Abstract
After sperm enter the female reproductive tract, the physicochemical and biochemical microenvironment undergoes significant changes. In particular, the large changes in various ions encountered by sperm may alter the physiology of sperm, ultimately compromising capacitation and fertilization. Thus, the rapid response to environmental variations is vital for sperm functions. For example, Calcium, the most crucial ion for sperm functions, enters into sperm via Ca2+ permeable ion channels. The cation channel of sperm (CatSper) is a sperm-specific, pH-sensitive, and Ca2+-permeable ion channel. It is responsible for the predominant Ca2+ entry in mammalian sperm and is involved in nearly every event of sperm to acquire fertilizing capability. In addition, CatSper also serves as a pivotal polymodal chemosensor in mammalian sperm by responding to multiple chemical cues. Physiological chemicals (such as progesterone, prostaglandins, β-defensins, and odorants) provoke Ca2+ entry into sperm by activating CatSper and thus triggering sperm functions. Additionally, synthetic and natural chemicals (such as medicines, endocrine disrupting chemicals, drugs of abuse, and antioxidants) affect sperm functions by regulating CatSper-dependent Ca2+ signaling. Therefore, understanding the interactions between CatSper and extracellular ligands sheds light on the mechanisms underlying male infertility and offers innovative diagnostic and treatment approaches. This underscores the importance of CatSper as a crucial regulatory target in male reproduction, linking sperm function with the extracellular environment. In conclusion, this review comprehensively summarizes the relevant studies describing the environmental factors that affect CatSper in humans and rodents.
1. Introduction
Mammalian sperm gain their fertilizing capacity after undergoing two vital processes, one in the male reproductive tract, known as epididymal maturation, and the other in the female reproductive tract, known as capacitation [1]. After capacitation, sperm hyperactivate with high-amplitude flagellar beats and vigorous movements to swim across the viscous environment in the female reproductive tract [2]. Meanwhile, multiple chemoattractants related to chemotaxis diffusing from the female reproductive tract to navigate sperm toward oocytes [3]. Later on, sperm become competent to undergo the acrosome reaction, which allows sperm to penetrate the zona pellucida (ZP) glycoprotein surrounding the oocytes. Capacitation is contingent upon the influx of Ca2+ into the sperm cytoplasm from both intracellular organelles and the extracellular environment [4]. During their journey to oocytes, mammalian sperms encounter a large number of physiological changes, especially the exchanges of ions [5]. Among these ions, Ca2+ plays a central role in the regulation of sperm motility, capacitation, hyperactivation, chemotaxis, and acrosome reaction [6]. The changes in sperm function that occur during capacitation depend on a combination of sequential signaling processes where intracellular Ca2+ concentration ([Ca2+]i) plays a central role. From sperm motility to acrosome reaction, [Ca2+]i orchestrates these key events of sperm function in the correct time and order [6]. Interestingly, membrane proteins, such as ion channels, ion transporters, and membrane receptors, play a critical role in these events [6].
Specifically, the cation channel of sperm (CatSper) is a sperm-specific, pH-sensitive, and Ca2+-permeable ion channel [7]. Crucially, this channel is responsible for the predominant Ca2+ entry in mammalian sperm and is involved in nearly every event by which sperm acquire their fertilizing capability. Additionally, ion channels are capable of transporting ions faster than transporters. This allows sperm to respond quickly to guidance cues within the female reproductive tract. Consequently, CatSper enables the translation of large changes in the microenvironment into changes of [Ca2+]i [8]. Although fertilization is at the center of creating new life, it is still a long way from being fully understood. A better understanding of the CatSper channel is important, not only to advance our knowledge of the cause of male infertility but also to inspire improvement in the development of male contraceptives. On one hand, the knockout of genes encoding the CatSper channel in male mice, as well as genetic mutations in CatSper genes in humans, lead to male infertility and the inability of sperm to undergo hyperactivation and to penetrate oocytes. On the other hand, CatSper plays a pivotal role in responding to multiple chemical cues, including physiological chemicals (such as progesterone [P4] and prostaglandins [PGs]), and synthetic and natural chemicals (such as medicines and endocrine disrupting chemicals [EDCs]). Therefore, CatSper is also a pivotal polymodal chemosensor in mammalian sperm [9]. Herein, this review comprehensively summarizes the relevant studies describing the physiological, synthetic, and natural chemicals targeting CatSper in humans and rodents.
2. Overview of CatSper
CatSper is located in the flagellar principal piece [7]. The CatSper complex consists of four pore-forming alpha subunits (CATSPER1–4) and at least eight auxiliary subunits (CATSPERβ, γ, δ, ε, ζ, and θ [10]; EF-hand calcium binding domain 9; and C2 calcium dependent domain containing 6 [11]) [12,13]. These subunits are conserved between mouse and human, and genetic variations in CATSPER1, CATSPER2, CATSPER3, and CATSPERE have been found in infertile men [14,15,16]. These results indicate that CatSper is essential for male fertility in mammals.
Ca2+ is crucial in almost every physiological activity by which sperm acquire their fertilizing capability, including motility, capacitation, hyperactivation, the acrosome reaction, and chemotaxis [4]. The knockout of mouse Catsper genes results in male infertility and a lack of CatSper current and hyperactivated motility in sperm [17,18,19,20]. In humans, CATSPER1 and CATSPER2 mutations have been reported to be involved in asthenoteratozoospermia in men. Their sperm lack the CatSper current, accompanied by lower sperm counts and motility [14,21]. In particular, our recent study found that the copy number variation of CATSPER2 causes idiopathic male infertility with normal semen parameters [15]. The sperm of this patient had very low CATSPER2 protein expression, no CatSper current, and failed to undergo hyperactivation. In addition, a CATSPER-current-deficient infertile man with a homozygous in-frame deletion in CATSPERE showed normal sperm quality but no hyperactivated motility [22,23]. Additionally, CATSPER3 mutations cause male infertility due to the failure of the acrosome reaction, but there were no defects in routine semen parameters [16]. Therefore, CatSper plays a central role in the fertilizing capacity of sperm.
CatSper cooperates with other sperm ion channels, exchangers, and transporters to regulate sperm functions in mammals. Sperm-specific Na+/H+ exchangers transport H+ out of the sperm while transporting Na+ into the sperm plasma membrane, and HV1 expels H+ from sperm, creating an alkaline environment within sperm [24]. Correspondingly, the pH-sensitive CatSper is activated, resulting in Ca2+ influx and the activation of Ca2+-dependent sperm functions. In addition, in mouse sperm, intracellular alkalinization activates KSper, a sperm-specific potassium channel, which further hyperpolarizes the sperm cellular membrane [25]. KSper-dependent membrane hyperpolarization increases the force driving Ca2+ influx through CatSper [26]. In humans, KSper-induced hyperpolarization further affects CatSper [26]. Furthermore, Na+/K+ ATPase α4 functions as transport to maintain the membrane potential and regulate CatSper directly or indirectly [24]. The HCO3− transporters (such as SLC26A3) carry HCO3− into sperm cells to activate soluble adenylyl cyclase and increase the sperm cyclic adenosine monophosphate (cAMP), which can stimulate CatSper in human and mouse sperm [24].
After sperm enter the female reproductive tract, the physicochemical and biochemical microenvironment undergo significant changes. As a result, the response of sperm to environmental factors is vital for successful fertilization. CatSper is a polymodal chemosensor in mammalian sperm. It plays a pivotal role in responding to multiple chemical cues including P4, PGs, cyclic nucleotides, ZP glycoproteins, serum albumin, β-defensins (DEFBs), and neurotransmitters, drugs, traditional Chinese medicine, EDCs, and antioxidants. Consequently, understanding the diverse mechanisms by which extracellular factors regulate CatSper is of the utmost importance.
3. CatSper and Physiological Chemicals
In the microenvironment of the female reproductive tract, many physiological chemicals, such as oviducal hormones, regulate sperm functions and increase [Ca2+]i [8]. In these hormones, P4 and PGs are the best known for the oviducal ligands of CatSper. They are secreted by the oviduct and serve as the predominant hormones in follicular fluid [8]. In addition, several physiological stimuli, including cyclic nucleotides, ZP glycoproteins, serum albumin, DEFBs, neurotransmitters, and odorant attractants, elicit a CatSper-dependent Ca2+ increase [27] (Summarized in Figure 1).
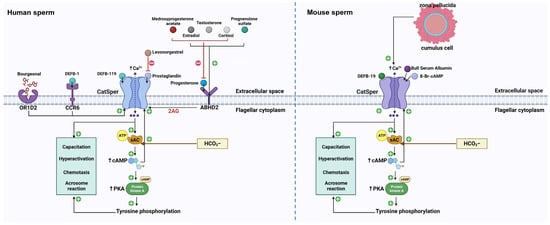
Figure 1.
The signaling pathways of different physiological ligands on mammalian CatSper. In human sperm, the P4 binding on the ABDH2 receptor provokes 2-AG depletion and thus removes the inhibition induced by 2-AG on the CatSper channel. Substantially, CatSper opens and allows the extracellular influx of Ca2+ and elevates the concentration of intracellular Ca2+. The activation of sAC triggered by HCO3− and Ca2+ increase the level of cAMP, which causes activation of PKA and tyrosine kinase. cAMP can also activate CatSper channel. As a result, the tyrosine phosphorylation leads to sperm capacitation, hyperactivation, chemotaxis, and acrosome reaction. Apart from P4, pregnenolone sulfate can complete the same ABDH2 binding sites to activate CatSper. Cortisol, testosterone, as well as estradiol, target the same binding sites of P4 to activate CatSper. The P4-induced CatSper activation is suppressed by these three molecules, while the PGE-induced CatSper activation is inhibited by levonorgestrel. Also, medroxyprogesterone acetate exerts an inhibitory effect on P4-induced CatSper activation. Additionally, DEFB-1 binding on the CCR6 receptor can activate CatSper and induce Ca2+ mobilization. In addition, CatSper is also activated by DEBF-19 and bourgeonal, but OR1D2 is involved in bourgeonal-induced CatSper activation. In mouse sperm, DEFB-19, BSA, as well as 8-BR- cAMP, activate the CatSper channel and induce the mobilization of Ca2+ in mouse sperm. Intracellular Ca2+ and HCO3− can activate sAC and elevate the level of cAMP, leading to the activation of protein kinase A and tyrosine kinases. Thus, the tyrosine phosphorylation initiates a certain process related to sperm function, including sperm capacitation, hyperactivation, chemotaxis, and acrosome reaction. In addition, the interaction between ZP and mouse sperm can elevate intracellular Ca2+, which require the CatSper channel to enter mouse sperm. The solid line with the arrow represents activation and the red line represents inhibition. ABDH2: α/β hydrolase domain containing protein 2, 2-AG: 2-arachidonoylglycerol, CCR6: C-C chemokine receptor, DEFB-1: β-defensins 1, DEFB-119: β-defensins 119, DEFB-19: β-defensins 19, OR1D2: olfactory receptor, sAC: soluble adenylyl cyclase, PKA: protein kinase A, BSA: bull serum albumin, ZP: zona pellucida.
3.1. CatSper and Endogenous Steroids
As sperm travel through the female reproductive tract, they are exposed to a variety of steroid hormones. Human follicular fluid (HFF) present in the female reproductive tract is a key factor for human fertilization; it is present at every stage of impregnation. P4, secreted by the oviductal epithelium and cumulus cells, is the predominant hormone in HFF [8]. P4 can elevate [Ca2+]i of mammalian sperm [28]. However, the activation of CatSper by P4 has only been reported in humans and rhesus macaques [29]. In murine sperm, P4 cannot activate mouse CatSper, although it increases sperm [Ca2+]i [30]. Therefore, CatSper regulation likely occurs via species-specific mechanisms. Under normal physiological conditions, endogenous P4 activates human CatSper through non-genomic actions mediated by the P4/abhydrolase domain containing the 2 (ABHD2)/CatSper/Ca2+ axis. This pathway relies on the coordinated action of ABHD2, a P4 receptor expressed in sperm, and endocannabinoid 2-arachidonoylglycerol (2-AG), an endogenous CatSper inhibitor [31]. P4 binds to ABHD2 and triggers the depletion of 2-AG within the sperm plasma membrane and the release of CatSper from 2-AG inhibition, allowing Ca2+ influx [31]. P4-induced Ca2+ influx triggers multiple Ca2+-dependent physiological responses, including hyperactivation, the acrosome reaction, and chemotaxis, which are critical for successful fertilization [30,32].
Another P4-like steroid hormone, pregnenolone sulfate, competes with P4 for the same ADBH2 binding site to activate CatSper in humans [33,34]. In addition, several endogenous steroids, such as testosterone, cortisol, and estradiol, have been identified as CatSper agonists [34]. Interestingly, in human sperm, these steroids target the same P4 binding site to activate CatSper, and they dose-dependently inhibit CatSper-dependent Ca2+ influx induced by P4 [35]. A recent study demonstrated that high cortisol levels in human sperm inhibit the P4-induced Ca2+ response. The presence of high cortisol levels resulting from anxiety symptoms exerts a competitive inhibitory effect on P4-induced Ca2+ influx and the acrosome reaction, ultimately compromising the quality of semen and fertility potential [36]. This suggests that cortisol, a potential stress biomarker, could negatively impact male reproductive health. Interestingly, certain steroids exhibit inhibitory effects on ligand-induced CatSper activation in a selective manner in human sperm [37]. Unlike mibefradil, which inhibits Ca2+ influx induced by all steroid hormones, medroxyprogesterone acetate, levonorgestrel, and aldosterone selectively suppress CatSper-dependent Ca2+ influx induced by P4, PGs, and the fungal pheromone sirenin in human sperm [37].
3.2. CatSper and PGs
Besides P4, PGs are also oviducal ligands for CatSper in human sperm. They are secreted by the oviduct, and the cumulus cells surrounding the oocyte are important ligands for CatSper. In HFF, the coexistence of P4 and PGs could elevate [Ca2+]i. In addition, seminal fluids contain high concentrations of PGs [38]. In the epididymis, sperm gain their fertilizing ability and maturity, and PGs may affect sperm function during this period. CatSper activation by PGs at the correct time is critical for successful fertilization. During the ejaculatory process, Zn2+ in seminal fluid inhibits PG-induced Ca2+ influx of human sperm, thereby preventing premature activation of CatSper and facilitating sperm escape into the female genital tract to localize the egg that is ready for fertilization [8]. Prostaglandin E1 (PGE1) activates CatSper, increases [Ca2+]I in a biphasic manner with similar amplitudes, and potentiates Ca2+ currents similarly to P4 in human sperm [39]. Consistently, PGs do not activate mouse sperm CatSper [30]. This emphasizes the differential regulation of CatSper between humans and mice. Interestingly, there is synergistic activation of human CatSper when PGE-1 and P4 are combined. This result indicates that PGE1 and P4 activate CatSper, apparently through two different binding sites or signaling mechanisms [38,39]. In addition, PGs activate human CatSper with different potencies: PGE1 > PGA1 > PGE2 ≫ PGD2 [30]. However, the mechanism of action of PGs on CatSper has yet to be fully elucidated [9,39].
3.3. CatSper and cAMP
The cAMP is a very important physiological chemical and plays a vital role in signaling transduction. In mammalian sperm, the cAMP pathway is essential for sperm functions, such as capacitation and hyperactivation. A study showed that 8-Br-cAMP, an analog of cAMP, increases CatSper-dependent [Ca2+]i [40] and modulates P4 to ultimately increase [Ca2+]i in mouse sperm [41]. In addition, bicarbonate can activate soluble adenylate cyclase, increase cAMP levels, and stimulate CatSper in human and mouse sperm [42,43,44].
3.4. CatSper and ZP Glycoproteins
The ZP acts as a protective matrix surrounding the oocyte in the female reproductive tract. In mammalian fertilization, the interaction between sperm and ZP glycoproteins triggers an increase in sperm [Ca2+]i [45]. Xia and Ren [45] found that ZP glycoproteins trigger Ca2+ entry into mouse sperm via CatSper. Balbach et al. [46] showed that ZP glycoproteins evoke a rapid increase in intracellular pH, and CatSper translates this change into a Ca2+ response in mouse sperm. In addition, sperm from Catsper1 knockout mice do not exhibit the ZP-glycoprotein-induced [Ca2+]I elevation. Indeed, the Ca2+ mobilized by ZP glycoproteins requires CatSper to enter sperm, implying that ZP-glycoprotein-induced Ca2+ influx is dependent on CatSper [45,47]. The knockout of Catsper genes in mice diminishes the ZP penetration and sperm motility. Thus, CatSper is necessary for sperm to penetrate the ZP effectively.
3.5. CatSper and Bovine Serum Albumin (BSA)
Capacitation is a functional maturation process that is necessary to produce hyperactivated motile sperm [5]. This process is dependent on extracellular Ca2+. BSA can induce sperm capacitation and increase [Ca2+]i in several mammals, but these effects are absent in the sperm of Catsper1-knockout mice and could be restored by an EGFP-CATSPER1 fusion protein [48]. These results suggest that BSA promotes Ca2+ entry into sperm via CatSper.
3.6. CatSper and DEFBs
The DEFB family includes small antimicrobial peptides expressed in the reproductive tract and involved in sperm motility and fertilization [49]. DEFB1 was the first identified member of the DEFB family; it is secreted by the epithelium of the male genital tract [50]. In human sperm, DEFB1 binds to its sperm receptor, C-C chemokine receptor 6, and evokes CatSper-dependent Ca2+ flux to regulate sperm motility, hyperactivation, and the acrosome reaction [51]. In addition, DEFB19/119 (mouse/human orthologs), secreted by the female germinal duct epithelium and the oocyte-ovarian complex, elicits Ca2+ mobilization via CatSper and induces sperm chemotaxis in capacitated sperm [52]. Mouse DEFB19 and human DEFB119 can activate the CatSper current in mouse and human sperm, respectively [52]. Defb19 knockdown in mouse oviducts and Defb19 knockout in male mice impairs sperm chemotaxis. In humans, DEFB119 expression and chemotactic activity are markedly decreased in HFF collected from women with idiopathic infertility [52]. These results indicate that DEFB19/DEFB119 play important roles in sperm chemotaxis and are associated with idiopathic infertility.
3.7. CatSper and Neurotransmitters
In mammals, receptors for many neurotransmitters and neuromodulators (such as acetylcholine, adenosine, adenosine triphosphate, γ-aminobutyric acid, serotonin, norepinephrine, and dopamine) are found in sperm. Therefore, a sperm is regarded as a neuron with a tail [53,54]. Interestingly, P4 activates CatSper in human sperm via an unconventional endocannabinoid signaling pathway (P4/ABHD2/2-AG/CatSper) [31]. In addition, serotonergic signals enhance hamster sperm hyperactivation via CatSper [55].
3.8. CatSper and Odorant Attractants
Sperm chemotaxis guides sperm toward the oocyte and is closely related to sperm capacitation, hyperactivation, the acrosome reaction, and male fertility. In humans, bourgeonal is a typical odorant and chemoattractant that is proposed to activate olfactory receptors (OR1D2) and to open CatSper to increase [Ca2+]i via a G-protein-coupled receptor/olfactory G-protein/cAMP/PKA pathway [9,56,57]. Moreover, men with idiopathic infertility and low sensitivity to bourgeonal have decreased OR1D2 protein expression and bourgeonal-activated CatSper current in their sperm [58]. These findings link odor perception to CatSper and male infertility. This sperm odorant attractant may provide a feasible screening method for CatSper-related male infertility.
4. CatSper and Medicines
In addition to physiological chemicals, some medicines have been shown to regulate CatSper functions. Some of them negatively affect CatSper, while some traditional Chinese medicines upregulate the expression of CatSper genes and ameliorate sperm function in infertile males (Summarized in Table 1).

Table 1.
The effect of different medicines on CatSper channel and sperm function.
4.1. CatSper and Traditional Medicine
CatSper is regarded as a primary target for the pharmacological treatment of male infertility and a novel non-hormone target for male contraception. Some traditional medicine has shown promise for improving male infertility through CatSper. Sheng Jing Shan (SJS), a traditional Chinese medicine, has shown efficacy in treating asthenozoospermia. Notably, SJS effectively improved the sperm motility of a rat model of cyclophosphamide (CP)-induced asthenozoospermia by upregulating Catsper1 expression [59]. Trigonelline semen (TS), also known as fenugreek, is a natural herbal substance recognized for its ability to improve sperm count and motility in infertile men [60]. In a rat model of CP-induced male infertility, TS effectively restored sperm count, motility, testosterone levels, and the expression of Catsper1, Catsper2, Catsper3, and Catsper4 [61]. Panax ginseng, a well-known traditional medicine with multiple pharmacological activities, is beneficial in treating various diseases [62]. Regarding male fertility, studies have noted that mice treated with P. ginseng exhibit increased sperm motility and Ca2+ levels [63]. P. ginseng significantly increases the expression of Catsper1, Catsper2, Catsper3, and Catsper4 in mouse sperm [63]. A recent investigation reported that a natural herb called Putranjiva roxburghii could effectively upregulate the expression of CatSper genes in bull sperm and markedly boost sperm motility [64]. In addition, escanbil is a traditional medicine applied to treat abnormal menstruation and menstrual cramps in folk medicine [65]. It improves sperm motility and alters the expression of CatSper genes in aging mice [66]. These results suggest that CatSper may be a potential therapeutic agent for natural medicine treatment of male infertility.
CatSper has attracted worldwide attention as a novel non-hormone target for male contraception. Matrine, a traditional Chinese medicine used for cancer treatment, has multiple effects, such as antiviral, antitumor, and insecticidal activities. We showed that matrine downregulated the expression of Catsper1, Catsper2, Catsper3, and Catsper4 in mouse testes. It decreased sperm CatSper current to disrupt a series of Ca2+-dependent sperm activities including motility, capacitation, and the P4-induced acrosome reaction [67]. We also found that another traditional medicine, anethole, suppressed CatSper current and inhibited the ability of human sperm to respond to P4 [68]. Rhynchosia volubilis, a traditional Chinese herb, is a major component of folk contraceptive prescriptions in China. Interestingly, we identified a new compound (rhynchone A) from R. volubilis. Rhynchone A could activate CatSper and induce Ca2+ signaling but suppress P4-induced Ca2+ signaling in human sperm [69]. In addition, two plant triterpenes, pristimerin and lupeol, were reported to inhibit P4 activation of human CatSper and are potential candidates for non-hormonal male contraception [33]. However, subsequent studies have contradicted these findings and confirmed that pristimerin and lupeol cannot inhibit CatSper activation in human sperm [34,35,70].
4.2. CatSper and Anti-Depressants
Selective serotonin reuptake inhibitors are the most widely used antidepressants in the United States and Europe, but recent research has highlighted their potential to impair male fertility [71]. Researchers have demonstrated that sertraline inhibits CatSper currents induced by intracellular alkalinization, voltage changes, P4, and PGs in human sperm [72]. Sertraline has a significant inhibitory effect on the acrosome reaction and viscous-medium penetration induced by P4 and PGs [72]. These findings suggest that the therapeutic administration of sertraline for depression may impair human reproduction.
4.3. CatSper and 5-Alpha Reductase Inhibitors
Finasteride (FS) and dutasteride (DS), two 5-alpha reductase inhibitors, are widely used to treat benign prostate hyperplasia. However, their prolonged use has been shown to adversely affect male semen quality [73]. FS activates CatSper, at least partially, via PG binding sites, whereas DS activates CatSper, at least partially, through P4 binding sites in human sperm [74]. Thus, they interfere with Ca2+ signaling mediated by PGs and P4. In addition, the exposure of mice to DS affected sperm count and motility and the expression of CatSper genes in caput and caudal epididymal sperm [75].
4.4. CatSper and Analgesics
Paracetamol is widely used as a mild analgesic to alleviate fever and pain. However, rodent studies have shown that paracetamol may have negative effects on sperm count and motility due to its endocrine effects. Additionally, high concentrations of paracetamol in male urine have been linked to lower sperm motility [76]. In human sperm, paracetamol is metabolized to N-arachidonoylphenolamine via fatty acid amide hydrolase expressed in the sperm neck region. N-arachidonoylphenolamine directly activates human CatSper, reduces sperm motility, and affects viscous-medium penetration [77].
4.5. CatSper and Ca2+ Channel Blockers
Nifedipine is a Ca2+ channel blocker and is used as an antihypertensive medicine. It exhibits anti-fertility effects in male rats, resulting in a significant reduction in sperm motility and count [78]. Nifedipine treatment reduces sperm motility and count and substantially downregulates the expression of CatSper genes in mouse epididymal sperm [75]. In addition, RU1968, a steroid-based selective and potent cross-species inhibitor of CatSper, has been demonstrated to suppress the activation of CatSper in human, mouse, and sea urchin sperm [79]. Therefore, nifedipine serves as a powerful tool for the investigation of the physiological function of CatSper in human sperm and for the promotion of the development of non-hormonal male contraceptives.
4.6. CatSper and Phosphodiesterase (PDE)-Inhibitors
Trequinsin hydrochloride, a PDE-3 inhibitor, has emerged as a promising CatSper agonist. In human sperm, trequinsin hydrochloride exhibits a P4-like agonist profile and significantly potentiates the CatSper current, effectively increasing sperm hyperactivation and viscous-medium penetration [80]. Additionally, this CatSper agonist induces a concentration-dependent elevation in Ca2+ levels through cross-desensitization with PGE1 [80].
4.7. CatSper and Anti-Inflammatory Drugs
Cisplatin is the most widely used drug in oncology treatment. However, cisplatin-based treatment of testicular cancer disrupts spermatogenesis and reduces the sperm motility of patients [81]. The indole derivative N′-(4-dimethylaminobenzylidene)-2-1-(4-(methylsulfinyl) benzylidene)-5-fluoro-2-methyl-1H-inden-3-yl) acetohydrazide (MMINA) has significant anti-inflammatory and antioxidant effects and can protect against the testicular toxicity induced by cisplatin [82]. Most importantly, MMINA activates CatSper by upregulating the expression of CatSper genes in rat sperm [83]. Moreover, MMINA is capable of forming hydrogen bonds with CatSper [83].
5. CatSper and EDCs
CatSper is not only a chemosensor for physiological chemicals and medicines, but is also a target for environmental chemicals. EDCs, a group of chemicals found in the environment, food, and consumer products, interfere with human hormone synthesis, metabolism, and reproduction. CatSper harbors binding sites for structurally diverse EDCs that potentially impact natural fertilization in several ways [84] (Summarized in Table 2).

Table 2.
The effect of different EDCs on CatSper and sperm function.
5.1. CatSper and Environmental Estrogens
Initially, EDCs were called xenoestrogens due to their estrogenic, antiestrogenic, androgenic, and antiandrogenic effects [85]. Steviol, a natural non-caloric sweetener metabolite, exerts endocrine effects on human sperm by antagonizing P4 and agonizing CatSper, resulting in a rapid influx of Ca2+ [86]. Bisphenol A (BPA), a ubiquitous EDC and synthetic organic compound, has been significantly and negatively associated with male fertility [87]. BPA binds to estrogen receptors α and β and exhibits estrogenic activity [88]. Animal studies have revealed that BPA impairs sperm function by reducing the expression of CatSper genes and the CatSper current [89]. In GC-2 cells, a mouse spermatogonia cell line, BPA decreased the growth rate and [Ca2+]i, and downregulated the expression of Catsper1, Catsper2, Catsper3, and Catsper4 through Ten-eleven translocation 1 [90]. In humans, bisphenol A diglycidyl ether and bisphenol analogs—but not BPA—activate CatSper [91]. Our study showed that diethylstilbestrol, a well-known, synthetic, non-steroidal estrogen, potentiates CatSper currents, increases the [Ca2+]i, and inhibits P4-induced Ca2+ influx and sperm functions in humans [92]. Perfluorooctane acid, an organic pollutant, activates CatSper to elevate the [Ca2+]i in human sperm [93]. Like diethylstilbestrol, perfluorooctane acid suppresses the P4-induced CatSper current, Ca2+ influx, and sperm functions [93]. In addition, the diversity of EDCs implies that even heavy metals may possess estrogenic activity. Cadmium is considered an EDC with significant toxicity to the reproductive system; it acts as an estrogen mimic and has the ability to bind ERs [94]. Cadmium impairs sperm function via a CatSper-mediated mechanism by affecting the expression of CatSper genes in mice [95].
5.2. CatSper and Pesticides
p,p′-Dichlorodiphenyldichloroethylene, a metabolite of dichloro-diphenyl-trichloroethane commonly found in human reproductive fluids, activates CatSper to induce Ca2+ entry into sperm and disrupts acrosome reaction [96]. Pentachlorophenol, a widely used pesticide, suppresses the P4-induced CatSper current, Ca2+ influx, and sperm functions in humans [97]. Recently, a study investigated the effect of 53 pesticides and pesticide metabolites on human sperm. The results demonstrated that, although 26 pesticides activated CatSper and interfered with signaling triggered by P4 and PGs, they may interact with the unique binding sites or the P4 and PG binding sites of CatSper [98]. Thus, pesticides, either alone or in low-dose mixtures, have the potential to negatively affect sperm function by interfering with normal Ca2+ signaling in human sperm via CatSper.
5.3. CatSper and Chemical Ultraviolet (UV) Filters
Chemical UV filters, commonly present in daily-use sunscreens, are among the most potent triggers of Ca2+ signaling. They directly activate CatSper in human sperm and elevate [Ca2+]i [84]. A recent study investigated the effect of 31 chemical UV filters approved in the European Union and the United States on human sperm. Although 29 of the 31 chemical UV filters induced Ca2+ signaling in human sperm, only nine of these chemicals could activate CatSper, including 4-Methylbenzylidene camphor, 3-Benzylidene camphor, meradimate, amiloxate, octisalate, benzylidene camphor sulfonic acid, homosalate, benzophenone-3, and octinoxate [99]. Of these chemicals, 3-Benzylidene camphor, benzylidene camphor sulfonic acid, and 4-Methylbenzylidene camphor have been found to competitively inhibit P4-induced Ca2+ signaling and target its binding sites in CatSper [84,99]. These results suggest that some chemical UV filters have the potential to interfere with P4-induced Ca2+ signaling and negatively affect sperm functions.
6. CatSper and Drugs of Abuse
Interestingly, some addictive drugs affect sperm functions through CatSper. Methamphetamine (METH) is a highly addictive central nervous system stimulant that has detrimental effects on male reproductive health, including impaired spermatogenesis, testicular damage, and abnormal sperm quality [100]. In particular, a novel investigation showed that rats receiving METH resulted in a decrease in testis and epididymis weight [101]. Meanwhile, the relative expression levels of Catsper1, Catsper2, Catsper3, and Catsper4, as well as the sperm motility associated gene Mvh, were decreased significantly [101]. In addition, the exclusive expression of Catsper1–4 in testes is required for sperm motility and fertility [21,102]. As a result, the downregulation of these genes induced by METH increases the possibility of male infertility. Therefore, men addicted to METH may encounter potential reproductive problems.
Ketamine, a dissociative anesthetic widely used in human and animal medicine, has become a popular recreational drug because it can induce hallucinatory effects. We showed that ketamine affects sperm motility, viscous-medium penetration, and the P4-induced acrosome reaction by inhibiting CatSper in human sperm, thus decreasing [Ca2+]i [103]. In addition, ketamine is an antagonist of the N-Methyl-D-aspartic acid (NMDA) receptor. In our recent study, we found that the NMDA receptor is expressed in human sperm and involved in the inhibitory effect of ketamine on human sperm functions [104]. Specifically, NMDA, the physiological ligand of NMDA, could partly alleviate the motility of human sperm and significantly recover the capacitation and acrosome reaction, as well as [Ca2+]i [104]. Therefore, the competitive receptor binding between ketamine and NMDA may provide novel insight for clinical diagnoses of ketamine abusers. Collectively, CatSper-related drugs of abuse have been implicated in impaired sperm function and/or male infertility.
7. CatSper and Antioxidants
Oxidative stress occurs when the generation of reactive oxygen species (ROS) exceeds the natural antioxidant defenses of bodies. Thus, the precise balance of ROS and antioxidants within sperm are necessary for capacitation and fertilization. The major effect of oxidative stress compromising sperm function is caused by two principal mechanisms, DNA damage and lipid peroxidation [105]. In human sperm, ROS damages DNA directly by the production of 1,N6-ethenoadenosine and 1,N2-ethenoguanosine, resulting in DNA structure instability and leading to single-strand breaks [106]. Once the transcription and translation of post-spermiogenesis stop, the DNA repair during developing sperm is terminated [107]. Hence, sperm function and pregnancy outcome are strongly impacted.
To counteract ROS damage, the human body has developed a variety of antioxidant strategies. For instance, non-enzymatic antioxidants contained within the seminal fluid, like vitamin E and selenium [108]. Interestingly, treatment with these two antioxidants upregulates the expression of Catsper in the testes of young adult and aged male mice, which are the genes responsible for sperm motility [109,110]. Meanwhile, sperm parameters such as viability rate and morphology also show an improvement after treatment [109,110]. Consequently, these two essential components play a crucial role in the maintenance of male reproduction.
8. Conclusions
CatSper plays a key role in male fertility by controlling extracellular Ca2+ influx into sperm and it is also a polymodal chemosensor that harbors structurally diverse binding sites for extracellular factors. CatSper regulates key sperm physiological processes, including capacitation, hyperactivation, the acrosome reaction, and chemotaxis, by responding to physiological ligands. These processes are necessary to produce sperm capable of fertilization. In addition, the interaction between CatSper and extracellular factors, such as EDCs and drugs, may potentially disrupt sperm function and induce male infertility [111]. Consequently, CatSper is a crucial regulatory target for male fertility. It links sperm function with the external environment. Therefore, CatSper is regarded as a primary target for the pharmacological treatment of male infertility. Future investigation is warranted to develop highly specific and effective CatSper inhibitors, which could serve as an alternative approach to male hormonal contraception. Although we know that all these mentioned ligands have different effects on the opening of CatSper, many questions about the physiology of CatSper remain unanswered; in particular, the mechanism by which these ligands directly or indirectly modulate CatSper is unclear. In addition, there is still a lack of understanding of how the interactions that exist between ligands affect CatSper regulation. Therefore, it is necessary to understand CatSper in a more physiological manner. Further studies should be based on the molecular basis of ligands during binding CatSper. This could facilitate the elucidation of how the CatSper-based pathway regulates multiple ligands within mammalian sperm.
Author Contributions
Conceptualization, T.L.; methodology, S.K. and T.L.; investigation, S.K. and T.L.; data curation, T.L.; writing—original draft preparation, S.K. and T.L.; writing—review and editing, S.K. and T.L.; supervision, T.L.; project administration, T.L.; funding acquisition, T.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (grant number: 82071708) and the Jiangxi Double Thousand Plan (grant number: jxsq2019201091).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank the online software BioRender (https://www.biorender.com, accessed on 18 May 2023) for the technical assistance of scientific image and illustration.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gervasi, M.G.; Visconti, P.E. Molecular changes and signaling events occurring in spermatozoa during epididymal maturation. Andrology 2017, 5, 204–218. [Google Scholar] [CrossRef]
- TMortimer, S. A critical review of the physiological importance and analysis of sperm movement in mammals. Hum. Reprod. 1997, 3, 403–439. [Google Scholar]
- Perez-Cerezales, S.; Boryshpolets, S.; Eisenbach, M. Behavioral mechanisms of mammalian sperm guidance. Asian J. Androl. 2015, 17, 628–632. [Google Scholar] [PubMed]
- Costello, S.; Michelangeli, F.; Nash, K.; Lefievre, L.; Morris, J.; Machado-Oliveira, G.; Barratt, C.; Kirkman-Brown, J.; Publicover, S. Ca2+-stores in sperm: Their identities and functions. Reproduction 2009, 138, 425–437. [Google Scholar] [CrossRef] [PubMed]
- Molina, L.C.P.; Luque, G.M.; Balestrini, P.A.; Marín-Briggiler, C.I.; Romarowski, A.; Buffone, M.G. Molecular Basis of Human Sperm Capacitation. Front. Cell Dev. Biol. 2018, 6, 72. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, M.; Etkovitz, N.; Breitbart, H. Ca(2+) signaling in mammalian spermatozoa. Mol. Cell. Endocrinol. 2020, 516, 110953. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.P.; Rajender, S. CatSper channel, sperm function and male fertility. Reprod. Biomed. Online 2015, 30, 28–38. [Google Scholar] [CrossRef]
- Jeschke, J.K.; Biagioni, C.; Schierling, T.; Wagner, I.V.; Börgel, F.; Schepmann, D.; Schüring, A.; Kulle, A.E.; Holterhus, P.M.; von Wolff, M.; et al. The Action of Reproductive Fluids and Contained Steroids, Prostaglandins, and Zn(2+) on CatSper Ca(2+) Channels in Human Sperm. Front. Cell Dev. Biol. 2021, 9, 699554. [Google Scholar] [CrossRef]
- Brenker, C.; Goodwin, N.; Weyand, I.; Kashikar, N.D.; Naruse, M.; Krähling, M.; Müller, A.; Kaupp, U.B.; Strünker, T. The CatSper channel: A polymodal chemosensor in human sperm. EMBO J. 2012, 31, 1654–1665. [Google Scholar] [CrossRef]
- Huang, X.; Miyata, H.; Wang, H.; Mori, G.; Iida-Norita, R.; Ikawa, M.; Percudani, R.; Chung, J.J. A CUG-initiated CATSPERθ functions in the CatSper channel assembly and serves as a checkpoint for flagellar trafficking. bioRxiv 2023. [Google Scholar] [CrossRef]
- Yang, F.; Gracia Gervasi, M.; Orta, G.; Tourzani, D.A.; De la Vega-Beltran, J.L.; Ruthel, G.; Darszon, A.; Visconti, P.E.; Wang, P.J. C2CD6 regulates targeting and organization of the CatSper calcium channel complex in sperm flagella. Development 2022, 149, dev199988. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Ke, M.; Zhang, Y.; Yan, Z.; Wu, J. Structure of a mammalian sperm cation channel complex. Nature 2021, 595, 746–750. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wang, H.; Wiesehoefer, C.; Shah, N.B.; Reetz, E.; Hwang, J.Y.; Huang, X.; Wang, T.E.; Lishko, P.V.; Davies, K.M.; et al. 3D structure and in situ arrangements of CatSper channel in the sperm flagellum. Nat. Commun. 2022, 13, 3439. [Google Scholar] [CrossRef] [PubMed]
- Avenarius, M.R.; Hildebrand, M.S.; Zhang, Y.; Meyer, N.C.; Smith, L.L.; Kahrizi, K.; Najmabadi, H.; Smith, R.J. Human male infertility caused by mutations in the CATSPER1 channel protein. Am. J. Hum. Genet. 2009, 84, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Luo, T.; Chen, H.Y.; Zou, Q.X.; Wang, T.; Cheng, Y.M.; Wang, H.F.; Wang, F.; Jin, Z.L.; Chen, Y.; Weng, S.Q.; et al. A novel copy number variation in CATSPER2 causes idiopathic male infertility with normal semen parameters. Hum. Reprod. 2019, 34, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tang, H.; Zou, Q.; Zheng, A.; Li, H.; Yang, S.; Xiang, J. Patient with CATSPER3 mutations-related failure of sperm acrosome reaction with successful pregnancy outcome from intracytoplasmic sperm injection (ICSI). Mol. Genet. Genom. Med. 2021, 9, e1579. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.J.; Navarro, B.; Krapivinsky, G.; Krapivinsky, L.; Clapham, D.E. A novel gene required for male fertility and functional CATSPER channel formation in spermatozoa. Nat. Commun. 2011, 2, 153. [Google Scholar] [CrossRef] [PubMed]
- Carlson, A.E.; Quill, T.A.; Westenbroek, R.E.; Schuh, S.M.; Hille, B.; Babcock, D.F. Identical phenotypes of CatSper1 and CatSper2 null sperm. J. Biol. Chem. 2005, 280, 32238–32244. [Google Scholar] [CrossRef]
- Jin, J.; Jin, N.; Zheng, H.; Ro, S.; Tafolla, D.; Sanders, K.M.; Yan, W. Catsper3 and Catsper4 are essential for sperm hyperactivated motility and male fertility in the mouse. Biol. Reprod. 2007, 77, 37–44. [Google Scholar] [CrossRef]
- Qi, H.; Moran, M.M.; Navarro, B.; Chong, J.A.; Krapivinsky, G.; Krapivinsky, L.; Kirichok, Y.; Ramsey, I.S.; Quill, T.A.; Clapham, D.E. All four CatSper ion channel protein are required for male fertility and sperm cell hyperactivated motility. Proc. Natl. Acad. Sci. USA 2007, 104, 1219–1223. [Google Scholar] [CrossRef]
- Avidan, N.; Tamary, H.; Dgany, O.; Cattan, D.; Pariente, A.; Thulliez, M.; Borot, N.; Moati, L.; Barthelme, A.; Shalmon, L.; et al. CATSPER2, a human autosomal nonsyndromic male infertility gene. Eur. J. Hum. Genet. 2003, 11, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.L.; Mansell, S.; Alasmari, W.; Brown, S.G.; Wilson, S.M.; Sutton, K.A.; Miller, M.R.; Lishko, P.V.; Barratt, C.L.R.; Publicover, S.J.; et al. Specific loss of CatSper function is sufficient to compromise fertilizing capacity of human spermatozoa. Hum. Reprod. 2015, 30, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.G.; Miller, M.R.; Lishko, P.V.; Lester, D.H.; Publicover, S.J.; Barratt, C.L.R.; Da Silva, S.M. Homozygous in-frame deletion in CATSPERE in a man producing spermatozoa with loss of CatSper function and compromised fertilizing capacity. Hum. Reprod. 2018, 33, 1812–1816. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; McGoldrick, L.L.; Chung, J.-J. Sperm ion channels and transporters in male fertility and infertility. Nat. Rev. Urol. 2021, 18, 46–66. [Google Scholar] [CrossRef]
- Navarro, B.; Kirichok, Y.; Clapham, D.E. KSper, a pH-sensitive K+ current that controls sperm membrane potential. Proc. Natl. Acad. Sci. USA 2007, 104, 7688–7692. [Google Scholar] [CrossRef] [PubMed]
- Chavez, J.C.; Ferreira, J.J.; Butler, A.; De La Vega Beltran, J.L.; Trevino, C.L.; Darszon, A.; Salkoff, L.; Santi, C.M. SLO3K+ channels control calcium entry through CATSPER channels in sperm. J. Biol. Chem. 2014, 289, 32266–32275. [Google Scholar] [CrossRef]
- Hwang, J.Y.; Chung, J.J. CatSper Calcium Channels: 20 Years On. Physiology 2023, 38, 125–140. [Google Scholar] [CrossRef]
- Brown, S.G.; Costello, S.; Kelly, M.C.; Ramalingam, M.; Drew, E.; Publicover, S.J.; Barratt, C.L.R.; Da Silva, S.M. Complex CatSper-dependent and independent [Ca2+]i signalling in human spermatozoa induced by follicular fluid. Hum. Reprod. 2017, 32, 1995–2006. [Google Scholar] [CrossRef]
- Sumigama, S.; Mansell, S.; Miller, M.; Lishko, P.V.; Cherr, G.N.; Meyers, S.A.; Tollner, T. Progesterone Accelerates the Completion of Sperm Capacitation and Activates CatSper Channel in Spermatozoa from the Rhesus Macaque. Biol. Reprod. 2015, 93, 130. [Google Scholar] [CrossRef]
- Lishko, P.V.; Botchkina, I.L.; Kirichok, Y. Progesterone activates the principal Ca2+ channel of human sperm. Nature 2011, 471, 387–391. [Google Scholar] [CrossRef]
- Miller, M.R.; Mannowetz, N.; Iavarone, A.T.; Safavi, R.; Gracheva, E.O.; Smith, J.F.; Hill, R.Z.; Bautista, D.M.; Kirichok, Y.; Lishko, P.V. Unconventional endocannabinoid signaling governs sperm activation via the sex hormone progesterone. Science 2016, 352, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Uhler, M.L.; Leungt, A.; Chan, S.Y.W.; Wang, C. Direct effects of progesterone and antiprogesterone on human sperm hyperactivated motility and acrosome reaction. Fertil. Steril. 1992, 58, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
- Mannowetz, N.; Miller, M.R.; Lishko, P.V. Regulation of the sperm calcium channel CatSper by endogenous steroids and plant triterpenoids. Proc. Natl. Acad. Sci. USA 2017, 114, 5743–5748. [Google Scholar] [CrossRef] [PubMed]
- Brenker, C.; Schiffer, C.; Wagner, I.V.; Tüttelmann, F.; Röpke, A.; Rennhack, A.; Kaupp, U.B.; Strünker, T. Action of steroids and plant triterpenoids on CatSper Ca(2+) channels in human sperm. Proc. Natl. Acad. Sci. USA 2018, 115, E344–E346. [Google Scholar] [CrossRef] [PubMed]
- Rehfeld, A. Revisiting the action of steroids and triterpenoids on the human sperm Ca2+ channel CatSper. Mol. Hum. Reprod. 2020, 26, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Sánchez González, S.R.; Mata Martínez, E.; Torres Juárez, J.A.; Arias, R.J.; De Blas, G.A.; Sánchez Tusie, A.A. Cortisol modulates Ca(2+) signaling and acrosome reaction in human sperm. Andrology 2023, 11, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Carlson, E.J.; Georg, G.I.; Hawkinson, J.E. Steroidal Antagonists of Progesterone- and Prostaglandin E(1)-Induced Activation of the Cation Channel of Sperm. Mol. Pharmacol. 2022, 101, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, Y.; Yorimitsu, A.; Maruyama, Y.; Kubota, T.; Aso, T.; ABronson, R. Prostaglandins induce calcium influx in human spermatozoa. Mol. Hum. Reprod. 1998, 4, 555–561. [Google Scholar] [CrossRef]
- Strünker, T.; Goodwin, N.; Brenker, C.; Kashikar, N.D.; Weyand, I.; Seifert, R.; Kaupp, U.B. The CatSper channel mediates progesterone-induced Ca2+ influx in human sperm. Nature 2011, 471, 382–386. [Google Scholar] [CrossRef]
- Xia, J.; Reigada, D.; Mitchell, C.H.; Ren, D. CATSPER channel-mediated Ca2+ entry into mouse sperm triggers a tail-to-head propagation. Biol. Reprod. 2007, 77, 551–559. [Google Scholar] [CrossRef]
- Kobori, H.; Miyazaki, S.; Kuwabara, Y. Characterization of intracellular Ca(2+) increase in response to progesterone and cyclic nucleotides in mouse spermatozoa. Biol. Reprod. 2000, 63, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Hereng, T.H.; Elgstoen, K.B.; Eide, L.; Rosendal, K.R.; Skalhegg, B.S. Serum albumin and HCO3− regulate separate pools of ATP in human spermatozoa. Hum. Reprod. 2014, 29, 918–930. [Google Scholar] [CrossRef] [PubMed]
- Boisen, I.M.; Rehfeld, A.; Mos, I.; Poulsen, N.N.; Nielsen, J.E.; Schwarz, P.; Rejnmark, L.; Dissing, S.; Bach-Mortensen, P.; Juul, A.; et al. The Calcium-Sensing Receptor Is Essential for Calcium and Bicarbonate Sensitivity in Human Spermatozoa. J. Clin. Endocrinol. Metab. 2021, 106, e1775–e1792. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.J.; Lybaert, P.; Puga-Molina, L.C.; Santi, C.M. Conserved Mechanism of Bicarbonate-Induced Sensitization of CatSper Channels in Human and Mouse Sperm. Front. Cell Dev. Biol. 2021, 9, 733653. [Google Scholar] [CrossRef]
- Xia, J.; Ren, D. Egg coat proteins activate calcium entry into mouse sperm via CATSPER channels. Biol. Reprod. 2009, 80, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Balbach, M.; Hamzeh, H.; Jikeli, J.F.; Brenker, C.; Schiffer, C.; Hansen, J.N.; Neugebauer, P.; Trötschel, C.; Jovine, L.; Han, L.; et al. Molecular Mechanism Underlying the Action of Zona-pellucida Glycoproteins on Mouse Sperm. Front. Cell Dev. Biol. 2020, 8, 572735. [Google Scholar] [CrossRef] [PubMed]
- Ren, D.; Navarro, B.; Perez, G.; Jackson, A.C.; Hsu, S.; Shi, Q.; Tilly, J.L.; Clapham, D.E. A sperm ion channel required for sperm motility and male fertility. Nature 2001, 413, 603–609. [Google Scholar] [CrossRef]
- Xia, J.; Ren, D. The BSA-induced Ca2+ influx during sperm capacitation is CATSPER channel-dependent. Reprod. Biol. Endocrinol. 2009, 7, 119. [Google Scholar] [CrossRef]
- Pazgier, M.; Hoover, D.M.; Yang, D.; Lu, W.; Lubkowski, J. Human beta-defensins. Cell. Mol. Life Sci. 2006, 63, 1294–1313. [Google Scholar] [CrossRef]
- Diao, R.; Fok, K.L.; Chen, H.; Mei Kuen, Y.; Duan, Y.; Chung, C.M.; Li, Z.; Wu, H.; Li, Z.; Zhang, H.; et al. Deficient human b-defensin 1 underlies male infertility associated with poor sperm motility and genital tract infection. Sci. Transl. Med. 2014, 6, 249ra108. [Google Scholar] [CrossRef]
- Diao, R.; Wang, T.; Fok, K.L.; Li, X.; Ruan, Y.; Yu, M.K.; Cheng, Y.; Chen, Y.; Chen, H.; Mou, L.; et al. CCR6 is required for ligand-induced CatSper activation in human sperm. Oncotarget 2017, 8, 91445–91458. [Google Scholar] [CrossRef]
- Li, X.; Yuan, C.; Shi, J.; Kang, H.; Chen, Y.; Duan, Y.; Jin, J.; Cheung, L.P.; Li, T.C.; Liu, Y.; et al. β-Defensin 19/119 mediates sperm chemotaxis and is associated with idiopathic infertility. Cell Rep. Med. 2022, 3, 100825. [Google Scholar] [CrossRef]
- Meizel, S. The sperm, a neuron with a tail: ‘Neuronal’ receptors in mammalian sperm. Biol. Rev. Camb. Philos. Soc. 2004, 79, 713–732. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Reveco, A.; Villarroel-Espindola, F.; Rodriguez-Gil, J.E.; Concha, I.I. Neuronal signaling repertoire in the mammalian sperm functionality. Biol. Reprod. 2017, 96, 505–524. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, C.; Fujinoki, M.; Kitazawa, M.; Obayashi, S. Serotonergic signals enhanced hamster sperm hyperactivation. J. Reprod. Dev. 2021, 67, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Yoshida, K. Sperm chemotaxis and regulation of flagellar movement by Ca2+. Mol. Hum. Reprod. 2011, 17, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.-M.; Luo, T.; Peng, Z.; Chen, H.-Y.; Zhang, J.; Zeng, X.-H. OR1D2 receptor mediates bourgeonal-induced human CatSper activation in a G-protein dependent manner. bioRxiv 2019, 757880. [Google Scholar] [CrossRef]
- Sinding, C.; Kemper, E.; Spornraft-Ragaller, P.; Hummel, T. Decreased Perception of Bourgeonal May Be Linked to Male Idiopathic Infertility. Chem. Senses 2013, 38, 439–445. [Google Scholar] [CrossRef]
- Wang, Y.N.; Wang, B.; Liang, M.; Han, C.Y.; Zhang, B.; Cai, J.; Sun, W.; Xing, G.G. Down-regulation of CatSper1 channel in epididymal spermatozoa contributes to the pathogenesis of asthenozoospermia, whereas up-regulation of the channel by Sheng-Jing-San treatment improves the sperm motility of asthenozoospermia in rats. Fertil. Steril. 2013, 99, 579–587. [Google Scholar] [CrossRef]
- Sadogh, A.; Gorji, N.; Moeini, R. Herbal foodstuffs in Avicenna’s recommended diet to improve sperm quality and increase male fertility; an evidence-based approach. J. Complement. Integr. Med. 2021, 19, 47–70. [Google Scholar] [CrossRef]
- Kim, D.R.; Kim, H.Y.; Kim, H.Y.; Chang, M.S.; Park, S.K. Trigonellae Semen Enhances Sperm Motility and the Expression of the Cation Sperm Channel Proteins in Mouse Testes. Evid.-Based Complement. Altern. Med. 2015, 2015, 817324. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, C.; Santangelo, R. Panax ginseng and Panax quinquefolius: From pharmacology to toxicology. Food Chem. Toxicol. 2017, 107, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Park, E.H.; Kim, D.R.; Kim, H.Y.; Park, S.K.; Chang, M.S. Panax ginseng induces the expression of CatSper genes and sperm hyperactivation. Asian J. Androl. 2014, 16, 845–851. [Google Scholar]
- Italiya, J.M.; Patel, M.R.; Golaviya, A.V.; Patel, S.S.; Thakkar, B.K.; Jakhesara, S.J.; Joshi, C.G.; Koringa, P.G. RNA-sequencing attest increased sperm motility in bovine spermatozoa treated with ethanolic extract of Putranjiva roxburghii. 3 Biotech 2023, 13, 33. [Google Scholar] [CrossRef] [PubMed]
- Kiani, K.; Rudzitis-Auth, J.; Scheuer, C.; Movahedin, M.; Sadati Lamardi, S.N.; Malekafzali Ardakani, H.; Becker, V.; Moini, A.; Aflatoonian, R.; Ostad, S.N.; et al. Calligonum comosum (Escanbil) extract exerts anti-angiogenic, anti-proliferative and anti-inflammatory effects on endometriotic lesions. J. Ethnopharmacol. 2019, 239, 111918. [Google Scholar] [CrossRef] [PubMed]
- Askari Jahromi, M.; Movahedin, M.; Mazaheri, Z.; Amanlu, M.; Mowla, S.J.; Batooli, H. Evaluating the effects of Escanbil (Calligonum) extract on the expression level of Catsper gene variants and sperm motility in aging male mice. Iran. J. Reprod. Med. 2014, 12, 459–466. [Google Scholar] [PubMed]
- Luo, T.; Zou, Q.X.; He, Y.Q.; Wang, H.F.; Wang, T.; Liu, M.; Chen, Y.; Wang, B. Matrine compromises mouse sperm functions by a [Ca(2+)]i-related mechanism. Reprod. Toxicol. 2016, 60, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Luo, T.; Wang, F.; Weng, S.; Chen, H.; Kang, H.; Wang, J.; Luo, S. Anethole compromises human sperm function by affecting the sperm intracellular calcium concentration and tyrosine phosphorylation. Reprod. Toxicol. 2020, 93, 99–105. [Google Scholar] [CrossRef]
- Guan, H.T.; Fang, F.; Xiong, Z.; Meng, T.Q.; Huang, S.X. n-Butanol extract of Rhynchosia volubilis Lour: A potent spermicidal agent In Vitro. J. Huazhong Univ. Sci. Technol. Med. Sci. 2014, 34, 398–402. [Google Scholar] [CrossRef]
- Rehfeld, A.; Marcus Pedersen, C. Lupeol and pristimerin do not inhibit activation of the human sperm CatSper Ca(2+)-channel. F1000Research 2022, 11, 222. [Google Scholar] [CrossRef]
- Kumar, V.S.; Sharma, V.L.; Tiwari, P.; Singh, D.; Maikhuri, J.P.; Gupta, G.; Singh, M.M. The spermicidal and antitrichomonas activities of SSRI antidepressants. Bioorg. Med. Chem. Lett. 2006, 16, 2509–2512. [Google Scholar] [CrossRef] [PubMed]
- Rahban, R.; Rehfeld, A.; Schiffer, C.; Brenker, C.; Egeberg Palme, D.L.; Wang, T.; Lorenz, J.; Almstrup, K.; Skakkebaek, N.E.; Strünker, T.; et al. The antidepressant Sertraline inhibits CatSper Ca2+ channels in human sperm. Hum. Reprod. 2021, 36, 2638–2648. [Google Scholar] [CrossRef] [PubMed]
- Amory, J.K.; Wang, C.; Swerdloff, R.S.; Anawalt, B.D.; Matsumoto, A.M.; Bremner, W.J.; Walker, S.E.; Haberer, L.J.; Clark, R.V. The effect of 5alpha-reductase inhibition with dutasteride and finasteride on semen parameters and serum hormones in healthy men. J. Clin. Endocrinol. Metab. 2007, 92, 1659–1665. [Google Scholar] [CrossRef] [PubMed]
- Birch, M.R.; Dissing, S.; Skakkebæk, N.E.; Rehfeld, A. Finasteride interferes with prostaglandin-induced CatSper signalling in human sperm. Reproduction 2021, 161, 561–572. [Google Scholar] [CrossRef]
- Srivastav, A.; Changkija, B.; Sharan, K.; Nagar, G.K.; Bansode, F.W. Influence of antifertility agents Dutasteride and Nifedipine on CatSper gene level in epididymis during sperm maturation in BALB/c mice. Reproduction 2018, 155, 347–359. [Google Scholar] [CrossRef]
- Smarr, M.M.; Kannan, K.; Chen, Z.; Kim, S.; Buck Louis, G.M. Male urinary paracetamol and semen quality. Andrology 2017, 5, 1082–1088. [Google Scholar] [CrossRef] [PubMed]
- Rehfeld, A.; Frederiksen, H.; Rasmussen, R.H.; David, A.; Chaker, J.; Nielsen, B.S.; Nielsen, J.E.; Juul, A.; Skakkebæk, N.E.; Kristensen, D.M. Human sperm cells can form paracetamol metabolite AM404 that directly interferes with sperm calcium signalling and function through a CatSper-dependent mechanism. Hum. Reprod. 2022, 37, 922–935. [Google Scholar] [CrossRef]
- Morakinyo, A.O.; Iranloye, B.O.; Adegoke, O.A. Antireproductive effect of calcium channel blockers on male rats. Reprod. Med. Biol. 2009, 8, 97–102. [Google Scholar] [CrossRef]
- Rennhack, A.; Schiffer, C.; Brenker, C.; Fridman, D.; Nitao, E.T.; Cheng, Y.M.; Tamburrino, L.; Balbach, M.; Stolting, G.; Berger, T.K.; et al. A novel cross-species inhibitor to study the function of CatSper Ca(2+) channels in sperm. Br. J. Pharmacol. 2018, 175, 3144–3161. [Google Scholar] [CrossRef]
- McBrinn, R.C.; Fraser, J.; Hope, A.G.; Gray, D.W.; Barratt, C.L.R.; da Silva, S.J.M.; Brown, S.G. Novel pharmacological actions of trequinsin hydrochloride improve human sperm cell motility and function. Br. J. Pharmacol. 2019, 176, 4521–4536. [Google Scholar] [CrossRef]
- Howell, S.J.; Shalet, S.M. Spermatogenesis after cancer treatment: Damage and recovery. J. Natl. Cancer Inst. Monogr. 2005, 2005, 12–17. [Google Scholar] [CrossRef]
- Razak, S.; Afsar, T.; Bibi, N.; Abulmeaty, M.; Qamar, W.; Almajwal, A.; Inam, A.; AI Disi, D.; Shabbir, M.; Bhat, M.A. Molecular docking, pharmacokinetic studies, and in vivo pharmacological study of indole derivative 2-(5-methoxy-2-methyl-1H-indole-3-yl)-N’-[(E)-(3-nitrophenyl) methylidene] acetohydrazide as a promising chemoprotective agent against cisplatin induced organ damage. Sci. Rep. 2021, 11, 6245. [Google Scholar] [PubMed]
- Afsar, T.; Razak, S.; Trembley, J.H.; Khan, K.; Shabbir, M.; Almajwal, A.; Alruwaili, N.W.; Ijaz, M.U. Prevention of Testicular Damage by Indole Derivative MMINA via Upregulated StAR and CatSper Channels with Coincident Suppression of Oxidative Stress and Inflammation: In Silico and In Vivo Validation. Antioxidants 2022, 11, 2063. [Google Scholar] [CrossRef] [PubMed]
- Schiffer, C.; Müller, A.; Egeberg, D.L.; Alvarez, L.; Brenker, C.; Rehfeld, A.; Frederiksen, H.; Wäschle, B.; Kaupp, U.B.; Balbach, M.; et al. Direct action of endocrine disrupting chemicals on human sperm. EMBO Rep. 2014, 15, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, B.; Terekeci, H.; Sandal, S.; Kelestimur, F. Endocrine disrupting chemicals: Exposure, effects on human health, mechanism of action, models for testing and strategies for prevention. Rev. Endocr. Metab. Disord. 2020, 21, 127–147. [Google Scholar] [CrossRef] [PubMed]
- Shannon, M.; Rehfeld, A.; Frizzell, C.; Livingstone, C.; McGonagle, C.; Skakkebaek, N.E.; Wielogórska, E.; Connolly, L. In vitro bioassay investigations of the endocrine disrupting potential of steviol glycosides and their metabolite steviol, components of the natural sweetener Stevia. Mol. Cell. Endocrinol. 2016, 427, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Xu, W.; Yuan, Y.; Luo, T. What is the Impact of Bisphenol A on Sperm Function and Related Signaling Pathways: A Mini-review? Curr. Pharm. Des. 2020, 26, 4822–4828. [Google Scholar] [CrossRef] [PubMed]
- Le Fol, V.; Ait-Aissa, S.; Sonavane, M.; Porcher, J.M.; Balaguer, P.; Cravedi, J.P.; Zalko, D.; Brion, F. In vitro and in vivo estrogenic activity of BPA, BPF and BPS in zebrafish-specific assays. Ecotoxicol. Environ. Saf. 2017, 142, 150–156. [Google Scholar] [CrossRef]
- Wang, H.F.; Liu, M.; Li, N.; Luo, T.; Zheng, L.P.; Zeng, X.H. Bisphenol A Impairs Mature Sperm Functions by a CatSper-Relevant Mechanism. Toxicol. Sci. 2016, 152, 145–154. [Google Scholar] [CrossRef]
- Yuan, W.B.; Chen, H.Q.; Li, J.Z.; Zhou, S.M.; Zeng, Y.; Fan, J.; Zhang, Z.; Liu, J.Y.; Cao, J.; Liu, W.B. TET1 mediated male reproductive toxicity induced by Bisphenol A through Catsper-Ca(2+) signaling pathway. Environ. Pollut. 2022, 296, 118739. [Google Scholar] [CrossRef]
- Rehfeld, A.; Andersson, A.M.; Skakkebaek, N.E. Bisphenol A Diglycidyl Ether (BADGE) and Bisphenol Analogs, but Not Bisphenol A (BPA), Activate the CatSper Ca(2+) Channel in Human Sperm. Front. Endocrinol. 2020, 11, 324. [Google Scholar] [CrossRef] [PubMed]
- Zou, Q.X.; Peng, Z.; Zhao, Q.; Chen, H.Y.; Cheng, Y.M.; Liu, Q.; He, Y.Q.; Weng, S.Q.; Wang, H.F.; Wang, T.; et al. Diethylstilbestrol activates CatSper and disturbs progesterone actions in human spermatozoa. Hum. Reprod. 2017, 32, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Ding, X.; Cheng, Y.; Kang, H.; Luo, T.; Zhang, X.; Kuang, H.; Chen, Y.; Zeng, X.; Zhang, D. PFOA evokes extracellular Ca(2+) influx and compromises progesterone-induced response in human sperm. Chemosphere 2020, 241, 125074. [Google Scholar] [CrossRef] [PubMed]
- Diamanti-Kandarakis, E.; Bourguignon, J.P.; Giudice, L.C.; Hauser, R.; Prins, G.S.; Soto, A.M.; Zoeller, R.T.; Gore, A.C. Endocrine-disrupting chemicals: An Endocrine Society scientific statement. Endocr. Rev. 2009, 30, 293–342. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.F.; Chang, M.; Peng, T.T.; Yang, Y.; Li, N.; Luo, T.; Zhou, M.Z.; Zeng, X.H.; Zheng, L.P. Exposure to Cadmium Impairs Sperm Functions by Reducing CatSper in Mice. Cell. Physiol. Biochem. 2017, 42, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Tavares, R.S.; Mansell, S.; Barratt, C.L.; Wilson, S.M.; Publicover, S.J.; Ramalho-Santos, J. p,p′-DDE activates CatSper and compromises human sperm function at environmentally relevant concentrations. Hum. Reprod. 2013, 28, 3167–3177. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Kang, H.; Peng, L.; Song, D.; Jiang, X.; Li, Y.; Chen, H.; Zeng, X. Pentachlorophenol inhibits CatSper function to compromise progesterone’s action on human sperm. Chemosphere 2020, 259, 127493. [Google Scholar] [CrossRef]
- Birch, M.R.; Johansen, M.; Skakkebaek, N.E.; Andersson, A.M.; Rehfeld, A. In vitro investigation of endocrine disrupting effects of pesticides on Ca(2+)-signaling in human sperm cells through actions on the sperm-specific and steroid-activated CatSper Ca(2+)-channel. Environ. Int. 2022, 167, 107399. [Google Scholar] [CrossRef]
- Rehfeld, A.; Dissing, S.; Skakkebaek, N.E. Chemical UV Filters Mimic the Effect of Progesterone on Ca(2+) Signaling in Human Sperm Cells. Endocrinology 2016, 157, 4297–4308. [Google Scholar] [CrossRef]
- Alavi, S.H.; Taghavi, M.M.; Moallem, S.A. Evaluation of effects of methamphetamine repeated dosing on proliferation and apoptosis of rat germ cells. Syst. Biol. Reprod. Med. 2008, 54, 85–91. [Google Scholar] [CrossRef]
- Allaeian Jahromi, Z.; Meshkibaf, M.H.; Naghdi, M.; Vahdati, A.; Makoolati, Z. Methamphetamine Downregulates the Sperm-Specific Calcium Channels Involved in Sperm Motility in Rats. ACS Omega 2022, 7, 5190–5196. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, J.; Cho, K.H.; Ren, D. A novel, single, transmembrane protein CATSPERG is associated with CATSPER1 channel protein. Biol. Reprod. 2009, 81, 539–544. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Zou, Q.; Li, B.; Chen, H.; Du, X.; Weng, S.; Luo, T.; Zeng, X. Ketamine inhibits human sperm function by Ca(2+)-related mechanism. Biochem. Biophys. Res. Commun. 2016, 478, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Xu, W.; Yuan, Y.; Chen, H.; Zheng, S.; He, Y.; Luo, T. N-Methyl-d-aspartic Acid (NMDA) Receptor Is Involved in the Inhibitory Effect of Ketamine on Human Sperm Functions. Int. J. Mol. Sci. 2021, 22, 12370. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.; Milne, S.; Leeson, H. Sperm DNA damage caused by oxidative stress: Modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod. Biomed. Online 2014, 28, 684–703. [Google Scholar] [CrossRef] [PubMed]
- Badouard, C.; Ménézo, Y.; Panteix, G.; Ravanat, J.L.; Douki, T.; Cadet, J.; Favier, A. Determination of new types of DNA lesions in human sperm. Zygote 2008, 16, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Marin, C.; Gosalvez, J.; Roy, R. Types, causes, detection and repair of DNA fragmentation in animal and human sperm cells. Int. J. Mol. Sci. 2012, 13, 14026–14052. [Google Scholar] [CrossRef]
- Tremellen, K. Oxidative stress and male infertility—A clinical perspective. Hum. Reprod. Update 2008, 14, 243–258. [Google Scholar] [CrossRef]
- Mohammadi, S.; Jalali, M.; Nikravesh, M.R.; Fazel, A.; Ebrahimzadeh, A.; Gholamin, M.; Sankian, M. Effects of Vitamin-E treatment on CatSper genes expression and sperm quality in the testis of the aging mouse. Iran. J. Reprod. Med. 2013, 11, 989–998. [Google Scholar]
- Mohammadi, S.; Movahedin, M.; Mowla, S.J. Up-regulation of CatSper genes family by selenium. Reprod. Biol. Endocrinol. 2009, 7, 126. [Google Scholar] [CrossRef]
- Agarwal, A.; Baskaran, S.; Parekh, N.; Cho, C.L.; Henkel, R.; Vij, S.; Arafa, M.; Panner Selvam, M.K.; Shah, R. Male infertility. Lancet 2021, 397, 319–333. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).