Association between Changing Mortality of Digestive Tract Cancers and Water Pollution: A Case Study in the Huai River Basin, China
Abstract
:1. Introduction
2. Results
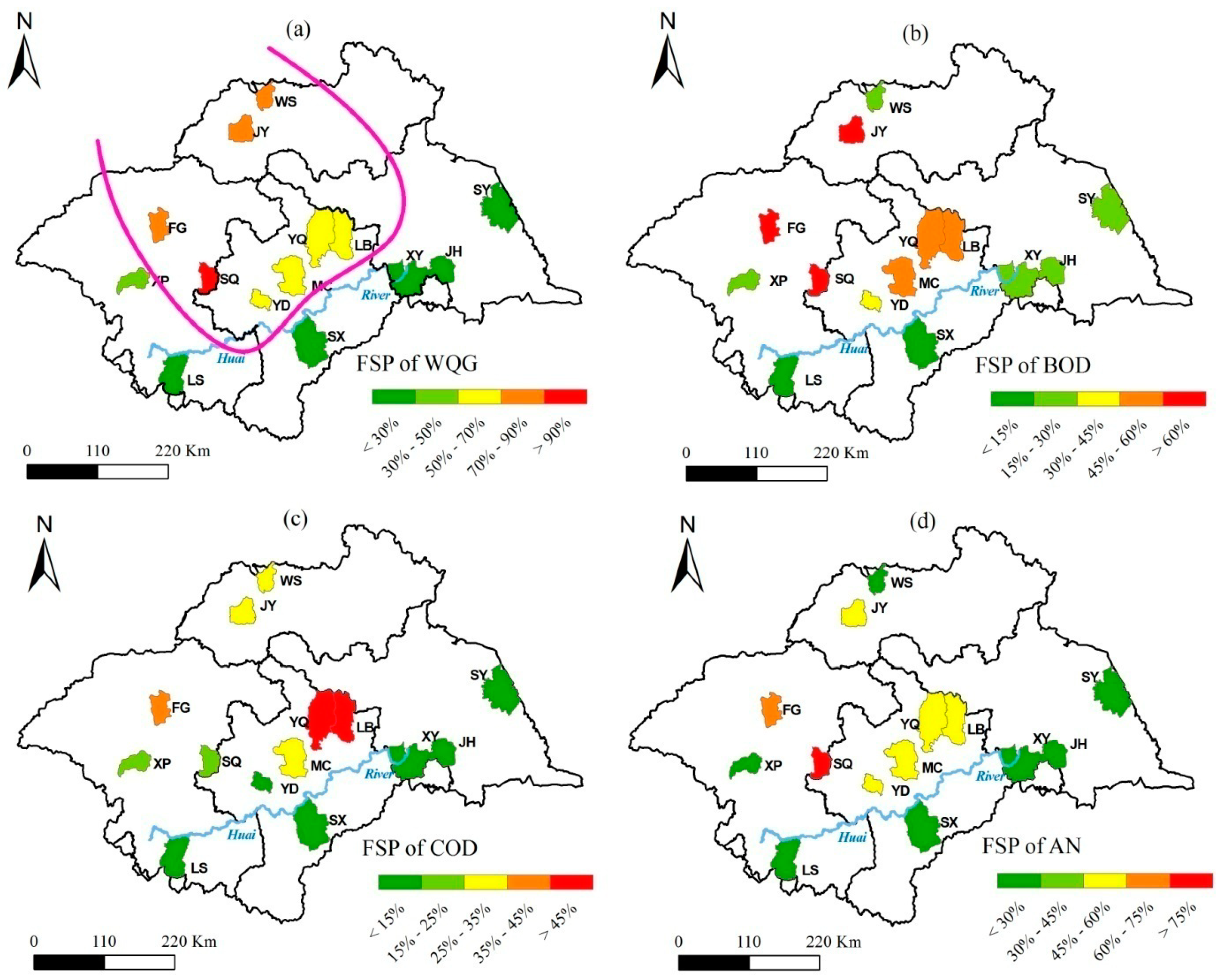
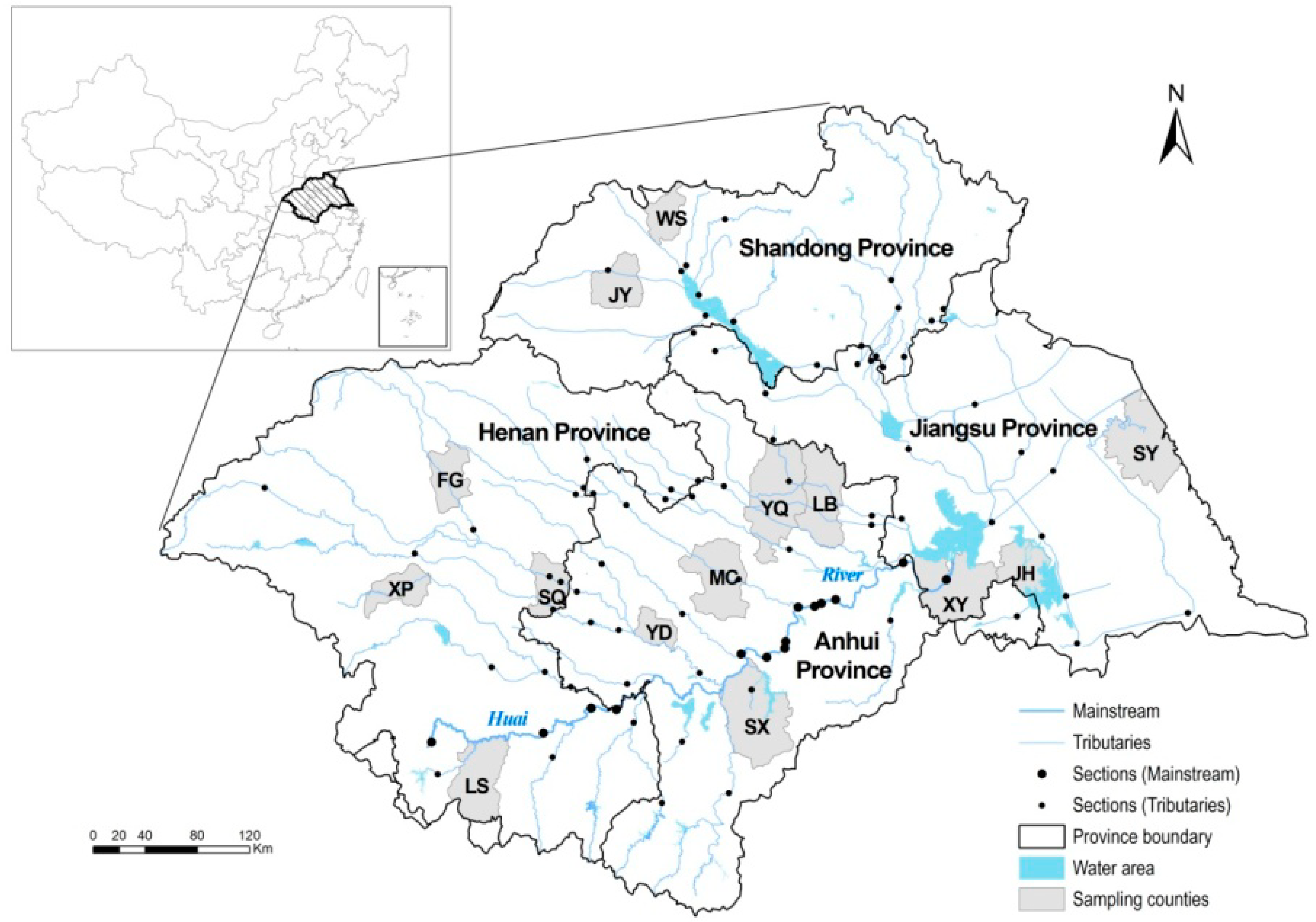
2.1. County-Level Water Pollution
2.2. CMs of Digestive Tract Cancers

2.3. Relation of Water Pollution to CMs at the County Level
| CMs | FSPWQG | FSPBOD | FSPCOD | FSPAN | GDP | POP | DWS |
|---|---|---|---|---|---|---|---|
| CMT | 0.78 ‡ | 0.72 ‡ | 0.42 | 0.83 ‡ | −0.13 | 0.45 | −0.58 † |
| CML | 0.72 ‡ | 0.62 † | 0.37 | 0.72 ‡ | −0.07 | 0.39 | −0.54 † |
| CMG | 0.73 ‡ | 0.62 † | 0.32 | 0.71 ‡ | −0.11 | 0.35 | −0.45 |
| CME | 0.47 * | 0.4 | 0.17 | 0.57 † | −0.34 | 0.32 | −0.37 |
| CMs | Control Variables: GDP-POP-DWS | Control Variables: GDP-POP | |||||||
|---|---|---|---|---|---|---|---|---|---|
| FSPWQG | FSPBOD | FSPCOD | FSPAN | FSPWQG | FSPBOD | FSPCOD | FSPAN | ||
| CMT | 0.67 † | 0.54 | 0.08 | 0.70 † | 0.72 ‡ | 0.62 † | 0.21 | 0.73 ‡ | |
| CML | 0.58 * | 0.41 | 0.05 | 0.57 * | 0.65 † | 0.50 * | 0.18 | 0.63 † | |
| CMG | 0.66 † | 0.45 | 0.06 | 0.56 * | 0.67 † | 0.50 * | 0.15 | 0.60 † | |
| CME | 0.27 | 0.07 | −0.14 | 0.22 | 0.29 | 0.12 | −0.08 | 0.24 | |
3. Discussion
4. Materials and Methods
4.1. Data Collection
4.1.1. Surface Water Quality
4.1.2. Cancer Mortality Data
| Deaths | ICD-10 |
|---|---|
| Neoplasm | C00-D48 |
| Digestive cancer | C15-C20 |
| Esophagus cancer | C15 |
| Gastric cancer | C16 |
| Liver cancer | C22 |
4.2. Socioeconomic Factors
4.3. Indices Calculation
4.3.1. Frequency of Serious Pollution
4.3.2. CM of Digestive Tract Cancers
4.4. Correlation Analysis
5. Conclusions
Supplementary Files
Supplementary File 1Acknowledgements
Author Contributions
Conflicts of interest
References
- Kan, H. Environment and health in China: Challenges and opportunities. Environ. Health Perspect. 2009, 117, 530–531. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Maurer, C.; Wang, Y.; Xue, S.; Davis, D.L. Water pollution and human health in China. Environ. Health Perspect. 1999, 107, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Environmental Protection of the People’s Republic of China. China Environmental Quality Report 1998–2007; China Environment Science Press: Beijing, China, 2008.
- Ji, W.; Zhuang, D.; Ren, H.; Jiang, D.; Huang, Y.; Xu, X.; Chen, W.; Jiang, X. Spatiotemporal variation of surface water quality for decades: A case study of huai river system, China. Water Sci. Technol. 2013, 68, 1233–1241. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.H.; Zhuang, D.F. Atlas of the Water Environment and Digestive Cancer Mortality in the Huai River Basin; Springer: Beijing, China, 2014; p. 249. [Google Scholar]
- Zhang, Y.; Xia, J.; Liang, T.; Shao, Q. Impact of water projects on river flow regimes and water quality in Huai River Basin. Water Resour. Manage. 2010, 24, 889–908. [Google Scholar] [CrossRef]
- Editorial Committee for the Atlas of Cancer Mortality in the People’s Republic of China. Atlas of Cancer Mortality in the People’s Republic of China; China Map Press: Beijing, China, 1979.
- China CDC. Study Report on Key Areas of Cancer Incidence in Huai River Basin and Risk Factors (Restricted); Peking Union Medical College Press: Beijing, China, 2006. (In Chinese) [Google Scholar]
- Wan, X.; Zhou, M.; Tao, Z.; Ding, D.; Yang, G. Epidemiologic application of verbal autopsy to investigate the high occurrence of cancer along the Huai River Basin, China. Popul. Health Metrics 2011, 9, 37–45. [Google Scholar] [CrossRef]
- Yu, J.L.; Zhang, S.Q. Analysis on Environmental Pollution and Public Health Reflected by “Cancer Villages” in China. In Proceedings of the Annual Meeting of Chinese Society for Environmental Science, Wuhan City, China, 28 June 2009; p. 10.
- Kulldorff, M.; Song, C.H.; Gregorio, D.; Samociuk, H.; DeChello, L. Cancer map patterns—Are they random or not? Amer. J. Prev. Med. 2006, 30, S37–S49. [Google Scholar] [CrossRef]
- Aragones, N.; Goicoa, T.; Pollan, M.; Militino, A.F.; Perez-Gomez, B.; Lopez-Abente, G.; Ugarte, M.D. Spatio-temporal trends in gastric cancer mortality in Spain: 1975–2008. Cancer Epidemiol. 2013, 37, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Belpomme, D.; Irigaray, P.; Hardell, L.; Clapp, R.; Montagnier, L.; Epstein, S.; Sasco, A.J. The multitude and diversity of environmental carcinogens. Environ. Res. 2007, 105, 414–429. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Hu, N.; Han, X.Y.; Ding, T.; Giffen, C.; Goldstein, A.M.; Taylor, P.R. Risk factors for esophageal and gastric cancers in Shanxi Province, China: A case–control study. Cancer Epidemiol. 2011, 35, 91–99. [Google Scholar] [CrossRef]
- Mayne, S.T.; Risch, H.A.; Dubrow, R.; Chow, W.-H.; Gammon, M.D.; Vaughan, T.L.; Farrow, D.C.; Schoenberg, J.B.; Stanford, J.L.; Ahsan, H.; et al. Nutrient intake and risk of subtypes of esophageal and gastric cancer. Cancer Epidemiol. Biomark. Prevent. 2001, 10, 1055–1062. [Google Scholar]
- Carpenter, D.O. Polychlorinated biphenyls (PCBS): Routes of exposure and effects on human health. Rev. Environ. Health 2006, 21, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Fantini, F.; Porta, D.; Fano, V.; de Felip, E.; Senofonte, O.; Abballe, A.; D’Ilio, S.; Ingelido, A.M.; Mataloni, F.; Narduzzi, S.; et al. Epidemiologic studies on the health status of the population living in the Sacco River valley. Epidemiol. Prevenz. 2012, 36, 44–52. [Google Scholar]
- Hendryx, M.; Conley, J.; Fedorko, E.; Luo, J.; Armistead, M. Permitted water pollution discharges and population cancer and non-cancer mortality: Toxicity weights and upstream discharge effects in U.S. rural-urban areas. Int. J. Health Geogr. 2012, 11, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Seker, S.; Arakawa, K.; Sekiguchi, M.; Ono, Y. Biomonitoring of polycyclic aromatic hydrocarbons on hepatocellular carcinoma cell line. Water Sci. Technol. 2005, 52, 219–224. [Google Scholar] [PubMed]
- Wang, M.; Xu, Y.; Pan, S.; Zhang, J.; Zhong, A.; Song, H.; Ling, W. Long-term heavy metal pollution and mortality in a Chinese population: An ecologic study. Biol. Trace Elem. Res. 2011, 142, 362–379. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Guo, Q.G.; Zhou, M.G.; Dou, Y.S.; Yu, T.; Liu, Y.N.; Wang, X.F.; Chen, Y.J.; Zhang, Y.W. Association between mortality rate of hepatic carcinoma and the distance from Suihe River in Lingbi County, Anhui Province. Chin. J. Prevent. Med. 2013, 47, 529–533. (In Chinese) [Google Scholar]
- Tian, D.; Zheng, W.; Wei, X.; Sun, X.; Liu, L.; Chen, X.; Zhang, H.; Zhou, Y.; Chen, H.; Wang, X.; et al. Dissolved microcystins in surface and ground waters in regions with high cancer incidence in the Huai River Basin of China. Chemosphere 2013, 91, 1064–1071. [Google Scholar] [CrossRef] [PubMed]
- Alberto, W.D.; del Pilar, D.A.M.; Valeria, A.M.; Fabiana, P.S.; Cecilia, H.A.; de los Ángeles, B.M. Pattern recognition techniques for the evaluation of spatial and temporal variations in water quality. A case study: Suquı́a River Basin (Córdoba-Argentina). Water Res. 2001, 35, 2881–2894. [Google Scholar] [CrossRef] [PubMed]
- Bengraı̈ne, K.; Marhaba, T.F. Using principal component analysis to monitor spatial and temporal changes in water quality. J. Hazard. Mater. 2003, 100, 179–195. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.P.; Malik, A.; Mohan, D.; Sinha, S. Multivariate statistical techniques for the evaluation of spatial and temporal variations in water quality of Gomti River (India)—A case study. Water Res. 2004, 38, 3980–3992. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.F.; Kuo, C.H.; Tsai, S.S.; Chen, C.C.; Wu, D.C.; Wu, T.N.; Yang, C.Y. Effect modification by drinking water hardness of the association between nitrate levels and gastric cancer: Evidence from an ecological study. J. Toxicol. Environ. Health. Pt. A 2012, 75, 684–693. [Google Scholar] [CrossRef]
- Wang, X.S.; Wu, D.L.; Zhang, X.F.; Jia, S.S.; Jin, F.; Pan, Z.Q.; Wu, M.H.; Qin, Y. A case-control study on factors for liver cancer in Ganyu County. Mod. Prevent. Med. 2009, 36, 823–824. (In Chinese) [Google Scholar]
- Zhitkovich, A. Chromium in drinking water: Sources, metabolism, and cancer risks. Chem. Res. Toxicol. 2011, 24, 1617–1629. [Google Scholar] [CrossRef] [PubMed]
- Barrett, J.H.; Parslow, R.C.; McKinney, P.A.; Law, G.R.; Forman, D. Nitrate in drinking water and the incidence of gastric, esophageal, and brain cancer in Yorkshire, England. Cancer Cause. Control 1998, 9, 153–159. [Google Scholar] [CrossRef]
- Nishiwaki-Matsushima, R.; Nishiwaki, S.; Ohta, T.; Yoshizawa, S.; Suganuma, M.; Harada, K.; Watanabe, M.F.; Fujiki, H. Structure-function relationships of microcystins, liver tumor promoters, in interaction with protein phosphatase. Jpn. J. Cancer Res. 1991, 82, 993–996. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Jing, J.X.; Sun, G.X. Study of environmental pollution and damage of cytogenetic materials in urban residents. Chin. J. Epidemiol. 1997, 18, 83–85. (In Chinese) [Google Scholar]
- Gallo, A.; Cha, C. Updates on esophageal and gastric cancers. World J. Gastroenterol. 2006, 12, 3237–3242. [Google Scholar] [PubMed]
- Guzman, R.E.; Solter, P.F. Characterization of sublethal microcystin-LR exposure in mice. Vet. Pathol. 2002, 39, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Igbinosa, E.O.; Odjadjare, E.E.; Chigor, V.N.; Igbinosa, I.H.; Emoghene, A.O.; Ekhaise, F.O.; Igiehon, N.O.; Idemudia, O.G. Toxicological profile of chlorophenols and their derivatives in the environment: The public health perspective. Sci. World J. 2013. [Google Scholar] [CrossRef]
- Xie, T.P.; Zhao, Y.F.; Chen, L.Q.; Zhu, Z.J.; Hu, Y.; Yuan, Y. Long-term exposure to sodium nitrite and risk of esophageal carcinoma: A cohort study for 30 years. Dis. Esophagus. 2011, 24, 30–32. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Li, K. Association between esophageal cancer and drought in china by using geographic information system. Environ. Int. 2007, 33, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Antunes, J.L.F.; Biazevic, M.G.H.; de Araujo, M.E.; Tomita, N.E.; Chinellato, L.E.M.; Narvai, P.C. Trends and spatial distribution of oral cancer mortality in São Paulo, Brazil, 1980–1998. Oral Oncol. 2001, 37, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Selinus, O.; Alloway, B.J. Essentials of Medical Geology: Impacts of the Natural Environment on Public Health; Elsevier Academic Press: Burlington, VT, USA, 2005. [Google Scholar]
- Ministry of Health of the People’s Republic of China. Survey of China’s Deaths from Cancers; The People’s Health Publishing House: Beijing, China, 1979.
- Ministry of Environmental Protection of the People’s Republic of China. Environmental Quality Standards for Surface Water; China Environmental Science Press: Beijing, China, 2002.
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ren, H.; Wan, X.; Yang, F.; Shi, X.; Xu, J.; Zhuang, D.; Yang, G. Association between Changing Mortality of Digestive Tract Cancers and Water Pollution: A Case Study in the Huai River Basin, China. Int. J. Environ. Res. Public Health 2015, 12, 214-226. https://doi.org/10.3390/ijerph120100214
Ren H, Wan X, Yang F, Shi X, Xu J, Zhuang D, Yang G. Association between Changing Mortality of Digestive Tract Cancers and Water Pollution: A Case Study in the Huai River Basin, China. International Journal of Environmental Research and Public Health. 2015; 12(1):214-226. https://doi.org/10.3390/ijerph120100214
Chicago/Turabian StyleRen, Hongyan, Xia Wan, Fei Yang, Xiaoming Shi, Jianwei Xu, Dafang Zhuang, and Gonghuan Yang. 2015. "Association between Changing Mortality of Digestive Tract Cancers and Water Pollution: A Case Study in the Huai River Basin, China" International Journal of Environmental Research and Public Health 12, no. 1: 214-226. https://doi.org/10.3390/ijerph120100214
APA StyleRen, H., Wan, X., Yang, F., Shi, X., Xu, J., Zhuang, D., & Yang, G. (2015). Association between Changing Mortality of Digestive Tract Cancers and Water Pollution: A Case Study in the Huai River Basin, China. International Journal of Environmental Research and Public Health, 12(1), 214-226. https://doi.org/10.3390/ijerph120100214






