Impact of Different Estimation Methods on Obesity-Attributable Mortality Levels and Trends: The Case of The Netherlands
Abstract
1. Introduction
2. Materials and Methods
2.1. Methods for Calculating Obesity-Attributable Mortality
2.2. Selected All-Cause Approaches
2.3. Comparative Risk Assessment (CRA) Approach
2.4. Adjustment of the CRA Approach
2.5. Data Sources
2.5.1. BMI Data
2.5.2. Mortality Data
2.6. Relative Risks (RRs)
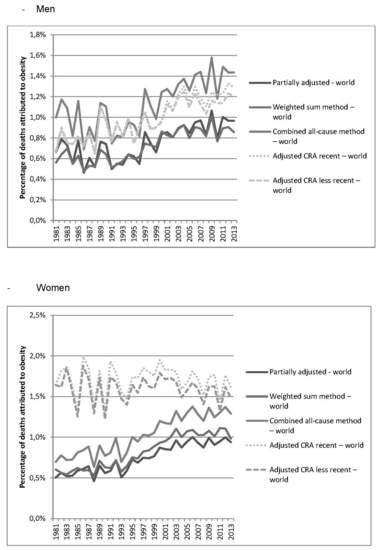
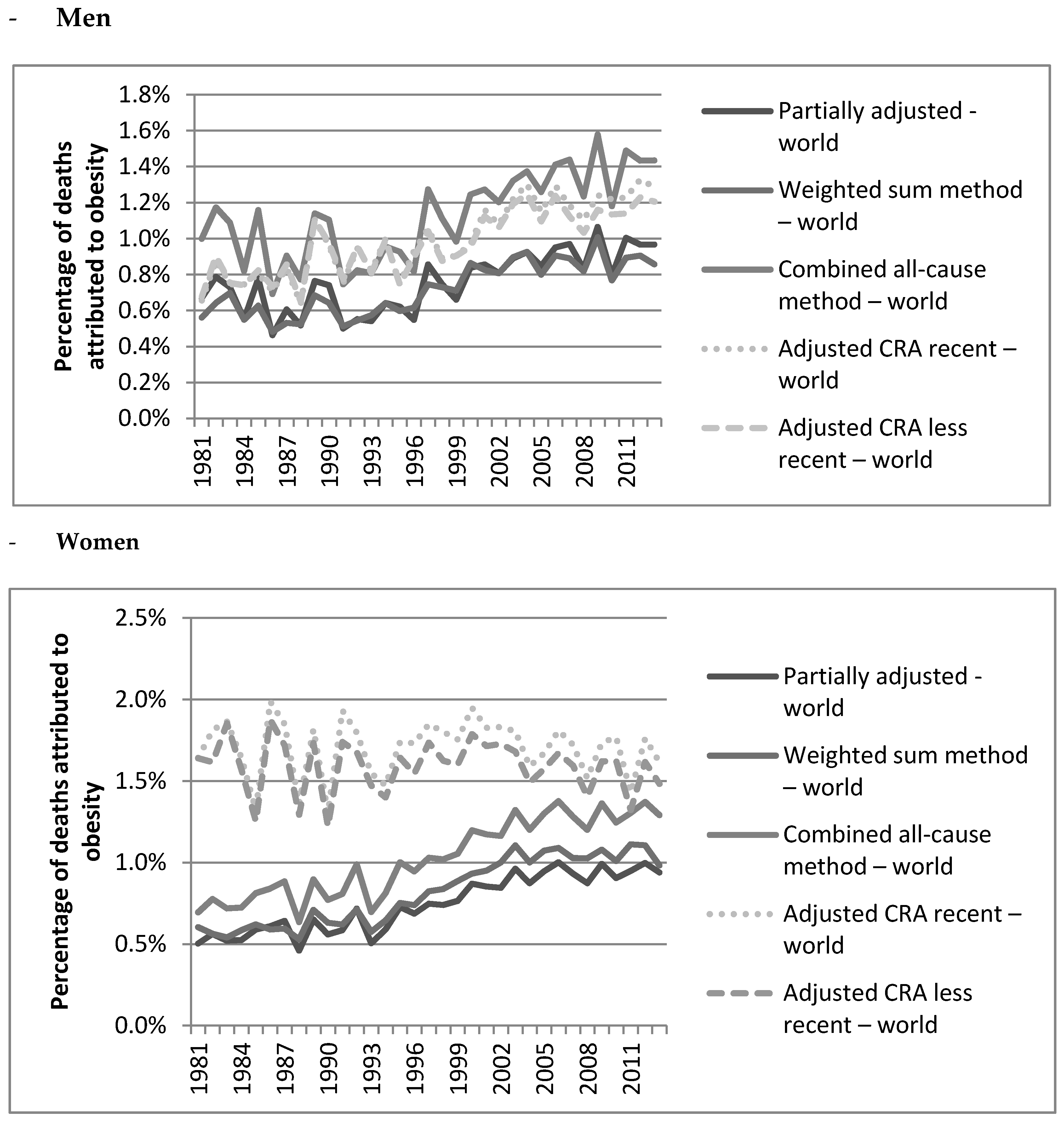
3. Results
4. Discussion
4.1. Summary of Results
4.2. Explanation of the Observed Results
4.3. Reflection on Our Approach
4.4. Reflection on the Different Methodologies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Finucane, M.M.; Stevens, G.A.; Cowan, M.J.; Danaei, G.; Lin, J.K.; Paciorek, C.J.; Singh, G.M.; Gutierrez, H.R.; Lu, Y.; Bahalim, A.N.; et al. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011, 377, 557–567. [Google Scholar] [CrossRef] [PubMed]
- WHO Obesity. Preventing and Managing the Global Epidemic. Report of a WHO Consultation (WHO Technical Report Series 894). Available online: http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ (accessed on 1 March 2016).
- Wang, Y.C.; McPherson, K.; Marsh, T.; Gortmaker, S.L.; Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011, 378, 815–825. [Google Scholar] [CrossRef]
- Berrington de Gonzalez, A.; Sweetland, S.; Spencer, E. A meta-analysis of obesity and the risk of pancreatic cancer. Br. J. Cancer 2003, 89, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Calle, E.E.; Kaaks, R. Overweight, obesity and cancer: Epidemiological evidence and proposed mechanisms. Nat. Rev. Cancer 2004, 4, 579–591. [Google Scholar] [CrossRef] [PubMed]
- Field, A.E.; Coakley, E.H.; Must, A.; Spadano, J.L.; Laird, N.; Dietz, W.H.; Rimm, E.; Colditz, G.A. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch. Intern. Med. 2001, 161, 1581–1586. [Google Scholar] [CrossRef] [PubMed]
- Preston, S.H.; Vierboom, Y.C.; Stokes, A. The role of obesity in exceptionally slow US mortality improvement. Proc. Natl. Acad. Sci. USA 2018, 115, 957–961. [Google Scholar] [CrossRef] [PubMed]
- Global BMI Mortality; Di Angelantonio, E.; Bhupathiraju, S.; Wormser, D.; Gao, P.; Kaptoge, S.; Berrington de Gonzalez, A.; Cairns, B.J.; Huxley, R.; Jackson, C.; Joshy, G.; et al. Body-mass index and all-cause mortality: Individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016, 388, 776–786. [Google Scholar] [CrossRef]
- Laaksonen, M.A.; Knekt, P.; Harkanen, T.; Virtala, E.; Oja, H. Estimation of the population attributable fraction for mortality in a cohort study using a piecewise constant hazards model. Am. J. Epidemiol. 2010, 171, 837–847. [Google Scholar] [CrossRef] [PubMed]
- Banegas, J.R.; Lopez-Garcia, E.; Gutierrez-Fisac, J.L.; Guallar-Castillon, P.; Rodriguez-Artalejo, F. A simple estimate of mortality attributable to excess weight in the European Union. Eur. J. Clin. Nutr. 2003, 57, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Allison, D.B.; Fontaine, K.R.; Manson, J.E.; Stevens, J.; VanItallie, T.B. Annual deaths attributable to obesity in the United States. JAMA 1999, 282, 1530–1538. [Google Scholar] [CrossRef] [PubMed]
- Borch, K.B.; Braaten, T.; Lund, E.; Weiderpass, E. Physical activity and mortality among Norwegian women —The Norwegian Women and Cancer Study. Clin. Epidemiol. 2011, 3, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Mokdad, A.H.; Marks, J.S.; Stroup, D.F.; Gerberding, J.L. Actual causes of death in the United States, 2000. JAMA 2004, 291, 1238–1245. [Google Scholar] [CrossRef] [PubMed]
- Rockhill, B.; Newman, B.; Weinberg, C. Use and misuse of population attributable fractions. Am. J. Public Health 1998, 88, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Graubard, B.I.; Williamson, D.F. Methods of calculating deaths attributable to obesity. Am. J. Epidemiol. 2004, 160, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Benichou, J. A review of adjusted estimators of attributable risk. Stat. Methods Med. Res. 2001, 10, 195–216. [Google Scholar] [CrossRef] [PubMed]
- Ezzati, M.; Lopez, A.D.; Rodgers, A.; Murray, C.J.L. Comparative Quantification of Health Risks: Global and Regional Burden Attributable to Selected Major Risk Factors; World Health Organisation: Geneva, Switzerland, 2004. [Google Scholar]
- Flegal, K.M.; Panagiotou, O.A.; Graubard, B.I. Estimating population attributable fractions to quantify the health burden of obesity. Ann. Epidemiol. 2015, 25, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Ardern, C.I. Overweight and obesity mortality trends in Canada, 1985–2000. Can. J. Public Health 2004, 95, 16–20. [Google Scholar] [PubMed]
- GBD 2015 Risk Factors Collaborators Global, Regional, and National Comparative Risk Assessment of 79 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks, 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [CrossRef]
- GBD 2013 Risk Factors Collaborators Global, Regional, and National Comparative Risk Assessment of 79 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks in 188 Countries, 1990–2013: A Systematic Analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [CrossRef]
- Danaei, G.; Ding, E.L.; Mozaffarian, D.; Taylor, B.; Rehm, J.; Murray, C.J.; Ezzati, M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009, 6, e1000058. [Google Scholar] [CrossRef] [PubMed]
- De Wit, L.M.; Van Straten, A.; Van Herten, M.; Penninx, B.W.; Cuijpers, P. Depression and body mass index, a u-shaped association. BMC Public Health 2009, 9. [Google Scholar] [CrossRef] [PubMed]
- Centraal Bureau voor de Statistiek. Lengte en Gewicht van Personen, Ondergewicht en Overgewicht; Vanaf 1981. Available online: http://statline.cbs.nl/ Statweb/selection/?VW=T&DM=SLNL&PA=81565NED&D1=4&D2=0&D3=a&D4=0&D5=0-34&HDR=G4&STB=G1,G3,T,G2 (accessed on 10 March 2016).
- Human Mortality Database University of California, Berkeley (USA), and Max Planck Institute for Demographic Research (Germany). Available online: http://www.mortality.org (accessed on 15 June 2016).
- WHO. WHO Mortality Database. Available online: http://www.who.int/healthinfo/mortality_data/en/ (accessed on 10 June 2016).
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z. Age-dependent decline of association between obesity and mortality: A systematic review and meta-analysis. Obes. Res. Clin. Pract. 2015, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lobstein, T.; Leach, R.J. Workpackage 7: Overweight and Obesity Report on Data Collection for Overweight and Obesity Prevalence and Related Relative Risks. 2010. Available online: https://www.dynamo-hia.eu/sites/default/files/2018-04/BMI_WP7-datareport_20100317.pdf (accessed on 15 June 2016).
- Kelly, C.; Pashayan, N.; Munisamy, S.; Powles, J.W. Mortality attributable to excess adiposity in England and Wales in 2003 and 2015: explorations with a spreadsheet implementation of the Comparative Risk Assessment methodology. Popul. Health. Metr. 2009, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Preston, S.H.; Stokes, A. Contribution of obesity to international differences in life expectancy. Am. J. Public Health 2011, 101, 2137–2143. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Hou, L.N.; Chen, W.; Chen, P.L.; Lei, C.Y.; Wei, Q.; Tan, W.L.; Zheng, S.B. Associations of dietary patterns with the risk of all-cause, CVD and stroke mortality: A meta-analysis of prospective cohort studies. Br. J. Nutr. 2015, 113, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Anderson, N.B.; Bulatao, R.A.; Cohen, B. (Eds.) Genetic Factors in Ethnic Disparities in Health. In Critical Perspectives on Racial and Ethnic Differences in Health in Late Life; National Academies Press (US): Washington, DC, USA, 2004; p. 269. [Google Scholar]
- Von Ruesten, A.; Steffen, A.; Floegel, A.; Van der, A.D.L.; Masala, G.; Tjonneland, A.; Halkjaer, J.; Palli, D.; Wareham, N.J.; Loos, R.J.; et al. Trend in obesity prevalence in European adult cohort populations during follow-up since 1996 and their predictions to 2015. PLoS ONE 2011, 6, e27455. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Janssen, F.; Kunst, A.E. ICD coding changes and discontinuities in trends in cause-specific mortality in six European countries, 1950–1999. Bull. World Health Organ. 2004, 82, 904–913. [Google Scholar]
| Adjusted CRA Less Recent | Adjusted CRA Recent | ||||
|---|---|---|---|---|---|
| Danaei et al. 2009 * | Relative Risks | GBD 2013 ** | Relative Risks | ||
| Causes of Death | Men Aged 50–54 | Women Aged 50–54 | Causes of Death | Men Aged 50–54 | Women Aged 50–54 |
| Colon and rectum cancers | 1.04 | 1.02 | Colon and rectum cancers | 1.03 | 1.01 |
| Breast cancer | - | 1.02 | Breast cancer | - | 1.02 |
| Corpus uteri cancer | - | 1.10 | Corpus uteri cancer | - | 1.10 |
| Diabetes mellitus | 1.20 | 1.20 | Diabetes mellitus | 1.21 | 1.21 |
| Hypertensive heart disease | 1.18 | 1.18 | Hypertensive heart disease | 1.18 | 1.18 |
| Ischemic heart disease | 1.09 | 1.09 | Ischemic heart disease | 1.09 | 1.09 |
| Cerebrovascular disease | 1.10 | 1.10 | Cerebrovascular disease | 1.10 | 1.10 |
| Kidney cancer | 1.05 | 1.05 | Kidney cancer | 1.04 | 1.06 |
| Pancreatic cancer | 1.01 | 1.02 | Pancreatic cancer | 1.01 | 1.02 |
| Esophageal cancer | 1.07 | 1.06 | |||
| Liver cancer | 1.05 | 1.03 | |||
| Gallbladder cancer | 1.03 | 1.06 | |||
| Leukemia | 1.02 | 1.02 | |||
| Approach | Geographical Context | Age | RR | Reference | |
|---|---|---|---|---|---|
| Men | Women | ||||
| Partially adjusted | Worldwide | All adult ages | 1.18 | Flegal et al. 2013 [27] | |
| Partially adjusted | Europe | All adult ages | 1.27 | Flegal et al. 2013 [27] | |
| Combined approach | Worldwide | All adult ages | 1.27 | 1.25 | Flegal et al. 2013 [27] |
| Weighted sum method | Europe | <50 | 1.55 | 1.5 | Lobstein & Leach 2010 [29] |
| 50–59 | 1.539 | 1.49 | |||
| 60–69 | 1.5225 | 1.475 | |||
| 70+ | 1.495 | 1.45 | |||
| Weighted sum method | Worldwide | < 35 | 1.59 | 1.60 | Wang 2015 [28] |
| 35–44 | 1.39 | 1.58 | |||
| 45–54 | 1.39 | 1.49 | |||
| 55–64 | 1.21 | 1.35 | |||
| 65–74 | 1.15 | 1.25 | |||
| 75+ | 1.11 | 1.11 | |||
| Approach | Men | Women | Men and Women |
|---|---|---|---|
| Partially adjusted – world | 0.97 | 0.94 | 1.00 |
| Partially adjusted – Europe | 1.45 | 1.37 | 1.41 |
| Weighted sum method – world | 0.86 | 0.98 | 0.92 |
| Weighted sum method – Europe | 1.88 | 1.68 | 1.78 |
| Combined all-cause method – world | 1.43 | 1.29 | 1.37 |
| Adjusted CRA, recent – world | 1.29 | 1.62 | 1.46 |
| Adjusted CRA, less recent – world | 1.21 | 1.48 | 1.35 |
| Change in OAMF (%) | 1981–1993 | 1993–2013 | 1981–2013 |
|---|---|---|---|
| Men | |||
| Partially adjusted - world | −19.1% | 78.7% | 44.5% |
| Partially adjusted – Europe | −14.8% | 73.2% | 47.5% |
| Weighted sum method – world | 2.3% | 49.3% | 52.7% |
| Weighted sum method – Europe | −13.6% | 74.4% | 50.6% |
| Combined all-cause method – world | −19.2% | 77.8% | 43.6% |
| Adjusted CRA recent – world | 25.3% | 56.4%% | 96.0% |
| Adjusted CRA less recent – world | 19.5% | 48.9% | 77.9% |
| Women | |||
| Partially adjusted - world | 0.26% | 85.9% | 86.4% |
| Partially adjusted – Europe | 31.5% | 77.1% | 133.0% |
| Weighted sum method – world | −4.8% | 70.8% | 62.6% |
| Weighted sum method – Europe | 2.1% | 79.5% | 83.3% |
| Combined all-cause method – world | 0.2% | 85.2% | 85.6% |
| Adjusted CRA recent – world | −5.8% | 4.3% | −1.7% |
| Adjusted CRA less recent – world | −10.3% | 0.7% | −9.6% |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vidra, N.; Bijlsma, M.J.; Janssen, F. Impact of Different Estimation Methods on Obesity-Attributable Mortality Levels and Trends: The Case of The Netherlands. Int. J. Environ. Res. Public Health 2018, 15, 2146. https://doi.org/10.3390/ijerph15102146
Vidra N, Bijlsma MJ, Janssen F. Impact of Different Estimation Methods on Obesity-Attributable Mortality Levels and Trends: The Case of The Netherlands. International Journal of Environmental Research and Public Health. 2018; 15(10):2146. https://doi.org/10.3390/ijerph15102146
Chicago/Turabian StyleVidra, Nikoletta, Maarten J. Bijlsma, and Fanny Janssen. 2018. "Impact of Different Estimation Methods on Obesity-Attributable Mortality Levels and Trends: The Case of The Netherlands" International Journal of Environmental Research and Public Health 15, no. 10: 2146. https://doi.org/10.3390/ijerph15102146
APA StyleVidra, N., Bijlsma, M. J., & Janssen, F. (2018). Impact of Different Estimation Methods on Obesity-Attributable Mortality Levels and Trends: The Case of The Netherlands. International Journal of Environmental Research and Public Health, 15(10), 2146. https://doi.org/10.3390/ijerph15102146