Exploring the Housing and Household Energy Pathways to Stress: A Mixed Methods Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Measures
2.3. Data Analysis
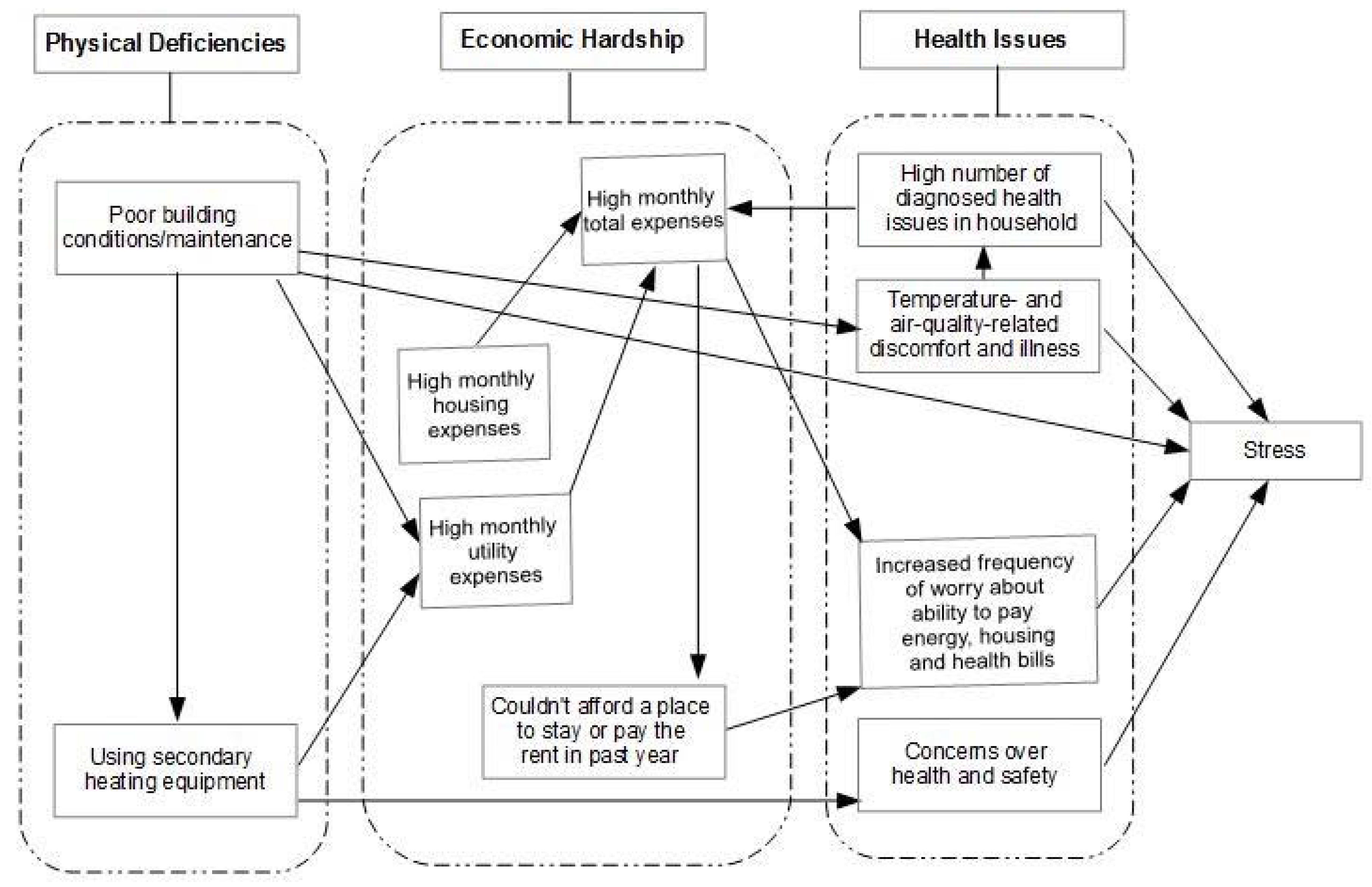
3. Results
3.1. Physical Deficiencies in the Home Environment
“My dogs couldn’t sleep, they would shiver... I mean literally, I had to put clothes in there, I gave them the heater, I put the heater for my dogs. And my wife was sleeping in a sweater like this, hoodied up, sweatpants, socks... she can’t stand it and it really affects her. And, it was a rough winter here.”—10011
“The front room, that’s why this is out here (pointing to bed in living room) because it’s like I’m not sleeping in there... F***ing cold, I mean it’s freezing. In there, I mean you can probably see your breath in the air. That’s how cold it is in that room alone.”—10010
“I would get snow and water (inside my home from) the draft on the door... If the wind would blow one way, we would have snow piling up in the house. I couldn’t get that fixed. I had the front door broken with no lock that you could just push it with a finger for years, because I couldn’t afford a new door... So for a few years I had no security whatsoever for the door.”—10003
“When I moved in here, the window in the kitchen, at the fire escape wouldn’t stay open. So you would have to prop it up... that’s messy, because it’s the window. It’s a method of escape and if you can’t keep the window open or to get out, it’s a dead weight window. And that took three months. And that was only because the city came and did that...”—10010
Interviewer: “Did you ever use your stove or oven to provide heat?”Respondent: “Yes... I only did it one time cause like I was telling her, running that gas is not healthy at all, but it was unbearable so it had to be done.”—10011
“Right now the (utility bill) I just got was not that high, it was two sixty five for one month. And then next month it’s gonna be a little higher, could be more... because my mother uses the electric heater.”—10009
3.2. Economic Hardship
“I was trying not to default on the mortgage. That was the main thing. The water bill was here, that was there, and you know, it was rough... you know, the anxiety would build. When it comes, the bills show up, and then there’s no money, and school started, and the kids have this, and then, you know, of course, it puts you in an emotional state.”—10002
“I’ve gotten a light bill for $1,100 dollars. That’s impossible, I don’t own a store. That is impossible. And who has to suffer and pay it? We did... How you gonna get that when you gotta pay $1,300 dollars rent? You know, we all have budgets, so. Yes it has been rough, as far as when it comes to that light.”—10011
“When I do the level billing at the end of the year, there’s always a large amount that I have to pay. So then I always have to tell them, you know, I can’t pay it all. It’s always in the thousands. So even though the level billing is great, because I’m fixed on one thing, but at the end of the year that’s when the stress level comes.”—10003
3.3. Health Issues
“I have low blood pressure, so with the asthma it’s a problem. Last year one Sunday I was sweeping the leaves. The next day I couldn’t even breathe, I had to go to the doctor. I ended up in the hospital period... So every time I get sick from the asthma it’s a problem, because of the medication issues. I can’t take inhalers.”—10009
“When we didn’t have a furnace... they would bundle up. Then her boyfriend loaned us three heaters... you had to do what you had to do. You know?... We had to deal with a lot of colds, my asthma.”—10003
“He’s gone through depression because he couldn’t find a job and he felt horrible. And a couple days ago he says, ‘Mom, I feel bad going to school... I’m a man now’... But, so he’s stressed out. And he’s been depressed with this now.”—10003
“I was hospitalized in February and so they made a single payment of like 9000 dollars and so there’s an outstanding balance of like sixty something thousand dollars and so sometimes they call me... how am I going to pay? Imagine that quantity.”—10008
Interviewer: “Now tell me a little about the anxiety you were describing, like feeling anxious…”Respondent: “Yeah, that’s a lot. Because I don’t know, like when I got injured it was like what’s gonna happen? And then I had the misfortune that the insurance company for compensation has been horrible. They delay my payments for three, four months, and I’ve had to fight. And I couldn’t go to work... the anxiety of you know, when was my next check? I was down to my last payment. After that I didn’t know how I was going to pay.”—10003
4. Discussion
Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wadsworth, M.E. Working with low-income families: Lessons learned from basic and applied research on coping with poverty-related stress. J. Contemp. Psychother. 2011, 42, 17–25. [Google Scholar] [CrossRef]
- Evans, G.W. The environment of childhood poverty. Am. Psychol. 2004, 59, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Dunn, J.R. Housing and inequalities in health: A study of socioeconomic dimensions of housing and self-reported health from a survey of Vancouver residents. J. Epidemiol. Community Health 2002, 56, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Adler, N.E.; Boyce, T.; Chesney, M.A.; Cohen, S.; Folkman, S.; Kahn, R.L.; Syme, S.L. Socioeconomic status and health: The challenge of the gradient. Am. Psychol. 1994, 49, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Baum, A.; Garofalo, J.P.; Yali, A.M. Socioeconomic status and chronic stress: Does stress account for SES effects on health? Ann. N. Y. Acad. Sci. 1999, 896, 131–144. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S.; Stellar, E. Stress and the individual mechanisms leading to disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology 2000, 22, 108–124. [Google Scholar] [CrossRef]
- National Institutes of Health. Q&A on Stress for Adults: How It Affects Your Health and What You Can Do about It. 2014. Available online: http://www.nimh.nih.gov/health/publications/stress/index.shtml (accessed on 12 November 2014). [Google Scholar]
- Shonkoff, J.P.; Garner, A.S. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012, 129, 232–246. [Google Scholar] [CrossRef] [PubMed]
- Harvard University Center on the Developing Child. Key Concepts: Toxic Stress. 2015. Available online: http://developingchild.harvard.edu/key_concepts/toxic_stress_response/ (accessed on 14 April 2015).
- Shonkoff, J.P.; Boyce, W.T.; McEwen, B.S. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA 2009, 301, 2252–2259. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.B.; Riley, A.W.; Granger, D.A.; Riis, J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics 2013, 131, 319–327. [Google Scholar] [CrossRef] [PubMed]
- De Carlo Santiago, C.; Wadsworth, M.E.; Stump, J. Socioeconomic status, neighborhood disadvantage, and poverty-related stress: Prospective effects on psychological syndromes among diverse low-income families. J. Econ. Psychol. 2011, 32, 218–230. [Google Scholar] [CrossRef]
- Evans, J.; Hyndman, S.; Stewart-Brown, S.; Smith, D.; Petersen, S. An epidemiological study of the relative importance of damp housing in relation to adult health. J. Epidemiol. Community Health 2000, 54, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Fullilove, M.T. Housing is health care. Am. J. Prev. Med. 2010, 39, 607–608. [Google Scholar] [CrossRef] [PubMed]
- Suglia, S.F.; Duarte, C.S.; Sandel, M.T. Housing quality, housing instability, and maternal mental health. J. Urban Health 2011, 88, 1105–1116. [Google Scholar] [CrossRef] [PubMed]
- Pollack, C.E.; Griffin, B.A.; Lynch, J. Housing Affordability and Health among Homeowners and Renters. Am. J. Prev. Med. 2010, 39, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Pollack, C.E.; Lynch, J. Health status of people undergoing foreclosure in the Philadelphia region. Am. J. Public Health 2009, 99, 1833–1839. [Google Scholar] [CrossRef] [PubMed]
- Hernández, D. Understanding “energy insecurity” and why it matters to health. Soc. Sci. Med. 2016, 167, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hernández, D. Energy insecurity: A framework for understanding energy, the built environment and health among vulnerable populations in the context of climate change. Am. J. Public Health 2013, 103, 32–34. [Google Scholar] [CrossRef] [PubMed]
- Coley, R.L.; Leventhal, T.; Lynch, A.D.; Kull, M. Relations between housing characteristics and the well-being of low-income children and adolescents. Dev. Psychol. 2013, 49, 1775. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.; Dixon, S.L.; Jacobs, D.E.; Breysse, J.; Akoto, J.; Tohn, E.; Isaacson, M.; Evens, A.; Hernandez, Y. Watts-to-wellbeing: Does residential energy conservation improve health? Energy Effic. 2013, 7, 151–160. [Google Scholar] [CrossRef]
- Gilbertson, J.; Grimsley, M.; Green, G. Psychosocial routes from housing investment to health: Evidence from England’s home energy efficiency scheme. Energy Policy 2012, 49, 122–133. [Google Scholar] [CrossRef]
- Harrington, B.E.; Heyman, B.; Merleau-Ponty, N.; Stockton, H.; Ritchie, N.; Heyman, A. Keeping warm and staying well: Findings from the qualitative arm of the Warm Homes Project. Health Soc. Care Community 2004, 13, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Hernández, D.; Phillips, D. Benefit or burden? Perceptions of energy efficiency efforts among low-income housing residents in New York City. Energy Res. Soc. Sci. 2015, 8, 52–59. [Google Scholar] [CrossRef] [PubMed]
- United States Census Bureau. Available online: http://www2.census.gov/programs-surveys/demo/tables/p60/252/table3.pdf (accessed on 5 August 2016).
- Institute for Child Poverty and Health. On the Brink: Homelessness a Reality in the South Bronx. 2011. Available online: http://www.icphusa.org/PDF/reports/ICPH_PolicyReprot_OnTheBrink_HomelessnessARealityInTheSouthBronx.pdf (accessed on 5 August 2016).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Olmedo, O.; Goldstein, I.F.; Acosta, L.; Divjan, A.; Rundle, A.G.; Chew, G.L.; Mellins, R.B.; Hoepner, L.; Andrews, H.; Lopez-Pintado, S.; et al. Neighborhood differences in exposure and sensitization to cockroach, mouse, dust mite, cat and dog allergens in New York City. J. Allergy Clin. Immunol. 2011, 128, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Colton, R. Measuring the Outcomes of Low-Income Energy Assistance Programs through a Home Energy Insecurity Scale. Available online: http://www.acf.hhs.gov/sites/default/files/ocs/measuring_outcome_0.pdf (accessed on 12 May 2015).
- United States Census Bureau. American Housing Survey. 2014. Available online: http://www.census.gov/programs-surveys/ahs.html (accessed on 12 May 2015). [Google Scholar]
- Tonn, B.; Schmory, R.; Wangner, S. Weatherizing the homes of low-income home energy assistance program clients: A programmatic assessment. Energy Policy 2003, 31, 735–744. [Google Scholar] [CrossRef]
- Ware, J.E.; Snow, K.K.; Kosinski, M.; Gandek, B. SF-36 Health Survey Manual and Interpretation Guide; The Health Institute, New England Medical Center: Boston, MA, USA, 2008; p. 1993. [Google Scholar]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Williamson, G. Perceived stress in a probability sample of the U.S. In The Social Psychology of Health: Claremont Symposium on Applied Social Psychology; Spacapam, S., Oskamp, S., Eds.; Sage: Newbury Park, CA, USA, 1988; pp. 31–67. [Google Scholar]
- Cohen, S.; Janicki-Deverts, D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006 and 2009. J. Appl. Soc. Psychol. 2012, 42, 1320–1334. [Google Scholar] [CrossRef]
- Ahrens, M. Home Fires Involving Cooking Equipment. 2013. Available online: http://www.nfpa.org/research/reports-and-statistics/fire-causes/appliances-and-equipment/cooking-equipment (accessed on 12 May 2015).
- Hall, J.R. Home Fires Involving Heating Equipment, National Fire Protection Association. 2013. Available online: http://www.nfpa.org/~/media/Files/Research/NFPA%20reports/Major%20Causes/osheating.pdf (accessed on 12 May 2015).
- Dennekamp, M.; Howarth, S.; Dick, C.A.; Cherria, J.W.; Donaldson, K.; Seaton, A. Ultrafine particles and nitrogen oxides generated by gas and electric cooking. Occup. Environ. Med. 2001, 58, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, D.J.; Adamkiewicz, G.; Heroux, M.E.; Rapp, R.; Kelly, F.J. Nitrogen dioxide. In WHO Guidelines for Indoor Air Quality: Selected Pollutants; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Howden-Chapman, P.; Matheson, A.; Crane, J.; Viggers, H.; Cunningham, M.; Blakely, T.; Cunningham, C.; Woodward, A.; Saville-Smith, K.; O’Dea, D.; et al. Effect of insulating existing houses on health inequality: Cluster randomised study in the community. BMJ 2007, 334, 460. [Google Scholar] [CrossRef] [PubMed]
- Braubach, M.; Heinen, D.; Dame, J. Preliminary Results of the WHO Frankfurt Housing Intervention Project. 2008. Available online: http://www.euro.who.int/__data/assets/pdf_file/0011/98696/E91699.pdf (accessed on 12 November 2014).
- Platt, S.; Mitchell, R.; Petticrew, M.; Walker, J.; Hopton, J.; Corbett, J.; Hope, S.; Martin, C. The Scottish Executive Central Heating Programme: Assessing Impacts on Health. 2007. Available online: http://www.sphsu.mrc.ac.uk/files/File/reports/Heat_Report.pdf (accessed on 12 November 2014).
- Green, G.; Gilbertson, J. Health Impact Evaluation of the Warm Front Scheme. 2008. Available online: http://fuelpoverty.thehealthwell.info/node/3571?&content=resource&member=6744&catalogue=Research%20and%20Evaluation,Report&collection=Fuel%20Poverty&tokens_complete=true (accessed on 12 November 2014).
- Allen, T. Private sector housing improvement in the UK and the chronically ill: Implications for collaborative working. Hous. Stud. 2005, 20, 63–80. [Google Scholar] [CrossRef]
- United States Department of Housing and Urban Development. The Healthy Homes Program Guidance Manual. 2012. Available online: http://portal.hud.gov/hudportal/documents/huddoc?id=hhpgm_final_ch1.pdf (accessed on 12 November 2014). [Google Scholar]
- Krieger, J. Healthy Homes II Asthma Project. 2014. Available online: http://www.kingcounty.gov/healthservices/health/chronic/asthma/past/HH2.aspx (accessed on 12 May 2015). [Google Scholar]
- Colton, M.D.; MacNaughton, P.; Vallarino, J.; Kane, J.; Bennett-Fripp, M.; Spengler, J.D.; Adamkiewicz, G. Indoor air quality in green vs. conventional multifamily low-income housing. Environ. Sci. Technol. 2014, 48, 7833–7841. [Google Scholar] [CrossRef] [PubMed]
| n (%) | |
|---|---|
| Gender | |
| Male Female | 6 (30) 14 (70) |
| Race/Ethnicity | |
| Non-Hispanic Black or African-American Hispanic or Latino | 4 (20) 16 (80) |
| Primary Language Spoken | |
| English Spanish | 10 (50) 10 (50) |
| Household Composition | |
| Households with Children (<18 y/o) Households with Elderly (>60 y/o) Households with Adults only (18–59 y/o) | 11 (55) 7 (35) 2 (10) |
| Age of Survey Participant | |
| 18–30 31–45 46–60 60+ | 2 (10) 3 (15) 8 (40) 7 (35) |
| Annual Household Income | |
| <$10,000 $10,000–$19,999 $20,000–$29,999 $30,000–$39,999 $40,000–$49,999 >$50,000 | 3 (15) 5 (25) 2 (10) 2 (10) 2 (10) 6 (30) |
| Housing—Rent/Own | |
| Private Homeowner Rental Apartment | 10 (50) 10 (50) |
| Health Problems | |
| 0–1 2–3 4+ | 5 (25) 9 (45) 6 (30) |
| Budget Category | Description | Avg. Homeowner | Avg. Renter |
|---|---|---|---|
| Housing | Rent or Mortgage, Insurance, Taxes, etc. | $1,310 | $1,158 |
| Food | Groceries and Eating Out | $389 | $522 |
| Utilities | Electricity and Gas, also Heating Fuel and Water for Homeowners | $393 | $245 |
| Telecommunications/Home * | Phone/Cable/Internet | $308 | $246 |
| Transportation | Public Transportation Costs, Taxis, Automobile Fuel, Automobile Insurance, etc. | $286 | $179 |
| Children | Clothing, School Tuition, Extracurricular Activites, etc. | $133 | $119 |
| Personal Care | Clothing, Haircuts, Manicures/Pedicures, etc. | $83 | $84 |
| Out of Home Entertainment | Movies, Theater, Music, Sporting Events, etc. | $13 | $132 |
| Medical Expenses * | Medical Care and Prescriptions | $53 | $16 |
| Other | Other Expenses, including Charitable Donations, Religious Tithes, Remittances, etc. | $39 | $15 |
| Pets | Food, Medicine, etc. | $3 | $20 |
| Total Monthly Expenses | $2,902 | $2,736 | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández, D.; Phillips, D.; Siegel, E.L. Exploring the Housing and Household Energy Pathways to Stress: A Mixed Methods Study. Int. J. Environ. Res. Public Health 2016, 13, 916. https://doi.org/10.3390/ijerph13090916
Hernández D, Phillips D, Siegel EL. Exploring the Housing and Household Energy Pathways to Stress: A Mixed Methods Study. International Journal of Environmental Research and Public Health. 2016; 13(9):916. https://doi.org/10.3390/ijerph13090916
Chicago/Turabian StyleHernández, Diana, Douglas Phillips, and Eva Laura Siegel. 2016. "Exploring the Housing and Household Energy Pathways to Stress: A Mixed Methods Study" International Journal of Environmental Research and Public Health 13, no. 9: 916. https://doi.org/10.3390/ijerph13090916
APA StyleHernández, D., Phillips, D., & Siegel, E. L. (2016). Exploring the Housing and Household Energy Pathways to Stress: A Mixed Methods Study. International Journal of Environmental Research and Public Health, 13(9), 916. https://doi.org/10.3390/ijerph13090916






