A Spatial, Social and Environmental Study of Tuberculosis in China Using Statistical and GIS Technology
Abstract
:1. Introduction
2. Materials and methods
2.1. Data Sources
| Observed Variable | Description of Observed Variable | Data Source | Period | Latent Risk Factor | % of Variance |
|---|---|---|---|---|---|
| X4 | Annual average precipitation (mm) | Meteorological Data Sharing Service System of China | 2002–2007 | Climatic factor | 93.2% |
| X7 | Annual average temperature (°C) | 2002–2007 | |||
| X8 | Annual average vapor pressure (Pa) | 2002–2007 | |||
| X9 | Annual average relative humidity (%) | 2002–2007 | |||
| X10 | Annual average minimum temperature (°C) | 2002–2007 | |||
| X11 | Annual average maximum temperature (°C) | 2002–2007 | |||
| X12 | Number of days in per year in which precipitation is greater than 0.1 mm (day) | 2002–2007 | Rainy day factor | 100% | |
| X5 | Average altitude (m) | 2002–2007 | Altitude factor | 98.7% | |
| X1 | Annual average air pressure (Pa) | 2002–2007 | |||
| X3 | Average longitude (degrees) | 2002–2007 | Longitude factor | 100% | |
| X15 | Air pollution index (API) | Ministry of Environmental Protection of China | 2002–2007 | Air quality | 100% |
| X16 | Per capita annual net income of rural residents (RMB yuan) | China Regional Economic Statistical Yearbook | 2002–2007 | Economic level | 88.2% |
| X17 | Per capita annual cost-of-living expense of rural residents (RMB yuan) | 2002–2007 | |||
| X18 | Per capita annual disposable income of urban residents (RMB yuan) | 2002–2007 | |||
| X19 | Per capita annual cost-of-living expense of urban residents (RMB yuan) | 2002–2007 | |||
| X20 | Per capita annual gross domestic product (RMB yuan) | 2002–2007 | |||
| X22 | Per capita annual fixed time deposit of urban and rural residents (RMB yuan) | 2002–2007 | |||
| X26 | Annual unemployment rate of urban residents (%) | 2002–2007 | Unemployment level | 100% | |
| X27 | Number of students per teacher of primary school | 2002–2007 | Education burden | 89.4% | |
| X28 | Number of students per teacher of ordinary high school | 2002–2007 | |||
| X30 | Population density (population/km2) | 2002–2007 | Population density | 100% | |
| X23 | Percentage of primary industry employees from the total number of employees (%) | 2002–2007 | Primary industry employment | 93.6% | |
| X36 | Percentage of primary industry employees from the total number of employees in rural areas (%) | 2002–2007 | |||
| X34 | Number of beds in medical institutions per thousand people | 2002–2007 | Health service | 97.3% | |
| X35 | Number of medical workers per thousand people | 2002–2007 |
2.2. Statistical Methods
2.3. Analysis Using a Geographical Statistical Model
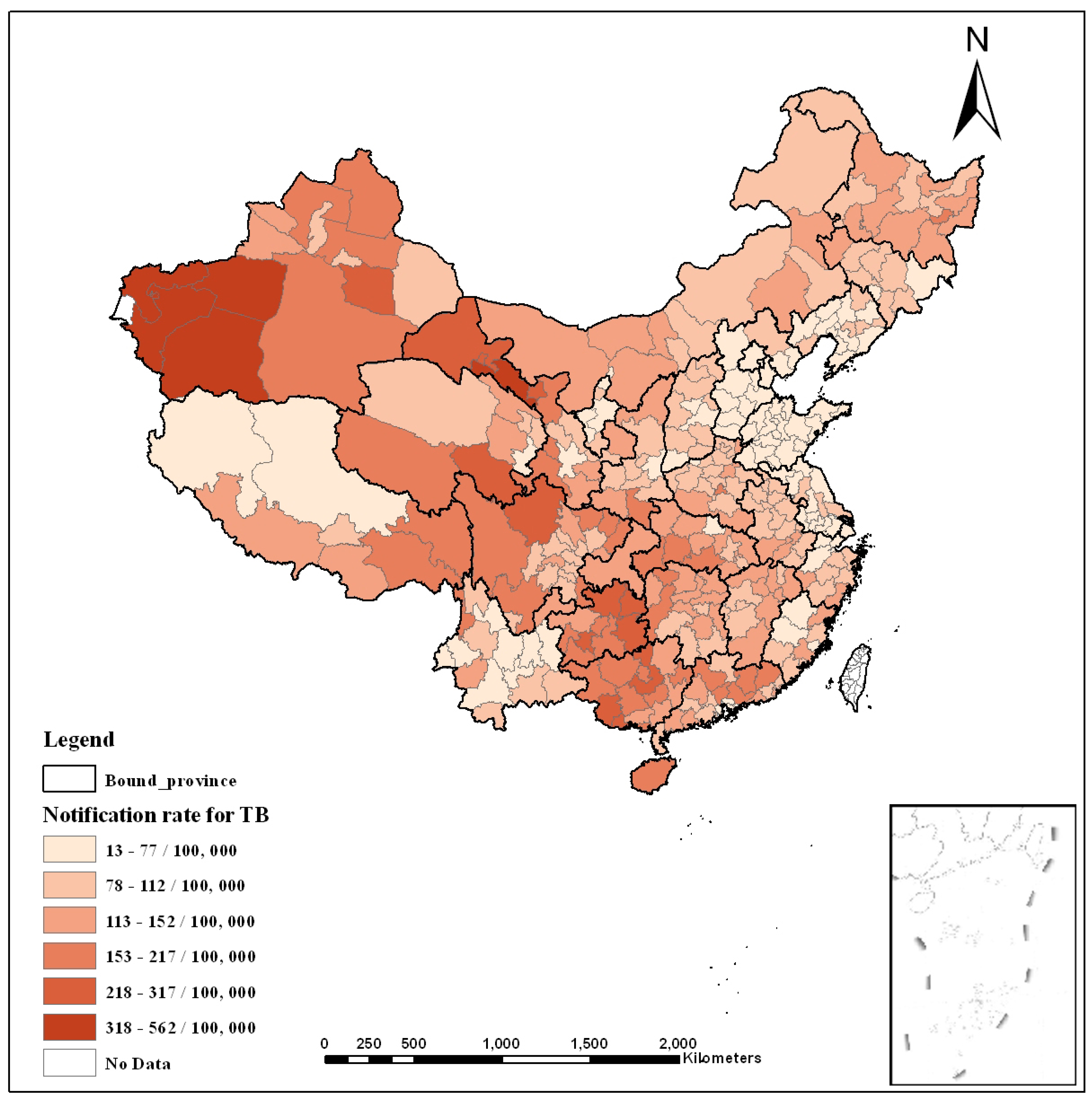
3. Results and Discussion
3.1. Extraction of Latent Risk Factors
3.2. Complex Relationship between TB Prevalence and Latent Risk Factors
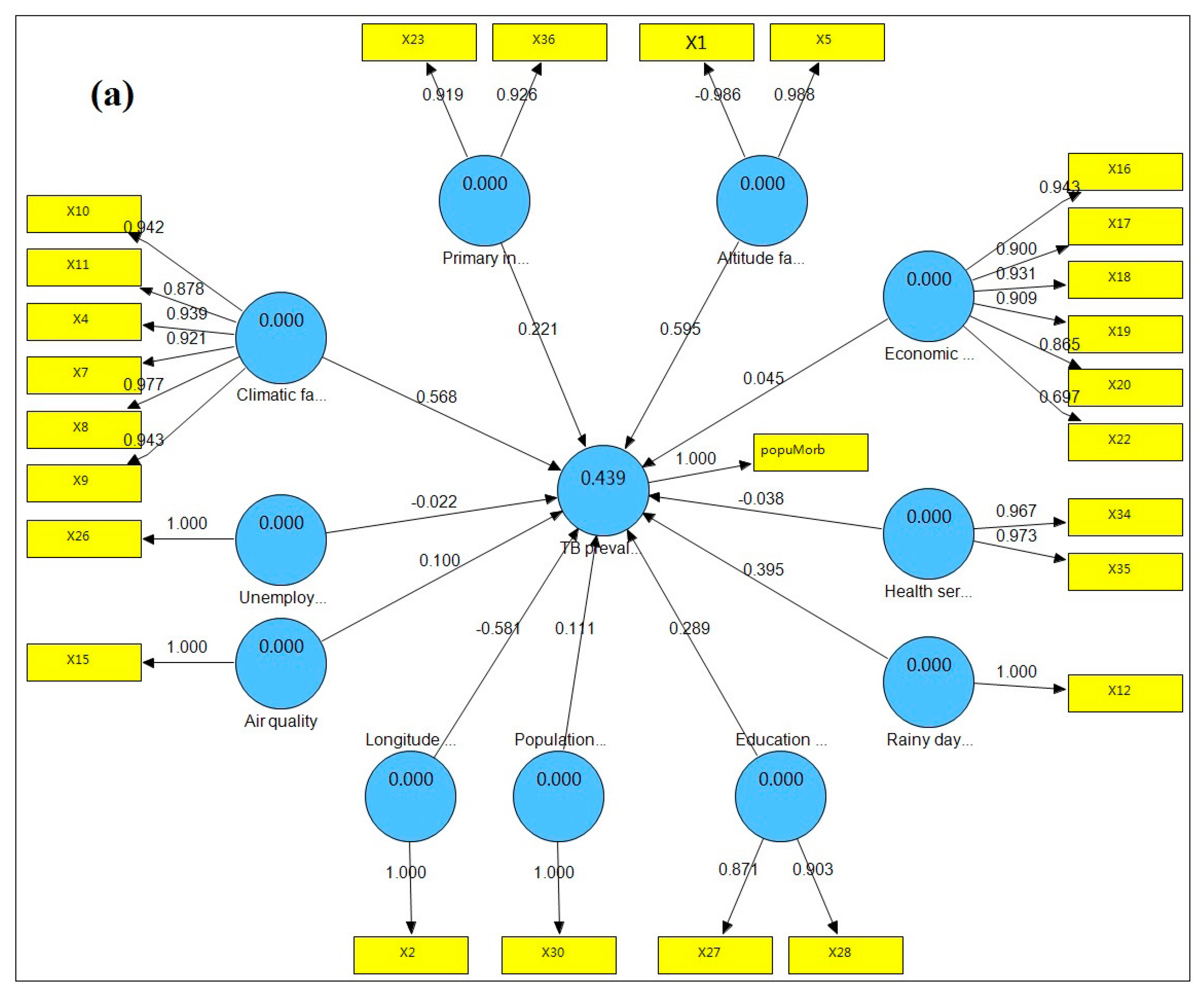
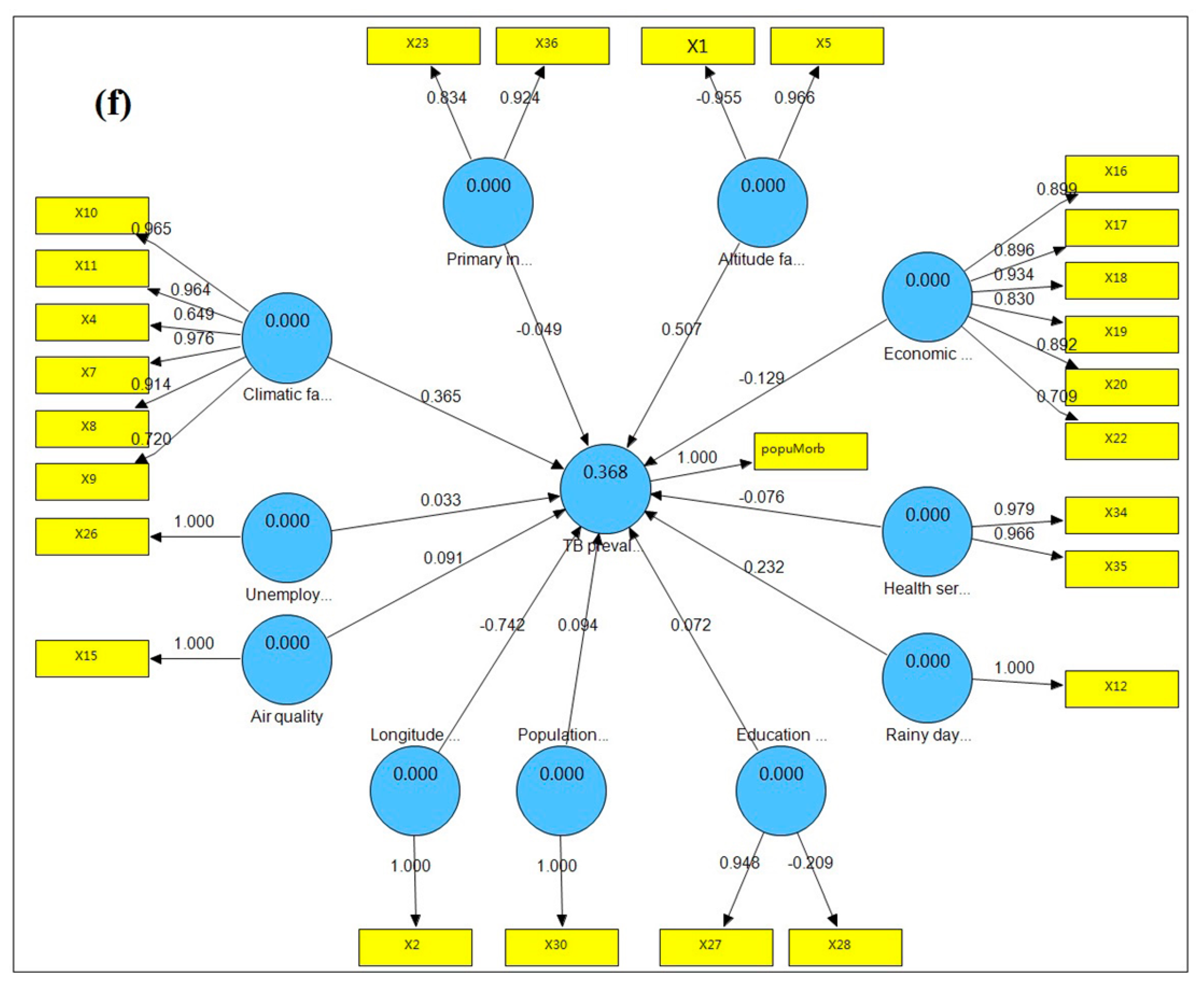
| Structural Model | Original Sample | Sample Mean | Standard Deviation | Standard Error | T Statistics |
|---|---|---|---|---|---|
| Air quality → TB prevalence | 0.1002 | 0.0757 | 0.0587 | 0.0587 | 1.4915 |
| Climatic factor → TB prevalence | 0.5681 | 0.5353 | 0.225 | 0.225 | 2.8004 ** |
| Education burden → TB prevalence | 0.2887 | 0.2454 | 0.0664 | 0.0664 | 3.5616 *** |
| Primary industry employment → TB prevalence | 0.2208 | 0.1814 | 0.1007 | 0.1007 | 1.9476 * |
| Altitude factor → TB prevalence | 0.5953 | 0.5947 | 0.1558 | 0.1558 | 4.1515 *** |
| Health service → TB prevalence | −0.0380 | −0.0151 | 0.08 | 0.08 | 0.0047 |
| Population density → TB prevalence | 0.1109 | 0.1344 | 0.0595 | 0.0595 | 1.9689 * |
| Longitude factor → TB prevalence | −0.5811 | −0.5112 | 0.1031 | 0.1031 | 5.0916 *** |
| Rainy day factor → TB prevalence | 0.3946 | 0.3982 | 0.151 | 0.151 | 3.0139 ** |
| Economic level → TB prevalence | 0.0452 | 0.035 | 0.0931 | 0.0931 | 0.404 |
| Unemployment → TB prevalence | −0.0221 | −0.009 | 0.0545 | 0.0545 | 0.2817 |
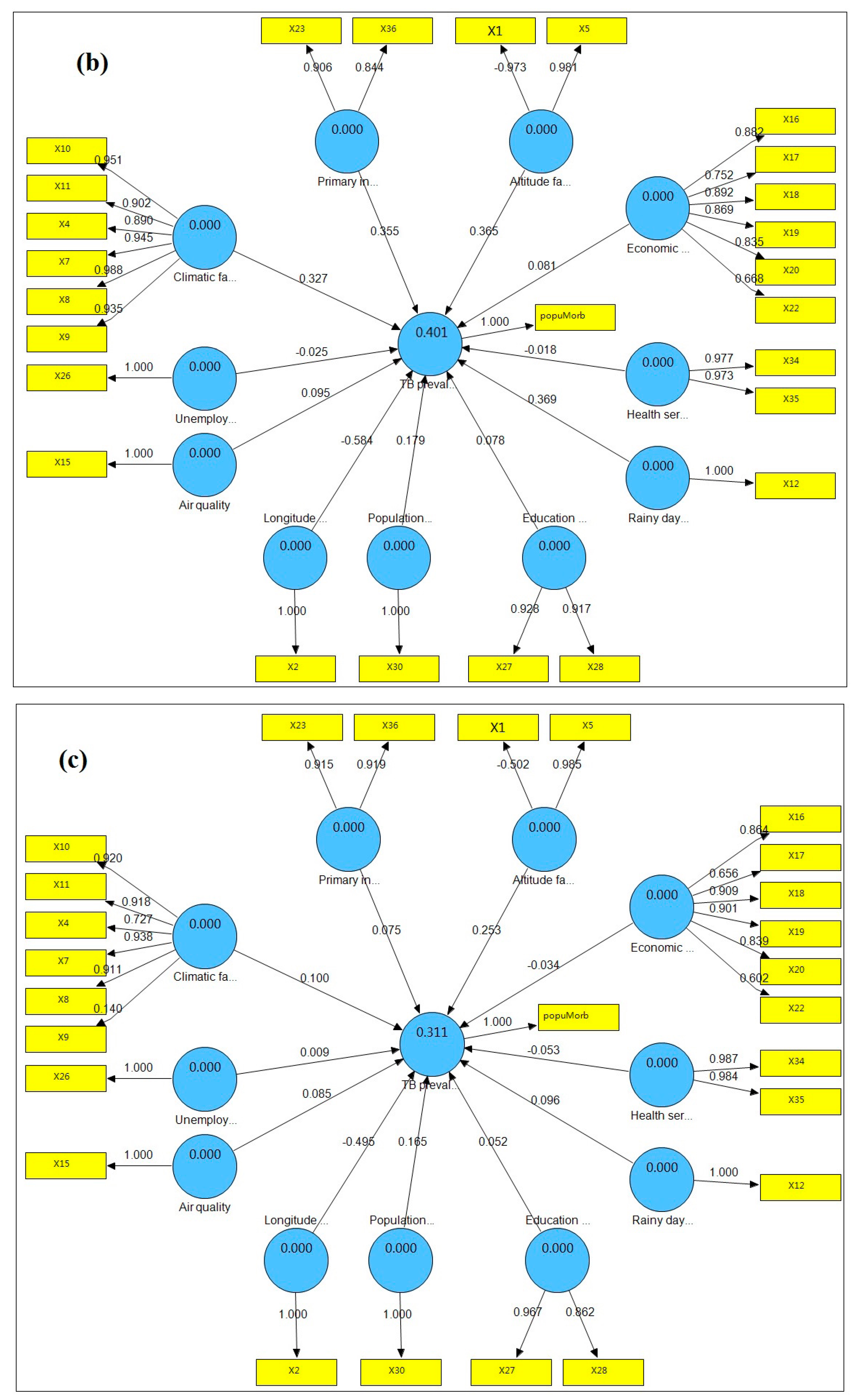
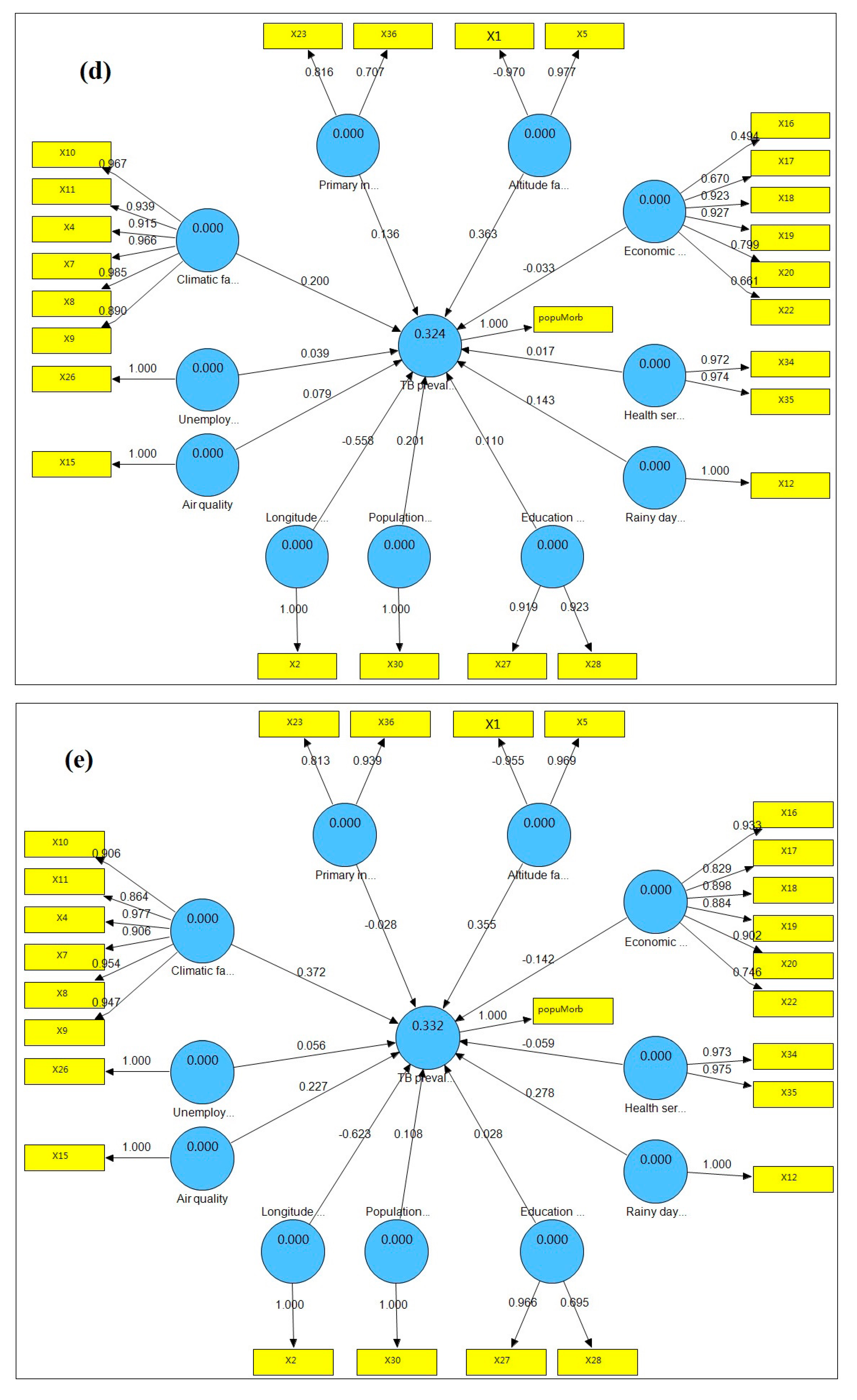
3.3. Hysteresis of the Relationship between TB Prevalence and Latent Risk Factors
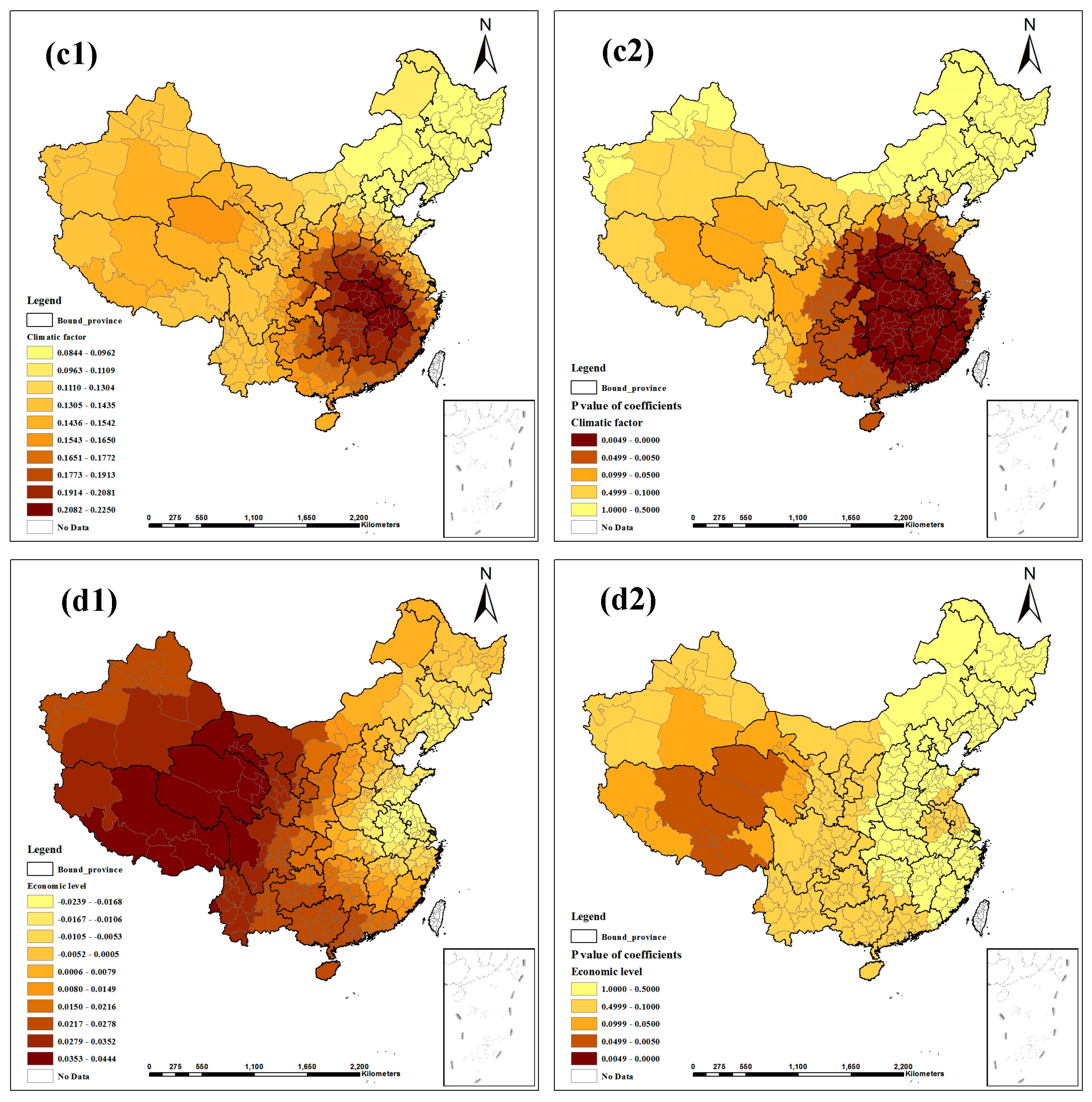
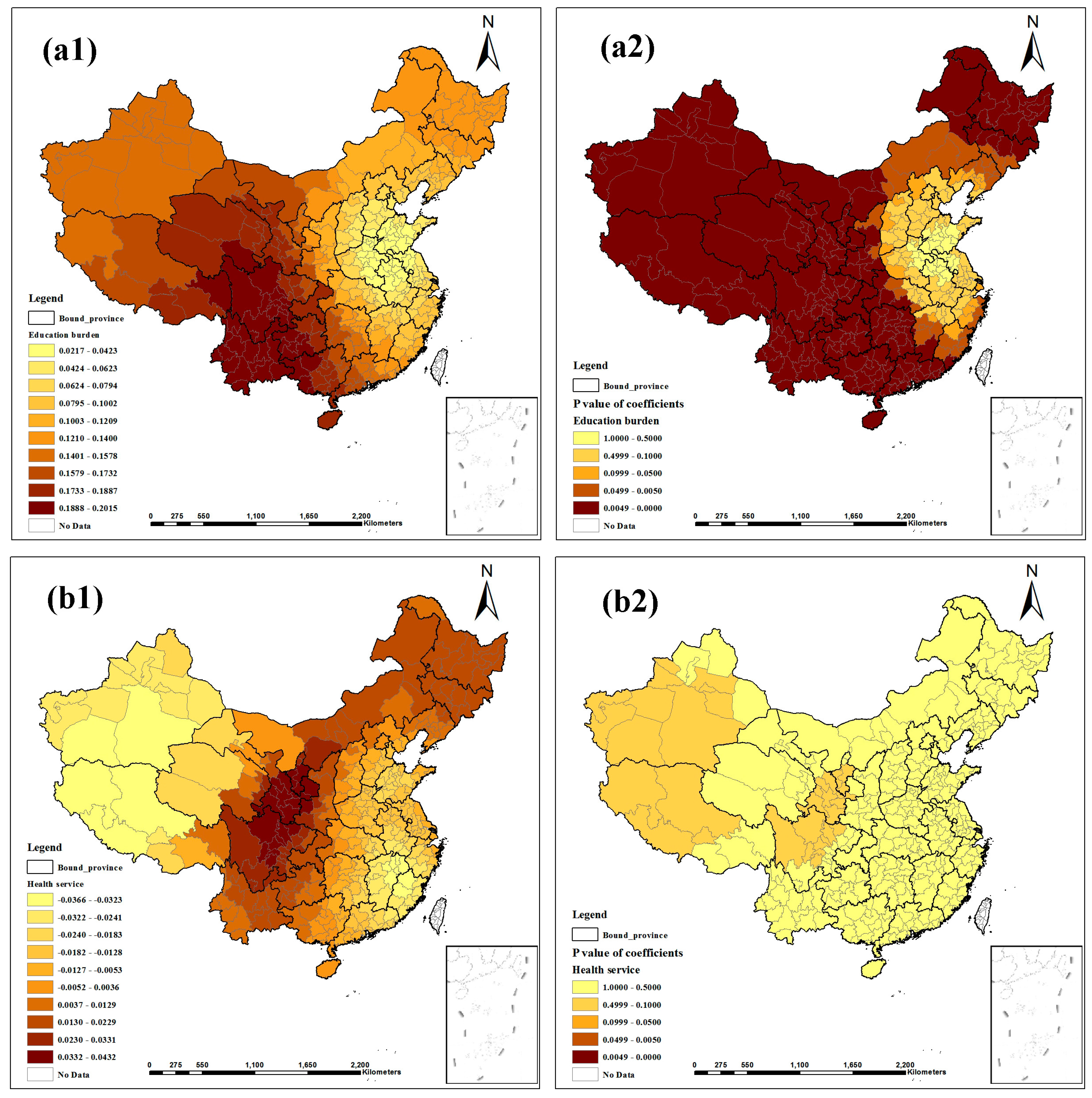
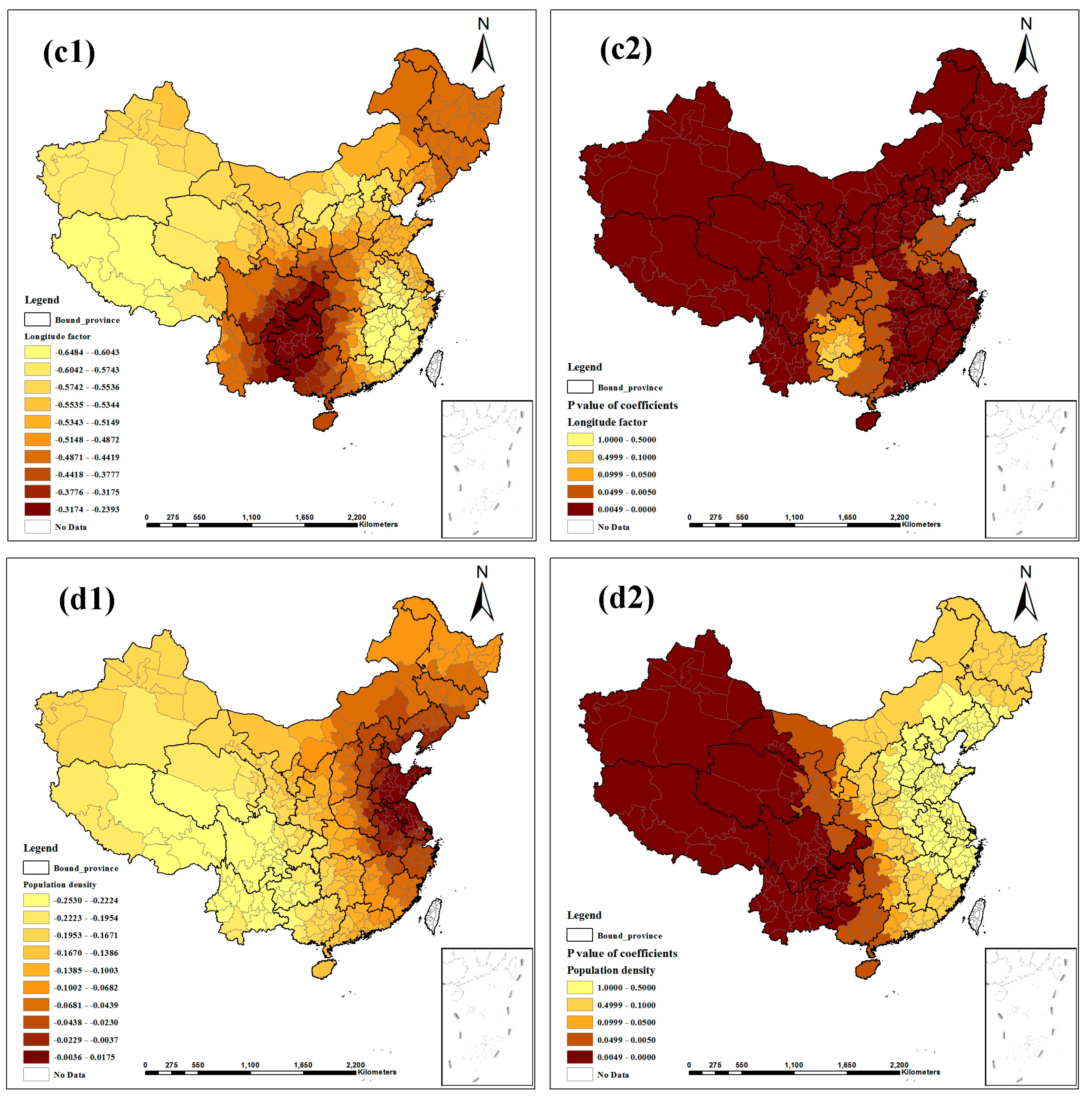
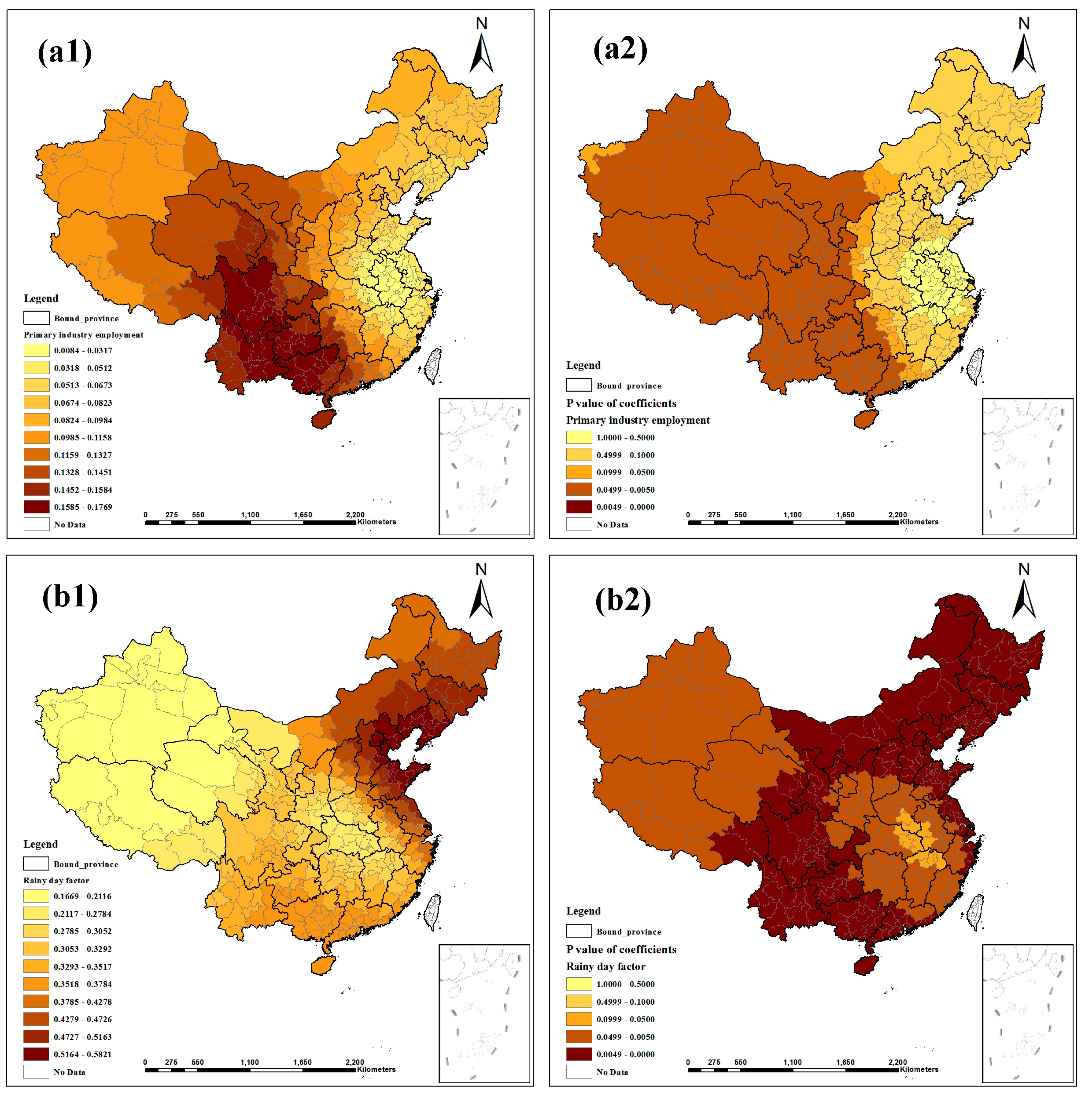
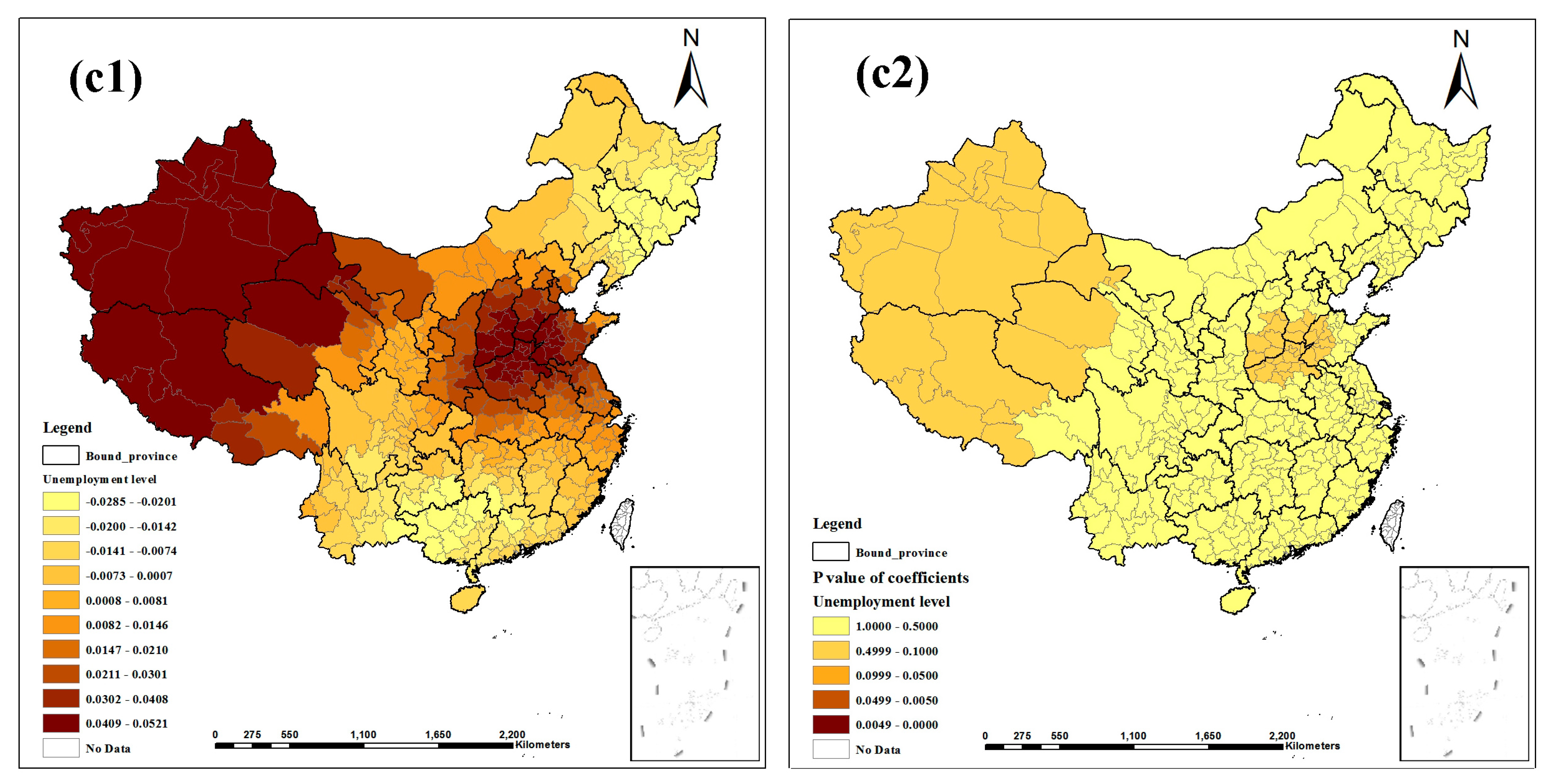
3.4. Local Spatial Heterogeneity of the Relationship
| Parameter | Min | 1st Quartile | Median | 3rd Quartile | Max | Mean |
|---|---|---|---|---|---|---|
| Intercept | −0.1539 | −0.1130 | −0.0686 | −0.0364 | −0.0126 | −0.0751 |
| Air quality | −0.1400 | −0.0534 | −0.0041 | 0.0375 | 0.0994 | −0.0108 |
| Climatic factor | 0.0686 | 0.1466 | 0.1976 | 0.2443 | 0.2877 | 0.1896 |
| Economic level | −0.1156 | −0.0655 | −0.0461 | −0.0179 | 0.0250 | −0.0462 |
| Education burden | −0.0239 | −0.0074 | 0.0099 | 0.0244 | 0.0444 | 0.0088 |
| Health service | 0.0217 | 0.0718 | 0.1264 | 0.1699 | 0.2015 | 0.1201 |
| Altitude factor | −0.0366 | −0.0180 | −0.0079 | 0.0158 | 0.0432 | −0.0020 |
| Unemployment level | −0.6484 | −0.5595 | −0.5170 | −0.4698 | −0.2393 | −0.4965 |
| Longitude factor | −0.2530 | −0.1798 | −0.0865 | −0.0312 | 0.0175 | −0.1039 |
| Primary industry employment | 0.0084 | 0.0623 | 0.0978 | 0.1426 | 0.1769 | 0.0979 |
| Rainy day factor | 0.1669 | 0.3046 | 0.3496 | 0.4271 | 0.5821 | 0.3633 |
| Population density | −0.0285 | −0.0124 | 0.0073 | 0.0281 | 0.0521 | 0.0089 |

4. Discussion
5. Conclusions
Supplementary Files
Supplementary File 1List of Abbreviations
| TB | tuberculosis |
| WHO | World Health Organization |
| API | air pollution index |
| EFA | exploratory factor analysis |
| PLS-PM | partial least squares path model |
| SEM | structure equation model |
| MDR-TB | multidrug-resistant tuberculosis |
| GWR | geographically weighted regression |
| AICc | Akaike information criterion with a correction |
| OLS | ordinary least squares |
| ANOVA | analysis of variance |
| BCG | Bacille Calmette Guerin |
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO Report 2007: Global Tuberculosis Control: Surveillance, Planning, Financing; World Health Organization: Geneva, Switzerland, 2007.
- 2012 Tuberculosis Global Facts; World Health Organization: Geneva, Switzerland, 2011.
- Disease Control Bureau of the Ministry of Health. Report on the 5th National Tuberculosis Epidemiological Survey in China; Military Medical Science Press: Beijing, China, 2010; pp. 30–37. (In Chinese)
- Brudey, K.; Driscoll, J.R.; Rigouts, L.; Prodinger, W.M.; Gori, A.; Al-Hajoj, S.A.; Allix, C.; Aristimuño, L.; Arora, J.; Baumanis, V. Mycobacterium tuberculosis complex genetic diversity: Mining the fourth international spoligotyping database (SpolDB4) for classification, population genetics and epidemiology. BMC Microbiol. 2006, 6. [Google Scholar] [CrossRef] [PubMed]
- Borgdorff, M.; Nagelkerke, N.; Dye, C.; Nunn, P. Gender and tuberculosis: A comparison of prevalence surveys with notification data to explore sex differences in case detection. Int. J. Tuberc. Lung Dis. 2000, 4, 123–132. [Google Scholar]
- Rubel, A.J.; Garro, L.C. Social and cultural factors in the successful control of tuberculosis. Public Health Rep. 1992, 107, 626–636. [Google Scholar]
- Serpa, J.A.; Teeter, L.D.; Musser, J.M.; Graviss, E.A. Tuberculosis disparity between U.S.-born blacks and whites, Houston, Texas, USA. Emerg. Infect. Dis. 2009. [Google Scholar] [CrossRef]
- Cantwell, M.F.; McKenna, M.T.; McCray, E.; Onorato, I.M. Tuberculosis and race/ethnicity in the United States: Impact of socioeconomic status. Amer. J. Respir. Crit. Care Med. 1998, 157, 1016–1020. [Google Scholar] [CrossRef]
- Myers, W.P.; Westenhouse, J.L.; Flood, J.; Riley, L.W. An ecological study of tuberculosis transmission in California. Amer. J. Public Health 2006. [Google Scholar] [CrossRef]
- Munch, Z.; van Lill, S.; Booysen, C.; Zietsman, H.; Enarson, D.; Beyers, N. Tuberculosis transmission patterns in a high-incidence area: A spatial analysis. Int. J. Tuberc. Lung Dis. 2003, 7, 271–277. [Google Scholar]
- Lin, H.-H.; Ezzati, M.; Murray, M. Tobacco smoke, indoor air pollution and tuberculosis: A systematic review and meta-analysis. PLoS Med. 2007. [Google Scholar] [CrossRef]
- Sonnenberg, P.; Glynn, J.R.; Fielding, K.; Murray, J.; Godfrey-Faussett, P.; Shearer, S. How soon after infection with HIV does the risk of tuberculosis start to increase? A retrospective cohort study in South African gold miners. J. Infect. Dis. 2005, 191, 150–158. [Google Scholar]
- Koo, B.K. Diabetes mellitus and tuberculosis. Diabetes Metab. J. 2013, 37, 249–251. [Google Scholar] [CrossRef]
- Hnizdo, E.; Murray, J. Risk of pulmonary tuberculosis relative to silicosis and exposure to silica dust in South African gold miners. Occup. Environ. Med. 1998, 55, 496–502. [Google Scholar] [CrossRef]
- Chan-Yeung, M.; Yeh, A.; Tam, C.; Kam, K.; Leung, C.; Yew, W.; Lam, C. Socio-demographic and geographic indicators and distribution of tuberculosis in Hong Kong: A spatial analysis. Int. J. Tuberc. Lung Dis. 2005, 9, 1320–1326. [Google Scholar]
- Leung, C.C.; Yew, W.W.; Chan, T.Y.K.; Tam, C.M.; Chan, C.Y.; Chan, C.K.; Tang, N.; Chang, K.C.; Law, W.S. Seasonal pattern of tuberculosis in Hong Kong. Int. J. Epidemiol. 2005, 34, 924–930. [Google Scholar] [CrossRef] [PubMed]
- Randremanana, R.V.; Sabatier, P.; Rakotomanana, F.; Randriamanantena, A.; Richard, V. Spatial clustering of pulmonary tuberculosis and impact of the care factors in Antananarivo City. Trop. Med. Int. Health 2009, 14, 429–437. [Google Scholar] [CrossRef]
- Hawker, J.I.; Bakhshi, S.S.; Ali, S.; Farrington, C. Ecological analysis of ethnic differences in relation between tuberculosis and poverty. BMJ 1999, 319, 1031–1034. [Google Scholar] [CrossRef] [PubMed]
- De Quijano, E.D.; Brugal, M.T.; Pasarín, M.; Galdós-Tangüís, H.; Caylà, J.; Borrell, C. The influence of social inequalities, social unrest and extreme poverty on tuberculosis morbidity in the city of Barcelona. Rev. Esp. Salud Pública 2001, 75, 517–528. [Google Scholar]
- Uthman, O. Spatial and temporal variations in incidence of tuberculosis in Africa, 1991 to 2005. World Health Popul. 2007, 10, 5–15. [Google Scholar]
- Disease Control Bureau of the Ministry of Health. Available online: http://www.moh.gov.cn/mohbgt/pw10409/200804/27103.shtml (accessed on 12 October 2014).
- Norris, M.; Lecavalier, L. Evaluating the use of exploratory factor analysis in developmental disability psychological research. J. Autism Dev. Disord. 2010, 40, 8–20. [Google Scholar] [CrossRef]
- Tenenhaus, M.; Vinzi, V.E.; Chatelin, Y.-M.; Lauro, C. PLS path modeling. Comput. Stat. Data Anal. 2005, 48, 159–205. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Wold, H.O. Systems under Indirect Observation: Causality, Structure, Prediction; North Holland: Amsterdam, The Netherlands, 1982; Volume 139. [Google Scholar]
- Wold, S. PLS for multivariate linear modeling. Chemom. Methods Mol. Design 1995, 2, 195–218. [Google Scholar]
- Vitaliano, P.P.; Scanlan, J.M.; Zhang, J.; Savage, M.V.; Hirsch, I.B.; Siegler, I.C. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom. Med. 2002, 64, 418–435. [Google Scholar] [CrossRef]
- Liu, Y.; Jiang, S.; Wang, R.; Li, X.; Yuan, Z.; Wang, L.; Xue, F. Spatial epidemiology and spatial ecology study of worldwide drug-resistant tuberculosis. Int. J. Health Geogr. 2011. [Google Scholar] [CrossRef]
- Wold, H. Model construction and evaluation when theoretical knowledge is scarce. In Evaluation of Econometric Models; Academic Press: Waltham, MA, USA, 1980; pp. 47–74. [Google Scholar]
- Fotheringham, A.S.; Charlton, M.E.; Brunsdon, C. Geographically weighted regression: A natural evolution of the expansion method for spatial data analysis. Environ. Plan. A 1998, 30, 1905–1927. [Google Scholar] [CrossRef]
- Nakaya, T. GWR 4.0. Available online: https://geodacenter.asu.edu/gwr_software (accessed on 26 December 2014).
- Charlton, M.; Fotheringham, S.; Brunsdon, C. Geographically Weighted Regression, White Paper; National Centre for Geocomputation, National University of Ireland Maynooth: Maynooth, ON, Canada, 2009. [Google Scholar]
- Nakaya, T. GWR4 User Manual. Available online: http://www. st-andrews. ac. uk/geoinformatics/wp-content/uploads/GWR4manual_201311. pdf (accessed on 26 December 2014).
- ArcGIS v10.1; ESRI Inc.: Redlands, CA, USA, 2012. Available online: http://www.esri.com (accessed on 26 December 2014).
- Fotheringham, A.S.; Brunsdon, C.; Charlton, M. Geographically Weighted Regression: The Analysis of Spatially Varying Relationships; John Wiley & Sons: Hoboken, NJ, USA, 2003. [Google Scholar]
- Siddiqi, K.; Barnes, H.; Williams, R. Tuberculosis and poverty in the ethnic minority population of West Yorkshire: An ecological study. Commun. Dis. Public Health 2001, 4, 242–246. [Google Scholar]
- Kakchapati, S.; Choonpradub, C.; Lim, A. Spatial and temporal variations in tuberculosis incidence, Nepal. Southeast Asian J. Trop. Med. Public Health 2014, 45, 95–102. [Google Scholar] [PubMed]
- Huang, Z.Y.; de Boer, W.F.; van Langevelde, F.; Xu, C.; Jebara, K.B.; Berlingieri, F.; Prins, H.H. Dilution effect in bovine tuberculosis: Risk factors for regional disease occurrence in Africa. Proc. R. Soc. B Biol. Sci. 2013. [Google Scholar] [CrossRef]
- Vargas, M.; Furuya, M.; Pérez-Guzmán, C. Effect of altitude on the frequency of pulmonary tuberculosis. Int. J. Tuberc. Lung Dis. 2004, 8, 1321–1324. [Google Scholar]
- Mansoer, J.; Kibuga, D.; Borgdorff, M. Altitude: A determinant for tuberculosis in Kenya? Int. J. Tuberc. Lung Dis. 1999, 3, 156–161. [Google Scholar]
- Guidi, E.; Angelini, L.; Lupi, S.; Vicentini, C.; Mares, D.; Manfredini, S.; Contini, C. Epidemiological, social and public health aspects of tuberculosis in Ferrara in the 19th century. Infez. Med. 2011, 19, 266–277. [Google Scholar]
- Sarkar, S.; Song, Y.; Sarkar, S.; Kipen, H.M.; Laumbach, R.J.; Zhang, J.; Strickland, P.A.O.; Gardner, C.R.; Schwander, S. Suppression of the NF-κB pathway by diesel exhaust particles impairs human antimycobacterial immunity. J. Immunol. 2012, 188, 2778–2793. [Google Scholar] [CrossRef]
- Ahlburg, D.A.; Initiative, S.T.; Organization, W.H. The Economic Impacts of Tuberculosis; Stop TB Initiative, World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Dos Santos, M.A.; Albuquerque, M.F.; Ximenes, R.A.; Lucena-Silva, N.L.; Braga, C.; Campelo, A.R.; Dantas, O.M.; Montarroyos, U.R.; Souza, W.V.; Kawasaki, A.M. Risk factors for treatment delay in pulmonary tuberculosis in Recife, Brazil. BMC Public Health 2005. [Google Scholar] [CrossRef]
- Mangtani, P.; Jolley, D.J.; Watson, J.M.; Rodrigues, L.C. Socioeconomic deprivation and notification rates for tuberculosis in London during 1982–1991. BMJ 1995, 310, 963–966. [Google Scholar] [CrossRef] [PubMed]
- Jakubowiak, W.; Bogorodskaya, E.; Borisov, E.; Danilova, D.; Kourbatova, E. Risk factors associated with default among new pulmonary TB patients and social support in six Russian regions. Int. J. Tuberc. Lung Dis. 2007, 11, 46–53. [Google Scholar]
- Jie, H.; Zhu, Y.; Wang, X.; Li, J.; Jin, Y. The clinical characteristics of tuberculosis of Tibetan Plateau area. Plateau Med. J. 2001, 4, 256–256. (In Chinese) [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, W.; Gong, J.; Zhou, J.; Zhao, Y.; Tan, J.; Ibrahim, A.N.; Zhou, Y. A Spatial, Social and Environmental Study of Tuberculosis in China Using Statistical and GIS Technology. Int. J. Environ. Res. Public Health 2015, 12, 1425-1448. https://doi.org/10.3390/ijerph120201425
Sun W, Gong J, Zhou J, Zhao Y, Tan J, Ibrahim AN, Zhou Y. A Spatial, Social and Environmental Study of Tuberculosis in China Using Statistical and GIS Technology. International Journal of Environmental Research and Public Health. 2015; 12(2):1425-1448. https://doi.org/10.3390/ijerph120201425
Chicago/Turabian StyleSun, Wenyi, Jianhua Gong, Jieping Zhou, Yanlin Zhao, Junxiang Tan, Abdoul Nasser Ibrahim, and Yang Zhou. 2015. "A Spatial, Social and Environmental Study of Tuberculosis in China Using Statistical and GIS Technology" International Journal of Environmental Research and Public Health 12, no. 2: 1425-1448. https://doi.org/10.3390/ijerph120201425
APA StyleSun, W., Gong, J., Zhou, J., Zhao, Y., Tan, J., Ibrahim, A. N., & Zhou, Y. (2015). A Spatial, Social and Environmental Study of Tuberculosis in China Using Statistical and GIS Technology. International Journal of Environmental Research and Public Health, 12(2), 1425-1448. https://doi.org/10.3390/ijerph120201425





