Is Vaginal Birth without an Episiotomy a Rarity in the 21st Century? Cross-Sectional Studies in Southern Poland
Abstract
1. Introduction
2. Methods
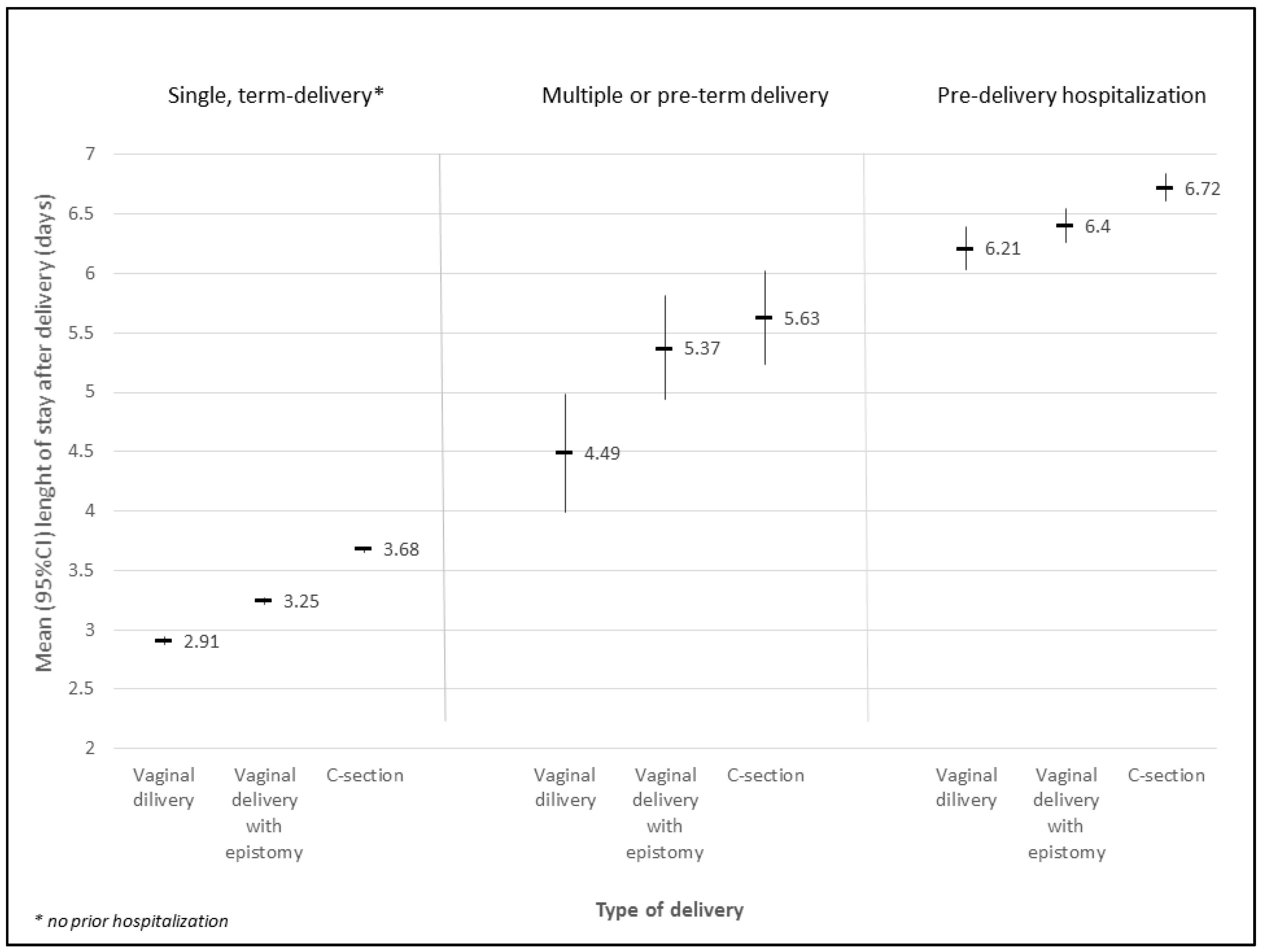
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Availability of Data and Materials
Conflicts of Interest
Abbreviations
| CI | confidence interval |
| CS | caesarean section |
| LOS | length of stay |
| NB | normal birth |
| NFZ | Polish National Health Fund |
| OR | odds ratio |
References
- World Health Organization. Report of a Technical Working Group, Care in Normal Birth: A Practical Guide. 1996. Available online: http://www.who.int/maternal_child_adolescent/documents/who_frh_msm_9624/en/ (accessed on 1 May 2018).
- World Health Organization. Appropriate technology for birth. Lancet 1985, 2, 436–443. [Google Scholar]
- Wax, J.R. Maternal request Caesarean versus planned spontaneous vaginal birth: Maternal morbidity and short term outcomes. Semin. Perinatol. 2006, 30, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Liston, R.M.; Joseph, K.S.; Heaman, M.; Sauve, R.; Kramer, M.S. Maternal mortality and severe morbidity associated with low-risk planned Caesarean birth versus planned vaginal birth at term. Can. Med. Assoc. J. 2007, 176, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Armson, B.A. Is planned Caesarean childbirth a safe alternative? Can. Med. Assoc. J. 2007, 176, 475–476. [Google Scholar] [CrossRef] [PubMed]
- Black, M.; Bhattacharya, S.; Philip, S.; Norman, J.E.; McLernon, D.J. Planned Caesarean Birth at Term and Adverse Outcomes in Childhood Health. JAMA 2015, 314, 2271–2279. [Google Scholar] [CrossRef] [PubMed]
- Luce, A.; Cash, M.; Hundley, V.; Cheyne, H.; van Teijlingen, E.; Angell, C. “Is it realistic?” the portrayal of pregnancy and childbirth in the media. BMC Pregnancy Childbirth 2016, 16, 40. [Google Scholar] [CrossRef] [PubMed]
- Fenwick, J.; Staff, L.; Gamble, J.; Creedy, D.K.; Bayes, S. Why do women request caesarean section in a normal, healthy first pregnancy? Midwifery 2010, 26, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Fahy, K.; Hastie, C.; Bisits, A.; Marsh, C.; Smith, L.; Saxton, A. Holistic physiological care compared with active management of the third stage of labour for women at low risk of postpartum haemorrhage: A cohort study. Women Birth 2010, 23, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Central Statistical Office of Poland. Available online: http://www.statystyka.medstat.waw.pl/wyniki/wyniki.htm (accessed on 1 May 2018).
- Central Statistical Office of Poland. Available online: http://demografia.stat.gov.pl/BazaDemografia/ (accessed on 1 May 2018).
- Loudon, I. Maternal mortality in the past and its relevance to developing countries today. Am. J. Clin. Nutr. 2000, 72 (Suppl. 1), 241S–246S. [Google Scholar] [CrossRef] [PubMed]
- Cowgill, K.D.; Bishop, J.; Norgaard, A.K.; Rubens, C.E.; Gravett, M.G. Obstetric fistula in low-resource countries: An under-valued and under-studied problem—Systematic review of its incidence, prevalence, and association with stillbirth. BMC Pregnancy Childbirth 2015, 15, 193. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, K.L.; Borup, K. Course of delivery in obese women after normal pregnancies. Ugeskr. Laeger 1991, 153, 514–516. [Google Scholar] [PubMed]
- Mizrachi, Y.; Leytes, S.; Levy, M.; Hiaev, Z.; Ginath, S.; Bar, J.; Kovo, M. Does midwife experience affect the rate of severe perineal tears? Birth 2017, 44, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Health Monitoring Programme. Reproductive Health Indicators in European Union. Available online: http://ec.europa.eu/health/ph_projects/2001/monitoring/fp_monitoring_2001_a1_frep_02_en.pdf (accessed on 1 May 2018).
- Myers-Helfgott, M.G.; Helfgptt, A. Routine use of episiotomy in modern obstetrics. Should it be performed? Obstet. Gynecol. Clin. N. Am. 1999, 26, 305–325. [Google Scholar] [CrossRef]
- Muhleman, M.A.; Aly, I.; Walters, A.; Topale, N.; Tubbs, R.S.; Loukas, M. To cut or not to cut, that is the question: A review of the anatomy, the technique, risks, and benefits of an episiotomy. Clin. Anat. 2017, 30, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.P.; Gülmezoglu, A.M.; Lumbiganon, P.; Laopaiboon, M.; Carroli, G.; Fawole, B.; Ruyan, P. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: The 2004–2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010, 10, 71. [Google Scholar] [CrossRef] [PubMed]
- Graham, I.D.; Carroli, G.; Davies, C.; Medves, J.M. Episiotomy Rates Around the World: An Update. Birth 2005, 32, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, B.E.; Martin, J.A.; Osterman, M.J.; Curtaun, S.C. Births: Preliminary data for 2014. Natl. Vital Stat. Rep. 2015, 64, 1–19. [Google Scholar] [PubMed]
- MacFarlane, A.J.; Blondel, B.; Mohangoo, A.D.; Cuttini, M.; Nijhuis, J.; Novak, Z.; Ólafsdóttir, H.S.; Zeitlin, J.; Euro-Peristat Scientific Committee. Wide differences in mode of birth within Europe: Risk stratified analyses of aggregated routine data from the Euro-Peristat study. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Mylonas, I.; Friese, K. Indications for and Risks of Elective Caesarean Section. Dtsch. Ärzteblatt Int. 2015, 112, 489–495. [Google Scholar] [CrossRef]
- Gorman, D.R.; Katikireddi, S.V.; Morris, C.; Chalmers, J.W.; Sim, J.; Szamotulska, K.; Mierzejewska, E.; Hughes, R.G. Ethnic variation in maternity care: A comparison of Polish and Scottish women delivering in Scotland 2004–2009. Public Health 2014, 128, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Lundgren, I.; van Limbeek, E.; Vehvilainen-Julkunen, K.; Nilsson, C. Clinicians’ views of factors of importance for improving the rate of VBAC (vaginal birth after caesarean section): A study from countries with low VBAC rates. BMC Pregnancy Childbirth 2016, 16, 350. [Google Scholar] [CrossRef] [PubMed]
- Albers, L.; Sedler, K.; Bedrick, E.; Teaf, D.; Peralta, P. Factors related to genital tract trauma in normal spontaneous vaginal births. Birth 2006, 33, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Rozanska, A.; Pac, A.; Romanik, M.; Bulanda, M.; Wojkowska-Mach, J. Outpatient post-partum antibiotic prescription: Method of identification of infection control areas demanding improvements and verification of sensitivity of infection registration. J. Antimicrob. Chemother. 2018, 73, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Shorten, A.; Donsante, J.; Shorten, B. Birth position, accoucheur, and perineal outcomes: Informing women about choices for vaginal birth. Birth 2002, 29, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Aasheim, V.; Nilsen, A.B.V.; Reinar, L.M.; Lukasse, M. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst. Rev. 2017, 6, CD006672. [Google Scholar] [CrossRef] [PubMed]
- Blomberg, M. Avoiding the first Caesarean section—Results of structured organizational and cultural changes. Acta Obstet. Gynecol. Scand. 2016, 95, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Swift, E.M.; Gottfredsdottir, H.; Zoega, H.; Gross, M.M.; Stoll, K. Opting for natural birth: A survey of birth intentions among young Icelandic women. Sex Reprod. Healthc. 2017, 11, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Brocklehurst, P.; Hardy, P.; Hollowell, J.; Linsell, L.; Macfarlane, A.; McCourt, C.; Marlow, N.; Miller, A.; Newburn, M.; Petrou, S.; et al. Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: The Birthplace in England national prospective cohort study. BMJ 2011, 343, d7400. [Google Scholar] [CrossRef] [PubMed]
- Walsh, S. Having a Baby in The Netherlands, Access Guide 2012. Available online: www.access-nl.org (accessed on 1 May 2018).
| Women Giving Birth N (%) | |
|---|---|
| Age (years) | |
| <18 | 393 (0.6) |
| 18–34 | 57,326 (84.4) |
| ≥35 | 10,198 (15.0) |
| Place of residence | |
| Village | 37,268 (54.9) |
| Town < 100,000 residents | 13,923 (20.5) |
| City > 100,000 residents | 16,679 (24.6) |
| Referral level of hospital where birth took place | |
| 1st | 15,875 (23.4) |
| 2nd | 46,502 (68.5) |
| 3rd | 5540 (8.2) |
| Clinical Characteristics of Women | Vaginal Birth N (%) | C-Section N (%) | Total N (%) | p-Value | |
|---|---|---|---|---|---|
| Without Episiotomy | With Episiotomy | ||||
| Age (years) | |||||
| <18 | 51 (13.0) | 211 (53.7) | 131 (33.3) | 393 (100.0) | Chi2(4) = 852.3; p < 0.001 |
| 18–34 | 12,634 (22.0) | 20,433 (35.6) | 24,259 (42.3) | 57,326 (100.0) | |
| ≥35 | 2842 (27.9) | 2195 (21.5) | 5161 (50.6) | 10,198 (100.0) | |
| Place of residence | |||||
| Village | 8982 (24.1) | 12,963 (34.8) | 15,323 (41.1) | 37,268 (100.0) | Chi2(4) = 280.7; p < 0.001 |
| Town < 100,000 residents | 2840 (20.4) | 4864 (34.9) | 6219 (44.7) | 13,923 (100.0) | |
| City > 100,000 residents | 3698 (22.2) | 4996 (30.0) | 7985 (47.9) | 16,679 (100.0) | |
| Day of the week of birth | |||||
| Monday | 2368 (21.4) | 3384 (30.6) | 5313 (48.0) | 11,065 (100.0) | Chi2(12) = 1140.0; p < 0.001 |
| Tuesday | 2341 (21.3) | 3546 (32.3) | 5078 (46.3) | 10,965 (100.0) | |
| Wednesday | 2375 (21.6) | 3474 (31.7) | 5122 (46.7) | 10,961 (100.0) | |
| Thursday | 2221 (21.1) | 3417 (32,4) | 4897 (46.5) | 10,535 (100.0) | |
| Friday | 2366 (22.6) | 3265 (31.2) | 4828 (46.2) | 4828 (100.0) | |
| Saturday | 1979 (27.8) | 2950 (41.5) | 2178 (30.6) | 7107 (100.0) | |
| Sunday | 1877 (27.5) | 2803 (41.1) | 2135 (31.3) | 6815 (100.0) | |
| Total | 15,527 (22.9) | 22,839 (33.6) | 29,551 (43.5) | 67,917 (100.0) | |
| Clinical Characteristics of Women | Childbirth * N (%) | Multiple or Premature Labour N (%) | Pre-Birth Hospitalization N (%) | p-Value |
|---|---|---|---|---|
| Age (years) | ||||
| <18 | 268 (68.2) | 10 (2.5) | 115 (29.3) | Chi2(4) = 67.5; p < 0.001 |
| 18–34 | 44,856 (78.2) | 1039 (1.8) | 11,431 (19.9) | |
| ≥35 | 7771 (76.2) | 276 (2.7) | 2151 (21.1) | |
| Place of residence | ||||
| Village | 29,461 (79.1) | 656 (1.8) | 7151 (19.2) | Chi2(4) = 121.5; p < 0.001 |
| Town < 100,000 residents | 10,872 (78.1) | 242 (1.7) | 2809 (20.2) | |
| City > 100,000 residents | 12,527 (75.1) | 427 (2.6) | 3725 (22.3) | |
| Day of the week of birth | ||||
| Monday | 8713 (78.7) | 167 (1.5) | 2185 (19.7) | Chi2(12) = 109.5; p < 0.001 |
| Tuesday | 8510 (77.6) | 199 (1.8) | 2256 (20.6) | |
| Wednesday | 8452 (77.0) | 190 (1.7) | 2329 (21.2) | |
| Thursday | 8047 (76.4) | 215 (2.0) | 2273 (21.6) | |
| Friday | 8066 (77.1) | 211 (2.0) | 2182 (20.9) | |
| Saturday | 5660 (79.6) | 186 (2.6) | 1261 (17.7) | |
| Sunday | 5447 (79.9) | 157 (2.3) | 1211 (17.8) | |
| Total | 15,527 (22.9) | 29,551 (43.5) | 67,917 (100.0) | |
| Clinical Characteristics of Birth Method | Vaginal Birth N (%) | C-Section N (%) | Total N (%) | |
|---|---|---|---|---|
| Without Episiotomy | With Episiotomy | |||
| Childbirth * | 13,330 (25.2) | 18,883 (35.7) | 20,682 (39.1) | 52,895 (100.0) |
| Multiple or premature childbirth | 272 (20.5) | 348 (26.3) | 705 (53.2) | 1325 (100.0) |
| Pregnancy pathology | 1925 (14.1) | 3608 (26.3) | 8164 (59.6) | 13,697 (100.0) |
| Total | 15,527 (22.9) | 22,839 (33.6) | 29,551 (43.5) | 67,917 (100.0) |
| Variable | Vaginal Birth | |||
|---|---|---|---|---|
| Without Episiotomy | With Episiotomy | |||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Referral level of hospital | ||||
| 1st | 2.00 (1.83–2.18) | <0.001 | 2.25 (2.08–2.43) | <0.001 |
| 2nd | 2.11 (1.95–2.27) | <0.001 | 2.51 (2.34–2.70) | <0.001 |
| 3rd | 1.00 | - | 1.00 | - |
| Day of the week | ||||
| Monday | 1.00 | - | 1.00 | - |
| Tuesday | 1.04 (0.97–1.12) | 0.242 | 1.10 (1.04–1.17) | 0.002 |
| Wednesday | 1.05 (0.98–1.12) | 0.194 | 1.07 (1.01–1.14) | 0.023 |
| Thursday | 1.03 (0.96–1.10) | 0.434 | 1.11 (1.04–1.18) | 0.001 |
| Friday | 1.11 (1.04–1.19) | 0.003 | 1.07 (1.00–1.14) | 0.041 |
| Saturday | 2.09 (1.93–2.26) | <0.001 | 2.17 (2.02–2.33) | <0.001 |
| Sunday | 1.99 (1.84–2.15) | <0.001 | 2.06 (1.92–2.21) | <0.001 |
| Place of residence | ||||
| Village | 1.00 | - | 1.00 | - |
| Town < 100,000 residents | 0.78 (0.74–0.82) | 0.780 | 0.94 (0.90–0.98) | 0.006 |
| City > 100,000 residents | 0.84 (0.80–0.88) | 0.839 | 0.81 (0.78–0.85) | <0.001 |
| Age [years] | ||||
| <18 | 0.75 (0.54–1.04) | 0.083 | 1.89 (1.51–2.36) | <0.001 |
| 18–34 | 1.00 | - | 1.00 | - |
| ≥35 | 1.10 (1.05–1.16) | <0.001 | 0.53 (0.50–0.56) | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kopeć-Godlewska, K.; Pac, A.; Różańska, A.; Wójkowska-Mach, J. Is Vaginal Birth without an Episiotomy a Rarity in the 21st Century? Cross-Sectional Studies in Southern Poland. Int. J. Environ. Res. Public Health 2018, 15, 2462. https://doi.org/10.3390/ijerph15112462
Kopeć-Godlewska K, Pac A, Różańska A, Wójkowska-Mach J. Is Vaginal Birth without an Episiotomy a Rarity in the 21st Century? Cross-Sectional Studies in Southern Poland. International Journal of Environmental Research and Public Health. 2018; 15(11):2462. https://doi.org/10.3390/ijerph15112462
Chicago/Turabian StyleKopeć-Godlewska, Katarzyna, Agnieszka Pac, Anna Różańska, and Jadwiga Wójkowska-Mach. 2018. "Is Vaginal Birth without an Episiotomy a Rarity in the 21st Century? Cross-Sectional Studies in Southern Poland" International Journal of Environmental Research and Public Health 15, no. 11: 2462. https://doi.org/10.3390/ijerph15112462
APA StyleKopeć-Godlewska, K., Pac, A., Różańska, A., & Wójkowska-Mach, J. (2018). Is Vaginal Birth without an Episiotomy a Rarity in the 21st Century? Cross-Sectional Studies in Southern Poland. International Journal of Environmental Research and Public Health, 15(11), 2462. https://doi.org/10.3390/ijerph15112462







