Eating Frequency Is Not Associated with Obesity in Chinese Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Assessment of Sociodemographic Characteristics
2.3. Assessment and Definition of EF
2.4. Evaluation of Nutrition Knowledge
2.5. Assessment of Overweight/Obesity and Physical Activity
2.6. Statistical Analysis
3. Results
3.1. Demographic Information
3.2. Differences in BMI Distribution, Nutrition Knowledge, and Food Budget among EF Patterns
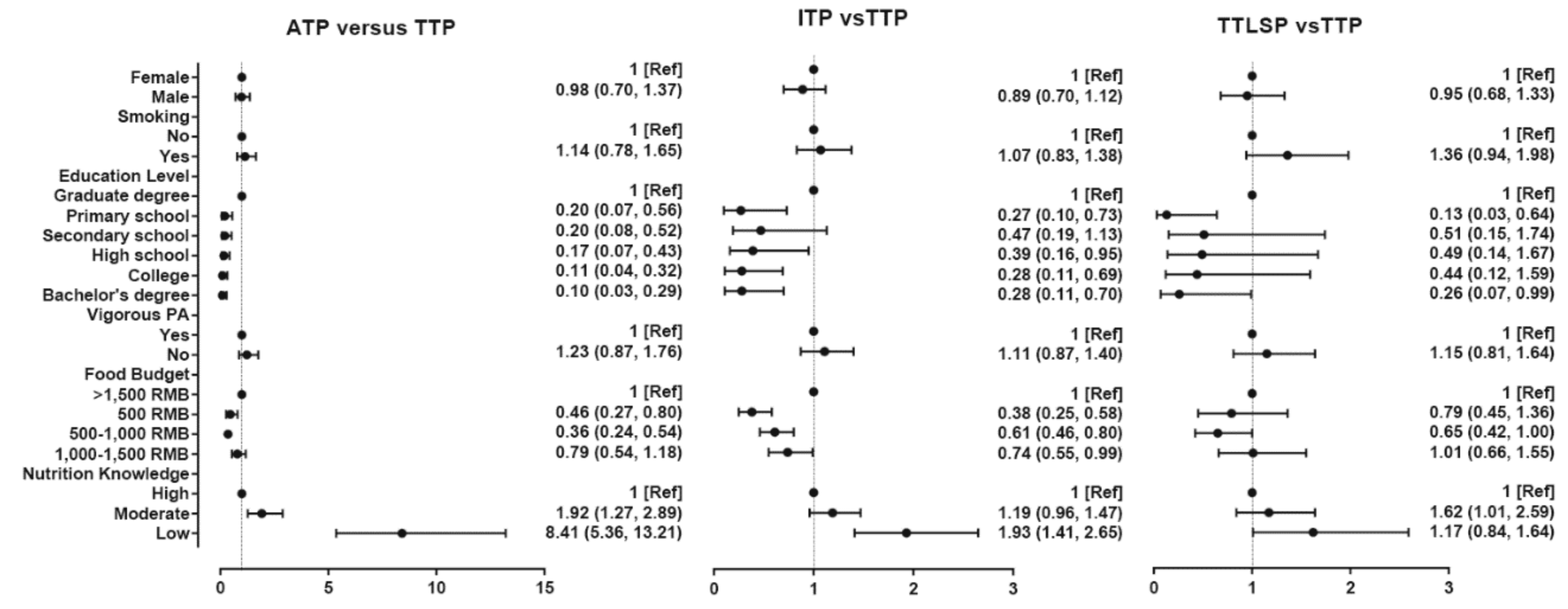
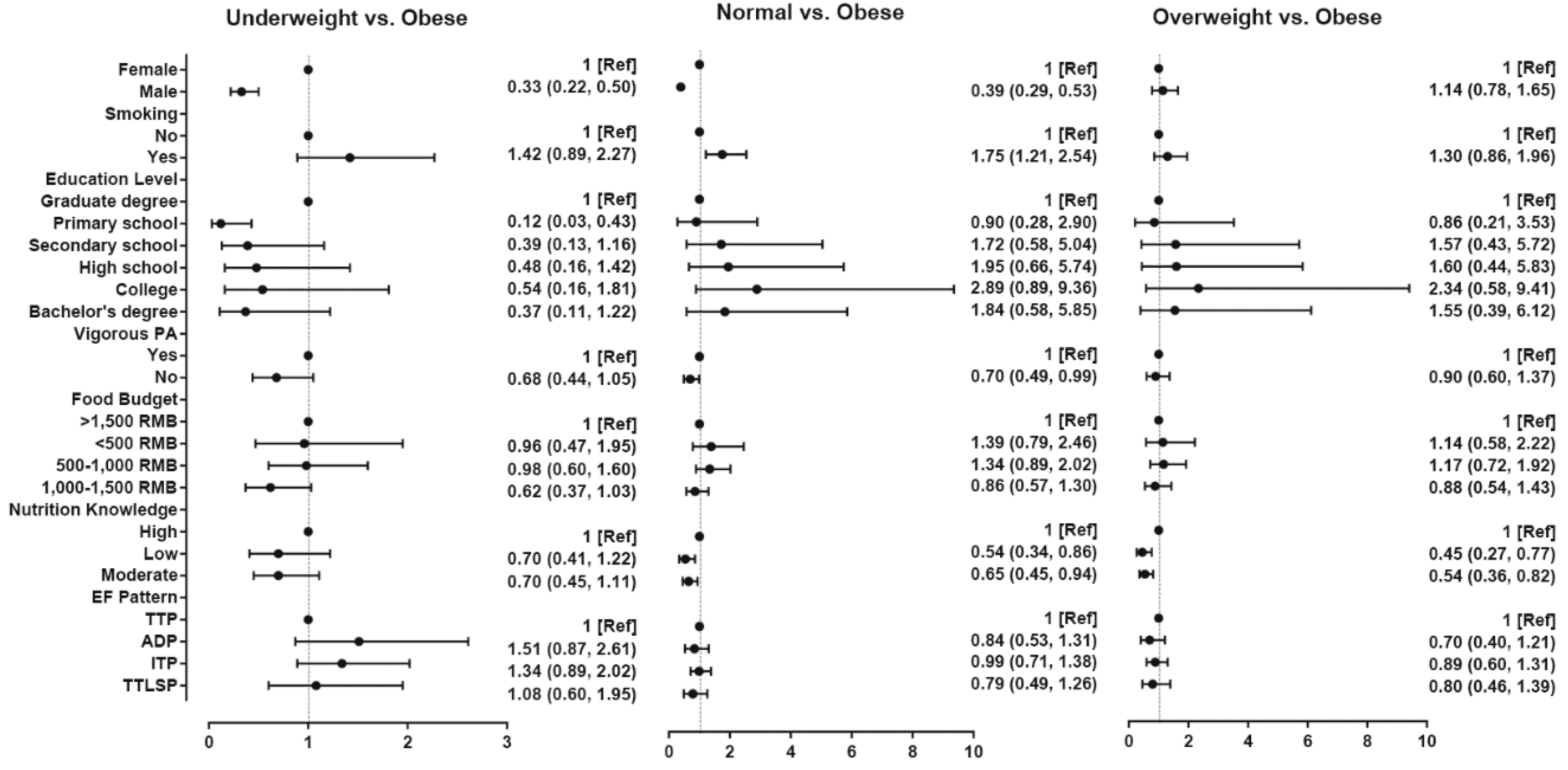
3.3. Associations among EF Pattern, Nutrition Knowledge, Sociodemographic, and Lifestyle Factors and BMI Group
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- World Health Organization. Obesity and Overweight. Available online: www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 30 June 2018).
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Zhang, C.; Rexrode, K.M.; van Dam, R.M.; Li, T.Y.; Hu, F.B. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality sixteen years of follow-up in US Women. Circulation 2008, 117, 1658–1667. [Google Scholar] [CrossRef] [PubMed]
- Felson, D.T.; Anderson, J.J.; Naimark, A.; Walker, A.M.; Meenan, R.F. Obesity and knee osteoarthritis: The Framingham study. Ann. Int. Med. 1988, 109, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Calle, E.E.; Rodriguez, C.; Walker-Thurmond, K.; Thun, M.J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N. Engl. J. Med. 2003, 348, 1625–1638. [Google Scholar] [CrossRef] [PubMed]
- Fábry, P.; Hejl, Z.; Fodor, J.; Braun, T. The frequency of meals: Its relation to overweight, hypercholesterolaemia, and decreased glucose-tolerance. Lancet 1964, 2, 614–615. [Google Scholar] [CrossRef]
- Yannakoulia, M.; Melistas, L.; Solomou, E.; Yiannakouris, N. Association of eating frequency with body fatness in pre- and postmenopausal women. Obesity 2012, 15, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Livingstone, M.B. Eating frequency in relation to body mass index and waist circumference in British adults. Int. J. Obes. (Lond.) 2014, 38, 1200–1206. [Google Scholar] [CrossRef] [PubMed]
- Jaaskelainen, A.; Schwab, U.; Kolehmainen, M.; Pirkola, J.; Jarvelin, M.R.; Laitinen, J. Associations of meal frequency and breakfast with obesity and metabolic syndrome traits in adolescents of Northern Finland Birth Cohort 1986. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 1002–1009. [Google Scholar] [CrossRef] [PubMed]
- Arciero, P.J.; Ormsbee, M.J.; Gentile, C.L.; Nindl, B.C.; Brestoff, J.R.; Ruby, M. Increased protein intake and meal frequency reduces abdominal fat during energy balance and energy deficit. Obesity 2013, 21, 1357–1366. [Google Scholar] [CrossRef] [PubMed]
- Marín-Guerrero, A.C.; Gutiérrez-Fisac, J.L.; Guallar-Castillón, P.; Banegas, J.R.; Rodríguez-Artalejo, F. Eating behaviors and obesity in the adult population of Spain. Br. J. Nutr. 2008, 100, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Bertone, E.R.; Stanek, E.J.; Reed, G.W.; Hebert, J.R.; Cohen, N.L.; Merriam, P.A.; Ockene, I.S. Association between eating patterns and obesity in a free-living US adult population. Am. J. Epidemiol. 2003, 158, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Drummond, S.E.; Crombie, N.E.; Cursiter, M.C.; Kirk, T.R. Evidence that eating frequency is inversely related to body weight status in male, but not female, non-obese adults reporting valid dietary intakes. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Bongard, V. Eating frequency and body fatness in middle-aged men. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 1476–1483. [Google Scholar]
- Huseinovic, E.; Winkvist, A.; Bertz, F.; Bertéus, F.H.; Brekke, H.K. Eating frequency, energy intake and body weight during a successful weight loss trial in overweight and obese postpartum women. Eur. J. Clin. Nutr. 2014, 68, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K.; Schatzkin, A.; Graubard, B.I.; Ballardbarbash, R. Frequency of eating occasions and weight change in the NHANES I Epidemiologic Follow-up Study. Int. J. Obes. Relat. Metab. Disord. 1995, 19, 468–474. [Google Scholar] [PubMed]
- Duval, K.; Strychar, I.; Cyr, M.J.; Prud’Homme, D.; Rabasa-Lhoret, R.; Doucet, E. Physical activity is a confounding factor of the relation between eating frequency and body composition. Am. J. Clin. Nutr. 2008, 88, 1200–1205. [Google Scholar] [PubMed]
- Murakami, K.; Livingstone, M.B. Eating frequency is positively associated with overweight and central obesity in US adults. J. Nutr. 2015, 145, 2715–2724. [Google Scholar] [CrossRef] [PubMed]
- Stote, K.S.; Baer, D.J.; Spears, K.; Paul, D.R.; Harris, G.K.; Rumpler, W.V.; Strycula, P.; Najjar, S.S.; Ferrucci, L.; Ingram, D.K. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults. Am. J. Clin. Nutr. 2007, 85, 981–988. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, L.D. Less frequent eating predicts greater BMI and waist circumference in female adolescents. Am. J. Clin. Nutr. 2012, 95, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Duffey, K.J.; Pereira, R.A.; Popkin, B.M. Prevalence and energy intake from snacking in Brazil: Analysis of the first nationwide individual survey. Eur. J. Clin. Nutr. 2013, 67, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K.; Graubard, B.I. 40-year trends in meal and snack eating behaviors of American adults. J. Acad. Nutr. Diet. 2015, 115, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Makela, J.; Kjaernes, U.; Pipping, E.M.; L’Orange, F.E.; Gronow, J.; Holm, L. Nordic meals: Methodological notes on a comparative survey. Appetite 1999, 32, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.K.; Rehkopf, D.H.; Deardorff, J.; Abrams, B. Education and obesity at age 40 among American adults. Soc. Sci. Med. 2013, 78, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Hankey, C.R.; Eley, S.; Leslie, W.S.; Hunter, C.M.; Lean, M.E. Eating habits, beliefs, attitudes and knowledge among health professionals regarding the links between obesity, nutrition and health. Public Health Nutr. 2004, 7, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di, C.A.; Costanzo, S.; De, L.F.; Olivieri, M.; Donati, M.B.; De, G.G.; Iacoviello, L.; Bonanni, A. Nutrition knowledge is associated with higher adherence to Mediterranean diet and lower prevalence of obesity. Results from the Moli-sani study. Appetite 2013, 68, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Chen, W.; Sun, D.; Li, S.; Millwood, I.Y.; Smith, M.; Guo, Y.; Bian, Z.; Yu, C.; Zhou, H. Gender-specific association between tobacco smoking and central obesity among 0.5 million Chinese people: The China kadoorie biobank study. PLoS ONE 2015, 10, e124586. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Carroll, M.D.; Kit, B.K.; Ogden, C.L. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 2012, 307, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Main, M.L.; Rao, S.C.; O’Keefe, J.H. Trends in obesity and extreme obesity among US adults. JAMA 2010, 303, 1695–1696. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Statistics of China. Statistical Communiqué of the People’s Republic of China on the 2013 National Economic and Social Development, 1st ed.; China Statistics Press: Beijing, China, 2014; pp. 12–16.
- Shi, Q.J. Analysis of Knowledge-Attitude-Practice and Health Intervention About Nutritional in Parents of Preschool Children in Yingkou. Master’s Thesis, Dalian Medical University, Dalian, China, 29 November 2017. [Google Scholar]
- Department of Disease Control, Ministry of Health of the People’s Republic of China. Guidelines for Prevention and Control of Overweight and Obesity in Adults in China; People’s Medical Publishing House: Beijing, China, 2006.
- Zhu, Y.; Hollis, J.H. Associations between eating frequency and energy intake, energy density, diet quality and body weight status in adults from the USA. Br. J. Nutr. 2016, 115, 2138–2144. [Google Scholar] [CrossRef] [PubMed]
- Beyene, M.; Worku, A.G.; Wassie, M.M. Dietary diversity, meal frequency and associated factors among infant and young children in Northwest Ethiopia: A cross-sectional study. BMC Public Health 2015, 15, 1007. [Google Scholar] [CrossRef] [PubMed]
- Nuvoli, G. Family meal frequency, weight status and healthy management in children, young adults and seniors. A study in Sardinia, Italy. Appetite 2015, 89, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Hassanzadeh, S.; Saneei, P.; Keshteli, A.H.; Daghaghzadeh, H.; Esmaillzadeh, A.; Adibi, P. Meal frequency in relation to prevalence of functional dyspepsia among Iranian adults. Nutrition 2015, 32, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Saunders, M. Trends in Overweight and Obesity Among Korean Children and Adolescents, 1998–2010. In Proceedings of the 141st APHA Annual Meeting and Exposition 2013, Boston, MA, USA, 2–6 November 2013. [Google Scholar]
- Flegal, K.M.; Kruszon-Moran, D.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016, 315, 2284–2291. [Google Scholar] [CrossRef] [PubMed]
- Hartlinegrafton, H.L.; Rose, D.; Johnson, C.C.; Rice, J.C.; Webber, L.S. The influence of weekday eating patterns on energy intake and BMI among female elementary school personnel. Obesity 2010, 18, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Mills, J.P.; Perry, C.D.; Reicks, M. Eating frequency is associated with energy intake but not obesity in midlife women. Obesity 2011, 19, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, A.T.; Heilbronn, L.K. Metabolic impacts of altering meal frequency and timing—Does when we eat matter? Biochimie 2016, 124, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Ohkawara, K.; Cornier, M.A.; Kohrt, W.M.; Melanson, E.L. Effects of increased meal frequency on fat oxidation and perceived hunger. Obesity 2013, 21, 336–343. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Male (N = 1162) | Female (N = 1128) | Total (N = 2290) | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Age group | ||||||
| 29–34 | 27 | 2% | 40 | 4% | 67 | 3% |
| 34–39 | 158 | 14% | 284 | 25% | 442 | 19% |
| 39–44 | 530 | 46% | 545 | 48% | 1075 | 47% |
| 44–49 | 356 | 31% | 213 | 19% | 569 | 25% |
| 49–54 | 70 | 6% | 32 | 3% | 102 | 4% |
| 54–59 | 13 | 1% | 6 | 1% | 19 | 1% |
| 59–64 | 5 | 0% | 3 | 0% | 8 | 0% |
| 64–69 | 2 | 0% | 4 | 0% | 6 | 0% |
| 69–74 | 1 | 0% | 1 | 0% | 2 | 0% |
| Highest level of education | ||||||
| Primary school | 49 | 4% | 68 | 6% | 117 | 5% |
| Secondary school | 420 | 36% | 409 | 36% | 829 | 36% |
| High school | 442 | 38% | 430 | 38% | 872 | 38% |
| College | 117 | 10% | 108 | 10% | 225 | 10% |
| Bachelor’s degree | 111 | 10% | 94 | 8% | 205 | 9% |
| Graduate degree | 23 | 2% | 19 | 2% | 42 | 2% |
| Smoking | ||||||
| Yes | 548 | 47% | 33 | 3% | 581 | 25% |
| No | 614 | 53% | 1095 | 97% | 1709 | 75% |
| Food budget monthly | ||||||
| Less than 500 RMB | 141 | 12% | 93 | 8% | 234 | 10% |
| 500–1000 RMB | 474 | 41% | 504 | 45% | 978 | 43% |
| 1000–1500 RMB | 350 | 30% | 338 | 30% | 688 | 30% |
| More than 1500 RMB | 197 | 17% | 193 | 17% | 390 | 17% |
| Vigorous PA (4+ days) | ||||||
| No | 878 | 76% | 916 | 81% | 1794 | 78% |
| Yes | 284 | 24% | 212 | 19% | 496 | 22% |
| Nutrition knowledge | ||||||
| Low | 220 | 19% | 168 | 15% | 388 | 17% |
| Moderate | 659 | 57% | 624 | 55% | 1283 | 56% |
| High | 283 | 24% | 336 | 30% | 619 | 27% |
| BMI Group | ||||||
| Normal | 613 | 53% | 724 | 64% | 1337 | 58% |
| Obese | 147 | 13% | 87 | 8% | 234 | 10% |
| Overweight | 278 | 24% | 134 | 12% | 412 | 18% |
| Underweight | 124 | 11% | 183 | 16% | 307 | 13% |
| EF pattern | ||||||
| ADP | 12.31% | 143 | 10.82% | 122 | 265 | 12% |
| TTLSP | 10.93% | 127 | 9.66% | 109 | 236 | 10% |
| ITP | 28.66% | 333 | 31.38% | 354 | 687 | 30% |
| TTP | 48.11% | 559 | 48.13% | 543 | 1102 | 48% |
| Underweight | Normal | Overweight | Obese | All | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | |
| EF Pattern | |||||||||
| ADP | 53 | 20.00% | 139 | 52.45% | 39 | 14.72% | 34 | 12.83% | 265 |
| TTLSP | 33 | 13.98% | 132 | 55.93% | 44 | 18.64% | 27 | 11.44% | 236 |
| ITP | 104 | 15.14% | 400 | 58.22% | 115 | 16.74% | 68 | 9.90% | 687 |
| TTP | 117 | 10.62% | 666 | 60.44% | 214 | 19.42% | 105 | 9.53% | 1102 |
| All | 307 | 13.41% | 1337 | 58.38% | 412 | 17.99% | 234 | 10.22% | 2290 |
| Low | Moderate | High | All | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | |
| EF Pattern | |||||||
| ADP | 110 | 41.51% | 121 | 45.66% | 34 | 12.83% | 265 |
| ITP | 122 | 17.76% | 389 | 56.62% | 176 | 25.62% | 687 |
| TTLSP | 36 | 15.25% | 137 | 58.05% | 63 | 26.69% | 236 |
| TTP | 120 | 10.89% | 636 | 57.71% | 346 | 31.40% | 1102 |
| All | 388 | 16.94% | 1283 | 56.03% | 619 | 27.03% | 2290 |
| Less than 500 RMB | 500–1000 RMB | 1000–1500 RMB | More than 1500 RMB | All | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | |
| EF Pattern | |||||||||
| ADP | 27 | 10.19% | 75 | 28.30% | 96 | 36.23% | 67 | 25.28% | 265 |
| ITP | 48 | 6.99% | 295 | 42.94% | 207 | 30.13% | 137 | 19.94% | 236 |
| TTLSP | 27 | 11.44% | 89 | 37.71% | 81 | 34.32% | 39 | 16.53% | 687 |
| TTP | 132 | 11.98% | 519 | 47.10% | 304 | 27.59% | 147 | 13.34% | 1102 |
| All | 27 | 10.19% | 75 | 28.30% | 96 | 36.23% | 67 | 25.28% | 2290 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, X.; Wang, Y.; Brinkley, J.S.; Oniffrey, T.M.; Zhang, R.; Chen, G.; Li, R.; Moore, J.B. Eating Frequency Is Not Associated with Obesity in Chinese Adults. Int. J. Environ. Res. Public Health 2018, 15, 2561. https://doi.org/10.3390/ijerph15112561
Zhang X, Wang Y, Brinkley JS, Oniffrey TM, Zhang R, Chen G, Li R, Moore JB. Eating Frequency Is Not Associated with Obesity in Chinese Adults. International Journal of Environmental Research and Public Health. 2018; 15(11):2561. https://doi.org/10.3390/ijerph15112561
Chicago/Turabian StyleZhang, Xinge, Yueqiao Wang, Jason S. Brinkley, Theresa M. Oniffrey, Rui Zhang, Guoxun Chen, Rui Li, and Justin B. Moore. 2018. "Eating Frequency Is Not Associated with Obesity in Chinese Adults" International Journal of Environmental Research and Public Health 15, no. 11: 2561. https://doi.org/10.3390/ijerph15112561
APA StyleZhang, X., Wang, Y., Brinkley, J. S., Oniffrey, T. M., Zhang, R., Chen, G., Li, R., & Moore, J. B. (2018). Eating Frequency Is Not Associated with Obesity in Chinese Adults. International Journal of Environmental Research and Public Health, 15(11), 2561. https://doi.org/10.3390/ijerph15112561







