An ICF-Based Model for Implementing and Standardizing Multidisciplinary Obesity Rehabilitation Programs within the Healthcare System
Abstract
:1. Introduction
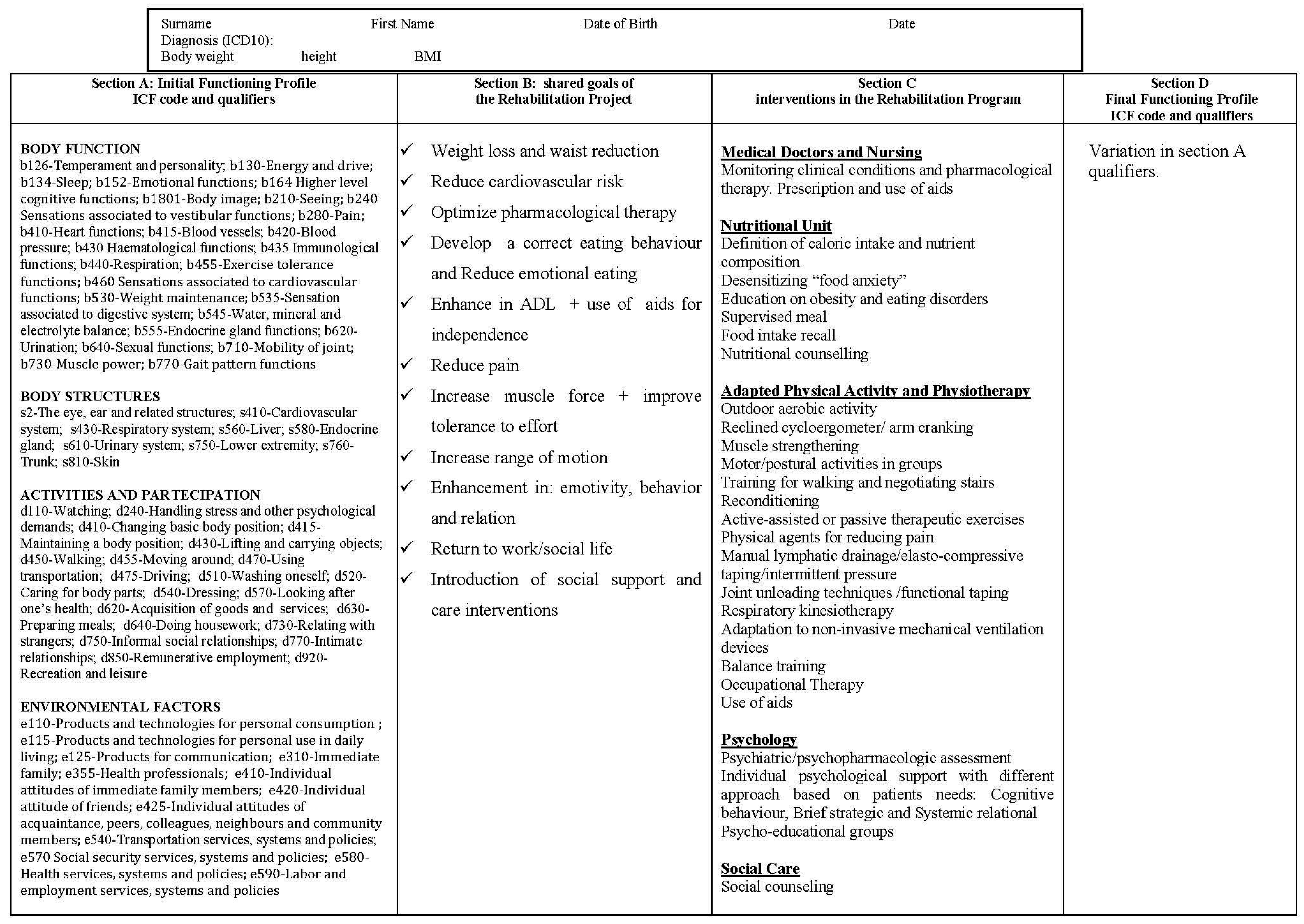
2. Methods
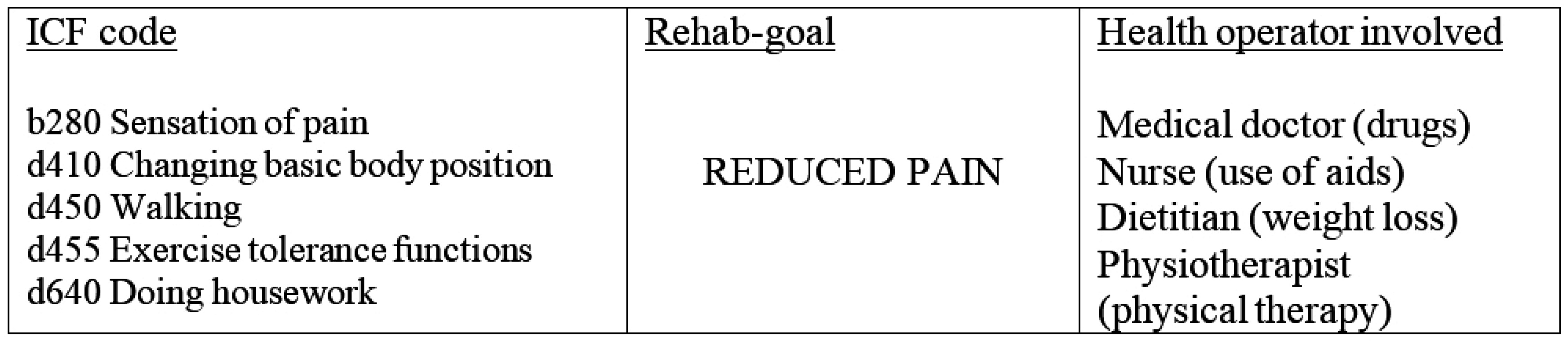
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Martin, L.G.; Schoeni, R.F. Trends in disability and related chronic conditions among the forty-and-over population: 1997–2010. Disabil. Health J. 2014, 7, S4–S14. [Google Scholar] [CrossRef] [PubMed]
- Capodaglio, P.; Castelnuovo, G.; Brunani, A.; Vismara, L.; Villa, V.; Capodaglio, E.M. Functional limitations and occupational issues in obesity: A review. Int. J. Occup. Saf. Ergon. 2010, 16, 407–423. [Google Scholar]
- Backholer, K.; Wong, E.; Freak-Poli, R.; Walls, H.L.; Peeters, A. Increasing body weight and risk of limitations in activities of daily living: A systematic review and meta-analysis. Obes. Rev. 2012, 13, 456–468. [Google Scholar] [CrossRef] [PubMed]
- World Report on Disability. World Health Organization (WHO): Geneva, Switzerland, 2011. Available online: http://www.who.int/disabilities/world_report/2011/en/ (accessed on 26 May 2015).
- Capodaglio, P.; Donini, L.M.; Petroni, M.L.; Brunani, A.; Dalle Grave, R.; di Flaviano, C.E.; Giorgetti, A.; Giustini, A.; Saraceni, L.M. Rehabilitation in obesity with comorbidities: A consensus document from experts of the Italian Society of Physical and Rehabilitation Medicine (SIMFER), the Italian Society of Obesity (SIO) and the Italian Society of Eating Disorders (SISDCA). Eat. Weight Disord. 2014, 19, 383–386. [Google Scholar] [CrossRef] [PubMed]
- La Centralità Della Persona in Riabilitazione: Nuovi Modelli Organizzativi E Gestionali. Quaderni del Ministero Della Salute 8, 2011. Available online: http://www.quadernidellasalute.it/archivio-quaderni/8-marzo-aprile-2011.php (accessed on 26 May 2015).
- International Classification of Functioning, Disability and Health, ICF. World Health Organization (WHO): Geneva, Switzerland, 2001. Available online: http://www.who.int/classifications/icf/en (accessed on 26 May 2015).
- Stucki, A.; Daansen, P.; Fuessl, M.; Cieza, A.; Huber, E.; Atkinson, R.; Kostanjsek, N.; Stucki, G.; Ruof, J. ICF core sets for obesity. J. Rehabil. Med. 2004, 44, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Brunani, A.; Liuzzi, A.; Sirtori, A.; Raggi, A.; Berselli, M.E.; Villa, V.; Ceriani, F.; Tacchini, E.; Vicari, V.; Parisio, C.; et al. Mapping an obesity clinical evaluation protocol to the International Classification of Functioning, Disability and Health (ICF). Disabil. Rehabil. 2010, 32, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Raggi, A.; Brunani, A.; Sirtori, A.; Liuzzi, A.; Berselli, M.E.; Villa, V.; Ceriani, F.; Leonardi, M.; ICF-Obesity Group. Obesity-related disability: Key factors identified by the International Classification of Functioning, Disability and Health. Disabil. Rehabil. 2010, 32, 2028–2034. [Google Scholar] [PubMed]
- Rauch, A.; Cieza, A.; Stucki, G. How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur. J. Phys. Rehabil. Med. 2008, 44, 329–342. [Google Scholar] [PubMed]
- Marzorati, D.; Liuzzi, A.; Brunani, A. La metodologia dei PDT applicata alla definizione e gestione dei protocolli riabilitativi per l’obesità grave e complicata. Mecosan 2003, 47, 125–134. [Google Scholar]
- Precilios, H.; Brunani, A.; Cimolin, V.; Tacchini, E.; Donini, L.M.; De Souza, S.F.; Capodaglio, P. Measuring changes after multidisciplinary rehabilitation of obese individuals. J. Endocrionol. Investig. 2013, 36, 72–77. [Google Scholar]
- Raggi, A.; Sirtori, A.; Brunani, A.; Liuzzi, A.; Leonardi, M. ICF classification to describe functioning and disability in patients with obesity. Disabil. Rehabil. 2009, 31, S153–S158. [Google Scholar] [CrossRef] [PubMed]
- Rentsch, H.P.; Bucher, P.; Dommen Nyffeler, I.; Wolf, C.; Hefti, H.; Fluri, E.; Wenger, U.; Wälti, C.; Boyer, I. The implementation of the ‘International Classification of Functioning, Disability and Health’ (ICF) in daily practice of neurorehabilitation: An interdisciplinary project at the Kantonsspital of Lucerne, Switzerland. Disabil. Rehabil. 2003, 25, 411–421. [Google Scholar] [PubMed]
- Forhan, M. An analysis of disability models and the application of the ICF to obesity. Disabil. Rehabil. 2009, 31, 1382–1388. [Google Scholar] [CrossRef] [PubMed]
- Martinuzzi, A.; Salghetti, A.; Betto, S.; Russo, E.; Leonardi, M.; Raggi, A.; Francescutti, C. The International Classification of Functioning Disability and Health, version for children and youth as a roadmap for projecting and programming rehabilitation in a neuropaediatric hospital unit. J. Rehabil. Med. 2010, 42, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Martinuzzi, A.; Carraro, E.; Petacchi, E.; Pasqualotti, S.; Costalunga, M.; Betto, S. Implementation of an ICF-based project/program in a pediatric neuro-rehabiltation hospital: Follow-up evaluation by stakeholders. Disabil. Rehabil. 2013, 35, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brunani, A.; Raggi, A.; Sirtori, A.; Berselli, M.E.; Villa, V.; Ceriani, F.; Corti, S.; Leonardi, M.; Capodaglio, P.; Group, I.-O. An ICF-Based Model for Implementing and Standardizing Multidisciplinary Obesity Rehabilitation Programs within the Healthcare System. Int. J. Environ. Res. Public Health 2015, 12, 6084-6091. https://doi.org/10.3390/ijerph120606084
Brunani A, Raggi A, Sirtori A, Berselli ME, Villa V, Ceriani F, Corti S, Leonardi M, Capodaglio P, Group I-O. An ICF-Based Model for Implementing and Standardizing Multidisciplinary Obesity Rehabilitation Programs within the Healthcare System. International Journal of Environmental Research and Public Health. 2015; 12(6):6084-6091. https://doi.org/10.3390/ijerph120606084
Chicago/Turabian StyleBrunani, Amelia, Alberto Raggi, Anna Sirtori, Maria Elisa Berselli, Valentina Villa, Francesca Ceriani, Stefania Corti, Matilde Leonardi, Paolo Capodaglio, and ICF-OBESITY Group. 2015. "An ICF-Based Model for Implementing and Standardizing Multidisciplinary Obesity Rehabilitation Programs within the Healthcare System" International Journal of Environmental Research and Public Health 12, no. 6: 6084-6091. https://doi.org/10.3390/ijerph120606084
APA StyleBrunani, A., Raggi, A., Sirtori, A., Berselli, M. E., Villa, V., Ceriani, F., Corti, S., Leonardi, M., Capodaglio, P., & Group, I.-O. (2015). An ICF-Based Model for Implementing and Standardizing Multidisciplinary Obesity Rehabilitation Programs within the Healthcare System. International Journal of Environmental Research and Public Health, 12(6), 6084-6091. https://doi.org/10.3390/ijerph120606084





