Disparities in Rates of Inpatient Mortality and Adverse Events: Race/Ethnicity and Language as Independent Contributors
Abstract
:1. Introduction
2. Methods
2.1. Data Source
2.2. Study Population
2.3. Demographic Characteristics
2.4. Data Analyses
3. Results
3.1. Demographic Characteristics
| Characteristic | Principal Language Spoken | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| English | Spanish | Languages of API | |||||||||
| Total | Chinese | Hindi | Japanese | Korean | Other | Tagalog | Thai | Vietnamese | |||
| Total discharges (N = 3,757,218) | 3,211,457 | 474,267 | 71,495 | 24,643 | 2592 | 2608 | 11,980 | 773 | 12,134 | 674 | 16,089 |
| Average age (years) | 46.0 | 35.4 | 58.4 | 59.0 | 48.5 | 57.6 | 57.9 | 44.8 | 68.0 | 53.9 | 53.1 |
| Gender (%) | |||||||||||
| Female | 58.0 | 63.9 | 61.6 | 60.2 | 64.2 | 70.3 | 64.2 | 67.4 | 61.7 | 68.4 | 59.4 |
| Male | 42.0 | 36.1 | 38.4 | 39.8 | 35.8 | 29.7 | 35.8 | 32.6 | 38.3 | 31.6 | 40.6 |
| Expected primary payment source (%) | |||||||||||
| Private insurance | 37.3 | 14.2 | 24.0 | 23.1 | 43.4 | 43.2 | 22.6 | 39.0 | 20.3 | 30.5 | 22.0 |
| Medicare | 33.4 | 18.0 | 46.1 | 49.0 | 25.8 | 47.1 | 47.1 | 21.2 | 53.3 | 27.9 | 40.5 |
| Medicaid | 21.3 | 57.8 | 21.6 | 17.7 | 24.1 | 5.3 | 19.0 | 32.3 | 21.2 | 29.4 | 31.1 |
| Self-pay or no charge | 3.3 | 4.7 | 5.0 | 8.1 | 3.5 | 3.2 | 7.8 | 3.5 | 1.8 | 5.6 | 1.3 |
| Median household income of patient’s ZIP Code (%) | |||||||||||
| First quartile (lowest income) | 16.0 | 31.6 | 15.3 | 11.0 | 6.9 | 11.5 | 43.0 | 9.4 | 12.4 | 23.7 | 5.4 |
| Second quartile | 18.9 | 24.7 | 14.6 | 20.5 | 14.6 | 12.1 | 8.0 | 14.6 | 9.3 | 16.3 | 14.7 |
| Third quartile | 29.1 | 29.1 | 29.9 | 28.5 | 17.5 | 28.0 | 21.9 | 24.5 | 27.1 | 27.8 | 42.6 |
| Fourth quartile (highest income) | 36.0 | 14.6 | 40.3 | 40.0 | 60.9 | 48.4 | 27.0 | 51.5 | 51.3 | 32.3 | 37.3 |
| Location of patient’s residence (%) | |||||||||||
| Large central metropolitan | 62.1 | 69.8 | 89.8 | 93.5 | 74.3 | 86.4 | 95.4 | 73.1 | 75.2 | 85.4 | 95.1 |
| Large fringe metropolitan | 13.3 | 8.3 | 6.6 | 4.9 | 8.9 | 8.0 | 3.0 | 11.3 | 17.8 | 8.7 | 2.8 |
| Medium metropolitan | 17.7 | 17.2 | 3.0 | 1.3 | 11.0 | 4.1 | 1.4 | 15.1 | 6.3 | 4.8 | 2.0 |
| Small metropolitan | 4.1 | 4.0 | 0.5 | 0.2 | 5.5 | 1.2 | 0.2 | DSU | 0.5 | DSU | 0.1 |
| Micropolitan | 2.0 | 0.5 | 0.1 | DSU | DSU | DSU | DSU | DSU | 0.1 | DSU | DSU |
| Not metropolitan or micropolitan | 0.8 | 0.3 | 0.0 | 0.06 | DSU | DSU | DSU | DSU | DSU | DSU | DSU |
| Race/ethnicity (%) | |||||||||||
| White | 57.0 | 2.7 | 2.0 | ||||||||
| Hispanic | 22.2 | 96.1 | 1.8 | ||||||||
| API | 7.3 | 0.1 | 93.2 | ||||||||
| Black | 10.2 | 0.1 | 0.2 | ||||||||
| Other | 3.2 | 1.0 | 2.9 | ||||||||
| Characteristic | Hispanic Patient, English Language | Hispanic Patient, Spanish Language | API Patient, English Language | API Patient, API Language |
|---|---|---|---|---|
| Total discharges (n) | 714,365 | 455,625 | 234,642 | 66,609 |
| Average age (years) | 30.8 | 35.5 | 39.2 | 58.5 |
| Gender (%) | ||||
| Female | 60.4 | 64.0 | 61.1 | 61.5 |
| Male | 39.6 | 36.0 | 38.9 | 38.5 |
| Expected primary payment source (%) | ||||
| Private insurance | 33.9 | 14.0 | 55.5 | 23.9 |
| Medicare | 16.0 | 18.0 | 22.7 | 46.6 |
| Medicaid | 40.6 | 57.9 | 16.2 | 21.3 |
| Self-pay/No charge | 4.1 | 4.8 | 2.5 | 5.0 |
| Median income of patient’s ZIP Code (%) | ||||
| First quartile (lowest income) | 22.7 | 31.7 | 10.0 | 15.5 |
| Second quartile | 24.2 | 24.8 | 12.2 | 14.5 |
| Third quartile | 31.8 | 29.1 | 26.8 | 30.0 |
| Fourth quartile (highest income) | 21.4 | 14.4 | 51.0 | 40.0 |
| Location of patient’s residence (%) | ||||
| Large central metropolitan | 64.2 | 70.2 | 76.5 | 90.4 |
| Large fringe metropolitan | 12.4 | 8.3 | 11.4 | 6.5 |
| Medium metropolitan | 18.9 | 16.8 | 10.5 | 2.6 |
| Small metropolitan | 3.8 | 4.0 | 1.2 | 0.4 |
| Micropolitan | 0.4 | 0.4 | 0.3 | 0.0 |
| Not metropolitan or micropolitan | 0.2 | 0.3 | 0.1 | 0.0 |
| Characteristic | Acute Myocardial Infarction, Inpatient Mortality, Mean (SD) | Congestive Heart Failure, Inpatient Mortality, Mean (SD) | Stroke, Inpatient Mortality, Mean (SD) | Gastro-Intestinal Hemorrhage, Inpatient Mortality, Mean (SD) | Pneumonia, Inpatient Mortality, Mean (SD) | Obstetric Trauma, Instrument-Assisted Deliveries, Mean (SD) | Obstetric Trauma, Unassisted Deliveries, Mean (SD) |
|---|---|---|---|---|---|---|---|
| White | |||||||
| English speakers (ref a) | 59.07 (1.26) | 28.03 (0.66) | 86.26 (1.33) | 21.58 (0.81) | 34.57 (0.68) | 119.62 (3.55) | 22.40 (0.51) |
| Hispanic | |||||||
| English speakers (ref b) | 56.91 (3.19) | 22.55 (1.69) c | 80.81 (2.84) | 18.09 (1.81) | 34.37 (1.72) | 92.65 (3.91) c | 14.98 (0.42) c |
| Spanish speakers | 60.42 (3.66) | 18.55 (1.70) c | 74.69 (3.20) c | 17.42 (2.13) | 28.19 (1.80) b,c | 98.66 (4.27) c | 18.59 (0.55) c,d |
| Asian and Pacific Islander | |||||||
| English speakers (ref b) | 62.38 (3.87) | 21.98 (2.23) c | 76.85 (3.45) a | 19.63 (2.58) | 30.82 (2.21) | 167.72 (7.49) c | 34.44 (1.29) c |
| API speakers | 56.61 (5.60) | 19.06 (2.78) c | 77.47 (4.74) | 23.04 (3.36) | 33.36 (2.59) | 165.02 (14.99) c | 50.01 (8.67) c |
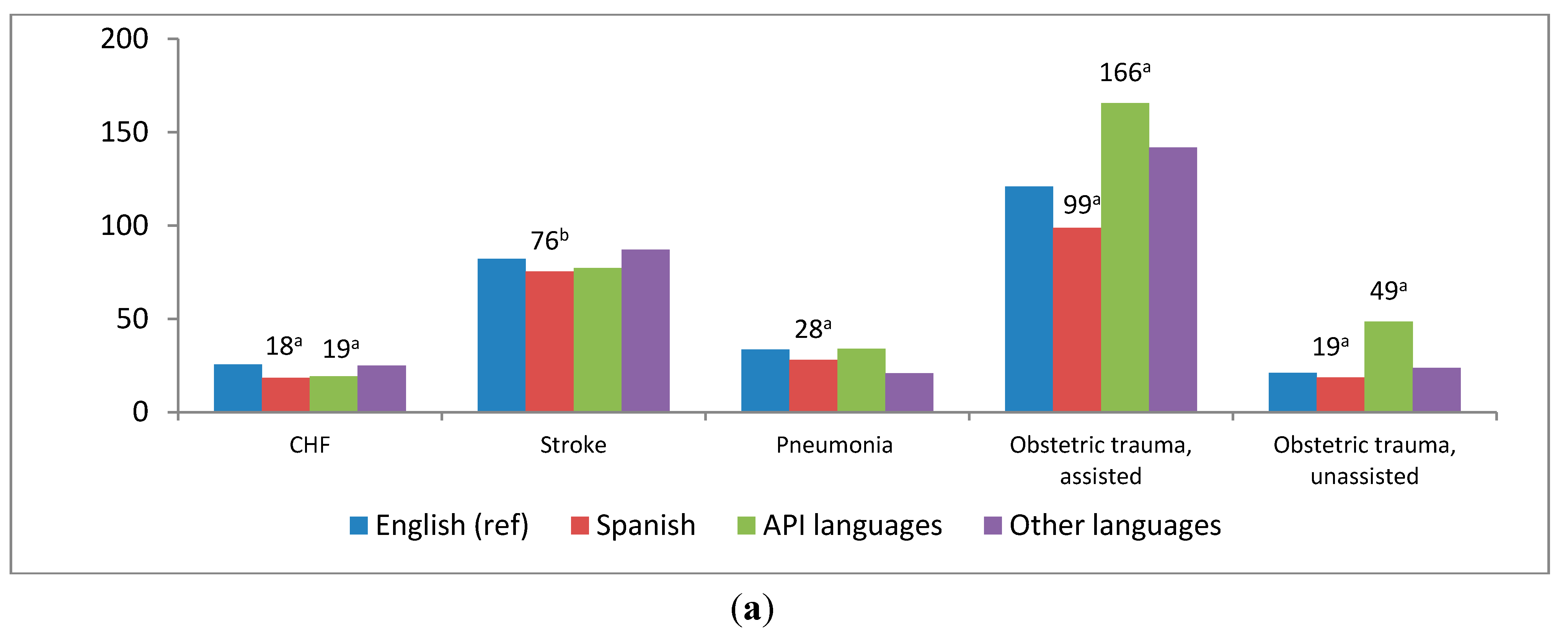
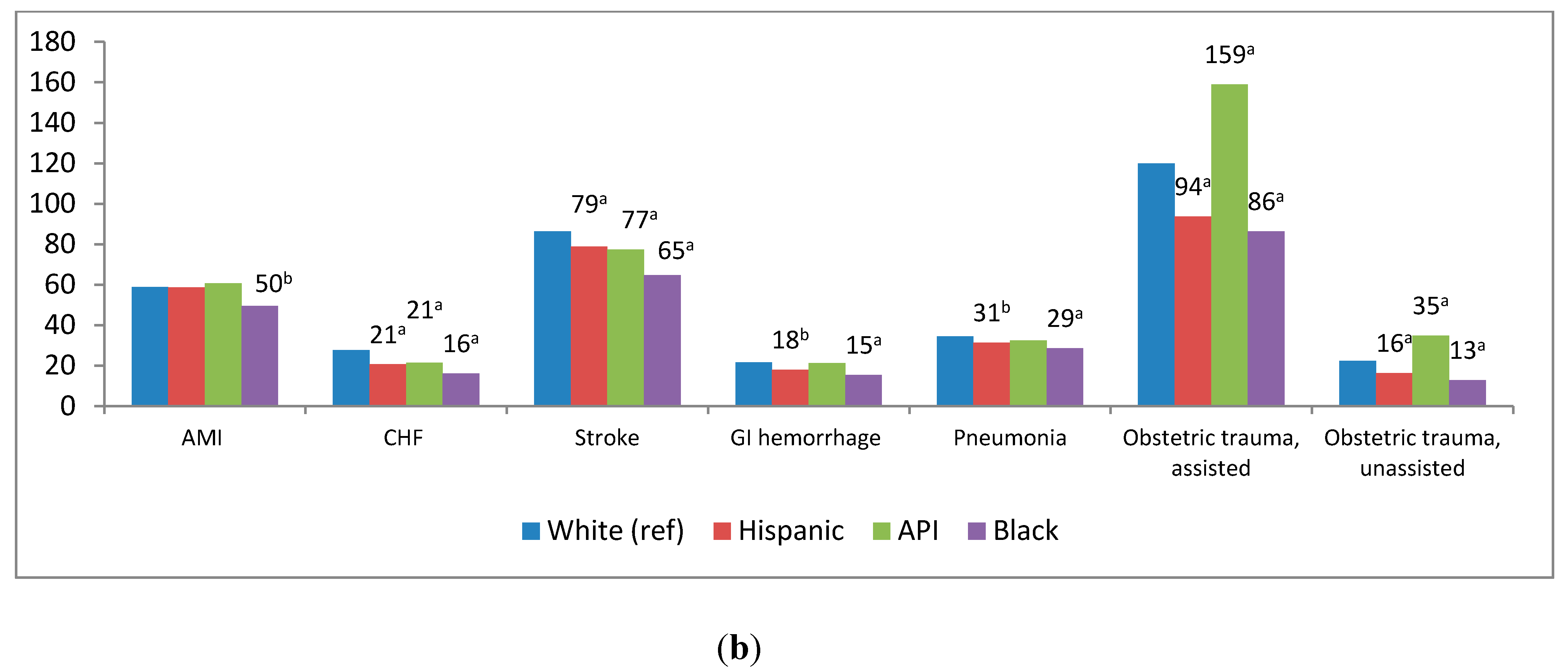
3.2. Risk-Adjusted Hospital Outcomes by Language and by Race/Ethnicity
3.3. Risk-Adjusted Hospital Outcomes within Race-Ethnicity Group by Language

4. Discussion
4.1. Obstetric Trauma
4.2. Collection and Reporting of Language Data
4.3. Interpretation Services in the Health Care Setting
4.4. Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Flores, G.; Tomany-Korman, S.C. The language spoken at home and disparities in medical and dental health, access to care, and use of services in U.S. children. Pediatrics 2008, 121, 1703–1714. [Google Scholar] [CrossRef]
- Cheng, E.M.; Chen, A.; Cunningham, W. Primary language and receipt of recommended health care among Hispanics in the United States. J. Gen. Intern. Med. 2007, 22, 283–238. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, M.; Kanitsaki, O. Cultural racism, language prejudice and discrimination in hospital contexts: An Australian study. Divers. Health Soc. Care 2008, 5, 19–30. [Google Scholar]
- Burchard, E.G.; Ziv, E.; Coyle, N.; Gomez, S.L.; Tang, H.; Karter, A.J.; Mountain, J.L.; Perez-Stable, E.J.; Sheppard, D.; Risch, N. The importance of race and ethnic background in biomedical research and clinical practice. N. Engl. J. Med. 2003, 348, 1170–1175. [Google Scholar] [CrossRef] [PubMed]
- Carrasquillo, O.; Orav, E.J.; Brennan, T.A.; Burstin, H.R. Impact of language barriers on patient satisfaction in an emergency department. J. Gen. Intern. Med. 1999, 14, 82–87. [Google Scholar]
- Weech-Maldonado, R.; Morales, L.S.; Elliott, M.; Spritzer, K.; Marshall, G.; Hayes, R.D. Race/ethnicity, language, and patients’ assessments of care in Medicaid managed care. Health Serv. Res. 2003, 38, 789–808. [Google Scholar] [CrossRef] [PubMed]
- Divi, C.; Koss, R.G.; Schmaltz, S.P.; Loeb, J.M. Language proficiency and adverse events in U.S. hospitals: A pilot study. Int. J. Qual. Health Care 2007, 9, 60–67. [Google Scholar] [CrossRef]
- John-Baptiste, A.; Naglie, G.; Tomlinson, G.; Alibhai, S.M.H.; Etchells, E.; Cheung, A.; Kapral, M.; Gold, W.L.; Abrams, H.; Bacchus, M.; Krahn, M. The effect of English language proficiency on length of stay and in-hospital mortality. J. Gen. Intern. Med. 2004, 19, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Grubbs, V.; Bibins-Domingo, K.; Fernandez, A.; Chattopadhyay, A.; Bindman, A.B. Acute myocardial infarction length of stay and hospital mortality are not associated with language preference. J. Gen. Intern. Med. 2008, 23, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Karliner, L.S.; Kim, S.E.; Meltzer, D.O.; Auerbach, A.D. Influence of language barriers on outcomes of hospital care for general medicine inpatients. J. Hosp. Med. 2010, 5, 278–282. [Google Scholar] [CrossRef]
- Renzaho, A. Ischaemic heart disease and Australian immigrants: The influence of birthplace and language skills on treatment and use of health services. HIMJ 2007, 36, 26–36. [Google Scholar] [PubMed]
- Healthcare Cost and Utilization Project. In Introduction to the HCUP State Inpatient Databases (SID); Agency for Healthcare Research and Quality: Rockville, MD, USA, 2012. Available online: https://www.hcup-us.ahrq.gov/db/state/siddist/Introduction_to_SID.pdf (assessed on 2 June 2014).
- Inpatient Data Reporting Manual, 7th ed.Office of Statewide Health Planning and Development, Healthcare Information Division: Sacramento, CA, USA, 2013. Available online: http://www.oshpd.ca.gov/HID/MIRCal/IPManual.html (assessed on 2 June 2014).
- Quality Indicators (QIs); Agency for Healthcare Research and Quality (AHRQ): Rockville, MD, USA, 2013. Available online: http://www.qualityindicators.ahrq.gov/ (assessed on 2 June 2014).
- Inpatient Quality Indicators: Software Documentation, Version 4.1 SAS; AHRQ: Rockville, MD, USA, 2009. Available online: http://www.qualityindicators.ahrq.gov/Downloads/Software/SAS/V41A/pqi_sas_documentation_v41.pdf (assessed on 4 June 2014).
- Patient Safety Indicators: Software Documentation, Version 4.1 SAS; AHRQ: Rockville, MD, USA, 2010. Available online: http://www.qualityindicators.ahrq.gov/downloads/software/sas/v42/psi_sas_documentation_v42.pdf (assessed on 4 June 2014).
- Ingram, D.D.; Franco, S.F. NCHS Urban-Rural Classification Scheme for Counties; National Center for Health Statistics; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2012. Available online: http://wonder.cdc.gov/wonder/help/CMF/sr02_154.pdf (assessed on 4 June 2014).
- Jha, A.K.; Shlipak, M.G.; Hosmer, W.; Frances, C.D.; Browner, W.S. Racial differences in mortality among men hospitalized in the Veterans Affairs health care system. JAMA 2001, 285, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Volpp, K.G.; Stone, R.; Lave, J.R.; Jha, A.K.; Pauly, M.; Klusaritz, H.; Chen, H.; Cen, L.; Brucker, N.; Polsky, D. Is thirty-day hospital mortality really lower for black veterans compared with white veterans? Health Serv. Res. 2007, 42, 1613–1631. [Google Scholar] [CrossRef] [PubMed]
- Polsky, D.; Lave, J.; Klusaritz, H.; Jha, A.; Pauly, M.V.; Cen, L.; Xie, H.; Stone, R.; Chen, Z.; Volpp, K. Is lower 30-day mortality posthospital admission among blacks unique to the Veterans Affairs health care system? Med. Care 2007, 45, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Markides, K.S.; Eschbach, K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J. Gerontol. Ser. B-Psychol .Sci. 2005, 60, 68–75. [Google Scholar] [CrossRef]
- Blondon, M.; Harrington, L.B.; Righini, M.; Boehlen, F.; Bounameaux, H; Smith, N.L. Racial and ethnic differences in the risk of postpartum venous thromboembolish: A population-based, case-control study. J. Thromb. Haemost 2014. [Google Scholar] [CrossRef]
- Wheeler, J.; Davis, D.; Fry, M.; Brodie, P.; Homer, C.S. Is Asian ethnicity an independent risk factor for severe perineal trauma in childbirth? A systematic review of the literature. Women Birth 2012, 25, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.; Chang, A.; Cheng, Y.; Miyamura, J. Maternal quality and safety outcomes for Asians and Pacific Islanders in Hawai’i: An observational study from five years of statewide data. BMC Pregnancy Childbirth 2014. [CrossRef]
- Green, J.R.; Soohoo, S.L. Factors associated with rectal injury and spontaneous deliveries. Obstet. Gynecol. 1989, 63, 732–738. [Google Scholar]
- Dahlen, H.G.; Ryan, M.; Homer, C. An Australian prospective cohort study of risk factors for severe perineal trauma during childbirth. Midwifery 2007, 23, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Denham, C.R. The partnership with patients: A call to action for leaders. J. Patient Saf. 2011, 7, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.B.; Kominski, R.A. Language Use in the United States: 2007; U.S. Census Bureau: Washington, D.C., USA, 2010.
- Frisbie, W.P.; Cho, Y.; Hummer, R.A. Immigration and the health of Asian and Pacific Islander adults in the United States. Amer. J. Epidemiol. 2001, 153, 372–380. [Google Scholar] [CrossRef]
- Chen, J.Y.; Diamant, A.L.; Kagawa-Singer, M.; Pourat, N.; Wold, C. Disaggregating data on Asian and Pacific Islander women to assess cancer screening. Amer. J. Prev. Med. 2004, 27, 139–145. [Google Scholar] [CrossRef]
- Yu, S.M.; Huang, Z.J.; Singh, G.K. Health status and health services utilization among U.S. Chinese, Asian Indian, Filipino, and other Asian/Pacific Islander children. Pediatrics 2004, 113, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Barnes, P.M.; Adams, P.F.; Powell-Griner, E. Health Characteristics of the Asian Adult Population: United States, 2004–2006; National Center for Health Statistics: Hyattsville, MD, USA, 2008. [Google Scholar]
- Moy, E.; Mau, M.K.; Raetzman, S.; Barrett, M.; Miyamura, J.B.; Chaves, K.H.; Andrews, R. Ethnic differences in potentially preventable hospitalizations among Asian Americans, native Hawaiians, and other Pacific Islanders: Implications for reducing health care disparities. Ethn. Dis. 2013, 23, 6–11. [Google Scholar] [PubMed]
- Green, A.R.; Ngo-Metzger, Q.; Legedza, A.T.; Massagli, M.P.; Phillips, R.S.; Iezzoni, L.I. Interpreter services, language concordance, and health care quality. Experiences of Asian Americans with limited English proficiency. J. Gen. Intern. Med. 2005, 20, 1050–1056. [Google Scholar] [CrossRef] [PubMed]
- Ngo-Metzger, Q.; Sorkin, D.H.; Phillips, R.S.; Greenfield, S.; Massagli, M.P.; Clarridge, B.; Kaplan, S.H. Providing high-quality care for limited English proficient patients: The importance of language concordance and interpreter use. J. Gen. Intern. Med. 2007, 22, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Office of Minority Health. U.S. National Standards on Culturally and Linguistically Appropriate Services (CLAS); U.S. Department of Health and Human Services: Rockville, MD, USA, 2007. Available online: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15 (assessed on 7 July 2014).
- Office of Minority Health. U.S. Data Collection Standards for Race, Ethnicity, Sex, Primary Language, and Disability Status; U.S. Department of Health and Human Services: Rockville, MD, USA, 2011. Available online: http://minorityhealth.hhs.gov/templates/content.aspx?ID=9227&lvl=2&lvlID=208 (assessed on 7 July 2014).
- Centers for Medicare & Medicaid Services. Electronic Health Record (EHR) Incentive Program. Eligible Hospital and Critical Access Hospital Meaningful Use Core Measures: Measure 6 of 14; EHR Incentive Program: Washington, D.C., USA, 2010. Available online: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/6_Record_Demographics.pdf (assessed on 16 June 2014).
- National Uniform Billing Committee. Official UB-04 Data Specifications Manual 2012, Version 6.00; American Hospital Association: Chicago, IL, USA, 2011. [Google Scholar]
- Schenker, Y.; Perez-Stable, E.J.; Nickleach, D.; Karliner, L.S. Patterns of interpreter use for hospitalized patients with limited English proficiency. J. Gen. Intern. Med. 2011, 26, 712–717. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hines, A.L.; Andrews, R.M.; Moy, E.; Barrett, M.L.; Coffey, R.M. Disparities in Rates of Inpatient Mortality and Adverse Events: Race/Ethnicity and Language as Independent Contributors. Int. J. Environ. Res. Public Health 2014, 11, 13017-13034. https://doi.org/10.3390/ijerph111213017
Hines AL, Andrews RM, Moy E, Barrett ML, Coffey RM. Disparities in Rates of Inpatient Mortality and Adverse Events: Race/Ethnicity and Language as Independent Contributors. International Journal of Environmental Research and Public Health. 2014; 11(12):13017-13034. https://doi.org/10.3390/ijerph111213017
Chicago/Turabian StyleHines, Anika L., Roxanne M. Andrews, Ernest Moy, Marguerite L. Barrett, and Rosanna M. Coffey. 2014. "Disparities in Rates of Inpatient Mortality and Adverse Events: Race/Ethnicity and Language as Independent Contributors" International Journal of Environmental Research and Public Health 11, no. 12: 13017-13034. https://doi.org/10.3390/ijerph111213017
APA StyleHines, A. L., Andrews, R. M., Moy, E., Barrett, M. L., & Coffey, R. M. (2014). Disparities in Rates of Inpatient Mortality and Adverse Events: Race/Ethnicity and Language as Independent Contributors. International Journal of Environmental Research and Public Health, 11(12), 13017-13034. https://doi.org/10.3390/ijerph111213017




