Outcomes in the Utilization of Single Percutaneous Cholecystostomy in a Low-Income Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects and Data Source
2.2. Data Protection and Permission
2.3. Data Definition
2.4. Patient Selection
2.5. Measurement Outcomes
2.5.1. Thirty-Day Mortality and In-Hospital Mortality
2.5.2. In-Hospital Complications
2.5.3. Routine Discharge
2.5.4. One-Year Recurrence
2.6. Statistical Analysis
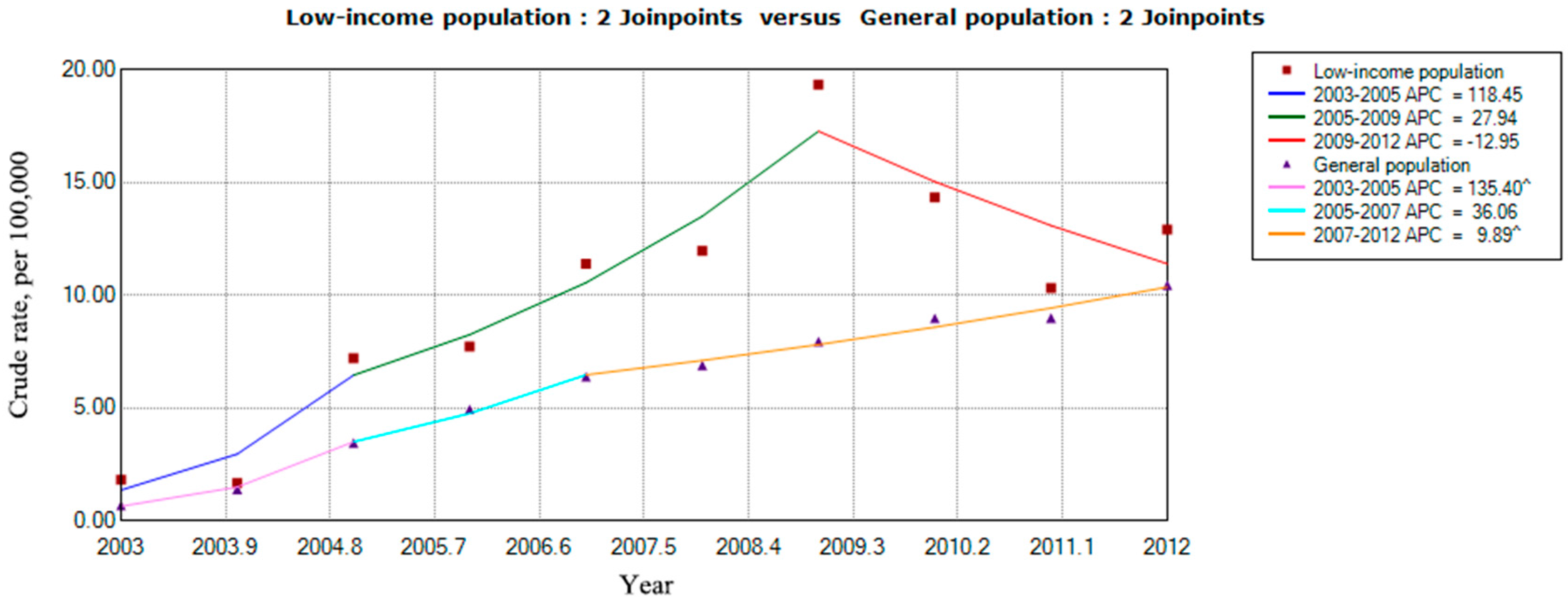
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Patterson, E.J.; Mcloughlin, R.F.; Mathieson, J.R.; Cooperberg, P.L.; Macfarlane, J.K. An alternative approach to acute cholecystitis. Percutaneous cholecystostomy and interval laparoscopic cholecystectomy. Surg. Endosc. 1996, 10, 1185–1188. [Google Scholar] [CrossRef] [PubMed]
- Abi-Haidar, Y.; Sanchez, V.; Williams, S.A.; Itani, K.M. Revisiting percutaneous cholecystostomy for acute cholecystitis based on a 10-year experience. Arch. Surg. 2012, 147, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Yoo, K.S. Efficacy of preoperative percutaneous cholecystostomy in the management of acute cholecystitis according to severity grades. Korean J. Intern. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Teoh, W.M.; Cade, R.J.; Banting, S.W.; Mackay, S.; Hassen, A.S. Percutaneous cholecystostomy in the management of acute cholecystitis. ANZ J. Surg. 2005, 75, 396–398. [Google Scholar] [CrossRef] [PubMed]
- Mckay, A.; Abulfaraj, M.; Lipschitz, J. Short- and long-term outcomes following percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Surg. Endosc. 2012, 26, 1343–1351. [Google Scholar] [CrossRef] [PubMed]
- Aljundi, W.; Cannon, T.; Antakia, R.; Anoop, U.; Balamurugan, R.; Everitt, N.; Ravi, K. Percutaneous cholecystostomy as an alternative to cholecystectomy in high risk patients with biliary sepsis: A district general hospital experience. Ann. R. Coll Surg. Engl. 2012, 94, 99–101. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.C.; Chang, C.W.; Chu, C.H. Percutaneous cholecystostomy for acute cholecystitis in high-risk elderly patients. Kaohsiung J. Med. Sci. 2016, 32, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Welschbilligmeunier, K.; Pessaux, P.; Lebigot, J.; Lermite, E.; Ch, A.; Brehant, O.; Hamy, A.; Arnaud, J.P. Percutaneous cholecystostomy for high-risk patients with acute cholecystitis. Surg. Endosc. Other Interv. Tech. 2005, 19, 1256–1259. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, R.L.; Ryan, C.M.; Lee, M.J.; Mueller, P.R.; Tompkins, R.G. Percutaneous cholecystostomy in the critically ill burn patient. J. Trauma 1995, 38, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Hermiz, S.J.; Diegidio, P.; Garimella, R.; Ortiz-Pujols, S.; Yu, H.; Isaacson, A.; Mauro, M.A.; Cairns, B.A.; Hultman, C.S. Acalculous Cholecystitis in Burn Patients: Is There a Role for Percutaneous Cholecystostomy? Clin. Plast. Surg. 2017, 44, 567–571. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.; Moonka, R.; Stelzner, M. Percutaneous cholecystostomy for acute cholecystitis in veteran patients. Am. J. Surg. 2000, 180, 198–202. [Google Scholar] [CrossRef]
- Caliskan, K. The use of percutaneous cholecystostomy in the treatment of acute cholecystitis during pregnancy. Clin. Exp. Obstet. Gynecol. 2017, 44, 11–13. [Google Scholar]
- Allmendinger, N.; Hallisey, M.J.; Ohki, S.K.; Straub, J.J. Percutaneous cholecystostomy treatment of acute cholecystitis in pregnancy. Obstet. Gynecol. 1995, 86, 653–654. [Google Scholar] [CrossRef]
- Bonito, A.J.; Bann, C.; Eicheldinger, C.; Carpenter, L. Creation of New Race-Ethnicity Codes and Socioeconomic Status (SES) Indicators for Medicare Beneficiaries; RTI International, Agency for Healthcare Research and Quality: Chapel Hill, NC, USA, 2008.
- Bennett, K.M.; Scarborough, J.E.; Pappas, T.N.; Kepler, T.B. Patient socioeconomic status is an independent predictor of operative mortality. Ann. Surg. 2010, 252, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Birkmeyer, N.J.; Gu, N.; Baser, O.; Morris, A.M.; Birkmeyer, J.D. Socioeconomic status and surgical mortality in the elderly. Med. Care 2008, 46, 893–899. [Google Scholar] [CrossRef] [PubMed]
- Diehl, A.K.; Rosenthal, M.; Hazuda, H.P.; Comeaux, P.J.; Stern, M.P. Socioeconomic status and the prevalence of clinical gallbladder disease. J. Chronic Dis. 1985, 38, 1019–1026. [Google Scholar] [CrossRef]
- Ambur, V.; Taghavi, S.; Kadakia, S.; Jayarajan, S.; Gaughan, J.; Sjoholm, L.O.; Pathak, A.; Santora, T.; Rappold, J.; Goldberg, A.J. Does socioeconomic status predict outcomes after cholecystectomy? Am. J. Surg. 2016, 221, S68. [Google Scholar] [CrossRef]
- Department of Statistics (DOS). Ministry of the Interior, Survey of Living Conditions of Low-Income Households in Taiwan-Fuchien Area. 2008. Available online: http://www.mohw.gov.tw/cht/DOS/Statistic.aspx?f_list_no=312&fod_list_no=4699 (accessed on 5 February 2015).
- Chou, Y.; Lin, S. Report of the Survey of the Basic Needs for Low-Income Families in Taoyuan County, Taiwan; Hsuan Chuang University: Hsinchu City, Taiwan, 2007. [Google Scholar]
- Department of Statistics Mohaw. Report on the Low-Income and Middle-Income Family Living Condition Survey 2013; Department of Health and Welfare of the Executive Yuan: Taipei City, Taiwan, 2014.
- Anderson, J.E.; Chang, D.C.; Talamini, M.A. A nationwide examination of outcomes of percutaneous cholecystostomy compared with cholecystectomy for acute cholecystitis, 1998–2010. Surg. Endosc. 2013, 27, 3406–3411. [Google Scholar] [CrossRef] [PubMed]
- Public Assistance Act. Available online: http://law.moj.gov.tw/LawClass/LawAll.aspx?PCode=D0050078 (accessed on 5 September 2017).
- Taiwan NHI Information for the Public: Essential Data of Ensured Affair. Available online: http://www.nhi.gov.tw/webdata/webdata.aspx?menu=17&menu_id=661&WD_ID=689&webdata_id=805 (accessed on 7 December 2013).
- Caliendo, M.; Kopeinig, S. Some Practical Guidance for the Implementation of Propensity Score Matching. J. Econ. Surv. 2008, 22, 31–72. [Google Scholar] [CrossRef]
- Joinpoint Regression Program; version 4.3.1.0; Statistical Methodology and Applications Branch, Surveillance Research Program; National Cancer Institute: Bethesda, MD, USA, April 2016.
- National Cancer Institute; version 4.3.1.0; Surveillance Research Program, Statistical Methodology and Applications Branch, Joinpoint Regression Program Online Help System; National Cancer Institute: Bethesda, MD, USA, April 2016.
- Clegg, L.X.; Hankey, B.F.; Tiwari, R.; Feuer, E.J.; Edwards, B.K. Estimating average annual per cent change in trend analysis. Stat. Med. 2009, 28, 3670–3682. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-T. Poverty in Taiwan: A review of related studies. NTU Soc. Work Rev. J. 2005, 10, 1–54. [Google Scholar]
- Chang, Y.R.; Ahn, Y.J.; Jang, J.Y.; Kang, M.J.; Kwon, W.; Jung, W.H.; Kim, S.W. Percutaneous cholecystostomy for acute cholecystitis in patients with high comorbidity and re-evaluation of treatment efficacy. Surgery 2014, 155, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Duszak, R.; Behrman, S.W. National trends in percutaneous cholecystostomy between 1994 and 2009: Perspectives from Medicare provider claims. J. Am. Coll. Radiol. 2012, 9, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.J.; Manske, J.G.; Mathiason, M.A.; Kallies, K.J.; Kothari, S.N. Changing trends and outcomes in the use of percutaneous cholecystostomy tubes for acute cholecystitis. Ann. Surg. 2013, 257, 1112–1115. [Google Scholar] [CrossRef] [PubMed]
- Cherng, N.; Witkowski, E.T.; Sneider, E.B.; Wiseman, J.T.; Lewis, J.; Litwin, D.E.M.; Santry, H.P.; Cahan, M.; Shah, S.A. Use of cholecystostomy tubes in the management of patients with primary diagnosis of acute cholecystitis. J. Am. Coll. Surg. 2012, 214, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Wada, K.; Takada, T.; Kawarada, Y.; Nimura, Y.; Miura, F.; Yoshida, M.; Mayumi, T.; Strasberg, S.; Pitt, H.A.; Gadacz, T.R.; et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo Guidelines. J. Hepato-Biliary-Pancreat. Surg. 2007, 14, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, Y.; Takada, T.; Strasberg, S.M.; Pitt, H.A.; Gouma, D.J.; Garden, O.J.; Buchler, M.W.; Gomi, H.; Dervenis, C.; Windsor, J.A.; et al. TG13 surgical management of acute cholecystitis. J. Hepato-Biliary-Pancreat. Sci. 2013, 20, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Li, J.C.; Lee, D.W.; Lai, C.W.; Li, A.C.; Chu, D.W.; Chan, A.C. Percutaneous cholecystostomy for the treatment of acute cholecystitis in the critically ill and elderly. Hong Kong Med. J. 2004, 10, 389–393. [Google Scholar] [PubMed]
- Horn, T.; Christensen, S.D.; Kirkegård, J.; Larsen, L.P.; Knudsen, A.R.; Mortensen, F.V. Percutaneous cholecystostomy is an effective treatment option for acute calculous cholecystitis: A 10-year experience. HPB Off. J. Int. Hepato Pancreato Biliary Assoc. 2015, 17, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Sanjay, P.; Mittapalli, D.; Marioud, A.; White, R.D.; Ram, R.; Alijani, A. Clinical outcomes of a percutaneous cholecystostomy for acute cholecystitis: A multicentre analysis. HPB Off. J. Int. Hepato Pancreato Biliary Assoc. 2013, 15, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Nasim, S.; Khan, S.; Alvi, R.; Chaudhary, M. Emerging indications for percutaneous cholecystostomy for the management of acute cholecystitis—A retrospective review. Int. J. Surg. 2011, 9, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Winbladh, A.; Gullstrand, P.; Svanvik, J.; Sandström, P. Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB Off. J. Int. Hepato Pancreato Biliary Assoc. 2009, 11, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Hadashalpern, I.; Patlas, M.; Knizhnik, M.; Zaghal, I.; Fisher, D. Percutaneous cholecystostomy in the management of acute cholecystitis. IMAJ 2003, 5, 170–171. [Google Scholar]
- Li, M.; Li, N.; Ji, W.; Quan, Z.; Wan, X.; Wu, X.; Li, J. Percutaneous cholecystostomy is a definitive treatment for acute cholecystitis in elderly high-risk patients. Am. Surg. 2013, 79, 524–527. [Google Scholar] [PubMed]
- Mcgillicuddy, E.A.; Schuster, K.M.; Barre, K.; Suarez, L.; Hall, M.R.; Kaml, G.J.; Davis, K.A.; Longo, W.E. Non-operative management of acute cholecystitis in the elderly. Br. J. Surg. 2012, 99, 1254–1261. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.H.; Wu, C.Y.; Yang, J.C.; Lien, W.C.; Wang, H.P.; Liu, K.L.; Wu, Y.M.; Chen, S.C. Long-Term Outcomes of Patients with Acute Cholecystitis after Successful Percutaneous Cholecystostomy Treatment and the Risk Factors for Recurrence: A Decade Experience at a Single Center. PLoS ONE 2016, 11, e0148017. [Google Scholar] [CrossRef] [PubMed]

| Variables | Low-Income Population (N = 152) | General Population (N = 11,032) | p Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | 0.005 | ||||
| Female | 45 | 29.61% | 4525 | 41.02% | |
| Male | 107 | 70.39% | 6507 | 58.98% | |
| Age Stratum | <0.001 | ||||
| 18–29 y/o | 0 | 0.00% | 111 | 1.01% | |
| 30–39 y/o | 8 | 5.26% | 302 | 2.74% | |
| 40–49 y/o | 27 | 17.76% | 614 | 5.57% | |
| 50–59 y/o | 31 | 20.39% | 1336 | 12.11% | |
| 60–69 y/o | 19 | 12.50% | 1856 | 16.82% | |
| 70 y/o or more | 67 | 44.08% | 6813 | 61.76% | |
| CCI Score | 0.445 | ||||
| 0 | 72 | 47.37% | 5422 | 49.15% | |
| 1 | 46 | 30.26% | 2782 | 25.22% | |
| 2 | 19 | 12.50% | 1407 | 12.75% | |
| ≥3 | 15 | 9.87% | 1421 | 12.88% | |
| Cause of Procedure | 0.386 | ||||
| AC with a C/S | 53 | 34.87% | 4063 | 36.83% | |
| AC without a C/S | 55 | 36.18% | 3369 | 30.54% | |
| Calculus without AC | 16 | 10.53% | 1228 | 11.13% | |
| ODGBT | 12 | 7.89% | 1369 | 12.41% | |
| MNDOP | 7 | 4.61% | 347 | 3.15% | |
| Other | 9 | 5.92% | 656 | 5.95% | |
| Hospital Level | <0.001 | ||||
| Medical Center | 60 | 39.47% | 6205 | 56.25% | |
| Regional Hospital | 76 | 50.00% | 4551 | 41.25% | |
| District Hospital | 16 | 10.53% | 276 | 2.50% | |
| Variables | Low-Income Population (N = 152) | Control Group (N = 760) | p Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | 1.00 | ||||
| Female | 45 | 29.61% | 225 | 29.61% | |
| Male | 107 | 70.39% | 535 | 70.39% | |
| Age Stratum | 0.927 | ||||
| 18–29 y/o | 0 | 0.00% | 4 | 0.53% | |
| 30–39 y/o | 8 | 5.26% | 32 | 4.21% | |
| 40–49 y/o | 27 | 17.76% | 126 | 16.58% | |
| 50–59 y/o | 31 | 20.39% | 166 | 21.84% | |
| 60–69 y/o | 19 | 12.50% | 99 | 13.03% | |
| 70 y/o or more | 67 | 44.08% | 333 | 43.82% | |
| CCI Score | 0.95 | ||||
| 0 | 72 | 47.37% | 377 | 49.61% | |
| 1 | 46 | 30.26% | 214 | 28.16% | |
| 2 | 19 | 12.50% | 97 | 12.76% | |
| ≥3 | 15 | 9.87% | 72 | 9.47% | |
| Cause of Procedure | 1.00 | ||||
| AC with a C/S | 53 | 34.87% | 265 | 34.87% | |
| AC without a C/S | 55 | 36.18% | 278 | 36.58% | |
| Calculus without AC | 16 | 10.53% | 84 | 11.05% | |
| ODGBT | 12 | 7.89% | 56 | 7.37% | |
| MNDOP | 7 | 4.61% | 36 | 4.74% | |
| Other | 9 | 5.92% | 41 | 5.39% | |
| Hospital Level | 0.865 | ||||
| Medical Center | 60 | 39.47% | 290 | 38.16% | |
| Regional Hospital | 76 | 50.00% | 397 | 52.24% | |
| District Hospital | 16 | 10.53% | 73 | 9.61% | |
| Outcome Variable | Total (N = 912) | Low-Income Population (N = 152) | Control (N = 760) | p Value a | |||
|---|---|---|---|---|---|---|---|
| n | Percent (%) | n | Percent (%) | n | Percent (%) | ||
| In-Hospital Mortality | 92 | 10.09% | 23 | 15.13% | 69 | 9.08% | 0.024 |
| Crude OR (95% CI) | -- | 1.786 (1.074, 2.967) | 1.0 | 0.025 | |||
| Adjusted OR (95% CI) | -- | 1.816 (1.079, 3.056) | 1.0 | 0.025 | |||
| 30-Day Mortality | 41 | 4.50% | 9 | 5.92% | 32 | 4.21% | 0.353 |
| Crude OR (95% CI) | -- | 1.432 (0.669, 3.064) | 1.0 | 0.355 | |||
| Adjusted OR (95% CI) | -- | 1.431 (0.651, 3.146) | 1.0 | 0.373 | |||
| In-Hospital Complications | 18 | 1.97% | 4 | 2.63% | 14 | 1.84% | 0.523 |
| Crude OR (95% CI) | -- | 1.440 (0.468, 4.436) | 1.0 | 0.525 | |||
| Adjusted OR (95% CI) | -- | 1.446 (0.464, 4.501) | 1.0 | 0.525 | |||
| Rate of Routine Discharge | 766 | 83.99% | 121 | 79.61% | 645 | 84.87% | 0.106 |
| Crude OR (95% CI) | -- | 0.696 (0.447, 1.082) | 1.0 | 0.108 | |||
| Adjusted OR (95% CI) | -- | 0.682 (0.430, 1.083) | 1.0 | 0.104 | |||
| One-Year Recurrence | 199 | 21.82% | 23 | 15.13% | 176 | 23.16% | 0.029 |
| Crude OR (95% CI) | -- | 0.592 (0.368, 0.951) | 1.0 | 0.030 | |||
| Adjusted OR (95% CI) | -- | 0.583 (0.360, 0.945) | 1.0 | 0.029 | |||
| Length of Hospital Stay (Mean ± SE) | -- | 18.26 ± 1.16 | 17.18 ± 0.15 | 0.894 | |||
| Hospital Costs (Mean ± SE) b | -- | 3914.52 ± 329.89 | 4109.36 ± 53.06 | 0.048 | |||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, P.; Yang, N.-P.; Chang, N.-T.; Lai, K.R.; Lin, K.-B.; Chan, C.-L. Outcomes in the Utilization of Single Percutaneous Cholecystostomy in a Low-Income Population. Int. J. Environ. Res. Public Health 2017, 14, 1601. https://doi.org/10.3390/ijerph14121601
Lu P, Yang N-P, Chang N-T, Lai KR, Lin K-B, Chan C-L. Outcomes in the Utilization of Single Percutaneous Cholecystostomy in a Low-Income Population. International Journal of Environmental Research and Public Health. 2017; 14(12):1601. https://doi.org/10.3390/ijerph14121601
Chicago/Turabian StyleLu, Ping, Nan-Ping Yang, Nien-Tzu Chang, K. Robert Lai, Kai-Biao Lin, and Chien-Lung Chan. 2017. "Outcomes in the Utilization of Single Percutaneous Cholecystostomy in a Low-Income Population" International Journal of Environmental Research and Public Health 14, no. 12: 1601. https://doi.org/10.3390/ijerph14121601
APA StyleLu, P., Yang, N.-P., Chang, N.-T., Lai, K. R., Lin, K.-B., & Chan, C.-L. (2017). Outcomes in the Utilization of Single Percutaneous Cholecystostomy in a Low-Income Population. International Journal of Environmental Research and Public Health, 14(12), 1601. https://doi.org/10.3390/ijerph14121601





