Respiratory Health in Waste Collection and Disposal Workers
Abstract
:1. Introduction
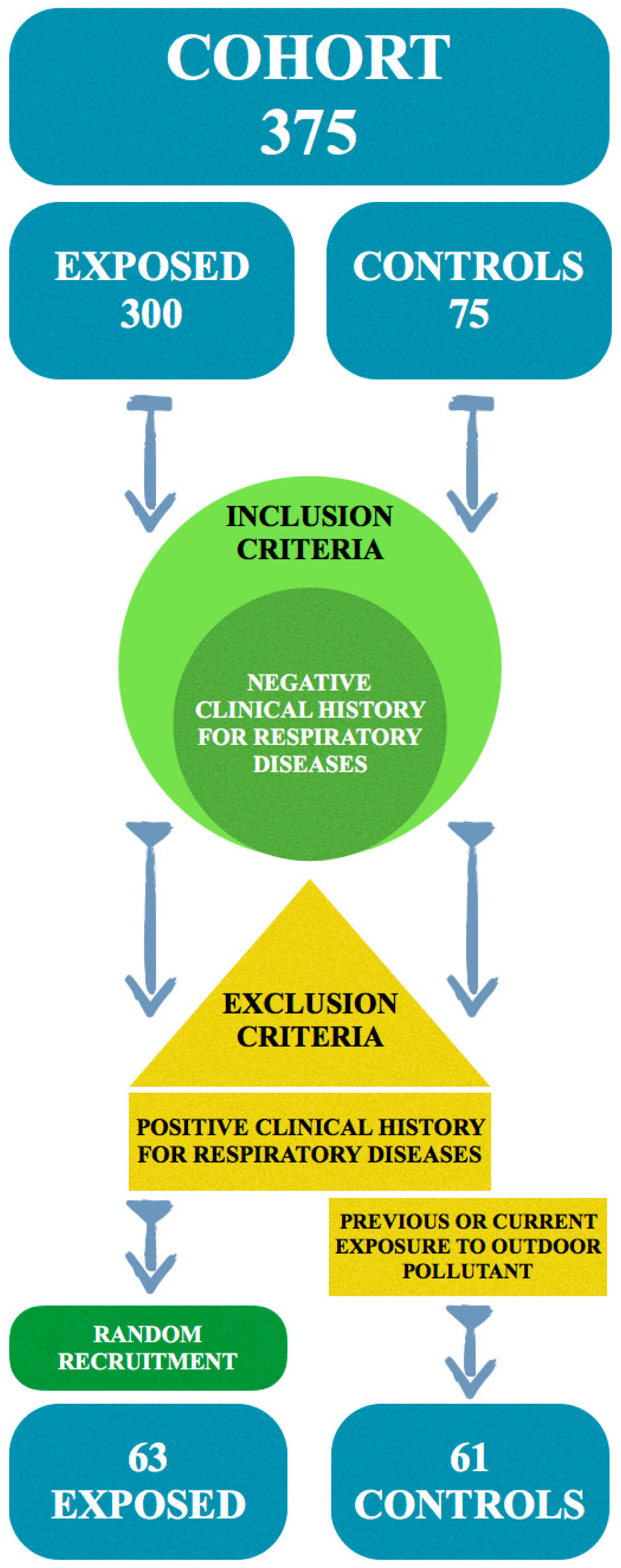
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Dolk, H.; Vrijheid, M.; Armstrong, B.; Abramsky, L.; Bianchi, F.; Garne, E.; Nelen, V.; Robert, E.; Scott, J.E.; Stone, D.; et al. Risk of congenital anomalies near hazardous-waste landfill sites in Europe: The eurohazcon study. Lancet 1998, 352, 423–427. [Google Scholar] [CrossRef]
- Elliott, P.; Briggs, D.; Morris, S.; de Hoogh, C.; Hurt, C.; Jensen, T.K.; Maitland, I.; Richardson, S.; Wakefield, J.; Jarup, L. Risk of adverse birth outcomes in populations living near landfill sites. Brit. Med. J. 2001, 323, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Jarup, L.; Briggs, D.; de Hoogh, C.; Morris, S.; Hurt, C.; Lewin, A.; Maitland, I.; Richardson, S.; Wakefield, J.; Elliott, P. Cancer risks in populations living near landfill sites in Great Britain. Brit. J. Cancer 2002, 86, 1732–1736. [Google Scholar] [CrossRef] [PubMed]
- Sikes, P.; Morris, R.H.; Allen, J.A.; Wilsmith, J.D.; Jones, K.P. Workers’ exposure to dust, endotoxin and beta-(1-3) glucan at four large scale composting facilities. Waste Manag. 2011, 31, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Heldal, K.K.; Halstensen, A.S.; Thorn, J.; Eduard, W.; Halstensen, T.S. Airway inflammation in waste handlers exposed to bioaerosols assessed by induced sputum. Eur. Resp. J. 2003, 21, 641–645. [Google Scholar] [CrossRef]
- Douwes, J.; Wouters, I.; Dubbeld, H.; van Zwieten, L.; Steerenberg, P.; Doekes, G.; Heederik, D. Upper airway inflammation assessed by nasal lavage in compost workers: A relation with bio-aerosol exposure. Am. J. Ind. Med. 2000, 37, 459–468. [Google Scholar] [CrossRef]
- Thorn, J.; Beijer, L.; Rylander, R. Airways inflammation and glucan exposure among household waste collectors. Am. J. Ind. Med. 1998, 33, 463–470. [Google Scholar] [CrossRef]
- Viegas, S.; Veiga, L.; Figueiredo, P.; Almeida, A.; Carolino, E.; Viegas, C. Assessment of workers’ exposure to aflatoxin B1 in a Portuguese waste industry. Ann. Occup. Hyg. 2015, 59, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Rylander, R.; Jacobs, R. ICOH committee on organic dust—Endotoxin in the environment: A criteria document. Int. J. Occup. Environ. Health 1997, 3, 1–48. [Google Scholar]
- Michel, O. Human challenge studies with endotoxins. Int. J. Occup. Environ. Health 1997, 3, 18–25. [Google Scholar]
- Ulmer, A.J. Biochemistry and cell biology of endotoxins. Int. J. Occup. Environ. Health 1997, 3, 8–17. [Google Scholar]
- Ling, S.H.; van Eeden, S.F. Particulate matter air pollution exposure: Role in the development and exacerbation of chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2009, 4, 233–243. [Google Scholar] [CrossRef]
- Fogelmark, B.; Thorn, J.; Rylander, R. Inhalation of (1->3)-beta-d-glucan causes airway eosinophilia. Mediat. Inflamm. 2001, 10, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Fogelmark, B.; Sjostrand, M.; Rylander, R. Pulmonary inflammation induced by repeated inhalations of beta(1,3)-d-glucan and endotoxin. Int. J. Exp. Pathol. 1994, 75, 85–90. [Google Scholar] [PubMed]
- Ray, M.R.; Roychoudhury, S.; Mukherjee, G.; Roy, S.; Lahiri, T. Respiratory and general health impairments of workers employed in a municipal solid waste disposal at an open landfill site in Delhi. Int. J. Hyg. Environ. Health 2005, 208, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.Y.; Chang, W.T.; Chuang, H.Y.; Tsai, S.S.; Wu, T.N.; Sung, F.C. Adverse health effects among household waste collectors in Taiwan. Environ. Res. 2001, 85, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Sigsgaard, T.; Malmros, P.; Nersting, L.; Petersen, C. Respiratory disorders and atopy in Danish refuse workers. Am. J. Respir. Crit. Care Med. 1994, 149, 1407–1412. [Google Scholar] [CrossRef] [PubMed]
- Zuskin, E.; Mustajbegovic, J.; Schachter, E.N.; Kern, J.; Pavicic, D.; Budak, A. Airway function and respiratory symptoms in sanitation workers. J. Occup. Environ. Med. 1996, 38, 522–527. [Google Scholar] [CrossRef] [PubMed]
- Ivens, U.I.; Ebbehoj, N.; Poulsen, O.M.; Skov, T. Season, equipment, and job function related to gastrointestinal problems in waste collectors. Occup. Environ. Med. 1997, 54, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Wouters, I.M.; Hilhorst, S.K.; Kleppe, P.; Doekes, G.; Douwes, J.; Peretz, C.; Heederik, D. Upper airway inflammation and respiratory symptoms in domestic waste collectors. Occup. Environ. Med. 2002, 59, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Matheson, M.C.; Benke, G.; Raven, J.; Sim, M.R.; Kromhout, H.; Vermeulen, R.; Johns, D.P.; Walters, E.H.; Abramson, M.J. Biological dust exposure in the workplace is a risk factor for chronic obstructive pulmonary disease. Thorax 2005, 60, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.N.; Kurup, V.P.; Fink, J.N. Allergic bronchopulmonary aspergillosis from a contaminated dump site. Am. Rev. Resp. Dis. 1989, 140, 1086–1088. [Google Scholar] [CrossRef] [PubMed]
- Allmers, H.; Huber, H.; Baur, X. Two year follow-up of a garbage collector with allergic bronchopulmonary aspergillosis (abpa). Am. J. Ind. Med. 2000, 37, 438–442. [Google Scholar] [CrossRef]
- Falcon-Rodriguez, C.I.; Osornio-Vargas, A.R.; Sada-Ovalle, I.; Segura-Medina, P. Aeroparticles, composition, and lung diseases. Front. Immunol. 2016, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Medical Research Council’s Committee on Environmental and Occupational Health. Questionnaire on Respiratory Symptoms; Medical Research Council: London, UK, 1986. [Google Scholar]
- Minette, A.; Aresini, G.; Sanna-Randaccio, F.; Seaton, A.; Smodt, U.; Teculescu, U. Promemoria Relativo al Questionario Della CECA, 3rd ed.; Commissione delle Comunità Europee: Luxembourg, Lussemburgo, 1988. [Google Scholar]
- ATS. Standardization of Spirometry. Available online: https://www.thoracic.org/statements/resources/pfet/PFT2.pdf (accessed on 2 February 2016).
- Athanasiou, M.; Makrynos, G.; Dounias, G. Respiratory health of municipal solid waste workers. Occup. Med. 2010, 60, 618–623. [Google Scholar] [CrossRef] [PubMed]
- De Meer, G.; Heederik, D.; Wouters, I.M. Change in airway responsiveness over a workweek in organic waste loaders. Int. Arch. Occup. Envir. Health 2007, 80, 649–652. [Google Scholar] [CrossRef] [PubMed]
- Neumann, H.D.; Balfanz, J.; Becker, G.; Lohmeyer, M.; Mathys, W.; Raulf-Heimsoth, M. Bioaerosol exposure during refuse collection: Results of field studies in the real-life situation. Sci. Total Environ. 2002, 293, 219–231. [Google Scholar] [CrossRef]
- Vimercati, L.; Gatti, M.F.; Baldassarre, A.; Nettis, E.; Favia, N.; Palma, M.; Martina, G.L.; Di Leo, E.; Musti, M. Occupational exposure to urban air pollution and allergic diseases. Int. J. Environ. Res. Public Health 2015, 12, 12977–12987. [Google Scholar] [CrossRef] [PubMed]
- Nordenhall, C.; Pourazar, J.; Ledin, M.C.; Levin, J.O.; Sandstrom, T.; Adelroth, E. Diesel exhaust enhances airway responsiveness in asthmatic subjects. Eur. Resp. J. 2001, 17, 909–915. [Google Scholar] [CrossRef]
- Behndig, A.F.; Larsson, N.; Brown, J.L.; Stenfors, N.; Helleday, R.; Duggan, S.T.; Dove, R.E.; Wilson, S.J.; Sandstrom, T.; Kelly, F.J.; et al. Proinflammatory doses of diesel exhaust in healthy subjects fail to elicit equivalent or augmented airway inflammation in subjects with asthma. Thorax 2011, 66, 12–19. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Exposed | Controls | p Values | |
|---|---|---|---|---|
| N | 63 | 61 | ||
| Sex | M | 63 | 61 | |
| F | 0 | 0 | ||
| Age | Average | 53 | 51 | 0.38 |
| SD | 7 | 7 | ||
| Median | 54 | 52 | ||
| Range | 32–66 | 36–63 | ||
| BMI | Average | 26.40 | 26.00 | 0.71 |
| SD | 11.06 | 4.36 | ||
| Median | 26.37 | 25.25 | ||
| Range | 16.90–34.84 | 18.36–40.14 | ||
| Smoking habit | Yes | 17 (27.00%) | 13 (21.30%) | 0.19 |
| No | 31 (49.20%) | 38 (62.30%) | ||
| Former | 15 (23.80%) | 10 (16.40%) | ||
| Spirometric Values | Exposed | Controls | p Values | |
|---|---|---|---|---|
| N | 63 | 61 | ||
| FVC | Average | 4.76 | 4.56 | 0.114 |
| SD | 0.99 | 1.09 | ||
| Median | 4.67 | 4.49 | ||
| % mean | 115.06 | 114.2 | ||
| % SD | 22.42 | 18.06 | ||
| % median | 113 | 112 | ||
| FEV1 | Average | 3.53 | 3.64 | 0.046 |
| SD | 0.73 | 0.85 | ||
| Median | 3.42 | 3.50 | ||
| % mean | 105.89 | 111.03 | ||
| % SD | 19.05 | 17.53 | ||
| % median | 107 | 110 | ||
| TIFFENAU INDEX | Average | 75.08 | 79.93 | 0.001 |
| SD | 9.06 | 3.89 | ||
| Median | 76.09 | 80.12 | ||
| Range | 32.62–93.43 | 67.57–87.31 | ||
| OR | 95% CI | p Value |
|---|---|---|
| 8.4 | 1.8–38.9 | 0.006 |
| 7.9 * | 1.7–37.0 | 0.008 |
| Symptoms | Exposed (N = 63) | Controls (N = 61) | OR | 95% CI | p Value | ||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Rhinitis symptoms | 11 | 17.4 | 19 | 31.1 | 0.41 | 0.17–1.00 | 0.051 |
| Bronchitis symptoms | 12 | 19.0 | 11 | 18.0 | 1.09 | 0.43–2.76 | 0.847 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vimercati, L.; Baldassarre, A.; Gatti, M.F.; De Maria, L.; Caputi, A.; Dirodi, A.A.; Cuccaro, F.; Bellino, R.M. Respiratory Health in Waste Collection and Disposal Workers. Int. J. Environ. Res. Public Health 2016, 13, 631. https://doi.org/10.3390/ijerph13070631
Vimercati L, Baldassarre A, Gatti MF, De Maria L, Caputi A, Dirodi AA, Cuccaro F, Bellino RM. Respiratory Health in Waste Collection and Disposal Workers. International Journal of Environmental Research and Public Health. 2016; 13(7):631. https://doi.org/10.3390/ijerph13070631
Chicago/Turabian StyleVimercati, Luigi, Antonio Baldassarre, Maria Franca Gatti, Luigi De Maria, Antonio Caputi, Angelica A. Dirodi, Francesco Cuccaro, and Raffaello Maria Bellino. 2016. "Respiratory Health in Waste Collection and Disposal Workers" International Journal of Environmental Research and Public Health 13, no. 7: 631. https://doi.org/10.3390/ijerph13070631
APA StyleVimercati, L., Baldassarre, A., Gatti, M. F., De Maria, L., Caputi, A., Dirodi, A. A., Cuccaro, F., & Bellino, R. M. (2016). Respiratory Health in Waste Collection and Disposal Workers. International Journal of Environmental Research and Public Health, 13(7), 631. https://doi.org/10.3390/ijerph13070631









