Predictors of Healthcare Service Utilization for Mental Health Reasons
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Setting
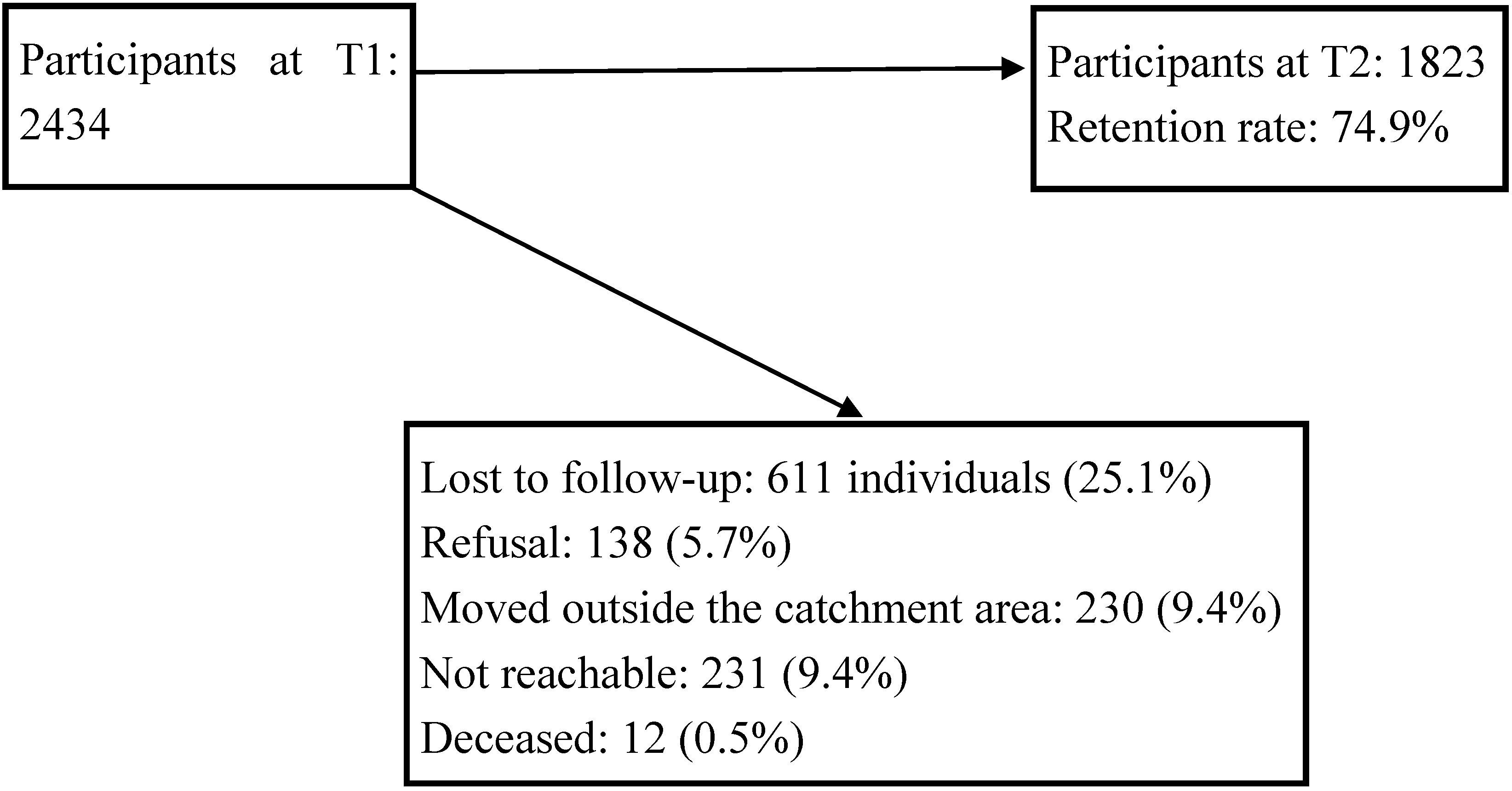
2.2. Selection Criteria and Survey Sample
2.3. Variables and Measuring Instruments
| Factors | No. | Name | Description |
|---|---|---|---|
| Predisposing factors | 1 | CCHS 1.2 [71] | Canadian Community Health Survey (CCHS): survey questionnaire for socio-demographic characteristics |
| 2 | Satisfaction with Life Domains Scale (SLDS) [72] | 20 items organized in 5 domains: daily living and social relationships, living environment, autonomy, intimate relationships, and leisure | |
| Enabling factors | 3 | Sense of Community Scale (SCS) [73] | 8 items |
| 4 | Community Participation Scale (CPS) [74] | 6 items Measures association between crime victimization, social organization, and participation in neighborhood organization | |
| 5 | Resident Disempowerment Scale (RDS) [75] | 3 items | |
| 6 | Sense of Collective Efficacy (SCE) [76] | Evaluates the effect of social and institutional mechanisms on people living in the neighborhood | |
| 7 | Neighborhood Disorder Scale (NDS) [75] | 9 items | |
| 8 | Physical Conditions of the Neighborhood (PCN) [73] | 7 items | |
| 9 | Facility in Neighborhood (FN) [77] | 13 items; measures 3 domains: availability, utilization and quality | |
| Enabling factors | 10 | Social Provisions Scale (SPS) [78] | Measures six items: emotional support, social integration, reassurance about his value, material help, counselling and information, need to feel useful |
| Needs factors | 11 | Composite International Diagnostic Interview (CIDI) and CIDI-SF [71,79] | Screening of mental disorders; was used in the World Mental Health 2000 (WMH 2000); included the most frequent mental disorders (mood disorders: depression, mania; anxiety disorders: social phobia, agoraphobia, and panic disorder, post-traumatic stress disorder (PTSD)). Screening of substance disorders (alcohol and drugs were based on the CIDI-Short Form (SF) |
| 12 | Modified Observed Aggression Scale (MOAS) for aggressive behaviors [80] | Assess 4 categories of aggressive behavior: verbal aggression, aggression to propriety, self-inflicted aggression, physical aggression | |
| 17 | K-10 psychological distress scale (K-10 PDS) [81] | 10 five-point Likert items; was used in the World Mental Health survey 2000 (WMH2000) | |
| 18 | Barratt Impulsivity Scale (BIS) [82] | 30 four-point scale items organized in three categories: motor impulsivity, cognitive impulsivity, impulsivity due to lack of planning |
2.4. Analyses
3. Results and Discussion
3.1. Descriptive Analyses
3.2. Comparison Analyses according to the Presence of Mental Disorders and Gender Difference
| Factors | Variables | Categories | Participant Characteristics at T1 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Sample | Mental Disorders | Gender | Healthcare Service Utilization at T2 | Healthcare Services Users by Gender (n = 243) | |||||||
| n = 1823 | No. | Yes | Female | Male | No | Yes | Female | Male | |||
| % | % | % | % | % | % | % | % | % | |||
| Predisposing factors | Gender | Female | 62.6 | 61.4 | 69.1 * | 62.2 | 65.4 | ||||
| Male | 37.4 | 38.6 | 30.9 | 37.8 | 34.6 | ||||||
| Education | Secondary school or less | 18.9 | 17.6 | 25.8 * | 19.4 | 18.2 | 18.0 | 24.7 * | 25.8 | 22.6 | |
| Over secondary school | 81.1 | 82.4 | 74.2 | 80.6 | 81.8 | 82.0 | 75.3 | 74.2 | 77.4 | ||
| Satisfaction with life | Satisfied or Very satisfied | 82.3 | 87.2 | 56.7 ** | 81.7 | 83.4 | 85.7 | 60.5 ** | 61.6 | 58.3 | |
| Neither satisfied nor dissatisfied | 11.6 | 9.4 | 23.4 | 12.2 | 10.7 | 10.0 | 22.2 | 19.5 | 27.4 | ||
| Very dissatisfied or dissatisfied | 6.0 | 3.4 | 19.9 | 6.1 | 5.9 | 4.3 | 17.3 | 18.9 | 14.3 | ||
| Self-perception of physical health | Excellent or very good | 45.6 | 49.5 | 25.1 * | 45.4 | 46.1 | 48.3 | 28.4 ** | 27.0 | 30.9 | |
| Good | 36.7 | 36.7 | 36.8 | 36.7 | 36.7 | 36.2 | 39.9 | 40.3 | 39.3 | ||
| Poor or fair | 17.7 | 13.8 | 38.1 | 18.0 | 17.2 | 15.5 | 31.7 | 32.7 | 29.8 | ||
| Self-perception of mental health | Excellent or very good | 58.6 | 65.5 | 22.3 ** | 55.9 | 63.1 * | 63.4 | 27.2 ** | 26.4 | 28.6 | |
| Good | 30.6 | 28.3 | 42.3 | 32.1 | 27.9 | 29.0 | 40.7 | 39.6 | 42.9 | ||
| Poor or fair | 10.9 | 6.2 | 35.4 | 12.0 | 9.0 | 7.6 | 32.1 | 34.0 | 28.6 | ||
| Importance attributed to spirituality | 57.8 | 57.1 | 61.2 | 60.9 | 52.6 * | 57.3 | 60.9 | 64.2 | 54.8 | ||
| Problems with the law in past 12 months | 1.1 | 0.6 | 3.8 ** | .4 | 2.2 ** | 1.0 | 1.6 | 0.0 | 4.8 * | ||
| Lifelong history of problems with the law | 5.4 | 3.8 | 13.7 ** | 2.8 | 9.7 ** | 4.3 | 12.3 ** | 6.9 | 22.6 * | ||
| Enabling factors | Source of income | From job | 58.9 | 61.1 | 47.1 ** | 58.5 | 59.5 | 60.7 | 46.9 ** | 54.0 | 51.2 |
| Others | 41.1 | 38.9 | 52.9 | 41.5 | 40.5 | 39.3 | 53.1 | 45.9 | 48.8 | ||
| Needs factors | Mental disordersin previous 12 months | Major depression | 8.6 | 0.0 | 54.0 | 9.6 | 6.9 * | 5.4 | 29.2 ** | 28.9 | 29.8 |
| Mania | 1.5 | 0.0 | 9.6 | 1.4 | 1.8 | 1.0 | 4.9 ** | 2.5 | 9.5 * | ||
| Panic Disorder | 1.8 | 0.0 | 11.3 | 2.4 | 0.9 * | 1.3 | 4.9 ** | 5.7 | 3.6 | ||
| Social Phobia | 3.3 | 0.0 | 21.0 | 4.4 | 1.6 * | 2.3 | 10.3 ** | 12.6 | 5.9 | ||
| Agoraphobia | 1.4 | 0.0 | 8.9 | 1.8 | 0.7 * | 0.8 | 5.8 ** | 6.3 | 4.8 | ||
| Alcohol Dependence | 2.7 | 0.0 | 17.2 | 1.9 | 4.1 * | 1.4 | 11.5 ** | 8.2 | 17.9 * | ||
| Drug Dependence | 2.2 | 0.0 | 13.7 | 1.5 | 3.4 * | 1.1 | 9.1 ** | 6.3 | 14.3 * | ||
| PTSD | 0.8 | 0.0 | 4.8 | 1.2 | 0 * | 0.4 | 2.9 ** | 4.4 | 0.0 * | ||
| Mental disorders in past 12 months (Yes/No) | 16.0 | 17.6 | 13.2 * | 10.9 | 49.0 ** | 30.8 | 20.2 | ||||
| Emotional problems in past 12 months | 33.2 | 28.9 | 55.7 ** | 36.9 | 27.0 ** | 31.4 | 44.9 ** | 50.3 | 34.5 * | ||
| Victim of violence in past 12 months | 5.1 | 4.0 | 11.0 ** | 5.0 | 5.3 | 4.3 | 10.3 ** | 8.2 | 14.3 | ||
| Aggressive behaviors in past 12 months | 13.4 | 11.2 | 25.1 ** | 13.3 | 13.7 | 13.0 | 16.5 | 15.7 | 17.9 | ||
| Factors | Participant Characteristics at T1 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Sample | Mental Disorders | Gender | Healthcare Service Utilization at T2 | Healthcare Services Users by Gender n = 243 | ||||||||||||||
| n = 1823 | No | Yes | Female | Male | No | Yes | Female | Male | ||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Predisposing factors | ||||||||||||||||||
| Age | 42.6 | 13.2 | 42.9 | 13.3 | 41.0 | 12.5 * | 42.7 | 13.1 | 42.3 | 13.3 | 42.7 | 13.2 | 41.5 | 12.9 | 42.5 | 3.0 | 39.6 | 12.5 |
| Number of children in household | 1.7 | 0.6 | 1.7 | 0.6 | 1.7 | 0.5 | 1.7 | 0.7 | 1.7 | 0.6 | 1.7 | 0.6 | 1.7 | 0.5 | 1.7 | 0.5 | 1.6 | 0.5 |
| Enabling factors | ||||||||||||||||||
| Household income | 60,803.5 | 49,127.4 | 63,746.2 | 50,791.2 | 45,311.4 | 35,462.8 ** | 59,848.4 | 48,790.5 | 62,405.1 | 49,682.2 | 62,832.3 | 50,392.2 | 47,612.0 | 37,424.9 ** | 48,708 | 39,282 | 45,538 | 33,759 |
| Personal income | 33879.1 | 31075.0 | 35515.8 | 32681.8 | 25262.8 | 18,425.6 ** | 30,996.0 | 23,895.7 | 38,713.9 | 39,898.7 ** | 34,974.5 | 32,182.1 | 26,756.7 | 21,305.6 ** | 26,027 | 20,441 | 28,137 | 22,915 |
| Quality of life | 109.4 | 15.9 | 111.9 | 14.3 | 96.5 | 17.4 ** | 109.8 | 15.6 | 108.9 | 16.3 | 111.2 | 14.7 | 97.8 | 17.9 ** | 98.6 | 17.9 | 96.3 | 18.0 |
| Physical Conditions of the Neighborhood score | 45.0 | 11.1 | 45.6 | 10.9 | 41.6 | 11.4 ** | 45.1 | 11.6 | 44.8 | 10.3 | 45.3 | 10.9 | 42.9 | 11.8 * | 44.0 | 12.0 | 40.8 * | 11.3 |
| Security score | 3.7 | 1.3 | 3.6 | 1.3 | 4.0 | 1.4 ** | 3.8 | 1.4 | 3.6 | 1.3 * | 3.7 | 1.3 | 3.9 | 1.4 * | 4.0 | 1.5 | 3.7 | 1.3 |
| Community involvement scale score | 9.1 | 1.1 | 9.1 | 1.1 | 9.2 | 1.0 | 9.1 | 1.1 | 9.2 | 1.0 * | 9.1 | 1.1 | 9.3 | 1.0 * | 9.2 | 1.1 | 9.4 | 1.0 |
| Sense of collective efficacy score | 26.4 | 6.0 | 26.2 | 5.9 | 27.5 | 6.5 ** | 26.0 | 6.0 | 27.0 | 5.9 * | 26.2 | 5.9 | 27.6 | 6.4 * | 26.9 | 6.5 | 29.0 * | 6.1 |
| Resident disempowerment scale score | 11.5 | 6.0 | 11.2 | 5.9 | 12.9 | 6.4 ** | 11.1 | 6.1 | 12.0 | 5.9 * | 11.3 | 6.0 | 12.5 | 6.2 * | 22.1 | 6.4 | 13.3 | 5.8 |
| Neighboring behavior scale score | 14.4 | 8.5 | 14.2 | 8.4 | 15.4 | 9.0 * | 14.7 | 8.6 | 14.0 | 8.3 | 14.3 | 8.5 | 15.1 | 8.4 | 15.3 | 8.4 | 14.9 | 8.3 |
| Social support score | 80.7 | 9.0 | 81.3 | 8.7 | 77.2 | 9.8 ** | 81.6 | 8.7 | 79.1 | 9.3 ** | 81.1 | 8.7 | 77.6 | 10.4 ** | 77.8 | 10.2 | 77.3 | 10.9 |
| Needs factors | ||||||||||||||||||
| Number of mental disorders in past 12 months | 0.2 | 0.6 | 0.0 | 0.0 | 1.4 | 0.7 ** | 0.2 | 0.6 | 0.2 | 0.6 | 0.1 | 0.4 | 0.8 | 1.0 ** | 1.0 | 0.0 | 1.0 | 0.0 |
| Psychological distress score | 8.2 | 6.5 | 6.8 | 5.3 | 15.4 | 7.6 ** | 8.5 | 6.8 | 7.5 | 6.0 * | 7.2 | 5.7 | 14.2 | 8.0 ** | 13.4 | 7.9 | 11.7 | 8.3 |
3.3. Variables Associated with Healthcare Service Utilization for Mental Health Reasons
| Predictors | Beta | SE | Wald | df | p | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| LL | UL | |||||||
| Gender (males) | −0.933 | 0.171 | 29.691 | 1 | 0.000 | 0.393 | 0.281 | 0.550 |
| Self-perception of physical health | 0.211 | 0.070 | 9.078 | 1 | 0.003 | 1.235 | 1.077 | 1.417 |
| Major Depressive Episode in past 12 months | 0.584 | 0.215 | 7.369 | 1 | 0.007 | 1.793 | 1.176 | 2.733 |
| Panic Disorder in past 12 months | 0.720 | 0.391 | 3.398 | 1 | 0.065 | 2.055 | 0.956 | 4.419 |
| Social Phobia in past 12 months | 0.844 | 0.297 | 8.104 | 1 | 0.004 | 2.326 | 1.301 | 4.159 |
| Emotional problems in past 12 months | 0.431 | 0.149 | 8.348 | 1 | 0.004 | 1.539 | 1.149 | 2.062 |
| Quality of life score | −0.022 | 0.001 | 217.466 | 1 | 0.000 | 0.978 | 0.976 | 0.981 |
3.4. Comparison Analyses between Participants with and without Mental Disorders
| Factors | Variables | Categories | Total Sample | No Mental Disorders | Mental Disorders | p value |
|---|---|---|---|---|---|---|
| (n = 243) | (n = 124) | (n = 119) | ||||
| n (%)/(Mean (SD)) | n (%)/(Mean (SD)) | n (%)/(Mean (SD)) | ||||
| Predisposing factors | Education (n (%)) | Secondary or more | 183 (75.3) | 101 (81.5) | 82 (68.9) | 0.023 PCT |
| Quality of life (Mean (SD)) | 97.8 (17.9) | 105.2 (15) | 90 (17.5) | 0.000 StT | ||
| Self-perception of physical health (n (%)) | Excellent or very good | 69 (28.4) | 41 (33.1) | 28 (23.5) | 0.001 PCT | |
| Good | 97 (39.9) | 57 (46) | 40 (33.6) | |||
| Poor or Fair | 77 (31.7) | 26 (21) | 51 (42.9) | |||
| Self-perception of mental health (n (%)) | Excellent or very good | 66 (27.2) | 50 (40.3) | 16 (13.4) | 0.000 PCT | |
| Good | 99 (40.7) | 52 (41.9) | 47 (39.5) | |||
| Poor or Fair | 78 (32.1) | 22 (17.7) | 56 (47.1) | |||
| Lifelong history of problems with the law (n (%)) | 30 (12.3) | 7 (5.6) | 23 (19.3) | 0.001 PCT | ||
| Enabling factors | Household income (Mean (SD)) | 47,612.0 (37,424.9) | 54,305.3 (42,077.7) | 40,637.5 (30,508.7) | 0.004 StT | |
| Social support score (Mean (SD)) | 77.6 (10.4) | 80 (9.6) | 75.2 (10.6) | 0.001 StT | ||
| Environmental variables | Neighborhood physical status (Mean (SD)) | 42.9 (11.8) | 45.3 (11.3) | 40.3 (11.9) | 0.027 StT | |
| Participation in activities in the neighborhood (Mean (SD)) | 9.3 (1.0) | 9.2 (1.2) | 9.4 (0.9) | 0.012 StT | ||
| Score of social cohesion: readiness to protect neighbor’s home when absent (Mean (SD)) | 15.1 (8.4) | 14.6 (8) | 15.7 (8.8) | 0.000 StT | ||
| Driving distance to the neighborhood community health center (in meters) (Mean (SD)) | 2099.5 (1329.9) | 2270 (1448.9) | 1921.8 (1173.3) | 0.041 StT | ||
| Proportion of immigrant population in the neighborhood (Mean (SD)) | 22.7 (9.8) | 24.6 (10.3) | 20.8 (9) | 0.003 | ||
| Mean household income in the neighborhood before income tax (Mean (SD)) | 61,932.5 (23,475.9) | 65,022.4 (25,139) | 58,712.9 (21,237.4) | 0.036 StT | ||
| Needs | Psychological distress score (Mean (SD)) | 14.2 (8.0) | 10.4 (6.5) | 18.3 (7.5) | 0.000 StT | |
| Impulsiveness score (Mean (SD)) | 64.2 (12.6) | 59.9 (10.3) | 68.6 (13.2) | 0.000 StT | ||
| Emotional problems in the 12 past months (n (%)) | 109 (44.9) | 41 (33.1) | 68 (57.1) | 0.000 PCT | ||
| Victim of violence in the 12 past months (n (%)) | 25 (10.3) | 4 (3.2) | 21 (17.6) | 0.000 FET | ||
| Aggressive behaviors in the 12 past months (n (%)) | 40 (16.5) | 9 (7.3) | 31 (26.1) | 0.000 PCT | ||
| Healthcare service professionals utilization | Visited a psychiatrist in the past 12 months (n (%)) | 64 (26.3) | 25 (20.2) | 39 (32.8) | 0.026 PCT | |
3.5. Discussion
3.5.1. Predictors of Healthcare Service Utilization for Mental Health Reasons
3.5.2. Correlates Associated with Healthcare Service Utilization for Mental Health Reasons among Individuals with and without Mental Disorders Respectively
3.6. Study Limitations
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Michaud, C.M.; Maurray, C.J.; Blonn, B.R. Burden of disease: Implications for future research. JAMA 2001, 285, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Warner, R.; de Girolamo, G. Épidémiologie des Troubles Mentaux et des Problèmes Psychosociaux: Schizophrénie; Organisation Mondiale de la Santé: Geneve, Switzerland, 1995. (In French) [Google Scholar]
- Honey, A.; Emerson, E.; Llewellyn, G.; Kariuki, M. Mental health and disability. In International Encyclopedia of Rehabilitation; Stone, J., Blouin, M., Eds.; CIRRIE: Buffalo, New York, NY, USA, 2013. [Google Scholar]
- Kohn, R.; Saxena, S.; Levav, I.; Saraceno, B. The treatment gap in mental health care. Bull. WHO 2004, 82, 858–866. [Google Scholar] [PubMed]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, severity, and comorbidity of twelve-month dsm-iv disorders in the National Comorbidity Survey Replication (NCS-R). Arch. Gen. Psychiat. 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Sunderland, A.; Findlay, L.C. Perceived need for mental health care in Canada: Results from the 2012 Canadian community health survey—Mental health. Health Rep. 2013, 24, 3–9. [Google Scholar] [PubMed]
- Lesage, A.; Émond, V. Surveillance of Mental Disorders in Québec: Prevalence, Mortality and Service Utilization Profile; Intitut National de Santé Publique: Quebec, Canada, 2013; Volume 6, p. 16. [Google Scholar]
- Thornicroft, G. Premature death among people with mental illness. BMJ 2013, 346. [Google Scholar] [CrossRef] [PubMed]
- Wilson, I.B.; Cleary, P.D. Linking clinical variables with health-related quality of life: A conceptual model of patient outcomes. JAMA 1995, 273, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Myers, A.; Rosen, J.C. Obesity stigmatization and coping: Relation to mental health symptoms, body image, and self-esteem. Int. J. Obes. Relat. Metab. Disord. 1999, 23, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.; Burns, T.; Fitzpatrick, R.; Pinfold, V.; Priebe, S. Social exclusion and mental health: Conceptual and methodological review. Brit. J. Psychiat. 2007, 191, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.M.; von Korff, M.; Angermeyer, M.C.; Benjet, C.; Bruffaerts, R.; de Girolamo, G.; Haro, J.M.; Lepine, J.P.; Ormel, J.; Posada-Villa, J.; et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Arch. Gen. Psychiat. 2011, 68, 838–844. [Google Scholar] [CrossRef]
- Schmitz, N.; Wang, J.; Malla, A.; Lesage, A. Joint effect of depression and chronic conditions on disability: Results from a population-based study. Psychosom. Med. 2007, 69, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Wonca: Integrating Mental Health into Primary Care; World Health Organization and World Organization of Family Doctors (Wonca): Singapore, Singapore, 2008.
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Caron, J. Mental health service utilization among patients with severe mental disorders. Community Ment. Health J. 2011, 47, 365–377. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Perreault, M.; Caron, J. Determinants of the utilization of diversified types of professionals for mental health reasons in a Montreal (Canadian) catchment area. Glob. J. Health Sci. 2012, 4, 13–29. [Google Scholar] [PubMed]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Perreault, M.; Caron, J. Determinants associated with the utilization of primary and specialized mental health services. Psychiat. Quart. 2012, 83, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Ngamini Ngui, A.; Perreault, M.; Fleury, M.J.; Caron, J. A multi-level study of the determinants of mental health service utilization. Rev. Epidemiol. Sante Publ. 2012, 60, 85–93. [Google Scholar]
- Bonin, J.P.; Fournier, L.; Blais, R. Predictors of mental health service utilization by people using resources for homeless people in Canada. Psychiatr. Services 2007, 58, 936–941. [Google Scholar] [CrossRef]
- Vasiliadis, H.M.; Lesage, A.; Adair, C.; Boyer, R. Service use for mental health reasons: Cross-provincial differences in rates, determinants, and equity of access. Can. J. Psychiatry 2005, 50, 614–619. [Google Scholar] [PubMed]
- Vasiliadis, H.M.; Lesage, A.; Adair, C.; Wang, P.S.; Kessler, R.C. Do Canada and the United States differ in prevalence of depression and utilization of services? Psychiatr. Serv. 2007, 58, 63–71. [Google Scholar]
- Crabb, R.; Hunsley, J. Utilization of mental health care services among older adults with depression. J. Clin. Psychol. 2006, 62, 299–312. [Google Scholar] [CrossRef] [PubMed]
- Faith, J.; Thorburn, S.; Tippens, K.M. Examining CAM use disclosure using the behavioral model of health services use. Complement. Ther. Med. 2013, 21, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Grant, J.; Westhues, A. Mental health respite services: A grounded service delivery model. Can. J. Commun. Ment. Health 2005, 24, 63–78. [Google Scholar] [PubMed]
- Grigoletti, L.; Amaddeo, F.; Grassi, A.; Boldrini, M.; Chiappelli, M.; Percudani, M.; Catapano, F.; Fiorillo, A.; Perris, F.; Bacigalupi, M.; et al. A predictive model to allocate frequent service users of community-based mental health services to different packages of care. Epidemiol. Psichiatr. Soc. 2010, 19, 168–177. [Google Scholar]
- Najimi, A.; Golshiri, P. Knowledge, beliefs and preventive behaviors regarding influenza A in students: A test of the health belief model. J. Educ. Health Promot. 2013, 2. [Google Scholar] [CrossRef]
- Montanaro, E.A.; Bryan, A.D. Comparing theory-based condom interventions: Health belief model vs. theory of planned behavior. Health Psychol. 2013, 33, 1251–1260. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.K.; Wong, M.L.; Chan, Y.H.; Feng, Z.; Wai, C.T.; Yeoh, K.G. Gender differences in predictors of colorectal cancer screening uptake: A national cross sectional study based on the health belief model. BMC Public Health 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- Baghianimoghadam, M.H.; Shogafard, G.; Sanati, H.R.; Baghianimoghadam, B.; Mazloomy, S.S.; Askarshahi, M. Application of the health belief model in promotion of self-care in heart failure patients. Acta Med. Iran. 2013, 51, 52–58. [Google Scholar] [PubMed]
- Ngamini Ngui, A.; Fleury, M.J.; Perreault, M.; Caron, J. Mental health services utilization in an inner-city of Montreal: A causal model approach. CJRS 2011, 33, 35–48. [Google Scholar]
- Andersen, R.; Harada, N.; Chiu, V.; Makinodan, T. Application of the behavioral model to health studies of Asian and Pacific Islander Americans. Asian Am. Pac. Isl. J. Health 1995, 3, 128–141. [Google Scholar] [PubMed]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Corso, K.A.; Bryan, C.J.; Corso, M.L.; Kanzler, K.E.; Houghton, D.C.; Ray-Sannerud, B.; Morrow, C.E. Therapeutic alliance and treatment outcome in the primary care behavioral health model. Fam. Syst. Health 2012, 30, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.R.; Fisher, J.D.; Cunningham, C.O.; Amico, K.R. Understanding the behavioral determinants of retention in HIV care: A qualitative evaluation of a situated information, motivation, behavioral skills model of care initiation and maintenance. AIDS Patient Care STDS 2012, 26, 344–355. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.; Golberstein, E.; Gollust, S.E. Help-seeking and access to mental health care in a university student population. Med. Care 2007, 45, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Hines-Martin, V.; Brown-Piper, A.; Kim, S.; Malone, M. Enabling factors of mental health service use among African Americans. Arch. Psychiatr. Nurs. 2003, 27, 197–294. [Google Scholar] [CrossRef]
- Fox, J.W. Sex, marital status, and age as social selection factors in recent psychiatric treatment. J. Health Soc. Behav. 1984, 25, 394–405. [Google Scholar] [CrossRef] [PubMed]
- Kirmayer, L.J.; Weinfeld, M.; Burgos, G.; Du Fort, G.G.; Lasry, J.C.; Young, A. Use of health care services for psychological distress by immigrants in an urban multicultural milieu. Can. J. Psychiatry 2007, 2, 295–304. [Google Scholar]
- Dutton, D. Explaining the low use of health services by poor: Costs, attitudes or delivery systems? Amer. Sociol. Rev. 1978, 43, 348–368. [Google Scholar] [CrossRef]
- Flett, G.L.; Blankstein, K.R.; Hicken, J.D.; Watson, M.S. Social support and help-seeking in daily hassles vs. major life events stress. J. Appl. Soc. Psychol. 1995, 25, 49–58. [Google Scholar] [CrossRef]
- Cannuscio, C.C.; Colditz, G.A.; Rimm, E.B.; Berkman, L.F.; Jones, C.P.; Kawachi, I. Employment status, social ties, and caregivers’ mental health. Soc. Sci. Med. 2004, 58, 1247–1256. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Berkman, L.F. Social ties and mental health. J. Urban Health 2001, 78, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Wray, T.B.; Dvorak, R.D.; Martin, S.L. Demographic and economic predictors of mental health problems and contact with treatment resources among adults in a low-income primary care setting. Psychol. Health Med. 2013, 18, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.; Livingston, G.; Katona, C. Mental health care for the elderly in low-income countries: A health systems approach. World Psychiat. 2007, 6, 5–13. [Google Scholar]
- Kuno, E.; Rothbard, A.B. The effect of income and race on quality of psychiatric care in community mental health centers. Community Ment. Health J. 2005, 41, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Dhingra, S.S.; Zack, M.M.; Strine, T.W.; Druss, B.G.; Berry, J.T.; Balluz, L.S. Psychological distress severity of adults reporting receipt of treatment for mental health problems in the BRFSS. Psychiatr. Services 2011, 62, 396–403. [Google Scholar] [CrossRef]
- McAlpine, D.D.; Mechanic, D. Utilization of specialty mental health care among persons with severe mental illness: The roles of demographics, need, insurance, and risk. Health Serv. Res. 2000, 35, 277–292. [Google Scholar] [PubMed]
- Lefebvre, J.; Lesage, A.; Cyr, M.; Toupin, J.; Fournier, L. Factors related to utilization of services for mental health reasons in Montreal, Canada. Soc. Psychiat. Psychiat. Epidem. 1998, 33, 291–298. [Google Scholar]
- Kessler, R.C.; Zhao, S.; Katz, S.J.; Kouzis, A.C.; Frank, R.G.; Edlund, M.; Leaf, P. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Amer. J. Psychiat. 1999, 156, 115–123. [Google Scholar] [PubMed]
- Urbanoski, K.; Rush, B.R.; Wild, T.C.; Bassani, D.G.; Castel, S. Use of mental health care services by Canadians with co-occurring substance dependence and mental disorders. Psychiatr. Serv. 2007, 58, 962–969. [Google Scholar] [CrossRef] [PubMed]
- Freeborn, D.K.; Pope, C.R.; Mullooly, J.P.; McFarland, B.H. Consistently high users of medical care among the elderly. Med. Care 1990, 28, 527–540. [Google Scholar] [CrossRef] [PubMed]
- Fasoli, D.R.; Glickman, M.E.; Eisen, S.V. Predisposing characteristics, enabling resources and need as predictors of utilization and clinical outcomes for veterans receiving mental health services. Med. Care 2010, 48, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Handy, J.R., Jr.; Child, A.I.; Grunkemeier, G.L.; Fowler, P.; Asaph, J.W.; Douville, E.C.; Tsen, A.C.; Ott, G.Y. Hospital readmission after pulmonary resection: Prevalence, patterns, and predisposing characteristics. Ann. Thorac. Surg. 2001, 72, 1855–1859. [Google Scholar] [CrossRef] [PubMed]
- Atchison, K.A.; Davidson, P.L.; Nakazono, T.T. Predisposing, enabling, and need for dental treatment characteristics of ICS-II USA ethnically diverse groups. Adv. Dent. Res. 1997, 11, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Sachdev, P.; Kruk, J. Clinical characteristics and predisposing factors in acute drug-induced akathisia. Arch. Gen. Psychiat. 1994, 51, 963–974. [Google Scholar] [PubMed]
- Regier, D.A.; Goldberg, I.D.; Taube, C.A. The de facto U.S. mental health services system: A public health perspective. Arch. Gen. Psychiat. 1978, 35, 685–693. [Google Scholar] [PubMed]
- Smith, S.L.; Melton, J.; Olyneolo, M.; Buchwald, K. Introducing trampoline use within an acute mental health care hospital setting. J. Psychiatr. Intensive Care 2009, 5, 113–121. [Google Scholar] [CrossRef]
- Caron, J.; Fleury, M.J.; Perreault, M.; Crocker, A.; Tremblay, J.; Tousignant, M.; Kestens, Y.; Cargo, M.; Daniel, M. Prevalence of psychological distress and mental disorders, and use of mental health services in the epidemiological catchment area of Montreal south-west. BMC Psychiat. 2012, 12. [Google Scholar] [CrossRef]
- Brugha, T.S.; Bebbington, P.E.; Singleton, N.; Melzer, D.; Jenkins, R.; Lewis, G.; Farrell, M.; Bhugra, D.; Lee, A.; Meltzer, H. Trends in service use and treatment for mental disorders in adults throughout Great Britain. Brit. J. Psychiat. 2004, 185, 378–384. [Google Scholar] [PubMed]
- Druss, B.G.; Wang, P.S.; Sampson, N.A.; Olfson, M.; Pincus, H.A.; Wells, K.B.; Kessler, R.C. Understanding mental health treatment in persons without mental diagnoses: Results from the national comorbidity survey replication. Arch. Gen. Psychiat. 2007, 64, 1196–1203. [Google Scholar] [CrossRef]
- Wang, P.S.; Lane, M.; Olfson, M.; Pincus, H.A.; Wells, K.B.; Kessler, R.C. Twelve-month use of mental health services in the United States: Results from the national comorbidity survey replication. Arch. Gen. Psychiat. 2005, 62, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Frank, R.G.; Edlund, M.; Katz, S.J.; Lin, E.; Leaf, P. Differences in the use of psychiatric outpatient services between the United States and Ontario. N. Engl. J. Med. 1997, 336, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Bijl, R.V.; de Graaf, R.; Hiripi, E.; Kessler, R.C.; Kohn, R.; Offord, D.R.; Ustun, T.B.; Vicente, B.; Vollebergh, W.A.; Walters, E.E.; et al. The prevalence of treated and untreated mental disorders in five countries. Health Affair 2003, 22, 122–133. [Google Scholar] [CrossRef]
- Demyttenaere, K.; Bruffaerts, J.; Posalada-Villa, J.; Gasquet, I.; Kovess, V.; Lepine, J.P.; Angermeyer, M.C.; Bernet, S.; de Girolamo, G.; Moriosini, P.; et al. Prevalence, severity and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA 2004, 291, 2581–2590. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Perreault, M.; Kestens, Y.; Caron, J. Comprehensive determinants of health service utilisation for mental health reasons in a Canadian catchment area. Int. J. Equity Health 2012, 11. [Google Scholar] [CrossRef]
- Eaton, W.W.; Anthony, J.C.; Tepper, S.; Dryman, A. Psychopathology and attrition in the epidemiologic catchment area surveys. Amer. J. Epidemiol. 1992, 135, 1051–1059. [Google Scholar]
- Park, S.; Sohn, J.H.; Hong, J.P.; Chang, S.M.; Lee, Y.M.; Jeon, H.J.; Cho, S.J.; Bae, J.N.; Lee, J.Y.; Son, J.W.; et al. Prevalence, correlates, and comorbidities of four DSM-IV specific phobia subtypes: Results from the Korean epidemiological catchment area study. Psychiat. Res. 2013. [Google Scholar] [CrossRef]
- Larson, S.L.; Clark, M.R.; Eaton, W.W. Depressive disorder as a long-term antecedent risk factor for incident back pain: A 13-year follow-up study from the Baltimore epidemiological catchment area sample. Psychol. Med. 2004, 34, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Pawlowski, T.; Kiejna, A. Pathways to psychiatric care. II. “Psie Pole” epidemiological catchment area. Psychiatr Pol. 2003, 37, 1063–1071. [Google Scholar] [PubMed]
- Messias, E.; Kirkpatrick, B. Summer birth and deficit schizophrenia in the epidemiological catchment area study. J. Nerv. Ment. Dis. 2001, 189, 608–612. [Google Scholar] [CrossRef] [PubMed]
- Statistiques Canada. Enquête sur la Santé Dans les Collectivités Canadiennes (ESCC-2002)—Santé Mentale et Bien-Être (Cycle 1.2); Santé Canada: Ottawa, Canada, 2003. (In French) [Google Scholar]
- Baker, F.; Intaglia, J. Quality of life in the evaluation of Community support systems. Eval. Program Plan. 1982, 5, 69–79. [Google Scholar] [CrossRef]
- Perkins, D.D.; Long, D.A. Neighborhoud sense of community and social capital: A multi-level analysis. In Psychological Sense of Community: Research, Applications and Implications; Fisher, A.T., Sonn, C.C., Bishop, B.J., Eds.; Springer: Berlin, Germany, 2002; pp. 291–318. [Google Scholar]
- Saegert, S.; Winke, G. Crime, social capital, and community participation. Amer. J. Community Psychol. 2004, 34, 219–233. [Google Scholar] [CrossRef]
- Nario-Redmond, M.; Coulton, C. Measuring resident perceptions of neighborhood conditions: Survey methodology. In Center of Urban Poverty and Social Change; Case Western Reserve University: Cleveland, OH, USA, 2000. [Google Scholar]
- Sampson, R.J.; Morenoff, J.D.; Gannon-Rowley, T. Assessing neighborhood effects: Social processes and new directions in research. Annu. Rev. Sociol. 2002, 28, 443–478. [Google Scholar] [CrossRef]
- Coulton, C.J.; Korbin, J.E.; Su, M. Measuring neighborhood context for young children in an urban area. Amer. J. Community Psychol. 1996, 24, 5–32. [Google Scholar] [CrossRef]
- Cutrona, C.E. Behavioral manifestation of social support: A micro-analytic study. J. Pers. Soc. Psychol. 1989, 51, 201–208. [Google Scholar]
- Kessler, R.C.; Andrews, G.; Mroczek, D.; Ustun, B.; Wittchen, H.U. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int. J. Meth. Psychiatr. Res. 1998, 7, 171–185. [Google Scholar] [CrossRef]
- Kay, S.R.; Wolkenfied, F.; Murrill, L.M. Profiles of aggression among psychiatrist patients. I. Nature and prevalence. J. Nerv. Ment. Dis. 1988, 176, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.L.; Mandercheid, R.W.; Walters, E.E.; et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiat. 2003, 60, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Barratt, E.S. Impulsiveness subtraits: Arousal and information processing. In Motivation, Emotion and Personality; Spence, J.T., Itard, C.E., Eds.; Elsevier: Amsterdam, The Netherlands, 1985; pp. 137–146. [Google Scholar]
- Dunlop, S.; Coyte, P.C.; McIsaac, W. Socio-economic status and the utilisation of physicians’ services: Results from the Canadian national population health survey. Soc. Sci. Med. 2000, 51, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Walters, V.; McDonough, P.; Strohschein, L. The influence of work, household structure, and social, personal and material resources on gender differences in health: An analysis of the 1994 Canadian national population health survey. Soc. Sci. Med. 2002, 54, 677–692. [Google Scholar] [CrossRef] [PubMed]
- Vasiliadis, H.M.; Gagne, S.; Jozwiak, N.; Preville, M. Gender differences in health service use for mental health reasons in community dwelling older adults with suicidal ideation. Int. Psychogeriatr. 2013, 25, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Drapeau, A.; Boyer, R.; Lesage, A. The influence of social anchorage on the gender difference in the use of mental health services. J. Behav. Health Serv. Res. 2009, 36, 372–384. [Google Scholar] [CrossRef] [PubMed]
- Drapeau, A.; Lesage, A.; Boyer, R. Is the statistical association between sex and the use of services for mental health reasons confounded or modified by social anchorage? Can. J. Psychiatry 2005, 50, 599–604. [Google Scholar]
- Bertakis, K.D.; Azari, R.; Helms, L.J.; Callahan, E.J.; Robbins, J.A. Gender differences in the utilization of health care services. J. Fam. Pract. 2000, 49, 147–152. [Google Scholar] [PubMed]
- Alexandrino-Silva, C.; Wang, Y.P.; Carmen Viana, M.; Bulhoes, R.S.; Martins, S.S.; Andrade, L.H. Gender differences in symptomatic profiles of depression: Results from the Sao Paulo megacity mental health survey. J. Affect. Disord. 2013, 147, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Swami, V. Mental health literacy of depression: Gender differences and attitudinal antecedents in a representative British sample. PLoS One 2012, 7. [Google Scholar] [CrossRef] [PubMed]
- Maguen, S.; Luxton, D.D.; Skopp, N.A.; Madden, E. Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. J. Psychiatr. Res. 2012, 46, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Grella, C.E.; Lovinger, K. Gender differences in physical and mental health outcomes among an aging cohort of individuals with a history of heroin dependence. Addict. Behav. 2012, 37, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Tamers, S.L.; Beresford, S.A.; Thompson, B.; Zheng, Y.; Cheadle, A.D. Exploring the role of co-worker social support on health care utilization and sickness absence. J. Occup. Environ. Med. 2011, 53, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.M.; Glazier, R.H.; Sibley, L.M. The predictors of self-rated health and the relationship between self-rated health and health service needs are similar across socioeconomic groups in Canada. J. Clin. Epidemiol. 2010, 63, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Trump, D. Self-rated health and health care utilization after military deployments. Mil. Med. 2006, 171, 662–668. [Google Scholar]
- Kim, C.; Vahratian, A. Self-rated health and health care use among women with histories of gestational diabetes mellitus. Diabetes Care 2010, 33, 41–42. [Google Scholar] [CrossRef] [PubMed]
- Pattussi, M.P.; Peres, K.G.; Boing, A.F.; Peres, M.A.; da Costa, J.S. Self-rated oral health and associated factors in Brazilian elders. Community Dent. Oral Epidemiol. 2010, 38, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Ostile, I.L.; Johansson, I.; Aasland, A.; Flato, B.; Moller, A. Self-rated physical and psychosocial health in a cohort of young adults with juvenile idiopathic arthritis. Scand. J. Rheumatol. 2010, 39, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Giatti, L.; Barreto, S.M.; Cesar, C.C. Unemployment and self-rated health: Neighborhood influence. Soc. Sci. Med. 2010, 71, 815–823. [Google Scholar] [CrossRef] [PubMed]
- Toft, A.M.; Moller, H.; Laursen, B. The years after an injury: Long-term consequences of injury on self-rated health. J. Trauma 2010, 69, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Sondergaard, H.; Juul, S. Self-rated health and functioning in patients with chronic renal disease. Dan. Med. Bull. 2010, 57, A4220. [Google Scholar] [PubMed]
- Farkas, J.; Kosnik, M.; Flezar, M.; Suskovic, S.; Lainscak, M. Self-rated health predicts acute exacerbations and hospitalizations in patients with COPD. Chest 2010, 138, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Galenkamp, H.; Deeg, D.J.; Braam, A.W.; Huisman, M. “How was your health 3 years ago”? Predicting mortality in older adults using a retrospective change measure of self-rated health. Geriatr. Gerontol. Int. 2013, 13, 678–686. [Google Scholar] [CrossRef] [PubMed]
- Ng, N.; Hakimi, M.; Santosa, A.; Byass, P.; Wilopo, S.A.; Wall, S. Is self-rated health an independent index for mortality among older people in Indonesia? PLoS One 2012, 7. [Google Scholar] [CrossRef]
- Wennberg, P.; Rolandsson, O.; Jerden, L.; Boeing, H.; Sluik, D.; Kaaks, R.; Teucher, B.; Spijkerman, A.; Bueno de Mesquita, B.; Dethlefsen, C.; et al. Self-rated health and mortality in individuals with diabetes mellitus: Prospective cohort study. BMJ Open 2012, 2. [Google Scholar] [CrossRef] [PubMed]
- Giltay, E.J.; Vollaard, A.M.; Kromhout, D. Self-rated health and physician-rated health as independent predictors of mortality in elderly men. Age Ageing 2012, 41, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.S.; Fink, P.; Frydenberg, M.; Oxhøj, M.L. Use of health services, mental illness, and self-rated disability and health in medical inpatients. Psychosom. Med. 2002, 64, 668–675. [Google Scholar] [PubMed]
- Valderas, J.M.; Starfield, B.; Sibbald, B.; Salisbury, C.; Roland, M. Defining comorbidity: Implications for understanding health and health services. Ann. Fam. Med. 2009, 7, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Bijl, R.V.; Ravelli, A. Psychiatric morbidity, service use, and need for care in the general population: Results of the Netherlands mental health survey and incidence study. Amer. J. Public Health 2000, 90, 602–607. [Google Scholar] [CrossRef]
- Jorm, A.F.; Christensen, H.; Griffiths, K.M.; Rodgers, B. Effectiveness of complementary and self-help treatments for depression. Med. J. Aust. 2002, 176, S84–S96. [Google Scholar] [PubMed]
- Ten Have, M.; de Graaf, R.; Vollebergh, W.; Beekman, A. What depressive symptoms are associated with the use of care services? Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). J. Affect. Disord. 2004, 80, 239–248. [Google Scholar] [PubMed]
- Koenig, H.G.; Kuchibhatla, M. Use of health services by hospitalized medically ill depressed elderly patients. Amer. J. Psychiat. 1998, 155, 871–877. [Google Scholar] [PubMed]
- Deacon, B.; Lickel, J.; Abramowitz, J.S. Medical utilization across the anxiety disorders. J. Anxiety Disord. 2008, 22, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.B.; McQuaid, J.R.; Laffaye, C.; McCahill, M.E. Social phobia in the primary care medical setting. J. Fam. Pract. 1999, 48, 514–519. [Google Scholar] [PubMed]
- Bystritsky, A.; Kerwin, L.; Niv, N.; Natoli, J.L.; Abrahami, N.; Klap, R.; Wells, K.; Young, A.S. Clinical and subthreshold panic disorder. Depress. Anxiety 2010, 27, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Dhingra, S.S.; Zack, M.; Strine, T.; Pearson, W.S.; Balluz, L. Determining prevalence and correlates of psychiatric treatment with Andersen’s behavorial model of health services use. Psychiatr. Serv. 2010, 61, 514–528. [Google Scholar] [CrossRef]
- Parslow, R.A.; Jorm, A.F. Who uses mental health services in Australia? An analysis of data from the national survey of mental health and wellbeing. Aust. N. Z. J. Psychiat. 2000, 34, 997–1008. [Google Scholar] [CrossRef]
- Mendenhall, A.N.; Demeter, C.; Findling, R.L.; Frazier, T.W.; Fristad, M.A.; Youngstrom, E.A.; Arnold, L.E.; Birmaher, B.; Gill, M.K.; Axelson, D.; et al. Factors influencing mental health service utilization by children with serious emotional and behavioral disturbance: Results from the LAMS study. Psychiatr. Serv. 2011, 62, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Teich, J.L.; Buck, J.A.; Graver, L.; Schroeder, D.; Zheng, D. Utilization of public mental health services by children with serious emotional disturbances. Adm. Policy Ment. Health 2003, 30, 523–534. [Google Scholar] [CrossRef] [PubMed]
- Kehusmaa, S.; Autti-Ramo, I.; Helenius, H.; Hinkka, K.; Valaste, M.; Rissanen, P. Factors associated with the utilization and costs of health and social services in frail elderly patients. BMC Health Serv. Res. 2012, 12. [Google Scholar] [CrossRef]
- Saarela, T.M.; Finne-Soveri, H.; Liedenpohja, A.M.; Noro, A. Comparing psychogeriatric units to ordinary long-term care units—Are there differences in case-mix or clinical symptoms? Nord. J. Psychiatr. 2008, 62, 32–38. [Google Scholar]
- Chen, T.; Li, L. Influence of health-related quality of life on health service utilization in addition to socio-demographic and morbidity variables among primary care patients in China. Int. J. Public Health 2009, 54, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Dominick, K.L.; Ahern, F.M.; Gold, C.H.; Heller, D.A. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clin. Exp. Res. 2002, 14, 499–508. [Google Scholar] [CrossRef] [PubMed]
- Albert, M.; Becker, T.; McCrone, P.; Thornicroft, G. Social networks and mental health service utilisation. A literature review. Int. J. Soc. Psychiatr. 1998, 44, 248–266. [Google Scholar] [CrossRef]
- Pescosolido, B.A.; Gardner, C.B.; Lubell, K.M. How people get into mental health services: Stories of choice, coercion and “muddling through” from “first-timers”. Soc. Sci. Med. 1998, 46, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Pescosolido, B.A.; Wright, E.R.; Alegria, M.; Vera, M. Social networks and patterns of use among the poor with mental health problems in Puerto Rico. Med. Care 1998, 36, 1057–1072. [Google Scholar] [CrossRef] [PubMed]
- Howard, K.I.; Cornille, T.A.; Lyons, J.S.; Vessey, J.T.; Lueger, R.J.; Saunders, S.M. Patterns of mental health service utilization. Arch. Gen. Psychiat. 1996, 53, 696–703. [Google Scholar] [CrossRef] [PubMed]
- Chartier-Otis, M.; Perreault, M.; Bélanger, C. Determinants of barriers to treatment for anxiety disorders. Psychiat. Quart. 2010, 81, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Whitley, R.; McKenzie, K. Social capital and psychiatry: Review of the literature. Harv. Rev. Psychiat. 2005, 13, 71–84. [Google Scholar] [CrossRef]
- Browning, C.R.; Cagney, K.A. Neighborhood structural disavantage, collective efficacy, and self-rated health in an urban setting. J. Health Soc. Behav. 2002, 43, 383–399. [Google Scholar] [CrossRef] [PubMed]
- Putnam, R.D. E Pluribus Unum: Diversity and community in the twenty-first century. The 2006 Johan Skytte Prize lecture. Scand. Polit. Stud. 2007, 30, 137–174. [Google Scholar] [CrossRef]
- Rios, R.; Aiken, L.S.; Zautra, A.J. Neighborhood contexts and the mediating role of neighborhood social cohesion on health and psychological distress among Hispanic and non-Hispanic residents. Ann. Behav. Med. 2012, 43, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Caron, J.; Liu, A. Factors associated with psychological distress in the Canadian population: A comparison of low-income and non low-income sub-groups. Community Ment. Health J. 2011, 47, 318–330. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.; Edlund, M. Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatr. Services 2005, 56, 954–959. [Google Scholar] [CrossRef]
- Tempier, R.; Meadows, G.N.; Vasiliadis, H.M.; Mosier, K.E.; Lesage, A.; Stiller, A.; Graham, A.; Lepnurm, M. Mental disorders and mental health care in Canada and Australia: Comparative epidemiological findings. Soc. Psychiat. Psychiat. Epidem. 2009, 44, 63–72. [Google Scholar] [CrossRef]
- Keene, J.; Li, X. Age and gender differences in health service utilization. J. Public Health 2005, 27, 74–79. [Google Scholar] [CrossRef]
- Elnitsky, C.; Chapman, P.; Thurman, R.; Pitts, B.; Figley, C.; Unwin, B. Gender differences in combat medic mental health services utilization, barriers, and stigma. Mil. Med. 2013, 178, 775–784. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fleury, M.-J.; Ngui, A.N.; Bamvita, J.-M.; Grenier, G.; Caron, J. Predictors of Healthcare Service Utilization for Mental Health Reasons. Int. J. Environ. Res. Public Health 2014, 11, 10559-10586. https://doi.org/10.3390/ijerph111010559
Fleury M-J, Ngui AN, Bamvita J-M, Grenier G, Caron J. Predictors of Healthcare Service Utilization for Mental Health Reasons. International Journal of Environmental Research and Public Health. 2014; 11(10):10559-10586. https://doi.org/10.3390/ijerph111010559
Chicago/Turabian StyleFleury, Marie-Josée, André Ngamini Ngui, Jean-Marie Bamvita, Guy Grenier, and Jean Caron. 2014. "Predictors of Healthcare Service Utilization for Mental Health Reasons" International Journal of Environmental Research and Public Health 11, no. 10: 10559-10586. https://doi.org/10.3390/ijerph111010559
APA StyleFleury, M.-J., Ngui, A. N., Bamvita, J.-M., Grenier, G., & Caron, J. (2014). Predictors of Healthcare Service Utilization for Mental Health Reasons. International Journal of Environmental Research and Public Health, 11(10), 10559-10586. https://doi.org/10.3390/ijerph111010559




