Abstract
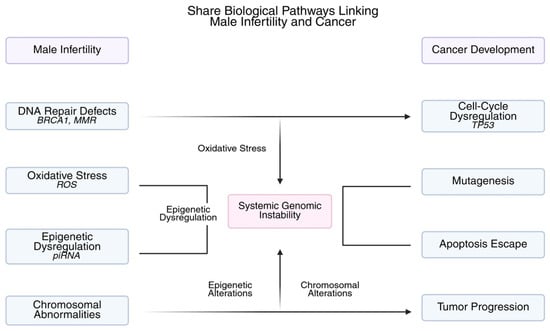
Approximately 7% of males globally suffer from male infertility, which is becoming more widely acknowledged as a clinical indicator of potential health hazards as well as a cause of reproductive failure. Among these, cancer has become a significant worry due to mounting evidence that spermatogenesis impairment is associated with increased risk of prostate, testicular, and other cancers. Male infertility may be an early clinical manifestation of systemic genomic instability due to shared biological pathways, such as Y-chromosome microdeletions (AZF regions), germline DNA repair defects, mutations in tumor suppressor genes (e.g., BRCA1/2, TP53), mismatch repair gene mutations (e.g., MLH1, MSH2), and dysregulated epigenetic profiles. This narrative review covers the most recent research on prognostic markers of cancer in infertile men. These include molecular biomarkers such as genetic, epigenetic, and proteomic signatures; endocrine and hormonal profiles; and clinical predictors such as azoospermia, severe oligozoospermia, and a history of cryptorchidism. The possibility of incorporating these indicators into risk stratification models for precision medicine and early cancer surveillance is highlighted. For this high-risk group, bridging the domains of andrology and oncology may allow for better counseling, earlier detection, and focused therapies.
1. Introduction
Approximately 40–50% of infertility cases are due to male factors, making it a global health concern that affects 15% of couples of reproductive age. While male infertility has traditionally been regarded as a reproductive disorder, emerging evidence now identifies it as an early marker of systemic disease, particularly malignancy. This review uniquely bridges the fields of andrology and oncology by synthesizing molecular, hormonal, and clinical predictors of cancer risk among infertile men, aiming to highlight translational opportunities for precision-based early cancer surveillance.
Male infertility is a complex condition with congenital, genetic, endocrine, environmental, and idiopathic determinants [1]. Although impaired male fertility has long been viewed primarily as a reproductive health problem, there is growing recognition that it can also serve as a clinical warning sign of systemic disease, associated with higher morbidity and mortality. Among these systemic risks, cancer represents one of the most significant and clinically relevant correlations [2].
According to epidemiological research, males who are infertile, especially those who have azoospermia or severe oligozoospermia, are more likely to develop cancer than their fertile counterparts [3]. Reports from large cohort studies have indicated a two- to three-fold increased relative risk, particularly for testicular germ cell tumors (the strongest association), hematological malignancies, and to a lesser extent, prostate cancer [4]. Common genetic and molecular pathways lend biological plausibility to this association: chromosomal abnormalities like Y-chromosome microdeletions in AZF regions, tumor suppressor gene mutations (e.g., TP53, RB1), and germline defects in DNA repair (e.g., MLH1, MSH2, MSH6, BRCA1/2) have all been linked to both impaired spermatogenesis and carcinogenesis [5]. Furthermore, systemic genomic instability may be reflected in altered sperm epigenetic profiles, such as aberrant DNA methylation and imprinting mistakes, which could predispose affected men to cancer in later life [6,7].
Infertility may offer a special window of opportunity for early cancer risk detection from a clinical standpoint [8,9]. In many andrology clinics, the diagnostic workup already includes genetic testing, hormone profile, and semen analysis. Implementing customized surveillance systems and risk categorization may be made possible by combining this data with newly discovered biomarkers [10]. Nevertheless, there is now no standardized method for screening for cancer in infertile males, and there is still little use of research findings in clinical settings, despite mounting evidence [11,12].
This narrative review aims to synthesize the existing data on prognostic markers of cancer in infertile men to bridge the domains of andrology and oncology. In addition to summarizing clinical, hormonal, and genetic biomarkers with possible prognostic significance, we also examine epidemiological data and emphasize common pathophysiological pathways. To enhance early cancer identification and improve clinical outcomes in this at-risk population, we conclude by discussing the implications for risk stratification, screening techniques, and future research prospects.
2. Methods
This study was intended to synthesize the most recent data on predictive markers of cancer in infertile males. It was structured as a narrative review. The following keyword combinations were used in a thorough literature search up to August 2025 in PubMed/MEDLINE, Scopus, and Web of Science: male infertility, azoospermia, oligozoospermia, cancer risk, testicular cancer, prostate cancer, hematologic malignancies, genetic biomarkers, epigenetics, and DNA repair. Additional research was found by screening the reference lists of pertinent papers.
Preclinical and clinical research, such as genetic association studies, case–control studies, epidemiological cohorts, and mechanistic studies, were taken into account. Systematic reviews, meta-analyses, large population-based research, and high-quality observational cohorts were prioritized. Single case reports, conference abstracts without full text, and articles not published in English were not included.
An official risk-of-bias assessment and meta-analysis were not conducted due to the narrative design. To emphasize important epidemiological correlations, common biological pathways, and new prognostic indicators, the findings were instead critically evaluated and compiled. Evidence with translational significance to clinical practice and cancer risk assessment was given special attention.
3. Male Infertility and Cancer Risk: The Evidence
Over the past 20 years, several extensive population-based studies have provided evidence supporting the link between male infertility and an elevated risk of cancer [13,14]. Scandinavian registries provided the first evidence that males with low-quality semen had a markedly increased risk of testicular germ cell tumors (TGCTs) in comparison to fertile controls. The range of cancers linked to infertility has been broadened by more recent studies, and now includes hematologic, colorectal, prostate, and melanoma cancers [12,15].
3.1. Testicular Cancer
The cancer that is most frequently associated with infertility is testicular germ cell tumor [15]. Over 30,000 men were assessed for infertility as part of a historic Danish cohort study, and among those with aberrant semen characteristics, the standardized incidence ratio (SIR) for testicular cancer was 1.6 (95% CI: 1.3–1.9). In comparison to the general population, the risk was almost three times higher for azoospermic men [16]. Given that germ cell cancers and spermatogenesis disorders share embryonic origins and may both result from testicular dysgenesis syndrome (TDS), which includes cryptorchidism, hypospadias, and decreased Leydig/Sertoli cell activity, this substantial relationship makes biological sense [17,18].
3.2. Prostate Cancer
Studies on the risk of prostate cancer in infertile males have produced conflicting results; some have found a higher risk, while others have suggested a decreased risk because of less exposure to androgen [19]. A twofold higher incidence of high-grade prostate cancer (Gleason score ≥8) but not of low-grade illness was found in a large US study involving over 76,000 infertile men. Even though later research has yielded contradictory results, it is still possible that infertility might be a sign of aggressive prostate cancer biology because oncogenesis and spermatogenic failure are both caused by common DNA repair deficits (such as BRCA2 mutations) [20].
Research on the risk of prostate cancer in guys who are infertile has yielded mixed findings; some indicate a higher risk, while others suggest a lower risk, maybe as a result of a decreased lifetime exposure to androgen. In contrast to Wirén et al. (2013) and Laukhtina et al. (2021), who found either no association or a slightly lower risk in population-based cohorts, Walsh et al. (2010) discovered a twofold greater incidence of high-grade prostate cancer among infertile males. Differences in cohort design, definitions of infertility, and confounding by age or hormonal milieu could all contribute to this discrepancy [19,20,21].
One significant moderator of this association is advanced age. Infertility is rarely a direct result of prostate pathology in this situation because infertility is normally identified decades earlier, whereas prostate cancer usually starts in the sixth decade of life [21]. Instead, OS, metabolic syndrome, and cumulative DNA damage are examples of age-related comorbidities that may affect spermatogenesis on their own and then contribute to prostate carcinogenesis. Therefore, infertility might be an early indicator of systemic genomic instability that occurs before age-related prostate cancer rather than arising as its consequence [22].
3.3. Hematologic and Other Malignancies
Men with poor semen quality had higher rates of hematologic malignancies, such as multiple myeloma, acute myeloid leukemia, and non-Hodgkin lymphoma, according to several registry-based studies [13,23]. Furthermore, albeit with smaller effect sizes and less consistent evidence, elevated risks have been noted for bladder cancer, thyroid cancer, colorectal cancer, and melanoma [24,25]. Together, these results imply that male infertility may not only be related to urogenital cancers but also represent a systemic propensity to cancer. Table 1 summarizes the major findings of important epidemiological research that link male infertility to cancer risk [11].

Table 1.
Summary of key mechanisms linking male infertility with increased cancer risk, highlighting major findings, representative genes or pathways, and their clinical implications.
3.4. Mortality and Longitudinal Outcomes
According to reports, infertile males had a lower life expectancy and a higher all-cause mortality rate than their fertile counterparts, in addition to incident cancer diagnoses [35]. Those with azoospermia experience the greatest burden, showing a ~2.2-fold higher risk of premature death, largely from malignancy [36]. These findings underscore the need to recognize infertility not merely as a reproductive limitation but as an early clinical signal of systemic disease, warranting long-term oncologic and metabolic surveillance.
5. Prognostic Indicators of Cancer Risk in Infertile Men
A thorough strategy that incorporates clinical traits, hormone profiles, semen measurements, and molecular indicators is needed to identify infertile men who are at higher risk for cancer. In cancer and andrology clinics, prognostic indications can direct counseling, early surveillance, and risk classification [80,81].
5.1. Clinical Indicators
Among infertile men, there is a clear correlation between certain clinical characteristics and an increased risk of cancer. The risk of testicular and hematologic cancers is two to three times higher in individuals with significant spermatogenic abnormalities, especially azoospermia and severe oligozoospermia [14]. A history of testicular dysgenesis syndrome, hypospadias, or cryptorchidism increases risk further since these conditions represent developmental abnormalities that predispose to poor spermatogenesis and malignancy. Comorbid conditions like metabolic syndrome and advanced age upon infertility diagnosis may also have prognostic significance [82,83].
5.2. Hormonal Profiles
Indirect indicators of underlying systemic or testicular pathology may be found in endocrine parameters. Reduced spermatogenesis is associated with elevated FSH and LH levels, which are suggestive of early testicular failure. They may also indicate ongoing death of germ cells and genomic stress. While aberrant cell proliferation may be a result of altered estrogen/testosterone ratios, low blood testosterone has been variably associated with aggressive prostate cancer phenotypes as well as infertility. These hormone measurements can improve risk prediction models when paired with clinical data [84,85].
5.3. Semen Parameters
Semen analysis, which offers predictive information beyond reproductive capacity, is still the mainstay of evaluating male infertility. Cancer risk has been linked to sperm concentration, motility, and morphology; the most severe abnormalities (azoospermia, severe oligozoospermia) are associated with the highest risk. Oxidative damage and increased sperm DNA fragmentation may also serve as early molecular markers of genomic instability that coincide with cancer susceptibility [86,87].
5.4. Genetic Biomarkers
Men with an inherited propensity for cancer can be identified by genetic screening. In addition to impairing spermatogenesis, mutations in the BRCA2, CHEK2, ATM, TP53, RB1, and MMR genes (MLH1, MSH2, MSH6, PMS2) significantly increase the risk of developing cancer [88,89]. Chromosome abnormalities such as Y-chromosome AZF microdeletions and Klinefelter syndrome (47,XXY) are strongly linked to infertility and specific cancers. For males who have a family history of cancer or severe, idiopathic infertility, genetic assessment may be especially helpful [90,91].
5.5. Epigenetic and Molecular Biomarkers
Systemic genomic instability is also reflected in epigenetic markers such as dysregulated piRNAs, altered histone-to-protamine ratios, and aberrant DNA methylation at imprinted loci (H19, MEST) [92,93]. Although they are still mostly in the research stage, proteomic and metabolomic patterns in seminal plasma are being investigated as possible indicators of early cancer risk. Precision risk stratification may become possible in the future if these molecular data are integrated with clinical and genetic indications [94,95,96].
5.6. Toward a Risk Stratification Model
A multi-parametric risk score that incorporates clinical, hormonal, genetic, and molecular markers could be a useful method for detecting high-risk infertile males [97]. Men who have pathogenic germline mutations, aberrant hormonal profiles, or severe spermatogenic abnormalities may be given preference for specialized surveillance programs that include hematologic examination, PSA monitoring, or testicular imaging. A paradigm like this would allow for early intervention, bridge the gap between oncology and andrology, and enhance long-term results [98,99]. Collectively, these parameters can be integrated into multiparametric models to improve cancer risk prediction among infertile men (Table 2).

Table 2.
Prognostic indicators of cancer among infertile men.
6. Translational and Clinical Implications
6.1. Predictive Biomarkers in Male Infertility
Early adulthood is a common time for male infertility examinations, which is a useful chance to identify those who are more likely to develop cancer before symptoms appear [121]. Semen analysis, hormonal profiling, and, in certain situations, genetic testing is already part of the diagnostic process for infertile males. These studies offer predictive data pertinent to systemic health in addition to assisting with reproductive counseling. Therefore, routine reproductive examinations could become more comprehensive health surveillance platforms if cancer risk assessment is included into infertility clinics [122,123]. In particular, high-risk populations of men who have pathogenic germline mutations, aberrant hormonal profiles, or severe spermatogenic abnormalities may need early screening. For instance, men with BRCA2 or mismatch repair gene mutations may need more thorough screening for prostate and colorectal cancer, whereas azoospermic males with increased gonadotropins or Y-chromosome microdeletions may benefit from testicular imaging and routine surveillance.
6.2. Counseling and Ethical Considerations
Important counseling and ethical issues are brought up when cancer susceptibility is discovered during an infertility evaluation [124]. Conversations on hereditary cancer syndromes or long-term cancer risk may come as a surprise to patients looking for fertility solutions. Thus, clinicians need to give patients balanced information, outlining the significance of aberrant findings for both reproduction and cancer [125]. Careful pre-test counseling is necessary for genetic testing, in particular, to address the potential for incidental discoveries, psychosocial discomfort, and family member consequences [126]. The advantages of early detection should be emphasized in informed consent, but so should the drawbacks of predictive testing and the possibility of error in risk assessments. To ensure that males and their partners can make informed choices without excessive worry or stigmatization, it is crucial to establish proper communication mechanisms [127].
6.3. Surveillance and Early Detection Strategies
The translation of prognostic markers into practice requires structured surveillance algorithms [128]. Men harboring BRCA2 or MMR mutations may benefit from earlier prostate-specific antigen (PSA) testing or colonoscopic screening, whereas azoospermic men with Y-chromosome deletions could undergo periodic testicular ultrasonography and serum tumor-marker assessment. Integrating these evaluations within fertility clinics provides a practical platform for early cancer detection before symptomatic onset.
Emerging liquid-biopsy and multi-omics assays of seminal plasma may further refine such precision-based surveillance. Prostate-specific antigen monitoring for men with pathogenic BRCA2 variants, testicular ultrasound and tumor marker evaluation for men at high risk of testicular cancer, and hematological evaluations for those with severe spermatogenic failure and inexplicable systemic symptoms are a few examples [129].
To prevent overdiagnosis and unnecessary interventions, surveillance must be tailored to each individual’s risk profile. Personalized and cost-effective programs are possible using precision medicine techniques that integrate clinical, hormonal, and molecular indications into risk classification models [130,131]. Finally, the need for a thorough long-term health-management plan that goes beyond cancer surveillance has been highlighted by the growing correlations between infertility and cardiometabolic disease and premature mortality [132,133].
6.4. Multidisciplinary Collaboration and Health System Needs
Coordinated care across disciplines is necessary for the successful implementation of cancer risk assessment among infertile men. Though they are in a unique position to recognize men who are at risk, andrologists frequently need to refer patients to primary care physicians, genetic counselors, and oncologists for appropriate management [134,135]. The creation of integrated care pathways can guarantee that prognostic markers found in the fertility clinic are converted into useful monitoring and prevention plans. To change the perspective of infertility from a solely reproductive problem to a sign of systemic health vulnerability, awareness campaigns and professional education are required at the health system level [136,137]. The development of evidence-based screening guidelines and the improvement of risk models will also require investments in registries and data-sharing programs. Ultimately, improving reproductive outcomes and promoting cancer prevention and early diagnosis in a high-risk but underappreciated group are two benefits of bridging the andrology-oncology divide [138,139].
7. Future Directions and Research Gaps
Although substantial progress has been made in elucidating the connection between male infertility and cancer, significant gaps remain in both mechanistic understanding and clinical translation. To go from association to causality and from prediction to prevention, these gaps must be filled [80,140].
7.1. Future Directions and Research Gaps
There is still little prospective evidence linking male infertility to cancer, although several registry and retrospective studies indicate this link. The complexity of spermatogenic dysfunction and its evolution over time may not be adequately captured by the majority of existing data, which rely on semen characteristics at a single time point [14,141]. There is an urgent need for longitudinal cohort studies that include regular semen testing, uniform definitions of infertility, and long-term follow-up for cancer outcomes. Such investigations would shed light on whether infertility is a reflection of underlying genetic predispositions or if it predicts cancer on its own [14,142]. Identifying temporal trends, such as whether certain cancers develop preferentially during particular time windows after an infertility diagnosis, would also be made possible by them [143].
7.2. Multi-Omics and Biomarker Discovery
Advances in genomics, transcriptomics, epigenomics, proteomics, and metabolomics provide unprecedented opportunities to unravel the biological links between impaired spermatogenesis and oncogenesis [144,145]. Novel biomarkers that not only reveal common biological pathways but also more precisely stratify cancer risk than clinical signs alone may be found using multi-omics techniques [146,147]. Proteomic profiles of seminal plasma or epigenomic signals in sperm DNA, for instance, could be early markers of systemic genomic instability. Before these potential biomarkers are used in clinical settings and across a range of demographics, they must first be thoroughly validated. One of the main challenges for the upcoming ten years of study will be to ensure clinical utility and reproducibility [148,149].
7.3. Emerging Technologies for Surveillance
Early cancer detection in infertile men may be possible thanks to advancements in non-invasive diagnostics. Techniques for liquid biopsies, such as the detection of cell-free DNA (cfDNA) and circulating tumor DNA (ctDNA), may offer sensitive indicators of occult cancer [150,151]. Similarly, RNA profiles and extracellular vesicles produced from sperm may be readily available biomarkers of systemic illness. These technologies are still in the experimental stage, but they have the potential to lessen dependence on invasive procedures and supplement traditional surveillance approaches. To evaluate patient acceptance, cost-effectiveness, and feasibility in relation to cancer risk associated with infertility, early pilot studies are required [152,153].
7.4. Artificial Intelligence and Predictive Models
Clinicians have difficulties due to the intricacy of combining clinical, hormonal, genetic, and molecular data. By making it possible to create multivariate prediction models, artificial intelligence and machine learning techniques present viable remedies [154,155]. These tools could create individualized surveillance suggestions and categorize infertile men into risk groups. Large infertility registries, for example, may teach machines to spot patterns that traditional statistical techniques would miss. However, to guarantee fair and clinically significant results, the use of AI in this field would necessitate strong datasets, close attention to algorithmic openness, and anti-bias measures [156].
7.5. Clinical Guidelines and Ethical Frameworks
There are currently no established standards for cancer screening in infertile males, despite mounting evidence. To create evidence-based recommendations, professional associations in cancer, urology, and andrology will need to work together internationally [21]. Guidelines must cover the psychological and ethical ramifications of predictive testing in addition to who should be examined and how frequently. Ethical frameworks will be crucial for handling incidental findings, protecting privacy, and facilitating well-informed decision-making as genomic technologies are progressively incorporated into fertility treatment [157]. The possible advantages of early detection must ultimately be weighed against the dangers of overdiagnosis and patient distress in practical application [158].
8. Conclusions
There is strong evidence that male infertility is a systemic health sign and that it is associated with an increased risk of cancer. Both infertility and carcinogenesis are caused by similar biological processes, such as chromosomal abnormalities, epigenetic instability, and problems in DNA repair. Promising methods for identifying males who are most at risk include clinical, hormonal, and molecular indications.
Utilizing these findings for the benefit of patients requires a bridge between oncology and andrology. Clinicians can advance earlier cancer identification, better counseling, and focused therapies by incorporating prognostic indications into risk stratification and monitoring plans. Therefore, infertility presents a crucial window of opportunity to improve long-term health outcomes for this susceptible population and advance precision medicine.
Despite mounting evidence, a number of obstacles lie in the way of practical translation, including a lack of standardized biomarkers, a small number of prospective cohorts, and ethical issues with predictive screening. Future developments will involve the creation of worldwide guidelines, AI-driven multi-omics integration, and customized cancer surveillance in infertility clinics bridging oncology and andrology. These trends will transform male infertility evaluation into a gateway for proactive health surveillance.
Author Contributions
Conceptualization, A.Z. (Athanasios Zachariou) and E.M.; methodology, M.F. and A.Z. (Athanasios Zikopoulos); formal analysis, N.M. and T.G.; investigation, E.M., M.F., M.T. and N.T.; data curation, A.P. and S.S.; writing—original draft preparation, A.Z. (Athanasios Zachariou) and E.M.; writing—review and editing, M.F., A.Z. (Athanasios Zikopoulos), A.P., N.M., T.G., M.T., N.T., N.K., E.D. and S.S.; visualization, E.M.; supervision, A.Z. (Athanasios Zachariou), and S.S.; project administration, S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data was created or analyzed in this study. Data sharing in not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| TGCTs | Testicular Germ Cell Tumors |
| SIR | Standardized Incidence Ratio |
| piRNAs | Piwi-interacting RNAs |
| OS | Oxidative Stress |
| ROS | Reactive Oxygen Species |
| DNMTs | DNA-methyltransferases |
| PSA | Prostate-specific antigen |
| cfDNA | Cell-free DNA |
References
- Leslie, S.W.; Soon-Sutton, T.L.; Khan, M.A. Male Infertility. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: http://www.ncbi.nlm.nih.gov/books/NBK562258/ (accessed on 12 August 2024).
- Gül, M.; Russo, G.I.; Kandil, H.; Boitrelle, F.; Saleh, R.; Chung, E.; Kavoussi, P.; Mostafa, T.; Shah, R.; Agarwal, A. Male Infertility: New Developments, Current Challenges, and Future Directions. World J. Men’s Health 2024, 42, 502–517. [Google Scholar] [CrossRef]
- Huyghe, E.; Chiu, P.K.F. Health risks associated with infertility and non-obstructive azoospermia. Asian J. Androl. 2025, 27, 428–432. [Google Scholar] [CrossRef]
- Gann, P.H. Risk factors for prostate cancer. Rev. Urol. 2002, 4 (Suppl. S5), S3–S10. [Google Scholar]
- Broustas, C.G.; Lieberman, H.B. DNA damage response genes and the development of cancer metastasis. Radiat. Res. 2014, 181, 111–130. [Google Scholar] [CrossRef]
- Chiba, H.; Hiura, H.; Okae, H.; Miyauchi, N.; Sato, F.; Sato, A.; Arima, T. DNA methylation errors in imprinting disorders and assisted reproductive technology. Pediatr. Int. 2013, 55, 542–549. [Google Scholar] [CrossRef]
- Adetunji, A.O.; Owusu, H.; Adewale, E.F.; Adesina, P.A.; Xedzro, C.; Saliu, T.P.; Islam, S.; Zhu, Z.; Morenikeji, O.B. DNA Methylation: A Key Regulator in Male and Female Reproductive Outcomes. Life 2025, 15, 1109. [Google Scholar] [CrossRef] [PubMed]
- Venn, A.; Healy, D.; McLachlan, R. Cancer risks associated with the diagnosis of infertility. Best Pract. Res. Clin. Obstet. Gynaecol. 2003, 17, 343–367. [Google Scholar] [CrossRef] [PubMed]
- Kroener, L.; Dumesic, D.; Al-Safi, Z. Use of fertility medications and cancer risk: A review and update. Curr. Opin. Obstet. Gynecol. 2017, 29, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Krzastek, S.C.; Smith, R.P.; Kovac, J.R. Future diagnostics in male infertility: Genomics, epigenetics, metabolomics and proteomics. Transl. Androl. Urol. 2020, 9 (Suppl. S2), S195–S205. [Google Scholar] [CrossRef]
- Behboudi-Gandevani, S.; Bidhendi-Yarandi, R.; Panahi, M.H.; Vaismoradi, M. A Systematic Review and Meta-Analysis of Male Infertility and the Subsequent Risk of Cancer. Front. Oncol. 2021, 11, 696702. [Google Scholar] [CrossRef]
- Maiolino, G.; Fernández-Pascual, E.; Ochoa Arvizo, M.A.; Vishwakarma, R.; Martínez-Salamanca, J.I. Male Infertility and the Risk of Developing Testicular Cancer: A Critical Contemporary Literature Review. Medicina 2023, 59, 1305. [Google Scholar] [CrossRef]
- Hanson, B.M.; Eisenberg, M.L.; Hotaling, J.M. Male infertility: A biomarker of individual and familial cancer risk. Fertil. Steril. 2018, 109, 6–19. [Google Scholar] [CrossRef]
- Nagirnaja, L.; Aston, K.I.; Conrad, D.F. Genetic intersection of male infertility and cancer. Fertil. Steril. 2018, 109, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Rajpert-De Meyts, E.; Aksglaede, L.; Bandak, M.; Toppari, J.; Jørgensen, N. Testicular Cancer: Pathogenesis, Diagnosis and Management with Focus on Endocrine Aspects. In Endotext [Internet]; Feingold, K.R., Ahmed, S.F., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: http://www.ncbi.nlm.nih.gov/books/NBK278992/ (accessed on 3 October 2025).
- Jacobsen, R.; Bostofte, E.; Engholm, G.; Hansen, J.; Olsen, J.H.; Skakkebaek, N.E.; Moller, H. Risk of testicular cancer in men with abnormal semen characteristics: Cohort study. BMJ 2000, 321, 789–792. [Google Scholar] [CrossRef]
- Hu, G.X.; Lian, Q.Q.; Ge, R.S.; Hardy, D.O.; Li, X.K. Phthalate-induced testicular dysgenesis syndrome: Leydig cell influence. Trends Endocrinol. Metab. TEM 2009, 20, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.M.; Skakkebaek, N.E. Testicular dysgenesis syndrome: Mechanistic insights and potential new downstream effects. Fertil. Steril. 2008, 89, e33–e38. [Google Scholar] [CrossRef]
- Wirén, S.M.; Drevin, L.I.; Carlsson, S.V.; Akre, O.; Holmberg, E.C.; Robinson, D.E.; Garmo, H.G.; Stattin, P.E. Fatherhood status and risk of prostate cancer: Nationwide, population-based case-control study. Int. J. Cancer 2013, 133, 937–943. [Google Scholar] [CrossRef]
- Walsh, T.J.; Schembri, M.; Turek, P.J.; Chan, J.M.; Carroll, P.R.; Smith, J.F.; Eisenberg, M.L.; Van Den Eeden, S.K.; Croughan, M.S. Increased risk of high-grade prostate cancer among infertile men. Cancer 2010, 116, 2140–2147. [Google Scholar] [CrossRef]
- Laukhtina, E.; Mori, K.; Pradere, B.; Shariat, S.F. Association between male infertility and prostate cancer: A systematic review and meta-analysis. Curr. Opin. Urol. 2021, 31, 346–353, Erratum in Curr. Opin. Urol. 2025, 35, 123. [Google Scholar] [CrossRef]
- Kaufman, J.M.; Lapauw, B.; Mahmoud, A.; T’Sjoen, G.; Huhtaniemi, I.T. Aging and the Male Reproductive System. Endocr. Rev. 2019, 40, 906–972. [Google Scholar] [CrossRef] [PubMed]
- Buonacquisto, A.; Del Principe, M.I.; Pallotti, F.; Bianchini, S.; Buzzatti, E.; Caponecchia, L.; Chiaretti, S.; Cicolani, G.; Conflitti, A.C.; Di Chiano, S.; et al. Semen quality in acute leukemia patients: A retrospective study. Ann. Hematol. 2025, 104, 4071–4080. [Google Scholar] [CrossRef] [PubMed]
- Melku, M.; Best, O.G.; Winter, J.M.; Thurgood, L.A.; Ahmed, M.; Kichenadasse, G.; Mittinty, M.; Wassie, M.M.; Symonds, E.L. Incidence, Risk and Trends of Multiple Primary Cancers in Patients With Colorectal Cancer: Evidence From the South Australian Cancer Registry. Cancer Med. 2025, 14, e70984. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Bi, X.; Pan, D.; Chen, Y.; Carling, T.; Ma, S.; Udelsman, R.; Zhang, Y. The risk of second cancers after diagnosis of primary thyroid cancer is elevated in thyroid microcarcinomas. Thyroid Off. J. Am. Thyroid Assoc. 2013, 23, 575–582. [Google Scholar] [CrossRef]
- Valkna, A.; Juchnewitsch, A.G.; Põlluaas, L.; Lillepea, K.; Tjagur, S.; Dutta, A.; Pomm, K.; Punab, M.; Laan, M. Significantly increased load of hereditary cancer-linked germline variants in infertile men. Hum. Reprod. Open 2025, 2025, hoaf008. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.M.; Demidova, E.V.; Lesh, R.W.; Hall, M.J.; Daly, M.B.; Meyer, J.E.; Edelman, M.J.; Arora, S. Therapeutic implications of germline vulnerabilities in DNA repair for precision oncology. Cancer Treat. Rev. 2022, 104, 102337. [Google Scholar] [CrossRef]
- Rotondo, J.C.; Lanzillotti, C.; Mazziotta, C.; Tognon, M.; Martini, F. Epigenetics of Male Infertility: The Role of DNA Methylation. Front. Cell Dev. Biol. 2021, 9, 689624. [Google Scholar] [CrossRef]
- Nicu, A.T.; Medar, C.; Chifiriuc, M.C.; Gradisteanu Pircalabioru, G.; Burlibasa, L. Epigenetics and Testicular Cancer: Bridging the Gap Between Fundamental Biology and Patient Care. Front. Cell Dev. Biol. 2022, 10, 861995. [Google Scholar] [CrossRef]
- Rehman, S.; Usman, Z.; Rehman, S.; AlDraihem, M.; Rehman, N.; Rehman, I.; Ahmad, G. Endocrine disrupting chemicals and impact on male reproductive health. Transl. Androl. Urol. 2018, 7, 490–503. [Google Scholar] [CrossRef]
- Sciorio, R.; Greco, P.F.; Greco, E.; Tramontano, L.; Elshaer, F.M.; Fleming, S. Potential effects of environmental toxicants on sperm quality and potential risk for fertility in humans. Front. Endocrinol. 2025, 16, 1545593. [Google Scholar] [CrossRef]
- Faja, F.; Esteves, S.; Pallotti, F.; Cicolani, G.; Di Chiano, S.; Delli Paoli, E.; Lenzi, A.; Lombardo, F.; Paoli, D. Environmental disruptors and testicular cancer. Endocrine 2022, 78, 429–435. [Google Scholar] [CrossRef]
- Maleknia, M.; Ahmadirad, N.; Golab, F.; Katebi, Y.; Haj Mohamad Ebrahim Ketabforoush, A. DNA Methylation in Cancer: Epigenetic View of Dietary and Lifestyle Factors. Epigenet. Insights 2023, 16, 25168657231199893. [Google Scholar] [CrossRef] [PubMed]
- Den Hond, E.; Tournaye, H.; De Sutter, P.; Ombelet, W.; Baeyens, W.; Covaci, A.; Cox, B.; Nawrot, T.S.; Van Larebeke, N.; D’Hooghe, T. Human exposure to endocrine disrupting chemicals and fertility: A case-control study in male subfertility patients. Environ. Int. 2015, 84, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Del Giudice, F.; Kasman, A.M.; Chen, T.; De Berardinis, E.; Busetto, G.M.; Sciarra, A.; Ferro, M.; Lucarelli, G.; Belladelli, F.; Salonia, A.; et al. The Association between Mortality and Male Infertility: Systematic Review and Meta-analysis. Urology 2021, 154, 148–157. [Google Scholar] [CrossRef]
- Eisenberg, M.L.; Betts, P.; Herder, D.; Lamb, D.J.; Lipshultz, L.I. Increased risk of cancer among azoospermic men. Fertil. Steril. 2013, 100, 681–685. [Google Scholar] [CrossRef]
- López-Gil, L.; Pascual-Ahuir, A.; Proft, M. Genomic Instability and Epigenetic Changes during Aging. Int. J. Mol. Sci. 2023, 24, 14279. [Google Scholar] [CrossRef]
- Requesens, M.; Foijer, F.; Nijman, H.W.; de Bruyn, M. Genomic instability as a driver and suppressor of anti-tumor immunity. Front. Immunol. 2024, 15, 1462496. [Google Scholar] [CrossRef] [PubMed]
- Elías-Llumbet, A.; Lira, S.; Manterola, M. Male aging in germ cells: What are we inheriting? Genet. Mol. Biol. 2025, 47 (Suppl. S1), e20240052. [Google Scholar] [CrossRef]
- Borbiev, T.; Babcock, K.; Sinopole, K.; Chesnut, G.T.; Petrovics, G. Ancestry-Specific DNA Damage Repair Gene Mutations and Prostate Cancer. Cancers 2025, 17, 682. [Google Scholar] [CrossRef]
- Pallatt, S.; Nambidi, S.; Adhikary, S.; Banerjee, A.; Pathak, S.; Duttaroy, A.K. A brief review of Lynch syndrome: Understanding the dual cancer risk between endometrial and colorectal cancer. Oncol. Rev. 2025, 19, 1549416. [Google Scholar] [CrossRef]
- Bhattacharya, P.; Leslie, S.W.; McHugh, T.W. Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer). In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK431096/ (accessed on 3 October 2025).
- Ibrahim, M.; Yadav, S.; Ogunleye, F.; Zakalik, D. Male BRCA mutation carriers: Clinical characteristics and cancer spectrum. BMC Cancer 2018, 18, 179. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, T.; Frost, D.; Barrowdale, D.; Evans, D.G.; Bancroft, E.; Adlard, J.; Ahmed, M.; Barwell, J.; Brady, A.F.; Brewer, C.; et al. Prostate Cancer Risks for Male BRCA1 and BRCA2 Mutation Carriers: A Prospective Cohort Study. Eur. Urol. 2020, 77, 24–35. [Google Scholar] [CrossRef]
- Dakal, T.C.; Dhabhai, B.; Pant, A.; Moar, K.; Chaudhary, K.; Yadav, V.; Ranga, V.; Sharma, N.K.; Kumar, A.; Maurya, P.K.; et al. Oncogenes and tumor suppressor genes: Functions and roles in cancers. MedComm 2024, 5, e582. [Google Scholar] [CrossRef]
- Stojchevski, R.; Sutanto, E.A.; Sutanto, R.; Hadzi-Petrushev, N.; Mladenov, M.; Singh, S.R.; Verma, P.; Sengupta, S.; Bhaskar, R.; Avtanski, D. Translational Advances in Oncogene and Tumor-Suppressor Gene Research. Cancers 2025, 17, 1008. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.R.; Bhaskar, R.; Ghosh, S.; Yarlagadda, B.; Singh, K.K.; Verma, P.; Sengupta, S.; Mladenov, M.; Hadzi-Petrushev, N.; Stojchevski, R.; et al. Exploring the Genetic Orchestra of Cancer: The Interplay Between Oncogenes and Tumor-Suppressor Genes. Cancers 2025, 17, 1082. [Google Scholar] [CrossRef]
- Olivier, M.; Hollstein, M.; Hainaut, P. TP53 mutations in human cancers: Origins, consequences, and clinical use. Cold Spring Harb. Perspect. Biol. 2010, 2, a001008. [Google Scholar] [CrossRef]
- Williams, L.A.; Pankratz, N.; Lane, J.; Krailo, M.; Roesler, M.; Richardson, M.; Frazier, A.L.; Amatruda, J.F.; Poynter, J.N. Klinefelter syndrome in males with germ cell tumors: A report from the Children’s Oncology Group. Cancer 2018, 124, 3900–3908. [Google Scholar] [CrossRef]
- Blackburn, J.; Ramakrishnan, A.; Graham, C.; Bambang, K.; Sriranglingam, U.; Senniappan, S. Klinefelter Syndrome: A Review. Clin. Endocrinol. 2025, 102, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Koh, E.; Sin, H.S.; Fukushima, M.; Namiki, M. Azoospermia factor and male infertility. Reprod. Med. Biol. 2010, 9, 129–137. [Google Scholar] [CrossRef]
- Colaco, S.; Modi, D. Genetics of the human Y chromosome and its association with male infertility. Reprod. Biol. Endocrinol. RBE 2018, 16, 14. [Google Scholar] [CrossRef] [PubMed]
- Jazayeri, M.; Alizadeh, A.; Sadighi, M.; Eftekhari-Yazdi, P.; Sharafi, M.; Shahverdi, A. Underestimated Aspects in Male Infertility: Epigenetics is A New Approach in Men with Obesity or Diabetes: A Review. Int. J. Fertil. Steril. 2022, 16, 132–139. [Google Scholar]
- Hosseini, M.; Khalafiyan, A.; Zare, M.; Karimzadeh, H.; Bahrami, B.; Hammami, B.; Kazemi, M. Sperm epigenetics and male infertility: Unraveling the molecular puzzle. Hum. Genom. 2024, 18, 57. [Google Scholar] [CrossRef]
- Tang, Q.; Pan, F.; Yang, J.; Fu, Z.; Lu, Y.; Wu, X.; Han, X.; Chen, M.; Lu, C.; Xia, Y.; et al. Idiopathic male infertility is strongly associated with aberrant DNA methylation of imprinted loci in sperm: A case-control study. Clin. Epigenet. 2018, 10, 134. [Google Scholar] [CrossRef]
- Ehrlich, M. DNA hypomethylation in cancer cells. Epigenomics 2009, 1, 239–259. [Google Scholar] [CrossRef]
- Netto, G.J.; Nakai, Y.; Nakayama, M.; Jadallah, S.; Toubaji, A.; Nonomura, N.; Albadine, R.; Hicks, J.L.; Epstein, J.I.; Yegnasubramanian, S.; et al. Global DNA hypomethylation in intratubular germ cell neoplasia and seminoma, but not in nonseminomatous male germ cell tumors. Mod. Pathol. 2008, 21, 1337–1344. [Google Scholar] [CrossRef]
- Simon, L.; Castillo, J.; Oliva, R.; Lewis, S.E.M. Relationships between human sperm protamines, DNA damage and assisted reproduction outcomes. Reprod. BioMed. Online 2011, 23, 724–734. [Google Scholar] [CrossRef]
- Punjabi, U.; Goovaerts, I.; Peeters, K.; Van Mulders, H.; De Neubourg, D. Sperm as a Carrier of Genome Instability in Relation to Paternal Lifestyle and Nutritional Conditions. Nutrients 2022, 14, 3155. [Google Scholar] [CrossRef]
- Du, L.; Chen, W.; Zhang, D.; Cui, Y.; He, Z. The functions and mechanisms of piRNAs in mediating mammalian spermatogenesis and their applications in reproductive medicine. Cell. Mol. Life Sci. CMLS 2024, 81, 379. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi Asouri, S.; Aghadavood, E.; Mirzaei, H.; Abaspour, A.; Esmaeil Shahaboddin, M. PIWI-interacting RNAs (PiRNAs) as emerging biomarkers and therapeutic targets in biliary tract cancers: A comprehensive review. Heliyon 2024, 10, e33767. [Google Scholar] [CrossRef] [PubMed]
- Behre, H.M.; Bergmann, M.; Simoni, M.; Tüttelmann, F. Primary Testicular Failure. In Endotext [Internet]; Feingold, K.R., Ahmed, S.F., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: http://www.ncbi.nlm.nih.gov/books/NBK279076/ (accessed on 3 October 2025).
- Parekh, N.V.; Lundy, S.D.; Vij, S.C. Fertility considerations in men with testicular cancer. Transl. Androl. Urol. 2020, 9 (Suppl. S1), S14–S23. [Google Scholar] [CrossRef] [PubMed]
- Alahmar, A.T. Role of Oxidative Stress in Male Infertility: An Updated Review. J. Hum. Reprod. Sci. 2019, 12, 4–18. [Google Scholar] [CrossRef]
- Harding, A.T.; Heaton, N.S. The Impact of Estrogens and Their Receptors on Immunity and Inflammation during Infection. Cancers 2022, 14, 909. [Google Scholar] [CrossRef]
- Chang, S.; Skakkebæk, A.; Gravholt, C.H. Klinefelter Syndrome and medical treatment: Hypogonadism and beyond. Hormones 2015, 14, 531–548. [Google Scholar] [CrossRef] [PubMed]
- Krzastek, S.C.; Farhi, J.; Gray, M.; Smith, R.P. Impact of environmental toxin exposure on male fertility potential. Transl. Androl. Urol. 2020, 9, 2797–2813. [Google Scholar] [CrossRef]
- Tesarik, J. Lifestyle and Environmental Factors Affecting Male Fertility, Individual Predisposition, Prevention, and Intervention. Int. J. Mol. Sci. 2025, 26, 2797. [Google Scholar] [CrossRef]
- Barati, E.; Nikzad, H.; Karimian, M. Oxidative stress and male infertility: Current knowledge of pathophysiology and role of antioxidant therapy in disease management. Cell. Mol. Life Sci. 2020, 77, 93–113. [Google Scholar] [CrossRef] [PubMed]
- Moustakli, E.; Zikopoulos, A.; Katopodis, P.; Dafopoulos, S.; Paraschos, V.S.; Zachariou, A.; Dafopoulos, K. Dietary and Lifestyle Interventions to Mitigate Oxidative Stress in Male and Female Fertility: Practical Insights for Infertility Management-A Narrative Review. Metabolites 2025, 15, 379. [Google Scholar] [CrossRef] [PubMed]
- Puzuka, A.; Alksere, B.; Gailite, L.; Erenpreiss, J. Idiopathic Infertility as a Feature of Genome Instability. Life 2021, 11, 628. [Google Scholar] [CrossRef]
- Mukherjee, S.; Ridgeway, A.D.; Lamb, D.J. DNA mismatch repair and infertility. Curr. Opin. Urol. 2010, 20, 525–532. [Google Scholar] [CrossRef]
- Li, N.; Wang, H.; Zou, S.; Yu, X.; Li, J. Perspective in the Mechanisms for Repairing Sperm DNA Damage. Reprod. Sci. 2025, 32, 41–51. [Google Scholar] [CrossRef]
- Glaviano, A.; Singh, S.K.; Lee, E.H.C.; Okina, E.; Lam, H.Y.; Carbone, D.; Reddy, E.P.; O’Connor, M.J.; Koff, A.; Singh, G.; et al. Cell cycle dysregulation in cancer. Pharmacol. Rev. 2025, 77, 100030. [Google Scholar] [CrossRef]
- Dutta, S.; Sengupta, P.; Slama, P.; Roychoudhury, S. Oxidative Stress, Testicular Inflammatory Pathways, and Male Reproduction. Int. J. Mol. Sci. 2021, 22, 10043. [Google Scholar] [CrossRef]
- Liu, S.; Liu, J.; Wang, Y.; Deng, F.; Deng, Z. Oxidative Stress: Signaling Pathways, Biological Functions, and Disease. MedComm 2025, 6, e70268. [Google Scholar] [CrossRef]
- Baumann, A.A.; Buribayev, Z.; Wolkenhauer, O.; Salybekov, A.A.; Wolfien, M. Epigenomic Echoes-Decoding Genomic and Epigenetic Instability to Distinguish Lung Cancer Types and Predict Relapse. Epigenomes 2025, 9, 5. [Google Scholar] [CrossRef] [PubMed]
- García-Guede, Á.; Vera, O.; Ibáñez-de-Caceres, I. When Oxidative Stress Meets Epigenetics: Implications in Cancer Development. Antioxidants 2020, 9, 468. [Google Scholar] [CrossRef]
- Vega, A.; Baptissart, M.; Caira, F.; Brugnon, F.; Lobaccaro, J.M.A.; Volle, D.H. Epigenetic: A molecular link between testicular cancer and environmental exposures. Front. Endocrinol. 2012, 3, 150. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, P.; Yadav, A.; Kaushik, M.; Dada, R. Cancer risk and male Infertility: Unravelling predictive biomarkers and prognostic indicators. Clin. Chim. Acta 2024, 558, 119670. [Google Scholar] [CrossRef]
- Assidi, M. Infertility in Men: Advances towards a Comprehensive and Integrative Strategy for Precision Theranostics. Cells 2022, 11, 1711. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, H.; Rajpertdemeyts, E.; Main, K.; Skakkebaek, N.; Toppari, J. Testicular dysgenesis syndrome and the development and occurrence of male reproductive disorders. Toxicol. Appl. Pharmacol. 2005, 207, 501–505. [Google Scholar] [CrossRef]
- Schneuer, F.J.; Milne, E.; Jamieson, S.E.; Pereira, G.; Hansen, M.; Barker, A.; Holland, A.J.A.; Bower, C.; Nassar, N. Association between male genital anomalies and adult male reproductive disorders: A population-based data linkage study spanning more than 40 years. Lancet Child Adolesc. Health 2018, 2, 736–743. [Google Scholar] [CrossRef]
- Sengupta, P.; Dutta, S.; Karkada, I.R.; Chinni, S.V. Endocrinopathies and Male Infertility. Life 2021, 12, 10. [Google Scholar] [CrossRef]
- Adamczewska, D.; Słowikowska-Hilczer, J.; Walczak-Jędrzejowska, R. The Fate of Leydig Cells in Men with Spermatogenic Failure. Life 2022, 12, 570. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.C.; Scott, M.; Eisenberg, M.L. Male Fertility as a Proxy for Health. J. Clin. Med. 2024, 13, 5559. [Google Scholar] [CrossRef]
- Khanam, M.; Banerjee, A.; Jerin, J.; Fazyl, M.M. The Study of Semen Quality for Evaluation of Male Factor Infertility. J. Chittagong Med. Coll. Teach. Assoc. 2020, 31, 13–18. [Google Scholar] [CrossRef]
- PDQ Cancer Genetics Editorial Board. Genetics of Prostate Cancer (PDQ®): Health Professional Version. In PDQ Cancer Information Summaries [Internet]; National Cancer Institute (US): Bethesda, MD, USA, 2002. Available online: http://www.ncbi.nlm.nih.gov/books/NBK65784/ (accessed on 3 October 2025).
- Finch, A.; Clark, R.; Vesprini, D.; Lorentz, J.; Kim, R.H.; Thain, E.; Fleshner, N.; Akbari, M.R.; Cybulski, C.; Narod, S.A. An appraisal of genetic testing for prostate cancer susceptibility. NPJ Precis. Oncol. 2022, 6, 43. [Google Scholar] [CrossRef] [PubMed]
- Sha, J.; Huang, G.; Zhang, B.; Wang, X.; Xu, Z.; Zhai, J. Chromosomal abnormalities and Y chromosome microdeletions in infertile men with azoospermia and oligozoospermia in Eastern China. J. Int. Med. Res. 2020, 48, 300060519896712. [Google Scholar] [CrossRef] [PubMed]
- Black, K.; Ølgaard, S.; Khoei, A.A.; Glazer, C.; Ohl, D.A.; Jensen, C.F.S. The Genetic Landscape of Male Factor Infertility and Implications for Men’s Health and Future Generations. Uro 2025, 5, 2. [Google Scholar] [CrossRef]
- Cescon, M.; Chianese, R.; Tavares, R.S. Environmental Impact on Male (In)Fertility via Epigenetic Route. J. Clin. Med. 2020, 9, 2520. [Google Scholar] [CrossRef]
- Babaei, K.; Aziminezhad, M.; Mirzajani, E.; Mozdarani, H.; Sharami, S.H.; Norollahi, S.E.; Samadani, A.A. A critical review of the recent concept of regulatory performance of DNA Methylations, and DNA methyltransferase enzymes alongside the induction of immune microenvironment elements in recurrent pregnancy loss. Toxicol. Rep. 2024, 12, 546–563. [Google Scholar] [CrossRef]
- Zhao, R.; Lu, H.; Yuan, H.; Chen, S.; Xu, K.; Zhang, T.; Liu, Z.; Jiang, Y.; Suo, C.; Chen, X. Plasma proteomic profiles for early detection and risk stratification of non-small cell lung carcinoma: A prospective cohort study with 52,913 participants. Int. J. Cancer 2025, 157, 1577–1589. [Google Scholar] [CrossRef]
- Al-Daffaie, F.M.; Al-Mudhafar, S.F.; Alhomsi, A.; Tarazi, H.; Almehdi, A.M.; El-Huneidi, W.; Abu-Gharbieh, E.; Bustanji, Y.; Alqudah, M.A.Y.; Abuhelwa, A.Y.; et al. Metabolomics and Proteomics in Prostate Cancer Research: Overview, Analytical Techniques, Data Analysis, and Recent Clinical Applications. Int. J. Mol. Sci. 2024, 25, 5071. [Google Scholar] [CrossRef]
- Hamed, M.A.; Wasinger, V.; Wang, Q.; Graham, P.; Malouf, D.; Bucci, J.; Li, Y. Prostate cancer-derived extracellular vesicles metabolic biomarkers: Emerging roles for diagnosis and prognosis. J. Control. Release 2024, 371, 126–145. [Google Scholar] [CrossRef]
- Pozzi, E.; Belladelli, F.; Corsini, C.; Boeri, L.; Capogrosso, P.; Fallara, G.; Candela, L.; Bertini, A.; Cattafi, F.; Raffo, M.; et al. Contemporary Diagnostic Work-Up for Male Infertility: Emphasizing Comprehensive Baseline Assessment. World J. Men’s Health 2025, 43, 265–281. [Google Scholar] [CrossRef]
- Leslie, S.W.; Soon-Sutton, T.L.; Skelton, W.P. Prostate Cancer. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK470550/ (accessed on 3 October 2025).
- Bancroft, E.K.; Page, E.C.; Brook, M.N.; Thomas, S.; Taylor, N.; Pope, J.; McHugh, J.; Jones, A.B.; Karlsson, Q.; Merson, S.; et al. A prospective prostate cancer screening programme for men with pathogenic variants in mismatch repair genes (IMPACT): Initial results from an international prospective study. Lancet Oncol. 2021, 22, 1618–1631. [Google Scholar] [CrossRef]
- Mancini, M.; Carmignani, L.; Gazzano, G.; Sagone, P.; Gadda, F.; Bosari, S.; Rocco, F.; Colpi, G.M. High prevalence of testicular cancer in azoospermic men without spermatogenesis. Hum. Reprod. 2007, 22, 1042–1046. [Google Scholar] [CrossRef] [PubMed]
- Wood, H.M.; Elder, J.S. Cryptorchidism and testicular cancer: Separating fact from fiction. J. Urol. 2009, 181, 452–461. [Google Scholar] [CrossRef]
- Lip, S.Z.L.; Murchison, L.E.D.; Cullis, P.S.; Govan, L.; Carachi, R. A meta-analysis of the risk of boys with isolated cryptorchidism developing testicular cancer in later life. Arch. Dis. Child. 2013, 98, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Song, M.Z.; Ye, L.J.; Xiao, W.Q.; Huang, W.S.; Wen, W.B.; Dai, S.; Lai, L.Y.; Peng, Y.Q.; Wu, T.H.; Sun, Q.; et al. Association of higher serum follicle-stimulating hormone levels with successful microdissection testicular sperm extraction outcomes in nonobstructive azoospermic men with reduced testicular volumes. Asian J. Androl. 2025, 27, 440–446. [Google Scholar] [CrossRef]
- Huddart, R.A.; Norman, A.; Moynihan, C.; Horwich, A.; Parker, C.; Nicholls, E.; Dearnaley, D.P. Fertility, gonadal and sexual function in survivors of testicular cancer. Br. J. Cancer 2005, 93, 200–207. [Google Scholar] [CrossRef]
- Gan, S.; Liu, J.; Chen, Z.; Xiang, S.; Gu, C.; Li, S.; Wang, S. Low serum total testosterone level as a predictor of upgrading in low-risk prostate cancer patients after radical prostatectomy: A systematic review and meta-analysis. Investig. Clin. Urol. 2022, 63, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.; Gu, J.; Meng, Q.H.; Kim, J.; Strom, S.; Davis, J.W.; He, Y.; Wagar, E.A.; Thompson, T.C.; Logothetis, C.J.; et al. Low serum testosterone is associated with tumor aggressiveness and poor prognosis in prostate cancer. Oncol. Lett. 2017, 13, 1949–1957. [Google Scholar] [CrossRef]
- Yao, S.; Till, C.; Kristal, A.R.; Goodman, P.J.; Hsing, A.W.; Tangen, C.M.; Platz, E.A.; Stanczyk, F.Z.; Reichardt, J.K.; Tang, L.; et al. Serum estrogen levels and prostate cancer risk in the prostate cancer prevention trial: A nested case-control study. Cancer Causes Control CCC 2011, 22, 1121–1131. [Google Scholar] [CrossRef]
- Black, A.; Pinsky, P.F.; Grubb, R.L.; Falk, R.T.; Hsing, A.W.; Chu, L.; Meyer, T.; Veenstra, T.D.; Xu, X.; Yu, K.; et al. Sex steroid hormone metabolism in relation to risk of aggressive prostate cancer. Cancer Epidemiol. Biomark. Prev. 2014, 23, 2374–2382. [Google Scholar] [CrossRef]
- Kliesch, S.; Bergmann, M.; Hertle, L.; Nieschlag, E.; Behre, H.M. Semen parameters and testicular pathology in men with testicular cancer and contralateral carcinoma in situ or bilateral testicular malignancies. Hum. Reprod. 1997, 12, 2830–2835. [Google Scholar] [CrossRef]
- Song, S.H.; Lee, T.H.; Her, Y.S.; Oh, M.; Shin, D.H.; Heo, Y.; Kim, D.K.; Kim, D.S. Semen quality and sperm DNA fragmentation in cancer patients undergoing sperm cryopreservation. Investig. Clin. Urol. 2023, 64, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Andrabi, S.W.; Ara, A.; Saharan, A.; Jaffar, M.; Gugnani, N.; Esteves, S.C. Sperm DNA Fragmentation: Causes, evaluation and management in male infertility. JBRA Assist. Reprod. 2024, 28, 306–319. [Google Scholar] [CrossRef]
- Cheng, H.H.; Shevach, J.W.; Castro, E.; Couch, F.J.; Domchek, S.M.; Eeles, R.A.; Giri, V.N.; Hall, M.J.; King, M.C.; Lin, D.W.; et al. BRCA1, BRCA2, and Associated Cancer Risks and Management for Male Patients: A Review. JAMA Oncol. 2024, 10, 1272–1281. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.H.; Liu, S.Y.; Wang, N.; Wu, Y.; Jin, F. Impact of DNA mismatch repair system alterations on human fertility and related treatments. J. Zhejiang Univ. Sci. B 2016, 17, 10–20. [Google Scholar] [CrossRef]
- Nichols, C.R.; Heerema, N.A.; Palmer, C.; Loehrer, P.J.; Williams, S.D.; Einhorn, L.H. Klinefelter’s syndrome associated with mediastinal germ cell neoplasms. J. Clin. Oncol. 1987, 5, 1290–1294. [Google Scholar] [CrossRef]
- Bonouvrie, K.; van der Werff Ten Bosch, J.; van den Akker, M. Klinefelter syndrome and germ cell tumors: Review of the literature. Int. J. Pediatr. Endocrinol. 2020, 2020, 18. [Google Scholar] [CrossRef] [PubMed]
- Amjadian, T.; Yaghmaei, P.; Nasim, H.R.; Yari, K. Impact of DNA methylation of the human mesoderm-specific transcript (MEST) on male infertility. Heliyon 2023, 9, e21099. [Google Scholar] [CrossRef]
- Cannarella, R.; Crafa, A.; Barbagallo, F.; Lundy, S.D.; La Vignera, S.; Condorelli, R.A.; Calogero, A.E. H19 Sperm Methylation in Male Infertility: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2023, 24, 7224. [Google Scholar] [CrossRef]
- Cui, X.; Jing, X.; Wu, X.; Yan, M.; Li, Q.; Shen, Y.; Wang, Z. DNA methylation in spermatogenesis and male infertility. Exp. Ther. Med. 2016, 12, 1973–1979. [Google Scholar] [CrossRef]
- Drabovich, A.P.; Saraon, P.; Drabovich, M.; Karakosta, T.D.; Dimitromanolakis, A.; Hyndman, M.E.; Jarvi, K.; Diamandis, E.P. Multi-omics Biomarker Pipeline Reveals Elevated Levels of Protein-glutamine Gamma-glutamyltransferase 4 in Seminal Plasma of Prostate Cancer Patients. Mol. Cell. Proteom. MCP 2019, 18, 1807–1823. [Google Scholar] [CrossRef] [PubMed]
- Fietz, D.; Sgaier, R.; O’Donnell, L.; Stanton, P.G.; Dagley, L.F.; Webb, A.I.; Schuppe, H.C.; Diemer, T.; Pilatz, A. Proteomic biomarkers in seminal plasma as predictors of reproductive potential in azoospermic men. Front. Endocrinol. 2024, 15, 1327800. [Google Scholar] [CrossRef] [PubMed]
- Duffin, K.; Mitchell, R.T.; Brougham, M.F.H.; Hamer, G.; Van Pelt, A.M.M.; Mulder, C.L. Impacts of cancer therapy on male fertility: Past and present. Mol. Asp. Med. 2024, 100, 101308. [Google Scholar] [CrossRef]
- Pelzman, D.L.; Hwang, K. Genetic testing for men with infertility: Techniques and indications. Transl. Androl. Urol. 2021, 10, 1354–1364. [Google Scholar] [CrossRef] [PubMed]
- Esteves, S.C.; Humaidan, P.; Ubaldi, F.M.; Alviggi, C.; Antonio, L.; Barratt, C.L.R.; Behre, H.M.; Jørgensen, N.; Pacey, A.A.; Simoni, M.; et al. APHRODITE criteria: Addressing male patients with hypogonadism and/or infertility owing to altered idiopathic testicular function. Reprod. Biomed. Online 2024, 48, 103647. [Google Scholar] [CrossRef]
- Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in cancer patients. Fertil. Steril. 2005, 83, 1622–1628. [Google Scholar] [CrossRef]
- Ahsan, M.D.; Levi, S.R.; Webster, E.M.; Bergeron, H.; Lin, J.; Narayan, P.; Nelson, B.B.; Li, X.; Fowlkes, R.K.; Brewer, J.T.; et al. Do people with hereditary cancer syndromes inform their at-risk relatives? A systematic review and meta-analysis. PEC Innov. 2023, 2, 100138. [Google Scholar] [CrossRef]
- Balcom, J.R.; Kotzer, K.E.; Waltman, L.A.; Kemppainen, J.L.; Thomas, B.C. The Genetic Counselor’s Role in Managing Ethical Dilemmas Arising in the Laboratory Setting. J. Genet. Couns. 2016, 25, 838–854. [Google Scholar] [CrossRef]
- Jansen, S.N.G.; Kamphorst, B.A.; Mulder, B.C.; van Kamp, I.; Boekhold, S.; van den Hazel, P.; Verweij, M.F. Ethics of early detection of disease risk factors: A scoping review. BMC Med. Ethics 2024, 25, 25. [Google Scholar] [CrossRef] [PubMed]
- Hauschild, A.C.; Martin, R.; Holst, S.C.; Wienbeck, J.; Heider, D. Guideline for software life cycle in health informatics. iScience 2022, 25, 105534. [Google Scholar] [CrossRef]
- Page, E.C.; Bancroft, E.K.; Brook, M.N.; Assel, M.; Hassan Al Battat, M.; Thomas, S.; Taylor, N.; Chamberlain, A.; Pope, J.; Raghallaigh, H.N.; et al. Interim Results from the IMPACT Study: Evidence for Prostate-specific Antigen Screening in BRCA2 Mutation Carriers. Eur. Urol. 2019, 76, 831–842. [Google Scholar] [CrossRef]
- Goetz, L.H.; Schork, N.J. Personalized medicine: Motivation, challenges, and progress. Fertil. Steril. 2018, 109, 952–963. [Google Scholar] [CrossRef]
- Ho, D.; Quake, S.R.; McCabe, E.R.B.; Chng, W.J.; Chow, E.K.; Ding, X.; Gelb, B.D.; Ginsburg, G.S.; Hassenstab, J.; Ho, C.M.; et al. Enabling Technologies for Personalized and Precision Medicine. Trends Biotechnol. 2020, 38, 497–518. [Google Scholar] [CrossRef]
- Yiallourou, S.R.; Magliano, D.; Haregu, T.N.; Carrington, M.J.; Rolnik, D.L.; Rombauts, L.; Rodrigues, A.; Ball, J.; Bruinsma, F.J.; Da Silva Costa, F. Long term all-cause and cardiovascular disease mortality among women who undergo fertility treatment. Med. J. Aust. 2022, 217, 532–537. [Google Scholar] [CrossRef]
- Blüher, M. An overview of obesity-related complications: The epidemiological evidence linking body weight and other markers of obesity to adverse health outcomes. Diabetes Obes. Metab. 2025, 27 (Suppl. S2), 3–19. [Google Scholar] [CrossRef] [PubMed]
- Grant, A.M.; Taylor, N.; Maguire, J.; de Graves, S.; Signorelli, C.; Fuentes-Bolanos, N.A.; Tucker, K.M.; Cruickshank, M. A coordinated multidisciplinary model of care is needed for child and family centered care in pediatric genetic cancer risk services: A scoping review. Fam. Cancer 2025, 24, 55. [Google Scholar] [CrossRef]
- Berliner, J.L.; Cummings, S.A.; Boldt Burnett, B.; Ricker, C.N. Risk assessment and genetic counseling for hereditary breast and ovarian cancer syndromes-Practice resource of the National Society of Genetic Counselors. J. Genet. Couns. 2021, 30, 342–360. [Google Scholar] [CrossRef] [PubMed]
- Nabhan, A.; Salama, M.; Elsayed, M.; Nawara, M.; Kamel, M.; Abuelnaga, Y.; Ghonim, M.; Elshafeey, F.; Abdelhadi, R.; Gebril, S.; et al. Indicators of infertility and fertility care: A systematic scoping review. Hum. Reprod. Open 2022, 2022, hoac047. [Google Scholar] [CrossRef]
- Sax, M.R.; Lawson, A.K. Emotional Support for Infertility Patients: Integrating Mental Health Professionals in the Fertility Care Team. Women 2022, 2, 68–75. [Google Scholar] [CrossRef]
- Galeș, L.N.; Păun, M.A.; Anghel, R.M.; Trifănescu, O.G. Cancer Screening: Present Recommendations, the Development of Multi-Cancer Early Development Tests, and the Prospect of Universal Cancer Screening. Cancers 2024, 16, 1191. [Google Scholar] [CrossRef]
- Laza, C.; Niño De Guzmán, E.; Gea, M.; Plazas, M.; Posso, M.; Rué, M.; Castells, X.; Román, M. “For and against” factors influencing participation in personalized breast cancer screening programs: A qualitative systematic review until March 2022. Arch. Public Health 2024, 82, 23. [Google Scholar] [CrossRef] [PubMed]
- Pichugova, S.V.; Chereshnev, V.A.; Beikin, Y.B. Characteristic of spermogram parameters in men with reproductive pathology in age-related aspect. Obstet. Gynecol. Reprod. 2022, 15, 715–725. [Google Scholar] [CrossRef]
- Barratt, C.L.R.; Björndahl, L.; De Jonge, C.J.; Lamb, D.J.; Osorio Martini, F.; McLachlan, R.; Oates, R.D.; van der Poel, S.; St John, B.; Sigman, M.; et al. The diagnosis of male infertility: An analysis of the evidence to support the development of global WHO guidance-challenges and future research opportunities. Hum. Reprod. Update 2017, 23, 660–680. [Google Scholar] [CrossRef]
- Wang, S.; Gaskins, A.J.; Farland, L.V.; Zhang, D.; Birmann, B.M.; Rich-Edwards, J.W.; Wang, Y.X.; Tamimi, R.M.; Missmer, S.A.; Chavarro, J.E. A prospective cohort study of infertility and cancer incidence. Fertil. Steril. 2023, 120, 134–142. [Google Scholar] [CrossRef]
- Ghantasala, G.S.P.; Dilip, K.; Vidyullatha, P.; Allabun, S.; Alqahtani, M.S.; Othman, M.; Abbas, M.; Soufiene, B.O. Enhanced ovarian cancer survival prediction using temporal analysis and graph neural networks. BMC Med. Inform. Decis. Mak. 2024, 24, 299. [Google Scholar] [CrossRef]
- Parkes, R.; Garcia, T.X. Bringing proteomics to bear on male fertility: Key lessons. Expert Rev. Proteom. 2024, 21, 181–203. [Google Scholar] [CrossRef] [PubMed]
- Podgrajsek, R.; Hodzic, A.; Stimpfel, M.; Kunej, T.; Peterlin, B. Insight into the complexity of male infertility: A multi-omics review. Syst. Biol. Reprod. Med. 2024, 70, 73–90. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Gómez, G.; Yañez, F.; Soler, Z.; Pons-Tarin, M.; Mayorga, L.; Herrera-deGuise, C.; Borruel, N.; Rodriguez-Sinovas, A.; Consegal, M.; Manjón, I.; et al. Microbiome multi-omics analysis reveals novel biomarkers and mechanisms linked with CD etiopathology. Biomark. Res. 2025, 13, 85. [Google Scholar] [CrossRef]
- Hachem, S.; Yehya, A.; El Masri, J.; Mavingire, N.; Johnson, J.R.; Dwead, A.M.; Kattour, N.; Bouchi, Y.; Kobeissy, F.; Rais-Bahrami, S.; et al. Contemporary Update on Clinical and Experimental Prostate Cancer Biomarkers: A Multi-Omics-Focused Approach to Detection and Risk Stratification. Biology 2024, 13, 762. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Encinas, A.; García-Peiró, A.; Del Rey, J.; Ribas-Maynou, J.; Abad, C.; Amengual, M.J.; Prada, E.; Navarro, J.; Benet, J. Proteomic Analysis in Seminal Plasma of Fertile Donors and Infertile Patients with Sperm DNA Fragmentation. Int. J. Mol. Sci. 2020, 21, 5046. [Google Scholar] [CrossRef]
- Panner Selvam, M.K.; Agarwal, A. Sperm and Seminal Plasma Proteomics: Molecular Changes Associated with Varicocele-Mediated Male Infertility. World J. Men’s Health. 2020, 38, 472–483. [Google Scholar] [CrossRef] [PubMed]
- Medina, J.E.; Dracopoli, N.C.; Bach, P.B.; Lau, A.; Scharpf, R.B.; Meijer, G.A.; Andersen, C.L.; Velculescu, V.E. Cell-free DNA approaches for cancer early detection and interception. J. ImmunoTher. Cancer 2023, 11, e006013. [Google Scholar] [CrossRef]
- Gao, Q.; Zeng, Q.; Wang, Z.; Li, C.; Xu, Y.; Cui, P.; Zhu, X.; Lu, H.; Wang, G.; Cai, S.; et al. Circulating cell-free DNA for cancer early detection. Innovation 2022, 3, 100259. [Google Scholar] [CrossRef] [PubMed]
- Larriba, S.; Vigués, F.; Bassas, L. Using Small Non-Coding RNAs in Extracellular Vesicles of Semen as Biomarkers of Male Reproductive System Health: Opportunities and Challenges. Int. J. Mol. Sci. 2023, 24, 5447. [Google Scholar] [CrossRef]
- Huang, J.; Chen, H.; Li, N.; Liu, P.; Yang, J.; Zhao, Y. Emerging technologies towards extracellular vesicles large-scale production. Bioact. Mater. 2025, 52, 338–365. [Google Scholar] [CrossRef]
- Duong, D.; Solomon, B.D. Artificial intelligence in clinical genetics. Eur. J. Hum. Genet. EJHG 2025, 33, 281–288. [Google Scholar] [CrossRef]
- Salemi, M.H.; Foroozandeh, E.; Ashkzari, M.K. Applications, Challenges, and Future Perspectives of Artificial Intelligence in Psychopharmacology, Psychological Disorders and Physiological Psychology: A Comprehensive Review. J. Pharm. Bioallied Sci. 2025, 17 (Suppl. S1), S229–S233. [Google Scholar] [CrossRef]
- Qaderi, K.; Sharifipour, F.; Dabir, M.; Shams, R.; Behmanesh, A. Artificial intelligence (AI) approaches to male infertility in IVF: A mapping review. Eur. J. Med. Res. 2025, 30, 246. [Google Scholar] [CrossRef]
- Beshir, L. A Framework to Ethically Approach Incidental Findings in Genetic Research. EJIFCC 2020, 31, 302–309. [Google Scholar] [PubMed]
- Piessens, V.; Van den Bruel, A.; Piessens, A.; Van Hecke, A.; Brodersen, J.B.; Lauwerier, E.; Stul, F.; De Sutter, A.; Heytens, S. Do health professionals know about overdiagnosis in screening, and how are they dealing with it? A mixed-methods systematic scoping review. PLoS ONE 2025, 20, e0315247. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).