Help Received for Perceived Needs Related to Mental Health in a Montreal (Canada) Epidemiological Catchment Area
Abstract
:1. Introduction
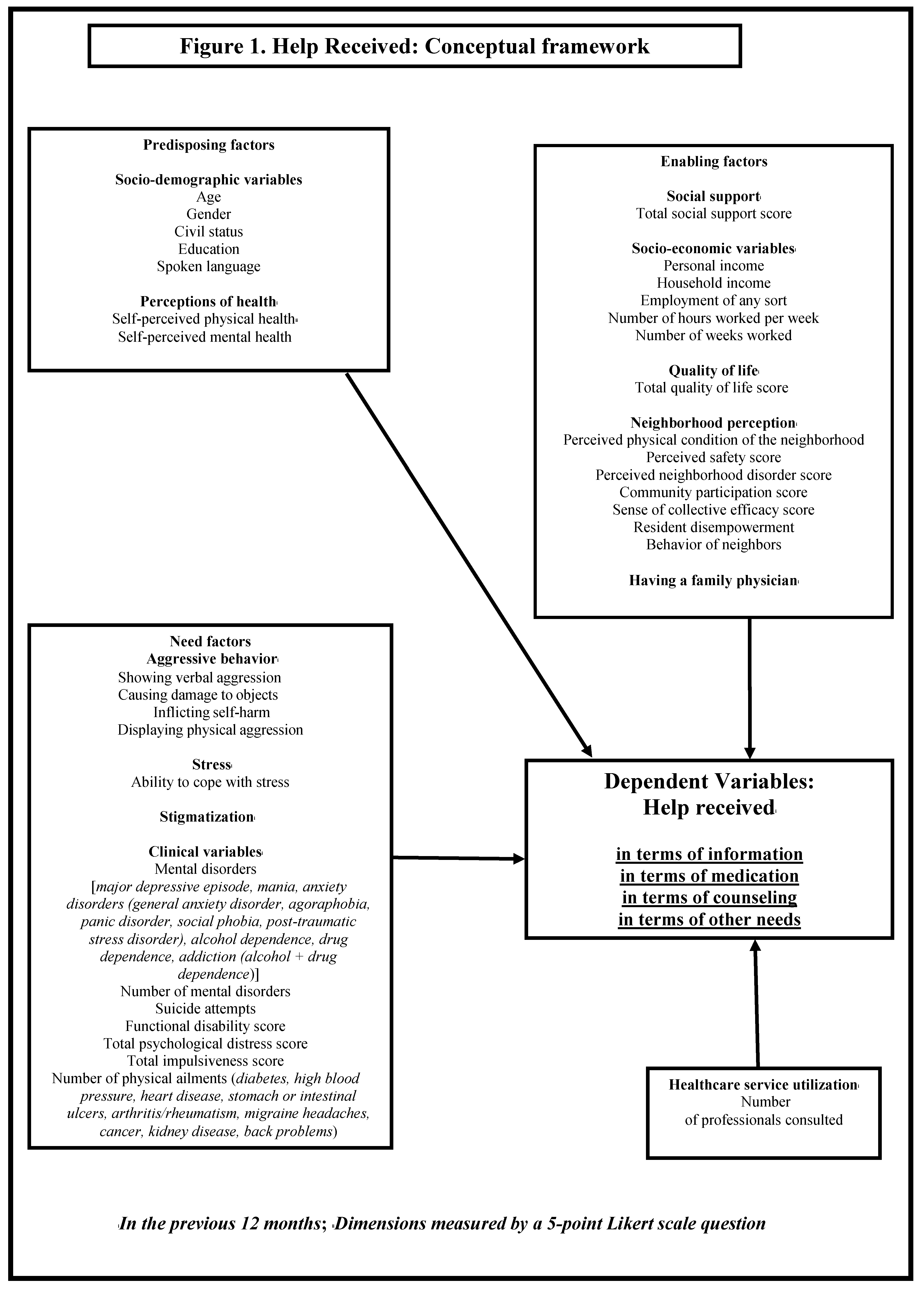
2. Methods
2.1. Study Design and Setting
2.2. Selection Criteria and Survey Sample
2.3. Variables and Measurement Instruments
2.4. Analyses
3. Results
| Variables | Total Sample | Information Help | Medication Help | Counselling Help | |||
|---|---|---|---|---|---|---|---|
| (N = 571) | Help Received (N = 229) | Help Received (N = 269) | Help Received (N = 277) | ||||
| N (%) Mean (SD) | N (%) Mean (SD) | N (%) Mean (SD) | N (%) Mean (SD) | ||||
| Predisposing factors | Socio-demographic | Age [Mean (SD)] | 42.6 (13.4) | 41.1 (12.8) | 46.0 (12.7) | 42.3 (12.7) | |
| Gender [N (%)] | Women | 386 (67.6) | 151 (65.9) | 180 (66.9) | 197 (71.1) | ||
| Men | 185 (32.4) | 78 (34.1) | 89 (33.1) | 80 (28.9) | |||
| Civil status [N (%)] | Single | 374 (65.5) | 149 (65.1) | 186 (69.1) | 182 (65.7) | ||
| In a conjugal relationship | 197 (34.5) | 80 (34.9) | 83 (30.9) | 95 (34.3) | |||
| Education [N (%)] | Less than high school | 101 (17.7) | 33 (14.4) | 55 (20.4) | 44 (15.9) | ||
| High school and above | 470 (82.3) | 196 (85.6) | 214 (79.6) | 233 (84.1) | |||
| Perceptions of health i | Self-perceived physical health [N (%)] | Poor or fair | 223 (39.1) | 90 (39.3) | 123 (45.7) | 103 (37.2) | |
| Good | 201 (35.2) | 79 (34.5) | 90 (33.5) | 98 (35.4) | |||
| Excellent or very good | 147 (25.7) | 60 (26.2) | 56 (20.8) | 76 (27.4) | |||
| Self-perceived mental health [N (%)] | Poor or fair | 239 (41.9) | 110 (48.0) | 134 (49.8) | 131 (47.3) | ||
| Good | 198 (34.7) | 70 (30.6) | 84 (31.2) | 82 (29.6) | |||
| Excellent or very good | 134 (23.5) | 49 (21.4) | 51 (19.0) | 64 (23.1) | |||
| Enabling factors | Socio-economic [Mean (SD)] | Income | Household income | 55,583.3 (45,704.6) | 55,702.6 (44,487.7) | 49,110.8 (45,112.5) | 57,878.6 (47,859.5) |
| Personal income | 32,413.1 (26,918.4) | 34,692.6 (30,336.4) | 31,165.0 (28,047.8) | 34,939.9 (30,792.6) | |||
| Total social support score | 79 (9.9) | 79 (9.7) | 77.4 (10.4) | 78.9 (10.4) | |||
| Total quality of life score | 101.6 (15.7) | 100.6 (15.3) | 99.6 (16.7) | 100.9 (16.7) | |||
| Have a family doctor i [N (%)] | 401 (70.2) | 172 (75.1) | 208 (77.3) | 208 (75.1) | |||
| Perception of neighborhood [Mean (SD)] | Perceived physical condition of neighborhood a | 44.6 (11.0) | 45.8 (10.1) | 44.6 (11.6) | 44.0 (11.3) | ||
| Perceived safety b | 3.7 (1.4) | 3.6 (1.4) | 3.9 (1.4) | 3.7 (1.4) | |||
| Perceived disorder in neighborhood c | 42.1 (21.4) | 41.4 (20.9) | 42.4 (21.7) | 44.2 (22.0) | |||
| Community participation score d | 0.9 (1.1) | 1.0 (1.1) | 0.8 (1.1) | 0.9 (1.1) | |||
| Sense of collective efficacy e | 34.4 (6.9) | 34.2 (7.1) | 34.1 (7.1) | 34.1 (7.2) | |||
| Resident disempowerment f | 12.4 (5.9) | 12.3 (5.9) | 12.9 (6.3) | 12.6 (6.3) | |||
| Behavior of neighbors g | 15.2 (9.9) | 15.5 (10.2) | 15.2 (9.9) | 14.9 (9.7) | |||
| Need factors | Behavior i | Total impulsiveness score [Mean (SD)] h | 69.3 (5.7) | 69.3 (5.3) | 69.7 (5.6) | 69.2 (5.3) | |
| Showing verbal aggression [N (%)] | 317 (55.5) | 127 (55.5) | 134 (49.8) | 151 (54.5) | |||
| Causing damage to objects [N (%)] | 167 (29.2) | 72 (31.4) | 54 (20.1) | 85 (30.7) | |||
| Inflicting self-harm [N (%)] | 42 (7.4) | 21 (9.2) | 19 (7.1) | 22 (7.9) | |||
| Displaying physical aggression [N (%)] | 52 (9.1) | 21 (9.2) | 15 (5.6) | 31 (11.2) | |||
| Clinical variables i | Health problems diagnosed [N (%)] | Major depressive episode | 117 (20.5) | 60 (26.2) | 68 (25.3) | 68 (24.5) | |
| Mania | 23 (4.0) | 10 (4.4) | 13 (4.8) | 15 (5.4) | |||
| General anxiety disorder | 11 (1.9) | 6 (2.6) | 5 (1.9) | 8 (2.9) | |||
| Panic disorder | 24 (4.2) | 11 (4.8) | 17 (6.3) | 19 (6.9) | |||
| Social phobia | 34 (6.0) | 17 (7.4) | 17 (6.3) | 19 (6.9) | |||
| Agoraphobia | 12 (2.1) | 7 (3.1) | 7 (2.6) | 6 (2.2) | |||
| Post-traumatic stress disorder | 45 (7.9) | 26 (11.4) | 32 (11.9) | 30 (10.8) | |||
| Alcohol dependence | 24 (4.2) | 7 (3.1) | 6 (2.2) | 14 (5.1) | |||
| Drug dependence | 25 (4.4) | 14 (6.1) | 10 (3.7) | 15 (5.4) | |||
| Addiction | 42 (7.4) | 18 (7.9) | 15 (5.6) | 24 (8.7) | |||
| Any MHD | 133 (23.3) | 67 (29.3) | 74 (27.5) | 78 (28.2) | |||
| [Mean (SD)] | Total psychological distress score j | 11.9 (6.9) | 12.7 (7.3) | 13.5 (7.4) | 12.5 (7.2) | ||
| Number of physical illnesses | 1.2 (1.4) | 1.1 (1.4) | 1.5 (1.5) | 1.1 (1.4) | |||
| Number of mental disorders | 0.3 (0.5) | 0.3 (0.5) | 0.3 (0.6) | 0.3 (0.6) | |||
| Healthcare service utilization [Mean (SD)] | Number of professionals consulted | 2.6 (1.8) | 3.2 (1.8) | 3 (1.8) | 3.5 (1.8) | ||
| Variables | Level of Help (Information, Medication, Counselling and Other) | Bivariate Multinomial Analyses | ||||||
|---|---|---|---|---|---|---|---|---|
| Help Needed But not Received (N = 104) | Help Partially Received (N = 374) | Help Fully Received (N = 93) | Help Partially Received vs. no Help Received | Help Fully Received vs. no Help Received | ||||
| N (%) Mean (SD) | N (%) Mean (SD) | N (% ) Mean (SD) | p Value | p Value | ||||
| Predisposing factors | Socio-demographic | Age [Mean (SD)] | 39.0 (13.5) | 43.4 (13.7) | 42.9 (11.7) | 0.003 t | 0.042 t | |
| Gender [N (%)] | Women | 70 (67.3) | 256 (68.4) | 60 (64.5) | 0.825 q | 0.680 q | ||
| Men | 34 (32.7) | 118 (31.6) | 33 (35.5) | |||||
| Civil status [N (%)] | Single | 66 (63.5) | 245 (65.5) | 63 (67.7) | 0.699 q | 0.528 q | ||
| In a conjugal relationship | 38 (36.5) | 129 (34.5) | 30 (32.3) | |||||
| Education [N (%)] | Less than high school | 19 (18.3) | 68 (18.2) | 14 (15.1) | 0.984 q | 0.547 q | ||
| High school and above | 85 (81.7) | 306 (81.8) | 79 (84.9) | |||||
| Perceptions of health i | Self-perceived physical health [N (%)] | Poor or fair | 39 (37.5) | 142 (38.0) | 42 (45.2) | 0.953 q | 0.220 q | |
| Good | 41 (39.4) | 130 (34.8) | 30 (32.3) | |||||
| Excellent or very good | 24 (23.1) | 102 (27.3) | 21 (22.6) | |||||
| Self-perceived mental health [N (%)] | Poor or fair | 44 (42.3) | 133 (35.6) | 62 (66.7) | 0.058 q | 0.004 q | ||
| Good | 45 (43.3) | 133 (35.6) | 20 (21.5) | |||||
| Excellent or very good | 15 (14.4) | 108 (28.9) | 11 (11.8) | |||||
| Enabling factors | Socio-economic [Mean (SD)] | Income | Household income | 55108.2 | 56701.0 | 51619.8 (51963.8) | 0.457 t | 0.420 t |
| (45707.9) | (44091.0) | |||||||
| Personal income | 29644.7 | 32557.8 | 34927.3 (39180.6) | |||||
| (22088.1) | (24294.2) | |||||||
| Total social support score | 78.6 (9.3) | 79.8 (9.9) | 76.4 (10.3) | 0.270 t | 0.135 t | |||
| Total quality of life score | 100.5 (14.7) | 103.1 (15.7) | 96.3 (15.7) | 0.126 t | 0.071 t | |||
| Having a family doctor i [N (%)] | 51 (49.0) | 281 (75.1) | 69 (74.2) | <0.001 q | <0.001 q | |||
| Perception of neighborhood [Mean (SD)] | Perceived physical condition of neighborhood a | 44.6 (10,7) | 44.5 (10.8) | 44.5 (11.8) | 0.934 t | 0.948 t | ||
| Perceived safety b | 3.6 (1.2) | 3.7 (1.4) | 3.8 (1.5) | 0.444 t | 0.418 t | |||
| Perceived disorder in neighborhood c | 39.9 (22.6) | 41.8 (20.7) | 45.7 (23) | 0.435 t | 0.062 t | |||
| Community participation score d | 0.8 (11) | 0.9 (1) | 1 (1.2) | 0.773 t | 0.286 t | |||
| Sense of collective efficacy e | 34.1 (6.6) | 34.9 (6.9) | 32.9 (7.3) | 0.314 t | 0.224 t | |||
| Resident disempowerment f | 12.2 (5.3) | 12.1 (5.9) | 13.7 (6.6) | 0.965 t | 0.086 t | |||
| Behavior of neighbors g | 15 (9.9) | 15.1 (9.9) | 15.5 (9.8) | 0.905 t | 0.732 t | |||
| Need factors | Behavior i | Total impulsiveness score [Mean (SD)] h | 69.4 (6.5) | 69.1 (5.6) | 70.2 (5.0) | 0.561 t | 0.334 t | |
| Showing verbal aggression [N (%)] | 68 (65.4) | 203 (54.3) | 46 (49.5) | 0.044 q | 0.025 q | |||
| Causing damage to objects [N (%)] | 39 (37.5) | 107 (28.6) | 21 (22.6) | 0.083 q | 0.024 q | |||
| Inflicting self-harm [N (%)] | 9 (8.7) | 22 (5.9) | 11 (11.8) | 0.313 q | 0.463 q | |||
| Displaying physical aggression [N (%)] | 12 (11.5) | 33 (8.8) | 7 (7.5) | 0.403 q | 0.344 q | |||
| Clinical variables i | Health problems diagnosed [N (%)] | Major depressive episode | 22 (21.2) | 60 (16.0) | 35 (37.6) | 0.223 q | 0.012 q | |
| Mania | 4 (3.8) | 13 (3.5) | 6 (6.5) | 0.857 q | 0.411 q | |||
| Panic disorder | 2 (1.9) | 13 (3.5) | 9 (9.7) | 0.429 q | 0.033 q | |||
| Social phobia | 7 (6.7) | 19 (5.1) | 8 (8.6) | 0.513 q | 0.622 q | |||
| Addiction | 13 (12.5) | 17 (4.5) | 12 (12.9) | 0.004 q | 0.932 q | |||
| Any mental disorder | 24 (23.1) | 72 (19.3) | 37 (39.8) | 0.390 q | 0.012 q | |||
| [Mean (SD)] | Total psychological distress score j | 12.0 (5.7) | 11.1 (6.8) | 15.4 (7.3) | 0.201 t | 0.001 t | ||
| Number of physical disorders | 0.8 (1.2) | 1.2 (1.4) | 1.3 (1.4) | 0.016 t | 0.019 t | |||
| Number of mental disorders | 0.3 (0.5) | 0.2 (0.5) | 0.5 (0.6) | 0.591 t | 0.015 t | |||
| Healthcare service utilization [Mean (SD)] | Number of professionals consulted | 1.3 (1.1) | 2.6 (1.7) | 3.9 (1.9) | <0.001 t | <0.001 t | ||
| Variable | Level of Help | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Help Partially Received | Help Fully Received | ||||||||||
| Beta | p | OR | 95% CI | Beta | p | OR | 95% CI | ||||
| LL | UL | LL | UL | ||||||||
| Predisposing factors | Age | 0.023 | 0.017 | 1.023 | 1.004 | 1.042 | 0.023 | 0.071 | 1.023 | 0.998 | 1.049 |
| Gender (men) | 0.425 | 0.116 | 1.530 | 0.900 | 2.601 | 0.798 | 0.027 | 2.221 | 1.097 | 4.499 | |
| Need factors | Showing verbal aggression in prior 12 months | 0.387 | 0.132 | 0.679 | 0.411 | 1.123 | 0.822 | 0.016 | 0.439 | 0.225 | 0.857 |
| Psychological distress score | 0.027 | 0.164 | 0.973 | 0.937 | 1.011 | 0.048 | 0.047 | 1.049 | 1.001 | 1.101 | |
| Addiction (drug and alcohol) in prior 12 months | 1.344 | 0.004 | 0.261 | 0.104 | 0.651 | 0.733 | 0.196 | 0.481 | 0.158 | 1.458 | |
| Healthcare service utilization | Number of healthcare professionals consulted in prior 12 months | 0.803 | <0.001 | 2.232 | 1.790 | 2.783 | 1.182 | <0.001 | 3.262 | 2.531 | 4.204 |
| Intercept | 0.659 | 0.214 | 4.231 | <0.001 | |||||||
4. Discussion
Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Demler, O.; Frank, R.G.; Olfson, M.; Pincus, H.A.; Walters, E.E.; Wang, P.; Wells, K.B.; Zaslavsky, A.M. Prevalence and treatment of mental disorders, 1990 to 2003. N. Engl. J. Med. 2005, 352, 2515–2523. [Google Scholar] [CrossRef] [PubMed]
- Andrews, G.; Issakidis, C.; Carter, G. Shortfall in mental health service utilisation. Br. J. Psychiat. 2001, 179, 417–425. [Google Scholar] [CrossRef]
- Whiteford, H.A.; Buckingham, W.J.; Harris, M.G.; Burgess, P.M.; Pirkis, J.E.; Barendregt, J.J.; Hall, W.D. Estimating treatment rates for mental disorders in Australia. Aust. Health Rev. 2014, 38, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Herman, A.; Stein, D.J.; Heeringa, S.G.; Jackson, P.B.; Moomal, H.; Kessler, R.C. Twelve-month mental disorders in South Africa: Prevalence, service use and demographic correlates in the population-based South African stress and health study. Psychol. Med. 2008, 38, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Oakley Browne, M.A.; Wells, J.E.; McGee, M.A.; New Zealand Mental Health Survey Research Team. Twelve-month and lifetime health service use in Te Rau Hinengaro: The New Zealand Mental Health Survey. Aust. N. Zeal. J. Psychiat. 2006, 40, 855–864. [Google Scholar] [CrossRef]
- Druss, B.G.; Wang, P.S.; Sampson, N.A.; Olfson, M.; Pincus, H.A.; Wells, K.B.; Kessler, R.C. Understanding mental health treatment in persons without mental diagnoses: Results from the National Comorbidity Survey Replication. Arch. Gen. Psychiat. 2007, 64, 1196–1203. [Google Scholar] [CrossRef] [PubMed]
- Demyttenaere, K.; Bruffaerts, R.; Posada-Villa, J.; Gasquet, I.; Kovess, V.; Lepine, J.P.; Angermeyer, M.C.; Bernert, S.; de Girolamo, G.; Morosini, P.; et al. Prevalence, severity and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 2004, 291, 2581–2590. [Google Scholar] [PubMed]
- Sunderland, A.; Findlay, L.C. Perceived need for mental health care in Canada: Results from the 2012 Canadian Community Heatlh Survey- Mental health. Health Reports 2013, 24, 3–9. [Google Scholar]
- Prins, M.; Meadows, G.; Bobevski, I.; Graham, A.; Verhaak, P.; van der Meer, K.; Penninx, B.; Bensing, J. Perceived need for mental health care and barriers to care in the Netherlands and Australia. Soc. Psychiat. Psychiatr. Epidemiol. 2011, 46, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Parslow, R.A.; Jorm, A.F. Who uses mental health services in Australia? An analysis of data from the National Survey of Mental Health and Wellbeing. Aust. N. Zeal. J. Psychiat. 2000, 34, 997–1008. [Google Scholar] [CrossRef]
- Wang, S.; Lane, M.; Olfson, M.; Pincus, H.A.; Wells, K.B.; Kessler, R.C. Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Arch. Gen. Psychiat. 2005, 62, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Meadows, G.N.; Burgess, M. Perceived need for mental health care: Findings from the 2007 Australian Survey of Mental Health and Wellbeing. Aust. N. Zeal. J. Psychiat. 2009, 43, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Prins, M.A.; Verhaak, P.F.; van der Meer, K.; Penninx, B.W.; Bensing, J.M. Primary care patients with anxiety and depression: Need for care from the patient’s perspective. J. Affect. Disord. 2009, 119, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Pagura, J.; Fotti, S.; Katz, L.Y.; Sareen, J.; Swampy Cree Suicide Prevention Team. Help seeking and perceived need for mental health care among individuals in Canada with suicidal behaviors. Psychiatr. Serv. 2009, 60, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Urbanoski, K.; Cairney, J.; Bassani, D.G.; Rush, B.R. Perceived unmet need for mental health care for Canadians with co-occurring mental and substance use disorders. Psychiatr. Serv. 2008, 59, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Starkes, J.M.; Poulin, C.C.; Kisely, S.R. Unmet need for the treatment of depression in Atlantic Canada. Can. J. Psychiat. 2005, 50, 580–590. [Google Scholar]
- Sareen, J.; Stein, M.B.; Campbell, D.W.; Hassard, T.; Menec, V. The relation between perceived need for mental health treatment, DSM diagnosis, and quality of life: A Canadian population-based survey. Can. J. Psychiat. 2005, 50, 87–94. [Google Scholar]
- Mojtabai, R.; Olfson, M.; Mechanic, D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch. Gen. Psychiat. 2002, 59, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.H.; Park, J. The nature and correlates of unmet health care needs in Ontario, Canada. Soc. Sci. Med. 2006, 62, 2291–2300. [Google Scholar] [CrossRef] [PubMed]
- Mojtabai, R. Unmet need for treatment of major depression in the United States. Psychiatr. Serv. 2009, 60, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Meadows, G.; Burgess, P.; Bobevski, I.; Fossey, E.; Harvey, C.; Liaw, S.T. Perceived need for mental health care: Influences of diagnosis, demography and disability. Psychol. Med. 2002, 32, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Meadows, G.N.; Burgess, P.; Fossey, E.; Harvey, C. Perceived need for mental health care—Findings from the Autralian National Survey of Mental Health and Wellbeing. Psychol. Med. 2000, 30, 645–656. [Google Scholar] [CrossRef] [PubMed]
- Van Beljouw, I.; Verhaak, P.; Prins, M.; Cuijpers, P.; Penninx, B.; Bensing, J. Reasons and determinants for not receiving treatment for common mental disorders. Psychiatr. Serv. 2010, 61, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Sareen, J.; Cox, B.J.; Afifi, T.O.; Yu, B.N.; Stein, M.B. Mental health service use in a nationally representative canadian survey. Can. J. Psychiat. 2005, 50, 753–761. [Google Scholar]
- Urbanoski, K.; Rush, B.R.; Wild, T.C.; Bassani, D.G.; Castel, S. Use of mental health care services by Canadians with co-occurring substance dependence and mental disorders. Psychiatr. Serv. 2007, 58, 962–969. [Google Scholar] [CrossRef] [PubMed]
- Sareen, J.; Jagdeo, A.; Cox, B.J.; Clara, I.; ten Have, M.; Belik, S.L.; de Graaf, R.; Stein, M.B. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatr. Serv. 2007, 58, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Wang, J. Perceived barriers to mental health service use among individuals with mental disorders in the Canadian general population. Med. Care 2006, 44, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Meadows, G.; Singh, B.; Burgess, P.; Bobevski, I. Psychiatry and the need for mental health care in Australia: Findings from the National Survey of Mental Health and Wellbeing. Aust. N. Zeal. J. Psychiat. 2002, 36, 210–216. [Google Scholar] [CrossRef]
- Kauer, S.D.; Mangan, C.; Sanci, L. Do online mental health services improve help-seeking for young people? A systematic review. J. Med. Internet. Res. 2014. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M. Predictors of frequent recourse to health professionals by people with severe mental disorders. Can. J. Psychiat. 2015, 60, 77–86. [Google Scholar]
- Pratt, L.A. Serious psychological distress, as measured by the K6, and mortality. Ann. Epidemiol. 2009, 19, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Perreault, M.; Kestens, Y.; Caron, J. Comprehensive determinants of health service utilisation for mental health reasons in a Canadian catchment area. Int. J. Equity Health 2012. [Google Scholar] [CrossRef] [PubMed]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kosidou, K.; Dalman, C.; Lundberg, M.; Hallqvist, J.; Isacsson, G.; Magnusson, C. Socioeconomic status and risk of psychological distress and depression in the Stockholm Public Health Cohort: A population-based study. J. Affect. Disord. 2011, 134, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Torvik, A.F.; Rognmo, K.; Tambs, K. Alcohol use and mental distress as predictors of non-response in a general population health survey: The HUNT study. Soc. Psychiat. Psychiat. Epidemiol. 2012, 47, 805–816. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Tremblay, J.; Schmitz, N.; Caron, J. Predictors of quality of life in a longitudinal study of users with severe mental disorders. Health Qual. Life Outcomes 2013. [Google Scholar] [CrossRef] [PubMed]
- Canadian Community Health Survey—Mental Health and Well-Being—Cycle 1.2; Statistics Canada: Ottawa, Ontario, Canada, 2002.
- Henderson, C.; Noblett, J.; Parke, H.; Clement, S.; Caffrey, A.; Gale-Grant, O.; Schulze, B.; Druss, B.; Thornicroft, G. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiat. 2014, 1, 467–482. [Google Scholar]
- Ngamini Ngui, A.; Perreault, M.; Fleury, M.J.; Caron, J. A multi-level study of the determinants of mental health service utilization. Rev. Epidemiol. Sante Publique 2012, 60, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Caron, J.; Mercier, C.; Tempier, R. L’échelle de satisfaction des Domaines de la vie: La validation québécoise du Satisfaction with Life Domains Scale. Sant. Ment. Que. 1997, 22, 195–217. (In French) [Google Scholar] [CrossRef]
- Kessler, R.C.; Andrews, G.; Mroczek, D.; Ustun, B.; Wittchen, H. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int. J. Meth. Psychiatr. Res. 1998, 7, 171–185. [Google Scholar] [CrossRef]
- Wittchen, H.U. Reliability and validity studies of the WHO–Composite International Diagnostic Interview (CIDI): A critical review. J. Psychiatr. Res. 1994, 28, 57–84. [Google Scholar] [CrossRef]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.L.; Manderscheid, R.W.; Walters, E.E.; et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiat. 2003, 60, 184–189. [Google Scholar] [PubMed]
- Barratt, E.S. Impulsiveness Subtraits: Arousal and Information Processing; Elsevier: Amsterdam, North Holland, Netherlands, 1985; pp. 137–146. [Google Scholar]
- Rue des Femmes de Montréal. Entendre la souffrance, comprendre la blessure, accueillir et soigner… Pour que cesse l’itinérance. In Commission Permanente du Conseil Municipal sur le Développement Culturel et la Qualité de vie; Rue des Femmes de Montréal: Montréal, QC, Canada, 2008. (In French)
- Plante, M.-C. Lutte contre la pauvreté au Québec: Le cas des jeunes femmes itinérantes. In Service Social; Université de Montréal: Montréal, QC, Canada, 2007. [Google Scholar]
- Kay, S.R.; Wolkenfeld, F.; Murrill, L.M. Profiles of aggression among psychiatric patients. I. Nature and prevalence. J. Nerv. Ment. Dis. 1988, 176, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Cutrona, C.E.; Russell, D.W. The provision of social support and adaptation to stress. Adv. Pers. Relationsh. 1987, 1, 37–67. [Google Scholar]
- Nario-Redmond, M.; Coulton, C. Measuring resident perceptions of neighborhood conditions: Survey methodology; Case Western Reserve University, Mandel School of Applied Social Sciences, Center of Urban Poverty and Social Change: Cleveland, Ohio, USA, 2000. [Google Scholar]
- Perkins, D.D.; Long, D.A. Neighborhoud Sense of Community and Social Capital: A Multi-Level Analysis; Plenum: New York, NY, USA, 2002; pp. 291–318. [Google Scholar]
- Saegert, S.; Winke, G. Crime, social capital, and community participation. Am. J. Community Psychol. 2004, 34, 219–233. [Google Scholar] [PubMed]
- Sampson, R.J.; Morenoff, J.D.; Gannon-Rowley, T. Assessing neighborhood effects: Social processes and new directions in research. Annu. Rev. Soc. 2002, 28, 443–478. [Google Scholar] [CrossRef]
- Morton, L.M.; Cahill, J.; Hartge, P. Reporting participation in epidemiologic studies: A survey of practice. Am. J. Epidemiol. 2006, 163, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Codony, M.; Kovess, V.; Angermeyer, M.C.; Katz, S.J.; Haro, J.M.; De Girolamo, G.; De Graaf, R.; Demyttenaere, K.; Vilagut, G.; et al. Population level of unmet need for mental healthcare in Europe. BR J. Psychiat. 2007, 190, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Grella, C.E.; Karno, M.P.; Warda, U.S.; Moore, A.A.; Niv, N. Perceptions of need and help received for substance dependence in a national probability survey. Psychiatr. Serv. 2009, 60, 1068–1074. [Google Scholar] [CrossRef] [PubMed]
- Caron, J.; Fleury, M.J.; Perreault, M.; Crocker, A.; Tremblay, J.; Tousignant, M.; Kestens, Y.; Cargo, M.; Daniel, M. Prevalence of psychological distress and mental disorders, and use of mental health services in the epidemiological catchment area of Montreal South-West. BMC Psychiat. 2012. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, J.; Gross, R.; Feldman, D. Correlates of a perceived need for mental health assistance and differences between those who do and do not seek help. Soc. Psychiat. Psychiatr. Epidemiol. 1999, 34, 141–146. [Google Scholar] [CrossRef]
- Kessler, R.C.; McGonagle, K.A.; Zhao, S.; Nelson, C.B.; Hughes, M.; Eshleman, S.; Wittchen, H.U.; Kendler, K.S. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results form the National Comorbidity Survey. Arch. Gen. Psychiat. 1994, 51, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.; Goering, P.; Offord, D.R.; Campbell, D.; Boyle, M.H. The use of mental health services in Ontario: Epidemiologic findings. Can. J. Psychiat. 1996, 41, 572–577. [Google Scholar]
- Bebbington, E.; Mardsen, L.; Brewin, C.R. The Need for Psychiatric Treatment in the General Population: The Camberwell Needs for Care Survey. Psychol. Med. 1997, 27, 821–834. [Google Scholar]
- Meadows, G.N.; Bobevski, I. Changes in met perceived need for mental healthcare in Australia from 1997 to 2007. Br. J. Psychiat. J. Ment. Sci. 2011, 199, 479–484. [Google Scholar]
- Lesage, A.; Vasiliadis, H.M.; Gagné, M.A.; Dudgeon, S.; Kasman, N.; Hay, C. Prevalence of Mental Illnesses and Related Service Utilization in Canada: An Analysis of the Canadian Community Health Survey. A Report for the Canadian Collaborative Mental Health Initiative; Canadian Collaborative Mental Health Initiative: Mississauga, ON, Canada, 2006. [Google Scholar]
- Middleboe, T.; Mackeprang, T.; Hansson, L.; Werdelin, G.; Karlsson, H.; Bjarnason, O.; Bengtsson-Tops, A.; Dybbro, J.; Nilsson, L.L.; Sandlund, M.; et al. The Nordic Study on schizophrenic patients living in the community. Subjective needs and perceived help. Eur. Psychiat. 2001, 16, 207–214. [Google Scholar]
- Fossey, E.; Harvey, C.; Mokhtari, M.R.; Meadows, G.N. Self-rated assessment of needs for mental health care: A qualitative analysis. Community Ment. Health J. 2012, 48, 407–419. [Google Scholar] [CrossRef] [PubMed]
- Fassaert, T.; de Wit, M.A.; Tuinebreijer, W.C.; Verhoeff, A.P.; Beekman, A.T.; Dekker, J. Perceived need for mental health care among non-western labour migrants. Soc. Psychiat. Psychiatr. Epidemiol. 2009, 44, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Dhingra, S.S.; Zack, M.; Strine, T.; Pearson, W.S.; Balluz, L. Determining prevalence and correlates of psychiatric treatment with Andersen’s behavorial model of health services use. Psychiatr. Serv. 2010, 61, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Dhingra, S.S.; Zack, M.M.; Strine, T.W.; Druss, B.G.; Berry, J.T.; Balluz, L.S. Psychological distress severity of adults reporting receipt of treatment for mental health problems in the BRFSS. Psychiatr. Serv. 2011, 62, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Caron, J. Determinants and patterns of service utilization and recourse to professionals for mental health reasons. BMC Health Serv. Res. 2014. [Google Scholar] [CrossRef] [PubMed]
- Huppert, F.A.; Whittington, J.E. Symptoms of psychological distress predict 7-year mortality. Psychol. Med. 1995, 25, 1073–1086. [Google Scholar] [CrossRef] [PubMed]
- Ferketich, A.K.; Binkley, F. Psychological distress and cardiosvascular disease: Results from the 2002 National Health Interview Survey. Eur. Heart J. 2005, 26, 1293–1296. [Google Scholar] [CrossRef] [PubMed]
- Rueve, M.E.; Welton, R.S. Violence and mental illness. Psychiat. 2008, 5, 34–48. [Google Scholar]
- Stewart, D.; Bowers, L. Inpatient verbal aggression: Content, target and patient characteristics. J. Psychiat. Ment. Health Nurs. 2013, 20, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Glied, S.; Frank, R.G. Mental illness and violence: Lessons from the evidence. Am. J. Public Health 2014, 104, 5–6. [Google Scholar] [CrossRef] [PubMed]
- Gascon, S.; Leiter, M.P.; Andrés, E.; Santed, M.A.; Pereira, J.P.; Cunha, M.J.; Albesa, A.; Montero-Marín, J.; García-Campayo, J.; Martínez-Jarreta, B. The role of aggressions suffered by healthcare workers as predictors of burnout. J. Clin. Nurs. 2013, 21–22, 3120–3129. [Google Scholar]
- Cunningham, J.A.; Breslin, F.C. Only one in three people with alcohol abuse or dependence ever seek treatment. Addict. Behav. 2004, 29, 221–223. [Google Scholar] [CrossRef]
- Rush, B.R.; Urbanoski, K.A.; Bassani, D.G.; Castel, S.; Wild, T.C. The epidemiology of co-occurring substance use and other mental disorders in Canada: Prevalence, service use, and unmet needs. In Mental Disorder in Canada. An Epidemiological Perspective; Cairney, J., Streiner, D.L., Eds.; University of Toronto Press: Toronto, ON, Canada, 2010; pp. 170–204. [Google Scholar]
- Hasin, D.S.; Stinson, F.S.; Ogburn, E.; Grant, B.F. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiat. 2007, 64, 830–842. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C. The epidemiology of dual diagnosis. Biol. Psychiat. 2004, 56, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Compton, W.M.; Thomas, Y.F.; Stinson, F.S.; Grant, B.F. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Arch. Gen. Psychiat. 2007, 64, 566–576. [Google Scholar] [CrossRef]
- Mojtabai, R. Use of specialty substance abuse and mental health services in adults with substance use disorders inthe community. Drug Alcohol. Depend. 2005, 78, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Imboua, A.; Aubé, D.; Farand, L.; Lambert, Y. General practitioners’ management of mental disorders: A rewarding practice with considerable obstacles. BMC Fam. Pract. 2012. [Google Scholar] [CrossRef]
- Van Boekel, L.C.; Brouwers, E.P.; van Weeghel, J. Garretsen HF Healthcare professionals’ regard towards working with patients with substance use disorders: Comparison of primary care, general psychiatry and specialist addiction services. Drug Alcohol. Depend. 2014, 134, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Berglund, P.A.; Bruce, M.L.; Koch, J.R.; Laska, E.M.; Leaf, P.J.; Manderscheid, R.W.; Rosenheck, R.A.; Walters, E.E.; Wang, P.S. The prevalence and correlates of untreated serious mental illness. Health Serv. Res. 2001, 36, 987–1007. [Google Scholar] [PubMed]
- Edlund, M.J.; Wang, P.S.; Berglund, P.A.; Katz, S.J.; Lin, E.; Kessler, R.C. Dropping out of mental health treatment: Patterns and predictors among epidemiological survey respondents in the United States and Ontario. Am. J. Psychiat. 2002, 159, 845–851. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, K.; Nadeau, L.; Flores-Aranda, J. Femmes, toxicomanie et inadaptation sociale grave: L’intégration des services au long cours. In L’intégration des Services en Toxicomanie; Landry, M., Brochu, S., Patenaude, C., Eds.; Presses de l’Université du Québec: Québec, QC, Canada, 2012. [Google Scholar]
- Wang, S.; Berglund, P.; Olfson, M.; Pincus, H.A.; Wells, K.B.; Kessler, R.C. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiat. 2005, 62, 603–613. [Google Scholar]
- Kuhn, R.; Culhane, D.P. Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: Results from the analysis of administrative data. Am. J. Community Psychol. 1998, 26, 207–232. [Google Scholar] [CrossRef] [PubMed]
- Vasiliadis, H.M.; Lesage, A.; Adair, C.; Wang, P.S.; Kessler, R.C. Do Canada and the United States differ in prevalence of depression and utilization of services? Psychiatr. Serv. 2007, 58, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Carr, V.J.; Johnston, P.J.; Lewin, T.J.; Rajkumar, S.; Carter, G.L.; Issakidis, C. Patterns of service use among persons with schizophrenia and other psychotic disorders. Psychiatr. Serv. 2003, 54, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Narrow, W.E.; Regier, D.A.; Norquist, G.; Rae, D.S.; Kennedy, C.; Arons, B. Mental health service use by Americans with severe mental illnesses. Soc. Psychiat. Psychiatr. Epidemiol. 2000, 35, 147–155. [Google Scholar] [CrossRef]
- Moller-Leimkuhler, A.M. Barriers to help-seeking by men: A review of sociocultural and clinical literature with particular reference to depression. J. Affect. Disord. 2002, 71, 1–9. [Google Scholar] [CrossRef]
- Bertakis, K.D.; Azari, R.; Helms, L.J.; Callahan, E.J.; Robbins, J.A. Gender differences in the utilization of health care services. J. Fam. Pract. 2000, 49, 147–152. [Google Scholar] [PubMed]
- Howard, K.I.; Cornille, T.A.; Lyons, J.S.; Vessey, J.T.; Lueger, R.J.; Saunders, S.M. Patterns of Mental Health Service Utilization. Arch. Gen. Psychiat. 1996, 53, 696–703. [Google Scholar] [CrossRef] [PubMed]
- Lasalvia, A.; Bonetto, C.; Salvi, G.; Bissoli, S.; Tansella, M.; Ruggeri, M. Predictors of changes in needs for care in patients receiving community psychiatric treatment: A 4-year follow-up study. Acta Psychiatr. Scand. Suppl. 2007, 116, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Zhao, S.; Katz, S.J.; Kouzis, A.C.; Frank, R.G.; Edlund, M.; Leaf, P. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am. J. Psychiat. 1999, 156, 115–123. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fleury, M.-J.; Bamvita, J.-M.; Grenier, G.; Caron, J. Help Received for Perceived Needs Related to Mental Health in a Montreal (Canada) Epidemiological Catchment Area. Int. J. Environ. Res. Public Health 2015, 12, 13016-13037. https://doi.org/10.3390/ijerph121013016
Fleury M-J, Bamvita J-M, Grenier G, Caron J. Help Received for Perceived Needs Related to Mental Health in a Montreal (Canada) Epidemiological Catchment Area. International Journal of Environmental Research and Public Health. 2015; 12(10):13016-13037. https://doi.org/10.3390/ijerph121013016
Chicago/Turabian StyleFleury, Marie-Josée, Jean-Marie Bamvita, Guy Grenier, and Jean Caron. 2015. "Help Received for Perceived Needs Related to Mental Health in a Montreal (Canada) Epidemiological Catchment Area" International Journal of Environmental Research and Public Health 12, no. 10: 13016-13037. https://doi.org/10.3390/ijerph121013016
APA StyleFleury, M.-J., Bamvita, J.-M., Grenier, G., & Caron, J. (2015). Help Received for Perceived Needs Related to Mental Health in a Montreal (Canada) Epidemiological Catchment Area. International Journal of Environmental Research and Public Health, 12(10), 13016-13037. https://doi.org/10.3390/ijerph121013016





