Nitric Oxide Synthesis Metabolites—As Potential Markers in Chronic Kidney Disease in Children
Abstract
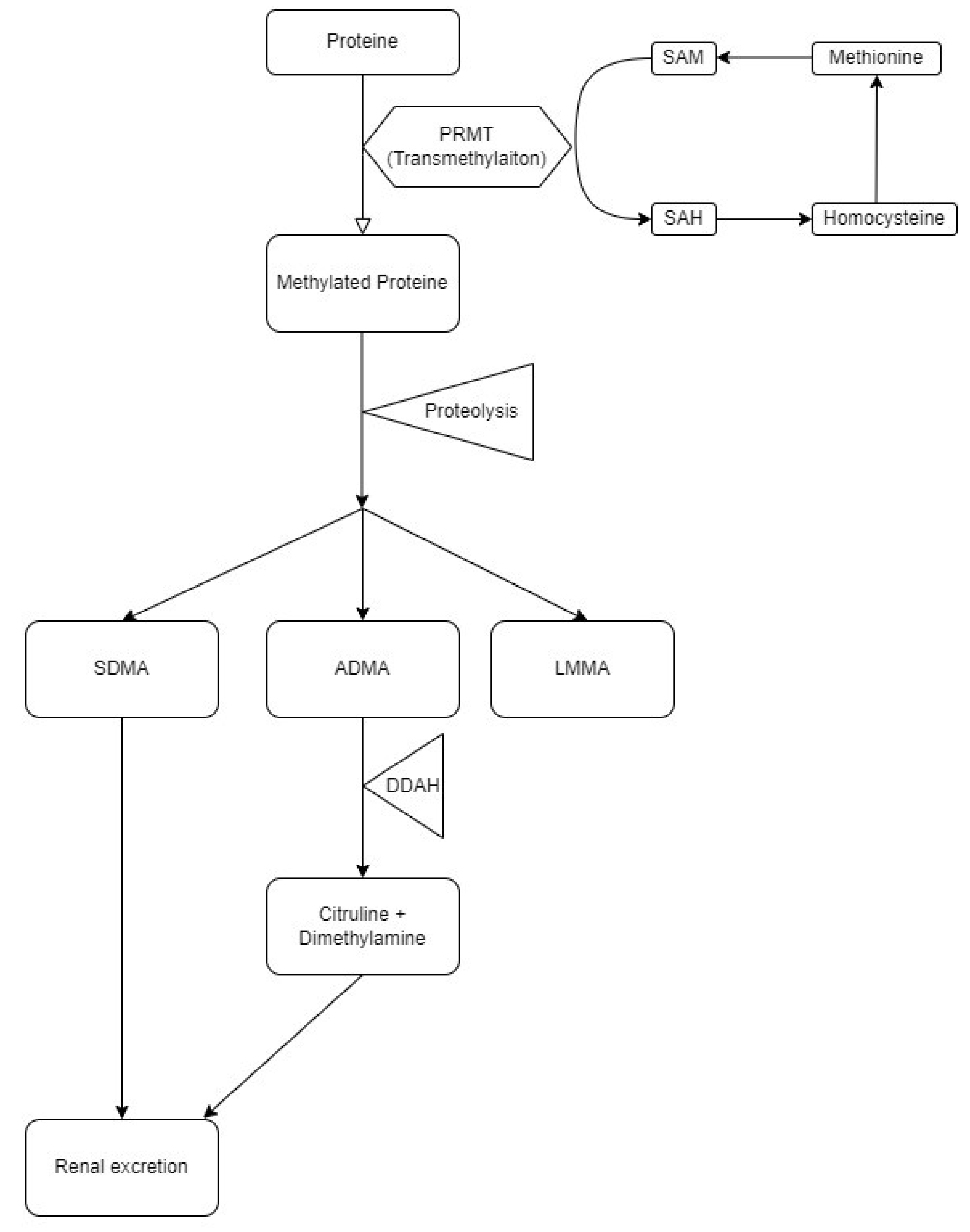
1. Introduction
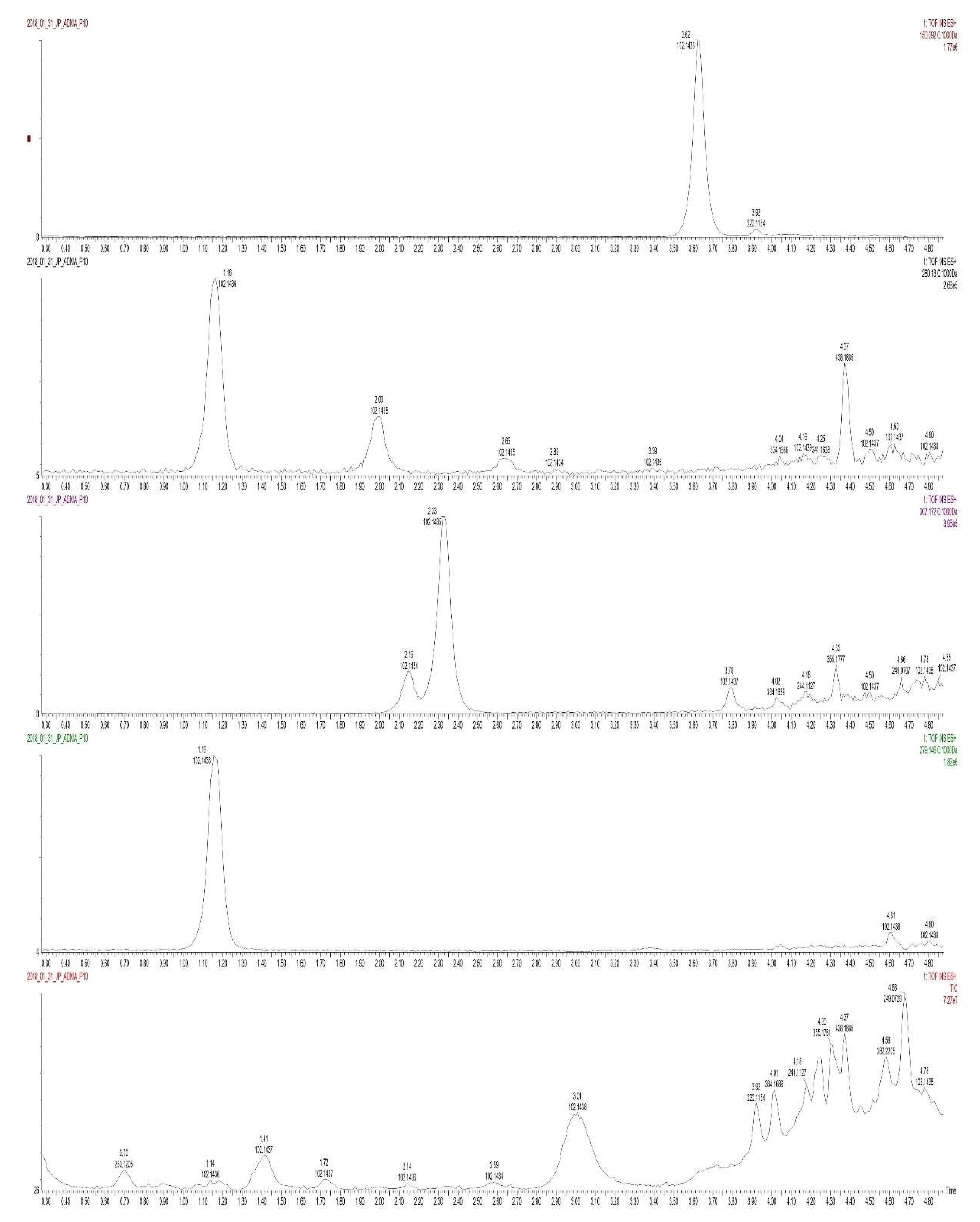
2. Materials and Methods
2.1. The Study Group
- age of 3–18 years;
- diagnosed CKD of varying degrees of progression;
- and written consent to participate in the study.
2.2. Ethical Issues
2.3. Collection of Test Material Samples
2.4. Statistical Analysis
3. Results
3.1. Clinical Characteristics
3.2. Determination of NO Synthesis Metabolites and Comparison between the Study and Control Group
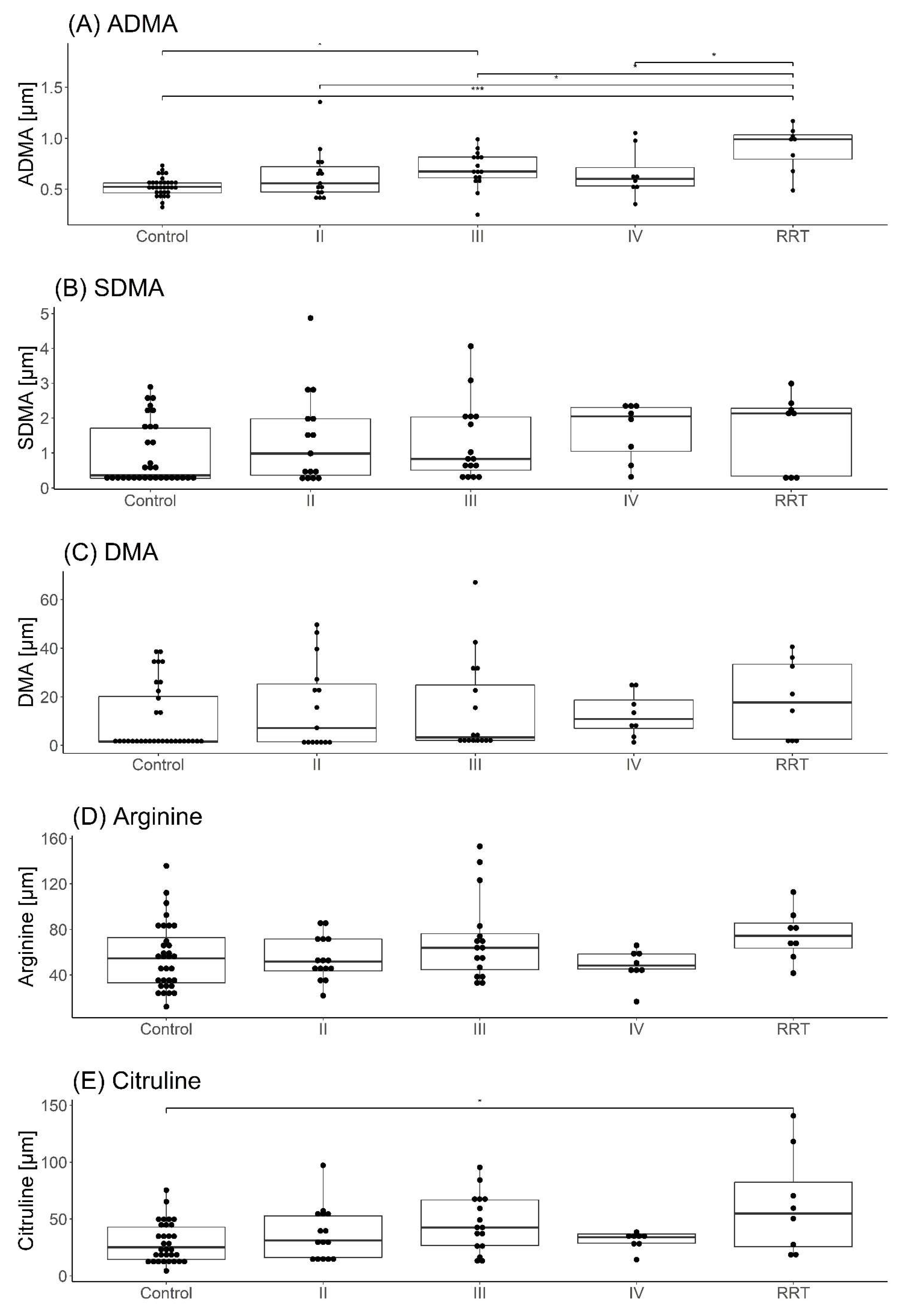
3.3. Comparison of the Results of Determinations with CKD Severity
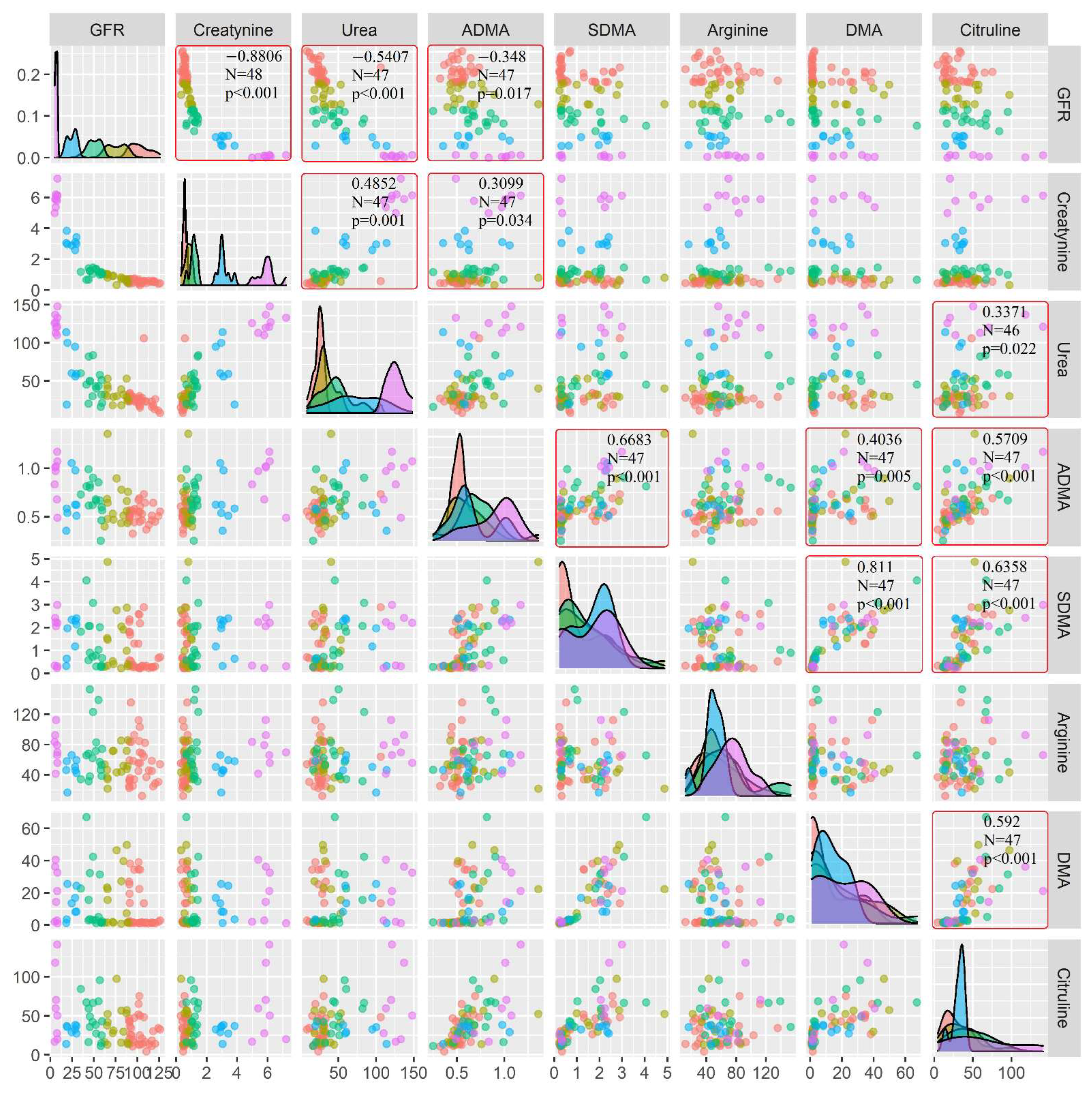
3.4. Evaluation of Relationships in the Group of Children with CKD
- ADMA and creatinine, SDMA, DMA, and citrulline;
- SDMA and DMA, citrulline;
- DMA and citrulline;
- Citrulline and urea (Figure 4).
4. Discussion
5. Limitations
6. Conclusions
- Children with CKD develop disturbances in most metabolites of NO synthesis.
- These disorders worsen with the progression of CKD.
- Dialysis children treated show the greatest disturbances of plasma ADMA and citrulline levels.
- ADMA seems to be a good indicator of the gradual progression of the CKD, which is proved by the negative correlation with eGFR.
- NO metabolites can possibly be promising markers of CKD stage and severity. Future research is needed to establish their clinical potential.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Emrich, I.E.; Zawada, A.M.; Martens-Lobenhoffer, J.; Fliser, D.; Wagenpfeil, S.; Heine, G.H.; Bode-Böger, S.M. Symmetric dimethylarginine (SDMA) outperforms asymmetric dimethylarginine (ADMA) and other methylarginines as predictor of renal and cardiovascular outcome in non-dialysis chronic kidney disease. Clin. Res. Cardiol. 2018, 107, 201–213. [Google Scholar] [CrossRef] [PubMed]
- Förstermann, U.; Sessa, W.C. Nitric oxide synthases: Regulation and function. Eur. Heart J. 2012, 33, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Ochoa-Martínez, C.; Cardona-Lozano, E.D.; Carrizales-Yáñez, L.; Pérez-Maldonado, I.N. Serum Concentrations of New Predictive Cardiovascular Disease Biomarkers in Mexican Women Exposed to Lead. Arch. Environ. Contam. Toxicol. 2018, 74, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Triches, C.B.; Quinto, M.; Mayer, S.; Batista, M.; Zanella, M.T. Relation of asymmetrical dimethylarginine levels with renal outcomes in hypertensive patients with and without type 2 diabetes mellitus. J. Diabetes Its Complicat. 2018, 32, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Otto, G.P.; Neugebauer, S.; Claus, R.A.; Sossdorf, M. Arginine metabolism is markedly impaired in polymicrobial infected mice. Crit. Care 2012, 16, 412. [Google Scholar] [CrossRef]
- Boelaert, J.; Schepers, E.; Glorieux, G.; Eloot, S.; Vanholder, R.; Lynen, F. Determination of Asymmetric and Symmetric Dimethylarginine in Serum from Patients with Chronic Kidney Disease: UPLC-MS/MS versus ELISA. Toxins 2016, 8, 149. [Google Scholar] [CrossRef]
- Lluch, P.; Mauricio, M.D.; Vila, J.M.; Segarra, G.; Medina, P.; Del Olmo, J.A.; Rodrigo, J.M.; Serra, M.A. Accumulation of Symmetric Dimethylarginine in Hepatorenal Syndrome. Exp. Biol. Med. 2006, 231, 70–75. [Google Scholar] [CrossRef]
- Morita, M.; Hayashi, T.; Ochiai, M.; Maeda, M.; Yamaguchi, T.; Ina, K.; Kuzuya, M. Oral supplementation with a combination of l-citrulline and l-arginine rapidly increases plasma l-arginine concentration and enhances NO bioavailability. Biochem. Biophys. Res. Commun. 2014, 454, 53–57. [Google Scholar] [CrossRef]
- Rysz, J.; Gluba-Brzózka, A.; Franczyk, B.; Jabłonowski, Z.; Ciałkowska-Rysz, A. Novel Biomarkers in the Diagnosis of Chronic Kidney Disease and the Prediction of Its Outcome. Int. J. Mol. Sci. 2017, 18, 1702. [Google Scholar] [CrossRef]
- Wu, G.Y.; Brosnan, J.T. Macrophages can convert citrulline into arginine. Biochem. J. 1992, 281, 45–48. [Google Scholar] [CrossRef]
- El-Sadek, A.E.; Behery, E.G.; Azab, A.A.; Kamal, N.M.; Salama, M.A.; Abdulghany, W.E.; Abdallah, E.A. Arginine dimethylation products in pediatric patients with chronic kidney disease. Ann. Med. Surg. 2016, 9, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Achan, V.; Broadhead, M.; Malaki, M.; Whitley, G.; Leiper, J.; MacAllister, R.; Vallance, P. Asymmetric Dimethylarginine Causes Hypertension and Cardiac Dysfunction in Humans and Is Actively Metabolized by Dimethylarginine Dimethylaminohydrolase. Arter. Thromb. Vasc. Biol. 2003, 23, 1455–1459. [Google Scholar] [CrossRef] [PubMed]
- Sibal, L.; Agarwal, S.C.; Home, P.D.; Boger, R.H. The Role of Asymmetric Dimethylarginine (ADMA) in Endothelial Dysfunction and Cardiovascular Disease. Curr. Cardiol. Rev. 2010, 6, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Ravani, P.; Tripepi, G.; Malberti, F.; Testa, S.; Mallamaci, F.; Zoccali, C. Asymmetrical Dimethylarginine Predicts Progression to Dialysis and Death in Patients with Chronic Kidney Disease: A Competing Risks Modeling Approach. J. Am. Soc. Nephrol. 2005, 16, 2449–2455. [Google Scholar] [CrossRef] [PubMed]
- Kielstein, J.T.; Salpeter, S.R.; Bode-Boeger, S.M.; Cooke, J.; Fliser, D. Symmetric dimethylarginine (SDMA) as endogenous marker of renal function—a meta-analysis. Nephrol. Dial. Transplant. 2006, 21, 2446–2451. [Google Scholar] [CrossRef]
- Marescau, B.; Nagels, G.; Possemiers, I.; De Broe, M.E.; Becaus, I.; Billiouw, J.M.; Lornoy, W.; De Deyn, P.P. Guanidino compounds in serum and urine of nondialyzed patients with chronic renal insufficiency. Metabolism 1997, 46, 1024–1031. [Google Scholar] [CrossRef]
- Blackwell, S.; O’Reilly, D.S.J.; Talwar, D. Biological variation of asymmetric dimethylarginine and related arginine metabolites and analytical performance goals for their measurement in human plasma. Eur. J. Clin. Investig. 2007, 37, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Hokamp, J.A.; Nabity, M.B. Renal biomarkers in domestic species. Veter.-Clin. Pathol. 2016, 45, 28–56. [Google Scholar] [CrossRef]
- Kielstein, J.T.; Fliser, D.; Veldink, H. Asymmetric dimethylarginine and symmetric dimethylarginine: Axis of evil or useful alliance? Semin. Dial. 2009, 22, 346–350. [Google Scholar] [CrossRef]
- Rao, P.N.S.; Bitla, A.R. Simultaneous determination of arginine, citrulline, and asymmetric dimethylarginine in plasma by reverse-phase high-performance liquid chromatography. J. Lab. Physicians 2017, 9, 243–248. [Google Scholar] [CrossRef]
- Schwartz, G.J.; Muñoz, A.; Schneider, M.F.; Mak, R.H.; Kaskel, F.; Warady, B.A.; Furth, S.L. New Equations to Estimate GFR in Children with CKD. J. Am. Soc. Nephrol. 2009, 20, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Graves, J.W. Diagnosis and Management of Chronic Kidney Disease. Mayo Clin. Proc. 2008, 83, 1064–1069. [Google Scholar] [CrossRef] [PubMed]
- Wiśniewski, J.; Fleszar, M.G.; Piechowicz, J.; Krzystek-Korpacka, M.; Chachaj, A.; Szuba, A.; Lorenc-Kukula, K.; Masłowski, L.; Witkiewicz, W.; Gamian, A. A novel mass spectrometry-based method for simultaneous determination of asymmetric and symmetric dimethylarginine, l -arginine and l -citrulline optimized for LC-MS-TOF and LC-MS/MS. Biomed. Chromatogr. 2017, 31, e3994. [Google Scholar] [CrossRef] [PubMed]
- Fleszar, M.G.; Wiśniewski, J.; Krzystek-Korpacka, M.; Misiak, B.; Frydecka, D.; Piechowicz, J.; Lorenc-Kukuła, K.; Gamian, A. Quantitative Analysis of l-Arginine, Dimethylated Arginine Derivatives, l-Citrulline, and Dimethylamine in Human Serum Using Liquid Chromatography–Mass Spectrometric Method. Chromatographia 2018, 81, 911–921. [Google Scholar] [CrossRef]
- Rosenberg, M.; Kalda, R.; Kasiulevicius, V.; Lember, M. Management of chronic kidney disease in primary health care: Position paper of the European Forum for Primary Care. Qual. Prim. Care 2008, 16, 279–294. [Google Scholar]
- Benito, S.; Sánchez-Ortega, A.; Unceta, N.; Jansen, J.J.; Postma, G.; Andrade, F.; Aldámiz-Echevarria, L.; Buydens, L.M.C.; Goicolea, M.A.; Barrio, R.J. Plasma biomarker discovery for early chronic kidney disease diagnosis based on chemometric approaches using LC-QTOF targeted metabolomics data. J. Pharm. Biomed. Anal. 2018, 149, 46–56. [Google Scholar] [CrossRef]
- Asmarawati, T.P.; Widodo, W.; Thaha, M.; Aditiawardana, A.; Mardiana, N.; Ardhany, A.R.; Tjempakasari, A.; Santoso, D.; Irwanadi, P.C. Comparison of Asymmetric Dimethylarginine Levels Between Stages Three, Four, and Five Non-dialysis of Chronic Kidney Disease. Acta Med. Indones. 2016, 48, 28–34. [Google Scholar]
- Benito, S.; Sánchez, A.; Unceta, N.; Andrade, F.; Aldámiz-Echevarria, L.; Goicolea, M.A.; Barrio, R.J. LC-QTOF-MS-based targeted metabolomics of arginine-creatine metabolic path-way-related compounds in plasma: Application to identify potential biomarkers in pediatric chronic kidney disease. Anal. Bioanal. Chem. 2016, 408, 747–760. [Google Scholar] [CrossRef]
- Oliva-Damaso, E.; Oliva-Damaso, N.; Rodriguez-Esparragon, F.; Payan, J.; Baamonde-Laborda, E.; Gonzalez-Cabrera, F.; Santana-Estupiñan, R.; Rodriguez-Perez, J.C. Asymmetric (ADMA) and Symmetric (SDMA) Dimethylarginines in Chronic Kidney Disease: A Clinical Approach. Int. J. Mol. Sci. 2019, 20, 3668. [Google Scholar] [CrossRef]
- Brooks, E.R.; Langman, C.B.; Wang, S.; Price, H.E.; Hodges, A.L.; Darling, L.; Yang, A.Z.; Smith, F.A. Methylated arginine derivatives in children and adolescents with chronic kidney disease. Pediatr. Nephrol. 2009, 24, 129–134. [Google Scholar] [CrossRef]
- Snauwaert, E.; Van Biesen, W.; Raes, A.; Glorieux, G.; Van Bogaert, V.; Van Hoeck, K.; Coppens, M.; Roels, S.; Walle, J.V.; Eloot, S. Concentrations of representative uraemic toxins in a healthy versus non-dialysis chronic kidney disease paediatric population. Nephrol. Dial. Transplant. 2017, 33, 978–986. [Google Scholar] [CrossRef] [PubMed]
- Schwedhelm, E.; Böger, R.H. The role of asymmetric and symmetric dimethylarginines in renal disease. Nat. Rev. Nephrol. 2011, 7, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Shafi, T.; Hostetter, T.H.; Meyer, T.W.; Hwang, S.; Hai, X.; Melamed, M.L.; Banerjee, T.; Coresh, J.; Powe, N.R. Serum Asymmetric and Symmetric Dimethylarginine and Morbidity and Mortality in Hemodialysis Patients. Am. J. Kidney Dis. 2017, 70, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-N.; Tain, Y.-L. Asymmetric Dimethylarginine (ADMA) in Pediatric Renal Diseases: From Pathophysiological Phenomenon to Clinical Biomarker and Beyond. Children 2021, 8, 837. [Google Scholar] [CrossRef]
- Lim, Y.J.; Sidor, N.A.; Tonial, N.C.; Che, A.; Urquhart, B.L. Uremic Toxins in the Progression of Chronic Kidney Disease and Cardi-ovascular Disease: Mechanisms and Therapeutic Targets. Toxins 2021, 13, 142. [Google Scholar] [CrossRef] [PubMed]
- Fleck, C.H.; Schweitzer, F.; Karge, E.; Busch, M.; Stein, G. Serum concentrations of asymmetric (ADMA) and symmetric (SDMA) dimethylarginine in patients with chronic kidney diseases. Clin. Chim. Acta 2003, 336, 1–12. [Google Scholar] [CrossRef]
- Zhang, A.; Mitchell, S.; Smith, R. Dimethylamine in human urine. Clin. Chim. Acta 1995, 233, 81–88. [Google Scholar] [CrossRef]
- Chen, J.; Hamm, L.L.; Mohler, E.R.; Hudaihed, A.; Arora, R.; Chen, C.-S.; Liu, Y.; Browne, G.; Mills, K.T.; Kleinpeter, M.A.; et al. Interrelationship of Multiple Endothelial Dysfunction Biomarkers with Chronic Kidney Disease. PLoS ONE 2015, 10, e0132047. [Google Scholar] [CrossRef]
- Lau, T.; Owen, W.; Yu, Y.M.; Noviski, N.; Lyons, J.; Zurakowski, D.; Tsay, R.; Ajami, A.; Young, V.R.; Castillo, L. Arginine, citrulline, and nitric oxide metabolism in end-stage renal disease patients. J. Clin. Investig. 2000, 105, 1217–1225. [Google Scholar] [CrossRef]
- Lin, Y.-J.; Hsu, C.-N.; Lo, M.-H.; Huang, C.-F.; Chien, S.-J.; Tain, Y.-L. High Citrulline-to-Arginine Ratio Associated With Blood Pressure Abnormalities in Children With Early Chronic Kidney Disease. Circ. J. 2013, 77, 181–187. [Google Scholar] [CrossRef]
- Martens-Lobenhoffer, J.; Bode-Böger, S.M. Simultaneous detection of arginine, asymmetric dimethylarginine, sym-metric dimethylarginine and citrulline in human plasma and urine applying liquid chromatography–mass spectrometry with very straightforward sample preparation. J. Chromatogr. B 2003, 798, 231–239. [Google Scholar] [CrossRef] [PubMed]
- DuPont, J.J.; Ramick, M.G.; Farquhar, W.B.; Townsend, R.R.; Edwards, D.G. NADPH oxidase-derived reactive oxygen species con-tribute to impaired cutaneous microvascular function in chronic kidney disease. Am. J. Physiol. Ren. Physiol. 2014, 306, 1499–1506. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Singh, P.; Khurana, S.; Ganguly, N.K.; Kukreti, R.; Saso, L.; Rana, D.S.; Taneja, V.; Bhargava, V. Implications of oxidative stress in chronic kidney disease: A review on current concepts and therapies. Kidney Res. Clin. Pract. 2021, 40, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Fliser, D.; Kielstein, J.T.; Haller, H.; Bode-Böger, S.M. Asymmetric dimethylarginine: A cardiovascular risk factor inrenal disease? Kidney Int. 2003, 63, 37. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tain, Y.-L.; Hsu, C.-N. Toxic Dimethylarginines: Asymmetric Dimethylarginine (ADMA) and Symmetric Dimethylarginine (SDMA). Toxins 2017, 9, 92. [Google Scholar] [CrossRef] [PubMed]
| Studied Parameter | Study Patient Group | Control Group | |||
|---|---|---|---|---|---|
| N | Median (IQR) | N | Median (IQR) | p-value | |
| GFR [mL/min/1.73 mpc] | 48 | 48.69 (23.36–65.38) | 33 | 102.12 (92.93–110.13) | <0.001 |
| creatinine (mg/dL) | 48 | 1.18 (0.92–3.06) | 33 | 0.55 (0.5–0.61) | <0.001 |
| inorganic phosphorus (mg/dL) | 44 | 4.9 (4.35–5.5) | 33 | 5.1 (4.6–6.1) | 0.142 |
| calcium (mg/dL) | 43 | 9.8 (9.6–10.1) | 32 | 10 (9.88–10.4) | 0.020 |
| sodium (mg/dL) | 48 | 139 (137–142) | 33 | 138 (137–140) | 0.376 |
| potassium (mg/dL) | 48 | 4.42 (4.19–4.66) | 32 | 4.3 (4.2–4.62) | 0.644 |
| urea (mg/dL) | 47 | 50 (30–89.5) | 32 | 24.5 (21.25–28.25) | <0.001 |
| Hb (g/dL) | 48 | 11.7 ± 1.51 | 33 | 14.4 ± 1.74 | <0.001 |
| Ht (%) | 48 | 34.33 ± 4.15 | 33 | 41.38 ± 4.88 | <0.001 |
| RBC [mln/mm3] | 48 | 4.14 ± 0.71 | 33 | 4.85 ± 0.55 | <0.001 |
| Studied Parameter | Study Group/CKD Group | Control Group | |
|---|---|---|---|
| N | 47 | 32 | |
| Median (IQR) | Median (IQR) | p-value | |
| ADMA [µM] | 0.66 (0.53–0.84) | 0.52 (0.47–0.56) | <0.001 |
| SDMA [µM] | 1.18 (0.38–2.17) | 0.36 (0.28–1.71) | 0.018 |
| Arginine [µM] | 57.04 (44.96–71.82) | 54.72 (33.1–72.91) | 0.230 |
| DMA [µM] | 8.08 (1.74–24.86) | 1.65 (1.28–20.15) | 0.029 |
| Citrulline [µM] | 37.01 (26.23–56.93) | 25.27 (14.38–42.89) | 0.012 |
| Control | II | III | IV | RRT | p-Value | |
|---|---|---|---|---|---|---|
| ADMA [µM] | 0.52 (0.47–0.56) | 0.56 (0.47–0.72) | 0.67 (0.61–0.82) | 0.6 (0.53–0.71) | 0.99 (0.8–1.03) | <0.001 |
| SDMA [µM] | 0.36 (0.28–1.71) | 0.99 (0.37–1.98) | 0.84 (0.51–2.03) | 2.05 (1.05–2.3) | 2.13 (0.34–2.28) | 0.14 |
| Arginine [µM] | 54.72 (33.1–72.91) | 51.82 (43.59–71.66) | 63.98 (44.64–76.33) | 48.36 (45.19–58.37) | 74.54 (63.54–85.74) | 0.151 |
| DMA [µM] | 1.65 (1.28–20.15) | 7.21 (1.46–25.27) | 3.36 (2.11–24.84) | 10.88 (6.94–18.75) | 17.73 (2.55–33.43) | 0.263 |
| Citrulline [µM] | 25.27 (14.38–42.89) | 31.16 (16.22–52.77) | 42.57 (26.77–66.72) | 34.12 (28.74–36.92) | 54.96 (25.71–82.3) | 0.048 |
| GFR [mL/min/1.73 mpc] | 102.12 (92.93–110.13) | 76.14 (65.58–85.64) | 50.53 (45.04–57.13) | 26.48 (19.3–29.08) | 6.58 (6.03–7.94) | <0.001 |
| Creatinine [mg/dL] | 0.55 (0.5–0.61) | 0.8 (0.69–0.96) | 1.17 (1.04–1.27) | 3.01 (2.94–3.18) | 5.89 (5.78–6.13) | <0.001 |
| Urea [mg/dL] | 24.5 (21.25–28.25) | 30 (27.5–39.5) | 44 (31.5–52.75) | 60 (57.5–97.5) | 126 (120–133) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piechowicz, J.; Gamian, A.; Chukwu, O.; Polak-Jonkisz, D. Nitric Oxide Synthesis Metabolites—As Potential Markers in Chronic Kidney Disease in Children. Curr. Issues Mol. Biol. 2022, 44, 3518-3532. https://doi.org/10.3390/cimb44080242
Piechowicz J, Gamian A, Chukwu O, Polak-Jonkisz D. Nitric Oxide Synthesis Metabolites—As Potential Markers in Chronic Kidney Disease in Children. Current Issues in Molecular Biology. 2022; 44(8):3518-3532. https://doi.org/10.3390/cimb44080242
Chicago/Turabian StylePiechowicz, Joanna, Andrzej Gamian, Ositadima Chukwu, and Dorota Polak-Jonkisz. 2022. "Nitric Oxide Synthesis Metabolites—As Potential Markers in Chronic Kidney Disease in Children" Current Issues in Molecular Biology 44, no. 8: 3518-3532. https://doi.org/10.3390/cimb44080242
APA StylePiechowicz, J., Gamian, A., Chukwu, O., & Polak-Jonkisz, D. (2022). Nitric Oxide Synthesis Metabolites—As Potential Markers in Chronic Kidney Disease in Children. Current Issues in Molecular Biology, 44(8), 3518-3532. https://doi.org/10.3390/cimb44080242






