The Impact of Relapses on Pain and Quality of Life in Patients with Multiple Sclerosis Treated with Corticosteroids
Abstract
1. Introduction
2. Results
Correlation between Pain and Physical and Psychological Impairment
3. Discussion
3.1. MS Relapses Were Associated with Pain
3.2. Worsening of Pain Is Associated with Worsening of Physical and Psychological Well-Being
3.3. Pain Significantly Impairs Quality of Life
3.4. Limitations
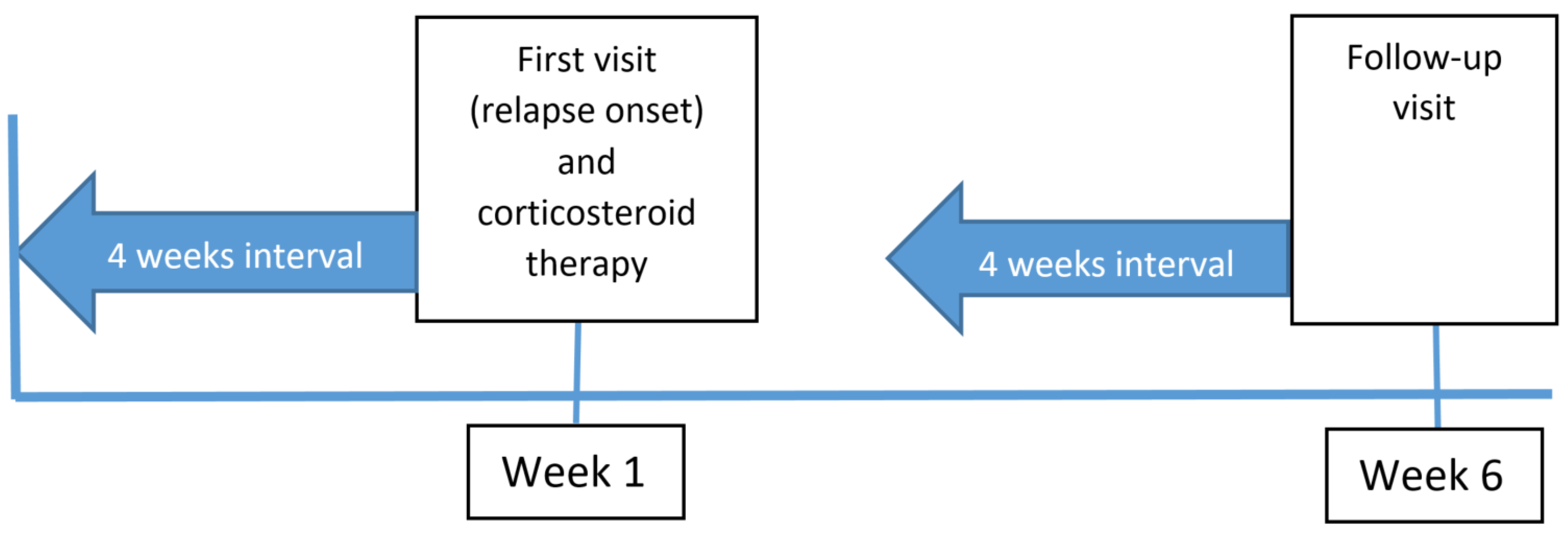
4. Materials and Methods
4.1. Patients
4.2. Clinical Evaluation
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sander, L.; Kugler, J.; Elsner, B. The Influence of Multiple Sclerosis-Related Symptoms on Health-Related Quality of Life. Fortschritte Neurol. Psychiatr. 2020, 88, 704–712. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Benito-León, J.; González, J.-M.M.; Rivera-Navarro, J. Quality of Life and Its Assessment in Multiple Sclerosis: Integrating Physical and Psychological Components of Wellbeing. Lancet Neurol. 2005, 4, 556–566. [Google Scholar] [CrossRef]
- Young, J.; Amatya, B.; Galea, M.P.; Khan, F. Chronic Pain in Multiple Sclerosis: A 10-Year Longitudinal Study. Scand. J. Pain 2017, 16, 198–203. [Google Scholar] [CrossRef]
- Veličkaitė, G.; Jucevičiūtė, N.; Balnytė, R.; Laucius, O.; Vaitkus, A. Pain Characteristics and Associations with Quality of Life in Patients with Multiple Sclerosis in Lithuania. Medicina 2020, 56, 596. [Google Scholar] [CrossRef]
- Gil-González, I.; Martín-Rodríguez, A.; Conrad, R.; Pérez-San-Gregorio, M.Á. Quality of Life in Adults with Multiple Sclerosis: A Systematic Review. BMJ Open 2020, 10, e041249. [Google Scholar] [CrossRef]
- O’Connor, A.B.; Schwid, S.R.; Herrmann, D.N.; Markman, J.D.; Dworkin, R.H. Pain Associated with Multiple Sclerosis: Systematic Review and Proposed Classification. Pain 2008, 137, 96–111. [Google Scholar] [CrossRef]
- Martinelli Boneschi, F.; Colombo, B.; Annovazzi, P.; Martinelli, V.; Bernasconi, L.; Solaro, C.; Comi, G. Lifetime and Actual Prevalence of Pain and Headache in Multiple Sclerosis. Mult. Scler. J. 2008, 14, 514–521. [Google Scholar] [CrossRef]
- Heitmann, H.; Haller, B.; Tiemann, L.; Mühlau, M.; Berthele, A.; Tölle, T.R.; Salmen, A.; Ambrosius, B.; Bayas, A.; Asseyer, S.; et al. Longitudinal Prevalence and Determinants of Pain in Multiple Sclerosis: Results from the German National Multiple Sclerosis Cohort Study. Pain 2020, 161, 787–796. [Google Scholar] [CrossRef]
- Foley, P.L.; Vesterinen, H.M.; Laird, B.J.; Sena, E.S.; Colvin, L.A.; Chandran, S.; MacLeod, M.R.; Fallon, M.T. Prevalence and Natural History of Pain in Adults with Multiple Sclerosis: Systematic Review and Meta-Analysis. Pain 2013, 154, 632–642. [Google Scholar] [CrossRef]
- Svendsen, K.B.; Jensen, T.S.; Overvad, K.; Hansen, H.J.; Koch-Henriksen, N.; Bach, F.W. Pain in Patients with Multiple Sclerosis. Arch. Neurol. 2003, 60, 1089. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Bjorner, J.B.; Turner-Bowker, D.M.B.G.; Maruish, M.E. User’s Manual for the SF-36v2 Health Survey; Quality Metric Incorporated: Lincoln, RI, USA, 2007; ISBN 1891810162/9781891810169. [Google Scholar]
- Bowling, A.; Bond, M.; Jenkinson, C.; Lamping, D.L. Short Form 36 (SF-36) Health Survey Questionnaire: Which Normative Data Should Be Used? Comparisons between the Norms Provided by the Omnibus Survey in Britain, the Health Survey for England and the Oxford Healthy Life Survey. J. Public Health Med. 1999, 21, 255–270. [Google Scholar] [CrossRef] [PubMed]
- Burholt, V.; Nash, P. Short Form 36 (SF-36) Health Survey Questionnaire: Normative Data for Wales. J. Public Health 2011, 33, 587–603. [Google Scholar] [CrossRef]
- Knowles, L.M.; Phillips, K.M.; Herring, T.E.; Alschuler, K.N.; Jensen, M.P.; Turner, A.P.; Ehde, D.M. Pain Intensity and Pain Interference in People with Progressive Multiple Sclerosis Compared with People with Relapsing-Remitting Multiple Sclerosis. Arch. Phys. Med. Rehabil. 2021, 102, 1959–1964. [Google Scholar] [CrossRef] [PubMed]
- Tutuncu, M.; Ertem, D.H.; Soysal, A. Prevalence and Impact of Myofascial Pain Syndrome in Relapsing-Remitting Multiple Sclerosis and The Effects of Local Anesthetic Injections For Short-Term Treatment. Mult. Scler. Relat. Disord. 2020, 46, 102528. [Google Scholar] [CrossRef]
- Michalski, D. Pain in Patients with Multiple Sclerosis: A Complex Assessment Including Quantitative and Qualitative Measurements Provides for a Disease-Related Biopsychosocial Pain Model. J. Pain Res. 2011, 4, 219. [Google Scholar] [CrossRef][Green Version]
- Ata, E.; Ozsoy-Unubol, T.; Demir, S. Evaluation of Neuropathic Extremity Pain in Patients with Multiple Sclerosis. Arch. Neuropsychiatry 2019, 58, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Moulin, D.E.; Foley, K.M.; Ebers, G.C. Pain Syndromes in Multiple Sclerosis. Neurology 1988, 38, 1830–1834. [Google Scholar] [CrossRef]
- Da Silva, J.V.M.; de Oliveira, B.F.A.; Nascimento, O.J.M.D.; Farinhas, J.G.D.; Cavaliere, M.G.; Cal, H.d.S.R.; Matta, A.P.d.C. Increased Multiple Sclerosis Relapses Related to Lower Prevalence of Pain. Arq. Neuropsiquiatr. 2015, 73, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Forbes, A.; While, A.; Mathes, L.; Griffiths, P. Health Problems and Health-Related Quality of Life in People with Multiple Sclerosis. Clin. Rehabil. 2006, 20, 67–78. [Google Scholar] [CrossRef]
- Somerset, M.; Peters, T.J.; Sharp, D.J.; Campbell, R. Factors That Contribute to Quality of Life Outcomes Prioritised by People with Multiple Sclerosis. Qual. Life Res. 2003, 12, 21–29. [Google Scholar] [CrossRef]
- Spain, L.A.; Tubridy, N.; Kilpatrick, T.J.; Adams, S.J.; Holmes, A.C.N. Illness Perception and Health-Related Quality of Life in Multiple Sclerosis. Acta Neurol. Scand. 2007, 116, 293–299. [Google Scholar] [CrossRef]
- Janardhan, V.; Bakshi, R. Quality of Life in Patients with Multiple Sclerosis. J. Neurol. Sci. 2002, 205, 51–58. [Google Scholar] [CrossRef]
- Tedman, B.; Young, C.; Williams, I. Assessment of Depression in Patients with Motor Neuron Disease and Other Neurologically Disabling Illness. J. Neurol. Sci. 1997, 152, s75–s79. [Google Scholar] [CrossRef]
- Zhao, Z.; Zhang, Y.; Du, Q.; Chen, H.; Shi, Z.; Wang, J.; Qiu, Y.; Yan, C.; Zhou, H. Differences in Physical, Mental, and Social Functions between Males and Females in Multiple Sclerosis: A Multicenter Cross-Sectional Study in China. Mult. Scler. Relat. Disord. 2021, 48, 102693. [Google Scholar] [CrossRef]
- Łabuz-Roszak, B.; Niewiadomska, E.; Kubicka-Bączyk, K.; Skrzypek, M.; Tyrpień-Golder, K.; Majewska, A.; Matejczyk, A.; Dobrakowski, P.; Pierzchała, K. Prevalence of Pain in Patients with Multiple Sclerosis and Its Association with Anxiety, Depressive Symptoms and Quality of Life. Psychiatr. Pol. 2019, 53, 475–486. [Google Scholar] [CrossRef]
- Seixas, D.; Foley, P.; Palace, J.; Lima, D.; Ramos, I.; Tracey, I. Pain in Multiple Sclerosis: A Systematic Review of Neuroimaging Studies. NeuroImage Clin. 2014, 5, 322–331. [Google Scholar] [CrossRef]
- Truini, A.; Aleksovska, K.; Anderson, C.C.; Attal, N.; Baron, R.; Bennett, D.L.; Bouhassira, D.; Cruccu, G.; Eisenberg, E.; Enax-Krumova, E.; et al. Joint European Academy of Neurology–European Pain Federation–Neuropathic Pain Special Interest Group of the International Association for the Study of Pain Guidelines on Neuropathic Pain Assessment. Eur. J. Neurol. 2023, 30, 2177–2196. [Google Scholar] [CrossRef]
- Chataway, J.; Porter, B.; Riazi, A.; Heaney, D.; Watt, H.; Hobart, J.; Thompson, A. Home versus Outpatient Administration of Intravenous Steroids for Multiple-Sclerosis Relapses: A Randomised Controlled Trial. Lancet Neurol. 2006, 5, 565–571. [Google Scholar] [CrossRef]
- Rakusa, M.; Cano, S.J.; Porter, B.; Riazi, A.; Thompson, A.J.; Chataway, J.; Hardy, T.A. A Predictive Model for Corticosteroid Response in Individual Patients with MS Relapses. PLoS ONE 2015, 10, e0120829. [Google Scholar] [CrossRef]
| With Pain | No Pain | Total | ||||
|---|---|---|---|---|---|---|
| At relapse onset a | ||||||
| N | 86 (74%) | 31 (26%) | 117 (100%) | |||
| Female | 71 (18%) | 21 (61%) | 92 (79%) | |||
| No./Mean (SD) | CI | No./Mean (SD) | CI | Mean (SD) | CI | |
| Age | 37.8 (7.8) | 36.1–39.4 | 39.9 (11.2) | 35.9–44.0 | 38.3 (8.8) | 36.7–39.9 |
| Number of relapses in last 2 years | 2.3 (1.4) | 2.0–2.6 | 1.3 (1.0) | 0.9–1.7 | 2.0 (1.4) | 1.8–2.3 |
| Years since diagnosis | 6.7 (6.2) | 5.4–8.1 | 8.2 (8.0) | 5.2–11.2 | 7.1 (6.7) | 5.9–8.4 |
| EDSS | 5.0 (1.3) | 4.7–5.3 | 4.7 (1.5) | 4.1–5.2 | 4.9 (1.4) *** | 4.6–5.1 |
| MSIS-29PHY | 67.2 (20.0) *** | 62.9–71.5 | 41.0 (25.8) | 31.6–50.5 | 60.3 (24.5) *** | 55.8–64.7 |
| MSIS-29PSY | 61.7 (22.8) *** | 56.8–66.6 | 36.5 (22.6) | 27.9–45.1 | 55.3 (25.2) *** | 50.7–60.0 |
| MSWS-12 | 74.6 (23.9) | 69.4–79.7 | 49.7 (32.1) | 37.7–61.7 | 68.1 (28.3) *** | 62.9–73.3 |
| SF-36 categories | ||||||
| Emotional role functioning | 37.2 (43.8) | 27.8–46.6 | 53.8 (46.9) | 36.6–71.0 | 41.6 (45.0) | 33.3–49.8 |
| Physical role functioning | 8.1 (22.2) *** | 3.4–12.9 | 29.0 (37.7) | 15.2–42.9 | 13.7 (28.5) ** | 8.5–18.9 |
| Bodily pain | 37.6 (21.6) *** | 32.9–42.2 | 95.9 (7.1) | 93.3–98.5 | 53.0 (32.0) ** | 47.2–58.9 |
| Vitality | 27.1 (18.6) *** | 23.1–31.0 | 43.2 (25.5) | 33.9–52.6 | 31.3 (21.8) ** | 27.4–35.3 |
| General health perceptions | 41.7 (21.5) *** | 37.0–46.4 | 61.1 (23.5) | 52.5–69.7 | 46.9 (23.6) | 42.6–51.3 |
| Social role functioning | 37.4 (26.1) *** | 31.8–43.0 | 56.9 (27.2) | 46.9–66.8 | 42.5 (27.7) *** | 37.5–47.6 |
| Physical functioning | 32.9 (25.2) | 27.5–38.3 | 57.7 (33.8) | 45.3–70.1 | 39.5 (29.7) * | 34.0–44.9 |
| Mental health | 53.3 (21.6) *** | 48.6–57.9 | 68.0 (19.7) | 60.8–75.2 | 57.2 (22.1) ** | 53.1–61.2 |
| Six weeks after relapse onset b | ||||||
| N | 73 (65%) | 39 (35%) | 112 (100%) | |||
| Female | 59 (53%) | 28 (25%) | 87 (78%) | |||
| Age | 38.7 (8.7) | 36.6–40.7 | 38.8 (8.9) | 35.9–41.6 | 38.3 (8.8) | 36.7–39.9 |
| Number of relapses in last 2 years | 2.0 (1.5) | 1.7–2.4 | 1.9 (1.3) | 1.5–2.3 | 2.0 (1.4) | 1.8–2.3 |
| Years since diagnosis | 6.7 (5.9) | 5.3–8.1 | 7.9 (8.1) | 5.2–10.6 | 7.1 (6.7) | 5.9–8.4 |
| EDSS | 3.9 (1.7) | 3.5–4.3 | 3.8 (2.1) | 3.1–4.5 | 3.9 (1.8) | 3.5–4.2 |
| MSIS-29PHY | 45.1 (23.0) *** | 39.6–50.7 | 26.7 (25.3) | 18.5–34.9 | 38.4 (25.4) | 33.5–43.3 |
| MSIS-29PSY | 42.7 (26.0) *** | 36.4–49.0 | 26.3 (22.8) | 18.9–33.7 | 36.7 (26.1) | 31.7–41.7 |
| MSWS-12 | 53.9 (26.8) *** | 47.6–60.1 | 35.1 (32.5) | 24.5–45.6 | 47.3 (30.2) | 41.7–53.0 |
| SF-36 categories | ||||||
| Emotional role functioning | 40.0 (42.9) *** | 29.9–50.0 | 70.9 (42.7) | 57.1–84.8 | 50.7 (45.2) | 42.3–59.2 |
| Physical role functioning | 14.9 (26.8) *** | 8.6–21.2 | 48.7 (43.7) | 34.6–62.9 | 26.8 (37.2) | 19.8–33.8 |
| Bodily pain | 46.9 (19.9) *** | 42.2–51.5 | 93.7 (8.0) | 91.1–96.4 | 63.2 (28.0) | 58.0–68.4 |
| Vitality | 34.5 (19.5) *** | 29.9–39.0 | 49.6 (24.1) | 41.7–57.4 | 39.8 (22.3) | 35.6–44.0 |
| General health perceptions | 46.2 (23.7) ** | 40.6–51.9 | 57.7 (22.9) | 50.3–65.2 | 50.3 (24.0) | 45.8–54.9 |
| Social role functioning | 47.6 (27.8) *** | 41.1–54.1 | 74.7 (26.0) | 66.2–83.1 | 57.0 (30.0) | 51.4–62.6 |
| Physical functioning | 41.2 (22.5) *** | 35.9–46.5 | 60.0 (33.8) | 49.0–71.0 | 47.8 (28.3) | 42.5–53.1 |
| Mental health | 59.5 (20.2) *** | 54.7–64.3 | 74.0 (21.8) | 66.9–81.0 | 64.6 (21.8) | 60.5–68.8 |
| Severity of Pain | At Relapse Onset (n = 117) | Six Weeks after Relapse Onset (n = 112) a | Changes |
|---|---|---|---|
| none | 24 (20.5%) | 25 (21.4%) | 0.9% |
| very mild | 14 (12.0%) | 24 (20.5%) | 8.5% |
| mild | 14 (12.0%) | 23 (19.7%) | 7.7% |
| moderate | 33 (28.2%) | 23 (19.7%) | −8.5% |
| severe | 23 (19.7%) | 15 (12.8%) | −6.8% |
| very severe | 9 (7.7%) | 2 (1.7%) | −6.0% |
| At Relapse Onset a | Six Weeks after Relapse Onset b | |||
|---|---|---|---|---|
| R | p | r | p | |
| Age | 0.043 | 0.649 | 0.051 | 0.594 |
| Number of relapses in last 2 years | −0.248 | 0.007 | −0.097 | 0.313 |
| Years since diagnosis | 0.047 | 0.624 | 0.103 | 0.281 |
| EDSS | −0.118 | 0.206 | −0.071 | 0.473 |
| MSIS-29PHY | −0.506 | <0.001 | −0.522 | <0.001 |
| MSIS-29PSY | −0.472 | <0.001 | −0.445 | <0.001 |
| MSWS-12 | −0.417 | <0.001 | −0.379 | <0.001 |
| SF-36 categories | ||||
| Emotional role functioning | 0.243 | 0.008 | 0.339 | <0.001 |
| Physical role functioning | 0.381 | <0.001 | 0.480 | <0.001 |
| Vitality | 0.379 | <0.001 | 0.503 | <0.001 |
| General health perceptions | 0.378 | <0.001 | 0.354 | <0.001 |
| Social role functioning | 0.385 | <0.001 | 0.536 | <0.001 |
| Physical functioning | 0.418 | <0.001 | 0.414 | <0.001 |
| Mental health | 0.325 | <0.001 | 0.400 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rakusa, M.; Chataway, J.; Hardy, T.A. The Impact of Relapses on Pain and Quality of Life in Patients with Multiple Sclerosis Treated with Corticosteroids. Pharmaceuticals 2023, 16, 1244. https://doi.org/10.3390/ph16091244
Rakusa M, Chataway J, Hardy TA. The Impact of Relapses on Pain and Quality of Life in Patients with Multiple Sclerosis Treated with Corticosteroids. Pharmaceuticals. 2023; 16(9):1244. https://doi.org/10.3390/ph16091244
Chicago/Turabian StyleRakusa, Martin, Jeremy Chataway, and Todd A. Hardy. 2023. "The Impact of Relapses on Pain and Quality of Life in Patients with Multiple Sclerosis Treated with Corticosteroids" Pharmaceuticals 16, no. 9: 1244. https://doi.org/10.3390/ph16091244
APA StyleRakusa, M., Chataway, J., & Hardy, T. A. (2023). The Impact of Relapses on Pain and Quality of Life in Patients with Multiple Sclerosis Treated with Corticosteroids. Pharmaceuticals, 16(9), 1244. https://doi.org/10.3390/ph16091244







