Abstract
Cardiovascular diseases (CVDs) are among the most impactful illnesses globally. Currently, the available therapeutic option has several side effects, including hypotension, bradycardia, arrhythmia, and alteration in different ion concentrations. Recently, bioactive compounds from natural sources, including plants, microorganisms, and marine creatures, have gained a lot of interest. Marine sources serve as reservoirs for new bioactive metabolites with various pharmacological activities. The marine-derived compound such as omega-3 acid ethyl esters, xyloketal B, asperlin, and saringosterol showed promising results in several CVDs. The present review focuses on marine-derived compounds’ cardioprotective potential for hypertension, ischemic heart disease, myocardial infarction, and atherosclerosis. In addition to therapeutic alternatives, the current use of marine-derived components, the future trajectory, and restrictions are also reviewed.
1. Introduction
Cardiovascular diseases (CVDs) are one of the most critical conditions affecting human health globally. It includes pulmonary circulation, heart, vascular, and cerebrovascular diseases with higher recurrence and incidence rates [1]. According to 2019 data, CVDs cover 32% with approximately 17.9 million of all deaths around the world. The incidence of CVD-related mortality has grown from 12.1 in 1991 to 18.6 million in 2019 and is expected to increase to 24 million by 2030 [2]. It has been estimated that CVDs will affect approximately 135 million people, with USD 1.1 trillion in costs [3]. Approximately one third of all fatalities worldwide in 2019 were attributable to CVDs, which caused the deaths of 8.9 million women and 9.6 million men. A total of 6.1 million of these fatalities occurred between the ages of 30 and 70. China had the most CVD fatalities, followed by India, the Russian Federation, the United States, and Indonesia [4]. An equal proportion of males and females are affected by CVDs globally, but mortality is higher among women [5]. The goal of the recommendations made by an international group of leaders and professionals in the area is to significantly lower the burden of cardiovascular disease worldwide by 2030 [6]. There are several possible causes of CVDs, such as obesity, smoking, high blood pressure, hyperlipidemia, and diabetes [7]. However, mitochondrial dysfunction is a major factor in CVDs’ pathogenesis via regulating ROS generation [8]. Diseases such as diabetes mellitus, COVID-19 [9], and chronic kidney disease (CKD) [10] also cause CVDs via various pathological pathways in both male and female populations around the world [11]. Currently, several synthetic drugs, including plasminogen activators, angiotensin-converting enzyme blockers, angiotensin-2 receptor blockers, calcium channel blockers, β-blockers, diuretics, and surgery, are used to treat CVDs. However, they are associated with severe adverse effects, including time-dependent effects, hypotension, hypersensitivity, bradycardia, arrhythmia, alteration in several ion levels, e.g., potassium and sodium, and surgical complications [12]. Thus, there is a gap in finding new molecular targets and mechanisms to overcome side effects associated with exitance therapy. Marine drugs have minimal toxicity, no multidrug resistance, and no immune system suppression in CVDs’ patients [13]. Marine natural drugs are more convenient for CVDs due to their high safety profile, numerous biological activities, and natural origin [14]. Furthermore, they demonstrate a wide range of biological actions against various CVDs, including antioxidant, lipid lowering, anti-inflammatory, thrombin inhibition, anti-coagulation, vasodilation, hypoglycemia inducing, antiplatelet activation, and enzyme and ion channel receptor blocking [15]. Thus, marine-derived natural compounds are novel candidates over synthetic drugs for the minimization of adverse effects in CVDs and associated complications. Marine pharmaceuticals are preferable to other products due to their low toxicity, chemical variety, economic effectiveness, and demonstrated therapeutic promise.
2. Marine Biodiversity: As Bioactive Reservoirs
The importance of marine natural products (MNPs) in drug discovery, particularly their role in creating current medications, has been well documented [16]. Marine species are the most current source of bioactive natural compounds compared to terrestrial plants and nonmarine microbes. By 2016, 28500 MNPs had been identified, and most had anticancer and cytotoxic properties [17].
The marine environment is a natural habitat for a wide diversity of species with varying physiologies and adaptability to the environment. Out of the more than 33 animal phyla known today, 32 phyla are represented in the marine environment, 15 of which are peculiar to the marine environment [18]. More than 80% of the world’s plant and animal species live in the oceans. Marine organisms include sponges, tunicates, fishes, soft corals, nudibranchs, sea hares, opisthobranch, mollusks, echinoderms, bryozoans, prawns, shells, sea slugs, and marine microorganisms are sources of bioactive compounds [19,20]. Marine ecosystems provide a rich reservoir of novel bioactive chemical entities with significant medicinal potential [21]. The diversity of such molecules is distinct, and their development is encouraged by the chemical and physical circumstances of the sea. It is well known that marine species can create bioactive chemicals to protect themselves against unusual environmental circumstances such as high salt, reactive oxygen species, photodynamic damage, and high temperatures [22]. The ancient Greek, Byzantium, and Mediterranean cultures used marine animals for therapeutic reasons. Since marine invertebrates have become so significant in medical practice, much work has been committed to utilizing them. The medicinal or therapeutic properties and how raw materials are handled and delivered were recorded in ancient literature. Several marine invertebrates have been utilized as fresh or dried meat in beverages, liquids, crushed goods, soups, and ointments [23]. Traditional Chinese medicine has also contributed to marine drug research. Local diaries, folk recipes, bibliographies, early prescriptions, and dietary advice have contributed to our comprehensive grasp of marine medicines and other species. All of this information, as well as subsequent discoveries, may be found in the Chinese marine Materia medica [24]. Despite over 250 years of marine research, over 91% of marine creatures still require a complete description. Since the earliest marine animals appeared around 3500 million years ago, adverse conditions fostered the evolution of a diverse range of bioactive chemicals to resist environmental stress [25].
The birth of marine drugs occurred in the 19th century, once biotechnology arose as a science that offered direction to the research of marine medication creation. These marine-derived medications have been utilized to treat various ailments, including cancer, heart disease, diabetes, and neurodegenerative disease [26]. Over the last five decades, evidence has accumulated that marine-based plants and microbes have a greater potential for cancer treatment. For example, cytarabine, eribulin mesylate, brentuximab vedotin, and trabectidine are marine-based drugs used to treat leukemia, metastatic breast cancer, soft tissue sarcoma, and ovarian cancer [21]. Currently, ≥26,680 have been isolated and identified from marine-derived sources, with an average addition of 1000 per year. Due to the specificity of bioactive compounds toward the targets, they are beneficial in cancer therapy targeting cancerous cells [27].
Classification of Marine Drugs
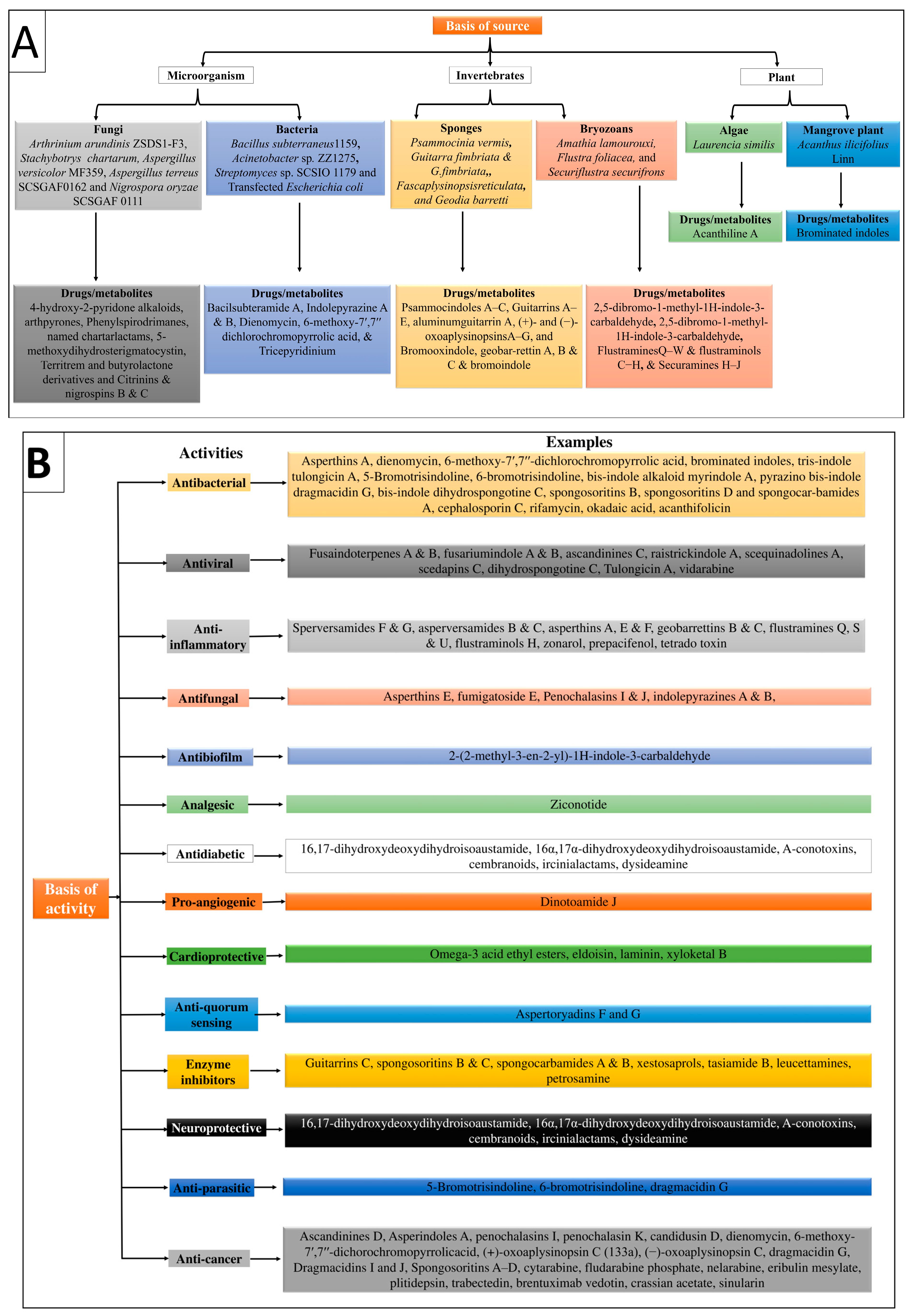
Marine drugs are classified based on their sources and pharmacological actions, compiled in Table 1, Figure 1A,B.

Table 1.
Classification of natural marine compounds.
Figure 1.
Illustration of the classification of marine-derived compounds based on (A) sources and (B) activity.
3. Role of Marine Drugs in CVDs Management
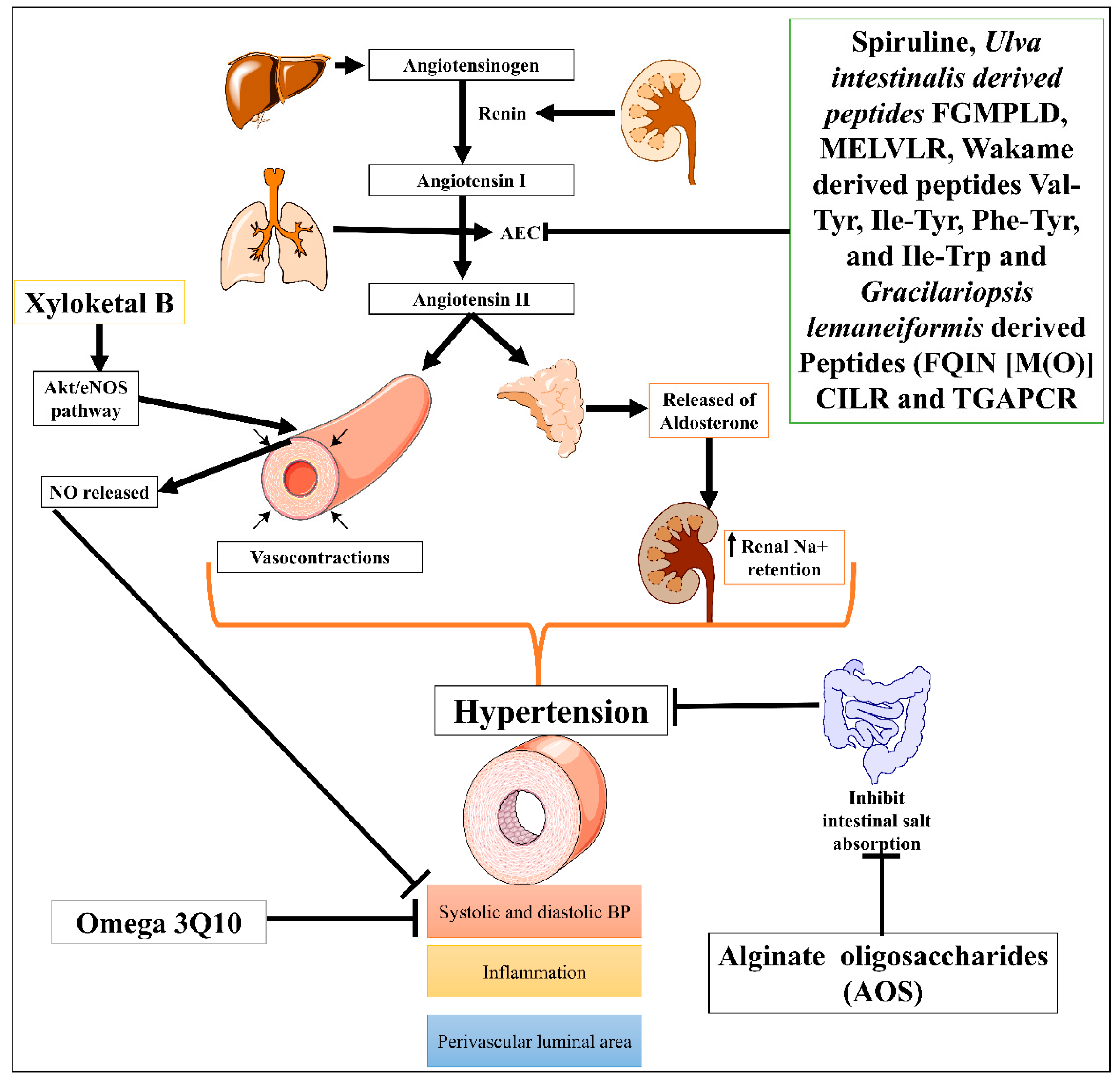
3.1. Hypertension
Hypertension is one of the most severe problems among all CVDs, and is responsible for stroke, ischemic heart disease, dementia, chronic kidney disease, and other CVDs [62]. According to 2019 age-standardized prevalence data, 32% of women and 34% of men aged 30–79 worldwide had hypertension [63]. Many marine natural compounds, including bioactive molecules, chito-oligosaccharide derivatives (COS), and phlorotannins, were obtained from marine species and are potential leads for ACE inhibitors and evolved as nutraceutical medicinal compounds for the treatment of hypertension [64,65]. Natural marine ACE inhibitors are being studied as alternatives to synthetic drugs to avoid several serious side effects and hold a significant potential to become new therapeutic options for the treatment of hypertension [66]. Biopeptides or ACE-inhibitory peptides derived from fish proteins are often made under controlled circumstances by proteolyzing marine proteins advanced for the treatment of hypertension [67]. Furthermore, marine red algae Gracilariopsis lemaneiformis have been identified as producing several marine-based new ACE inhibiting peptides, FQIN [M(O)] CILR and TGAPCR, discovered by LC-MS/MS screening in G. lemaneiformis protein hydrolysates. These peptides significantly decreased systolic and diastolic blood pressure (DBP) in the spontaneously hypertensive rat model [68]. In the same direction, Sato M. et al. identified seven peptides: Val-Tyr, Ile-Tyr, Ala-Trp, Phe-Tyr, Val-Trp, Ile-Trp, and Leu-Trp from hydrolysates of wakame (Undaria pinnatifida) brown seaweed using three steps, HPLC and liquid chromatography-mass spectroscopy. Four of seven seaweed-derived peptides (Val-Tyr, Ile-Tyr, Phe-Tyr, and Ile-Trp) significantly reduced systolic blood pressure in spontaneously hypertensive rats at a dose of 1 mg/kg. This offers a possible source of new AEC inhibitors as antihypertensives [69]. In addition, Sun et al. also identified two Phe-Gly-Met-Pro-Leu-Asp-Arg (FGMPLDR; MW 834.41 Da) and Met-Glu-Leu-Val-Leu-Arg (MELVLR; MW 759.43 Da) ACE inhibitory peptides from the protein hydrolysate marine macroalga of Ulva intestinalis. In silico and in vitro molecular docking studies revealed these two peptides have ACE binding and inhibitory activity [70].
One of the most well-known marine-derived compounds is alginate oligosaccharides (AOS) that offer protection against perivascular inflammation, reduction in the vascular luminal area, and hemodynamic alterations of pulmonary hypertension in the rat produced by monocrotaline (MCT) model via downregulating P-selectin [71]. Another study demonstrated that omega-3 Q10, a polyunsaturated fatty acid (n3-PUFA) formulation, appears to be more effective than soybean oil supplementation at reducing diastolic blood pressure and associated symptoms with hypertension in older adults [72]. Moreover, mangrove fungus-isolated xyloketal B showed phenylephrine (Phe)-induced contractions induced hypertension protection by decreasing the systolic and diastolic blood pressure via enhancing endothelial NO release through the Akt/eNOS pathway [51]. In addition, a controlled trial study conducted by Sámano MJ et al. evaluated the combination of Spirulina (Arthrospira) maxima (filamentous, gram-negative cyanobacterium) with angiotensin-converting enzyme (ACE) inhibitors in patients with systemic arterial hypertension (SAH) and accessed its effects on endothelial damage and oxidative stress. Results showed that Spirulina significantly reduced systolic blood pressure, increased anti-oxidant level (glutathione peroxidase activity and oxidized glutathione), and decreased endothelial damage markers (sVCAM-1, sE-selectin, and endothelin-1) [73]. It has other properties such as antiviral, anti-dyslipidemic, and antioxidant [74]. Low molecular mass potassium alginate (L-PA), brown algae, shows an antihypertensive effect on DOCA salt-induced hypertension in rats (Figure 2) [75]. Overall, data suggested that marine-derived compounds have the potential to cure hypertension, but a detailed mechanistic study is still needed. Moreover, Therapeutic potential of marine drugs in CVDs management has been tubulated in Table 2.
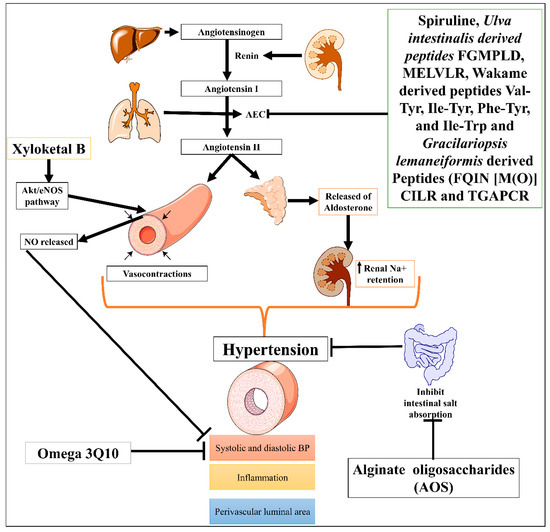
Figure 2.
Possible mechanism of different marine-derived compounds in CVDs.

Table 2.
Preclinical study of marine drugs in various CVDs.
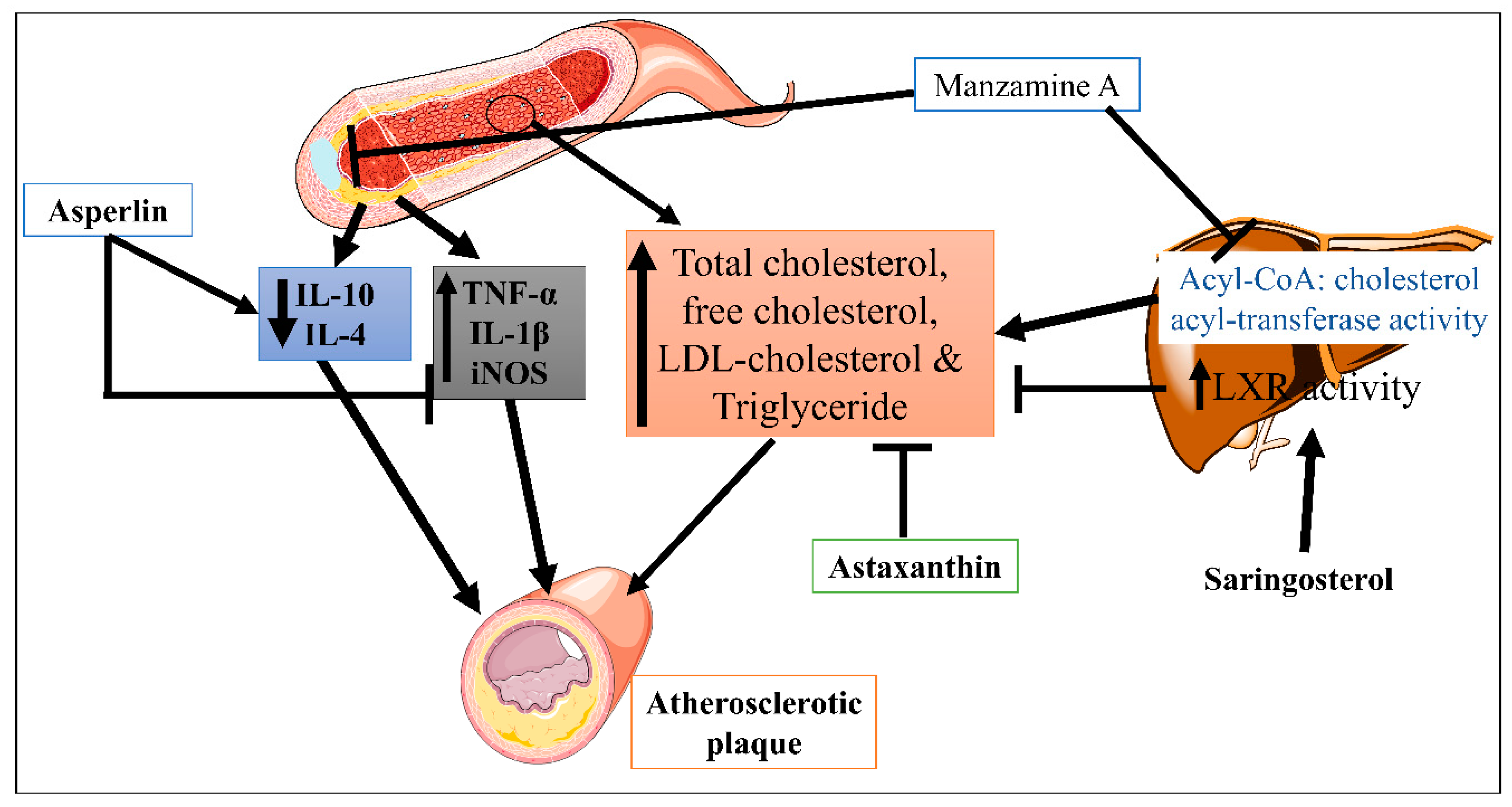
3.2. Atherosclerosis
Atherosclerosis is a chronic, inflammatory, progressive cardiovascular disease that results from ongoing blood vessel damage brought on by hyperlipidemia and increased cholesterol levels [93]. Marine-based derived compounds have been effective against atherosclerosis since ancient times. These compounds have advantages over synthetic compounds in atherosclerosis due to greater effectiveness and lower side effects [94]. Marine-derived algal polysaccharides are the active ingredients in products made from marine sources that have a hypolipidemic impact and cure atherosclerosis.
Saringosterol, a phytosterol derived from the edible marine seaweed Sargassum fusiforme, has high and selective liver X receptor (LXR) activity [95]. Yan et. al. reported that saringosterol treatment reduced the burden of atherosclerotic plaques while having no negative effects on the liver of apoE-deficient rats. Saringosterol reduces cholesterol homeostasis disruption, influencing atherosclerosis’s progression [79]. However, asperlin is derived from the marine fungus Aspergillus versicolor LZD4403 and possesses antifungal and anti-inflammatory properties. Zhou Y et. al. reported that asperlin has atheroprotective potential in vitro and in vivo. Results indicated that asperlin treatment significantly reduced inflammatory cytokines (iNOS, IL-1β, and TNF-α), increased protective cytokines (IL-10 and IL-4), and reduced aortic dilation and atherosclerosis plaque formation in the aorta [77]. This suggested that the anti-inflammatory properties of asperlin could be beneficial against atherosclerosis. Manzamine A is a naturally occurring alkaloid obtained from the sea sponge Acanthostrongylophora ingens [96]. In atherosclerosis, Eguchi et al. conducted a study where Manzamine A suppressed acyl-CoA: cholesterol acyl-transferase activity in hamster ovary cells. In addition, Manzamine A treatment significantly reduced the serum level of total cholesterol, free cholesterol, LDL-cholesterol, triglyceride, and atherosclerotic lesion formation in apolipoprotein E (apoE)-deficient mice [80]. Astaxanthin is a xanthophyll pigment obtained from microalgae, fungi, complex plants, seafood, and flamingos. As an antioxidant with anti-inflammatory characteristics, it has the potential to be used as a treatment for atherosclerotic cardiovascular disease [97]. Yang Y et. al. demonstrated the hypocholesterolemic effect of astaxanthin via reducing total plasma cholesterol, TG and increased LDL receptor (LDLR), 3-hydroxy-3-methylglutaryl CoA reductase, and sterol regulatory element binding-protein 2 (SREBP-2) and greater mature SREBP-2 protein apoE(-/-) mice (Figure 3) [81]. In high-fat diet mice, Xyloketal B also protects against atherosclerosis through a strong antioxidant effect [78].
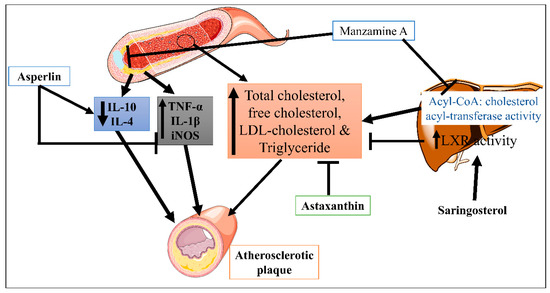
Figure 3.
Mechanisms of Manzamine A, Astaxanthin, and Asperlin in CVDs.
Moreover, there are several major causes of atherosclerosis. However, thermo-inflmation plays a crucial role in atherosclerosis pathogenesis via influencing the plague formation. Thrombo-inflammation refers to the complex cascading interaction between the blood coagulation process and inflammation in the pathogenesis of CVDs [98]. The formation of arterial thrombosis is mostly caused by platelet adhesion under high shear stress, which arises in stenotic atherosclerotic arteries [99]. Meanwhile, platelet-activating factor (PAF) is a powerful lipid mediator that acts through PAF/PAF-R pathways and is a key player in inflammation by recruiting neutrophils and activating platelets in the development of atherosclerosis [100].
Several marine-derived drugs have been investigated to inhibit thrombo-inflammation in CVDs. Fascaplysin is a Fijian marine sponge derived from the genus Fascaplysinopsis [101], which is a kinase inhibitor with anti-thrombotic properties via inhibiting GPIIb/IIIa activation, platelet aggregation, and thrombus formation [83]. Another cyclodepsipeptide marine compound Isaridin E derived from the Amphichorda feline (Beauveria feline) fungus [102], demonstrated the dose-dependent inhibition of platelet activation, aggregation, and secretion. However, it does not have any effect against thrombin- or collagen-induced platelet aggregation. Isaridin E also showed an antithrombotic effect without increasing bleeding time in a dose-dependent manner against the FeCl3-induced carotid mouse model [84]. F-fucoidan (FD) is a polysaccharide compound derived from the brown alga Laminaria japonica that also shows an antithrombotic effect through shortening the blood lysis time, H2O2 expression stimulation, and H2O2 released after induction of PGI2 production and might be effective in CVDs’ patients [103]. The anti-thrombotic and anti-atherosclerotic properties of marine-derived omega 3 polyunsaturated fatty acids (n-3 PUFA) may help to reduce heart failure by lowering the risk of ischemic heart disease. It is known that n-3 PUFA enhances plasminogen activator inhibitor-1 by lowering fibrinogen and decreasing platelet-derived thromboxane A2 (TXA2), which increases platelet aggregation and vasoconstriction [104]. Therefore, So, overall, it seems like marine-based drugs could be used to treat atherosclerosis, but a more detailed mechanistic study is still needed.
3.3. Myocardial Infarction (MI)
MI occurs due to the occlusion of the coronary artery, leads to a shortage in oxygen and nutrients, and causes irreversible necrosis and death of cardiomyocytes [105]. It is the major cause of death and disability among other CVDs worldwide [106]. Using marine-derived metal nanoparticles, a novel method for treating thrombus dissolution and myocyte healing in infarcted areas (myocardial infarction) [107]. The anti-myocardial infarction activity of the gold nanoparticles (GNPs) was an innovative method in which cyanobacterial extract, GNP solution, and a combination of both were developed [85]. Omega-3 polyunsaturated fatty acids (PUFA), a marine compound, have shown beneficial benefits on myocardial infarction by reducing MI size in experimental and clinical research (Figure 3) [104]. Docosahexaenoic acid (DHA) is a long-chain omega-3 PUFA obtained from the marine source that has shown a protective effect against myocardial infarction [87]. An in vivo study of DHA in a rat model showed a protective effect against MI at 5 g/kg [108]. There are few marine-derived compounds in MI that have been investigated until now. Thus, in addition, a more detailed mechanistic study is needed.
3.4. Ischemic Heart Disease (IHD)
IHD is an inadequate blood supply of the coronary artery to the myocardium. Endothelial dysfunction is the main involvement in the mechanism of IHD [109]. It is the main cause of morbidity and mortality among all CVDs globally [110]. A 2016 report states it is responsible for 9 million deaths worldwide [111]. Marine-derived drugs are better than synthetic drugs to treat IHD due to their affective action and better results [104]. Histochrome, a sodium salt of echinochrome A, is a marine drug found as a common sea urchin pigment. It is a powerful and biosafe cell-priming agent that prevents cardiac progenitor cells (CPCs) from cellular apoptosis via the downregulation of BCL2-associated X (Bax) cleaved caspase-3, and phosphorylated histone, whereas upregulation of Bcl-xL and B-cell lymphoma 2 (Bcl-2) proteins, utilizing patient-derived human CPCs in treating heart disease [112]. In vitro study of echinochrome A (Ech A), a naturally occurring pigment from sea urchins, showed marine anti-thrombotics, especially sulfated polysaccharides, are relevant due to their distinct modes of action and absence of bleeding. Their distinct modes of action as an antithrombotic are due to the high negative charge that sulfation imparts, which enables them to interact with proteins and molecules involved in vital biological processes such as coagulation [113]. In addition, both polysaccharides Enteromorpha prolifera polysaccharides (EPPs), produced from green algae, and fucoidan, extracted from brown algae, have anti-oxidant, lipid-lowering, and antiangiogenic properties [114]. Alginate (ALG), mostly derived from brown seaweed, can lower TC, TG, and LDL-C serum levels and upregulate HDL-C concentrations, making it an effective treatment for coronary artery disease [15].
3.5. Cardiac Stroke
Cardiac stroke is the most severe complication of CVDs, causing sudden death. CVDs are mostly caused by cardiac arrest or stroke in individuals with elevated blood pressure, high cholesterol, obesity, increased blood glucose levels, and weight gain [115]. Natural compounds derived from marine sources have already been regarded as lead molecules for treating CVDs and cardiac arrest due to their varied chemical compositions and pharmacological characteristics [116]. A carotenoid molecule called fucoxanthin, obtained from brown algae, prevents lipids’ oxidation and buildup [117]. Fucoxanthin protects against cardiac stroke by regulating metabolic syndrome [118]. Another carotenoid, astaxanthin, showed a positive effect in cardiac stroke via the modulating number of biological processes, including the reduction in inflammation, augmentation of oxidative stress, enhancement of antioxidants, and the modification of lipid and glucose concentrations via suppressing TLR4/NF-κB/ROS signaling pathway [119]. A new type of unique structure called Xyloketal B contains a marine component derived from Xylaria species. Xyloketal B can benefit cardiac stroke due to its protective effect in the two-clip stroke-prone hypertensive model [120].
3.6. Cardiac Arrhythmia
Cardiac arrhythmias account for 10%–15% of fatalities, making them a substantial reason for morbidity and mortality worldwide [121]. Tetrodotoxin (TTX) is a marine compound obtained from the actinomycetes of marine sediments and has a beneficial effect on cardiac arrhythmia. It is also known as the puffer fish toxin that prevents sodium channels in excitable neurons [122]. It has also shown an antiarrhythmic effect in combinatorial therapy with lidocaine [123].
Many toxins, including tetrodotoxin, saxitoxin, brevetoxins, antillatoxin, conotoxins, and cnidarians, are found in marine species such as pufferfish, shellfish, sea anemones, and cone snails, are voltage-gated sodium channels (VGSCs) blockers, and show protective effects against cardiac arrhythmia [124]. Other marine drugs, omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid, have shown antiarrhythmic effects against various arrhythmic disturbances, including atrial fibrillation and ventricular arrhythmia [125]. Eicosapentaenoic acid shows antiarrhythmic activity when added to the superfusate before adding the toxins, including ouabain, lysophosphatidylcholine, high Ca2+, acylcarnitine, β-adrenergic agonist, and the Ca2+ ionophore [90]. Botulinum toxin is obtained from the marine source Clostridium botulinum. Clostridium botulinum is a Gram-positive anaerobic spore-forming bacterium found in marine environments [126]. The botulinum toxin (BoNT/A1)–chitosan nanoparticles (BTN) formulation inhibits arrhythmia caused by sodium, calcium, and potassium channel activation [89].
3.7. Cardiac Dysfunction
Chronic cardiac dysfunction is caused by contractility overload on the heart myocardium. Different etiologies may favor existing compensatory mechanisms such as excentric (dilatation) and concentric hypertrophy. Chronic left ventricular dysfunction is the most prevalent complication of MI. Chronic cardiac dysfunction worsens left ventricular ejection fraction and stroke volume as dilatation progresses, eventually leading to heart failure [127]. Retinoid receptors play a crucial role in several diseases, including diabetes [128], cancer [129], and CVDs [130]. A research study reported that the retinoid receptor is essential for heart function. Moreover, tamoxifen-induced myocardial specific RARα deletion (RARαKO) mice showed significant diastolic dysfunction, increased intracellular ROS, NOX2 (NADPH oxidase 2), NOX4 and decreased antioxidant level (SOD1 and SOD2). This effect is reversed by overexpression of retinoid receptors [131]. In addition, Guleria RS et al. also demonstrated that retinoid receptors play a role in diabetic-induced cardiomyopathy [132]. In the same way, zeaxanthin heneicosylate (ZH) extracted from microalgae Dunaliella salina significantly reduced plasma biochemical alteration (AST, ALT, urea, and creatinine level), pro-inflammatory level (IL-6, NF-κB, and iNOS), antioxidant level (SOD), and histological changes in D-galactose-induced cardiac dysfunction rats through stimulating the retinoid receptors [92]. There are only a few studies on cardiac dysfunction; thus, detailed mechanistic studies are needed.
3.8. Heart Valve Disease or Valvular Heart Disease
Valvular heart disease (VHD) is a cluster of frequent cardiovascular disorders that account for 10–20% of all cardiac surgical operations in the United States. Heart valve problems include regurgitation (valve flaps do not close properly), stenosis (narrowed valve opening), and atresia (valve does not have a proper opening). Fucoxanthin is a marine carotenoid obtained from the seaweed microalgae Phaeodactylum tricornutum and possesses antioxidant and anti-inflammatory properties [133]. A report by Chiang et al. demonstrated the protective potential of heart valves in heart valve interstitial cells and dogs. Results showed that fucoxanthin treatment significantly reduced H2O2-induced ROS level, DNA damage, cell survival, and protein-related apoptosis and calcification expression via modulating the Akt/ERK pathway. In addition, long-term (0.5 to 2 years) supplementation to the dog also improved the left atrium to aortic (LA/AO) dimension ratio and E/e value (indicate mitral valve inflow, mitral valve leakage, and left ventricular diastolic dysfunction) [91]. This suggests that marine-derived compounds hold a diverse therapeutic potential. In addition, marine drugs which hold biological effects in CVDs tubulated in Table 3.

Table 3.
Marine drugs class, source, and their biological effects in CVDs.
4. Clinical Trial Studies of Marine-Derived Drugs in CVDs
Several marine-derived drugs, such as astaxanthin, alginate, eicosapentaenoic acid, etc., have been approved for clinical trial studies in various CVDs. These are effective when used with CVDs patients in clinical trial studies. However, more studies are required to collect data to prove that marine drugs provide a better therapy for CVDs. All the clinical studies on marine-derived drugs for CVDs are compiled in Table 4.

Table 4.
List of marine drugs under clinical trials.
5. Marine Lipid Bioactive Compounds with Potent Cardio-Protective Properties
Omega-3 polyunsaturated fatty acids (PUFA), carotenoids, lipid vitamins, and polar lipid bioactives from fish sources have been shown to have potent biological effects against inflammation and CVDs [157]. Fish is a good source of bio-functional marine polar lipids (PL), rich in n-3 PUFA, and have powerful antithrombotic, anti-inflammatory, and cardio-protective properties. The amphiphilic features of bioactive fish PL, such as several phospholipids and glycolipids bearing n-3 PUFA in their structure, resulted in a significant increase in the bioavailability of n-3 PUFA content [157]. It has been demonstrated that n-3 PUFA-rich fish lowers the incidence of inflammation-related CVDs. Additionally, it has anti-inflammatory and anti-thrombotic characteristics and transports n-3 PUFA to different bodily organs more effectively than triglycerides [158]. In addition to n-3 PUFA, other fish-lipid bioactive nutrients such as fish carotenoids, lipid vitamins A, D, and E, and polar fish lipids (glycolipids and phospholipids) have also shown anti-thrombotic, anti-inflammatory, and antioxidant, cardioprotective effects and reduced CVD risk [158,159]. Polar lipid fractions of sea bass (Dicentrarchus labrax) and gilthead sea bream (Sparus aurata) treated with fish feed enhanced with olive pomace showed powerful antithrombotic properties [160]. The cold-water marine fish cod (Gadus morhua) is a major source of fat-soluble vitamins, EPA and DHA, and high-quality protein. Cod is a lean fish that maintains its fat reserves in the liver as triacylglycerols. It has been reported to possess cardioprotective effects against atherosclerosis and platelet aggregation [161]. Sardines (Sardina pilchardus) are a significant Mediterranean commercial fish that reserves fats in the tissue as triacylglycerols. Sardines have shown a potent cardioprotective effect against platelet aggregation or PAF-induced platelet aggregation [162]. Microalgae are abundant sources of bioactive lipids, including polar lipids and omega-3 and -6 PUFA, which have strong anti-inflammatory properties in CVDs [163].
It has been shown that dietary polar lipids of marine origin can either directly inhibit PAF-binding on a particular cell membrane receptor for PAF or indirectly influence the phospholipid microenvironment in those membranes. These lipids could also prevent PAF production, bringing blood PAF levels to homeostatic levels, which has several anti-inflammatory and anti-atherogenic health effects for cardiovascular [159]. Spirulina-extracted lipid substances, including lipid extracts, phycocyanin protein, phycocyanobilin (PCB), polysaccharides (PS), and bioactive lipid fractions have shown strong cardioprotective effects such as antithrombotic and anti-PAF in washed rabbit platelets stimulated by PAF and thrombin [164]. Gilthead sea bream (Sparus aurata) polar lipids have shown an anti-atherosclerotic effect via modulation of PAF metabolism and decreasing activity and levels of PAF in the blood [165]. Phosphatidylcholine (PC) is the most predominant phospholipid (PL) found in marine sources such as mackerel, rainbow trout, tuna, and salmon, followed by phosphatidylethanolamine (PE). Krill (Euphausia superba) oil (KO), a prominent source of marine PLs, show a protective effect on heart failure by reducing heart remodeling [166]. KO increases the amount of n-3 PUFA in the myocardial tissue and reduces the risk of left ventricular (LV) remodeling when taken before myocardial infarction (MI) induction [167]. It also shows a cardioprotective effect by improving blood lipids in dyslipidemia [166]. Marine carotenoids are important bioactive substances with physiological effects connected to the protection of chronic illnesses such as CVDs. These chronic illnesses, including CVDs, have been caused by oxidative stress and inflammation [168]. The dietary supplement, astaxanthin, a xanthophyll carotenoid, is an effective anti-inflammatory and antioxidant in the CVD model. Astaxanthin has been used in human clinical research to evaluate its bioavailability, safety, and clinical features related to oxidative stress and inflammation in CVDs, and no negative consequences were found [118].
Vitamins A and E are abundant in shark liver oil and possess important bio-functionalities, cardio-protective, and antioxidant effects. Their antioxidant effects protect the body against free radicals [157]. Vitamin D and its derivatives, mainly paricalcitol, have shown powerful anti-thrombotic and anti-inflammatory effects against thrombotic PAF and inflammatory-related pathways [169]. Vitamin D insufficiency has been related to greater mortality and CVD incidence via several mechanisms, including the activation of the renin-angiotensin-aldosterone system, oxidative stress, altered inflammatory pathways, and aberrant nitric oxide regulation [170]. Vitamin E has anti-inflammatory, anti-thrombotic, and antioxidant properties. Its antioxidant properties lower the incidence of CVDs by preventing LDL oxidation [157]. Vitamin E or fish oil was proven to reduce atherosclerosis in rabbits with high cholesterol [82]. Fish oil and n-3 PUFA have been adversely linked to higher levels of LDL cholesterol as well as a possible increase in LDL oxidizability owing to unfavorable lipid changes, overcome by vitamin E co-supplementation, which promotes anti-atherogenic lipid modifications and overall cardiovascular protection, including elevated HDL(2)-cholesterol levels, lowered postprandial lipemia, decreased triacylglycerol-rich lipoprotein levels, and lowered remnant levels [171].
6. Potential Effect of Marine Drug Targeting ROS in CVDs
Reactive oxygen species (ROS) have been generated in terms of H2O2, hydroxyl radicals, and superoxide anions (O2−) during numerous cascades of cellular processes, including mitochondria respiration. It is also involved in various biological processes, including regulating cellular homeostasis and cell signaling [112]. Researchers have already even reported a significant positive correlation between increased ROS levels and the severity of CVDs [172]. ROS have been implicated in cellular damage, apoptosis, and necrosis, as well as the direct oxidizing effect on several macromolecules such as DNA, RNA, and proteins during CVDs pathogenesis [173]. Moreover, decreased in endothelial nitric oxide synthase leads to decreased in nitric oxide (NO) production, which consequences in an increase in ROS that has been linked to endothelial damage by its interaction with other molecules to produce peroxynitrite radical in hypertension [174]. In addition, patients with systemic arterial hypertension have shown higher ROS levels and reduced NO availability [73]. Several marine drugs, including astaxanthin, fucoidan, fucoxanthin, xyloketal B, histochrome, and spirulina maxima, show potential effects via targeting ROS in CVDs. The antioxidant activity of astaxanthin has been proven in in vivo and in vitro studies via scavenging superoxide, hydroxyl radicals, and hydrogen peroxide and protection from lipid peroxidation [134]. Astaxanthin has shown antioxidant activity through inhibition of ROS generation and is effective against CVDs. A study on rabbits confirmed that it decreased non-protein thiol levels and lipid peroxidation by increasing CAT, SOD, and thioredoxin activity and inhibited ROS generation in the aortic valve [175].
Fucoidan has shown an anti-atherosclerotic effect by triggering various signaling pathways that control lipid metabolism, inhibit inflammation, and reduce oxidative stress. An in vivo study revealed that fucoidan treatment shows a preventive effect against atherosclerosis through the reduction in ROS generation and the expression of ROS generation-related proteins such as endothelial nitric oxide synthase, superoxide dismutase 1, and NADPH oxidase subunit 2/4 in the aorta of LDLR-/-mice. Fucoidan also partially recovers the lipid peroxidation and antioxidant defense system in a mouse model of alimentary hyperlipidemia [176]. Fucoxanthin is another marine drug with a powerful antioxidant effect by inhibiting ROS generation in heart valve cells. In an in vivo study on rats, fucoxanthin has shown a protective effect against H2O2-induced ROS generation through decreasing oxidative stress, promoting better cell survival, and preventing DNA damage [91]. Xyloketal B has also shown potent antioxidant activity in atherosclerotic disease through scavenging DPPH free radicals and inhibiting ROS generation induced by oxidized low-density lipoprotein (LDL). It might preserve nitric oxide bioavailability in the existence of higher ROS. It has also shown antioxidant activity in the zebrafish model and vascular endothelial cells by heme oxygenase-1 (HO-1) induction [78]. Histochrome is a bio-safe and potent agent that shows a cardioprotective effect against ROS generation or oxidative stress in human cardiac progenitor cells [112]. In the clinical trial study, Spirulina maxima showed a cardioprotective effect against systemic arterial hypertension after decreasing oxidative stress and endothelial damage [73].
7. Future Prospectus
CVDs are the leading cause of death, affecting millions of people worldwide [177]. Various drugs have been approved to treat CVDs, including antithrombotic agents, beta-blockers, diuretics, calcium channel blockers, lipid-lowering drugs, and renin-angiotensin system (RAS)-acting agents [178]. Several other new synthetics and natural herbal drugs have been recently discovered to treat CVDs globally. However, CVDs are not completely cured or eradicated by these drugs, and cases are still increasing at a high rate globally. Researchers are continuously exploring novel targets and agents that can reduce the burden of CVDs. Marine-derived drugs are emerging therapeutics in the recent era [179,180]. Experiments and investigations have indicated several marine natural products that are effective for CVDs with minimum adverse effects. Marine drugs can be used in severe conditions for multiple complications such as hypertension, atherosclerosis, myocardial infarction, etc. These drugs may decrease the severe chest pain of anginal pectoris and some other CVDs complications. In the present review, we have emphasized different marine-derived compounds such as asperlin, saringosterol, astaxanthin, manzamine A, xyloketal B, docosahexaenoic acid, echinochrome A, tetrodotoxin, botulinum toxin, zeaxanthin heneicosylate, and fucoxanthin for various CVDs. All of these marine-derived compounds have shown very encouraging results in the in vitro and in vivo studies. Moreover, thousands of marine-derived compounds are added every year to the library of marine compounds. Those compounds need to be explored for their therapeutics in CVDs. A nano-formulation-based approach must also be developed to delivered marine-based compound and are the particular target of interest to avoid side effects. Researchers may directly utilize marine-derived compounds as initial leads for the development of new medications that are more specialized than the original molecule. Based on this, it appears that marine natural products could represent a promising “library” of natural compounds for developing new therapies as adjuvants to gold standard therapies, enhancing the efficacy of conventional drugs, and exerting synergistic or additive positive effects for cardiovascular diseases.
8. Conclusions
Several synthetic drugs are those most often used today in pharmaceutical corporations. Pharmaceutical corporations have given up on bioactive chemical research for many years in favor of developing and manufacturing synthetic molecules. However, research into natural substances has resumed since the early 2000s and has a place within biomedical investigations. The superior biocompatibility of natural chemicals compared to manufactured pharmaceutical products, without discounting the significant variety of these molecules and their effects, are one of the primary drivers for this return to natural medicines. Marine chemicals and their derivatives have grown in pharmaceutical and medical research during the last 10 years. Unquestionably, one of the reasons is the abundance of available molecules and secondary metabolites, as well as their diversity due to the many unfavorable habitats of the seas and the virtually endless variety of creatures that inhabit them. Antioxidant and anti-inflammatory characteristics, particularly useful for treating cardiovascular disorders, are among the many pharmacological activities on which the research is focused. This review has discussed the therapeutic potential of these marine-derived compounds for CVDs with underlying mechanisms.
Author Contributions
Conceptualization, W.A. and S.A. (Sakeel Ahmed); Methodology, W.A. and S.A. (Sakeel Ahmed); Software, W.A. and S.A. (Sakeel Ahmed); Data curation, W.A., S.A. (Sakeel Ahmed); Manuscript writing, M.R., Writing—original draft, W.A., S.A. (Sakeel Ahmed), and M.R., Writing—review and editing, M.R., R.V., S.A. (Swamita Arora), and W.A.; Figure drawing, M.R.; Visualization, R.V., S.A. (Sameer Ahmad) and W.A.; Investigation, R.V., W.A. and S.A. (Sakeel Ahmed); Supervision, Rahul Vashishth, W.A. and S.A. (Sameer Ahmad). All authors have read and agreed to the published version of the manuscript.
Funding
This review work received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Xiang, Z.; Han, M.; Zhang, H. Nanomaterials Based Flexible Devices for Monitoring and Treatment of Cardiovascular Diseases (CVDs). Nano Res. 2022, 89, 248. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Abd, M.; Mohammed, E.; Badawy, D.; Naing, L.; Johar, S.; Ong, S.; Rahman, H.A.; Lin, C.; Raja, C.; Pengiran, I.; et al. Scoping Review: Are CVDs Risk Calculators Using the Digital Platform Benecial for CVDs Prevention and Management? Res. Sq. 2022. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Fuster, V. The Global Burden of Cardiovascular Diseases and Risks: A Compass for Global Action. J. Am. Coll. Cardiol. 2020, 76, 2980–2981. [Google Scholar] [CrossRef]
- Woodward, M. Cardiovascular Disease and the Female Disadvantage. Int. J. Environ. Res. Public Health 2019, 16, 1165. [Google Scholar] [CrossRef]
- Vogel, B.; Acevedo, M.; Appelman, Y.; Bairey Merz, C.N.; Chieffo, A.; Figtree, G.A.; Guerrero, M.; Kunadian, V.; Lam, C.S.P.; Maas, A.H.E.M.; et al. The Lancet Women and Cardiovascular Disease Commission: Reducing the Global Burden by 2030. Lancet 2021, 397, 2385–2438. [Google Scholar] [CrossRef]
- Fuchs, F.D.; Whelton, P.K. High Blood Pressure and Cardiovascular Disease. Hypertension 2020, 75, 285–292. [Google Scholar] [CrossRef]
- Dabravolski, S.A.; Sukhorukov, V.N.; Kalmykov, V.A.; Orekhov, N.A.; Grechko, A.V.; Orekhov, A.N. Heat Shock Protein 90 as Therapeutic Target for CVDs and Heart Ageing. Int. J. Mol. Sci. 2022, 23, 649. [Google Scholar] [CrossRef]
- Valipour, M.; Irannejad, H.; Emami, S. Papaverine, a Promising Therapeutic Agent for the Treatment of COVID-19 Patients with Underlying Cardiovascular Diseases (CVDs). Drug Dev. Res. 2022, 83, 1246–1250. [Google Scholar] [CrossRef]
- Ho, C.K.; Kleeff, J.; Friess, H.; Büchler, M.W. Complications of Pancreatic Surgery. HPB 2005, 7, 99–108. [Google Scholar] [CrossRef]
- Jankowski, J.; Floege, J.; Fliser, D.; Böhm, M.; Marx, N. Cardiovascular Disease in Chronic Kidney Disease Pathophysiological Insights and Therapeutic Options. Circulation 2021, 143, 1157–1172. [Google Scholar] [CrossRef]
- Festa, M.; Sansone, C.; Brunet, C.; Crocetta, F.; Di Paola, L.; Lombardo, M.; Bruno, A.; Noonan, D.M.; Albini, A. Cardiovascular Active Peptides of Marine Origin with ACE Inhibitory Activities: Potential Role as Anti-Hypertensive Drugs and in Prevention of SARSCoV-2 Infection. Int. J. Mol. Sci. 2020, 21, 8364. [Google Scholar] [CrossRef]
- Ferraz, C.A.A.; Grougnet, R.; Nicolau, E.; Picot, L.; de Oliveira Junior, R.G. Carotenoids from Marine Microalgae as Antimelanoma Agents. Mar. Drugs 2022, 20, 618. [Google Scholar] [CrossRef]
- Zhou, J.-B.; Luo, R.; Zheng, Y.-L.; Pang, J.-Y. Recent Advances in the Discovery and Development of Marine Natural Products with Cardiovascular Pharmacological Effects. Mini-Rev. Med. Chem. 2017, 18, 527–550. [Google Scholar] [CrossRef]
- Liang, B.; Cai, X.-Y.; Gu, N. Marine Natural Products and Coronary Artery Disease. Front. Cardiovasc. Med. 2021, 8, 739932. [Google Scholar] [CrossRef]
- Newman, D.J.; Cragg, G.M. Natural Products as Sources of New Drugs from 1981 to 2014. J. Nat. Prod. 2016, 79, 629–661. [Google Scholar] [CrossRef]
- Jiménez, C. Marine Natural Products in Medicinal Chemistry. ACS Med. Chem. Lett. 2018, 9, 959–961. [Google Scholar] [CrossRef]
- Raven, P.H.; Margulis, L.; Schwartz, K.V. Five Kingdoms: An Illustrated Guide to the Phyla of Life on Earth. Bryologist 1988, 91, 382. [Google Scholar] [CrossRef]
- Donia, M.; Hamann, M.T. Marine Natural Products and Their Potential Applications as Anti-Infective Agents. Lancet Infect. Dis. 2003, 3, 338–348. [Google Scholar] [CrossRef]
- Malve, H. Exploring the Ocean for New Drug Developments: Marine Pharmacology. J. Pharm. Bioallied Sci. 2016, 8, 83–91. [Google Scholar] [CrossRef]
- Khalifa, S.A.M.; Elias, N.; Farag, M.A.; Chen, L.; Saeed, A.; Hegazy, M.E.F.; Moustafa, M.S.; El-Wahed, A.A.; Al-Mousawi, S.M.; Musharraf, S.G.; et al. Marine Natural Products: A Source of Novel Anticancer Drugs. Mar. Drugs 2019, 17, 491. [Google Scholar] [CrossRef]
- Catanesi, M.; Caioni, G.; Castelli, V.; Benedetti, E.; D’angelo, M.; Cimini, A. Benefits under the Sea: The Role of Marine Compounds in Neurodegenerative Disorders. Mar. Drugs 2021, 19, 24. [Google Scholar] [CrossRef] [PubMed]
- Voultsiadou Eleni, E. Therapeutic Properties and Uses of Marine Invertebrates in the Ancient Greek World and Early Byzantium. J. Ethnopharmacol. 2010, 130, 237–247. [Google Scholar] [CrossRef]
- Fu, X.M.; Zhang, M.Q.; Shao, C.L.; Li, G.Q.; Bai, H.; Dai, G.L.; Chen, Q.W.; Kong, W.; Fu, X.J.; Wang, C.Y. Chinese Marine Materia Medica Resources: Status and Potential. Mar. Drugs 2016, 14, 46. [Google Scholar] [CrossRef]
- Pohnert, G. Chemical Defense Strategies of Marine Organisms. In The Chemistry of Pheromones and Other Semiochemicals I; Schulz, S., Ed.; Springer: Berlin/Heidelberg, Germany, 2004; pp. 179–219. ISBN 978-3-540-39868-4. [Google Scholar]
- Ahmed, I.; Asgher, M.; Sher, F.; Hussain, S.M.; Nazish, N.; Joshi, N.; Sharma, A.; Parra-Saldívar, R.; Bilal, M.; Iqbal, H.M.N. Exploring Marine as a Rich Source of Bioactive Peptides: Challenges and Opportunities from Marine Pharmacology. Mar. Drugs 2022, 20, 208. [Google Scholar] [CrossRef] [PubMed]
- Nigam, M.; Suleria, H.A.R.; Farzaei, M.H.; Mishra, A.P. Marine Anticancer Drugs and Their Relevant Targets: A Treasure from the Ocean. DARU, J. Pharm. Sci. 2019, 27, 491–515. [Google Scholar] [CrossRef] [PubMed]
- Liming, J.; Chunshan, Q.; Xiyan, H.; Shengdi, F. Potential Pharmacological Resources: Natural Bioactive Compounds from Marine-Derived Fungi. Mar. Drugs 2016, 14, 76. [Google Scholar] [CrossRef]
- Wibowo, J.T.; Ahmadi, P.; Rahmawati, S.I.; Bayu, A.; Putra, M.Y.; Kijjoa, A. Marine-Derived Indole Alkaloids and Their Biological and Pharmacological Activities. Mar. Drugs 2022, 20, 3. [Google Scholar] [CrossRef]
- Kwon, O.S.; Ahn, S.; Jeon, J.E.; Park, I.G.; Won, T.H.; Sim, C.J.; Park, H.G.; Oh, D.C.; Oh, K.B.; Noh, M.; et al. Psammocindoles A-C: Isolation, Synthesis, and Bioactivity of Indole-γ-Lactams from the Sponge Psammocinia Vermis. Org. Lett. 2021, 23, 4667–4671. [Google Scholar] [CrossRef] [PubMed]
- Kleks, G.; Holland, D.C.; Kennedy, E.K.; Avery, V.M.; Carroll, A.R. Antiplasmodial Alkaloids from the Australian Bryozoan Amathia Lamourouxi. J. Nat. Prod. 2020, 83, 3435–3444. [Google Scholar] [CrossRef]
- Li, M.C.; Sun, W.S.; Cheng, W.; Liu, D.; Liang, H.; Zhang, Q.Y.; Lin, W.H. Four New Minor Brominated Indole Related Alkaloids with Antibacterial Activities from Laurencia Similis. Bioorganic Med. Chem. Lett. 2016, 26, 3590–3593. [Google Scholar] [CrossRef]
- Yang, J.; Gong, L.; Guo, M.; Jiang, Y.; Ding, Y.; Wang, Z.; Xin, X.; An, F. Bioactive Indole Diketopiperazine Alkaloids from the Marine Endophytic Fungus Aspergillus sp. YJ191021. Mar. Drugs 2021, 19, 157. [Google Scholar] [CrossRef]
- Song, Y.; Yang, J.; Yu, J.; Li, J.; Yuan, J.; Wong, N.K.; Ju, J. Chlorinated Bis-Indole Alkaloids from Deep-Sea Derived Streptomyces sp. SCSIO 11791 with Antibacterial and Cytotoxic Activities. J. Antibiot. (Tokyo) 2020, 73, 542–547. [Google Scholar] [CrossRef]
- Wright, A.E.; Killday, K.B.; Chakrabarti, D.; Guzmán, E.A.; Harmody, D.; McCarthy, P.J.; Pitts, T.; Pomponi, S.A.; Reed, J.K.; Roberts, B.F.; et al. Dragmacidin G, a Bioactive Bis-Indole Alkaloid from a Deep-Water Sponge of the Genus Spongosorites. Mar. Drugs 2017, 15, 16. [Google Scholar] [CrossRef]
- Chen, G.; Seukep, A.J.; Guo, M. Recent Advances in Molecular Docking for the Research and Discovery of Potential Marine Drugs. Mar. Drugs 2020, 18, 545. [Google Scholar] [CrossRef]
- Guo, Y.W.; Liu, X.J.; Yuan, J.; Li, H.J.; Mahmud, T.; Hong, M.J.; Yu, J.C.; Lan, W.J. L-Tryptophan Induces a Marine-Derived Fusarium sp. to Produce Indole Alkaloids with Activity against the Zika Virus. J. Nat. Prod. 2020, 83, 3372–3380. [Google Scholar] [CrossRef]
- Zhou, G.; Sun, C.; Hou, X.; Che, Q.; Zhang, G.; Gu, Q.; Liu, C.; Zhu, T.; Li, D. Ascandinines A-D, Indole Diterpenoids, from the Sponge-Derived Fungus Aspergillus candidus HDN15-152. J. Org. Chem. 2021, 86, 2431–2436. [Google Scholar] [CrossRef]
- Li, J.; Hu, Y.; Hao, X.; Tan, J.; Li, F.; Qiao, X.; Chen, S.; Xiao, C.; Chen, M.; Peng, Z.; et al. Raistrickindole A, an Anti-HCV Oxazinoindole Alkaloid from Penicillium Raistrickii IMB17-034. J. Nat. Prod. 2019, 82, 1391–1395. [Google Scholar] [CrossRef]
- Huang, L.H.; Xu, M.Y.; Li, H.J.; Li, J.Q.; Chen, Y.X.; Ma, W.Z.; Li, Y.P.; Xu, J.; Yang, D.P.; Lan, W.J. Amino Acid-Directed Strategy for Inducing the Marine-Derived Fungus Scedosporium Apiospermum F41-1 to Maximize Alkaloid Diversity. Org. Lett. 2017, 19, 4888–4891. [Google Scholar] [CrossRef]
- Liu, H.B.; Lauro, G.; O’Connor, R.D.; Lohith, K.; Kelly, M.; Colin, P.; Bifulco, G.; Bewley, C.A. Tulongicin, an Antibacterial Tri-Indole Alkaloid from a Deep-Water Topsentia sp. Sponge. J. Nat. Prod. 2017, 80, 2556–2560. [Google Scholar] [CrossRef]
- Limbadri, S.; Luo, X.; Lin, X.; Liao, S.; Wang, J.; Zhou, X.; Yang, B.; Liu, Y. Bioactive Novel Indole Alkaloids and Steroids from Deep Sea-Derived Fungus Aspergillus fumigatus SCSIO 41012. Molecules 2018, 23, 2379. [Google Scholar] [CrossRef]
- Huang, S.; Chen, H.; Li, W.; Zhu, X.; Ding, W.; Li, C. Bioactive Chaetoglobosins from the Mangrove Endophytic Fungus Penicillium Chrysogenum. Mar. Drugs 2016, 14, 172. [Google Scholar] [CrossRef]
- Zhu, X.; Zhou, D.; Liang, F.; Wu, Z.; She, Z.; Li, C. Penochalasin K, a New Unusual Chaetoglobosin from the Mangrove Endophytic Fungus Penicillium Chrysogenum V11 and Its Effective Semi-Synthesis. Fitoterapia 2017, 123, 23–28. [Google Scholar] [CrossRef]
- Anjum, K.; Kaleem, S.; Yi, W.; Zheng, G.; Lian, X.; Zhang, Z. Novel Antimicrobial Indolepyrazines A and B from the Marine-Associated Acinetobacter sp. ZZ1275. Mar. Drugs 2019, 17, 89. [Google Scholar] [CrossRef]
- May Zin, W.W.; Buttachon, S.; Dethoup, T.; Pereira, J.A.; Gales, L.; Inácio, Â.; Costa, P.M.; Lee, M.; Sekeroglu, N.; Silva, A.M.S.; et al. Antibacterial and Antibiofilm Activities of the Metabolites Isolated from the Culture of the Mangrove-Derived Endophytic Fungus Eurotium Chevalieri KUFA 0006. Phytochemistry 2017, 141, 86–97. [Google Scholar] [CrossRef]
- Li, H.; Sun, W.; Deng, M.; Zhou, Q.; Wang, J.; Liu, J.; Chen, C.; Qi, C.; Luo, Z.; Xue, Y.; et al. Asperversiamides, Linearly Fused Prenylated Indole Alkaloids from the Marine-Derived Fungus Aspergillus versicolor. J. Org. Chem. 2018, 83, 8483–8492. [Google Scholar] [CrossRef]
- Park, J.S.; Cho, E.; Hwang, J.Y.; Park, S.C.; Chung, B.; Kwon, O.S.; Sim, C.J.; Oh, D.C.; Oh, K.B.; Shin, J. Bioactive Bis(Indole) Alkaloids from a Spongosorites sp. Sponge. Mar. Drugs 2021, 19, 3. [Google Scholar] [CrossRef]
- Di, X.; Wang, S.; Oskarsson, J.T.; Rouger, C.; Tasdemir, D.; Hardardottir, I.; Freysdottir, J.; Wang, X.; Molinski, T.F.; Omarsdottir, S. Bromotryptamine and Imidazole Alkaloids with Anti-Inflammatory Activity from the Bryozoan Flustra Foliacea. J. Nat. Prod. 2020, 83, 2854–2866. [Google Scholar] [CrossRef]
- El-Hawary, S.S.; Sayed, A.M.; Mohammed, R.; Hassan, H.M.; Rateb, M.E.; Amin, E.; Mohammed, T.A.; El-Mesery, M.; Muhsinah, A.B.; Alsayari, A.; et al. Bioactive Brominated Oxindole Alkaloids from the Red Sea Sponge Callyspongia Siphonella. Mar. Drugs 2019, 17, 465. [Google Scholar] [CrossRef]
- Zhao, L.Y.; Li, J.; Huang, X.Q.; Wang, G.H.; Lv, X.F.; Meng, W.F.; Chen, W.L.; Pang, J.Y.; Lin, Y.C.; Sun, H.S.; et al. Xyloketal B Exerts Antihypertensive Effect in Renovascular Hypertensive Rats via the NO-SGC-CGMP Pathway and Calcium Signaling. Acta Pharmacol. Sin. 2018, 39, 875–884. [Google Scholar] [CrossRef]
- Marchioli, R. Uses and Benefits of Omega-3 Ethyl Esters in Patients with Cardiovascular Disease. J. Multidiscip. Healthc. 2010, 3, 79. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.D.; Zhang, S.L.; Zhou, S.Q.; Ma, Q.Y.; Xie, Q.Y.; Chen, J.P.; Li, J.H.; Zhou, L.M.; Yuan, J.Z.; Hu, Z.; et al. Quinazoline-Containing Indole Alkaloids from the Marine-Derived Fungus Aspergillus sp. HNMF114. J. Nat. Prod. 2019, 82, 3456–3463. [Google Scholar] [CrossRef]
- Li, P.; Zhang, M.; Li, H.; Wang, R.; Hou, H.; Li, X.; Liu, K.; Chen, H. New Prenylated Indole Homodimeric and Pteridine Alkaloids from the Marine-Derived Fungus Aspergillus austroafricanus Y32-2. Mar. Drugs 2021, 19, 98. [Google Scholar] [CrossRef] [PubMed]
- Ivanets, E.V.; Yurchenko, A.N.; Smetanina, O.F.; Rasin, A.B.; Zhuravleva, O.I.; Pivkin, M.V.; Popov, R.S.; Von Amsberg, G.; Afiyatullov, S.S.; Dyshlovoy, S.A. Asperindoles A–D and a p-Terphenyl Derivative from the Ascidian-Derived Fungus Aspergillus sp. KMM 4676. Mar. Drugs 2018, 16, 232. [Google Scholar] [CrossRef] [PubMed]
- Buttachon, S.; Ramos, A.A.; Inácio, Â.; Dethoup, T.; Gales, L.; Lee, M.; Costa, P.M.; Silva, A.M.S.; Sekeroglu, N.; Rocha, E.; et al. Bis-Indolyl Benzenoids, Hydroxypyrrolidine Derivatives and Other Constituents from Cultures of the Marine Sponge-Associated Fungus Aspergillus candidus KUFA0062. Mar. Drugs 2018, 16, 119. [Google Scholar] [CrossRef]
- Cruz, P.G.; Martínez Leal, J.F.; Daranas, A.H.; Pérez, M.; Cuevas, C. On the Mechanism of Action of Dragmacidins i and J, Two New Representatives of a New Class of Protein Phosphatase 1 and 2A Inhibitors. ACS Omega 2018, 3, 3760–3767. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.D.; Fan, P.; Zhou, L.M.; Ma, Q.Y.; Xie, Q.Y.; Zheng, H.Z.; Zheng, Z.H.; Zhang, R.S.; Yuan, J.Z.; Dai, H.F.; et al. Penerpenes A-D, Four Indole Terpenoids with Potent Protein Tyrosine Phosphatase Inhibitory Activity from the Marine-Derived Fungus Penicillium sp. KFD28. Org. Lett. 2019, 21, 4864–4867. [Google Scholar] [CrossRef]
- Zhou, L.M.; Kong, F.D.; Fan, P.; Ma, Q.Y.; Xie, Q.Y.; Li, J.H.; Zheng, H.Z.; Zheng, Z.H.; Yuan, J.Z.; Dai, H.F.; et al. Indole-Diterpenoids with Protein Tyrosine Phosphatase Inhibitory Activities from the Marine-Derived Fungus Penicillium sp. KFD28. J. Nat. Prod. 2019, 82, 2638–2644. [Google Scholar] [CrossRef]
- Cho, K.H.; Sohn, J.H.; Oh, H. Isolation and Structure Determination of a New Diketopiperazine Dimer from Marine-Derived Fungus Aspergillus sp. SF-5280. Nat. Prod. Res. 2018, 32, 214–221. [Google Scholar] [CrossRef]
- Guzii, A.G.; Makarieva, T.N.; Denisenko, V.A.; Gerasimenko, A.V.; Udovenko, A.A.; Popov, R.S.; Dmitrenok, P.S.; Golotin, V.A.; Fedorov, S.N.; Grebnev, B.B.; et al. Guitarrins A–E and Aluminumguitarrin A: 5-Azaindoles from the Northwestern Pacific Marine Sponge Guitarra Fimbriata. J. Nat. Prod. 2019, 82, 1704–1709. [Google Scholar] [CrossRef]
- Zhou, B.; Perel, P.; Mensah, G.A.; Ezzati, M. Global Epidemiology, Health Burden and Effective Interventions for Elevated Blood Pressure and Hypertension. Nat. Rev. Cardiol. 2021, 18, 785–802. [Google Scholar] [CrossRef]
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide Trends in Hypertension Prevalence and Progress in Treatment and Control from 1990 to 2019: A Pooled Analysis of 1201 Population-Representative Studies with 104 Million Participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef] [PubMed]
- Erdmann, K.; Cheung, B.W.Y.; Schröder, H. The Possible Roles of Food-Derived Bioactive Peptides in Reducing the Risk of Cardiovascular Disease. J. Nutr. Biochem. 2008, 19, 643–654. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, K.; Chiba, H.; Yoshikawa, M. Peptide Inhibitors for Angiotensin I-Converting Enzyme from Thermolysin Digest of Dried Bonito. Biosci. Biotechnol. Biochem. 1992, 56, 1541–1545. [Google Scholar] [CrossRef]
- Wijesekara, I.; Kim, S.K. Angiotensin-I-Converting Enzyme (ACE) Inhibitors from Marine Resources: Prospects in the Pharmaceutical Industry. Mar. Drugs 2010, 8, 1080–1093. [Google Scholar] [CrossRef] [PubMed]
- Abachi, S.; Bazinet, L.; Beaulieu, L. Antihypertensive and Angiotensin-i-Converting Enzyme (ACE)-Inhibitory Peptides from Fish as Potential Cardioprotective Compounds. Mar. Drugs 2019, 17, 613. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.; Liu, Y.; Wang, J.; Wu, S.; Geng, L.; Sui, Z.; Zhang, Q. Antihypertensive Effects of Two Novel Angiotensin I-Converting Enzyme (Ace) Inhibitory Peptides from Gracilariopsis Lemaneiformis (Rhodophyta) in Spontaneously Hypertensive Rats (SHRs). Mar. Drugs 2018, 16, 299. [Google Scholar] [CrossRef]
- Sato, M.; Hosokawa, T.; Yamaguchi, T.; Nakano, T.; Muramoto, K.; Kahara, T.; Funayama, K.; Kobayashi, A.; Nakano, T. Angiotensin I-Converting Enzyme Inhibitory Peptides Derived from Wakame (Undaria Pinnatifida) and Their Antihypertensive Effect in Spontaneously Hypertensive Rats. J. Agric. Food Chem. 2002, 50, 6245–6252. [Google Scholar] [CrossRef]
- Sun, S.; Xu, X.; Sun, X.; Zhang, X.; Chen, X.; Xu, N. Preparation and Identification of ACE Inhibitory Peptides from the Marine Macroalga Ulva Intestinalis. Mar. Drugs 2019, 17, 179. [Google Scholar] [CrossRef]
- Hu, Y.; Feng, Z.; Feng, W.; Hu, T.; Guan, H.; Mao, Y. AOS Ameliorates Monocrotaline-Induced Pulmonary Hypertension by Restraining the Activation of P-Selectin/P38MAPK/NF-ΚB Pathway in Rats. Biomed. Pharmacother. 2019, 109, 1319–1326. [Google Scholar] [CrossRef]
- Shen, T.; Xing, G.; Zhu, J.; Zhang, S.; Cai, Y.; Li, D.; Xu, G.; Xing, E.; Rao, J.; Shi, R. Effects of 12-Week Supplementation of Marine Omega-3 PUFA-Based Formulation Omega3Q10 in Older Adults with Prehypertension and/or Elevated Blood Cholesterol. Lipids Health Dis. 2017, 16, 253. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Sámano, J.; De Oca, A.T.M.; O.-Bocardo, O.I.L.; Torres-Durán, P.V.; Juárez-Oropeza, M.A. Spirulina Maxima Decreases Endothelial Damage and Oxidative Stress Indicators in Patients with Systemic Arterial Hypertension: Results from Exploratory Controlled Clinical Trial. Mar. Drugs 2018, 16, 496. [Google Scholar] [CrossRef] [PubMed]
- Nuhu, A.A. Spirulina (Arthrospira): An Important Source of Nutritional and Medicinal Compounds. J. Mar. Biol. 2013, 2013, 325636. [Google Scholar] [CrossRef]
- Chen, Y.Y.; Ji, W.; Du, J.R.; Yu, D.K.; He, Y.; Yu, C.X.; Li, D.S.; Zhao, C.-Y.; Qiao, K. yun Preventive Effects of Low Molecular Mass Potassium Alginate Extracted from Brown Algae on DOCA Salt-Induced Hypertension in Rats. Biomed. Pharmacother. 2010, 64, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Cho, C.H.; Lu, Y.A.; Kim, M.Y.; Jeon, Y.J.; Lee, S.H. Therapeutic Potential of Seaweed–Derived Bioactive Compounds for Cardiovascular Disease Treatment. Appl. Sci. 2022, 12, 1025. [Google Scholar] [CrossRef]
- Zhou, Y.; Chen, R.; Liu, D.; Wu, C.; Guo, P.; Lin, W. Asperlin Inhibits LPS-Evoked Foam Cell Formation and Prevents Atherosclerosis in ApoE−/− Mice. Mar. Drugs 2017, 15, 358. [Google Scholar] [CrossRef]
- Zhao, L.Y.; Li, J.; Yuan, F.; Li, M.; Zhang, Q.; Huang, Y.Y.; Pang, J.Y.; Zhang, B.; Sun, F.Y.; Sun, H.S.; et al. Xyloketal B Attenuates Atherosclerotic Plaque Formation and Endothelial Dysfunction in Apolipoprotein E Deficient Mice. Mar. Drugs 2015, 13, 2306–2326. [Google Scholar] [CrossRef]
- Yan, Y.; Niu, Z.; Wang, B.; Zhao, S.; Sun, C.; Wu, Y.; Li, Y.; Ying, H.; Liu, H. Saringosterol from Sargassum Fusiforme Modulates Cholesterol Metabolism and Alleviates Atherosclerosis in ApoE-Deficient Mice. Mar. Drugs 2021, 19, 485. [Google Scholar] [CrossRef]
- Eguchi, K.; Fujiwara, Y.; Hayashida, A.; Horlad, H.; Kato, H.; Rotinsulu, H.; Losung, F.; Mangindaan, R.E.P.; De Voogd, N.J.; Takeya, M.; et al. Manzamine A, a Marine-Derived Alkaloid, Inhibits Accumulation of Cholesterol Ester in Macrophages and Suppresses Hyperlipidemia and Atherosclerosis In Vivo. Bioorganic Med. Chem. 2013, 21, 3831–3838. [Google Scholar] [CrossRef]
- Yang, Y.; Seo, J.M.; Nguyen, A.; Pham, T.X.; Park, H.J.; Park, Y.; Kim, B.; Bruno, R.S.; Lee, J. Astaxanthin-Rich Extract from the Green Alga Haematococcus Pluvialis Lowers Plasma Lipid Concentrations and Enhances Antioxidant Defense in Apolipoprotein E Knockout Mice. J. Nutr. 2011, 141, 1611–1617. [Google Scholar] [CrossRef]
- Chen, M.F.; Hsu, H.C.; Liau, C.S.; Lee, Y.T. The Role of Vitamin E on the Anti-Atherosclerotic Effect of Fish Oil in Diet-Induced Hypercholesterolemic Rabbits. Prostaglandins Other Lipid Mediat. 1999, 57, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Ampofo, E.; Später, T.; Müller, I.; Eichler, H.; Menger, M.D.; Laschke, M.W. The Marine-Derived Kinase Inhibitor Fascaplysin Exerts Anti-Thrombotic Activity. Mar. Drugs 2015, 13, 6774–6791. [Google Scholar] [CrossRef] [PubMed]
- Pan, N.; Li, Z.C.; Li, Z.H.; Chen, S.H.; Jiang, M.H.; Yang, H.Y.; Liu, Y.S.; Hu, R.; Zeng, Y.W.; Dai, L.H.; et al. Antiplatelet and Antithrombotic Effects of Isaridin E Isolated from the Marine-Derived Fungus via Downregulating the PI3K/Akt Signaling Pathway. Mar. Drugs 2022, 20, 23. [Google Scholar] [CrossRef] [PubMed]
- Bakir, E.M.; Younis, N.S.; Mohamed, M.E.; El Semary, N.A. Cyanobacteria as Nanogold Factories: Chemical and Anti-Myocardial Infarction Properties of Gold Nanoparticles Synthesized by Lyngbya Majuscula. Mar. Drugs 2018, 16, 217. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.F.; Sigg, D.C.; Ujhelyi, M.R.; Wilhelm, J.J.; Richardson, E.S.; Iaizzo, P.A. Pericardial Delivery of Omega-3 Fatty Acid: A Novel Approach to Reducing Myocardial Infarct Sizes and Arrhythmias. Am. J. Physiol. Heart Circ. Physiol. 2008, 294, 2212–2218. [Google Scholar] [CrossRef] [PubMed]
- Desnoyers, M.; Gilbert, K.; Rousseau, G. Cardioprotective Effects of Omega-3 Polyunsaturated Fatty Acids: Dichotomy between Experimental and Clinical Studies. Mar. Drugs 2018, 16, 234. [Google Scholar] [CrossRef]
- Pan, N.; Lu, L.Y.; Li, M.; Wang, G.H.; Sun, F.Y.; Sun, H.S.; Wen, X.J.; Cheng, J.D.; Chen, J.W.; Pang, J.Y.; et al. Xyloketal B Alleviates Cerebral Infarction and Neurologic Deficits in a Mouse Stroke Model by Suppressing the ROS/TLR4/NF-ΰ B Inflammatory Signaling Pathway. Acta Pharmacol. Sin. 2017, 38, 1236–1247. [Google Scholar] [CrossRef]
- Sergeevichev, D.; Fomenko, V.; Strelnikov, A.; Dokuchaeva, A.; Vasilieva, M.; Chepeleva, E.; Rusakova, Y.; Artemenko, S.; Romanov, A.; Salakhutdinov, N.; et al. Botulinum Toxin-Chitosan Nanoparticles Prevent Arrhythmia in Experimental Rat Models. Mar. Drugs 2020, 18, 410. [Google Scholar] [CrossRef]
- Kang, J.X.; Leaf, A. Prevention of Fatal Cardiac Arrhythmias by Polyunsaturated Fatty Acids. Am. J. Clin. Nutr. 2000, 71, 202S–207S. [Google Scholar] [CrossRef]
- Chiang, Y.F.; Tsai, C.H.; Chen, H.Y.; Wang, K.L.; Chang, H.Y.; Huang, Y.J.; Hong, Y.H.; Ali, M.; Shieh, T.M.; Huang, T.C.; et al. Protective Effects of Fucoxanthin on Hydrogen Peroxide-Induced Calcification of Heart Valve Interstitial Cells. Mar. Drugs 2021, 19, 307. [Google Scholar] [CrossRef]
- El-Baz, F.K.; Hussein, R.A.; Saleh, D.O.; Jaleel, G.A.R.A. Zeaxanthin Isolated from Dunaliella Salina Microalgae Ameliorates Age Associated Cardiac Dysfunction in Rats through Stimulation of Retinoid Receptors. Mar. Drugs 2019, 17, 290. [Google Scholar] [CrossRef] [PubMed]
- Soehnlein, O.; Libby, P. Targeting Inflammation in Atherosclerosis–from Experimental Insights to the Clinic. Nat. Rev. Drug Discov. 2021, 20, 589–610. [Google Scholar] [CrossRef] [PubMed]
- Patil, N.P.; Le, V.; Sligar, A.D.; Mei, L.; Chavarria, D.; Yang, E.Y.; Baker, A.B. Algal Polysaccharides as Therapeutic Agents for Atherosclerosis. Front. Cardiovasc. Med. 2018, 5, 153. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Liu, J.; Fu, Z.; Ye, C.; Zhang, R.; Song, Y.; Zhang, Y.; Li, H.; Ying, H.; Liu, H. 24(S)-Saringosterol from Edible Marine Seaweed Sargassum Fusiforme Is a Novel Selective LXRβ Agonist. J. Agric. Food Chem. 2014, 62, 6130–6137. [Google Scholar] [CrossRef]
- Munekata, P.E.S.; Pateiro, M.; Conte-Junior, C.A.; Domínguez, R.; Nawaz, A.; Walayat, N.; Fierro, E.M.; Lorenzo, J.M. Marine Alkaloids: Compounds with in Vivo Activity and Chemical Synthesis. Mar. Drugs 2021, 19, 374. [Google Scholar] [CrossRef]
- Fassett, R.G.; Coombes, J.S. Astaxanthin: A Potential Therapeutic Agent in Cardiovascular Disease. Mar. Drugs 2011, 9, 447–465. [Google Scholar] [CrossRef]
- D’Alessandro, E.; Becker, C.; Bergmeier, W.; Bode, C.; Bourne, J.H.; Brown, H.; Buller, H.R.; Ten Cate-Hoek, A.J.; Ten Cate, V.; Van Cauteren, Y.J.M.; et al. Thrombo-Inflammation in Cardiovascular Disease: An Expert Consensus Document from the Third Maastricht Consensus Conference on Thrombosis. Thromb Haemost 2020, 120, 538–564. [Google Scholar] [CrossRef]
- Lordan, R.; Tsoupras, A.; Zabetakis, I. Platelet Activation and Prothrombotic Mediators at the Nexus of Inflammation and Atherosclerosis: Potential Role of Antiplatelet Agents. Blood Rev. 2021, 45, 100694. [Google Scholar] [CrossRef]
- Palur Ramakrishnan, A.V.K.; Varghese, T.P.; Vanapalli, S.; Nair, N.K.; Mingate, M.D. Platelet Activating Factor: A Potential Biomarker in Acute Coronary Syndrome? Cardiovasc. Ther. 2017, 35, 64–70. [Google Scholar] [CrossRef]
- Soni, R.; Muller, L.; Furet, P.; Schoepfer, J.; Stephan, C.; Zumstein-Mecker, S.; Fretz, H.; Chaudhuri, B. Inhibition of Cyclin-Dependent Kinase 4 (Cdk4) by Fascaplysin, a Marine Natural Product. Biochem. Biophys. Res. Commun. 2000, 275, 877–884. [Google Scholar] [CrossRef]
- Jiang, M.; Wu, Z.; Wu, Q.; Yin, H.; Guo, H.; Yuan, S.; Liu, Z.; Chen, S.; Liu, L. Amphichoterpenoids A–C, Unprecedented Picoline-Derived Meroterpenoids from the Ascidian-Derived Fungus Amphichorda Felina SYSU-MS7908. Chin. Chem. Lett. 2021, 32, 1893–1896. [Google Scholar] [CrossRef]
- Ren, R.; Azuma, Y.; Ojima, T.; Hashimoto, T.; Mizuno, M.; Nishitani, Y.; Yoshida, M.; Azuma, T.; Kanazawa, K. Modulation of Platelet Aggregation-Related Eicosanoid Production by Dietary F-Fucoidan from Brown Alga Laminaria Japonica in Human Subjects. Br. J. Nutr. 2013, 110, 880–890. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, A.; Saotome, M.; Iguchi, K.; Maekawa, Y. Marine-Derived Omega-3 Polyunsaturated Fatty Acids and Heart Failure: Current Understanding for Basic to Clinical Relevance. Int. J. Mol. Sci. 2019, 20, 4025. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Chang, T.; Chen, W.; Wang, X.; Li, J.; Chen, Y.; Yu, Y.; Shen, Z.; Yu, Q.; Zhang, Y. Release of VEGF and BMP9 from Injectable Alginate Based Composite Hydrogel for Treatment of Myocardial Infarction. Bioact. Mater. 2021, 6, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Liu, W. Functional Hydrogels for the Treatment of Myocardial Infarction. NPG Asia Mater. 2022, 14, 1–15. [Google Scholar] [CrossRef]
- Fan, C.; Joshi, J.; Li, F.; Xu, B.; Khan, M.; Yang, J.; Zhu, W. Nanoparticle-Mediated Drug Delivery for Treatment of Ischemic Heart Disease. Front. Bioeng. Biotechnol. 2020, 8, 687. [Google Scholar] [CrossRef]
- Ogita, H.; Node, K.; Asanuma, H.; Sanada, S.; Takashima, S.; Minamino, T.; Soma, M.; Kim, J.; Hori, M.; Kitakaze, M. Eicosapentaenoic Acid Reduces Myocardial Injury Induced by Ischemia and Reperfusion in Rabbit Hearts. J. Cardiovasc. Pharmacol. 2003, 41, 964–969. [Google Scholar] [CrossRef]
- Severino, P.; D’Amato, A.; Prosperi, S.; Magnocavallo, M.; Mariani, M.V.; Netti, L.; Birtolo, L.I.; De Orchi, P.; Chimenti, C.; Maestrini, V.; et al. Potential Role of ENOS Genetic Variants in Ischemic Heart Disease Susceptibility and Clinical Presentation. J. Cardiovasc. Dev. Dis. 2021, 8, 116. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Hashim, M.J.; Mustafa, H.; Baniyas, M.Y.; Al Suwaidi, S.K.B.M.; AlKatheeri, R.; Alblooshi, F.M.K.; Almatrooshi, M.E.A.H.; Alzaabi, M.E.H.; Al Darmaki, R.S.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, e9349. [Google Scholar] [CrossRef]
- Papier, K.; Knuppel, A.; Syam, N.; Jebb, S.A.; Key, T.J. Meat Consumption and Risk of Ischemic Heart Disease: A Systematic Review and Meta-Analysis. Crit. Rev. Food Sci. Nutr. 2023, 63, 426–437. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, N.K.; Lim, H.J.; Mazumder, S.; Rethineswaran, V.K.; Kim, Y.J.; Jang, W.B.; Ji, S.T.; Kang, S.; Kim, D.Y.; et al. Therapeutic Cell Protective Role of Histochrome under Oxidative Stress in Human Cardiac Progenitor Cells. Mar. Drugs 2019, 17, 368. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, R.; Pomin, V.H. Marine Antithrombotics. Mar. Drugs 2020, 18, 514. [Google Scholar] [CrossRef] [PubMed]
- Zhong, R.; Wan, X.; Wang, D.; Zhao, C.; Liu, D.; Gao, L.; Wang, M.; Wu, C.J.; Nabavid, S.M.; Daglia, M.; et al. Polysaccharides from Marine Enteromorpha: Structure and Function. Trends Food Sci. Technol. 2020, 99, 11–20. [Google Scholar] [CrossRef]
- Akil, L.; Anwar Ahmad, H. Relationships between Obesity and Cardiovascular Diseases in Four Southern States and Colorado. J. Health Care Poor Underserved 2011, 22, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.; Makkar, R.; Behl, T.; Sehgal, A.; Singh, S.; Rachamalla, M.; Mani, V.; Iqbal, M.S.; Bungau, S.G. Biotechnological Innovations from Ocean: Transpiring Role of Marine Drugs in Management of Chronic Disorders. Molecules 2022, 27, 1539. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Cao, Q.; Xing, M.; Xiao, H.; Cheng, Z.; Song, S.; Ji, A. Advances in the Study of Marine Products with Lipid-Lowering Properties. Mar. Drugs 2020, 18, 390. [Google Scholar] [CrossRef]
- Riccioni, G.; D’Orazio, N.; Franceschelli, S.; Speranza, L. Marine Carotenoids and Cardiovascular Risk Markers. Mar. Drugs 2011, 9, 1166–1175. [Google Scholar] [CrossRef]
- Kishimoto, Y.; Yoshida, H.; Kondo, K. Potential Anti-Atherosclerotic Properties of Astaxanthin. Mar. Drugs 2016, 14, 35. [Google Scholar] [CrossRef]
- Chen, W.L.; Qian, Y.; Meng, W.F.; Pang, J.Y.; Lin, Y.C.; Guan, Y.Y.; Chen, S.P.; Liu, J.; Pei, Z.; Wang, G.L. A Novel Marine Compound Xyloketal B Protects against Oxidized LDL-Induced Cell Injury in Vitro. Biochem. Pharmacol. 2009, 78, 941–950. [Google Scholar] [CrossRef]
- Blackwell, D.J.; Schmeckpeper, J.; Knollmann, B.C. Animal Models to Study Cardiac Arrhythmias. Circ. Res. 2022, 130, 1926–1964. [Google Scholar] [CrossRef]
- Do, H.K.; Kogure, K.; Imada, C.; Noguchi, T.; Ohwada, K.; Simidu, U. Tetrodotoxin Production of Actinomycetes Isolated from Marine Sediment. J. Appl. Bacteriol. 1991, 70, 464–468. [Google Scholar] [CrossRef]
- Hong, B.; He, J.; Le, Q.; Bai, K.; Chen, Y.; Huang, W. Combination Formulation of Tetrodotoxin and Lidocaine as a Potential Therapy for Severe Arrhythmias. Mar. Drugs 2019, 17, 685. [Google Scholar] [CrossRef] [PubMed]
- Mackieh, R.; Abou-Nader, R.; Wehbe, R.; Mattei, C.; Legros, C.; Fajloun, Z.; Sabatier, J.M. Voltage-Gated Sodium Channels: A Prominent Target of Marine Toxins. Mar. Drugs 2021, 19, 562. [Google Scholar] [CrossRef] [PubMed]
- Saravanan, P.; Davidson, N.C.; Schmidt, E.B.; Calder, P.C. Cardiovascular Effects of Marine Omega-3 Fatty Acids. Lancet 2010, 376, 540–550. [Google Scholar] [CrossRef]
- Bali, J.; Thakur, R. Poison as Cure: A Clinical Review of Botulinum Toxin as an Invaluable Drug. J. Venom. Anim. Toxins Incl. Trop. Dis. 2005, 11, 412–421. [Google Scholar] [CrossRef]
- Ertl, G.; Gaudran, P.; Neubauer, S.; Bauer, B.; Horn, M.; Hu, K.; Tian, R. Cardiac Dysfunction and Development of Heart Failure. Eur. Heart J. 1993, 14, 33–37. [Google Scholar] [CrossRef]
- Rhee, E.J.; Plutzky, J. Retinoid Metabolism and Diabetes Mellitus. Diabetes Metab. J. 2012, 36, 167–180. [Google Scholar] [CrossRef]
- Tang, X.H.; Gudas, L.J. Retinoids, Retinoic Acid Receptors, and Cancer. Annu. Rev. Pathol. Mech. Dis. 2011, 6, 345–364. [Google Scholar] [CrossRef]
- Shao, M.; Lu, L.; Wang, Q.; Ma, L.; Tian, X.; Li, C.; Li, C.; Guo, D.; Wang, Q.; Wang, W.; et al. The Multi-Faceted Role of Retinoid X Receptor in Cardiovascular Diseases. Biomed. Pharmacother. 2021, 137, 111264. [Google Scholar] [CrossRef]
- Zhu, S.; Guleria, R.S.; Thomas, C.M.; Roth, A.; Gerilechaogetu, F.; Kumar, R.; Dostal, D.E.; Baker, K.M.; Pan, J. Loss of Myocardial Retinoic Acid Receptor α Induces Diastolic Dysfunction by Promoting Intracellular Oxidative Stress and Calcium Mishandling in Adult Mice. J. Mol. Cell. Cardiol. 2016, 99, 100–112. [Google Scholar] [CrossRef]
- Guleria, R.S.; Singh, A.B.; Nizamutdinova, I.T.; Souslova, T.; Mohammad, A.A.; Kendall, J.A.; Baker, K.M.; Pan, J. Activation of Retinoid Receptor-Mediated Signaling Ameliorates Diabetes-Induced Cardiac Dysfunction in Zucker Diabetic Rats. J. Mol. Cell. Cardiol. 2013, 57, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Méresse, S.; Fodil, M.; Fleury, F.; Chénais, B. Fucoxanthin, a Marine-Derived Carotenoid from Brown Seaweeds and Microalgae: A Promising Bioactive Compound for Cancer Therapy. Int. J. Mol. Sci. 2020, 21, 9273. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Shibata, T.; Hisaka, S.; Osawa, T. Astaxanthin Inhibits Reactive Oxygen Species-Mediated Cellular Toxicity in Dopaminergic SH-SY5Y Cells via Mitochondria-Targeted Protective Mechanism. Brain Res. 2009, 1254, 18–27. [Google Scholar] [CrossRef]
- Fakhri, S.; Aneva, I.Y.; Farzaei, M.H.; Sobarzo-Sánchez, E. The Neuroprotective Effects of Astaxanthin: Therapeutic Targets and Clinical Perspective. Molecules 2019, 24, 2640. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, Y.; Tsuji, S.; Satoh, A.; Ishikura, M.; Shirasawa, T.; Shimizu, T. Protective Effects of Astaxanthin on 6-Hydroxydopamine-Induced Apoptosis in Human Neuroblastoma SH-SY5Y Cells. J. Neurochem. 2008, 107, 1730–1740. [Google Scholar] [CrossRef] [PubMed]
- Suleria, H.A.R.; Gobe, G.; Masci, P.; Osborne, S.A. Marine Bioactive Compounds and Health Promoting Perspectives; Innovation Pathways for Drug Discovery. Trends Food Sci. Technol. 2016, 50, 44–55. [Google Scholar] [CrossRef]
- Cardoso, S.M.; Pereira, O.R.; Seca, A.M.L.; Pinto, D.C.G.A.; Silva, A.M.S. Seaweeds as Preventive Agents for Cardiovascular Diseases: From Nutrients to Functional Foods. Mar. Drugs 2015, 13, 6838–6865. [Google Scholar] [CrossRef] [PubMed]
- Spoială, A.; Ilie, C.I.; Ficai, D.; Ficai, A.; Andronescu, E. From Biomedical Applications of Alginate towards CVD Implications Linked to COVID-19. Pharmaceuticals 2022, 15, 318. [Google Scholar] [CrossRef]
- Xu, Z.; Lam, M.T. Alginate Application for Heart and Cardiovascular Diseases. Springer Ser. Biomater. Sci. Eng. 2018, 11, 185–212. [Google Scholar] [CrossRef]
- Sokolova, E.V.; Bogdanovich, L.N.; Ivanova, T.B.; Byankina, A.O.; Kryzhanovskiy, S.P.; Yermak, I.M. Effect of Carrageenan Food Supplement on Patients with Cardiovascular Disease Results in Normalization of Lipid Profile and Moderate Modulation of Immunity System Markers. PharmaNutrition 2014, 2, 33–37. [Google Scholar] [CrossRef]
- Gioele, C.; Marilena, S.; Valbona, A.; Nunziacarla, S.; Andrea, S.; Antonio, M. Gracilaria Gracilis, Source of Agar: A Short Review. Curr. Org. Chem. 2017, 21, 380–386. [Google Scholar] [CrossRef]
- Zhang, B.; Zhang, X. Separation and Nanoencapsulation of Antitumor Polypeptide from Spirulina Platensis. Biotechnol. Prog. 2013, 29, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- Cian, R.E.; Martínez-Augustin, O.; Drago, S.R. Bioactive Properties of Peptides Obtained by Enzymatic Hydrolysis from Protein Byproducts of Porphyra Columbina. Food Res. Int. 2012, 49, 364–372. [Google Scholar] [CrossRef]
- Furuta, T.; Miyabe, Y.; Yasui, H.; Kinoshita, Y.; Kishimura, H. Angiotensin I Converting Enzyme Inhibitory Peptides Derived from Phycobiliproteins of Dulse Palmaria Palmata. Mar. Drugs 2016, 14, 32. [Google Scholar] [CrossRef] [PubMed]
- Harnedy, P.A.; O’Keeffe, M.B.; Fitzgerald, R.J. Purification and Identification of Dipeptidyl Peptidase (DPP) IV Inhibitory Peptides from the Macroalga Palmaria Palmata. Food Chem. 2015, 172, 400–406. [Google Scholar] [CrossRef] [PubMed]
- You, H.N.; Lee, H.A.; Park, M.H.; Lee, J.H.; Han, J.S. Phlorofucofuroeckol A Isolated from Ecklonia Cava Alleviates Postprandial Hyperglycemia in Diabetic Mice. Eur. J. Pharmacol. 2015, 752, 92–96. [Google Scholar] [CrossRef]
- Lozano-Muñoz, I.; Muñoz, S.; Díaz, N.F.; Medina, A.; Bazaes, J.; Riquelme, C. Nutritional Enhancement of Farmed Salmon Meat via Non-GMO Nannochloropsis Gaditana: Eicosapentaenoic Acid (EPA, 20:5 n-3), Docosapentaenoic Acid (DPA, 22:5 n-3) and Vitamin D3 for Human Health. Molecules 2020, 25, 4615. [Google Scholar] [CrossRef]
- Rayaroth, A.C.; Tomar, R.S.; Mishra, R.K. Arachidonic Acid Synthesis in Mortierella Alpina: Origin, Evolution and Advancements. Proc. Natl. Acad. Sci. India Sect. B–Biol. Sci. 2017, 87, 1053–1066. [Google Scholar] [CrossRef]
- Agarwal, S.; Chauhan, K. Fucoidan: A Promising Target for Dyslipidemia-A Concise Review. Pharma Innov. J. 2019, 8, 62–67. [Google Scholar]
- Kordjazi, M.; Etemadian, Y.; Shabanpour, B.; Pourashouri, P. Chemical Composition Antioxidant and Antimicrobial Activities of Fucoidan Extracted from Two Species of Brown Seaweeds (Sargassum Ilicifolium and S.Angustifolium) around Qeshm Island. Iran. J. Fish. Sci. 2019, 18, 457–475. [Google Scholar] [CrossRef]
- Mattei, C. Tetrodotoxin, a Candidate Drug for Nav1.1-Induced Mechanical Pain? Mar. Drugs 2018, 16, 72. [Google Scholar] [CrossRef] [PubMed]
- González-Cano, R.; Tejada, M.Á.; Artacho-Cordón, A.; Nieto, F.R.; Entrena, J.M.; Wood, J.N.; Cendán, C.M. Effects of Tetrodotoxin in Mouse Models of Visceral Pain. Mar. Drugs 2017, 15, 188. [Google Scholar] [CrossRef]
- Biessy, L.; Smith, K.F.; Wood, S.A.; Tidy, A.; van Ginkel, R.; Bowater, J.R.D.; Hawes, I. A Microencapsulation Method for Delivering Tetrodotoxin to Bivalves to Investigate Uptake and Accumulation. Mar. Drugs 2021, 19, 33. [Google Scholar] [CrossRef]
- Durán-Riveroll, L.M.; Cembella, A.D. Guanidinium Toxins and Their Interactions with Voltage-Gated Sodium Ion Channels. Mar. Drugs 2017, 15, 303. [Google Scholar] [CrossRef] [PubMed]
- Xiao, A.J.; Chen, W.; Xu, B.; Liu, R.; Turlova, E.; Barszczyk, A.; Sun, C.L.; Liu, L.; Deurloo, M.; Wang, G.L.; et al. Marine Compound Xyloketal B Reduces Neonatal Hypoxic-Ischemic Brain Injury. Mar. Drugs 2015, 13, 29–47. [Google Scholar] [CrossRef] [PubMed]
- Tsoupras, A.; Brummell, C.; Kealy, C.; Vitkaitis, K.; Redfern, S.; Zabetakis, I. Cardio-Protective Properties and Health Benefits of Fish Lipid Bioactives; The Effects of Thermal Processing. Mar. Drugs 2022, 20, 187. [Google Scholar] [CrossRef] [PubMed]
- Lordan, R.; Redfern, S.; Tsoupras, A.; Zabetakis, I. Inflammation and Cardiovascular Disease: Are Marine Phospholipids the Answer? Food Funct. 2020, 11, 2861–2885. [Google Scholar] [CrossRef]
- Tsoupras, A.; Lordan, R.; Zabetakis, I. Inflammation, Not Cholesterol, Is a Cause of Chronic Disease. Nutrients 2018, 10, 604. [Google Scholar] [CrossRef]
- Nasopoulou, C.; Nomikos, T.; Demopoulos, C.A.; Zabetakis, I. Comparison of Antiatherogenic Properties of Lipids Obtained from Wild and Cultured Sea Bass (Dicentrarchus Labrax) and Gilthead Sea Bream (Sparus Aurata). Food Chem. 2007, 100, 560–567. [Google Scholar] [CrossRef]
- Panayiotou, A.; Samartzis, D.; Nomikos, T.; Fragopoulou, E.; Karantonis, H.C.; Demopoulos, C.A.; Zabetakis, I. Lipid Fractions with Aggregatory and Antiaggregatory Activity toward Platelets in Fresh and Fried Cod (Gadus Morhua): Correlation with Platelet-Activating Factor and Atherogenesis. J. Agric. Food Chem. 2000, 48, 6372–6379. [Google Scholar] [CrossRef]
- De Leonardis, A.; Macciola, V. A Study on the Lipid Fraction of Adriatic Sardine Filets (Sardina Pilchardus). Nahrung–Food 2004, 48, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Conde, T.A.; Zabetakis, I.; Tsoupras, A.; Medina, I.; Costa, M.; Silva, J.; Neves, B.; Domingues, P.; Domingues, M.R. Microalgal Lipid Extracts Have Potential to Modulate the Inflammatory Response: A Critical Review. Int. J. Mol. Sci. 2021, 22, 9825. [Google Scholar] [CrossRef] [PubMed]
- Koukouraki, P.; Tsoupras, A.; Sotiroudis, G.; Demopoulos, C.A.; Sotiroudis, T.G. Antithrombotic Properties of Spirulina Extracts against Platelet-Activating Factor and Thrombin. Food Biosci. 2020, 37, 100686. [Google Scholar] [CrossRef]
- Nasopoulou, C.; Tsoupras, A.B.; Karantonis, H.C.; Demopoulos, C.A.; Zabetakis, I. Fish Polar Lipids Retard Atherosclerosis in Rabbits by Down-Regulating PAF Biosynthesis and up-Regulating PAF Catabolism. Lipids Health Dis. 2011, 10, 213. [Google Scholar] [CrossRef]
- Burri, L.; Hoem, N.; Banni, S.; Berge, K. Marine Omega-3 Phospholipids: Metabolism and Biological Activities. Int. J. Mol. Sci. 2012, 13, 15401–15419. [Google Scholar] [CrossRef] [PubMed]
- Fosshaug, L.E.; Berge, R.K.; Beitnes, J.O.; Berge, K.; Vik, H.; Aukrust, P.; Gullestad, L.; Vinge, L.E.; Oie, E. Krill Oil Attenuates Left Ventricular Dilatation after Myocardial Infarction in Rats. Lipids Health Dis. 2011, 10, 245. [Google Scholar] [CrossRef]
- Granger, D.N.; Rodrigues, S.F.; Yildirim, A.; Senchenkova, E.Y. Microvascular Responses to Cardiovascular Risk Factors. Microcirculation 2010, 17, 192–205. [Google Scholar] [CrossRef]
- Verouti, S.N.; Tsoupras, A.B.; Alevizopoulou, F.; Demopoulos, C.A.; Iatrou, C. Paricalcitol Effects on Activities and Metabolism of Platelet Activating Factor and on Inflammatory Cytokines in Hemodialysis Patients. Int. J. Artif. Organs 2013, 36, 87–96. [Google Scholar] [CrossRef]
- de la Guía-Galipienso, F.; Martínez-Ferran, M.; Vallecillo, N.; Lavie, C.J.; Sanchis-Gomar, F.; Pareja-Galeano, H. Vitamin D and Cardiovascular Health. Clin. Nutr. 2021, 40, 2946–2957. [Google Scholar] [CrossRef]
- Nestel, P.J. Fish Oil and Cardiovascular Disease: Lipids and Arterial Function. Am. J. Clin. Nutr. 2000, 71, 228S–231S. [Google Scholar] [CrossRef]
- Kander, M.C.; Cui, Y.; Liu, Z. Gender Difference in Oxidative Stress: A New Look at the Mechanisms for Cardiovascular Diseases. J. Cell. Mol. Med. 2017, 21, 1024–1032. [Google Scholar] [CrossRef] [PubMed]
- Moris, D.; Spartalis, M.; Spartalis, E.; Karachaliou, G.S.; Karaolanis, G.I.; Tsourouflis, G.; Tsilimigras, D.I.; Tzatzaki, E.; Theocharis, S. The Role of Reactive Oxygen Species in the Pathophysiology of Cardiovascular Diseases and the Clinical Significance of Myocardial Redox. Ann. Transl. Med. 2017, 5, 326. [Google Scholar] [CrossRef] [PubMed]
- Guerby, P.; Tasta, O.; Swiader, A.; Pont, F.; Bujold, E.; Parant, O.; Vayssiere, C.; Salvayre, R.; Negre-Salvayre, A. Role of Oxidative Stress in the Dysfunction of the Placental Endothelial Nitric Oxide Synthase in Preeclampsia. Redox Biol. 2021, 40, 101861. [Google Scholar] [CrossRef]
- Augusti, P.R.; Conterato, G.M.M.; Somacal, S.; Sobieski, R.; Quatrin, A.; Maurer, L.; Rocha, M.P.; Denardin, I.T.; Emanuelli, T. Astaxanthin Reduces Oxidative Stress, but Not Aortic Damage in Atherosclerotic Rabbits. J. Cardiovasc. Pharmacol. Ther. 2009, 14, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Cao, Q.; Zhao, J.; Xing, M.; Xiao, H.; Zhang, Q.; Liang, H.; Ji, A.; Song, S. Current Research Landscape of Marine-Derived Anti-Atherosclerotic Substances. Mar. Drugs 2020, 18, 440. [Google Scholar] [CrossRef] [PubMed]
- Akram, W.; Tagde, P.; Ahmed, S.; Arora, S.; Emran, T.B.; Babalghith, A.O.; Sweilam, S.H.; Simal-Gandara, J. Guaiazulene and Related Compounds: A Review of Current Perspective on Biomedical Applications. Life Sci. 2023, 316, 121389. [Google Scholar] [CrossRef]
- Cong, L.; Ren, Y.; Hou, T.; Han, X.; Dong, Y.; Wang, Y.; Zhang, Q.; Liu, R.; Xu, S.; Wang, L.; et al. Use of Cardiovascular Drugs for Primary and Secondary Prevention of Cardiovascular Disease Among Rural-Dwelling Older Chinese Adults. Front. Pharmacol. 2020, 11, 608136. [Google Scholar] [CrossRef]
- Papon, N.; Copp, B.R.; Courdavault, V. Marine Drugs: Biology, Pipelines, Current and Future Prospects for Production. Biotechnol. Adv. 2022, 54, 107871. [Google Scholar] [CrossRef]
- Rihan, M.; Sharma, S.S. Role of Pyruvate Kinase M2 (PKM2) in Cardiovascular Diseases. J. Cardiovasc. Transl. Res. 2022, 1–21. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).