Fuel for Life: Domestic Cooking Fuels and Women’s Health in Rural China
Abstract
:1. Introduction
2. Prior Studies
2.1. Fuel-Based HAP and Respiratory Diseases
2.2. Fuel-Based HAP and Non-Respiratory Diseases
3. Data and Methods
3.1. Study Population
3.2. Health Measures
3.3. Household Cooking Fuels (HCF)
3.4. Independent Variables
3.5. Estimation Approaches
4. Results
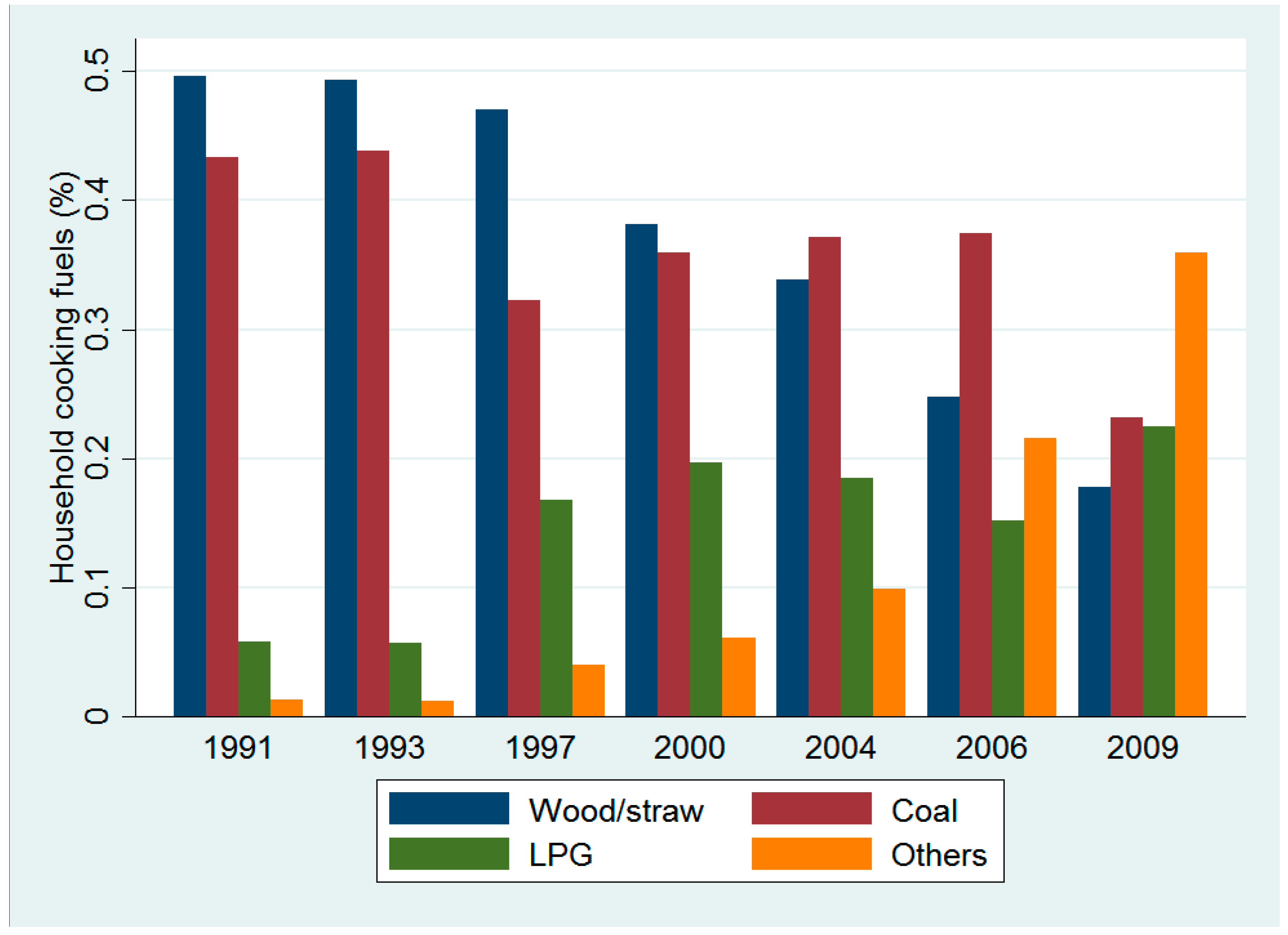
4.1. Descriptive Statistics
4.2. Cross-Sectional Evidence of HCF and Health: The CFPS and the CHNS
4.3. Panel Evidence for HCF and Health: The CFPS
4.4. Panel Evidence for HCF and Health: The CHNS
4.5. HCF and Major Risk Predictors of Cardiovascular Diseases (CVD): The CHNS
4.6. HCF and Specific Symptoms of Chronic or Acute Diseases
5. Discussion
5.1. Key Findings
5.2. Limitations
5.3. Future Research Directions
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Independent Variables | Definitions |
|---|---|
| Individual characteristics | |
| Age | Years of age |
| Working status | 1, if the respondent is currently employed and 0 otherwise. |
| Education levels | Measured on a 6-point scale recoded as a dummy variable: 1 = illiterate, 2 = primary school, 3 = middle school, 4 = high school, 5 = vocational school and 6 = university or higher. |
| Marital status | 1, if the respondent is married/living together with a partner and 0 if the respondent is divorced/separated/widowed. |
| Currently smoking | 1, if the respondent has smoked in the past month and 0 otherwise. |
| Time spent cooking | In the CHNS, based on the interview question: “During the previous week, how much time (in hours) did you spend per day, on average, cooking food for the household?”. |
| Family characteristics | |
| Household cooking fuels | Measured on a 3-point scale, 0 = wood/straw, 1 = coal and 2 = liquefied petroleum gas (LPG), based on the interview question: “What kind of fuel does you household normally use for cooking?”. |
| Household income | Total amount of household income (in Yuan, adjusted to 2012 in the CFPS and to 2011 in the CHNS). |
| Household size | Number of people in the household. |
| Drinking water | In the CFPS, 1 if the household’s drinking source is tap water or mineral/purified water, 0 otherwise. In the CHNS, 1 if the household’s water source is a water plant or ground water above 5 m deep, 0 otherwise. |
| Electricity | In the CFPS, 1 if the household has occasional or no power outage, 0 otherwise. In the CHNS, 1 if electric facilities are accessible for the household, 0 otherwise. |
| Flushing toilet | In the CFPS, 1 if the household mostly use an indoor/outdoor flushing toilet, 0 otherwise. In the CHNS, 1 if the household can access an in-house/out-house flushing toilet facility, 0 otherwise. |
| Clean trash treatment | In the CFPS, 1 if the household dumps the trash in the public dustbin/garbage can, 0 otherwise. |
| Existence of excreta | In the CHNS, 1 if there is no excreta around the dwelling place, 0 otherwise. |
| Community Characteristics | |
| Location of ealth facility | In the CHNS, the availability of health facilities in the community is defined by a dummy variable equal to 1 if a health facility is located in the village/neighbourhood and 0 if in another village/town/city or in the respondent’s city but in a different neighbourhood. |
| Distance to the health facility | Distance (in km) in the community to the nearest health facility like hospital/medical center. |
| Health Measures | Description | Definition | Data Source | Years | Methodology |
|---|---|---|---|---|---|
| Self-reported acute/chronic disease | Have you felt any physical discomfort during the preceding two weeks? | A binary variable equal to 1 if the respondent has felt discomfort, and 0 otherwise. | CFPS | 2010–2012 | Probit model Random effect probit model |
| Have you suffered from a chronic or acute disease during the past 4 weeks? | A dummy that equals 1 if the respondent has suffered from a chronic or acute disease, and 0 otherwise. | CHNS | 1991–2009 | Probit model Random effect probit model | |
| Self-reported health (SRH) | How would you rate your health status? 1 = excellent, 2 = very good, 3 = good, 4 = fair and 5 = poor. | A 5-point scale ranging from 1 = poor to 5 = excellent. | CFPS | 2010–2012 | Ordered probit model Random effect ordered probit model |
| Right now, how would you describe your health compared to that of other people your age? 1 = bad; 2 = fair; 3 = good; 4 = excellent. | A 4-point scale ranging from 1 = bad to 4 = excellent. | CHNS | 1997–2006 | Ordered probit model Random effect ordered probit model | |
| Systolic blood pressure (SBP) | Measurements are taken three times by a health professional using a mercury sphygmomanometer. | The average value of SBP based on the second and third measurements. | CHNS | 1991–2009 | Ordinary least squares model Fixed effect model |
| Diastolic blood pressure (DBP) | Measurements are taken three times by a health professional using a mercury sphygmomanometer. | The average value of SBP based on the second and third measurements. | CHNS | 1991–2009 | Ordinary least square model Fixed effect model |
| Inflammation | Using high sensitivity C-reactive protein. | A dummy equal to 1 if the high sensitivity C-reactive protein exceeds 3 mg/dL, 0 otherwise. | CHNS | 2009 | Probit model |
| Variable | CFPS | CHNS | ||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| 16–50 | 50+ | 16–50 | 50+ | |
| Coal | 0.010 | 0.027 ** | 0.016 | 0.003 |
| (0.015) | (0.012) | (0.012) | (0.006) | |
| 95% CI | [−0.020, 0.039] | [0.004, 0.050] | [−0.008, 0.041] | [−0.009, 0.015] |
| LPG | 0.025 ** | 0.035 *** | 0.014 | 0.022 *** |
| (0.012) | (0.011) | (0.013) | (0.007) | |
| 95% CI | [0.002, 0.048] | [0.014, 0.056] | [−0.011, 0.038] | [0.008, 0.037] |
| N | 7958 | 4945 | 5107 | 3302 |
| Pseudo R2 | 0.140 | 0.109 | 0.052 | 0.042 |
| Variable | Random Effects Ordered Probit: 16–50 | Random Effects Ordered Probit: 50+ |
|---|---|---|
| Coal | 0.021 | 0.024 * |
| (0.016) | (0.013) | |
| 95% CI | [−0.011, 0.052] | [−0.001, 0.048] |
| LPG | 0.012 | 0.027 *** |
| (0.011) | (0.009) | |
| 95% CI | [−0.010, 0.033] | [0.009, 0.046] |
| N | 6011 | 3989 |
| Variable | Chronic/Acute Disease | Self-Reported Health (Excellent) |
|---|---|---|
| Random Effects Probit | Random Effects Ordered Probit | |
| Coal | −0.007 | 0.002 |
| (0.006) | (0.005) | |
| 95% CI | [−0.019, 0.005] | [−0.008, 0.012] |
| LPG | −0.013 | 0.022 *** |
| (0.009) | (0.006) | |
| 95% CI | [−0.029, 0.004] | [0.009, 0.034] |
| 1 ≤ TSC < 2 h/day | −0.003 | −0.005 |
| (0.008) | (0.006) | |
| 95% CI | [−0.018, 0.012] | [−0.016, 0.006] |
| 2 ≤ TSC < 3 h/day | −0.011 | 0.003 |
| (0.008) | (0.006) | |
| 95% CI | [−0.027, 0.005] | [−0.010, 0.015] |
| TSC ≥ 3 h/day | −0.012 | −0.011 |
| (0.009) | (0.008) | |
| 95% CI | [−0.029, 0.006] | [−0.026, 0.004] |
| Number of surveyed years | 0.001 | −0.0005 |
| (0.002) | (0.002) | |
| 95% CI | [−0.003, 0.005] | [−0.004, 0.003] |
| N | 10,090 | 7023 |
| Variable | Random Effects Ordered Probit: 16–50 | Random Effects Ordered Probit: 50+ |
|---|---|---|
| Coal | −0.001 | 0.005 |
| (0.009) | (0.004) | |
| 95% CI | [−0.019, 0.017] | [−0.004, 0.013] |
| LPG | 0.020 * | 0.020 *** |
| (0.011) | (0.006) | |
| 95% CI | [−0.002, 0.041] | [0.008, 0.031] |
| 1 ≤ TSC < 2 h/day | 0.001 | −0.007 |
| (0.010) | (0.005) | |
| 95% CI | [−0.019, 0.020] | [−0.016, 0.003] |
| 2 ≤ TSC < 3 h/day | 0.007 | −0.001 |
| (0.011) | (0.005) | |
| 95% CI | [−0.015, 0.029] | [−0.012, 0.009] |
| TSC ≥ 3 h/day | −0.001 | −0.014 ** |
| (0.013) | (0.007) | |
| 95% CI | [−0.027, 0.026] | [−0.028, −0.001] |
| N | 4085 | 2938 |
References
- United Nations Development Group. A Million Voices: The World We Want; United Nations Development Group: New York, NY, USA, 2013. [Google Scholar]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Reid, B.C.; Ghazarian, A.A.; DeMarini, D.M.; Sapkota, A.; Jack, D.; Lan, Q.; Winn, D.M.; Birnbaum, L.S. Research opportunities for cancer associated with indoor air pollution from solid-fuel combustion. Environ. Health Perspect. 2012, 120, 1495–1498. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Jiang, Y.; Wang, B.; Zhao, X.; Shen, G.; Cao, S.; Huang, N.; Qian, Y.; Chen, Y.; Wang, L. Household fuel use for cooking and heating in China: Results from the first Chinese environmental exposure-related human activity patterns survey (CEERHAPS). Appl. Energy 2014, 136, 692–703. [Google Scholar] [CrossRef]
- Zhang, Y.B.; Wu, Y. China—Health Impacts of Indoor Air Pollution: At a Glance. East Asia and Pacific (EAP) Clean Stove Initiative Knowledge Exchange Series; World Bank: Washington, DC, USA, 2012. [Google Scholar]
- Zhang, J.J.; Smith, K.R. Household air pollution from coal and biomass fuels in China: Measurements, health impacts, and interventions. Environ. Health Perspect. 2007, 115, 848–855. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; United Nations Development Programme. The Energy Access Situation in Developing Countries; United Nations Development Programme: New York, NY, USA, 2009. [Google Scholar]
- Baumgartner, J.; Schauer, J.J.; Ezzati, M.; Lu, L.; Cheng, C.; Patz, J.A.; Bautista, L.E. Indoor air pollution and blood pressure in adult women living in rural China. Environ. Health Perspect. 2011, 119, 1390–1395. [Google Scholar] [CrossRef] [PubMed]
- Finkelman, R.B.; Belkin, H.E.; Zheng, B. Health impacts of domestic coal use in China. Proc. Natl. Acad. Sci. USA 1999, 96, 3427–3431. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.Y.; Wu, M.; Han, R.Q.; Zhang, X.F.; Wang, X.S.; Liu, A.M.; Zhou, J.Y.; Lu, Q.Y.; Kim, C.H.; Mu, L.; et al. Household ventilation may reduce effects of indoor air pollutants for prevention of lung cancer: A case-control study in a Chinese population. PLoS ONE 2014. [Google Scholar] [CrossRef] [PubMed]
- Kan, X.; Chiang, C.Y.; Enarson, D.A.; Chen, W.; Yang, J.; Chen, G. Indoor solid fuel use and tuberculosis in China: A matched case-control study. BMC Public Health 2011. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Zheng, L.; Duzgoren-Aydin, N.; Gao, L.; Liu, J.; Peng, Z. Health effects of arsenic, fluorine, and selenium from indoor burning of Chinese coal. In Reviews of Environmental Contamination and Toxicology; Whitacre, D., Ware, G., Nigg, H., Doerge, D., Albert, L., de Voogt, P., Gerba, C., Hutzinger, O., Knaak, J., Mayer, F., et al., Eds.; Springer: New York, NY, USA, 2007; pp. 89–106. [Google Scholar]
- Peabody, J.W.; Riddell, T.J.; Smith, K.R.; Liu, Y.; Zhao, Y.; Gong, J.; Milet, M.; Sinton, J.E. Indoor air pollution in rural China: Cooking fuels, stoves, and health status. Arch. Environ. Occup. Health 2005, 60, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.R.; Mehta, S.; Maeusezahl-Feuz, M. Indoor air pollution from household use of solid fuels. In Comparative Quantification of Health Risks; Ezzati, M., Lopez, A.D., Rodgers, A., Murray, C.J.L., Eds.; World Health Organization: Geneva, Switzerland, 2004; pp. 1435–1493. [Google Scholar]
- Zhao, Y.; Wang, S.; Aunan, K.; Seip, H.M.; Hao, J. Air pollution and lung cancer risks in China—A meta-analysis. Sci. Total Environ. 2006, 366, 500–513. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, D.G.; Bruce, N.; Gordon, S.B. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Zhou, Y.; Wang, X.; Wang, D.; Lu, J.; Zheng, J.; Zhong, N.; Ran, P. Biomass fuels are the probable risk factor for chronic obstructive pulmonary disease in rural South China. Thorax 2007, 62, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.C.; Dong, Z.; Wang, L.; Yue, W. An evaluation of the indoor/outdoor air pollution and respiratory health of farmers living in rural areas of Anhui Province, China. In Proceedings of the Indoor Air 2002, Monterey, CA, USA, 30 June–5 July 2002; International Academy of Indoor Air Sciences: Monterey, CA, USA, 2002. [Google Scholar]
- Bentayeb, M.; Simoni, M.; Norback, D.; Baldacci, S.; Maio, S.; Viegi, G.; Annesi-Maesano, I. Indoor air pollution and respiratory health in the elderly. J. Environ. Sci. Health A Tox. Hazard. Subst. Environ. Eng. 2013, 48, 1783–1789. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Yin, X.; Shen, H.; Xu, Y.; Ware, R.S.; Owen, N. Better understanding the influence of cigarette smoking and indoor air pollution on chronic obstructive pulmonary disease: A case-control study in Mainland China. Respirology 2007, 12, 891–897. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.H.; Suk, C.W.; Lo, H.L.; Huang, R.Y.; Enarson, D.A.; Chiang, C.Y. Indoor air pollution from solid fuel and tuberculosis: A systematic review and meta-analysis. Int. J. Tuberc. Lung Dis. 2014, 18, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zheng, R.; Zeng, H.; Zhang, S. The epidemiology of lung cancer. J. Cancer Biol. Res. 2014, 2, 1043. [Google Scholar]
- She, J.; Yang, P.; Hong, Q.; Bai, C. Lung cancer in China: Challenges and interventions. Chest 2013, 143, 1117–1126. [Google Scholar] [CrossRef] [PubMed]
- Kurmi, O.P.; Arya, P.H.; Lam, K.B.; Sorahan, T.; Ayres, J.G. Lung cancer risk and solid fuel smoke exposure: A systematic review and meta-analysis. Eur. Respir. J. 2012, 40, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Gao, Y.T.; Xiang, Y.B.; Barone-Adesi, F.; Zhang, Y.; Hosgood, H.D.; Ma, S.; Shu, X.O.; Ji, B.T.; Chow, W.H.; et al. Home kitchen ventilation, cooking fuels, and lung cancer risk in a prospective cohort of never smoking women in Shanghai, China. Int. J. Cancer 2014, 136, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Barone-Adesi, F.; Chapman, R.S.; Silverman, D.T.; He, X.; Hu, W.; Vermeulen, R.; Ning, B.; Fraumeni, J.F., Jr.; Rothman, N.; Lan, Q. Risk of lung cancer associated with domestic use of coal in Xuanwei, China: Retrospective cohort study. BMJ 2012, 345, e5414. [Google Scholar] [CrossRef] [PubMed]
- Jie, Y.; Houjin, H.; Xun, M.; Kebin, L.; Xuesong, Y.; Jie, X. Relationship between pulmonary function and indoor air pollution from coal combustion among adult residents in an inner-city area of southwest China. Braz. J. Med. Biol. Res. 2014, 47, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Zhou, X.; He, X. Study on effect of indoor pollutants of lung functionalities from combustion of fuel. China Public Health 1995, 11, 18–19. [Google Scholar]
- Zhou, B.S.; Wang, T.J.; Guan, P.; Wu, J.M. Indoor air pollution and pulmonary adenocarcinoma among females: A case-control study in Shenyang, China. Oncol. Rep. 2000, 7, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zou, Y.; Li, X.; Chen, S.; Zhao, Z.; He, F.; Zou, W.; Luo, Q.; Li, W.; Pan, Y.; et al. Lung function and incidence of chronic obstructive pulmonary disease after improved cooking fuels and kitchen ventilation: A 9-year prospective cohort study. PLoS Med. 2014, 11, e1001621. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, J.; Zhang, Y.; Schauer, J.J.; Huang, W.; Wang, Y.; Ezzati, M. Highway proximity and black carbon from cookstoves as a risk factor for higher blood pressure in rural China. Proc. Natl. Acad. Sci. USA 2014, 111, 13229–13234. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Hang, J.Q.; Zhang, F.Y.; Dai, H.L.; Su, L.; Christiani, D.C. In-home solid fuel use and cardiovascular disease: A cross-sectional analysis of the Shanghai Putuo study. Environ. Health 2012, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shraim, A.; Cui, X.; Li, S.; Ng, J.C.; Wang, J.; Jin, Y.; Liu, Y.; Guo, L.; Li, D.; Wang, S.; et al. Arsenic speciation in the urine and hair of individuals exposed to airborne arsenic through coal-burning in Guizhou, PR China. Toxicol. Lett. 2003, 137, 35–48. [Google Scholar] [CrossRef]
- Li, D.S.; An, D.; Zhou, Y.S.; Liu, J.; Waalkes, M.P. Current status and prevention strategy for coal-arsenic poisoning in Guizhou, China. J. Health Popul. Nutr. 2006, 24, 273–276. [Google Scholar] [PubMed]
- Zheng, B.S.; Wang, B.B.; Ding, Z.H.; Zhou, D.X.; Zhou, Y.S.; Chen, Z.; Chen, C.C.; Finkelman, R.B. Endemic arsenosis caused by indoor combustion of high-as coal in Guizhou Province, P.R. China. Environ. Geochem. Health 2005, 27, 521–528. [Google Scholar]
- Li, C.; Ma, H.L. Risk factors of non-occupational carbon monoxide poisoning during the 2008 ice storm in Guiyang county, Hunan province, China. Public Health Rep. 2010, 125, 605–610. [Google Scholar]
- Mackay, J.; Mensa, G.A. The Atlas of Heart Disease and Stroke; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Xie, Y.; Hu, J.; Zhang, C. The China Family Panel Studies (CFPS): Design and practice. Chin. J. Sociol. 2014, 34, 1–33. [Google Scholar]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China health and nutrition survey, 1989–2011. Obes. Rev. 2014, 15, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Xie, S.; Mo, T. The impact of education on health in China. China Econ. Rev. 2014, 29, 1–18. [Google Scholar] [CrossRef]
- Lei, X.; Yin, N.; Zhao, Y. Socioeconomic status and chronic diseases: The case of hypertension in China. China Econ. Rev. 2012, 23, 105–121. [Google Scholar] [CrossRef]
- Pearson, T.A.; Mensah, G.A.; Hong, Y.; Smith, S.C. CDC/AHA workshop on markers of inflammation and cardiovascular disease: Application to clinical and public health practice: Overview. Circulation 2004, 110, e543–e544. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Li, J.; Li, S.; Zhang, B.; Du, S.; Gordon-Larsen, P.; Adair, L.; Popkin, B. The expanding burden of cardiometabolic risk in China: The China health and nutrition survey. Obes. Rev. 2012, 13, 810–821. [Google Scholar] [CrossRef] [PubMed]
- Mestl, H.E.; Edwards, R. Global burden of disease as a result of indoor air pollution in Shaanxi, Hubei and Zhejiang, China. Sci. Total Environ. 2011, 409, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, M.; Nijman, T. Testing for selectivity bias in panel data models. Int. Econ. Rev. 1992, 33, 681–703. [Google Scholar] [CrossRef]
- Gordon-Larsen, P.; Adair, L.S.; Meigs, J.B.; Mayer-Davis, E.; Herring, A.; Yan, S.K.; Zhang, B.; Du, S.; Popkin, B.M. Discordant risk: Overweight and cardiometabolic risk in Chinese adults. Obesity 2013, 21, e166–e174. [Google Scholar] [CrossRef] [PubMed]
- Barregard, L.; Sällsten, G.; Gustafson, P.; Andersson, L.; Johansson, L.; Basu, S.; Stigendal, L. Experimental exposure to wood-smoke particles in healthy humans: Effects on markers of inflammation, coagulation, and lipid peroxidation. Inhal. Toxicol. 2006, 18, 845–853. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A.I.; Dockery, D.W. Health effects of fine particulate air pollution: Lines that connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef] [PubMed]
- Bautista, L.E.; Vera, L.M.; Arenas, I.A.; Gamarra, G. Independent association between inflammatory markers (C-reactive protein, interleukin-6, and TNF-(alpha)) and essential hypertension. J. Hum. Hypertens. 2004, 19, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Bruce, N.; Perez-Padilla, R.; Albalak, R. Indoor air pollution in developing countries: A major environmental and public health challenge. Bull. World Health Organ. 2000, 78, 1078–1092. [Google Scholar] [PubMed]
- Zhang, J.; Wang, L.; Liu, J.; Zhou, Y.; Wen, T.; Meng, D. 24-h NO2 level in kitchen air and 24-hour NO2 personal exposure level and its effect on urinary HOP. Environ. Health 1996, 13, 193–196. [Google Scholar]
- Duflo, E.; Greenstone, M.; Hanna, R. Indoor air pollution, health and economic well-being. Surv. Perspect. Integr. Environ. Soc. 2008, 1, 1–9. [Google Scholar] [CrossRef]
- Sinton, J.E.; Smith, K.R.; Peabody, J.W.; Liu, Y.P.; Zhang, X.L.; Edwards, R.; Gan, Q. An assessment of programs to promote improved household stoves in China. Energy Sustain. Dev. 2004, 8, 33–52. [Google Scholar] [CrossRef]
- Baumgartner, J.; Smith, K.R.; Chockalingam, A. Reducing CVD through improvements in household energy. Glob. Heart 2012, 7, 243–247. [Google Scholar] [CrossRef] [PubMed]
- McCracken, J.P.; Wellenius, G.A.; Bloomfield, G.S.; Brook, R.D.; Tolunay, H.E.; Dockery, D.W.; Rabadan-Diehl, C.; Checkley, W.; Rajagopalan, S. Household air pollution from solid fuel use: Evidence for links to CVD. Glob. Heart 2012, 7, 223–234. [Google Scholar] [CrossRef] [PubMed]
| Variable | N | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| Dependent variable | |||||
| Chronic/acute disease | 12,901 | 0.347 | 0.476 | 0 | 1 |
| Fever | 12,901 | 0.022 | 0.147 | 0 | 1 |
| Pain | 12,901 | 0.156 | 0.363 | 0 | 1 |
| Cough | 12,901 | 0.015 | 0.121 | 0 | 1 |
| Palpitation | 12,901 | 0.033 | 0.177 | 0 | 1 |
| Self-reported health (SRH) | |||||
| Poor | 12,901 | 0.146 | 0.353 | 0 | 1 |
| Fair | 12,901 | 0.154 | 0.361 | 0 | 1 |
| Good | 12,901 | 0.171 | 0.376 | 0 | 1 |
| Very good | 12,901 | 0.262 | 0.440 | 0 | 1 |
| Excellent | 12,901 | 0.267 | 0.443 | 0 | 1 |
| Household cooking fuels | |||||
| Wood/straw | 12,901 | 0.637 | 0.481 | 0 | 1 |
| Coal | 12,901 | 0.106 | 0.308 | 0 | 1 |
| liquefied petroleum gas (LPG) | 12,901 | 0.257 | 0.437 | 0 | 1 |
| Individual characteristics | |||||
| Age | 12,901 | 46.059 | 16.053 | 16 | 97 |
| Working status | 12,901 | 0.490 | 0.500 | 0 | 1 |
| Education levels | |||||
| Illiterate | 12,901 | 0.516 | 0.500 | 0 | 1 |
| Primary school | 12,901 | 0.220 | 0.414 | 0 | 1 |
| Middle school | 12,901 | 0.194 | 0.395 | 0 | 1 |
| High school | 12,901 | 0.052 | 0.223 | 0 | 1 |
| Vocational school | 12,901 | 0.012 | 0.110 | 0 | 1 |
| University or higher | 12,901 | 0.005 | 0.073 | 0 | 1 |
| Marital status | 12,901 | 0.834 | 0.372 | 0 | 1 |
| Currently smoking | 12,901 | 0.039 | 0.195 | 0 | 1 |
| Family characteristics | |||||
| Household income (log) | 12,901 | 9.877 | 1.148 | 0.693 | 14.253 |
| Household size | 12,901 | 4.674 | 1.922 | 1 | 26 |
| Drinking water | 12,901 | 0.421 | 0.494 | 0 | 1 |
| Electricity | 12,901 | 0.944 | 0.230 | 0 | 1 |
| Flushing toilet | 12,901 | 0.209 | 0.407 | 0 | 1 |
| Clean trash treatment | 12,901 | 0.148 | 0.355 | 0 | 1 |
| Community Characteristics | |||||
| Distance to the health facility (km) | 12,901 | 1.247 | 1.670 | 0.001 | 9.500 |
| Variable | N | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| Dependent variable | |||||
| Chronic/acute disease | 15,539 | 0.109 | 0.311 | 0 | 1 |
| Fever | 15,539 | 0.046 | 0.210 | 0 | 1 |
| Asthma | 1078 | 0.001 | 0.031 | 0 | 1 |
| Eye disease | 15,539 | 0.004 | 0.066 | 0 | 1 |
| Heart disease/chest pain | 15,539 | 0.009 | 0.092 | 0 | 1 |
| Self-reported health (SRH) | |||||
| Bad | 8409 | 0.070 | 0.256 | 0 | 1 |
| Fair | 8409 | 0.317 | 0.465 | 0 | 1 |
| Good | 8409 | 0.492 | 0.500 | 0 | 1 |
| Excellent | 8409 | 0.121 | 0.326 | 0 | 1 |
| Household cooking fuels | |||||
| Wood/straw | 15,539 | 0.409 | 0.492 | 0 | 1 |
| Coal | 15,539 | 0.420 | 0.494 | 0 | 1 |
| liquefied petroleum gas (LPG) | 15,539 | 0.171 | 0.377 | 0 | 1 |
| Individual characteristics | |||||
| Age | 15539 | 44.959 | 15.728 | 16 | 97.84 |
| Working status | 15539 | 0.705 | 0.456 | 0 | 1 |
| Education levels | |||||
| Illiterate | 15,539 | 0.300 | 0.458 | 0 | 1 |
| Primary school | 15,539 | 0.337 | 0.473 | 0 | 1 |
| Middle school | 15,539 | 0.263 | 0.440 | 0 | 1 |
| High school | 15,539 | 0.073 | 0.260 | 0 | 1 |
| Vocational school | 15,539 | 0.020 | 0.140 | 0 | 1 |
| University or higher | 15,539 | 0.007 | 0.083 | 0 | 1 |
| Marital status | 15,539 | 0.799 | 0.400 | 0 | 1 |
| Currently smoking | 15,539 | 0.037 | 0.189 | 0 | 1 |
| Time spent cooking (hours/day) | 10,227 | 1.728 | 0.932 | 0.017 | 4.667 |
| Family characteristics | |||||
| Household income (log) | 15,539 | 9.390 | 1.011 | 1.156 | 13.414 |
| Household size | 15,539 | 4.198 | 1.591 | 1 | 13 |
| Water | 15,539 | 0.827 | 0.378 | 0 | 1 |
| Flushing toilet | 15,539 | 0.207 | 0.405 | 0 | 1 |
| No excreta around the dwelling place | 15,539 | 0.568 | 0.495 | 0 | 1 |
| Electricity | 15,539 | 0.984 | 0.127 | 0 | 1 |
| Community characteristics | |||||
| Location of health facility | 15,539 | 0.752 | 0.432 | 0 | 1 |
| Distance to the health facility (km) | 15,539 | 0.923 | 3.573 | 0 | 60 |
| Variable | CFPS | CHNS | ||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Chronic/Acute Disease | Self-Reported Health (Excellent) | Chronic/Acute Disease | Self-Reported Health (Excellent) | |
| Coal | 0.010 | 0.019 * | −0.008 | 0.009 |
| (0.020) | (0.011) | (0.008) | (0.007) | |
| 95% CI | [−0.030, 0.050] | [−0.002, 0.040] | [−0.025, 0.008] | [−0.005, 0.023] |
| LPG | −0.044 *** | 0.029 *** | −0.009 | 0.021 *** |
| (0.015) | (0.009) | (0.010) | (0.008) | |
| 95% CI | [−0.075, −0.014] | [0.012, 0.046] | [−0.028, 0.010] | [0.006, 0.037] |
| N | 12,901 | 12,901 | 15,539 | 8409 |
| Pseudo R2 | 0.065 | 0.147 | 0.090 | 0.081 |
| Variable | Random Effects Probit (1) Chronic/Acute Disease | Random Effects Ordered Probit (2) Self-Reported Health (Excellent) |
|---|---|---|
| Coal | −0.006 | 0.023 ** |
| (0.020) | (0.010) | |
| 95% CI | [−0.046, 0.034] | [0.003, 0.044] |
| LPG | −0.052 *** | 0.020 *** |
| (0.015) | (0.007) | |
| 95% CI | [−0.081, −0.024] | [0.006, 0.035] |
| N | 9770 | 10,000 |
| Variable | Random Effects Probit (1) Chronic/Acute Disease | Random Effects Ordered Probit (2) Self-Reported Health (Excellent) |
|---|---|---|
| Coal | −0.007 | 0.002 |
| (0.006) | (0.005) | |
| 95% CI | [−0.019, 0.005] | [−0.008, 0.012] |
| LPG | −0.013 | 0.022 *** |
| (0.008) | (0.006) | |
| 95% CI | [−0.030, 0.004] | [0.009, 0.034] |
| 1 ≤ TSC < 2 h/day | −0.003 | −0.005 |
| (0.008) | (0.006) | |
| 95% CI | [−0.018, 0.011] | [−0.016, 0.006] |
| 2 ≤ TSC < 3 h/day | −0.011 | 0.003 |
| (0.008) | (0.006) | |
| 95% CI | [−0.027, 0.005] | [−0.010, 0.015] |
| TSC ≥ 3 h/day | −0.012 | −0.011 |
| (0.009) | (0.008) | |
| 95% CI | [−0.029, 0.006] | [−0.026, 0.004] |
| N | 10,090 | 7023 |
| Variable | OLS Estimate | Probit Estimate | |||
|---|---|---|---|---|---|
| 16–50 | 50+ | 16–50 | 50+ | ||
| Systolic Blood Pressure | Diastolic Blood Pressure | Inflammation | |||
| (1) | (2) | (3) | (4) | (5) | |
| Coal | 0.110 | 2.295 * | 0.567 | 0.957 | 0.025 |
| (0.703) | (1.282) | (0.453) | (0.760) | (0.032) | |
| 95% CI | [−1.279, 1.499] | [−0.239, 4.829] | [−0.329, 1.462] | [−0.545, 2.459] | [−0.037, 0.088] |
| LPG | 0.345 | 0.936 | 0.512 | 0.873 | 0.021 |
| (0.750) | (1.427) | (0.480) | (0.841) | (0.032) | |
| 95% CI | [−1.138, 1.828] | [−1.883, 3.755] | [−0.437, 1.460] | [−0.789, 2.535] | [−0.041, 0.083] |
| N | 6389 | 3838 | 6389 | 3838 | 1637 |
| Pseudo/Adjusted R2 | 0.146 | 0.109 | 0.128 | 0.062 | 0.058 |
| Variable | Systolic Blood Pressure | Diastolic Blood Pressure | ||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| 16–50 | 50+ | 16–50 | 50+ | |
| Coal | −0.599 | 2.267 * | 0.288 | 0.079 |
| (0.669) | (1.229) | (0.481) | (0.707) | |
| 95% CI | [−1.910, 0.713] | [−0.144, 4.677] | [−0.655, 1.232] | [−1.308, 1.466] |
| LPG | −0.131 | −0.573 | 0.654 | −0.215 |
| (0.768) | (1.438) | (0.553) | (0.827) | |
| 95% CI | [−1.637, 1.375] | [−3.392, 2.246] | [−0.430, 1.738] | [−1.838, 1.407] |
| 1 ≤ TSC < 2 h/day | 0.524 | 1.536 | 1.076 ** | −0.111 |
| (0.612) | (1.006) | (0.440) | (0.579) | |
| 95% CI | [−0.676, 1.724] | [−0.435, 3.508] | [0.212, 1.940] | [−1.246, 1.023] |
| 2 ≤ TSC < 3 h/day | −0.036 | 1.731 | 0.920 * | −0.110 |
| (0.664) | (1.129) | (0.478) | (0.649) | |
| 95% CI | [−1.337, 1.265] | [−0.483, 3.944] | [−0.016, 1.857] | [−1.384, 1.164] |
| TSC ≥ 3 h/day | −1.064 | 2.603 ** | −0.008 | 0.417 |
| (0.726) | (1.300) | (0.523) | (0.748) | |
| 95% CI | [−2.488, 0.359] | [0.055, 5.152] | [−1.033, 1.017] | [−1.049, 1.884] |
| N | 6252 | 3838 | 6252 | 3838 |
| R2 | 0.088 | 0.102 | 0.066 | 0.028 |
| CFPS | ||||
| Variable | Fever | Cough | Pain | Palpitation |
| Coal | −0.003 | 0.003 | 0.007 | 0.006 |
| (0.005) | (0.004) | (0.015) | (0.005) | |
| 95% CI | [−0.013, 0.007] | [−0.005, 0.010] | [−0.021, 0.036] | [−0.003, 0.016] |
| LPG | 0.001 | 0.003 | −0.018 | −0.008 * |
| (0.004) | (0.003) | (0.012) | (0.004) | |
| 95% CI | [−0.006, 0.008] | [−0.003, 0.009] | [−0.041, 0.005] | [−0.017, 0.0003] |
| N | 12,637 | 12,623 | 12,901 | 12,901 |
| Pseudo R2 | 0.023 | 0.031 | 0.059 | 0.072 |
| CHNS | ||||
| Variable | Fever/Cough | Asthma | Eye | Heart/Chest Pain |
| Coal | −0.003 | −0.007 | −0.003 * | 0.004 * |
| (0.005) | (0.007) | (0.002) | (0.002) | |
| 95% CI | [−0.013, 0.007] | [−0.021, 0.006] | [−0.006, 0.0002] | [−0.0004, 0.008] |
| LPG | −0.001 | −0.007 | −0.004 ** | 0.003 |
| (0.006) | (0.010) | (0.002) | (0.002) | |
| 95% CI | [−0.012, 0.010] | [−0.027, 0.013] | [−0.008, −0.001] | [−0.002, 0.008] |
| N | 15,539 | 1078 | 14,299 | 15,539 |
| Pseudo R2 | 0.081 | 0.297 | 0.208 | 0.172 |
| CFPS | ||||
| Variable | Fever | Cough | Pain | Palpitation |
| Coal | −0.002 | 0.003 | 0.001 | 0.003 |
| (0.004) | (0.002) | (0.001) | (0.003) | |
| 95% CI | [−0.010, 0.007] | [−0.002, 0.007] | [−0.002, 0.004] | [−0.002, 0.008] |
| LPG | 0.002 | −0.002 | 0.002 | −0.003 |
| (0.003) | (0.002) | (0.001) | (0.002) | |
| 95% CI | [−0.004, 0.007] | [−0.006, 0.001] | [−0.001, 0.004] | [−0.007, 0.001] |
| N | 10,002 | 10,002 | 10,002 | 10,002 |
| CHNS | ||||
| Variable | Fever | Eye | Heart/Chest Pain | |
| Coal | −0.008 * | −0.001 | 0.001 | |
| (0.004) | (0.001) | (0.001) | ||
| 95% CI | [−0.017, 0.00004] | [−0.003, 0.001] | [−0.001, 0.003] | |
| LPG | −0.012 ** | −0.001 | 0.001 | |
| (0.006) | (0.001) | (0.001) | ||
| 95% CI | [−0.024, −0.0003] | [−0.003, 0.001] | [−0.002, 0.003] | |
| N | 10,090 | 10,090 | 10,090 | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nie, P.; Sousa-Poza, A.; Xue, J. Fuel for Life: Domestic Cooking Fuels and Women’s Health in Rural China. Int. J. Environ. Res. Public Health 2016, 13, 810. https://doi.org/10.3390/ijerph13080810
Nie P, Sousa-Poza A, Xue J. Fuel for Life: Domestic Cooking Fuels and Women’s Health in Rural China. International Journal of Environmental Research and Public Health. 2016; 13(8):810. https://doi.org/10.3390/ijerph13080810
Chicago/Turabian StyleNie, Peng, Alfonso Sousa-Poza, and Jianhong Xue. 2016. "Fuel for Life: Domestic Cooking Fuels and Women’s Health in Rural China" International Journal of Environmental Research and Public Health 13, no. 8: 810. https://doi.org/10.3390/ijerph13080810
APA StyleNie, P., Sousa-Poza, A., & Xue, J. (2016). Fuel for Life: Domestic Cooking Fuels and Women’s Health in Rural China. International Journal of Environmental Research and Public Health, 13(8), 810. https://doi.org/10.3390/ijerph13080810







