Usage of DNA Fingerprinting Technology to Check Sample Error and Contamination in Molecular Laboratories
Abstract
1. Introduction
2. Materials and Methods
3. Results
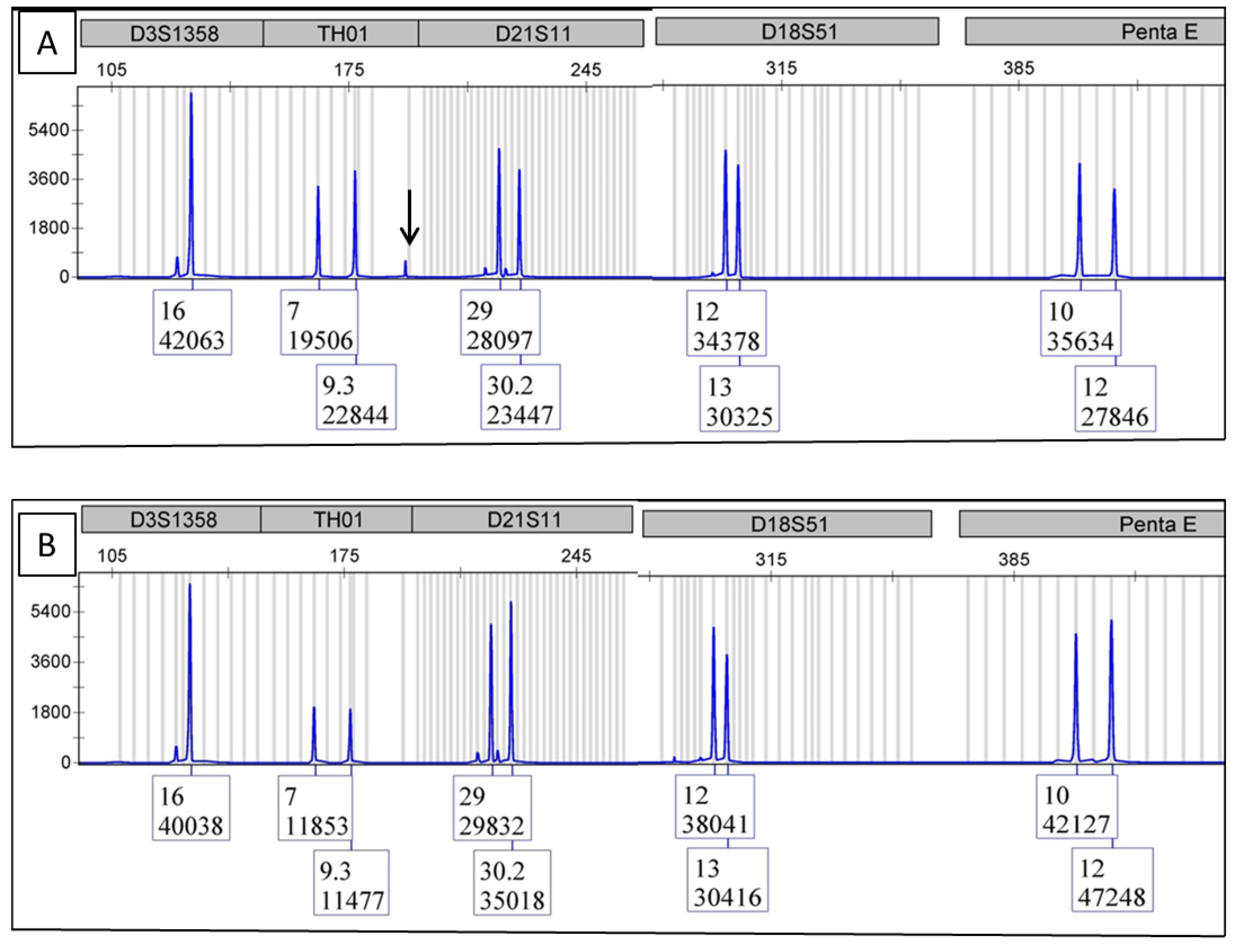
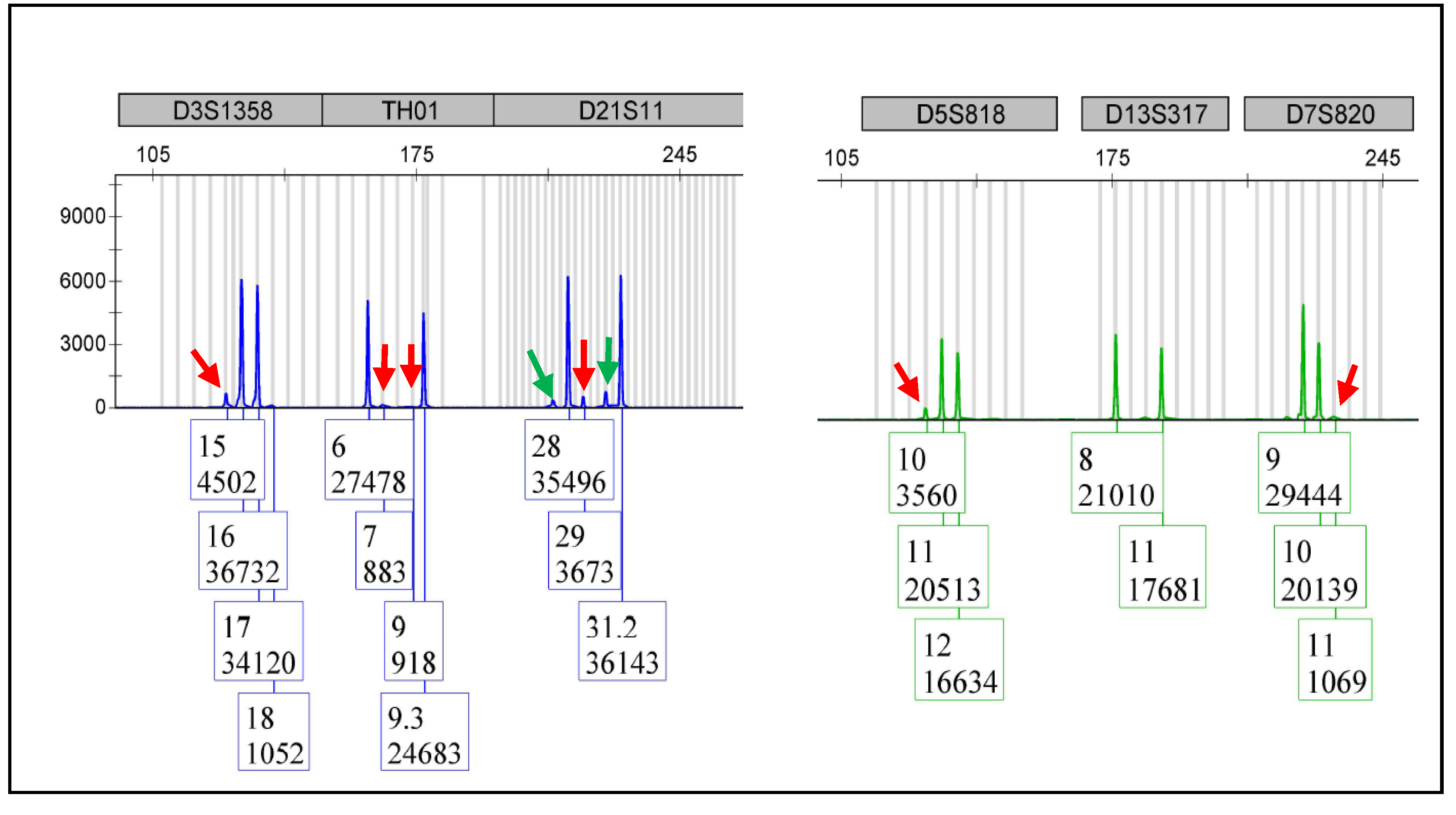
3.1. DNA Fingerprinting Test on NGS Library
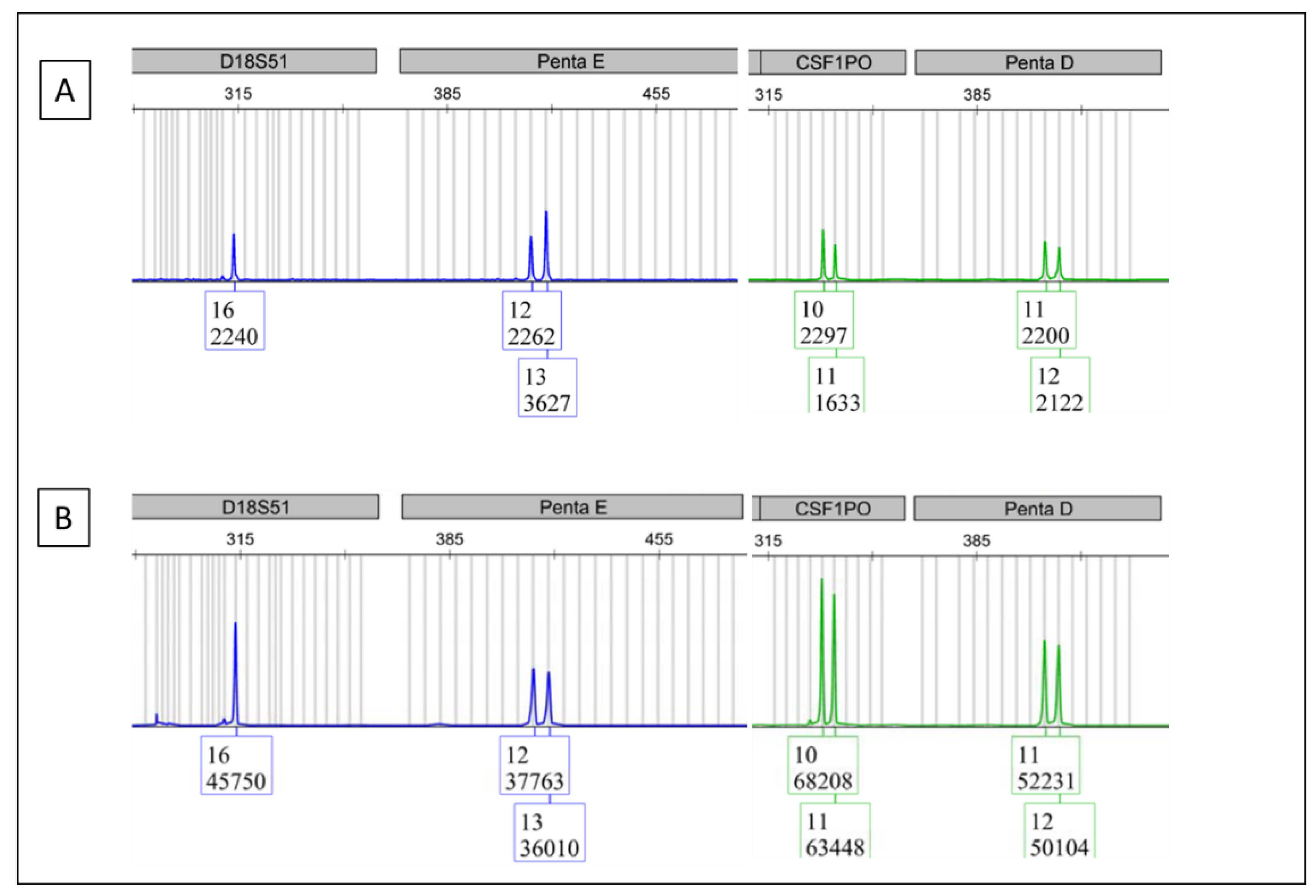
3.2. DNA Fingerprinting Test on the Samples in the BCR/ABL1 Real-Time Assay
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Logtenberg, H.; Bakker, E. The DNA fingerprint. Endeavour 1988, 12, 28–33. [Google Scholar] [CrossRef]
- Thein, S.L.; Jeffreys, A.J.; Blacklock, H.A. Identification of post-transplant cell population by DNA fingerprint analysis. Lancet 1986, 2, 37. [Google Scholar] [CrossRef]
- Van Deerlin, V.M.; Leonard, D.G. Bone marrow engraftment analysis after allogeneic bone marrow transplantation. Clin. Lab. Med. 2000, 20, 197–225. [Google Scholar] [CrossRef]
- Hampikian, G. Correcting forensic DNA errors. Forensic Sci. Int. Genet. 2019, 41, 32–33. [Google Scholar] [CrossRef] [PubMed]
- Parson, W. Age Estimation with DNA: From Forensic DNA Fingerprinting to Forensic (Epi) Genomics: A Mini-Review. Gerontology 2018, 64, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Sucher, N.J.; Hennell, J.R.; Carles, M.C. DNA fingerprinting, DNA barcoding, and next generation sequencing technology in plants. Methods Mol. Biol. 2012, 862, 13–22. [Google Scholar] [PubMed]
- McIntosh, L.Y.; Lal, J.E.; Qin, D. Usage of DNA Fingerprinting Technology for Quality Control in Molecular Lab Bench Work. Appl. Immunohistochem. Mol. Morphol. 2018, 26, 79–81. [Google Scholar] [CrossRef] [PubMed]
- Ensenberger, M.G.; Thompson, J.; Hill, B.; Homick, K.; Kearney, V.; Mayntz-Press, K.A.; Mazur, P.; McGuckian, A.; Myers, J.; Raley, K.; et al. Developmental validation of the PowerPlex 16 HS System: An improved 16-locus fluorescent STR multiplex. Forensic Sci. Int. Genet. 2010, 4, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Slatko, B.E.; Gardner, A.F.; Ausubel, F.M. Overview of Next-Generation Sequencing Technologies. Curr. Protoc. Mol. Biol. 2018, 122, e59. [Google Scholar] [CrossRef] [PubMed]
- Beillard, E.; Pallisgaard, N.; van der Velden, V.H.; Bi, W.; Dee, R.; van der Schoot, E.; Delabesse, E.; MacIntyre, E.; Gottardi, E.; Saglio, G.; et al. Evaluation of candidate control genes for diagnosis and residual disease detection in leukemic patients using ‘real-time’ quantitative reverse-transcriptase polymerase chain reaction (RQ-PCR)—A Europe against cancer program. Leukemia 2003, 17, 2474–2486. [Google Scholar] [CrossRef] [PubMed]
- Gabert, J.; Beillard, E.; van der Velden, V.H.; Bi, W.; Grimwade, D.; Pallisgaard, N.; Barbany, G.; Cazzaniga, G.; Cayuela, J.M.; Cavé, H.; et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia—A Europe Against Cancer program. Leukemia 2003, 17, 2318–2357. [Google Scholar] [CrossRef] [PubMed]
- Hares, D.R. Selection and implementation of expanded CODIS core loci in the United States. Forensic Sci. Int. Genet. 2015, 17, 33–34. [Google Scholar] [CrossRef] [PubMed]
- Gill, P.; Fereday, L.; Morling, N.; Schneider, P.M. The evolution of DNA databases--recommendations for new European STR loci. Forensic Sci. Int. 2006, 156, 242–244. [Google Scholar] [CrossRef] [PubMed]
- Gill, P.; Fereday, L.; Morling, N.; Schneider, P.M. New multiplexes for Europe-amendments and clarification of strategic development. Forensic Sci. Int. 2006, 163, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Rodovalho, R.G.; Rodrigues, E.L.; Santos, G.S.; Cavalcanti, L.M.; Lima, P.R.; Rodovalho, A.G.; Vital, R.G.; Gigonzac, M.A.D.; da Cruz, A.D. Development of a polymorphic short tandem repeat locus multiplex system for efficient human identification. Genet. Mol. Res. 2017, 16, 1–9. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qin, D.; Forster, M.; Gandhi, S.M.; Akabari, R.; Zheng, Z.; Lal, J.; Lovinger, K. Usage of DNA Fingerprinting Technology to Check Sample Error and Contamination in Molecular Laboratories. Curr. Issues Mol. Biol. 2022, 44, 5543-5549. https://doi.org/10.3390/cimb44110375
Qin D, Forster M, Gandhi SM, Akabari R, Zheng Z, Lal J, Lovinger K. Usage of DNA Fingerprinting Technology to Check Sample Error and Contamination in Molecular Laboratories. Current Issues in Molecular Biology. 2022; 44(11):5543-5549. https://doi.org/10.3390/cimb44110375
Chicago/Turabian StyleQin, Dahui, Mark Forster, Shital M. Gandhi, Ratilal Akabari, Zhong Zheng, Janella Lal, and Katherine Lovinger. 2022. "Usage of DNA Fingerprinting Technology to Check Sample Error and Contamination in Molecular Laboratories" Current Issues in Molecular Biology 44, no. 11: 5543-5549. https://doi.org/10.3390/cimb44110375
APA StyleQin, D., Forster, M., Gandhi, S. M., Akabari, R., Zheng, Z., Lal, J., & Lovinger, K. (2022). Usage of DNA Fingerprinting Technology to Check Sample Error and Contamination in Molecular Laboratories. Current Issues in Molecular Biology, 44(11), 5543-5549. https://doi.org/10.3390/cimb44110375





