Prevalence of Oral Clefts among Live Births in Gansu Province, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Quality Control
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Dixon, M.J.; Marazita, M.L.; Beaty, T.H.; Murray, J.C. Cleft lip and palate: Synthesizing genetic and environmental influences. Nat. Rev. Genet. 2011, 12, 167. [Google Scholar] [CrossRef] [PubMed]
- Mossey, P.A.; Little, J.; Munger, R.G.; Dixon, M.J.; Shaw, W.C. Cleft lip and palate. Trop. Dr. 2009, 374, 1773–1785. [Google Scholar] [CrossRef]
- Jugessur, A.; Murray, J.C. Orofacial clefting: Recent insights into a complex trait. Curr. Opin. Genet. Dev. 2005, 15, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Wantia, N.; Rettinger, G. The current understanding of cleft lip malformations. Facial Plast. Surg. 2002, 18, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Mossey, P. Epidemiology underpinning research in the aetiology of orofacial clefts. Orthod. Craniofac. Res. 2007, 10, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q. Analysis of birth defects of 48 perinatal newborns. China Health Care Nutri. 2012, 7, 294. (In Chinese) [Google Scholar]
- Cheng, N.; Bai, Y.; Hu, X.; Pei, H.; Li, Y.; Zhang, W.; Fan, X.; Zhang, P.; Zhou, X.; Chen, Z.; et al. A base-line survey on birth defects in Gansu province, West China. Ann. Trop. Paediatr. 2003, 23, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.; Zhu, J.; Mao, M.; Li, Y.; Deng, Y.; Wang, Y.; Liang, J.; Tang, L.; Wang, H.; Kilfoy, B.A.; et al. Time trends in oral clefts in Chinese newborns: Data from the Chinese National Birth Defects Monitoring Network. Birth Defects Res. Part A 2010, 88, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Shu, Z.; Yang, Z.; Meng, R.; Zhan, S.; Cooperative Group of Smile Train cleft-free Demonstrative Province Project of Gansu. Detection rate on un-repaired cleft lip/palate patients in Gansu province in 2008. Chin. J. Epidemiol. 2010, 31, 659–661. [Google Scholar] [CrossRef]
- Kling, R.R.; Taub, P.J.; Ye, X.; Jabs, E.W. Oral clefting in china over the last decade, 205,679 patients. Plast. Reconstr. Surg. Glob. Open 2014, 2, e236. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M.E.; Ratay, J.S.; Marazita, M.L. Asian oral-facial clefts birth prevalence. Clefts Palate Craniofac. J. 2006, 43, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Chou, J.; Wu, J.; Sun, Q.; Lin, X.; Tang, Z.; Zhao, Y.; Song, X. Time trends in birth defects in Gansu Province. Health Vocational Education 2015, 33, 118–120. (In Chinese) [Google Scholar]
- Wang, M.; Yuan, Y.; Wang, Z.; Liu, D.; Wang, Z.; Sun, F.; Wang, P.; Zhu, H.; Li, J.; Wu, T.; et al. Prevalence of orofacial clefts among live births in China: A systematic review and meta-analysis. Birth Defects Res. 2017, 109, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- European Surveillance of Congenital Anomalies. 2014. Available online: http://www.eurocat-network.eu/AccessPrevalenceData/PrevalenceTables (accessed on 16 October 2017).
- Pei, L.; Kang, Y.; Cheng, Y.; Yan, H. The Association of Maternal Lifestyle with Birth Defects in Shaanxi Province, Northwest China. PLoS ONE 2015, 10, e0139452. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, X.H.; Wang, F.Y.; Zhao, X.L.; Zhang, X.; Zhang, Y.P. Analysis of the birth defects among 61272 live born infants in Beijing. Acta Scientiarum Naturalium Universitatis Pekinensis 2009, 41, 414–417. [Google Scholar] [CrossRef]
- Mossey, P.A.; Shaw, W.C.; Munger, R.G.; Murray, J.C.; Murthy, J.; Little, J. Global Oral Health Inequalities: Challenges in the Prevention and Management of Orofacial Clefts and Potential Solutions. Adv. Dent. Res. 2011, 23, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Messer, L.C.; Luben, T.J.; Mendola, P.; Carozza, S.E.; Horel, S.A.; Langlois, P.H. Urban-rural residence and the occurrence of cleft lip and cleft palate in Texas, 1999–2003. Ann. Epidemiol. 2010, 20, 32–39. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Statistics of China. China Statistical Yearbook-2015; China Statistics Press: Beijing, China, 2009. [Google Scholar]
- National Bureau of Statistics of China. China Statistical Yearbook-2015; China Statistics Press: Beijing, China, 2013. [Google Scholar]
- National Bureau of Statistics of China. China Statistical Yearbook-2015; China Statistics Press: Beijing, China, 2016. [Google Scholar]
- Panamonta, V.; Pradubwong, S.; Panamonta, M.; Chowchuen, B. Global birth prevalence of orofacial clefts: A Systematic Review. J. Med. Assoc. Thail. 2015, 98, S11–S21. [Google Scholar]
- Gupta, K.; Bansal, P.; Dev, N.; Tyagi, S.K. Smile Train project: A blessing for population of lower socio-economic status. J. Indian Med. Assoc. 2010, 108, 723–725. [Google Scholar] [PubMed]
- Massenburg, B.B.; Jenny, H.E.; Saluja, S.; Meara, J.G.; Shrime, M.G.; Alonso, N. Barriers to Cleft Lip and Palate Repair Around the World. J. Craniofac. Surg. 2016, 27, 1741–1745. [Google Scholar] [CrossRef] [PubMed]
- Poenaru, D.; Lin, D.; Corlew, S. Economic valuation of the global burden of cleft disease averted by a large cleft charity. World J. Surg. 2016, 40, 1053–1059. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.D.; Babigian, A.; McCormack, S.; Alkire, B.C.; Wong, A.; Pap, S.A.; Vincent, J.R.; Meara, J.G.; Castiglione, C.; Silverman, R. The clinical and economic impact of a sustained program in global plastic surgery: Valuing cleft care in resource-poor settings. Plast. Reconstr. Surg. 2012, 130, 87e–94e. [Google Scholar] [CrossRef] [PubMed]
- Mock, C.; Cherian, M.; Juillard, C.; Donkor, P.; Bickler, S.; Jamison, D.; McQueen, K. Developing priorities for addressing surgical conditions globally: Furthering the link between surgery and public health policy. World J. Surg. 2010, 34, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Magee, W.P., Jr.; Vander Burg, R.; Hatcher, K.W. Cleft lip and palate as a cost-effective health care treatment in the developing world. World J. Surg. 2010, 34, 420–427. [Google Scholar] [CrossRef] [PubMed]
| Subtype of Cleft | Number of Oral Clefts (%) | Prevalence a (95% CI) |
|---|---|---|
| Cleft lip only | 295 (63.03) | 0.85 (0.76–0.95) |
| Cleft lip and palate | 118 (25.21) | 0.34 (0.28–0.41) |
| Cleft palate only | 37 (7.91) | 0.11 (0.08–0.15) |
| Unknown b | 18 (3.85) | 0.05 (0.03–0.08) |
| Total | 468 (100.00) | 1.35 (1.23–1.48) |
| Characteristics | Number of Oral Clefts | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 289 | 61.75 |
| Female | 179 | 38.25 |
| Area | ||
| Town area | 76 | 16.24 |
| Rural area | 359 | 76.71 |
| Unknown a | 33 | 7.05 |
| Economic status b | ||
| Poverty counties | 277 | 59.19 |
| Non-poverty counties | 189 | 40.38 |
| Unknown c | 2 | 0.43 |
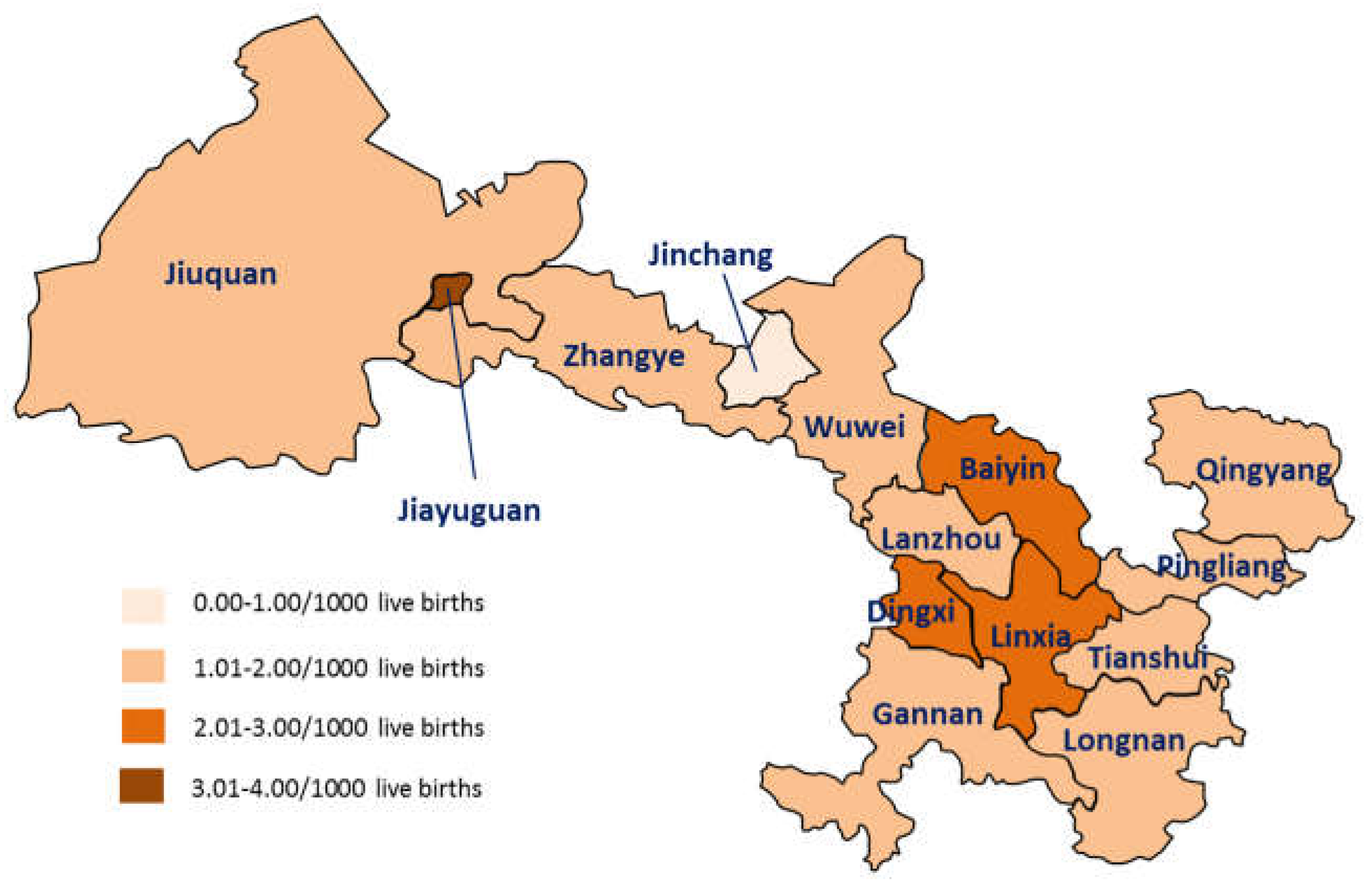
| Region | Number of Oral Clefts | Number of Live Births a | Prevalence b (95% CI) |
|---|---|---|---|
| Jiayuguan | 6 | 1769 | 3.39 (1.24–7.38) |
| Dingxi | 74 | 27,318 | 2.71 (2.13–3.40) |
| Linxia | 60 | 24,423 | 2.46 (1.87–3.16) |
| Baiyin | 33 | 16,073 | 2.05 (1.41–2.88) |
| Lanzhou | 55 | 28,854 | 1.91 (1.44–2.48) |
| Jiuquan | 14 | 8094 | 1.73 (0.95–2.90) |
| Tianshui | 61 | 35,897 | 1.70 (1.30–2.18) |
| Qingyang | 44 | 26,800 | 1.64 (1.19–2.20) |
| Longnan | 40 | 26,452 | 1.51 (1.08–2.06) |
| Pingliang | 32 | 22,265 | 1.44 (0.98–2.03) |
| Gannan | 13 | 9369 | 1.39 (0.74–2.37) |
| Wuwei | 20 | 17,085 | 1.17 (0.72–1.81) |
| Zhangye | 13 | 12,512 | 1.04 (0.55–1.78) |
| Jinchang | 2 | 4758 | 0.42 (0.05–1.52) |
| Unknown c | 1 | 7809 | 0.13 (3.24 × 10−3–0.71) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, M.; Meng, R.; Wang, Z.; Liu, D.; Huang, H.; Kang, C.; Li, H.; Wu, T.; Zhan, S. Prevalence of Oral Clefts among Live Births in Gansu Province, China. Int. J. Environ. Res. Public Health 2018, 15, 380. https://doi.org/10.3390/ijerph15020380
Wang M, Meng R, Wang Z, Liu D, Huang H, Kang C, Li H, Wu T, Zhan S. Prevalence of Oral Clefts among Live Births in Gansu Province, China. International Journal of Environmental Research and Public Health. 2018; 15(2):380. https://doi.org/10.3390/ijerph15020380
Chicago/Turabian StyleWang, Mengying, Ruogu Meng, Zhuqing Wang, Dongjing Liu, Hui Huang, Chuyun Kang, Hongtian Li, Tao Wu, and Siyan Zhan. 2018. "Prevalence of Oral Clefts among Live Births in Gansu Province, China" International Journal of Environmental Research and Public Health 15, no. 2: 380. https://doi.org/10.3390/ijerph15020380
APA StyleWang, M., Meng, R., Wang, Z., Liu, D., Huang, H., Kang, C., Li, H., Wu, T., & Zhan, S. (2018). Prevalence of Oral Clefts among Live Births in Gansu Province, China. International Journal of Environmental Research and Public Health, 15(2), 380. https://doi.org/10.3390/ijerph15020380





