Review of Non-Respiratory, Non-Cancer Physical Health Conditions from Exposure to the World Trade Center Disaster
Abstract
:1. Introduction
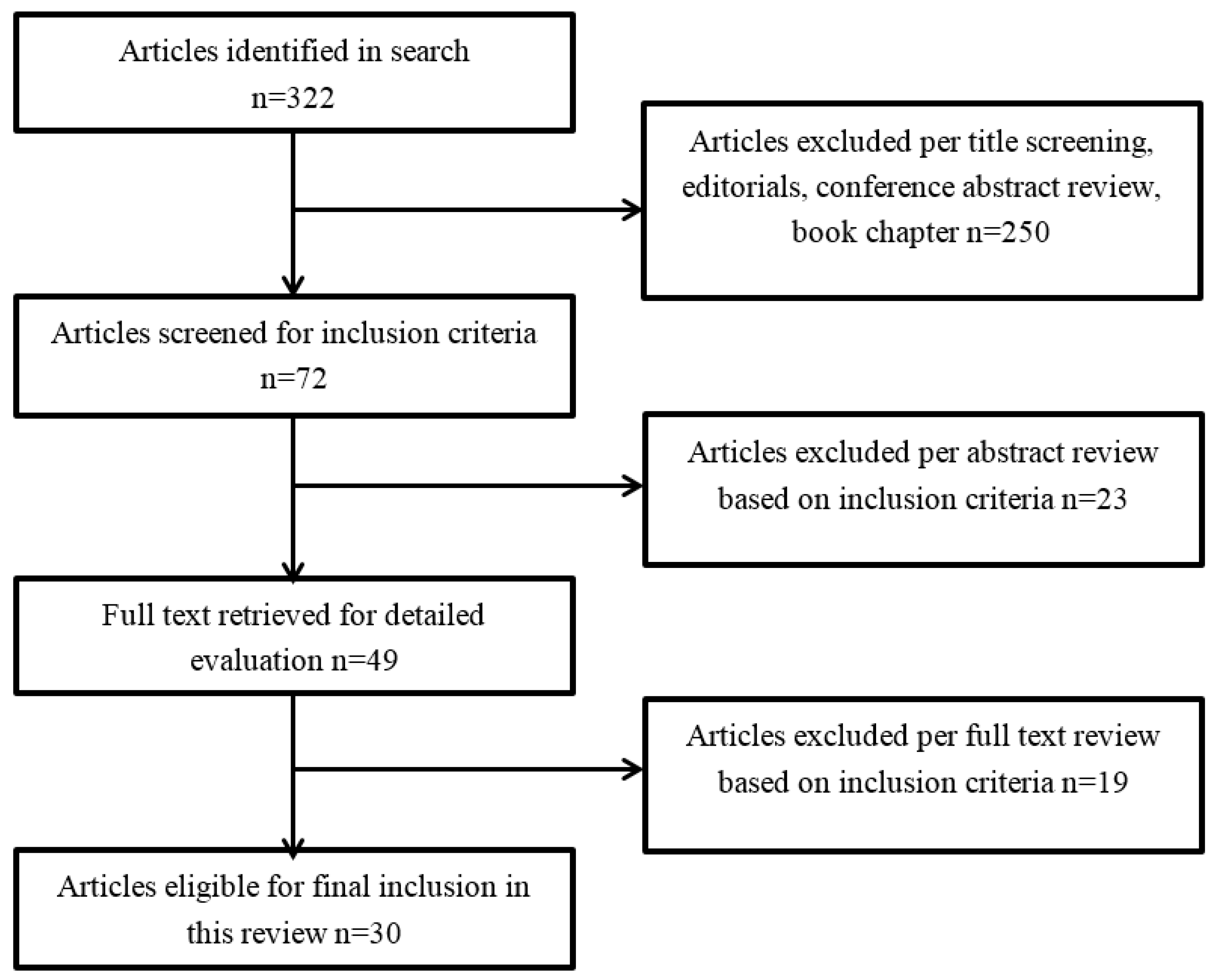
2. Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Study Selection
3. Results
3.1. Cardiovascular/Cerebrovascular Diseases
3.2. Autoimmune Diseases
3.3. Gastroesophageal Reflux Disease/Gastrointestinal Conditions
3.4. Obstructive Sleep Apnea
3.5. Skin Conditions
3.6. Rhinosinusitis
3.7. Other Emerging Conditions
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Moscato, G.; Yacoub, M.R. World Trade Center disaster: Short- and medium-term health outcome. Monaldi Arch. Chest Dis. 2007, 67, 154–158. [Google Scholar] [CrossRef] [PubMed]
- Safirstein, B.H.; Klukowicz, A.; Miller, R.; Teirstein, A. Granulomatous pneumonitis following exposure to the World Trade Center collapse. Chest 2003, 123, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Offenberg, J.H.; Eisenreich, S.J.; Chen, L.C.; Cohen, M.D.; Chee, G.; Prophete, C.; Weisel, C.; Lioy, P.J. Persistent organic pollutants in the dusts that settled across lower Manhattan after September 11, 2001. Environ. Sci. Technol. 2003, 37, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Lioy, P.J.; Weisel, C.P.; Millette, J.R.; Eisenreich, S.; Vallero, D.; Offenberg, J.; Buckley, B.; Turpin, B.; Zhong, M.; Cohen, M.D.; et al. Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in lower Manhattan after the collapse of the WTC 11 September 2001. Environ. Health Perspect. 2002, 110, 703–714. [Google Scholar] [CrossRef] [PubMed]
- McGee, J.K.; Chen, L.C.; Cohen, M.D.; Chee, G.R.; Prophete, C.M.; Haykal-Coates, N.; Wasson, S.J.; Conner, T.L.; Costa, D.L.; Gavett, S.H. Chemical analysis of World Trade Center fine particulate matter for use in toxicologic assessment. Environ. Health Perspect. 2003, 111, 972–980. [Google Scholar] [CrossRef] [PubMed]
- Levin, S.; Herbert, R.; Skloot, G.; Szeinuk, J.; Teirstein, A.; Fischler, D.; Milek, D.; Piligian, G.; Wilk-Rivard, E.; Moline, J. Health effects of World Trade Center site workers. Am. J. Ind. Med. 2002, 42, 545–547. [Google Scholar] [CrossRef] [PubMed]
- Mayo Clinic. Heart Disease—Overview. Available online: http://www.mayoclinic.org/home/ovc-20341555 (accessed on 8 August 2017).
- Simkhovich, B.Z.; Kleinman, M.T.; Kloner, R.A. Particulate air pollution and coronary heart disease. Curr. Opin. Cardiol. 2009, 24, 604–609. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Xu, X.; Chu, M.; Guo, Y.; Wang, J. Air particulate matter and cardiovascular disease: The epidemiological, biomedical and clinical evidence. J. Thorac. Dis. 2016, 8, E8–E19. [Google Scholar] [PubMed]
- Mani, V.; Wong, S.K.; Sawit, S.T.; Calcagno, C.; Maceda, C.; Ramachandran, S.; Fayad, Z.A.; Moline, J.; McLaughlin, M.A. Relationship between particulate matter exposure and atherogenic profile in “Ground Zero” workers as shown by dynamic contrast enhanced MR imaging. Int. J. Cardiovasc. Imaging 2013, 29, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Moline, J.M.; McLaughlin, M.A.; Sawit, S.T.; Maceda, C.; Croft, L.B.; Goldman, M.E.; Garcia, M.J.; Iyengar, R.L.; Woodward, M. The prevalence of metabolic syndrome among law enforcement officers who responded to the 9/11 World Trade Center attacks. Am. J. Ind. Med. 2016, 59, 752–760. [Google Scholar] [CrossRef] [PubMed]
- Perritt, K.R.; Herbert, R.; Levin, S.M.; Moline, J. Work-related injuries and illnesses reported by World Trade Center response workers and volunteers. Prehosp. Disaster Med. 2011, 26, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Jordan, H.T.; Stellman, S.D.; Morabia, A.; Miller-Archie, S.A.; Alper, H.; Laskaris, Z.; Brackbill, R.M.; Cone, J.E. Cardiovascular disease hospitalizations in relation to exposure to the September 11, 2001 World Trade Center disaster and posttraumatic stress disorder. J. Am. Heart Assoc. 2013, 2, e000431. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Gomez, M.I.; Gensburg, L.; Liu, W.; Hwang, S.A. Respiratory and cardiovascular hospitalizations after the World Trade Center disaster. Arch. Environ. Occup. Health 2010, 65, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Brackbill, R.M.; Thorpe, L.E.; DiGrande, L.; Perrin, M.; Sapp, J.H., 2nd; Wu, D.; Campolucci, S.; Walker, D.J.; Cone, J.; Pulliam, P.; et al. Surveillance for World Trade Center disaster health effects among survivors of collapsed and damaged buildings. MMWR Surveill. Summ. 2006, 55, 1–18. [Google Scholar] [PubMed]
- Brackbill, R.M.; Cone, J.E.; Farfel, M.R.; Stellman, S.D. Chronic physical health consequences of being injured during the terrorist attacks on World Trade Center on September 11, 2001. Am. J. Epidemiol. 2014, 179, 1076–1085. [Google Scholar] [CrossRef] [PubMed]
- Jordan, H.T.; Miller-Archie, S.A.; Cone, J.E.; Morabia, A.; Stellman, S.D. Heart disease among adults exposed to the September 11, 2001 World Trade Center disaster: Results from the World Trade Center Health Registry. Prev. Med. 2011, 53, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Alper, H.E.; Yu, S.; Stellman, S.D.; Brackbill, R.M. Injury, intense dust exposure, and chronic disease among survivors of the World Trade Center terrorist attacks of September 11, 2001. Inj. Epidemiol. 2017, 4, 17. [Google Scholar] [CrossRef] [PubMed]
- Diot, E.; Lesire, V.; Guilmot, J.L.; Metzger, M.D.; Pilore, R.; Rogier, S.; Stadler, M.; Diot, P.; Lemarie, E.; Lasfargues, G. Systemic sclerosis and occupational risk factors: A case-control study. Occup. Environ. Med. 2002, 59, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Makol, A.; Reilly, M.J.; Rosenman, K.D. Prevalence of connective tissue disease in silicosis (1985–2006)—A report from the state of Michigan surveillance system for silicosis. Am. J. Ind. Med. 2011, 54, 255–262. [Google Scholar] [CrossRef] [PubMed]
- McCormic, Z.D.; Khuder, S.S.; Aryal, B.K.; Ames, A.L.; Khuder, S.A. Occupational silica exposure as a risk factor for scleroderma: A meta-analysis. Int. Arch. Occup. Environ. Health 2010, 83, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Parks, C.G.; Conrad, K.; Cooper, G.S. Occupational exposure to crystalline silica and autoimmune disease. Environ. Health Perspect. 1999, 107 (Suppl. S5), 793–802. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.J.; Van de Water, J.; Gershwin, M.E. Evidence for the role of environmental agents in the initiation or progression of autoimmune conditions. Environ. Health Perspect. 1999, 107 (Suppl. S5), 667–672. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Puerta, J.A.; Gedmintas, L.; Costenbader, K.H. The association between silica exposure and development of ANCA-associated vasculitis: Systematic review and meta-analysis. Autoimmun. Rev. 2013, 12, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- Goronzy, J.J.; Fujii, H.; Weyand, C.M. Telomeres, immune aging and autoimmunity. Exp. Gerontol. 2006, 41, 246–251. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, A.; Epel, E.; Lin, J.; Wolkowitz, O.; Cohen, B.; Maguen, S.; Metzler, T.; Lenoci, M.; Blackburn, E.; Neylan, T.C. Childhood trauma associated with short leukocyte telomere length in posttraumatic stress disorder. Biol. Psychiatry 2011, 70, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Pace, T.W.; Wingenfeld, K.; Schmidt, I.; Meinlschmidt, G.; Hellhammer, D.H.; Heim, C.M. Increased peripheral NF-kappaB pathway activity in women with childhood abuse-related posttraumatic stress disorder. Brain Behav. Immun. 2012, 26, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Yehuda, R.; Cai, G.; Golier, J.A.; Sarapas, C.; Galea, S.; Ising, M.; Rein, T.; Schmeidler, J.; Muller-Myhsok, B.; Holsboer, F.; et al. Gene expression patterns associated with posttraumatic stress disorder following exposure to the World Trade Center attacks. Biol. Psychiatry 2009, 66, 708–711. [Google Scholar] [CrossRef] [PubMed]
- Yehuda, R.; Golier, J.A.; Kaufman, S. Circadian rhythm of salivary cortisol in Holocaust survivors with and without PTSD. Am. J. Psychiatry 2005, 162, 998–1000. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, A.; Cohen, B.E.; Seal, K.H.; Bertenthal, D.; Margaretten, M.; Nishimi, K.; Neylan, T.C. Elevated risk for autoimmune disorders in iraq and afghanistan veterans with posttraumatic stress disorder. Biol. Psychiatry 2015, 77, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Loupasakis, K.; Berman, J.; Jaber, N.; Zeig-Owens, R.; Webber, M.P.; Glaser, M.S.; Moir, W.; Qayyum, B.; Weiden, M.D.; Nolan, A.; et al. Refractory sarcoid arthritis in World Trade Center-exposed New York City firefighters: A case series. J. Clin. Rheumatol. 2015, 21, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Webber, M.P.; Moir, W.; Zeig-Owens, R.; Glaser, M.S.; Jaber, N.; Hall, C.; Berman, J.; Qayyum, B.; Loupasakis, K.; Kelly, K.; et al. Nested case-control study of selected systemic autoimmune diseases in World Trade Center rescue/recovery workers. Arthritis Rheumatol. 2015, 67, 1369–1376. [Google Scholar] [CrossRef] [PubMed]
- Webber, M.P.; Moir, W.; Crowson, C.S.; Cohen, H.W.; Zeig-Owens, R.; Hall, C.B.; Berman, J.; Qayyum, B.; Jaber, N.; Matteson, E.L.; et al. Post-September 11, 2001, Incidence of Systemic Autoimmune Diseases in World Trade Center-Exposed Firefighters and Emergency Medical Service Workers. Mayo Clin. Proc. 2016, 91, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Webber, M.P.; Yip, J.; Zeig-Owens, R.; Moir, W.; Ungprasert, P.; Crowson, C.S.; Hall, C.B.; Jaber, N.; Weiden, M.D.; Matteson, E.L.; et al. Post-9/11 sarcoidosis in WTC-exposed firefighters and emergency medical service workers. Respir. Med. 2017, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Mayo Clinic. Sarcoidosis. Available online: http://www.mayoclinic.org/diseases-conditions/sarcoidosis/symptoms-causes/syc-20350358 (accessed on 4 October 2017).
- Newman, L.S.; Rose, C.S.; Bresnitz, E.A.; Rossman, M.D.; Barnard, J.; Frederick, M.; Terrin, M.L.; Weinberger, S.E.; Moller, D.R.; McLennan, G.; et al. A case control etiologic study of sarcoidosis: Environmental and occupational risk factors. Am. J. Respir. Crit. Care Med. 2004, 170, 1324–1330. [Google Scholar] [CrossRef] [PubMed]
- Jordan, H.T.; Stellman, S.D.; Prezant, D.; Teirstein, A.; Osahan, S.S.; Cone, J.E. Sarcoidosis diagnosed after September 11, 2001, among adults exposed to the World Trade Center disaster. J. Occup. Environ. Med. 2011, 53, 966–974. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Diabetes and Digestive and Kideny Diseases. Acid Reflux (GER & GERD) in Adults. Available online: https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults (accessed on 8 August 2017).
- Kaji, M.; Fujiwara, Y.; Shiba, M.; Kohata, Y.; Yamagami, H.; Tanigawa, T.; Watanabe, K.; Watanabe, T.; Tominaga, K.; Arakawa, T. Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J. Gastroenterol. Hepatol. 2010, 25, 1151–1156. [Google Scholar] [CrossRef] [PubMed]
- Milani, D.C.; Venturini, A.P.; Callegari-Jacques, S.M.; Fornari, F. Gastro-oesophageal reflux disease and dental erosions in adults: Influence of acidified food intake and impact on quality of life. Eur. J. Gastroenterol. Hepatol. 2016, 28, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Coppeta, L.; Pietroiusti, A.; Magrini, A.; Somma, G.; Bergamaschi, A. Prevalence and characteristics of functional dyspepsia among workers exposed to cement dust. Scand. J. Work Environ. Health 2008, 34, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Mayo Clinic. Barrett’s Esophagus. Available online: http://www.mayoclinic.org/diseases-conditions/barretts-esophagus/home/ovc-20322957 (accessed on 9 August 2017).
- Prezant, D.J.; Weiden, M.; Banauch, G.I.; McGuinness, G.; Rom, W.N.; Aldrich, T.K.; Kelly, K.J. Cough and bronchial responsiveness in firefighters at the World Trade Center site. N. Engl. J. Med. 2002, 347, 806–815. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Brackbill, R.M.; Stellman, S.D.; Farfel, M.R.; Miller-Archie, S.A.; Friedman, S.; Walker, D.J.; Thorpe, L.E.; Cone, J. Gastroesophageal reflux symptoms and comorbid asthma and posttraumatic stress disorder following the 9/11 terrorist attacks on World Trade Center in New York City. Am. J. Gastroenterol. 2011, 106, 1933–1941. [Google Scholar] [CrossRef] [PubMed]
- Wisnivesky, J.P.; Teitelbaum, S.L.; Todd, A.C.; Boffetta, P.; Crane, M.; Crowley, L.; de la Hoz, R.E.; Dellenbaugh, C.; Harrison, D.; Herbert, R.; et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: A cohort study. Lancet 2011, 378, 888–897. [Google Scholar] [CrossRef]
- Webber, M.P.; Gustave, J.; Lee, R.; Niles, J.K.; Kelly, K.; Cohen, H.W.; Prezant, D.J. Trends in respiratory symptoms of firefighters exposed to the world trade center disaster: 2001–2005. Environ. Health Perspect. 2009, 117, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Almadi, M.A.; Almousa, M.A.; Althwainy, A.F.; Altamimi, A.M.; Alamoudi, H.O.; Alshamrani, H.S.; Alharbi, O.R.; Azzam, N.A.; Sadaf, N.; Aljebreen, A.M. Prevalence of symptoms of gastroesopahgeal reflux in a cohort of Saudi Arabians: A study of 1265 subjects. Saudi J. Gastroenterol. 2014, 20, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Song, J.H.; Chung, S.J.; Lee, J.H.; Kim, Y.H.; Chang, D.K.; Son, H.J.; Kim, J.J.; Rhee, J.C.; Rhee, P.L. Relationship between gastroesophageal reflux symptoms and dietary factors in Korea. J. Neurogastroenterol. Motil. 2011, 17, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Icitovic, N.; Onyebeke, L.C.; Wallenstein, S.; Dasaro, C.R.; Harrison, D.; Jiang, J.; Kaplan, J.R.; Lucchini, R.G.; Luft, B.J.; Moline, J.M.; et al. The association between body mass index and gastroesophageal reflux disease in the World Trade Center Health Program General Responder Cohort. Am. J. Ind. Med. 2016, 59, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Yip, J.; Zeig-Owens, R.; Webber, M.P.; Kablanian, A.; Hall, C.B.; Vossbrinck, M.; Liu, X.; Weakley, J.; Schwartz, T.; Kelly, K.J.; et al. World Trade Center-related physical and mental health burden among New York City Fire Department emergency medical service workers. Occup. Environ. Med. 2016, 73, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Icitovic, N.; Crane, M.A.; Dasaro, C.R.; Kaplan, J.R.; Lucchini, R.G.; Luft, B.J.; Moline, J.M.; Pendem, L.; Shapiro, M.; et al. Sex differences in asthma and gastroesophageal reflux disease incidence among the World Trade Center Health Program General Responder Cohort. Am. J. Ind. Med. 2016, 59, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Yip, J.; Zeig-Owens, R.; Weakley, J.; Webber, M.P.; Schwartz, T.M.; Prezant, D.J.; Weiden, M.D.; Hall, C.B. The Effect of World Trade Center Exposure on the Timing of Diagnoses of Obstructive Airway Disease, Chronic Rhinosinusitis, and Gastroesophageal Reflux Disease. Front. Public Health 2017, 5, 2. [Google Scholar] [CrossRef] [PubMed]
- Litcher-Kelly, L.; Lam, Y.; Broihier, J.A.; Brand, D.L.; Banker, S.V.; Kotov, R.; Bromet, E.; Bucobo, J.C.; Shaw, R.D.; Luft, B.J. Longitudinal study of the impact of psychological distress symptoms on new-onset upper gastrointestinal symptoms in World Trade Center responders. Psychosom. Med. 2014, 76, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Brackbill, R.M.; Jordan, H.T.; Cone, J.E.; Farfel, M.R.; Stellman, S.D. Effect of asthma and PTSD on persistence and onset of gastroesophageal reflux symptoms among adults exposed to the September 11, 2001, terrorist attacks. Am. J. Ind. Med. 2016, 59, 805–814. [Google Scholar] [CrossRef] [PubMed]
- Webber, M.P.; Lee, R.; Soo, J.; Gustave, J.; Hall, C.B.; Kelly, K.; Prezant, D. Prevalence and incidence of high risk for obstructive sleep apnea in World Trade Center-exposed rescue/recovery workers. Sleep Breath 2011, 15, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Glaser, M.S.; Shah, N.; Webber, M.P.; Zeig-Owens, R.; Jaber, N.; Appel, D.W.; Hall, C.B.; Weakley, J.; Cohen, H.W.; Shulman, L.; et al. Obstructive sleep apnea and World Trade Center exposure. J. Occup. Environ. Med. 2014, 56 (Suppl. S10), S30–S34. [Google Scholar] [CrossRef] [PubMed]
- Lachapelle, J.M. Industrial airborne irritant or allergic contact dermatitis. Contact Dermat. 1986, 14, 137–145. [Google Scholar] [CrossRef]
- Meo, S.A. Health hazards of cement dust. Saudi Med. J. 2004, 25, 1153–1159. [Google Scholar] [PubMed]
- Winder, C.; Carmody, M. The dermal toxicity of cement. Toxicol. Ind. Health 2002, 18, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Jeffery, N.L.; D’Andrea, C.; Leighton, J.; Rodenbeck, S.E.; Wilder, L.; DeVoney, D.; Neurath, S.; Lee, C.V.; Williams, R.C. Potential exposures to airborne and settled surface dust in residential areas of lower Manhattan following the collapse of the World Trade Center—New York City, November 4–December 11, 2001. MMWR Morb. Mortal Wkly. Rep. 2003, 52, 131–136. [Google Scholar]
- Huang, M.J.; Li, J.; Liff, J.M.; Cohen, D.E.; Cone, J. Self-reported skin rash or irritation symptoms among World Trade Center Health Registry participants. J. Occup. Environ. Med. 2012, 54, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, R.M.; Piccirillo, J.F.; Chandrasekhar, S.S.; Brook, I.; Kumar, K.A.; Kramper, M.; Orlandi, R.R.; Palmer, J.N.; Patel, Z.M.; Peters, A.; et al. Clinical practice guideline (update): Adult Sinusitis Executive Summary. Otolaryngol. Head Neck Surg. 2015, 152, 598–609. [Google Scholar] [CrossRef] [PubMed]
- Weakley, J.; Hall, C.B.; Liu, X.; Zeig-Owens, R.; Webber, M.P.; Schwartz, T.; Prezant, D. The effect of World Trade Center exposure on the latency of chronic rhinosinusitis diagnoses in New York City firefighters: 2001–2011. Occup. Environ. Med. 2016, 73, 280–283. [Google Scholar] [CrossRef] [PubMed]
- Miller-Archie, S.A.; Jordan, H.T.; Ruff, R.R.; Chamany, S.; Cone, J.E.; Brackbill, R.M.; Kong, J.; Ortega, F.; Stellman, S.D. Posttraumatic stress disorder and new-onset diabetes among adult survivors of the World Trade Center disaster. Prev. Med. 2014, 66, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Tapp, L.C.; Baron, S.; Bernard, B.; Driscoll, R.; Mueller, C.; Wallingford, K. Physical and mental health symptoms among NYC transit workers seven and one-half months after the WTC attacks. Am. J. Ind. Med. 2005, 47, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Pietrzak, R.H.; Goldstein, R.B.; Southwick, S.M.; Grant, B.F. Medical comorbidity of full and partial posttraumatic stress disorder in US adults: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom. Med. 2011, 73, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Brackbill, R.M.; Hadler, J.L.; DiGrande, L.; Ekenga, C.C.; Farfel, M.R.; Friedman, S.; Perlman, S.E.; Stellman, S.D.; Walker, D.J.; Wu, D.; et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA 2009, 302, 502–516. [Google Scholar] [CrossRef] [PubMed]
- Farfel, M.; DiGrande, L.; Brackbill, R.; Prann, A.; Cone, J.; Friedman, S.; Walker, D.J.; Pezeshki, G.; Thomas, P.; Galea, S.; et al. An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees. J. Urban Health 2008, 85, 880–909. [Google Scholar] [CrossRef] [PubMed]
- Stein, C.R.; Lee, D.J.; Flamme, G.A.; Cone, J.E. Persistent Post-9/11 Hearing Problems Among World Trade Center Health Registry Rescue and Recovery Workers, 2001 to 2007. J. Occup. Environ. Med. 2017, 59, 1229–1234. [Google Scholar] [CrossRef] [PubMed]
- World Trade Center Health Program. Health Conditions Covered by the WTC Health Program. Available online: https://www.cdc.gov/wtc/faq.html#hlthcond (accessed on 4 October 2017).
- Boffetta, P.; Zeig-Owens, R.; Wallenstein, S.; Li, J.; Brackbill, R.; Cone, J.; Farfel, M.; Holden, W.; Lucchini, R.; Webber, M.P.; et al. Cancer in World Trade Center responders: Findings from multiple cohorts and options for future study. Am. J. Ind. Med. 2016, 59, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Caplan-Shaw, C.E.; Kazeros, A.; Cotrina, M.L.; Amin, M.; Rosen, R.; Ferri, L.; Zhao, S.; Marmor, M.; Liu, M.; Shao, Y.; et al. Paradoxical Vocal Cord Motion In Wtc-Exposed Community Members With Lower Respiratory Symptoms; American Thoracic Society: Washington, DC, USA, 2017; Volume 195. [Google Scholar]
- Berger, K.I.; Caplan-Shaw, C.E.; Kazeros, A.; Pradhan, D.; Goldring, R.M.; Reibman, J. Small Airway Dysfunction as a Mechanism for Persistence of Lower Respiratory Symptoms Despite Treatment in Patients Exposed to World Trade Center Dust; American Thoracic Society: San Francisco, CA, USA, 2016; Volume 193, p. A5425. [Google Scholar]
| Author, Year | Condition | Study Design | Data Source of Condition | Population | Sample Size of Interest |
|---|---|---|---|---|---|
| Alper et al., 2017 [18] | Cardiovascular disease | Cohort | Self-report | WTC Health Registry Adult enrollees (18–64 years old) | 8701 |
| Brackbill et al., 2014 [16] | Cardiovascular disease | Cohort | Self-report | WTC Health Registry Adult enrollees (18–63 years old) | 14,087 |
| Jordan et al., 2011 [17] | Cardiovascular disease | Cohort | Self-report | WTC Health Registry: Residence of lower Manhattan and Rescue and Recovery Workers | 39,324 |
| Jordan et al., 2013 [13] | Cardiovascular disease | Cohort | Hospitalization records | WTC Health Registry: Residence of lower Manhattan and Rescue and Recovery Workers who lived in New York State | 46,417 |
| Lin et al., 2010 [14] | Cardiovascular disease | Case-Control | Hospitalization records | Affected population in Manhattan living near Ground Zero; Control population in Queens County | Affected population: 56,013 Control population: 88,017 |
| Mani et al., 2012 [10] | Cardiovascular disease | Cohort | Clinical assessment | WTCHC: Rescue and Recovery Workers (Law Enforcement) | 31 |
| Moline et al., 2016 [11] | Cardiovascular disease | Cohort | Clinical assessment | WTCHC: Rescue and Recovery Workers (Law Enforcement) | 2497 |
| Jordan et al., 2011 [37] | Autoimmune disease (sarcoidosis) | Case-control | Clinical assessment | WTC Health Registry: Residence of lower Manhattan and Rescue and Recovery Workers | Cases: 28 Controls: 109 |
| Loupasakis et al., 2015 [31] | Autoimmune disease (sarcoid arthritis) | Cohort | Clinical assessment | FDNY: Rescue and Recovery Workers | 13,468 |
| Webber et al., 2015 [32] | Autoimmune disease (systemic autoimmune diseases) | Case-control | Clinical assessment | FDNY: Rescue and Recovery Workers | Cases: 59 Controls: 236 |
| Webber et al., 2016 [33] | Autoimmune disease (systemic autoimmune diseases) | Case-cohort | Clinical assessment | FDNY: Rescue and Recovery Workers | 13,892 |
| Webber et al., 2017 [34] | Autoimmune disease (sarcoidosis) | Case-cohort | Clinical assessment | FDNY: Rescue and Recovery Workers (Firefighters and EMT) | 13,098 |
| Li et al., 2011 [44] | GERD/GI | Cohort | Self-report | WTC Health Registry: Residence of lower Manhattan and Rescue and Recovery Workers | 37,118 |
| Li et al., 2016 [54] | GERD/GI | Cohort | Self-report | WTC Health Registry: Residence of lower Manhattan and Rescue and Recovery Workers | 29,406 |
| Litcher-Kelly et al., 2014 [53] | GERD | Cohort | Clinical assessment | WTCHC: Rescue and Recovery Workers (Law Enforcement and Nontraditional) | 10,953 |
| Webber et al., 2009 [46] | GERD/GI | Cohort | Self-report | FDNY: Rescue and Recovery Workers | 10,378 |
| Glaser et al., 2014 [56] | Obstructive sleep apnea | Cross-sectional | Clinical assessment | FDNY: Rescue and Recovery Workers | 636 |
| Webber et al., 2011 [55] | Obstructive sleep apnea | Cohort | Self-report | FDNY: Rescue and Recovery Workers | 13,330 |
| Huang et al., 2012 [61] | Skin rash or irritation | Cohort | Self-report | WTC Health Registry: Residence of lower Manhattan and Rescue and Recovery Workers | 42,025 |
| Weakley et al., 2015 [63] | Rhinosinusitis | Cohort | Clinical assessment | FDNY: Rescue and Recovery Workers | 9848 |
| Miller-Archie et al., 2014 [64] | Other (diabetes) | Cohort | Self-report | WTC Health Registry: Residence of lower Manhattan and Rescue and Recovery Workers | 36,899 |
| Stein et al., 2017 [69] | Other (hearing loss) | Cohort | Self-report | WTC Health Registry: Rescue and Recovery Workers | 16,579 |
| Tapp et al., 2005 [65] | Other (headaches) | Cross-sectional | Self-report | NYC Transit Workers | 269 |
| Multiple conditions | |||||
| Brackbill et al., 2006 [15] | GERD/GI, Other (headaches, hearing problems/loss), Skin rash, Cardiovascular disease | Cohort | Self-report | WTC Health Registry Adult enrollees (survivors of collapsed and damage buildings) | 8418 |
| Liu et al., 2017 [52] | Rhinosinusitis; GERD | Cohort | Clinical assessment | FDNY: Rescue and Recovery Workers | 8968 |
| Perritt et al., 2011 [12] | Cardiovascular disease; GERD/GI; Skin rash/irritation; Other (headaches) | Cohort | Self-report | WTCHC: Rescue and Recovery Workers and Volunteers | 7810 |
| Wisnivesky et al., 2011 [45] | Rhinosinusitis; GERD | Cohort | Self-report | WTCHC: Rescue and Recovery Workers; Construction Workers; Municipal Workers | 27,449 |
| Yip et al., 2016 [50] | Rhinosinusitis; GERD | Cohort | Clinical assessment | FDNY: Rescue and Recovery Workers (EMT) | 2281 |
| Author, Year | Condition | 9/11-Exposure | Comorbid Conditions Reported |
|---|---|---|---|
| Alper et al., 2017 [18] | Cardiovascular disease | Injury | PTSD |
| Brackbill et al., 2006 [15] | GERD/GI, Other (headaches, hearing problems/loss), Skin rash, Cardiovascular disease (heart disease, stroke, hypertension) | Dust/debris cloud; building type | None assessed |
| Brackbill et al., 2014 [16] | Cardiovascular disease | Injury | PTSD |
| Glaser et al., 2014 [56] | Obstructive sleep apnea | Arrival to Ground Zero on 9/11 | GERD and comorbid GERD/Rhinosinusitis |
| Huang et al., 2012 [61] | Skin rash or irritation | Dust/debris cloud; home/workplace damage; working more than 90 days or 31 to 90 days at the World Trade Center site | None found |
| Icitovic et al., 2016 [49] | GERD/GI | RRW | Obesity |
| Jiang et al., 2016 [51] | GERD/GI | RRW | None assessed |
| Jordan et al., 2011 [37] | Autoimmune disease (sarcoidosis) | Worked on the pile at ground zero on 9/11 | None assessed |
| Jordan et al., 2011 [17] | Cardiovascular disease | Dust cloud (women); injury (men and women) | PTSD |
| Jordan et al., 2013 [13] | Cardiovascular disease | RRW | PTSD |
| Li et al., 2011 [44] | GERD/GI | RRW; dust cloud; not evacuating home (residents) | PTSD; asthma; PTSD/asthma comorbidity |
| Li et al., 2016 [54] | GERD/GI | RRW | PTSD; asthma |
| Lin et al., 2010 [14] | Cardiovascular disease | Resident proximity to Ground Zero | None assessed |
| Litcher-Kelly et al., 2014 [53] | GERD | RRW; worked on the pile at ground zero on 9/11 | Depression; generalized anxiety; panic; PTSD |
| Liu et al., 2017 [52] | Rhinosinusitis; GERD | Arrival to Ground Zero on 9/11 | OAD |
| Loupasakis et al., 2015 [31] | Autoimmune disease (sarcoid arthritis) | RRW | None assessed |
| Mani et al., 2012 [10] | Cardiovascular disease | Arrival to Ground Zero on 9/11 | None assessed |
| Miller-Archie et al., 2014 [64] | Other (diabetes) | Exposure index (Very high/high) | PTSD |
| Moline et al., 2016 [11] | Cardiovascular disease | RRW | None assessed |
| Perritt et al., 2011 [12] | Cardiovascular disease; GERD/GI; Skin rash/irritation; Other (headaches) | RRW | None assessed |
| Stein et al., 2017 [69] | Other (hearing loss) | RRW; dust cloud | PTSD |
| Tapp et al., 2005 [65] | Other (headaches) | Dust cloud | None assessed |
| Weakley et al., 2015 [63] | Rhinosinusitis | Earlier time of arrival at the WTC site (morning of 9/11 through 9/12) | None assessed |
| Webber et al., 2009 [46] | GERD/GI | Arrival on 9/11 and prolonged work at Ground Zero | Lower respiratory symptoms; Rhinosinusitis |
| Webber et al., 2011 [55] | Obstructive sleep apnea | Earlier time of arrival at the WTC site (morning of 9/11 through 9/12) | GERD; chronic rhinosinusitis; PTSD |
| Webber et al., 2015 [32] | Autoimmune disease (systemic autoimmune diseases) | Prolonged work at Ground Zero | None assessed |
| Webber et al., 2016 [33] | Autoimmune disease (systemic autoimmune diseases) | Arrival on 9/11 and/or prolonged work at Ground Zero | None assessed |
| Webber et al., 2017 [34] | Autoimmune disease (sarcoidosis) | Arrival on 9/11 and/or prolonged work at Ground Zero | None assessed |
| Wisnivesky et al., 2011 [45] | Rhinosinusitis; GERD | Dust cloud; Prolonged work at Ground Zero | GERD; asthma; Rhinosinusitis |
| Yip et al., 2016 [50] | Rhinosinusitis; GERD | Earlier arrival at Ground Zero | GERD; Rhinosinusitis; obstructive airway disease; mental health disorders |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gargano, L.M.; Mantilla, K.; Fairclough, M.; Yu, S.; Brackbill, R.M. Review of Non-Respiratory, Non-Cancer Physical Health Conditions from Exposure to the World Trade Center Disaster. Int. J. Environ. Res. Public Health 2018, 15, 253. https://doi.org/10.3390/ijerph15020253
Gargano LM, Mantilla K, Fairclough M, Yu S, Brackbill RM. Review of Non-Respiratory, Non-Cancer Physical Health Conditions from Exposure to the World Trade Center Disaster. International Journal of Environmental Research and Public Health. 2018; 15(2):253. https://doi.org/10.3390/ijerph15020253
Chicago/Turabian StyleGargano, Lisa M., Kimberly Mantilla, Monique Fairclough, Shengchao Yu, and Robert M. Brackbill. 2018. "Review of Non-Respiratory, Non-Cancer Physical Health Conditions from Exposure to the World Trade Center Disaster" International Journal of Environmental Research and Public Health 15, no. 2: 253. https://doi.org/10.3390/ijerph15020253
APA StyleGargano, L. M., Mantilla, K., Fairclough, M., Yu, S., & Brackbill, R. M. (2018). Review of Non-Respiratory, Non-Cancer Physical Health Conditions from Exposure to the World Trade Center Disaster. International Journal of Environmental Research and Public Health, 15(2), 253. https://doi.org/10.3390/ijerph15020253




