The Efficacy of Inpatient vs. Home-Based Physiotherapy Following Coronary Artery Bypass Grafting
Abstract
1. Introduction
2. Material and Methods
2.1. Pre-Operative Data
2.2. Treatment and Principles of Applied Physiotherapy
2.3. Spirometry Test
2.4. Statistical Analysis
2.5. Characteristics of Patients
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Szychta, W.; Majstrak, F.; Opolski, G.; Filipiak, K.J. Change in the clinical profile of patients referred for coronary artery bypass grafting from 2004 to 2008. Trends in a single-centre study. Kardiol. Pol. 2015, 73, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Rogowski, J.; Jarmoszewicz, K.; Siondalski, P.; Pawlaczyk, R. Opieka pooperacyjna po zabiegach kardiochirurgicznych. Chor. Serca Naczyń 2006, 3, 115–122. (In Polish) [Google Scholar]
- Head, S.J.; Kieser, T.M.; Falk, V.; Huysmans, H.A.; Kappetein, A.P. Coronary artery bypass grafting: Part 1: The evolution over the first 50 years. Eur. Heart J. 2013, 34, 2862–2872. [Google Scholar] [CrossRef] [PubMed]
- Working Group of the European Society of Cardiology (ESC) and the European Association of Heart and Chest Surgery (EACTS) for myocardial revascularization. Developed with a special participation European Association for Percutaneous Cardiovascular Interventions (EAPCI). ESC/EACTS guidelines on myocardial revascularization in 2014. Kardiol. Pol. 2014, 72, 1253–1379.
- Ettema, R.G.A.; Van Koeven, H.; Peelen, L.M.; Kalkman, C.J.; Schuurmans, M.J. Preadmission interventions to prevent postoperative complications in older cardiac surgery patients: A systematic review. Int. J. Nurs. Stud. 2014, 51, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Ettema, R.G.A.; Peelen, L.P.; Kalkman, C.J.; Nierich, A.P.; Moons, K.G.M.; Schuurmans, M.J. Predicting prolonged Intensive Care Unit stays in older cardiac surgery patients: A validation study. Intensiv. Care Med. 2011, 37, 1480–1487. [Google Scholar] [CrossRef] [PubMed]
- Dziduszko-Fedorko, E.; Zawadzka-Byśko, M. Rehabilitacja po zabiegach rewaskularyzacji tętnic wieńcowych. Przew. Lek. 2004, 7, 118–126. (In Polish) [Google Scholar]
- Aykut, K.; Albayrak, G.; Guzeloglu, M.; Baysak, AE.; Hazan, E. Preoperative mild cognitive dysfunction predicts pulmonary complications after coronary artery bypass graft surgery. J. Cardiothorac. Vasc. Anesth. 2013, 27, 1267–1270. [Google Scholar] [CrossRef] [PubMed]
- Tung, H.H.; Jan, M.S.; Huang, C.M.; Shih, C.C.; Chang, C.Y.; Liau, C.Y. Using the theory of planned behavior to predict the use of incentive spirometry among cardiac surgery patients in Taiwan. Heart Lung 2011, 40, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Kotfis, K.; Szylińska, A.; Listewnik, M.; Lechowicz, K.; Kosiorowska, M.; Drożdżal, S.; Brykczyński, M.; Rotter, I.; Żukowski, M. Balancing intubation time with postoperative risk in cardiac surgery patients—A retrospective cohort analysis. Ther. Clin. Risk Manag. 2018, 14, 2203–2212. [Google Scholar] [CrossRef]
- Piotrowicz, R.; Wolszakiewicz, J. Rehabilitacja kardiologiczna pacjentów po zawale serca. Folia Cardiol. Excerpta 2008, 3, 559–565. (In Polish) [Google Scholar]
- Mampuya, W.M. Cardiac rehabilitation past, present and future: An overview. Cardiovasc. Diagn. Ther. 2012, 2, 38–49. [Google Scholar] [PubMed]
- Pouwels, S.; Hageman, D.; Gommans, L.N.M.; Willigendael, E.M.; Nienhuijs, S.W.; Scheltinga, M.R. Preoperative exercise therapy in surgical care: A scoping review. J. Clin. Anesth. 2016, 33, 476–490. [Google Scholar] [CrossRef] [PubMed]
- Maddocks, S.; Cobbing, S. Patients’ Experiences of and Perspectives on Phase 1 Cardiac Rehabilitation after Coronary Artery Bypass Graft Surgery. Physiother. Can. 2017, 69, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Cesario, A.; Ferri, L.; Galetta, D.; Cardaci, V.; Biscione, G.; Pasqua, F.; Piraino, A.; Bonassi, S.; Russo, P.; Sterzi, S.; et al. Pre-operative pulmonary rehabilitation and surgery for lung cancer. Lung Cancer 2007, 57, 118–119. [Google Scholar] [CrossRef] [PubMed]
- Kowalewski, J.; Dancewicz, M. Rak płuca: Leczenie chorych z ograniczoną rezerwą oddechową. Kardiochir. Torakochir. 2008, 5, 413–417. (In Polish) [Google Scholar]
- AlOtaibi, K.D.; El-Sobkey, S.B. Spirometric values and chest pain intensity three days post-operative coronary artery bypass graft surgery. J. Saudi Heart Assoc. 2015, 27, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.V.; Van Der Grinten, C.P.M.; Gustafsson, P.; et al. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society. Standardization of spirometry, 1994 update. Am. J. Respir. Crit. Care Med. 1955, 152, 1107–1136. [Google Scholar]
- American Thoracic Society Single-breath carbon monoxide diffusing capacity (transfer factor). Recommendations for a standard technique—1995 update. Am. J. Respir. Crit. Care Med. 1995, 152, 2185–2198. [CrossRef] [PubMed]
- Jaxa-Chamiec, T. Rehabilitacja kardiologiczna—Definicja, historia, cele, znaczenie, korzyści. Postep. Nauk Med. 2008, 10, 634–642. [Google Scholar]
- Piepoli, M.F.; Corra, U.; Benzer, W.; Bjarnason-Wehrens, B.; Dendale, P.; Gaita, D.; McGee, H.; Mendes, M.; Niebauer, J.; Zwisler, A.D.O.; et al. Secondary prevention through cardiac rehabilitation: From knowledge to implementation. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur. J. Cardiovasc. Prev. Rehabil. 2010, 17, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Jegier, B.; Pietka, I.; Wojtczak-Soska, K.; Jaszewski, R.; Lelonek, M. Cardiac rehabilitation after cardiac surgery is limited by gender and length of hospitalisation. Kardiol. Pol. 2011, 69, 42–46. [Google Scholar] [PubMed]
- Martin, B.J.; Hauer, T.; Arena, R.; Austford, L.D.; Galbraith, PD.; Lewin, A.M.; Knudtson, M.L.; Ghali, W.A.; Stone, J.A.; et al. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation 2012, 126, 677–687. [Google Scholar] [CrossRef] [PubMed]
- Dobson, L.E.; Lewin, R.J.; Doherty, P.; Batin, P.D.; Megarry, S.; Gale, C.P. Is cardiac rehabilitation still relevant in the new millennium? J. Cardiovasc. Med. 2012, 13, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.J.; King, M.; Lui, K.; Oldridge, N.; Pina, I.L.; Spertus, J.; Bonow, R.O.; Estes, N.M.; Goff, D.C.; Grady, K.L.; et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. Circulation 2007, 116, 1611–1642. [Google Scholar] [PubMed]
- Williams, M.A.; Ades, P.A.; Hamm, L.F.; Keteyian, S.J.; LaFontaine, TP.; Roitman, J.L.; Squires, R.W. Clinical evidence for a health benefit from cardiac rehabilitation: An update. Am. Heart J. 2006, 152, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Suaya, J.A.; Stason, W.B.; Ades, P.A.; Normand, S.L.; Shepard, D.S. Cardiac rehabilitation and survival in older coronary patients. J. Am. Coll. Cardiol. 2009, 54, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Alter, D.A.; Oh, P.I.; Chong, A. Relationship between cardiac rehabilitation and survival after acute cardiac hospitalization within a universal health care system. Eur. J. Cardiovasc. Prev. Rehabil. 2009, 16, 102–113. [Google Scholar] [CrossRef] [PubMed]
- Trzos, E.; Kurpesa, M.; Rechciński, T.; Wierzbowska-Drabik, K.; Krzemińska-Pakuła, M. The influence of physical rehabilitation on arterial compliance in patients after myocardial infarction. Cardiol. J. 2007, 14, 366–371. [Google Scholar] [PubMed]
- Listerman, J.; Bittner, V.; Sanderson, B.K.; Brown, T.M. Cardiac rehabilitation outcomes: Impact of comorbidities and age. J. Cardiopulm. Rehabil. Prev. 2011, 31, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Frengley, J.D.; Sansone, G.R.; Alba, A.; Uppal, K.; Kleinfeld, J. Influence of age on rehabilitation outcomes and survival in post-acute inpatient cardiac rehabilitation. J. Cardiopulm. Rehabil. Prev. 2011, 31, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Socha, M.; Wronecki, K.; Sobiech, KA. Gender and age-dependent differences in body composition changes in response to cardiac rehabilitation exercise training in patients after coronary artery bypass grafting. Ann. Agric. Environ. Med. 2017, 24, 517–521. [Google Scholar] [CrossRef] [PubMed]
- Borowicz-Bieńkowska, S.; Deskur-Smielecka, E.; Maleszka, M.; Przywarska, I.; Wilk, M.; Pilaczyńska-Szcześniak, L.; Dylewicz, P. The impact of short-term cardiac rehabilitation on changing dietary habits in patients after acute coronary syndrome. J. Cardiopulm. Rehabil. Prev. 2013, 33, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Boyden, T.; Rubenfire, M.; Franklin, B. Will increasing referral to cardiac rehabilitation improve participation? Prev. Cardiol. 2010, 13, 198–202. [Google Scholar] [CrossRef]
- Jankowski, P.; Czarnecka, D.; Wolfshaut-Wolak, R.; Łysek, R.; Łukaszewska, A.; Bogacki, P.; Grodecki, J.; Mirek-Bryniarska, E.; Nessler, J.; Podolec, P.; et al. Secondary prevention of coronary artery disease in contemporary clinical practice. Cardiol. J. 2015, 22, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Youn, J.E.; Choi, H.E. The effect of a self-exercise program in cardiac rehabilitation for patients with coronary artery disease. Ann. Rehabil. Med. 2011, 35, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Wróblewska, I.; Oleśniewicz, P.; Kurpas, D.; Sołtysik, M.; Błaszczuk, J. Analysis of spirometry results in hospitalized patients aged over 65 years. Clin. Interv. Aging 2015, 10, 1071–1076. [Google Scholar] [CrossRef] [PubMed]
- McAllister, D.A.; Wild, S.H.; MacLay, J.D.; Robson, A.; Newby, D.E.; MacNee, W.; Innes, J.A.; Zamvar, V.; Mills, N.L. Forced expiratory volume in one second predicts length of stay and in-hospital mortality in patients undergoing cardiac surgery: A retrospective cohort study. PLoS ONE 2013, 8, e64565. [Google Scholar] [CrossRef] [PubMed]
- Shakouri, S.K.; Salekzamani, Y.; Taghizadieh, A. Effect of respiratory rehabilitation before open cardiac surgery on respiratory function: A randomized clinical trial. Cardiovasc. Thorac. Res. 2015, 7, 13–17. [Google Scholar] [CrossRef]
- Urell, C.; Westerdahl, E.; Hedenstrom, H.; Janson, C.; Emtner, M. Lung Function before and Two Days after Open-Heart Surgery. Crit. Care Res. Pract. 2012, 2012, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, M.A.Q.; Hosain, N.; Maruf, M.F.; Rahman, M.; Aftabuddin, M.; Adhikary, A.B. Evaluation of Pulmonary Function after Off-pump Coronary Artery Bypass Grafting in Patients Treated with Preoperative Bronchodilator. Cardiovasc. J. 2015, 7, 123–127. [Google Scholar] [CrossRef]
- El-Sobkey, S.; Gomaa, M. Assessment of pulmonary function tests in cardiac patients. J. Saudi Heart Assoc. 2011, 23, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Moreno, A.M.; Castro, R.R.; Sorares, P.P.; Sant’Anna, M.; Cravo, S.L.; Nóbrega, A.C. Longitudinal evaluation the pulmonary function of the pre and postoperative periods in the coronary artery bypass graft surgery of patients treated with a physiotherapy protocol. J. Cardiothorac. Surg. 2011, 62, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Renault, J.A.; Costa-Val, R.; Rosseti, M.B.; Houri, N.M. Comparison between deep breathing exercises and incentive spirometry after CABG surgery. Braz. J. Cardiovasc. Surg. 2009, 24, 165–172. [Google Scholar] [CrossRef]
- Smolis-Bąk, E.; Kazimierska, B.; Kaszczyński, T.; Smolis, R.; Dąbrowski, R.; Kowalik, I. Czy czas trwania intubacji ma wpływ na parametry oddechowe u pacjentów po wszczepieniu pomostów aortalno-wieńcowych? Fizjoter Pol. 2010, 1, 78–83. (In Polish) [Google Scholar]
- Morsch, K.T.; Leguisamo, C.P.; Camargo, M.D.; Coronel, CC.; Mattos, W.; Ortiz, L.D.; Lima, G.G.D. Ventilatory profile of patients undergoing CABG surgery. Braz. J. Cardiovasc. Surg. 2009, 24, 180–187. [Google Scholar] [CrossRef]
- Rachwalik, M.; Pelczer, M.; Goździk, A.; Kustrzycki, W. Ocena wydolności układu oddechowego w obserwacji krótko-I długoterminowej u pacjentów po rewaskularyzacji mięśnia sercowego z krążeniem pozaustrojowym i bez krążenia pozaustrojowego. Kardiochir. Torakochir. Pol. 2007, 4, 252–260. (In Polish) [Google Scholar]
- Westerdahl, E.; Lindmark, B.; Almgren, S.O.; Tenling, A. Chest physiotherapy after coronary artery bypass graft surgery—A comparison of three different deep breathing techniques. J. Rehabil. Med. 2001, 33, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Van der Peijl, I.D.; Vliet Vlieland, T.P.; Versteegh, M.I.; Lok, J.J.; Munneke, M.; Dion, R.A. Exercise therapy after coronary artery bypass graft surgery: A randomized comparison of a high and low frequency exercise therapy program. Ann. Thorac. Surg. 2004, 77, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Shakuri, S.K.; Salekzamani, Y.; Taghizadieh, A.; Sabbagh-Jadid, H.; Soleymani, J.; Sahebi, L. Pulmonary physiotherapy effect on patients undergoing open cardiac surgery. Rus. Open Med. J. 2014, 3, 1–4. [Google Scholar] [CrossRef]
- Spiroski, D.; Andić, M.; Stojanović, O.I.; Lazović, M.; Dikić, A.D.; Ostojić, M.; Beleslin, B.; Kostić, S.; Zdravković, M.; Lović, D. Very short/short-term benefit of inpatient/outpatient cardiac rehabilitation programs after coronary artery bypass grafting surgery. Clin. Cardiol. 2017, 40, 281–286. [Google Scholar] [CrossRef] [PubMed]
| Variables | InPhysio (n = 52) | HomePhysio (n = 52) | p-Value | |
|---|---|---|---|---|
| Demographic data | ||||
| Age ( ± SD, years) | 64.23 ± 8.31 | 65.06 ± 7.89 | 0.329 | |
| Sex | Women (n = 41) | 19 (36.54%) | 22 (42.31%) | 0.547 * |
| Men (n = 63) | 33 (63.46%) | 30 (57.69%) | ||
| BMI ( ± SD, kg/m2) | 30.12 ± 5.00 | 29.73 ± 4.35 | 0.881 | |
| Smoking | Smokers (n = 36) | 20 (38.46%) | 16 (30.77%) | 0.409 * |
| ( ± SD, years) | 29.62 ± 12.16 | 35.00 ± 10.69 | 0.259 | |
| Operative risk | ||||
| EuroScore II ( ± SD, %) | 4.28 ± 4.80 | 4.87 ± 3.70 | 0.072 | |
| Pre-operative data | ||||
| Duration of the underlying disease ( ± SD, months) | 47.85 ± 66.20 | 49.76 ± 63.36 | 0.996 | |
| EF ( ± SD, %) | 48.08 ± 8.70 | 47.37 ± 8.40 | 0.666 | |
| CKMB ( ± SD, IU/L) | 22.10 ± 9.54 | 24.07 ± 9.59 | 0.221 | |
| Glycated hemoglobin ( ± SD, %) | 6.28 ± 1.02 | 6.35 ± 1.06 | 0.691 | |
| Creatinine ( ± SD, mg/dL) | 0.86 ± 0.24 | 0.92 ± 0.51 | 0.647 | |
| GFR ( ± SD, mL/min/1.73 m2) | 84.51 ± 16.01 | 83.98 ± 16.16 | 0.500 | |
| CRP ( ± SD, mg/L) | 4.63 ± 9.89 | 2.67 ± 3.81 | 0.097 | |
| Intra-operative data | ||||
| Perfusion time ( ± SD, min) | 49.02 ± 11.04 | 53.25 ± 11.34 | 0.070 | |
| Aortic clamping time ( ± SD, min) | 29.69 ± 9.46 | 32.71 ± 8.42 | 0.056 | |
| Post-operative data | ||||
| Intubation time ( ± SD, min) | 634.12 ± 234.29 | 689.81 ± 253.63 | 0.199 | |
| CKMB ( ± SD, IU/L) | 42.35 ± 16.28 | 47.58 ± 18.55 | 0.124 | |
| Creatinine max ( ± SD, mg/dL) | 0.99 ± 0.38 | 1.07 ± 0.65 | 0.762 | |
| GFR min ( ± SD, mL/min/1.73 m2) | 77.67 ± 21.22 | 76.25 ± 22.51 | 0.908 | |
| CRP—second day ( ± SD, mg/L) | 64.61 ± 31.42 | 62.16 ± 36.29 | 0.484 | |
| CRP—fourth day ( ± SD, mg/L) | 220.82 ± 67.91 | 223.45 ± 75.14 | 0.964 | |
| Post-Operative Complications | InPhysio (n = 52) | HomePhysio (n = 52) | p-Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Acute renal failure treated with hemofiltration | 0 (0.00%) | 1 (1.92%) | 0.500 |
| Re-intubation | 1 (1.92%) | 3 (5.77%) | 0.618 |
| Hydrothorax/hemothorax requiring drainage | 3 (5.77%) | 3 (5.77%) | 0.661 |
| Post-operative delirium | 3 (5.77%) | 3 (5.77%) | 0.661 |
| Re-operation due to bleeding or tamponade | 0 (0.00%) | 1 (1.92%) | 0.500 |
| Atrial fibrillation | 5 (9.61) | 9 (17.31%) | 0.250 |
| Sternal wound infection | 1 (1.92%) | 4 (7.69%) | 0.363 |
| Infection after endoscopic vein harvest | 2 (3.85%) | 2 (3.85%) | 0.691 |
| Sternum instability requiring intervention | 0 (0.00%) | 1 (1.92%) | 0.500 |
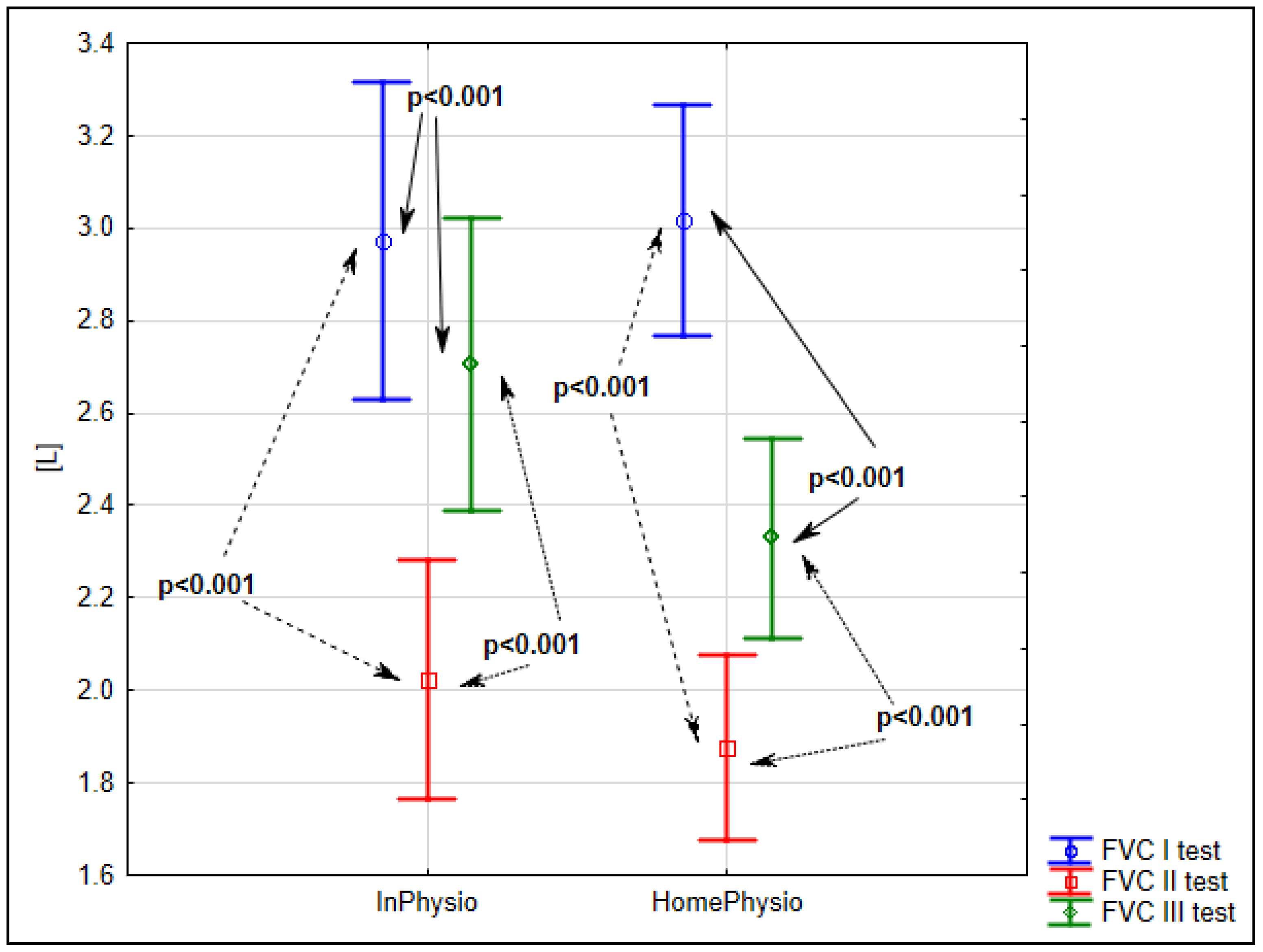
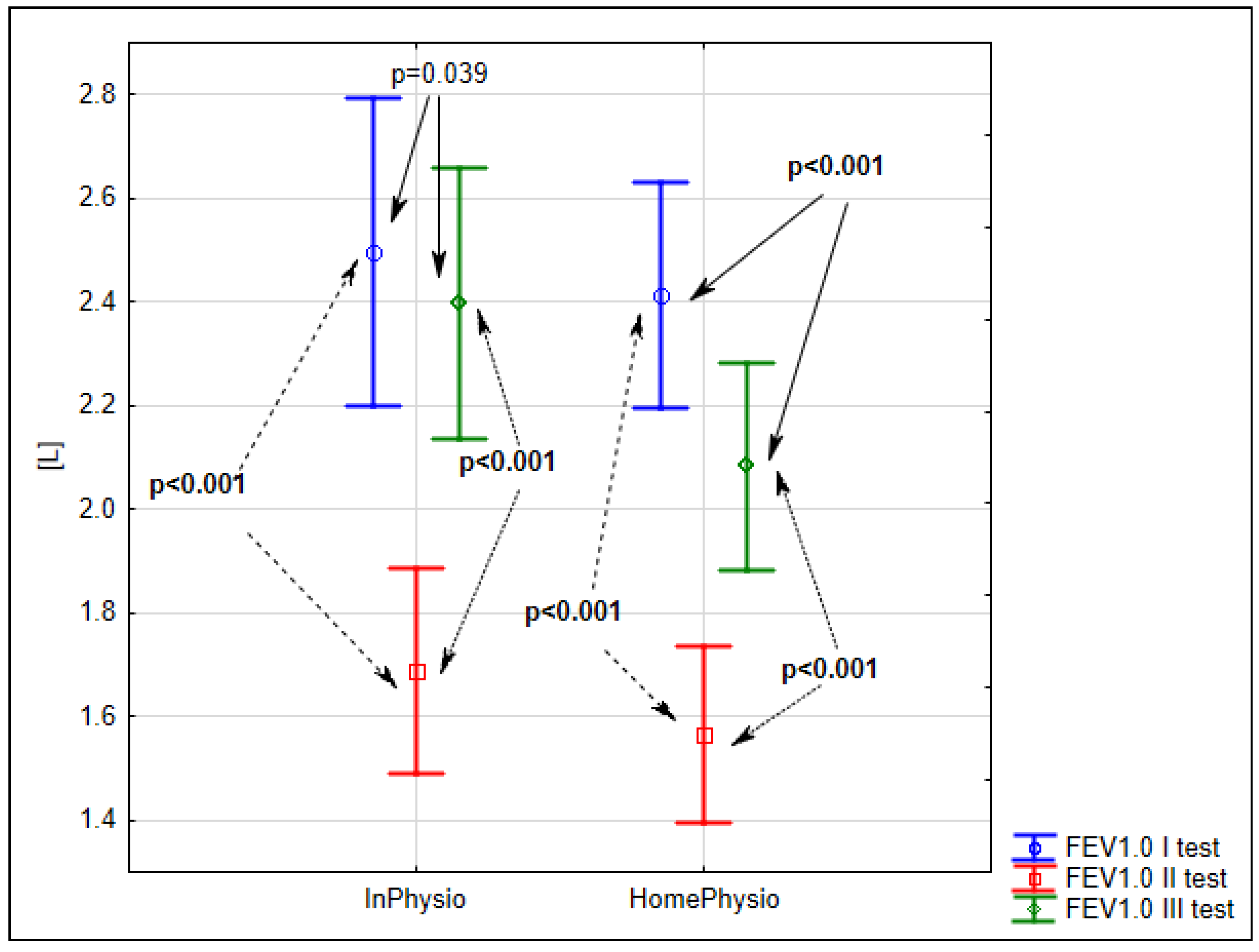
| Gradients of Spirometry Tests | InPhysio (n = 52) | HomePhysio (n = 52) | p-Value | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Gradient of S1 and S2 spirometry tests | FVC (L) | −0.95 ± 0.61 | −1.14 ± 0.6 | NS |
| FEV 1.0 (L) | −0.81 ± 0.74 | −0.85 ± 0.58 | NS | |
| PEF (L/s) | −1.34 ± 1.98 | −1.54 ± 2.23 | NS | |
| Gradient of S1 and S3 spirometry tests | FVC (L) | −0.27 ± 0.57 | −0.69 ± 0.51 | <0.001 |
| FEV 1.0 (L) | −0.10±0.65 | −0.33 ± 0.57 | NS | |
| PEF (L/s) | −0.17 ± 2.24 | −0.18 ± 2.56 | NS | |
| Gradient of S2 and S3 spirometry tests | FVC (L) | 0.68 ± 0.54 | 0.45 ± 0.47 | 0.009 |
| FEV 1.0 (L) | 0.71 ± 0.55 | 0.52 ± 0.46 | NS | |
| PEF (L/s) | 1.17 ± 2.21 | 1.36 ± 1.57 | NS | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szylińska, A.; Listewnik, M.; Rotter, I.; Rył, A.; Kotfis, K.; Mokrzycki, K.; Kuligowska, E.; Walerowicz, P.; Brykczyński, M. The Efficacy of Inpatient vs. Home-Based Physiotherapy Following Coronary Artery Bypass Grafting. Int. J. Environ. Res. Public Health 2018, 15, 2572. https://doi.org/10.3390/ijerph15112572
Szylińska A, Listewnik M, Rotter I, Rył A, Kotfis K, Mokrzycki K, Kuligowska E, Walerowicz P, Brykczyński M. The Efficacy of Inpatient vs. Home-Based Physiotherapy Following Coronary Artery Bypass Grafting. International Journal of Environmental Research and Public Health. 2018; 15(11):2572. https://doi.org/10.3390/ijerph15112572
Chicago/Turabian StyleSzylińska, Aleksandra, Mariusz Listewnik, Iwona Rotter, Aleksandra Rył, Katarzyna Kotfis, Krzysztof Mokrzycki, Ewelina Kuligowska, Paweł Walerowicz, and Mirosław Brykczyński. 2018. "The Efficacy of Inpatient vs. Home-Based Physiotherapy Following Coronary Artery Bypass Grafting" International Journal of Environmental Research and Public Health 15, no. 11: 2572. https://doi.org/10.3390/ijerph15112572
APA StyleSzylińska, A., Listewnik, M., Rotter, I., Rył, A., Kotfis, K., Mokrzycki, K., Kuligowska, E., Walerowicz, P., & Brykczyński, M. (2018). The Efficacy of Inpatient vs. Home-Based Physiotherapy Following Coronary Artery Bypass Grafting. International Journal of Environmental Research and Public Health, 15(11), 2572. https://doi.org/10.3390/ijerph15112572





