Laboratory-Assessed Markers of Cardiometabolic Health and Associations with GIS-Based Measures of Active-Living Environments
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Neighborhood Active-Living Environments
2.3. Markers of Cardiometabolic Health
2.4. Physical Activity
2.5. Covariates
2.6. Statistical Analyses
3. Results
3.1. Participant Characteristics
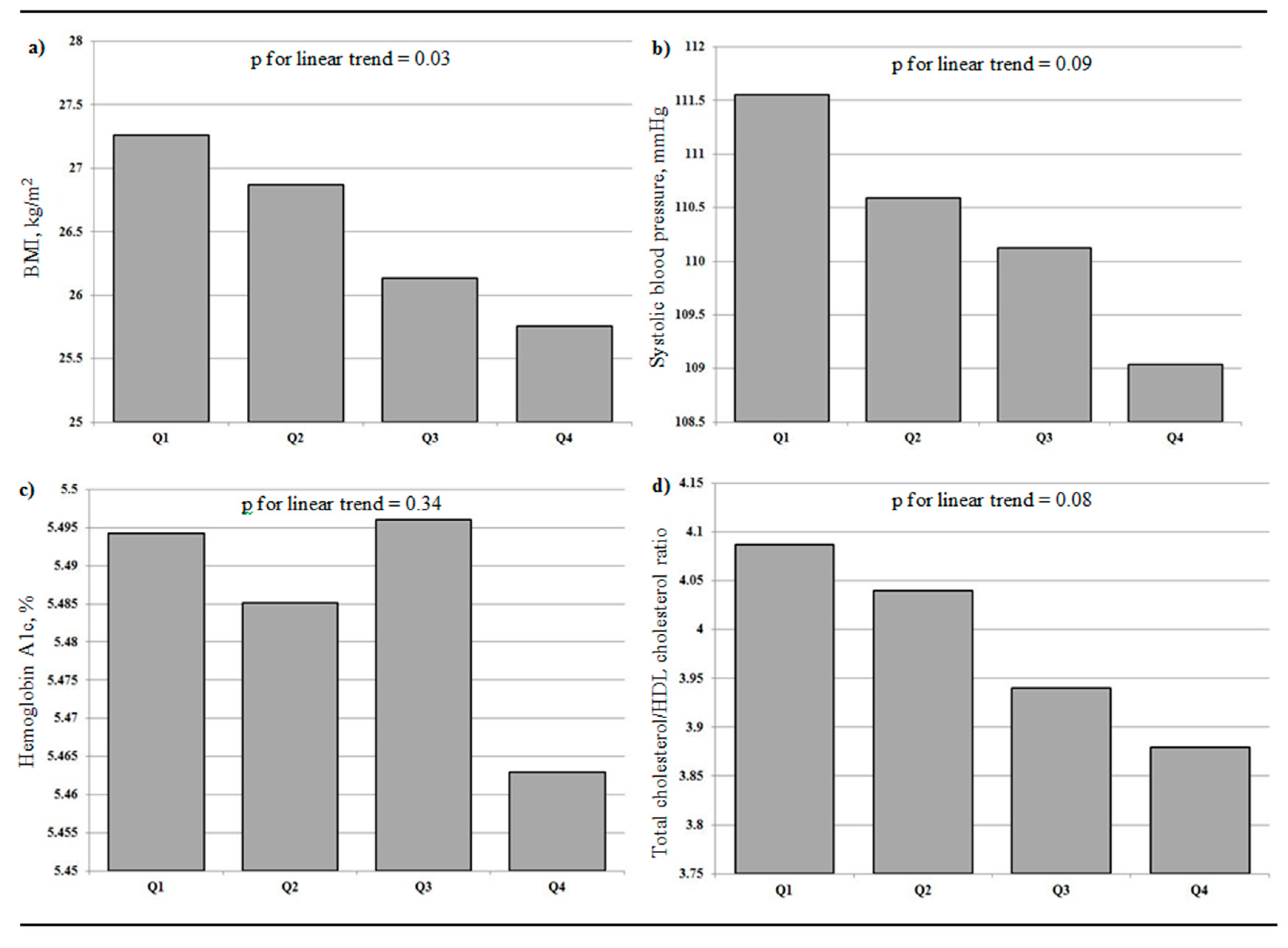
3.2. Neighborhood Active-Living Environments and Markers of Cardiometablic Health
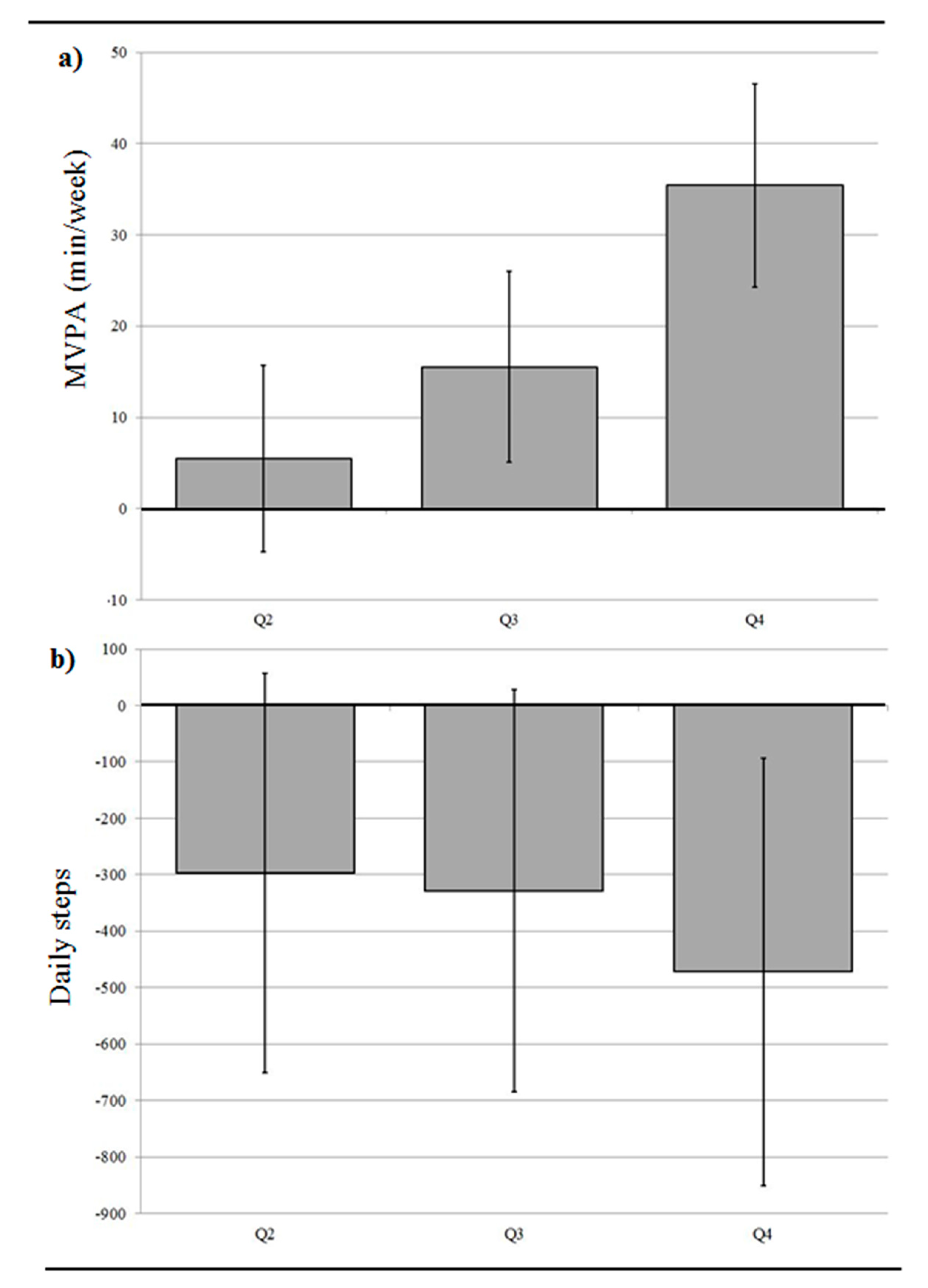
3.3. Neighborhood Active-Living Environments, Daily Step Count, and MVPA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Glazier, R.H.; Creatore, M.I.; Weyman, J.T.; Fazli, G.; Matheson, F.I.; Gozdyra, P.; Moineddin, R.; Shriqui, V.K.; Booth, G.L. Density, destinations or both? A comparison of measures of walkability in relation to transportation behaviors, obesity and diabetes in Toronto, Canada. PLoS ONE 2014, 9, E85295. [Google Scholar] [CrossRef] [PubMed]
- Creatore, M.I.; Glazier, R.H.; Moineddin, R.; Fazli, G.S.; Johns, A.; Gozdyra, P.; Matheson, F.I.; Kaufman-Shriqui, V.; Rosella, L.C.; Manuel, D.G.; et al. Association of Neighborhood Walkability with Change in Overweight, Obesity, and Diabetes. JAMA 2016, 315, 2211–2220. [Google Scholar] [CrossRef] [PubMed]
- Muller-Riemenschneider, F.; Pereira, G.; Villanueva, K.; Christian, H.; Knuiman, M.; Giles-Corti, B.; Bull, F.C. Neighborhood walkability and cardiometabolic risk factors in Australian adults: An observational study. BMC Public Health 2013, 13, 755. [Google Scholar] [CrossRef] [PubMed]
- Meline, J.; Chaix, B.; Pannier, B.; Ogedegbe, G.; Trasande, L.; Athens, J.; Duncan, D.T. Neighborhood walk score and selected Cardiometabolic factors in the French RECORD cohort study. BMC Public Health 2017, 17, 960. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Booth, G.L.; Creatore, M.I.; Moineddin, R.; Gozdyra, P.; Weyman, J.T.; Matheson, F.I.; Glazier, R.H. Unwalkable neighborhoods, poverty, and the risk of diabetes among recent immigrants to Canada compared with long-term residents. Diabetes Care 2013, 36, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Sundquist, K.; Eriksson, U.; Mezuk, B.; Ohlsson, H. Neighborhood walkability, deprivation and incidence of type 2 diabetes: A population-based study on 512,061 Swedish adults. Health Place 2015, 31, 24–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Auchincloss, A.H.; Diez Roux, A.V.; Brown, D.G.; Erdmann, C.A.; Bertoni, A.G. Neighborhood resources for physical activity and healthy foods and their association with insulin resistance. Epidemiology 2008, 19, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Chiu, M.; Rezai, M.R.; Maclagan, L.C.; Austin, P.C.; Shah, B.R.; Redelmeier, D.A.; Tu, J.V. Moving to a Highly Walkable Neighborhood and Incidence of Hypertension: A Propensity-Score Matched Cohort Study. Environ. Health Perspect. 2016, 124, 754–760. [Google Scholar] [CrossRef] [PubMed]
- AlEssa, H.B.; Chomistek, A.K.; Hankinson, S.E.; Barnett, J.B.; Rood, J.; Matthews, C.E.; Rimm, E.B.; Willett, W.C.; Hu, F.B.; Tobias, D.K. Objective Measures of Physical Activity and Cardiometabolic and Endocrine Biomarkers. Med. Sci. Sports Exerc. 2017, 49, 1817–1825. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Schuna, J.M., Jr.; Han, H.; Aguiar, E.J.; Green, M.A.; Busa, M.A.; Larrivee, S.; Johnson, W.D. Step-Based Physical Activity Metrics and Cardiometabolic Risk: NHANES 2005–2006. Med. Sci. Sports Exerc. 2017, 49, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Ferdinand, A.O.; Sen, B.; Rahurkar, S.; Engler, S.; Menachemi, N. The Relationship between Built Environments and Physical Activity: A Systematic Review. Am. J. Public Health 2012, 102, e7–e13. [Google Scholar] [CrossRef] [PubMed]
- Hajna, S.; Ross, N.A.; Joseph, L.; Harper, S.; Dasgupta, K. Neighbourhood walkability, daily steps and utilitarian walking in Canadian adults. BMJ Open 2015, 5, E008964. [Google Scholar] [CrossRef] [PubMed]
- Oakes, J.M.; Forsyth, A.; Schmitz, K.H. The effects of neighborhood density and street connectivity on walking behavior: The Twin Cities walking study. Epidemiol. Perspect. Innov. 2007, 4, 16. [Google Scholar] [CrossRef] [PubMed]
- Canadian Health Measures Survey (CHMS) Data User Guide: Cycle 1; Statistics Canada: Ottawa, ON, Canada, 2011.
- Bow, J.D.; Waters, N.M.; Faris, P.D.; Seidel, J.E.; Galbraith, P.D.; Knudtson, M.L.; Ghali, W.A. Accuracy of city postal code coordinates as a proxy for location of residence. Int. J. Health Geogr. 2004, 3, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kondo, K.; Lee, J.S.; Kawakubo, K.; Kataoka, Y.; Asami, Y.; Mori, K.; Umezaki, M.; Yamauchi, T.; Takagi, H.; Sunagawa, H.; et al. Association between daily physical activity and neighborhood environments. Environ. Health Prev. Med. 2009, 14, 196–206. [Google Scholar] [CrossRef] [PubMed]
- Hajna, S.; Dasgupta, K.; Joseph, L.; Ross, N.A. A call for caution and transparency in the calculation of land use mix: Measurement bias in the estimation of associations between land use mix and physical activity. Health Place 2014, 29, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Leslie, E.; Coffee, N.; Frank, L.; Owen, N.; Bauman, A.; Hugo, G. Walkability of local communities: Using geographic information systems to objectively assess relevant environmental attributes. Health Place 2007, 13, 111–122. [Google Scholar] [CrossRef] [PubMed]
- DMTI Spatial Inc. CanMap Streetfiles. v2009; DMTI Spatial Inc.: Markham, ON, Canada, 2009. [Google Scholar]
- Unadjusted 2006 Canadian Census Population Counts File; Statistics Canada: Ottawa, ON, Canada, 2006.
- Ettehad, D.; Emdin, C.A.; Kiran, A.; Anderson, S.G.; Callender, T.; Emberson, J.; Chalmers, J.; Rodgers, A.; Rahimi, K. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet 2016, 387, 957–967. [Google Scholar] [CrossRef]
- Castelli, W.P.; Anderson, K.; Wilson, P.W.; Levy, D. Lipids and risk of coronary heart disease. The Framingham Study. Ann. Epidemiol. 1992, 2, 23–28. [Google Scholar] [CrossRef]
- McQueen, M.J.; Hawken, S.; Wang, X.; Ounpuu, S.; Sniderman, A.; Probstfield, J.; Steyn, K.; Sanderson, J.E.; Hasani, M.; Volkova, E.; et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): A case-control study. Lancet 2008, 372, 224–233. [Google Scholar] [CrossRef]
- Yusuf, S.; Hawken, S.; Ounpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Dudina, A.; Cooney, M.T.; Bacquer, D.D.; Backer, G.D.; Ducimetiere, P.; Jousilahti, P.; Keil, U.; Menotti, A.; Njølstad, I.; Oganov, R.; et al. Relationships between body mass index, cardiovascular mortality, and risk factors: A report from the SCORE investigators. Eur. J. Cardiovasc. Prev. Rehabil. 2011, 18, 731–742. [Google Scholar] [CrossRef] [PubMed]
- Emerging Risk Factors Collaboration; Sarwar, N.; Gao, P.; Seshasai, S.R.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E.; Ingelsson, E.; Lawlor, D.A.; Selvin, E.; et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [PubMed]
- Fitness Canada. Canadian Standardized Test of Fitness (CSTF): Operations Manual, 3rd ed.; Government of Canada, Fitness and Amateur Sport: Ottawa, ON, Canada, 1986. [Google Scholar]
- Bryan, S.; Larose, M.S.-P.; Campbell, N.; Clarke, J.; Tremblay, M.S. Resting Blood Pressure and Heart Rate Measurement in the Canadian Health Measures Survey. Health Rep. 2010, 21, 71–78. [Google Scholar] [PubMed]
- Colley, R.C.; Garriguet, D.; Janssen, I.; Craig, C.L.; Clarke, J.; Tremblay, M.S. Physical activity of Canadian adults: Accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011, 22, 7–14. [Google Scholar] [PubMed]
- Colley, R.; Connor Gorber, S.; Tremblay, M.S. Quality control and data reduction procedures for accelerometry-derived measures of physical activity. Health Rep. 2010, 21, 63–69. [Google Scholar] [PubMed]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Esliger, D.W.; Probert, A.; Connor Gorber, S.; Bryan, S.; Laviolette, M.; Tremblay, M.S. Validity of the Actical accelerometer step-count function. Med. Sci. Sports Exerc. 2007, 39, 1200–1204. [Google Scholar] [CrossRef] [PubMed]
- Wasfi, R.A.; Dasgupta, K.; Orpana, H.; Ross, N.A. Neighborhood Walkability and Body Mass Index Trajectories: Longitudinal Study of Canadians. Am. J. Public Health 2016, 106, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Polsky, J.Y.; Moineddin, R.; Glazier, R.H.; Dunn, J.R.; Booth, G.L. Relative and absolute availability of fast-food restaurants in relation to the development of diabetes: A population-based cohort study. Can. J. Public Health 2016, 107, 5312. [Google Scholar] [CrossRef] [PubMed]
- Burgoine, T.; Forouhi, N.G.; Griffin, S.J.; Brage, S.; Wareham, N.J.; Monsivais, P. Does neighborhood fast-food outlet exposure amplify inequalities in diet and obesity? A cross-sectional study. Am. J. Clin. Nutr. 2016, 103, 1540–1547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hajna, S.; Ross, N.A.; Brazeau, A.S.; Belisle, P.; Joseph, L.; Dasgupta, K. Associations between neighbourhood walkability and daily steps in adults: A systematic review and meta-analysis. BMC Public Health 2015, 15, 768. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Characteristics | n | Mean (SD) |
| Age, years | 2809 | 41.5 (15.1) |
| % (n) | ||
| Women | 2809 | 54.2 (1521) |
| Married/common-law | 2807 | 58.3 (1635) |
| Education, bachelor degree or higher | 2789 | 26.9 (751) |
| Ever smoker | 2803 | 49.2 (1379) |
| Depressed | 2805 | 8.5 (238) |
| Children <15 years in household | 2809 | 41.0 (1151) |
| Working | 2101 | 75.9 (2768) |
| Cardiometabolic Measures | Mean (SD) | |
| BMI, kg/m2 | 2776 | 26.5 (5.4) |
| Systolic blood pressure, mmHg | 2807 | 110.3 (14.7) |
| Hemoglobin A1c, % | 2706 | 5.5 (0.4) |
| Total cholesterol/HDL cholesterol ratio | 2744 | 4.0 (1.3) |
| Physical Activity | Mean (SD) | |
| Daily step count | 2251 | 8820 (3655) |
| MVPA, minutes/week | 2254 | 167.3 (150.3) |
| Neighborhood Features | Mean (SD) | |
| Active-living environment index | 2809 | 0.06 (2.15) |
| Street connectivity, ≥3 way intersections/km2 | 2809 | 55 (31) |
| Land use mix, Range: 0 to 1 | 2809 | 0.22 (0.24) |
| Population density, population count/km2 | 2809 | 5381 (25,146) |
| Modela,b | Body Mass Index (kg/m2) c | Systolic Blood Pressure (mm/Hg) | Hemoglobin A1c (%) | Total Cholesterol/HDL Cholesterol Ratio |
|---|---|---|---|---|
| n = 2180 | n = 2179 | n = 2113 | n = 2136 | |
| Model 1 | ||||
| Quartile 2 | −0.39 (−0.93 to 0.16) | −0.50 (−2.14 to 1.14) | 0.01 (−0.03 to 0.05) | −0.01 (−0.16 to 0.14) |
| Quartile 3 | −1.24 (−1.79 to −0.69) | −0.77 (−2.42 to 0.88) | −0.01 (−0.04 to 0.03) | −0.15 (−0.30 to 0.01) |
| Quartile 4 | −1.49 (−2.03 to −0.95) | −2.82 (−4.46 to −1.18) | −0.04 (−0.07 to 0.001) | −0.17 (−0.32 to −0.02) |
| Model 2 | ||||
| Quartile 2 | −0.05 (−0.56 to 0.45) | 0.41 (−0.99 to 1.81) | 0.03 (−0.001 to 0.07) | 0.08 (−0.06 to 0.21) |
| Quartile 3 | −0.90 (−1.41 to −0.38) | −0.27 (−1.69 to 1.14) | 0.01 (−0.03 to 0.04) | −0.06 (−0.20 to 0.08) |
| Quartile 4 | −0.98 (−1.50 to −0.46) | −1.63 (−3.07 to −0.19) | −0.004 (−0.04 to 0.03) | −0.01 (−0.15 to 0.13) |
| Model 3 | ||||
| Quartile 2 | −0.08 (−0.59 to 0.42) | 0.29 (−1.11 to 1.68) | 0.04 (0.001 to 0.07) | 0.08 (−0.06 to 0.21) |
| Quartile 3 | −0.94 (−1.45 to −0.43) | −0.50 (−1.91 to 0.91) | 0.01 (−0.02 to 0.05) | −0.05 (−0.19 to 0.09) |
| Quartile 4 | −1.03 (−1.55 to −0.51) | −2.02 (−3.47 to −0.58) | 0.0001 (−0.04 to 0.04) | −0.02 (−0.16 to 0.12) |
| Model 4 | ||||
| Quartile 2 | 0.003 (−0.50 to 0.51) | 0.41 (−0.99 to 1.81) | 0.04 (0.001 to 0.07) | 0.09 (−0.05 to 0.23) |
| Quartile 3 | −0.81 (−1.32 to −0.29) | −0.29 (−1.71 to 1.13) | 0.01 (−0.02 to 0.05) | −0.02 (−0.16 to 0.12) |
| Quartile 4 | −0.79 (−1.31 to −0.27) | −1.65 (−3.10 to −0.20) | 0.002 (−0.03 to 0.04) | 0.02 (−0.12 to 0.17) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hajna, S.; Dasgupta, K.; Ross, N.A. Laboratory-Assessed Markers of Cardiometabolic Health and Associations with GIS-Based Measures of Active-Living Environments. Int. J. Environ. Res. Public Health 2018, 15, 2079. https://doi.org/10.3390/ijerph15102079
Hajna S, Dasgupta K, Ross NA. Laboratory-Assessed Markers of Cardiometabolic Health and Associations with GIS-Based Measures of Active-Living Environments. International Journal of Environmental Research and Public Health. 2018; 15(10):2079. https://doi.org/10.3390/ijerph15102079
Chicago/Turabian StyleHajna, Samantha, Kaberi Dasgupta, and Nancy A. Ross. 2018. "Laboratory-Assessed Markers of Cardiometabolic Health and Associations with GIS-Based Measures of Active-Living Environments" International Journal of Environmental Research and Public Health 15, no. 10: 2079. https://doi.org/10.3390/ijerph15102079
APA StyleHajna, S., Dasgupta, K., & Ross, N. A. (2018). Laboratory-Assessed Markers of Cardiometabolic Health and Associations with GIS-Based Measures of Active-Living Environments. International Journal of Environmental Research and Public Health, 15(10), 2079. https://doi.org/10.3390/ijerph15102079




