The Polymorphisms of Genes Encoding Catalytic Antioxidant Proteins Modulate the Susceptibility and Progression of Testicular Germ Cell Tumor
Abstract
Simple Summary
Abstract
1. Introduction
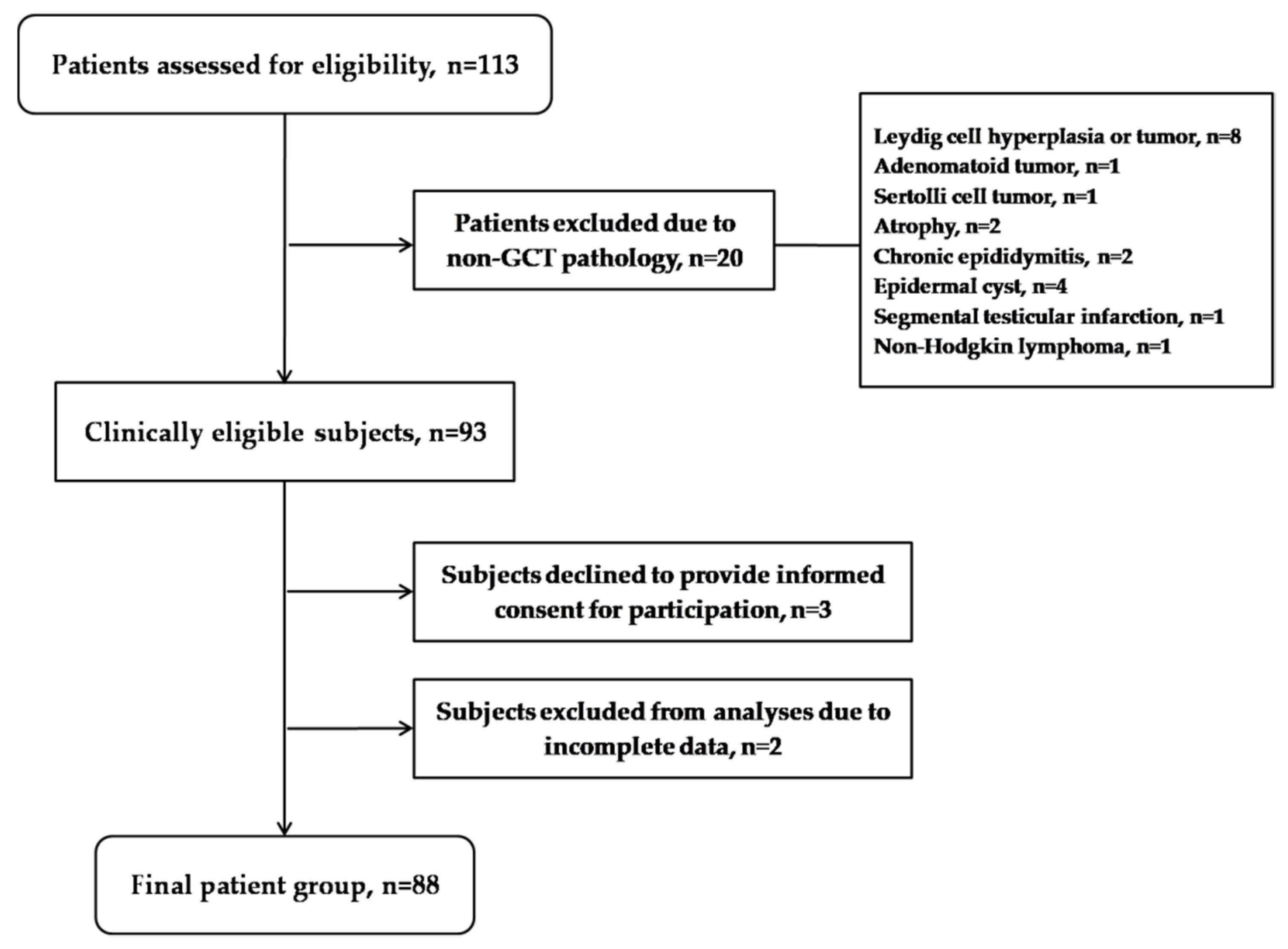
2. Materials and Methods
3. Results
3.1. The Characteristics of Patients with Testicular GCT and Respective Controls
3.2. The Association of Polymorphisms Encoding for Regulatory and Catalytic Antioxidant Proteins with the Risk for Testicular GCT Development
3.3. The Association between Polymorphisms Encoding for Regulatory and Catalytic Antioxidant Proteins with the Risk of Disease Progression
3.4. The Association between Polymorphisms Encoding for Regulatory and Catalytic Antioxidant Proteins with Redox Biomarkers in Patients with Testicular GCT
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Winter, C.; Albers, P. Testicular germ cell tumors: Pathogenesis, diagnosis and treatment. Nat. Rev. Endocrinol. 2011, 7, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Baroni, T.; Arato, I.; Mancuso, F.; Calafiore, R.; Luca, G. On the Origin of Testicular Germ Cell Tumors: From Gonocytes to Testicular Cancer. Front. Endocrinol. 2019, 10, 343. [Google Scholar] [CrossRef] [PubMed]
- Williamson, S.R.; Delahunt, B.; Magi-Galluzzi, C.; Algaba, F.; Egevad, L.; Ulbright, T.M.; Tickoo, S.K.; Srigley, J.R.; Epstein, J.I.; Berney, D.M.; et al. The World Health Organization 2016 classification of testicular germ cell tumours: A review and update from the International Society of Urological Pathology Testis Consultation Panel. Histopathology 2017, 70, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Skakkebæk, N.E.; Rajpert-De Meyts, E.; Main, K.M. Testicular dysgenesis syndrome: An increasingly common developmental disorder with environmental aspects: Opinion. Hum. Reprod. 2001, 16, 972–978. [Google Scholar] [CrossRef] [PubMed]
- Garner, M.J.; Turner, M.C.; Ghadirian, P.; Krewski, D. Epidemiology of testicular cancer: An overview. Int. J. Cancer 2005, 116, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Batool, A.; Karimi, N.; Wu, X.-N.; Chen, S.-R.; Liu, Y.-X. Testicular germ cell tumor: A comprehensive review. Cell. Mol. Life Sci. 2019, 76, 1713–1727. [Google Scholar] [CrossRef] [PubMed]
- FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and Other Tools) Resource; Food and Drug Administration (US): Silver Spring, MD, USA, 2016. [Google Scholar]
- Assi, M. The differential role of reactive oxygen species in early and late stages of cancer. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2017, 313, R646–R653. [Google Scholar] [CrossRef] [PubMed]
- Sosa, V.; Moliné, T.; Somoza, R.; Paciucci, R.; Kondoh, H.; LLeonart, M.E. Oxidative stress and cancer: An overview. Ageing Res. Rev. 2013, 12, 376–390. [Google Scholar] [CrossRef] [PubMed]
- Mijatović, S.; Savić-Radojević, A.; Plješa-Ercegovac, M.; Simić, T.; Nicoletti, F.; Maksimović-Ivanić, D. The Double-Faced Role of Nitric Oxide and Reactive Oxygen Species in Solid Tumors. Antioxidants 2020, 9, 374. [Google Scholar] [CrossRef] [PubMed]
- Rojo de la Vega, M.; Chapman, E.; Zhang, D.D. NRF2 and the Hallmarks of Cancer. Cancer Cell 2018, 34, 21–43. [Google Scholar] [CrossRef] [PubMed]
- Tonelli, C.; Chio, I.I.C.; Tuveson, D.A. Transcriptional Regulation by Nrf2. Antioxid Redox Signal 2018, 29, 1727–1745. [Google Scholar] [CrossRef] [PubMed]
- Marzec, J.M.; Christie, J.D.; Reddy, S.P.; Jedlicka, A.E.; Vuong, H.; Lanken, P.N.; Aplenc, R.; Yamamoto, T.; Yamamoto, M.; Cho, H.-Y. Functional polymorphisms in the transcription factor NRF2 in humans increase the risk of acute lung injury. FASEB J. 2007, 21, 2237–2246. [Google Scholar] [CrossRef] [PubMed]
- Pljesa-Ercegovac, M.; Savic-Radojevic, A.; Matic, M.; Coric, V.; Djukic, T.; Radic, T.; Simic, T. Glutathione Transferases: Potential Targets to Overcome Chemoresistance in Solid Tumors. Int. J. Mol. Sci. 2018, 19, 3785. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Yang, J.; You, L.; Dai, M.; Zhao, Y. GSTM3 Function and Polymorphism in Cancer: Emerging but Promising. CMAR 2020, 12, 10377–10388. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.; Wang, Y.; Han, Y.; Chang, W.; Su, T.; Hou, J.; Xu, D.; Yu, Y.; Ma, W.; Thompson, T.C.; et al. Genetic variation in the GSTM3 promoter confer risk and prognosis of renal cell carcinoma by reducing gene expression. Br. J. Cancer 2013, 109, 3105–3115. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chang, C.; Worley, B.L.; Phaëton, R.; Hempel, N. Extracellular Glutathione Peroxidase GPx3 and Its Role in Cancer. Cancers 2020, 12, 2197. [Google Scholar] [CrossRef] [PubMed]
- Voetsch, B.; Jin, R.C.; Bierl, C.; Benke, K.S.; Kenet, G.; Simioni, P.; Ottaviano, F.; Damasceno, B.P.; Annichino-Bizacchi, J.M.; Handy, D.E. Promoter polymorphisms in the plasma glutathione peroxidase (GPx-3) gene: A novel risk factor for arterial ischemic stroke among young adults and children. Stroke 2007, 38, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Sutton, A.; Khoury, H.; Prip-Buus, C.; Cepanec, C.; Pessayre, D.; Degoul, F. The Ala16Val genetic dimorphism modulates the import of human manganese superoxide dismutase into rat liver mitochondria. Pharm. Genom. 2003, 13, 145–157. [Google Scholar] [CrossRef]
- Sutton, A.; Imbert, A.; Igoudjil, A.; Descatoire, V.; Cazanave, S.; Pessayre, D.; Degoul, F. The manganese superoxide dismutase Ala16Val dimorphism modulates both mitochondrial import and mRNA stability. Pharm. Genom. 2005, 15, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Paner, G.P.; Stadler, W.M.; Hansel, D.E.; Montironi, R.; Lin, D.W.; Amin, M.B. Updates in the Eighth Edition of the Tumor-Node-Metastasis Staging Classification for Urologic Cancers. Eur. Urol. 2018, 73, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Moch, H.; Cubilla, A.L.; Humphrey, P.A.; Reuter, V.E.; Ulbright, T.M. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. Eur. Urol. 2016, 70, 93–105. [Google Scholar] [CrossRef] [PubMed]
- Shimoyama, Y.; Mitsuda, Y.; Tsuruta, Y.; Hamajima, N.; Niwa, T. Polymorphism of Nrf2, an Antioxidative Gene, is Associated with Blood Pressure and Cardiovascular Mortality in Hemodialysis Patients. Int. J. Med. Sci. 2014, 11, 726–731. [Google Scholar] [CrossRef] [PubMed]
- Jocelyn, P.C. Spectrophotometric assay of thiols. In Methods in Enzymology; Elsevier: Amsterdam, The Netherlands, 1987; Volume 143, pp. 44–67. ISBN 978-0-12-182043-5. [Google Scholar]
- Walmsley, T.A.; Abernethy, M.H.; Fitzgerald, H.P. Effect of daylight on the reaction of thiols with Ellman’s reagent, 5,5′-dithiobis(2-nitrobenzoic acid). Clin. Chem. 1987, 33, 1928–1931. [Google Scholar] [CrossRef] [PubMed]
- Günzler, W.A.; Kremers, H.; Flohé, L. An Improved Coupled Test Procedure for Glutathione Peroxidase (EC 1.11.1.9.) in Blood. Clin. Chem. Lab. Med. 1974, 12, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Sies, H. Hydrogen peroxide as a central redox signaling molecule in physiological oxidative stress: Oxidative eustress. Redox Biol. 2017, 11, 613–619. [Google Scholar] [CrossRef]
- Suzuki, T.; Shibata, T.; Takaya, K.; Shiraishi, K.; Kohno, T.; Kunitoh, H.; Tsuta, K.; Furuta, K.; Goto, K.; Hosoda, F.; et al. Regulatory nexus of synthesis and degradation deciphers cellular Nrf2 expression levels. Mol. Cell. Biol. 2013, 33, 2402–2412. [Google Scholar] [CrossRef] [PubMed]
- Sporn, M.B.; Liby, K.T. NRF2 and cancer: The good, the bad and the importance of context. Nat. Rev. Cancer 2012, 12, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.-Y.; Marzec, J.; Kleeberger, S.R. Functional polymorphisms in Nrf2: Implications for human disease. Free Radic. Biol. Med. 2015, 88, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Dhar, S.K.; Clair, D.K.S. Manganese superoxide dismutase regulation and cancer. Free Radic. Biol. Med. 2012, 52, 2209–2222. [Google Scholar] [CrossRef] [PubMed]
- Biggs, M.L. Polymorphisms in genes encoding oxidative stress defense enzymes and risk of testicular germ cell carcinoma. Proc. Amer. Assoc. Cancer Res. 2004, 64, 255. [Google Scholar]
- Yu, B.; Huang, Z. Variations in Antioxidant Genes and Male Infertility. BioMed Res. Int. 2015, 2015, 1–10. [Google Scholar] [CrossRef]
- Nirgude, S.; Choudhary, B. Insights into the role of GPX3, a highly efficient plasma antioxidant, in cancer. Biochem. Pharmacol. 2021, 184, 114365. [Google Scholar] [CrossRef] [PubMed]
- Lan, D.; Wang, L.; He, R.; Ma, J.; Bin, Y.; Chi, X.; Chen, G.; Cai, Z. Exogenous glutathione contributes to cisplatin resistance in lung cancer A549 cells. Am. J. Transl. Res. 2018, 10, 1295–1309. [Google Scholar]
- Strange, R.C.; Spiteri, M.A.; Ramachandran, S.; Fryer, A.A. Glutathione-S-transferase family of enzymes. Mutat. Res./Fundam. Mol. Mech. Mutagenesis 2001, 482, 21–26. [Google Scholar] [CrossRef]
- Hayes, J.D.; Flanagan, J.U.; Jowsey, I.R. Glutathione transferases. Annu. Rev. Pharmacol. Toxicol. 2005, 45, 51–88. [Google Scholar] [CrossRef]
- Yadav, P.; Chatterjee, A.; Bhattacharjee, A. Identification of deleterious nsSNPs in α, μ, π and θ class of GST family and their influence on protein structure. Genom. Data 2014, 2, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Campbell, M.R.; Pittman, G.S.; Faulkner, E.C.; Watson, M.A.; Bell, D.A. Expression-based discovery of variation in the human glutathione S-transferase M3 promoter and functional analysis in a glioma cell line using allele-specific chromatin immunoprecipitation. Cancer Res. 2005, 65, 99–104. [Google Scholar] [PubMed]
- Zimmermann, U.; Junker, H.; Krämer, F.; Balabanov, S.; Kleist, B.; Kammer, W.; Nordheim, A.; Walther, R. Comparative proteomic analysis of neoplastic and non-neoplastic germ cell tissue. Biol. Chem. 2006, 387, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Patskovsky, Y.V.; Huang, M.-Q.; Takayama, T.; Listowsky, I.; Pearson, W.R. Distinctive Structure of the HumanGSTM3Gene—Inverted Orientation Relative to the Mu Class Glutathione Transferase Gene Cluster. Arch. Biochem. Biophys. 1999, 361, 85–93. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Inskip, A.; Elexperu-Camiruaga, J.; Buxton, N.; Dias, P.S.; MacIntosh, J.; Campbell, D.; Jones, P.W.; Yengi, L.; Talbot, J.A.; Strange, R.C.; et al. Identification of polymorphism at the glutathione S-transferase, GSTM3 locus: Evidence for linkage with GSTM1*A. Biochem. J. 1995, 312, 713–716. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Coric, V.M.; Simic, T.P.; Pekmezovic, T.D.; Basta-Jovanovic, G.M.; Savic-Radojevic, A.R.; Radojevic-Skodric, S.M.; Matic, M.G.; Suvakov, S.R.; Dragicevic, D.P.; Radic, T.M.; et al. GSTM1 genotype is an independent prognostic factor in clear cell renal cell carcinoma. Urol. Oncol. 2017, 35, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Radic, T.; Coric, V.; Bukumiric, Z.; Pljesa-Ercegovac, M.; Djukic, T.; Avramovic, N.; Matic, M.; Mihailovic, S.; Dragicevic, D.; Dzamic, Z.; et al. GSTO1*CC Genotype (rs4925) Predicts Shorter Survival in Clear Cell Renal Cell Carcinoma Male Patients. Cancers 2019, 11, 2038. [Google Scholar] [CrossRef] [PubMed]
- Checa-Rojas, A.; Delgadillo-Silva, L.F.; del Castillo Velasco-Herrera, M.; Andrade-Domínguez, A.; Gil, J.; Santillán, O.; Lozano, L.; Toledo-Leyva, A.; Ramírez-Torres, A.; Talamas-Rohana, P.; et al. GSTM3 and GSTP1: Novel players driving tumor progression in cervical cancer. Oncotarget 2018, 9, 21696–21714. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Testicular GCT Patients | Control Group | OR (95%CI) | p |
|---|---|---|---|---|
| Age (years) | 33.5 (19–54) 1 | 36.5 (18–54) 1 | - | 0.266 2 |
| Body mass index, n (%) 3 | ||||
| <30 kg/m2 | 73 (88) | 63 (84) | 1.00 4 | |
| >30 kg/m2 | 10 (12) | 12 (16) | 0.72 (0.29–1.77) | 0.475 5 |
| Smoking status, n (%) 3 | ||||
| Never | 36 (44) | 42 (48) | 1.00 4 | |
| Ever | 45 (56) | 46 (52) | 1.14 (0.62–2.09) | 0.669 5 |
| Factors associated with higher risk for testicular GCT development, n (%) 3 | ||||
| Cryptorchismus | 8 (9) | - | - | - |
| Infertility | 4 (5) | - | - | - |
| Family history | 4 (5) | - | - | - |
| Testicular atrophy | 7 (8) | - | - | - |
| Tumor type, n (%) | ||||
| Seminoma | 52 (59) | - | - | - |
| Non-seminoma | 36 (41) | - | - | - |
| Clinical stage, n (%) | ||||
| I | 61 (69) | - | - | - |
| II | 18 (21) | - | - | - |
| III | 9 (10) | - | - | - |
| Genotype | Testicular GCT Patients, n (%) | Control Group, n (%) | OR (95%CI) 1 | p | OR (95%CI) 2 | p |
|---|---|---|---|---|---|---|
| NRF2 (rs6721961) | ||||||
| AA | 2 (2) | 3 (4) | 1.00 3 | 1.00 3 | ||
| CC + CA | 84 (98) | 73 (96) | 1.72 (0.28–10.61) | 0.556 | 1.42 (0.20–9.72) | 0.719 |
| GSTM3 (rs1332018) | ||||||
| CC | 10 (12) | 19 (22) | 1.00 3 | 1.00 3 | ||
| AA + AC | 73 (88) | 67 (78) | 2.07 (0.90–4.76) | 0.087 | 1.23 (0.48–3.10) | 0.662 |
| SOD2 (rs4880) | ||||||
| CC + CT | 54 (67) | 69 (79) | 1.00 3 | 1.00 3 | ||
| TT | 26 (33) | 18 (21) | 1.84 (0.91–3.71) | 0.086 | 2.12 (0.97–4.62) | 0.057 |
| GPX3 (rs8177412) | ||||||
| TT | 38 (44) | 58 (67) | 1.00 3 | 1.00 3 | ||
| TC + CC | 48 (56) | 28 (33) | 2.61 (1.40–4.86) | 0.002 | 2.14 (1.09–4.19) | 0.027 |
| Genotypes | Testicular GCT Patients, n (%) 1 | Control Group, n (%) 1 | OR (95%CI) 2 | p |
|---|---|---|---|---|
| SOD2*CC + CT/GPX3*TT | 25 (32) | 44 (52) | 1.00 3 | |
| SOD2*TT/GPX3*TC + CC | 17 (22) | 4 (5) | 7.48 (2.26–24.70) | 0.001 |
| Genotype | Seminoma Patients, n (%) | Control Group, n (%) | OR (95%CI) 1 | p | OR (95%CI) 2 | p |
|---|---|---|---|---|---|---|
| NRF2 (rs6721961) | ||||||
| AA | 2 (4) | 3 (4) | 1.00 3 | 1.00 3 | ||
| CC + CA | 49 (96) | 73 (96) | 1.70 (0.16–6.24) | 0.994 | 0.801 (0.32–2.70) | 0.942 |
| GSTM3 (rs1332018) | ||||||
| CC | 7 (14) | 19 (22) | 1.00 3 | 1.00 3 | ||
| AA + AC | 43 (86) | 67 (78) | 1.74 (0.67–4.49) | 0.251 | 0.94 (0.32–2.70) | 0.912 |
| SOD2 (rs4880) | ||||||
| CC + CT | 28 (61) | 69 (79) | 1.00 3 | 1.00 3 | ||
| TT | 18 (39) | 18 (21) | 2.46 (1.12–5.41) | 0.025 | 2.84 (1.20–6.74) | 0.017 |
| GPX3 (rs8177412) | ||||||
| TT | 21 (41) | 58 (67) | 1.00 3 | 1.00 3 | ||
| TC + CC | 30 (59) | 28 (33) | 2.95 (1.44–6.06) | 0.003 | 2.29 (1.04–5.06) | 0.039 |
| Genotype | Stage I, n (%) | Stages II + III, n (%) | OR (95%CI) 1 | p | OR (95%CI) 2 | p |
|---|---|---|---|---|---|---|
| NRF2 (rs6721961) | ||||||
| CC | 43 (72) | 18 (69) | 1.00 3 | 1.00 3 | ||
| CA + AA | 17 (28) | 8 (31) | 1.12 (0.41–3.06) | 0.819 | 0.82 (0.22–3.01) | 0.769 |
| GSTM3 (rs1332018) | ||||||
| AA | 31 (53) | 7 (28) | 1.00 | 1.00 3 | ||
| AC + CC | 27 (47) | 18 (72) | 2.95 (1.07–8.13) | 0.036 | 4.51 (1.30–15.63) | 0.018 |
| SOD2 (rs4880) | ||||||
| CC | 11 (20) | 7 (28) | 1.00 3 | 1.00 3 | ||
| CT + TT | 44 (80) | 18 (72) | 0.64 (0.21–1.92) | 0.429 | 0.389 (0.14–1.45) | 0.160 |
| GPX3 (rs8177412) | ||||||
| TT | 28 (47) | 10 (38) | 1.00 3 | 1.00 3 | ||
| TC + CC | 32 (53) | 16 (62) | 1.40 (0.54–3.58) | 0.482 | 2.21 (0.69–7.09) | 0.182 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bumbasirevic, U.; Bojanic, N.; Pljesa-Ercegovac, M.; Zivkovic, M.; Djukic, T.; Zekovic, M.; Milojevic, B.; Kajmakovic, B.; Janicic, A.; Simic, T.; et al. The Polymorphisms of Genes Encoding Catalytic Antioxidant Proteins Modulate the Susceptibility and Progression of Testicular Germ Cell Tumor. Cancers 2022, 14, 1068. https://doi.org/10.3390/cancers14041068
Bumbasirevic U, Bojanic N, Pljesa-Ercegovac M, Zivkovic M, Djukic T, Zekovic M, Milojevic B, Kajmakovic B, Janicic A, Simic T, et al. The Polymorphisms of Genes Encoding Catalytic Antioxidant Proteins Modulate the Susceptibility and Progression of Testicular Germ Cell Tumor. Cancers. 2022; 14(4):1068. https://doi.org/10.3390/cancers14041068
Chicago/Turabian StyleBumbasirevic, Uros, Nebojsa Bojanic, Marija Pljesa-Ercegovac, Marko Zivkovic, Tatjana Djukic, Milica Zekovic, Bogomir Milojevic, Boris Kajmakovic, Aleksandar Janicic, Tatjana Simic, and et al. 2022. "The Polymorphisms of Genes Encoding Catalytic Antioxidant Proteins Modulate the Susceptibility and Progression of Testicular Germ Cell Tumor" Cancers 14, no. 4: 1068. https://doi.org/10.3390/cancers14041068
APA StyleBumbasirevic, U., Bojanic, N., Pljesa-Ercegovac, M., Zivkovic, M., Djukic, T., Zekovic, M., Milojevic, B., Kajmakovic, B., Janicic, A., Simic, T., & Coric, V. (2022). The Polymorphisms of Genes Encoding Catalytic Antioxidant Proteins Modulate the Susceptibility and Progression of Testicular Germ Cell Tumor. Cancers, 14(4), 1068. https://doi.org/10.3390/cancers14041068









