community Change: A Review of Representations of Environmental Health Literacy. Int. J. Environ. Res. Public Health 2018, 15, 466. https://doi.org/10.3390/ijerph15030466
Gray KM. From Content Knowledge to Community Change: A Review of Representations of Environmental Health Literacy. International Journal of Environmental Research and Public Health. 2018; 15(3):466. https://doi.org/10.3390/ijerph15030466
Chicago/Turabian StyleGray, Kathleen M. 2018. "From Content Knowledge to Community Change: A Review of Representations of Environmental Health Literacy" International Journal of Environmental Research and Public Health 15, no. 3: 466. https://doi.org/10.3390/ijerph15030466
APA StyleGray, K. M. (2018). From Content Knowledge to Community Change: A Review of Representations of Environmental Health Literacy. International Journal of Environmental Research and Public Health, 15(3), 466. https://doi.org/10.3390/ijerph15030466




