Making the Case for “Whole System” Approaches: Integrating Public Health and Housing
Abstract
1. Introduction
2. Housing, Habitation and Health
2.1. Air Pollution
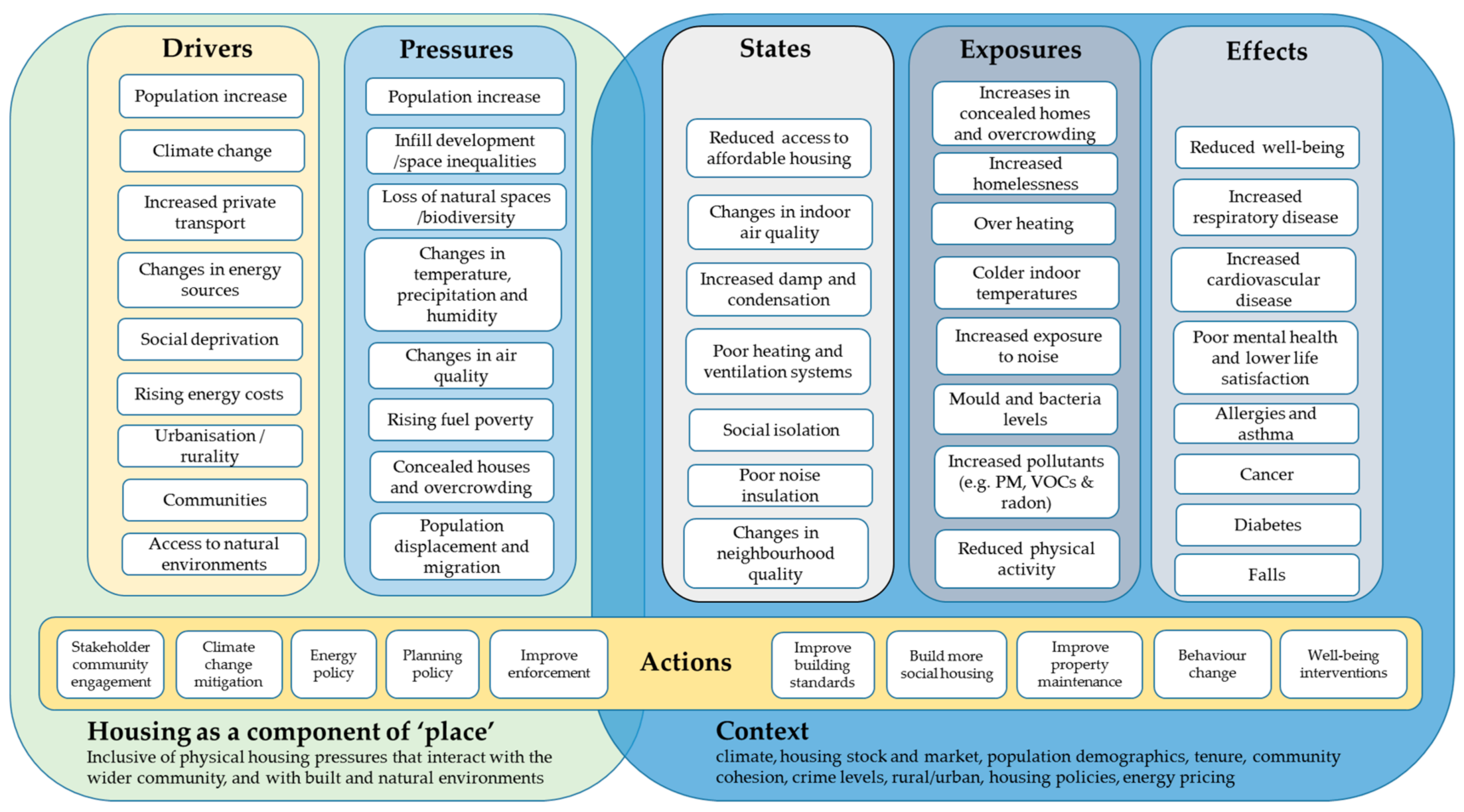
2.2. Aeroallergens
2.3. Cold and Damp Homes
2.4. Overheating of Homes
2.5. Noise Pollution
3. Factors Which Can Influence the Individual’s Ability to Secure Healthy Housing
3.1. Housing Standards
3.2. Housing Affordability
3.3. Health and Housing: Housing Tenure
3.4. Over-Crowding (A Function of Affordability and Tenure)
4. Housing in the Context of “Place”
Neighbourhoods, Communities and Access to Natural Spaces
5. Discussion
5.1. Home Improvements
5.2. Long-Term Prevention, and Community Involvement
5.3. Implications
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Engels, F. Condition of the Working Class in England. 1845. Available online: https://www.marxists.org/archive/marx/works/download/pdf/condition-working-class-england.pdf (accessed on 21 July 2018).
- Green, J.; Labonte, R. Critical Perspectives in Public Health; Routledge: London, UK, 2008. [Google Scholar]
- Krieger, J.; Higgins, D.L. Housing and health: Time again for public health action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Bambra, C.E. A Tackling the wider social determinants of health and health inequalities: Evidence from systematic reviews. J. Epidemiol. Community Health 2010, 64, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Kessel, A. Air, the Environment and Public Health; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar]
- Lalonde, M. A New Perspective on the Health of Canadians: A Working Document = Nouvelle Perspective De La Sante Des Canadiens; Government of Canada: Ottawa, ON, Canada, 1974.
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in health; Institute for Future Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Ratzan, S.C. Health literacy: Communication for the public good. Health Promot. Int. 2001, 16, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.; Stoddart, G. Producing health, consuming healthcare. Soc. Sci. Med. 1990, 31, 1347–1363. [Google Scholar] [CrossRef]
- Barton, H.; Grant, M. A health map for the local human habitat. J. R. Soc. Promot. Health 2006, 126, 252–253. [Google Scholar] [CrossRef] [PubMed]
- Lang, T.; Rayner, G. Ecological public health: The 21st century’s big idea? An essay by Tim Lang and Geof Rayner. BMJ 2012, 345. [Google Scholar] [CrossRef]
- Staatsen, B.; Van Der Vliet, N.; Kruise, H. INHERIT: Exploring Triple-Win Solutions for Living, Moving and Consuming that Encourage Behavioural Change, Protect the Environment, Promote Health and Health Equity; EuroHealthNet: Brussels, Belgium, 2017; Available online: https://issuu.com/revolve-magazine/docs/inherit_baseline_review (accessed on 16 September 2018).
- Sharpe, R.A.; Thornton, C.R.; Nikolaou, V.; Osborne, N.J. Higher energy efficient homes are associated with increased risk of doctor diagnosed asthma in a UK sub population. Environ. Int. 2015, 75, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Bell, R. Fair society, healthy lives. Public Health 2012, 126, S4–S10. [Google Scholar] [CrossRef] [PubMed]
- Bosma, H.; Marmot, M.G.; Hemingway, H.; Nicholson, A.C.; Brunner, E.; Stansfeld, S.A. Low job control and risk of coronary heart disease in whitehall ii (prospective cohort) study. BMJ 1997, 314, 558–565. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.G.; Stansfeld, S.; Patel, C.; North, F.; Head, J.; White, I.; Brunner, E.; Feeney, A.; Marmot, M.G.; Smith, G.D. Health inequalities among British civil servants: The Whitehall II study. Lancet 1991, 337, 1387–1393. [Google Scholar] [CrossRef]
- Brown, V.M.; Crump, D.R.; Harrison, P.T. Assessing and controlling risks from the emission of organic chemicals from construction products into indoor environments. Environ. Sci. Process. Impacts 2013, 15, 2164–2177. [Google Scholar] [CrossRef] [PubMed]
- Mcgratha, J.A.; Sheahan, J.N.; Dimitroulopoulouc, C.; Ashmored, M.R.; Terrye, A.C.; Byrnea, M.A. PM exposure variations due to different time activity profile simulations within a single dwelling. Build. Environ. 2017, 116, 55–63. [Google Scholar] [CrossRef]
- Klepeis, N.E.; Nelson, W.C.; Ott, W.R.; Robinson, J.P.; Tsang, A.M.; Switzer, P.; Behar, J.V.; Hern, S.C.; Engelmann, W.H. The National Human Activity Pattern Survey (NHAPS): A resource for assessing exposure to environmental pollutants. Anal. Environ. Epidemiol. J. Expo. 2001, 11, 231–252. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, C.; Edwards, R.D.; Bayer-Oglesby, L.; Gauderman, W.J.; Ilacqua, V.; Jantunen, M.J.; Lai, H.K.; Nieuwenhuijsen, M.; KüNzli, M. Indoor time microenvironment activity patterns in seven regions of Europe. J. Expo. Sci. Environ. Epidemiol. 2006, 17, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Torfs, R.; Brouwere, K.D.; Spruyt, M.; Goelen, E.; Nickmilder, M.; Bernard, A. Exposure and Risk Assessment of Air Fresheners; Flemish Institute for Technological Research NV (VITO): Mol, Belgium, 2008. [Google Scholar]
- Hodas, N.; Loh, M.; Shin, H.M.; Li, D.; Bennett, D.; Mckone, T.E.; Jolliet, O.; Weschler, C.J.; Jantunen, M.; Lioy, P.; et al. Indoor inhalation intake fractions of fine particulate matter: Review of influencing factors. Indoor Air 2016, 26, 836–856. [Google Scholar] [CrossRef] [PubMed]
- Royal Colleage of Physicians. Every Breath We Take: The Lifelong Impact of Air Pollution; RCP policy and Public health: London, UK, 2016. [Google Scholar]
- Sharpe, R.A.; Thornton, C.R.; Osborne, N.J. Modifiable Factors Governing Indoor Fungal Diversity and Risk of Asthma. Clin. Exp. Allergy 2014, 44, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Semple, S.; Garden, C.; Coggins, M.; Galea, K.S.; Whelan, P.; Cowie, H.; Sánchez-Jiménez, A.; Thorne, P.S.; Hurley, J.F.; Ayres, J.G. Contribution of solid fuel, gas combustion, or tobacco smoke to indoor air pollutant concentrations in Irish and Scottish homes. Indoor Air 2012, 22, 212–223. [Google Scholar] [CrossRef] [PubMed]
- Dales, R.; Liu, L.; Wheeler, A.J.; Gilbert, N.L. Quality of indoor residential air and health. Can. Med Assoc. J. 2008, 179, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Ikeda, K. Variations of formaldehyde and VOC levels during 3 years in new and older homes. Indoor Air 2006, 16, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Jaakkola JJ, K.; Ieromnimon, A.; Jaakkola, M.S. Interior Surface Materials and Asthma in Adults: A Population-based Incident Case-Control Study. Am. J. Epidemiol. 2006, 164, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Darby, S.; Hill, D.; Auvinen, A.; Barros-Dios, J.M.; Baysson, H.; Bochicchio, F.; Deo, H.; Falk, R.; Forastiere, F.; Hakama, M.; et al. Radon in homes and risk of lung cancer: Collaborative analysis of individual data from 13 European case-control studies. BMJ 2005, 330, 223. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.G.; Cote, M.L. Epidemiology of Lung Cancer. Adv. Exp. Med. Biol. 2016, 893, 21–41. [Google Scholar] [PubMed]
- RCPCH (Royal College of Physicians). Every Breath We Take: The Lifelong Impact of Air Pollution; Royal College of Physicians: London, UK, 2016. Available online: https://www.rcplondon.ac.uk/projects/outputs/every-breath-we-take-lifelong-impact-air-pollution (accessed on 11 December 2016).
- Gordon, S.B.; Bruce, N.G.; Grigg, J.; Hibberd, P.L.; Kurmi, O.P.; Lam, K.-B.H.; Mortimer, K.; Asante, K.P.; Balakrishnan, K.; Balmes, J. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2014, 2, 823–860. [Google Scholar] [CrossRef]
- Torres-Duque, C.E. A Biomass Fuels and Respiratory Diseases. Proc. Am. Thorac. Soc. 2008, 5, 577–590. [Google Scholar] [CrossRef] [PubMed]
- Gaffin, J.; Phipatanakul, W. The role of indoor allergens in the development of asthma. Curr. Opin. Allergy Clin. Immunol. 2009, 9, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Haverinen-Shaughnessy, U. Prevalence of dampness and mold in European housing stock. J. Expo. Sci. Environ. Epidemiol. 2012, 22, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Weschler, C.J.; Nazaroffc, W.W. Semivolatile organic compounds in indoor environments. Atmos. Environ. 2008, 42, 9018–9040. [Google Scholar] [CrossRef]
- Arundel, A.V.; Sterling, E.M.; Biggin, J.H.; Sterling, T.D. Indirect health effects of relative humidity in indoor environments. Environ. Health Perspect. 1986, 65, 351. [Google Scholar] [PubMed]
- Sharpe, R.A.; Thornton, C.R.; Tyrrell, J.; Nikolaou, V.; Osborne, N.J. Variable risk of atopic disease due to indoor fungal exposure in NHANES 2005–2006. Clin. Exp. Allergy 2015, 45, 1566–1578. [Google Scholar] [CrossRef] [PubMed]
- Strachan, D.P. Hay fever, hygiene, and household size. BMJ 1989, 299, 1259–1260. [Google Scholar] [CrossRef] [PubMed]
- Heederik, D.; Von Mutius, E. Does diversity of environmental microbial exposure matter for the occurrence of allergy and asthma? J. Allergy Clin. Immunol. 2012, 130, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Ehrenstein, V.; Mutius, V.; Illi, S.; Baumann, L.; Böhm, O.; Kries, V. Reduced risk of hay fever and asthma among children of farmers. Clin. Exp. Allergy 2000, 30, 187–193. [Google Scholar] [CrossRef]
- Von Mutius, E.; Radon, K. Living on a Farm: Impact on Asthma Induction and Clinical Course. Immunol. Allergy Clin. N. Am. 2008, 28, 631–647. [Google Scholar] [CrossRef] [PubMed]
- Braun-Fahrlander, C.H.; Gassner, M.; Sennhauser, F.H.; Wuthrich, B.; Scarpol-Team. Lower Risk of Allergic Sensitization and Hay Fever in Farmers’ Children in Switzerland: T 114. Epidemiology 1996, 7, S47. [Google Scholar] [CrossRef]
- Nehr, S.; Hosen, E.; Tanabe, S.I. Emerging developments in the standardized chemical characterization of indoor air quality. Environ. Int. 2017, 98, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Liddell, C.; Morris, C. Fuel poverty and human health: A review of recent evidence. Energy Policy 2010, 38, 2987–2997. [Google Scholar] [CrossRef]
- Healy, J. Excess winter mortality in Europe: A cross country analysis identifying key risk factors. J. Epidemiol. Community Health 2003, 57, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Bouzarovski, S.; Tirado Herrero, S. The energy divide: Integrating energy transitions, regional inequalities and poverty trends in the European Union. Eur. Urban Reg. Stud. 2017, 24, 69–86. [Google Scholar] [CrossRef] [PubMed]
- Thomson, H.; Snell, C.; Bouzarovski, S. Health, Well-Being and Energy Poverty in Europe: A Comparative Study of 32 European Countries. Int. J. Environ. Res. Public Health 2017, 14, 584. [Google Scholar] [CrossRef] [PubMed]
- Tod, A.M.; Lusambili, A.; Homer, C.; Abbott, J.; Cooke, J.M.; Stocks, A.J.; Mcdaid, K.A. Understanding factors influencing vulnerable older people keeping warm and well in winter: A qualitative study using social marketing techniques. BMJ Open 2012, 2, e000922. [Google Scholar] [CrossRef] [PubMed]
- Tanner, L.M.; Moffatt, S.; Milne, E.M.; Mills, S.D.; White, M. Socioeconomic and behavioural risk factors for adverse winter health and social outcomes in economically developed countries: A systematic review of quantitative observational studies. J. Epidemiol. Community Health 2013, 67, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- De Vries, R.; Blane, D. Fuel poverty and the health of older people: The role of local climate. J. Public Health 2013, 35, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Barnes, C.S.; Alexis, N.E.; Bernstein, J.A.; Cohn, J.R.; Demain, J.G.; Horner, E.; Levetin, E.; Nel, A.; Phipatanakul, W. Climate Change and Our Environment: The Effect on Respiratory and Allergic Disease. J. Allergy Clin. Immunol. Pract. 2013, 1, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, P.; Pattenden, S.; Armstrong, B.; Fletcher, A.; Kovats, R.S.; Mangtani, P.; Mcmichael, A.J. Vulnerability to winter mortality in elderly people in Britain: Population based study. BMJ 2004, 329, 647. [Google Scholar] [CrossRef] [PubMed]
- Bundle, N.; O’connell, E.; O’connor, N.; Bone, A. A public health needs assessment for domestic indoor overheating. Public Health 2018, 161, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Bone, A.; Murray, V.; Myers, I.; Dengel, A.; Crump, D. Will drivers for home energy efficiency harm occupant health? Perspect. Public Health 2010, 130, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Vandentorren, S.; Bretin, P.; Zeghnoun, A.; Mandereau-Bruno, L.; Croisier, A.; Cochet, C.; Riberon, J.; Siberan, I.; Declercq, B.; Ledrans, M. August 2003 heat wave in France: Risk factors for death of elderly people living at home. Eur. J. Public Health 2006, 16, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Kovats, R.S.; Kristie, L.E. Heatwaves and public health in Europe. Eur. J. Public Health 2006, 16, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Stansfeld, S.; Clark, C. Health Effects of Noise Exposure in Children. Curr. Environ. Health Rep. 2015, 2, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Hammer, M.S.; Swinburn, T.K.; Neitzel, R.L. Environmental Noise Pollution in the United States: Developing an Effective Public Health Response. Environ. Health Perspect. 2014, 122, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Vienneau, D.; Perez, L.; Schindler, C.; Lieb, C.; Sommer, H.; Probst-Hensch, N.; Kunzli, N.; Roosli, M. Years of life lost and morbidity cases attributable to transportation noise and air pollution: A comparative health risk assessment for Switzerland in 2010. Int. J. Hyg. Environ. Health 2015, 218, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Vienneau, D.; Schindler, C.; Perez, L.; Probst-Hensch, N.; Roosli, M. The relationship between transportation noise exposure and ischemic heart disease: A meta-analysis. Environ. Res 2015, 138, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Harding, A.-H.; Frost, G.; Tan, E.; Tsuchiya, A.; Mason, H. The cost of hypertension-related ill-health attributable to environmental noise. Noise Health 2013, 15, 437–445. [Google Scholar] [CrossRef] [PubMed]
- WHO. Burden of Disease from Environmental Noise: Quantification of Healthy Life Years Lost in Europe. Bonn: World Health Organisation 2011. Available online: http://www.euro.who.int/__data/assets/pdf_file/0008/136466/e94888.pdf?ua=1 (accessed on 11 December 2016).
- Fietze, I.; Barthe, C.; Holzl, M.; Glos, M.; Zimmermann, S.; Bauer-Diefenbach, R.; Penzel, T. The effect of room acoustics on the sleep quality of healthy sleepers. Noise Health 2016, 18, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Hume, K.I.; Brink, M.; Basner, M. Effects of environmental noise on sleep. Noise Health 2012, 14, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Basner, M.; Brink, M.; Bristow, A.; De Kluizenaar, Y.; Finegold, L.; Hong, J.; Janssen, S.A.; Klaeboe, R.; Leroux, T.; Liebl, A.; et al. ICBEN review of research on the biological effects of noise 2011–2014. Noise Health 2015, 17, 57–82. [Google Scholar] [CrossRef] [PubMed]
- Vogel, I.; Van De Looij-Jansen, P.M.; Mieloo, C.L.; Burdorf, A.; De Waart, F. Risky music listening, permanent tinnitus and depression, anxiety, thoughts about suicide and adverse general health. PLoS ONE 2014, 9, e98912. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, M.M.; Jerrett, M.; Deluca, P.; Finkelstein, N.; Verma, D.K.; Chapman, K.; Sears, M.R. Relation between income, air pollution and mortality: A cohort study. Can. Med Assoc. J. 2003, 169, 397–402. [Google Scholar]
- WHO (World Health Organisation). Housing and Health; World Health Organisation: Geneva, Switzerland, 2010. [Google Scholar]
- Environmental Protection Agency. Green Building Standards. 2017. Available online: https://www.epa.gov/smartgrowth/green-building-standards (accessed on 1 October 2017).
- Legislation. The Housing Act: New System for Assessing Housing Conditions and Enforcing Housing Standards. 2004. Available online: http://www.legislation.gov.uk/ukpga/2004/34/part/1 (accessed on 30 September 2017).
- UK Office of the Deputy Prime Minister. Housing Health and Safety Rating System: Enforcement Guidance for the Housing Act. 2006. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/7853/safetyratingsystem.pdf (accessed on 30 September 2017).
- National Center for Healthy Housing. National Healthy Housing Standard. 2014. Available online: http://www.nchh.org/Policy/NationalHealthyHousingStandard.aspx (accessed on 28 October 2017).
- Jacobs, D.E.; Wilson, J.; Dixon, S.L.; Smith, J.; Evens, A. The Relationship of Housing and Population Health: A 30-Year Retrospective Analysis. Environ. Health Persepct. 2009, 117, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Healthy Housing. Housing, Heating and Health Study. 2017. Available online: http://www.healthyhousing.org.nz/research/past-research/housing-heating-and-health-study/ (accessed on 28 October 2017).
- Ellaway, A.; Macdonald, L.; Kearns, A. Are housing tenure and car access still associated with health? A repeat cross-sectional study of UK adults over a 13-year period. BMJ Open 2016, 6, e012268. [Google Scholar] [CrossRef] [PubMed]
- Thomson, H.; Thomas, S.; Sellstrom, E.; Petticrew, M. Housing Improvements for Health and Associated Socio-economic Outcomes Cochrane Database of Systematic Reviews; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Gurran, N.; Phibbs, P. Housing supply and urban planning reform: The recent Australian experience, 2003–2012. Int. J. Hous. Policy 2013, 13, 381–407. [Google Scholar] [CrossRef]
- Ball, M. Planning delay and the responsiveness of English housing supply. Urban Stud. 2011, 48, 349–362. [Google Scholar] [CrossRef] [PubMed]
- Caldera, A.; Johansson, Å. The price responsiveness of housing supply in OECD countries. J. Hous. Econ. 2013, 22, 231–249. [Google Scholar] [CrossRef]
- Gurran, N.; Whitehead, C. Planning and Affordable Housing in Australia and the UK: A Comparative Perspective. Hous. Stud. 2011, 26, 1193–1214. [Google Scholar] [CrossRef]
- Van Den Nouwelant, R.; Davison, G.; Gurran, N.; Pinnegar, S.; Randolph, B. Delivering affordable housing through the planning system in urban renewal contexts: Converging government roles in Queensland, South Australia and New South Wales. Aust. Plan. 2015, 52, 77–89. [Google Scholar] [CrossRef]
- Moon, C.-G.; Stotsky, J.G. The effect of rent control on housing quality change: A longitudinal analysis. J. Political Econ. 1993, 101, 1114–1148. [Google Scholar] [CrossRef]
- Cairney, J.; Boyle, M.H. Home ownership, mortgages and psychological distress. Hous. Stud. 2004, 19, 161–174. [Google Scholar] [CrossRef]
- Sodini, P.; Van Nieuwerburgh, S.; Vestman, R.; Von Lilienfeld-Toal, U. Identifying the Benefits from Home Ownership: A Swedish Experiment; National Bureau of Economic Research: Paris, France, 2016. [Google Scholar]
- Hurst, E.; Stafford, F. Home is where the equity is: Mortgage refinancing and household consumption. J. Money Credit Bank. 2004, 36, 985–1014. [Google Scholar] [CrossRef]
- PHE (Public Health England). Commissioning Cost-Effective Services for Promotion of Mental Health and Wellbeing and Prevention of Mental Ill-Health; Public Health England: London, UK, 2017.
- Wallace, A. Homeowners and Poverty: A Literature Review. In A Report for the Joseph Rowntree Foundation; CHP: New York, NY, USA, 2016. [Google Scholar]
- Pollack, C.; Von Dem, K.O.; Siegrist, J. Housing and health in Germany. J. Epidemiol. Community Health 2004, 58, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, D. The fall and rise of the private rented sector in England. Built Environ. 2015, 41, 258–270. [Google Scholar] [CrossRef]
- Fenelon, A.; Mayne, P.; Simon, A.E.; Rossen, L.M.; Helms, V.; Lloyd, P.; Sperling, J.; Steffen, B.L. Housing Assistance Programs and Adult Health in the United States. Am. J. Public Health 2017, 107, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Bevan, M. Retirement lifestyles in a niche housing market: Park-home living in England. Ageing Soc. 2010, 30, 965–985. [Google Scholar] [CrossRef]
- Bevan, M. Living in Non-permanent Accommodation in England: Liminal Experiences of Home. Hous. Stud. 2011, 26, 541–554. [Google Scholar] [CrossRef]
- Busch-Geertsema, V.; Sahlin, I. The role of hostels and temporary accommodation. Eur. J. Homelessness 2007, 1, 67–93. [Google Scholar]
- Please, N. At What Cost? An Estimation of the Financial Costs of Single Homelessness in UK; Crisis: London, UK, 2015. [Google Scholar]
- Bassuk, E.L.; Richard, M.K.; Tsertsvadze, A. The prevalence of mental illness in homeless children: A systematic review and meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 86–96.e2. [Google Scholar] [CrossRef] [PubMed]
- White, B.M.; Logan, A.; Magwood, G.S. Access to Diabetes Care for Populations Experiencing Homelessness: An Integrated Review. Curr. Diab. Rep. 2016, 16, 112. [Google Scholar] [CrossRef] [PubMed]
- CRISIS. Homelessness: A silent killer. In A Research Briefing on Mortality Amongst Homeless People; CRISIS: London, UK, 2011. [Google Scholar]
- Montgomery, A.E.; Szymkowiak, D.; Marcus, J.; Howard, P.; Culhane, D.P. Homelessness, Unsheltered Status, and Risk Factors for Mortality: Findings From the 100,000 Homes Campaign. Public Health Rep. 2016, 131, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Van Hooff, M.L. The daily commute from work to home: Examining employees’ experiences in relation to their recovery status. Stress Health 2015, 31, 124–137. [Google Scholar] [CrossRef] [PubMed]
- Pierse, N.; Carter, K.; Bierre, S.; Law, D.; Howden-Chapman, P. Examining the role of tenure, household crowding and housing affordability on psychological distress, using longitudinal data. J. Epidemiol. Community Health 2016, 70, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Anderson, W.; White, V.; Finney, A. Coping with low incomes and cold homes. Energy Policy 2012, 49, 40–52. [Google Scholar] [CrossRef]
- Heath, H. Housing Demand and Need (England), SN06921 ed.; Library House of Commons: London, UK, 2014. [Google Scholar]
- The National Archives. Definition of Overcrowding. 2017. Available online: https://www.legislation.gov.uk/ukpga/1985/68/part/X/crossheading/definition-of-overcrowding (accessed on 29 October 2017).
- Tunstall, B. Relative housing space inequality in England and Wales, and its recent rapid resurgence. Int. J. Hous. Policy 2015, 15, 105–126. [Google Scholar] [CrossRef]
- Bashir, M.E.; Louie, S.; Shi, H.N.; Nagler-Anderson, C. Toll-Like Receptor 4 Signaling by Intestinal Microbes Influences Susceptibility to Food Allergy. J. Immunol. 2004, 172, 6978–6987. [Google Scholar] [CrossRef] [PubMed]
- Lopoo, L.M.; London, A.S. Household Crowding During Childhood and Long-Term Education Outcomes. Demography 2016, 53, 699–721. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.; Davies, M.; Mavrogianni, A.; Shrubsole, C.; Hamilton, I.; Das, P.; Jones, B.; Oikonomou, E.; Biddulph, P. Mapping indoor overheating and air pollution risk modification across Great Britain: A modelling study. Build. Environ. 2016, 99, 1–12. [Google Scholar] [CrossRef]
- Pickett, K.E.; Pearl, M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. J. Epidemiol. Community Health 2001, 55, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Scottish Government. Good Places Better Health for Scotland’s Children. 2011. Available online: https://www.gov.scot/Resource/0039/00398236.pdf (accessed on 16 September 2018).
- Malambo, P.; Kengne, A.P.; De Villiers, A.; Lambert, E.V.; Puoane, T. Built Environment, Selected Risk Factors and Major Cardiovascular Disease Outcomes: A Systematic Review. PLoS ONE 2016, 11, e0166846. [Google Scholar] [CrossRef] [PubMed]
- Joss, S. Eco-cities: The mainstreaming of urban sustainability–key characteristics and driving factors. Int. J. Sustain. Dev. Plan. 2011, 6, 268–285. [Google Scholar] [CrossRef]
- Local Government Association. Building the Foundations: Tackling Obesity through Planning and Development. 2016. Available online: http://www.local.gov.uk/publications/-/journal_content/56/10180/7716564/PUBLICATION (accessed on 5 January 2017).
- Town and Country Planning Association. Planning Healthy Weight Environments—A TCPA Reuniting Health with Planning Project. 2014. Available online: File:///C:/Users/Richard/Downloads/PHWE_Report_Final.pdf (accessed on 5 January 17).
- PHE (Public Health England). Local Action on Health Inequalities: Understanding the Economics of Investments in the Social Determinants of Health; Public Health England: London, UK, 2014. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/356051/Briefing9_Economics_of_investments_health_inequalities.pdf (accessed on 18 January 2017).
- Lorenc, T.; Petticrew, M.; Whitehead, M.; Neary, D.; Clayton, S.; Wright, K.; Thomson, H.; Cummins, S.; Sowden, A.; Renton, A. Crime, fear of crime and mental health: Synthesis of theory and systematic reviews of interventions and qualitative evidence. Health Place 2012, 18, 757–765. [Google Scholar] [CrossRef] [PubMed]
- Shelter. The Living Home Standard; Shelter. 2016. Available online: http://www.shelter.org.uk/livinghomestandard (accessed on 6 December 2017).
- Kondo, M.C.; South, E.C.; Branas, C.C. Nature-Based Strategies for Improving Urban Health and Safety. J. Urban Health 2015, 92, 800–814. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, B.; White, M.; Stahl-Timmins, W.; Depledge, M. Does living by the coast improve health and wellbeing? Health Place 2012, 18, 1198–1201. [Google Scholar] [CrossRef] [PubMed]
- White, M.; Elliott, L.; Taylor, T.; Wheeler, B.; Spencer, A.; Bone, A.; Depledge, M.; Fleming, L. Recreational physical activity in natural environments and implications for health: A population based cross-sectional study in England. Prev. Med. 2016, 91, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.; Popham, F. Effect of exposure to natural environment on health inequalities: An observational population study. Lancet 2008, 372, 1655–1660. [Google Scholar] [CrossRef]
- Mitchell, R.; Popham, F. Greenspace, urbanity and health: Relationships in England. J. Epidemiol. Community Health 2007, 61, 681–683. [Google Scholar] [CrossRef] [PubMed]
- PHE (Public Health England). Improving Access to Green Space; University College of London: London, UK, 2014. Available online: http://www.instituteofhealthequity.org/projects/improving-access-to-green-spaces (accessed on 12 January 2017).
- Gee, G.C.; Payne-Sturges, D.C. Environmental health disparities: A framework integrating psychosocial and environmental concepts. Environ. Health Perspect. 2004, 112, 1645–1653. [Google Scholar] [CrossRef] [PubMed]
- Ormandy, D. Housing and Health in Europe: The WHO LARES Project; Routledge: London, UK, 2009. [Google Scholar]
- Scottish Government. Good Places Better Health: A New Approach to Environment and Health in Scotland—Implementation Plan. 2008. Available online: https://www.noexperiencenecessarybook.com/1w0vv/good-places-better-health-a-new-approach-to-the-environment-and-health-in-scotland-implementation-plan.html (accessed on 7 June 2017).
- Willand, N.; Ridley, I.; Maller, C. Towards explaining the health impacts of residential energy efficiency interventions—A realist review. Part 1: Pathways. Soc. Sci. Med. 2015, 133, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Grey CN, B.; Schmieder-Gaite, T.; Jiang, S.; Nascimento, C.; Poortinga, W. Cold homes, fuel poverty and energy efficiency improvements: A longitudinal focus group approach. Indoor Built Environ. 2017, 26, 902–913. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, I.; Milner, J.; Chalabi, Z.; Das, P.; Jones, B.; Shrubsole, C.; Davies, M.; Wilkinson, P. Health effects of home energy efficiency interventions in England: A modelling study. BMJ Open 2015, 5, e007298. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.A.; Locoq, K.; Thornton, C.R.; Osborne, N.J. Identifying risk factors for allergenic fungal exposure in energy efficient homes by using highly specific monoclonal antibodies. Environ. Res. 2016, 144, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Spertini, F.; Berney, M.; Foradini, F.; Roulet, C.A. Major mite allergen Der f 1 concentration is reduced in buildings with improved energy performance. Allergy 2010, 65, 623–629. [Google Scholar] [CrossRef] [PubMed]
- NICE (National Institute for Health and Care Excellence). Excess Winter Deaths and Illness and the Health Risks Associated with Cold Homes. Available online: https://www.nice.org.uk/guidance/ng6 (accessed on 25 May 2016).
- Thomson, H.; Thomas, S.; Sellstrom, E.; Petticrew, M. The Health Impacts of Housing Improvement: A Systematic Review of Intervention Studies From 1887 to 2007. Am. J. Public Health 2009, 99, S6816–S6892. [Google Scholar] [CrossRef] [PubMed]
- Maidment, C.D.; Jones, C.R.; Webb, T.L.; Hathway, E.A.; Gilbertson, J.M. The impact of household energy efficiency measures on health: A meta-analysis. Energy Policy 2014, 65, 583–593. [Google Scholar] [CrossRef]
- Gibson, M.; Petticrew, M.; Bambra, C.; Sowden, A.J.; Wright, K.E.; Whitehead, M. Housing and health inequalities: A synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health Place 2011, 17, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Curl, A.; Kearns, A.; Mason, P.; Egan, M.; Tannahill, C.; Ellaway, A. Physical and mental health outcomes following housing improvements: Evidence from the GoWell study. J. Epidemiol. Community Health 2015, 69, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Keall, M.D.; Pierse, N.; Howden-Chapman, P.; Cunningham, C.; Cunningham, M.; Guria, J.; Baker, M.G. Home modifications to reduce injuries from falls in the Home Injury Prevention Intervention (HIPI) study: A cluster-randomised controlled trial. Lancet 2015, 385, 231–238. [Google Scholar] [CrossRef]
- Preston, L.C.; Cantell, A.; Paisley, S.; Peasgood, T.; Brazier, J. Housing and Wellbeing: A Rapid Scoping Review of Reviews on the Evidence on Housing and Its Relationship with Wellbeing; School for Health and Related Research (ScHARR), University of Sheffield: Sheffield, UK, 2017. [Google Scholar]
- Welsh Government. The Fuel Poverty Data Linking Project Findings Report No.1: Initial Findings on the Impact on Health of the Warm Homes Nest Scheme 2017. Available online: https://gov.wales/docs/caecd/research/2017/170404-fuel-poverty-data-linking-project-findings-report-1-en.pdf (accessed on 5 July 2018).
- Rodgers, S.E.; Bailey, R.; Johnson, R.; Poortinga, W.; Smith, R.; Berridge, D.; Anderson, P.; Phillips, C.; Lannon, S.; Jones, N. Health Impact, and Economic Value, of Meeting Housing Quality Standards: A Retrospective Longitudinal Data Linkage Study; Public Health Research: London, UK, 2018. [Google Scholar]
- Shrubsole, C.; Macmillan, A.; Davies, M.; May, N. 100 Unintended consequences of policies to improve the energy efficiency of the UK housing stock. Indoor Built Environ. 2014, 23, 340–352. [Google Scholar] [CrossRef]
- Richardson, G.; Barton, A.; Basham, M.; Foy, C.; Eick, S.A.; Somerville, M. The Watcombe housing study: The short-term effect of improving housing conditions on the indoor environment. Sci. Total. Environ. 2005, 361, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.A.; Machray, K.E.; Fleming, L.E.; Taylor, T.; Henley, W.; Chenore, T.; Hutchcroft, I.; Lemon, S.; Merrifield, R.; Heeler, B.W. Modelling the Impact of Fuel Poverty and Energy Efficiency on Health; Eaga Charitable Trust: Kendal, UK, 2017. [Google Scholar]
- Laverge, J.; Janssens, A. Heat recovery ventilation operation traded off against natural and simple exhaust ventilation in Europe by primary energy factor, carbon dioxide emission, household consumer price and energy. Energy Build. 2012, 50, 315–323. [Google Scholar] [CrossRef]
- Colton, M.D.; Laurent JG, C.; Macnaughton, P.; Kane, J.; Bennett-Fripp, M.; Spengler, J.; Adamkiewicz, G. Health Benefits of Green Public Housing: Associations With Asthma Morbidity and Building-Related Symptoms. Am. J. Public Health 2015, 105, 2482–2489. [Google Scholar] [CrossRef] [PubMed]
- Breysse, J.; Jacobs, D.E.; Weber, W.; Dixon, S.; Kawecki, C.; Aceti, S.; Lopez, J. Health outcomes and green renovation of affordable housing. Public Health Rep. 2011, 126, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Howden-Chapman, P.; Pierse, N.; Nicholls, S.; Gillespie-Bennett, J.; Viggers, H.; Cunningham, M.; Phipps, R.; Boulic, M.; Fjallstrom, P.; Free, S.; et al. Effects of improved home heating on asthma in community dwelling children: Randomised controlled trial. BMJ 2008, 337, a1411. [Google Scholar] [CrossRef] [PubMed]
- Howden-Chapman, P.; Matheson, A.; Crane, J.; Viggers, H.; Cunningham, M.; Blakely, T.; Cunningham, C.; Woodward, A.; Saville-Smith, K.; O’dea, D.; et al. Effect of insulating existing houses on health inequality: Cluster randomised study in the community. BMJ 2007, 334, 460. [Google Scholar] [CrossRef] [PubMed]
- Howden-Chapman, P.; Crane, J.; Chapman, R.; Fougere, G. Improving health and energy efficiency through community-based housing interventions. Int. J. Public Health 2011, 56, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Francisco, P.W.; Jacobs, D.E.; Targos, L.; Dixon, S.L.; Breysse, J.; Rose, W.; Cali, S. Ventilation, indoor air quality, and health in homes undergoing weatherization. Indoor Air 2017, 27, 463–477. [Google Scholar] [CrossRef] [PubMed]
- Mc Conalogue, D.; Kierans, C.; Moran, A. The hidden practices and experiences of healthcare practitioners dealing with fuel poverty. J. Public Health 2016, 38, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.; Thornton, C.; Osborne, N. Energy Efficiency, Indoor Fungi, and Asthma in a Population Residing in Social Housing; University of Exeter Medical School: Exeter, UK, 2014. [Google Scholar]
- Fenwick, E.; Macdonald, C.; Thomson, H. Economic analysis of the health impacts of housing improvement studies: A systematic review. J. Epidemiol. Community Health 2013, 67, 835–845. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.; Jacobs, D.E.; Ashley, P.J.; Baeder, A.; Chew, G.L.; Dearborn, D.; Hynes, H.P.; Miller, J.D.; Morley, R.; Rabito, F.; et al. Housing Interventions and Control of Asthma-Related Indoor Biologic Agents: A Review of the Evidence. J. Public Health Manag. Pract. 2010, 16, 112. [Google Scholar] [CrossRef] [PubMed]
- Milner, J.; Shrubsole, C.; Das, P.; Jones, B.; Ridley, I.; Chalabi, Z.; Hamilton, I.; Armstrong, B.; Davies, M.; Wilkinson, P. Home energy efficiency and radon related risk of lung cancer: Modelling study. BMJ 2014, 348, f7493. [Google Scholar] [CrossRef] [PubMed]
- Nelson, G.; Aubry, T.; Lafrance, A. A review of the literature on the effectiveness of housing and support, assertive community treatment, and intensive case management interventions for persons with mental illness who have been homeless. Am. J. Orthopsychiatry 2007, 77, 350–361. [Google Scholar] [CrossRef] [PubMed]
- Blackman, T.; Harvey, J.; Lawrence, M.; Simon, A. Neighbourhood renewal and health: Evidence from a local case study. Health Place 2001, 7, 93–103. [Google Scholar] [CrossRef]
- Durand, C.P.; Andalib, M.; Dunton, G.F.; Wolch, J.; Pentz, M.A. A systematic review of built environment factors related to physical activity and obesity risk: Implications for smart growth urban planning. Obes. Rev. 2011, 12, e173–e182. [Google Scholar] [CrossRef] [PubMed]
- Jeste, D.V.; Blazer, D.G.; Buckwalter, K.C., 2nd; Cassidy, K.K.; Fishman, L.; Gwyther, L.P.; Levin, S.M.; Phillipson, C.; Rao, R.R.; Schmeding, E.; et al. Age-Friendly Communities Initiative: Public Health Approach to Promoting Successful Aging. Am. J. Geriatr. Psychiatry 2016, 24, 1158–1170. [Google Scholar] [CrossRef] [PubMed]
- Bunn, F.; Burn, A.M.; Goodman, C.; Robinson, L.; Rait, G.; Norton, S.; Bennett, H.; Poole, M.; Schoeman, J.; Brayne, C.; Health Services and Delivery Research. Comorbidity and Dementia: A Mixed-Method Study on Improving Health Care for People with Dementia (CoDem); NIHR: Southampton, UK, 2016. [Google Scholar]
- Evans, S.C.; Bray, J.; Robertson, G. Best practice for providing social care and support to people living with concurrent sight loss and dementia: Professional perspectives. Work. Older People 2016, 20, 86–93. [Google Scholar] [CrossRef]
- Komro, K.A.; Tobler, A.L.; Delisle, A.L.; O’mara, R.J.; Wagenaar, A.C. Beyond the clinic: Improving child health through evidence-based community development. BMC Pediatr. 2013, 13, 172. [Google Scholar] [CrossRef] [PubMed]
- Well London. Phase 1 Research and Evaluation. 2016. Available online: http://www.welllondon.org.uk/1621/phase-1.html (accessed on 18 January 2017).
- Wall, M.; Hayes, R.; Moore, D.; Petticrew, M.; Clow, A.; Schmidt, E.; Draper, A.; Lock, K.; Lynch, R.; Renton, A. Evaluation of community level interventions to address social and structural determinants of health: A cluster randomised controlled trial. BMC Public Health 2009, 9, 207. [Google Scholar] [CrossRef] [PubMed]
- Phillips, G.; Bottomley, C.; Schmidt, E.; Tobi, P.; Lais, S.; Yu, G.; Lynch, R.; Lock, K.; Draper, A.; Moore, D.; et al. Well London Phase-1: Results among adults of a cluster-randomised trial of a community engagement approach to improving health behaviours and mental well-being in deprived inner-city neighbourhoods. J. Epidemiol. Community Health 2014, 68, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Hassen, N.; Kaufman, P. Examining the role of urban street design in enhancing community engagement: A literature review. Health Place 2016, 41, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Lorenc, T.; Clayton, S.; Neary, D.; Whitehead, M.; Petticrew, M.; Thomson, H.; Cummins, S.; Sowden, A.; Renton, A. Crime, fear of crime, environment, and mental health and wellbeing: Mapping review of theories and causal pathways. Health Place 2012, 18, 757–765. [Google Scholar] [CrossRef] [PubMed]
- Derges, J.; Clow, A.; Lynch, R.; Jain, S.; Phillips, G.; Petticrew, M.; Renton, A.; Draper, A. ‘Well London’and the benefits of participation: Results of a qualitative study nested in a cluster randomised trial. BMJ Open 2014, 4, e003596. [Google Scholar] [CrossRef] [PubMed]
- Zapata, M.A.R.; Navarro, Y.C.J. Impact of area regeneration policies: Performing integral interventions, changing opportunity structures and reducing health inequalities. J. Epidemiol. Community Health 2016, 71, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Kok, A.A.L.; Aartsen, M.J.; Deeg, D.J.H.; Huisman, M. Socioeconomic inequalities in a 16-year longitudinal measurement of successful ageing. J. Epidemiol.Community Health 2016, 70, 1106–1113. [Google Scholar] [CrossRef] [PubMed]
- Scott, F.L.; Jones, C.R.; Webb, T.L. What do people living in deprived communities in the UK think about household energy efficiency interventions? Energy Policy 2014, 66, 335–349. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Dimitroulopoulou, C.; Thornes, J.; Lai, K.M.; Taylor, J.; Myers, I.; Heaviside, C.; Mavrogianni, A.; Shrubsole, C.; Chalabi, Z.; et al. Impact of climate change on the domestic indoor environment and associated health risks in the UK. Environ. Int. 2015, 85, 299–313. [Google Scholar] [CrossRef] [PubMed]
- D’amato, G.; Holgate, S.T.; Pawankar, R.; Ledford, D.K.; Cecchi, L.; Al-Ahmad, M.; Al-Enezi, F.; Al-Muhsen, S.; Ansotegui, I.; Baena-Cagnani, C.E.; et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J. 2015, 8, 25. [Google Scholar] [CrossRef] [PubMed]
- HPA. Health Effects of Climate Change in the UK. 2012. Available online: http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317135969235 (accessed on 26 September 2012).
- PHE (Public Health England). A Guide to Community-Centred Approaches for Health and Wellbeing; Public Health England: London, UK, 2015. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/417515/A_guide_to_community-centred_approaches_for_health_and_wellbeing__full_report_.pdf (accessed on 7 June 2017).
- Archer, P.; Murie, A.; Turkington, R.; Watson, C. Good Housing Better Health; Housing and Communities Research Group: Birmingham, UK, 2016. [Google Scholar]
- Nhs England. Integrated Care Systems. 2018. Available online: https://www.england.nhs.uk/integratedcare/integrated-care-systems/ (accessed on 27 July 2018).
- PHE (Public Health England). Spatial Planning for Health: An Evidence Resource for Planning and Designing Healthier Places; Public Health England: London, UK, 2017. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/625568/Spatial_planning_for_health_an_evidence_resource.pdf (accessed on 30 September 2017).
- Buck, D.; Gregory, S. Housing and Health; The King’s Fund: London, UK, 2018. [Google Scholar]
- PHE. Improving Health and Care through the Home: MoU. 2018. Available online: https://www.gov.uk/government/publications/improving-health-and-care-through-the-home-mou (accessed on 27 July 2018).
- Orton, L.; Lloyd-Williams, F.; Taylor-Robinson, D.; O’flaherty, M.; Capewell, S. The use of research evidence in public health decision making processes: Systematic review. PLoS ONE 2011, 6, e21704. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharpe, R.A.; Taylor, T.; Fleming, L.E.; Morrissey, K.; Morris, G.; Wigglesworth, R. Making the Case for “Whole System” Approaches: Integrating Public Health and Housing. Int. J. Environ. Res. Public Health 2018, 15, 2345. https://doi.org/10.3390/ijerph15112345
Sharpe RA, Taylor T, Fleming LE, Morrissey K, Morris G, Wigglesworth R. Making the Case for “Whole System” Approaches: Integrating Public Health and Housing. International Journal of Environmental Research and Public Health. 2018; 15(11):2345. https://doi.org/10.3390/ijerph15112345
Chicago/Turabian StyleSharpe, Richard A., Tim Taylor, Lora E. Fleming, Karyn Morrissey, George Morris, and Rachel Wigglesworth. 2018. "Making the Case for “Whole System” Approaches: Integrating Public Health and Housing" International Journal of Environmental Research and Public Health 15, no. 11: 2345. https://doi.org/10.3390/ijerph15112345
APA StyleSharpe, R. A., Taylor, T., Fleming, L. E., Morrissey, K., Morris, G., & Wigglesworth, R. (2018). Making the Case for “Whole System” Approaches: Integrating Public Health and Housing. International Journal of Environmental Research and Public Health, 15(11), 2345. https://doi.org/10.3390/ijerph15112345





