Development of Diclofenac Sodium 3D Printed Cylindrical and Tubular-Shaped Tablets through Hot Melt Extrusion and Fused Deposition Modelling Techniques
Abstract
1. Introduction
2. Results and Discussion
2.1. Preliminary Formulation Experiments
2.2. QTPP of 3D Printed Tablets
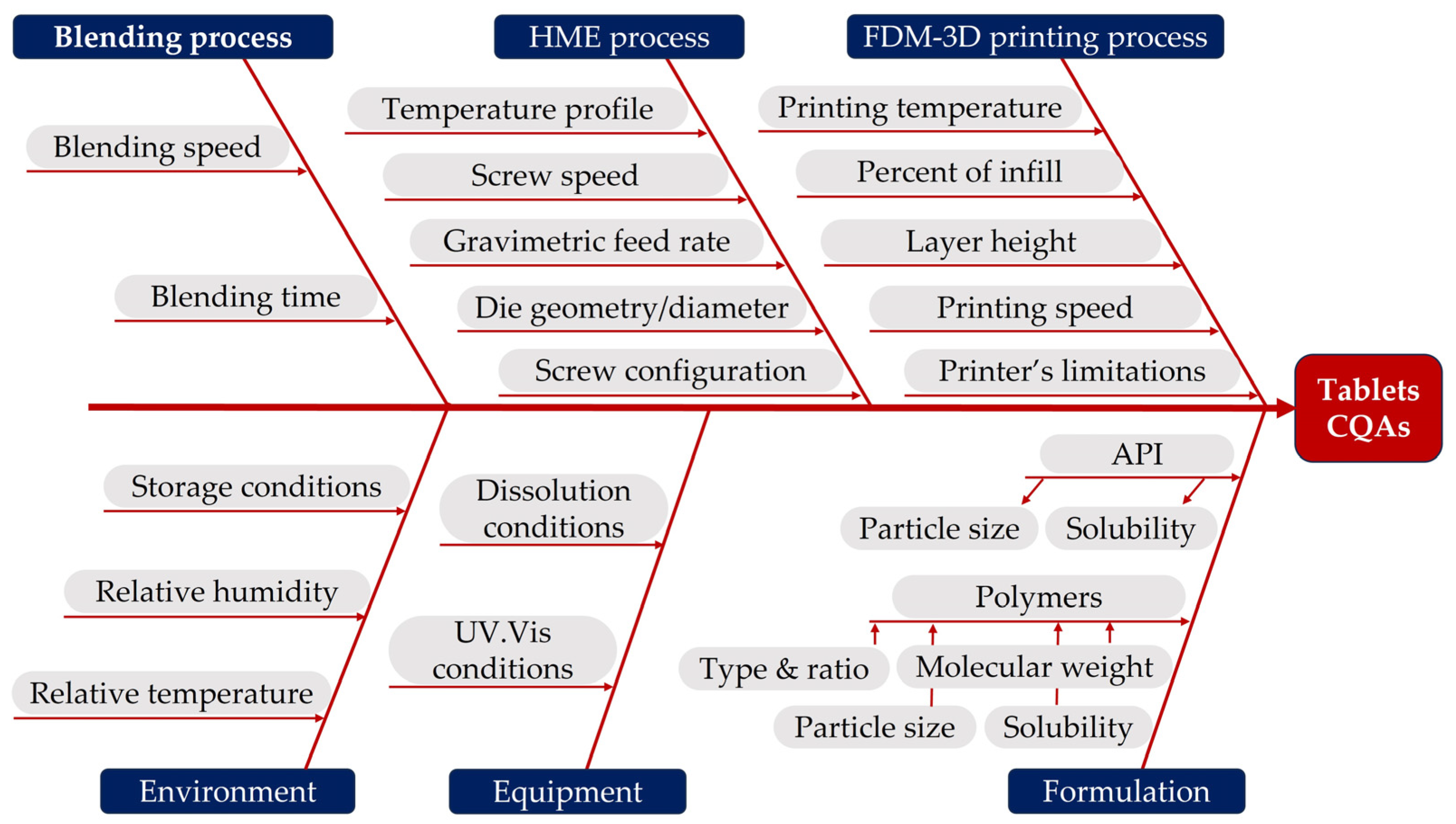
2.3. Risk Identification and Evaluation
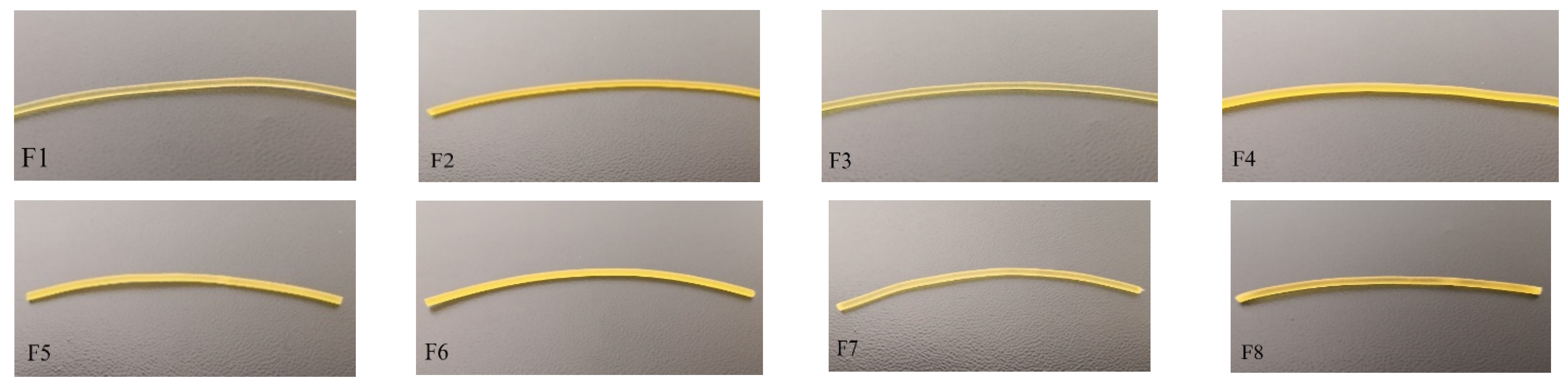
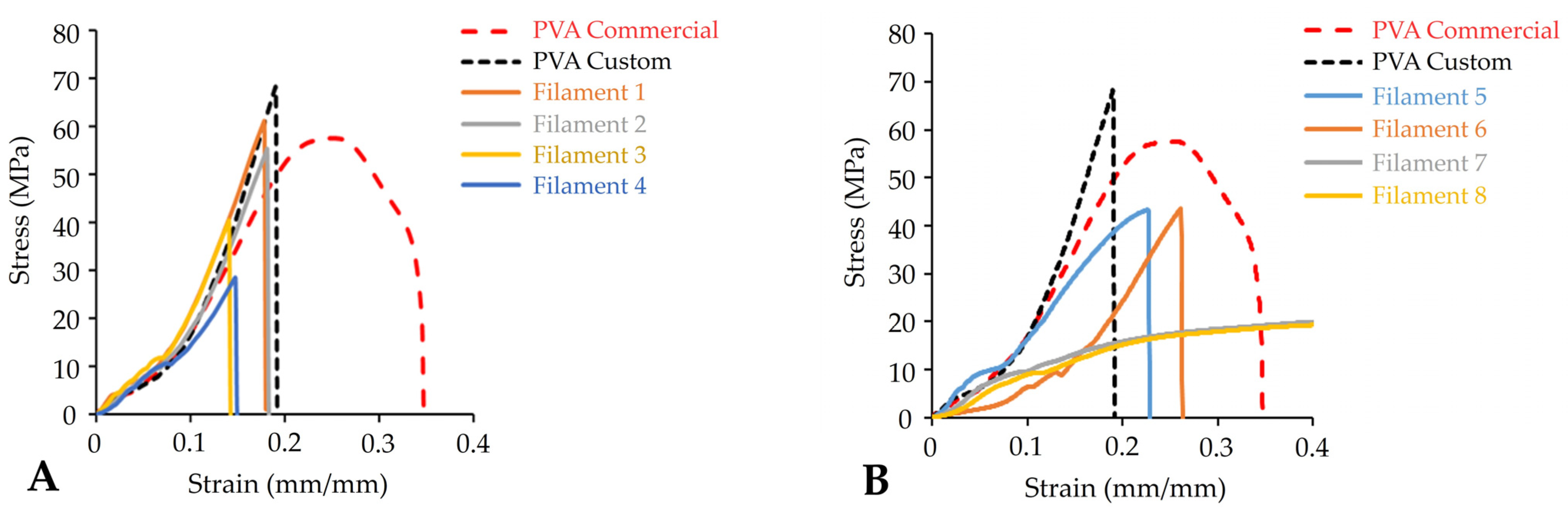
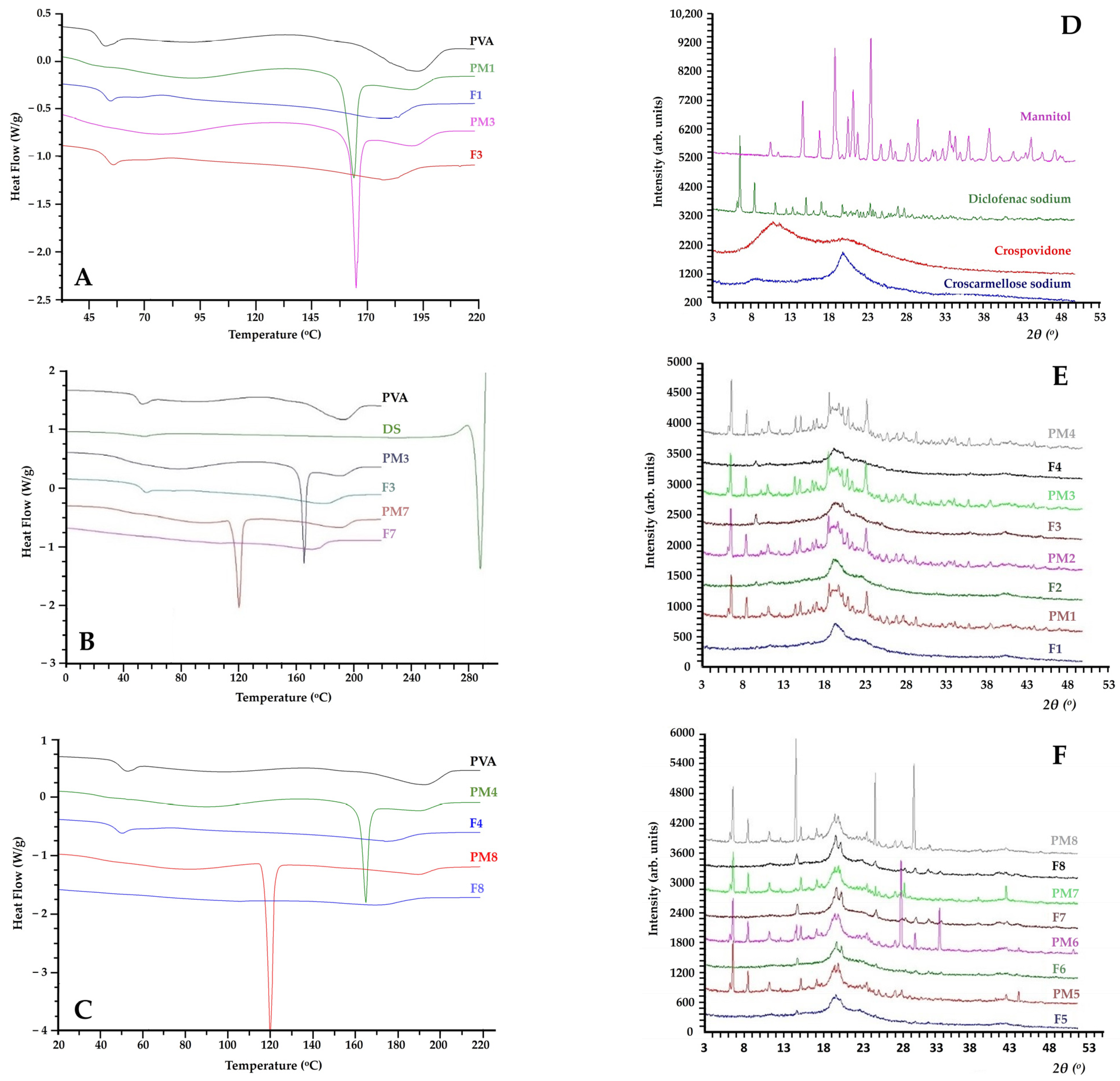
2.4. Filaments’ Preparation and Characterisation
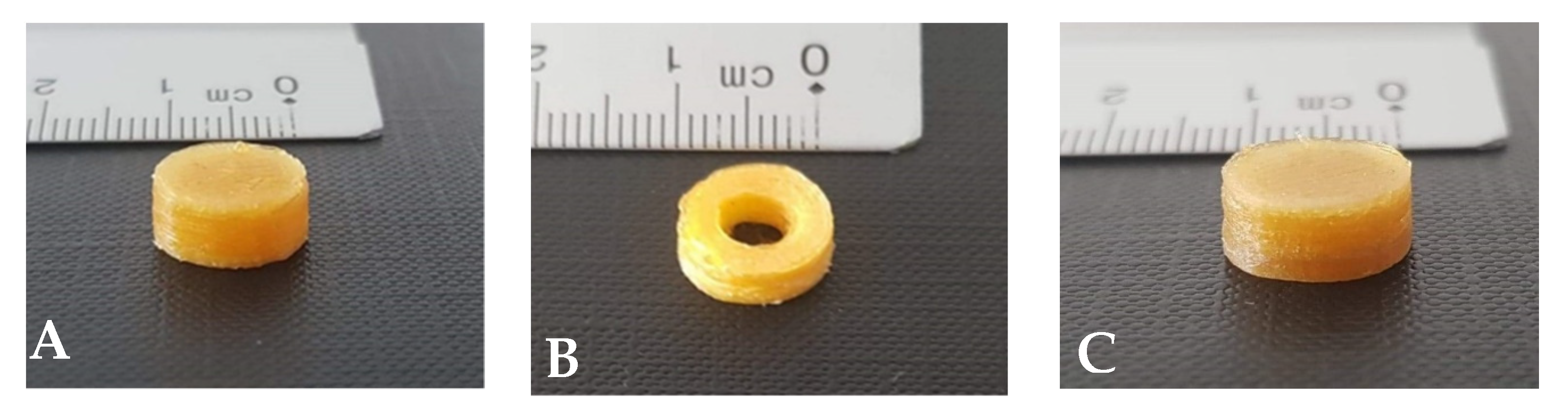
2.5. 3D Printed Tablets
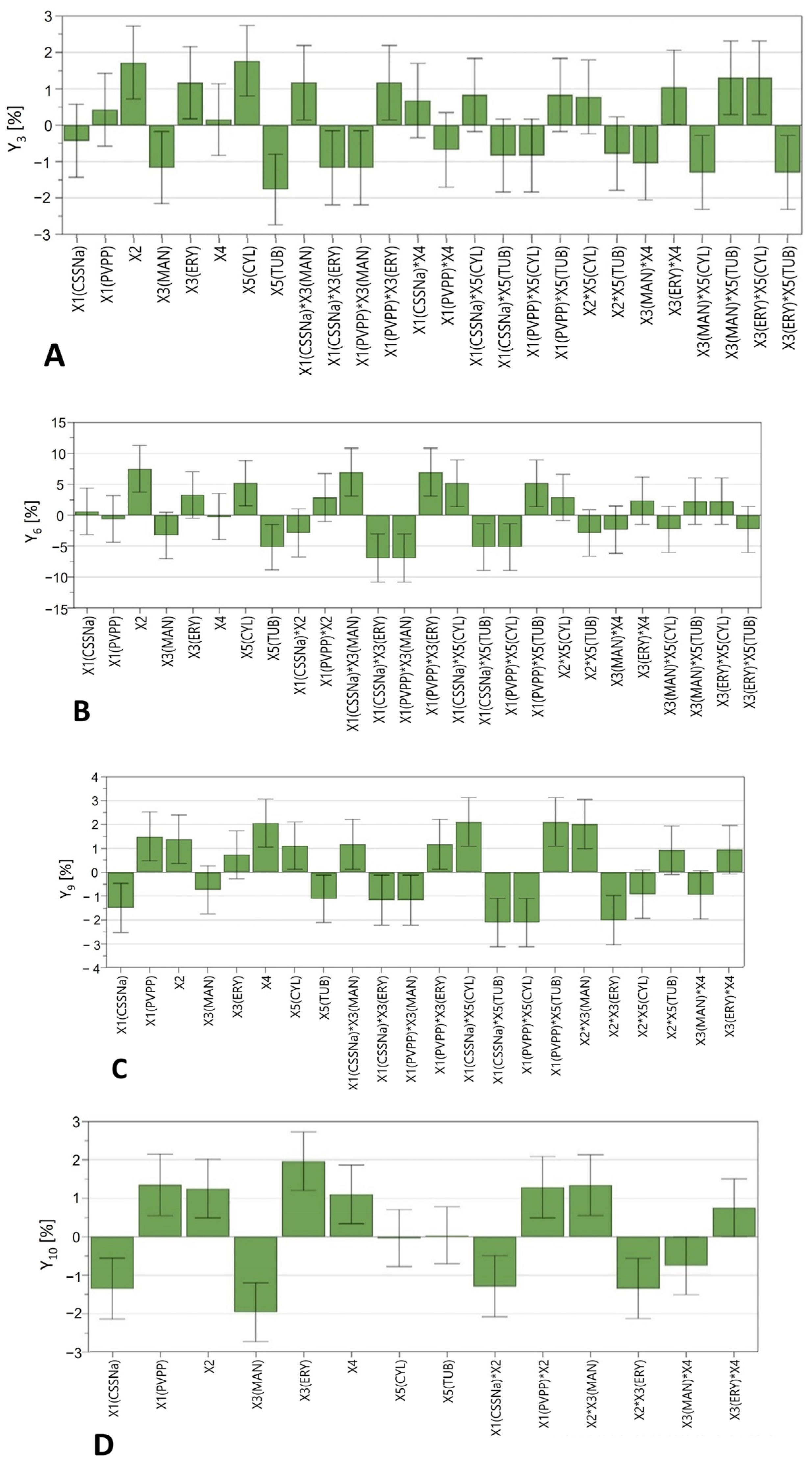
2.6. DoE Analysis
3. Materials and Methods
3.1. Materials
3.2. Preliminary Experiments
3.3. Filaments’ Characterisation
3.3.1. Drug Content
3.3.2. Tensile Measurements
3.3.3. DSC Measurements
3.3.4. XRD Measurements
3.3.5. Humidity Measurements
3.3.6. SME Measurements
3.4. Development of 3D Printed Tablets Using the Quality by Design Approach
3.5. Tablet Characterisation
3.5.1. Size and Mass Measurements
3.5.2. In Vitro Dissolution Studies
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goole, J.; Amighi, K. 3D Printing in Pharmaceutics: A New Tool for Designing Customized Drug Delivery Systems. Int. J. Pharm. 2016, 499, 376–394. [Google Scholar] [CrossRef] [PubMed]
- Arafat, B.; Wojsz, M.; Isreb, A.; Forbes, R.T.; Isreb, M.; Ahmed, W.; Arafat, T.; Alhnan, M.A. Tablet Fragmentation without a Disintegrant: A Novel Design Approach for Accelerating Disintegration and Drug Release from 3D Printed Cellulosic Tablets. Eur. J. Pharm. Sci. 2018, 118, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Yang, W.; Vo, A.Q.; Feng, X.; Ye, X.; Kim, D.W.; Repka, M.A. Hydroxypropyl Methylcellulose-Based Controlled Release Dosage by Melt Extrusion and 3D Printing: Structure and Drug Release Correlation. Carbohydr. Polym. 2017, 177, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Rahman, Z.; Barakh Ali, S.F.; Ozkan, T.; Charoo, N.A.; Reddy, I.K.; Khan, M.A. Additive Manufacturing with 3D Printing: Progress from Bench to Bedside. AAPS J. 2018, 20, 101. [Google Scholar] [CrossRef]
- Goyanes, A.; Robles Martinez, P.; Buanz, A.; Basit, A.W.; Gaisford, S. Effect of Geometry on Drug Release from 3D Printed Tablets. Int. J. Pharm. 2015, 494, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, R.V.; Patil, H.; Repka, M.A. Contribution of Hot-Melt Extrusion Technology to Advance Drug Delivery in the 21st Century. Expert Opin. Drug Deliv. 2016, 13, 451–464. [Google Scholar] [CrossRef]
- Elbadawi, M. Rheological and Mechanical Investigation into the Effect of Different Molecular Weight Poly(Ethylene Glycol)s on Polycaprolactone-Ciprofloxacin Filaments. ACS Omega 2019, 4, 5412–5423. [Google Scholar] [CrossRef]
- Samaro, A.; Janssens, P.; Vanhoorne, V.; Van Renterghem, J.; Eeckhout, M.; Cardon, L.; De Beer, T.; Vervaet, C. Screening of Pharmaceutical Polymers for Extrusion-Based Additive Manufacturing of Patient-Tailored Tablets. Int. J. Pharm. 2020, 586, 119591. [Google Scholar] [CrossRef] [PubMed]
- Oladeji, S.; Mohylyuk, V.; Jones, D.S.; Andrews, G.P. 3D Printing of Pharmaceutical Oral Solid Dosage Forms by Fused Deposition: The Enhancement of Printability Using Plasticised HPMCAS. Int. J. Pharm. 2022, 616, 121553. [Google Scholar] [CrossRef]
- Sandler, N.; Salmela, I.; Fallarero, A.; Rosling, A.; Khajeheian, M.; Kolakovic, R.; Genina, N.; Nyman, J.; Vuorela, P. Towards Fabrication of 3D Printed Medical Devices to Prevent Biofilm Formation. Int. J. Pharm. 2014, 459, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Gioumouxouzis, C.I.; Katsamenis, O.L.; Bouropoulos, N.; Fatouros, D.G. 3D Printed Oral Solid Dosage Forms Containing Hydrochlorothiazide for Controlled Drug Delivery. J. Drug Deliv. Sci. Technol. 2017, 40, 164–171. [Google Scholar] [CrossRef]
- Goyanes, A.; Chang, H.; Sedough, D.; Hatton, G.B.; Wang, J.; Buanz, A.; Gaisford, S.; Basit, A.W. Fabrication of Controlled-Release Budesonide Tablets via Desktop (FDM) 3D Printing. Int. J. Pharm. 2015, 496, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Skowyra, J.; Pietrzak, K.; Alhnan, M.A. Fabrication of Extended-Release Patient-Tailored Prednisolone Tablets via Fused Deposition Modelling (FDM) 3D Printing. Eur. J. Pharm. Sci. 2015, 68, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Pietrzak, K.; Isreb, A.; Alhnan, M.A. A Flexible-Dose Dispenser for Immediate and Extended Release 3D Printed Tablets. Eur. J. Pharm. Biopharm. 2015, 96, 380–387. [Google Scholar] [CrossRef]
- Gan, T.J. Diclofenac: An Update on Its Mechanism of Action and Safety Profile. Curr. Med. Res. Opin. 2010, 26, 1715–1731. [Google Scholar] [CrossRef]
- Tudja, P.; Khan, M.Z.I.; Meštrović, E.; Horvat, M.; Golja, P. Thermal Behaviour of Diclofenac Sodium: Decomposition and Melting Characteristics. Chem. Pharm. Bull. 2001, 49, 1245–1250. [Google Scholar] [CrossRef]
- Jennotte, O.; Koch, N.; Lechanteur, A.; Evrard, B. Three-Dimensional Printing Technology as a Promising Tool in Bioavailability Enhancement of Poorly Water-Soluble Molecules: A Review. Int. J. Pharm. 2020, 580, 119200. [Google Scholar] [CrossRef]
- Chuasuwan, B.; Binjesoh, V.; Polli, J.E.; Zhang, H.; Amidon, G.L.; Junginger, H.E.; Midha, K.K.; Shah, V.P.; Stavchansky, S.; Dressman, J.B.; et al. Biowaiver Monographs for Immediate Release Solid Oral Dosage Forms: Diclofenac Sodium and Diclofenac Potassium. J. Pharm. Sci. 2009, 98, 1206–1219. [Google Scholar] [CrossRef]
- Juansang, J.; Puttanlek, C.; Rungsardthong, V.; Puncha-Arnon, S.; Jiranuntakul, W.; Uttapap, D. Pasting Properties of Heat-Moisture Treated Canna Starches Using Different Plasticizers during Treatment. Carbohydr. Polym. 2015, 122, 152–159. [Google Scholar] [CrossRef]
- Rowe, R.C.; Sheskey, P.J.; Owen, S.C. Handbook of Pharmaceutical Excipients, 5th ed.; American Pharmacists Association: Washington, DC, USA, 2006; ISBN 1582120587. [Google Scholar]
- Dissolution Testing and Acceptance Criteria for Immediate-Release Solid Oral Dosage Form Drug Products Containing High Solubility Drug Substances—Guidance for Industry; FDA: Silver Spring, MD, USA, 2018.
- Samaro, A.; Shaqour, B.; Goudarzi, N.M.; Ghijs, M.; Cardon, L.; Boone, M.N.; Verleije, B.; Beyers, K.; Vanhoorne, V.; Cos, P.; et al. Can Filaments, Pellets and Powder Be Used as Feedstock to Produce Highly Drug-Loaded Ethylene-Vinyl Acetate 3D Printed Tablets Using Extrusion-Based Additive Manufacturing? Int. J. Pharm. 2021, 607, 120922. [Google Scholar] [CrossRef]
- Ilyés, K.; Kovács, N.K.; Balogh, A.; Borbás, E.; Farkas, B.; Casian, T.; Marosi, G.; Tomuță, I.; Nagy, Z.K. The Applicability of Pharmaceutical Polymeric Blends for the Fused Deposition Modelling (FDM) 3D Technique: Material Considerations–Printability–Process Modulation, with Consecutive Effects on in Vitro Release, Stability and Degradation. Eur. J. Pharm. Sci. 2019, 129, 110–123. [Google Scholar] [CrossRef]
- Butreddy, A.; Bandari, S.; Repka, M.A. Quality-by-Design in Hot Melt Extrusion Based Amorphous Solid Dispersions: An Industrial Perspective on Product Development. Eur. J. Pharm. Sci. 2021, 158, 105655. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, K.; Asgarzadeh, F.; Dassinger, T.; Albers, J.; Repka, M.A. A Quality by Design Approach to Understand Formulation and Process Variability in Pharmaceutical Melt Extrusion Processes. J. Pharm. Pharmacol. 2015, 67, 673–684. [Google Scholar] [CrossRef] [PubMed]
- Kristiawan, R.B.; Imaduddin, F.; Ariawan, D.; Ubaidillah; Arifin, Z. A Review on the Fused Deposition Modeling (FDM) 3D Printing: Filament Processing, Materials, and Printing Parameters. Open Eng. 2021, 11, 639–649. [Google Scholar] [CrossRef]
- Pires, F.Q.; Alves-Silva, I.; Pinho, L.A.G.; Chaker, J.A.; Sa-Barreto, L.L.; Gelfuso, G.M.; Gratieri, T.; Cunha-Filho, M. Predictive Models of FDM 3D Printing Using Experimental Design Based on Pharmaceutical Requirements for Tablet Production. Int. J. Pharm. 2020, 588, 119728. [Google Scholar] [CrossRef]
- Crișan, A.G.; Iurian, S.; Porfire, A.; Rus, L.M.; Bogdan, C.; Casian, T.; Lucacel, R.C.; Turza, A.; Porav, S.; Tomuță, I. QbD Guided Development of Immediate Release FDM-3D Printed Tablets with Customizable API Doses. Int. J. Pharm. 2022, 613, 121411. [Google Scholar] [CrossRef]
- Sadia, M.; Arafat, B.; Ahmed, W.; Forbes, R.T.; Alhnan, M.A. Channelled Tablets: An Innovative Approach to Accelerating Drug Release from 3D Printed Tablets. J. Control. Release 2018, 269, 355–363. [Google Scholar] [CrossRef]
- Neumann, H.; Burger, D.; Taftanazi, Y.; Alferez Luna, M.P.; Haussmann, T.; Hagelstein, G.; Gschwander, S. Thermal Stability Enhancement of D-Mannitol for Latent Heat Storage Applications. Sol. Energy Mater. Sol. Cells 2019, 200, 109913. [Google Scholar] [CrossRef]
- Tomassetti, S.; Aquilanti, A.; Muciaccia, P.F.; Coccia, G.; Mankel, C.; Koenders, E.A.B.; Di Nicola, G. A Review on Thermophysical Properties and Thermal Stability of Sugar Alcohols as Phase Change Materials. J. Energy Storage 2022, 55, 105456. [Google Scholar] [CrossRef]
- Tong, Q.; Xiao, Q.; Lim, L.T. Effects of Glycerol, Sorbitol, Xylitol and Fructose Plasticisers on Mechanical and Moisture Barrier Properties of Pullulan-Alginate-Carboxymethylcellulose Blend Films. Int. J. Food Sci. Technol. 2013, 48, 870–878. [Google Scholar] [CrossRef]
- Gombás, Á.; Szabó-Révész, P.; Regdon, G.; Erös, I. Study of Thermal Behaviour of Sugar Alcohols. J. Therm. Anal. Calorim. 2003, 73, 615–621. [Google Scholar] [CrossRef]
- Pasquali, I.; Bettini, R.; Giordano, F. Thermal Behaviour of Diclofenac, Diclofenac Sodium and Sodium Bicarbonate Compositions. J. Therm. Anal. Calorim. 2007, 90, 903–907. [Google Scholar] [CrossRef]
- Korkiatithaweechai, S.; Umsarika, P.; Praphairaksit, N.; Muangsin, N. Controlled Release of Diclofenac from Matrix Polymer of Chitosan and Oxidized Konjac Glucomannan. Mar. Drugs 2011, 9, 1649–1663. [Google Scholar] [CrossRef] [PubMed]
- Goyanes, A.; Fina, F.; Martorana, A.; Sedough, D.; Gaisford, S.; Basit, A.W. Development of Modified Release 3D Printed Tablets (Printlets) with Pharmaceutical Excipients Using Additive Manufacturing. Int. J. Pharm. 2017, 527, 21–30. [Google Scholar] [CrossRef] [PubMed]
- European Directorate for the Quality of Medicines & Healthcare. 2.9.5. Uniformity of Mass of Single-Dose Preparations. In European Pharmacopoeia 10.0; EDQM Council of Europe: Strasbourg, France, 2019; pp. 335–336. Available online: https://www.google.com/url?sa=i&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=0CAIQw7AJahcKEwjQyq-9gKyAAxUAAAAAHQAAAAAQAg&url=https%3A%2F%2Fwww.nihs.go.jp%2Fdnfi%2Fpdf%2FRI_PDF%2FEP1-1.pdf&psig=AOvVaw0HJTZHU_5uOGul6kBEE3Ze&ust=1690448181102018&opi=89978449 (accessed on 22 June 2023).
- Pyteraf, J.; Jamróz, W.; Kurek, M.; Szafraniec-Szczęsny, J.; Kramarczyk, D.; Jurkiewicz, K.; Knapik-Kowalczuk, J.; Tarasiuk, J.; Wroński, S.; Paluch, M.; et al. How to Obtain the Maximum Properties Flexibility of 3D Printed Ketoprofen Tablets Using Only One Drug-Loaded Filament? Molecules 2021, 26, 3106. [Google Scholar] [CrossRef]
- Gouda, A.A.; Kotb El-Sayed, M.I.; Amin, A.S.; El Sheikh, R. Spectrophotometric and Spectrofluorometric Methods for the Determination of Non-Steroidal Anti-Inflammatory Drugs: A Review. Arab. J. Chem. 2013, 6, 145–163. [Google Scholar] [CrossRef]
- Villmow, T.; Kretzschmar, B.; Pötschke, P. Influence of Screw Configuration, Residence Time, and Specific Mechanical Energy in Twin-Screw Extrusion of Polycaprolactone/Multi-Walled Carbon Nanotube Composites. Compos. Sci. Technol. 2010, 70, 2045–2055. [Google Scholar] [CrossRef]
- ICH Expert Working Group Pharmaceutical Development Q8 (R2). 2009. Available online: https://database.ich.org/sites/default/files/Q8_R2_Guideline.pdf (accessed on 22 June 2023).
- Varelas, C.G.; Dixon, D.G.; Steiner, C.A. Zero-Order Release from Biphasic Polymer Hydrogels. J. Control. Release 1995, 34, 185–192. [Google Scholar] [CrossRef]
- Savaşer, A.; Özkan, Y.; Işimer, A. Preparation and in Vitro Evaluation of Sustained Release Tablet Formulations of Diclofenac Sodium. Farmaco 2005, 60, 171–177. [Google Scholar] [CrossRef]
- Higuchi, T. Mechanism of Sustained-action Medication. Theoretical Analysis of Rate of Release of Solid Drugs Dispersed in Solid Matrices. J. Pharm. Sci. 1963, 52, 1145–1149. [Google Scholar] [CrossRef]
- Korsmeyer, R.W.; Gurny, R.; Doelker, E.; Buri, P.; Peppas, N.A. Mechanisms of Solute Release from Porous Hydrophilic Polymers. Int. J. Pharm. 1983, 15, 25–35. [Google Scholar] [CrossRef]
- Wang, X.; Yang, Y.; Liu, C.; Guo, H.; Chen, Z.; Xia, J.; Liao, Y.; Tang, C.Y.; Law, W.C. Photo- and PH-Responsive Drug Delivery Nanocomposite Based on o-Nitrobenzyl Functionalized Upconversion Nanoparticles. Polymer 2021, 229, 123961. [Google Scholar] [CrossRef]
- Akaike, H. A New Look at the Statistical Model Identification. IEEE Trans. Automat. Contr. 1974, 19, 716–723. [Google Scholar] [CrossRef]

| Preliminary Studies | |||||||||
| Exp | Polymer | % w/w | API | % w/w | Plasticiser | % w/w | Disintegrant | % w/w | Feed Rate (g/h) |
| PF | PVA | 100 | - | - | - | - | - | - | 300 |
| PF0 | PVA | 80 | DS | 20 | - | - | - | - | 500 |
| PF1 | PVA | 75 | DS | 15 | Mannitol | 10 | - | - | 300 |
| PF2 | PVA | 75 | DS | 15 | PEG4000 | 10 | - | - | 300 |
| PF3 | PVA | 89 | DS | - | PEG1500 | 8 | PVPP | 3 | 300 |
| PF4 | PVA | 82 | DS | - | PEG1500 | 15 | PVPP | 3 | 300 |
| PF5 | PVA | 85 | DS | - | Lutrol F68 | 12 | PVPP | 3 | 300 |
| PF6 | PVA | 87 | DS | - | Maltodextrin | 10 | PVPP | 3 | 300 |
| PF7 | PVA | 87 | DS | - | Isomalt | 10 | PVPP | 3 | 300 |
| PF8 | PVA | 87 | DS | - | Erythritol | 10 | PVPP | 3 | 300 |
| HME Process Parameters | |||||||||
| Exp | Zone 2 ( °C ) | Zone 3 ( °C ) | Zones 4–7 ( °C ) | Screw Speed (rpm) | Torque (%) | Filament Aspect | |||
| PF | 30 | 170 | 190 | 90 | - | Transparent | |||
| 25 | 160 | 180 | 100 | - | Transparent | ||||
| 20 | 150 | 170 | 110 | - | Transparent | ||||
| PF0 | 30 | 140 | 160 | 70 | 70 | Transparent | |||
| 30 | 130 | 150 | 90 | 40 | Transparent | ||||
| 30 | 120 | 140 | 95 | 50 | Transparent | ||||
| PF1 | 25 | 160 | 180 | 160 | 42 | Yellow, transparent | |||
| PF2 | 25 | 160 | 180 | 160 | 19 | White, opacified | |||
| PF3 | 25 | 160 | 180 | 90 | 14 | White, opacified | |||
| PF4 | 25 | 160 | 180 | 90 | 14 | White, opacified | |||
| PF5 | 25 | 160 | 180 | 90 | 14 | White, opacified, | |||
| PF6 | 25 | 160 | 180 | 90 | 14 | White, opacified | |||
| PF7 | 25 | 160 | 180 | 90 | 54 | Orange, transparent | |||
| PF8 | 25 | 160 | 180 | 90 | 54 | White, transparent | |||
| QTPP Elements | Target | Is This a CQA? | Justification | |
|---|---|---|---|---|
| Dosage form | Uncoated tablets | No | Pharmaceutical equivalence requirement: same dosage form. | |
| Dosage design | Cylindrical/tubular tablets | No | Pharmaceutical equivalence requirement: same dosage form. The geometrical design may affect the drug release performance and thus product efficacy and patient compliance. | |
| Route of administration | Oral | No | Pharmaceutical equivalence requirement: same route of administration. Ensures patient compliance and acceptability. | |
| Dosage strength | 50 mg | Yes | To ensure therapeutic efficacy. | |
| Biopharmaceutical properties | Tmax not greater than 2 h | Yes | Needed to ensure rapid onset and efficacy. | |
| Product quality attributes | Identification | Positive for diclofenac Na | No | API identification is critical for safety and efficacy. However, this feature will be monitored at drug product release. |
| Assay of active substances | 90% to 110% of the labelled content | Yes | Drug assay and mass variability are directly linked with the drug content uniformity and affect safety and efficacy. | |
| Average mass Uniformity of mass | The unit dose variation should not exceed ±5% of the average mass | Yes | Drug assay and mass variability are directly linked with the drug content uniformity and affect safety and efficacy. | |
| Dissolution at pH 6.8 | Not less than 20% at 15 min Not less than 50% at 60 min Not less than 95% at 120 min | Yes | Failure to meet dissolution specification can impact bioavailability. Both formulation and process variables affect dissolution profile. | |
| Filaments | Drug Content (%) | Loss on Drying (%) | Torque (Nm) | SME (Kwh/Kg) | Ultimate Tensile Strength (MPa) | Strain Failure (%) | Toughness (Jm−1) |
|---|---|---|---|---|---|---|---|
| F | - | - | - | - | 67.27 ± 9.74 | 19.98 ± 1.00 | 4.9 ± 0.7 |
| F1 | 93.78 | 1.80 | 9.8 | 0.52 | 54.83 ± 5.60 | 17.38 ± 0.81 | 3.3 ± 0.7 |
| F2 | 96.22 | 1.81 | 10 | 0.53 | 53.64 ± 1.62 | 17.44 ± 0.87 | 3.3 ± 0.4 |
| F3 | 95.63 | 1.90 | 7.9 | 0.42 | 40.50 ± 3.30 | 14.28 ± 0.40 | 2.3 ± 0.3 |
| F4 | 98.05 | 2.67 | 8.8 | 0.47 | 32.58 ± 6.18 | 14.43 ± 1.02 | 2.0 ± 0.5 |
| F5 | 94.90 | 1.30 | 9.3 | 0.49 | 38.87 ± 4.20 | 21.02 ± 1.64 | 3.6 ± 1.1 |
| F6 | 93.44 | 1.41 | 9.6 | 0.51 | 43.43 ± 1.91 | 23.67 ± 3.02 | 3.6 ± 0.3 |
| F7 | 94.45 | 1.39 | 8.4 | 0.45 | 25.47 ± 1.71 | 449.6 ± 80.8 | 99.6 ± 22.9 |
| F8 | 97.24 | 2.10 | 8.8 | 0.47 | 29.86 ± 0.49 | 433.0 ± 375.0 | 162.4 ± 4.6 |
| PVA * | - | - | - | - | 56.96 ± 1.94 | 34.06 ± 2.73 | 11.2 ± 0.3 |
| Exp. | X1 | X2 | X3 | LH (X4)/Design (X5) | Mass (mg) | CV % | Exp. | X1 | X2 | X3 | LH (X4)/Design (X5) | Weight (mg) | CV % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N1 | CSSNa | 10 | MAN | 0.2/CYL | 380.5 | 0.10 | N17 | CSSNa | 10 | ERY | 0.2/CYL | 450.1 | 0.10 |
| N2 | CSSNa | 10 | MAN | 0.05/CYL | 381.4 | 0.10 | N18 | CSSNa | 10 | ERY | 0.05/CYL | 449.2 | 0.10 |
| N3 | CSSNa | 10 | MAN | 0.2/TUB | 310.7 | 0.01 | N19 | CSSNa | 10 | ERY | 0.2/TUB | 374.2 | 0.10 |
| N4 | CSSNa | 10 | MAN | 0.05/TUB | 356.7 | 0.20 | N20 | CSSNa | 10 | ERY | 0.05/TUB | 393.6 | 0.10 |
| N5 | PVPP | 10 | MAN | 0.2/CYL | 424.4 | 0.10 | N21 | PVPP | 10 | ERY | 0.2/CYL | 339.9 | 0.10 |
| N6 | PVPP | 10 | MAN | 0.05/CYL | 432.6 | 0.10 | N22 | PVPP | 10 | ERY | 0.05/CYL | 429.1 | 0.01 |
| N7 | PVPP | 10 | MAN | 0.2/TUB | 315.6 | 0.10 | N23 | PVPP | 10 | ERY | 0.2/TUB | 365.5 | 0.10 |
| N8 | PVPP | 10 | MAN | 0.05/TUB | 380.0 | 0.10 | N24 | PVPP | 10 | ERY | 0.05/TUB | 333.3 | 0.01 |
| N9 | CSSNa | 15 | MAN | 0.2/CYL | 395.8 | 0.10 | N25 | CSSNa | 15 | ERY | 0.2/CYL | 399.6 | 0.10 |
| N10 | CSSNa | 15 | MAN | 0.05/CYL | 409.4 | 0.01 | N26 | CSSNa | 15 | ERY | 0.05/CYL | 342.3 | 0.01 |
| N11 | CSSNa | 15 | MAN | 0.2/TUB | 326.0 | 0.20 | N27 | CSSNa | 15 | ERY | 0.2/TUB | 334.0 | 0.10 |
| N12 | CSSNa | 15 | MAN | 0.05/TUB | 361.6 | 0.01 | N28 | CSSNa | 15 | ERY | 0.05/TUB | 299.0 | 0.10 |
| N13 | PVPP | 15 | MAN | 0.2/CYL | 428.6 | 0.01 | N29 | PVPP | 15 | ERY | 0.2/CYL | 418.4 | 0.10 |
| N14 | PVPP | 15 | MAN | 0.05/CYL | 373.2 | 0.10 | N30 | PVPP | 15 | ERY | 0.05/CYL | 394.6 | 0.10 |
| N15 | PVPP | 15 | MAN | 0.2/TUB | 348.7 | 0.10 | N31 | PVPP | 15 | ERY | 0.2/TUB | 312.3 | 0.10 |
| N16 | PVPP | 15 | MAN | 0.05/TUB | 369.2 | 0.10 | N32 | PVPP | 15 | ERY | 0.05/TUB | 385.7 | 0.01 |
| Exp Name | Y1 | Y2 | Y3 | Y4 | Y5 | Y6 | Y7 | Y8 | Y9 | Y10 |
|---|---|---|---|---|---|---|---|---|---|---|
| N1 | 8.51 | 15.51 | 19.38 | 45.59 | 70.92 | 89.49 | 95.05 | 94.68 | 95.02 | 94.30 |
| N3 | 7.11 | 11.81 | 17.34 | 33.63 | 48.42 | 62.78 | 76.50 | 87.06 | 92.21 | 92.98 |
| N5 | 7.18 | 13.22 | 19.52 | 37.36 | 53.30 | 67.57 | 81.58 | 93.91 | 98.32 | 97.53 |
| N6 | 6.06 | 11.25 | 15.26 | 26.84 | 37.40 | 48.00 | 60.62 | 75.60 | 93.37 | 95.03 |
| N7 | 8.68 | 15.49 | 22.09 | 41.53 | 59.33 | 75.22 | 85.55 | 92.44 | 97.11 | 96.72 |
| N8 | 4.88 | 8.87 | 12.94 | 26.46 | 37.93 | 50.03 | 62.99 | 73.36 | 88.58 | 92.67 |
| N9 | 7.95 | 15.14 | 22.28 | 41.67 | 59.39 | 75.49 | 89.08 | 92.52 | 92.14 | 93.36 |
| N10 | 8.09 | 15.15 | 22.45 | 42.86 | 60.78 | 85.72 | 95.33 | 95.70 | 99.77 | 96.05 |
| N11 | 7.49 | 14.35 | 20.64 | 39.42 | 56.07 | 75.71 | 88.66 | 94.84 | 96.34 | 96.66 |
| N12 | 8.03 | 12.09 | 16.79 | 32.60 | 46.92 | 61.30 | 73.41 | 84.40 | 93.91 | 97.07 |
| N13 | 8.32 | 15.72 | 23.52 | 42.31 | 57.89 | 74.34 | 88.28 | 98.18 | 101.84 | 102.55 |
| N14 | 7.41 | 13.87 | 21.30 | 42.23 | 61.69 | 83.29 | 95.38 | 95.71 | 96.69 | 96.58 |
| N15 | 7.15 | 13.25 | 19.15 | 36.11 | 51.90 | 67.66 | 81.10 | 91.61 | 99.80 | 100.91 |
| N16 | 8.78 | 14.92 | 21.07 | 39.46 | 57.18 | 72.94 | 87.53 | 97.52 | 102.38 | 102.91 |
| N17 | 15.57 | 14.20 | 20.20 | 36.54 | 51.77 | 66.47 | 78.95 | 89.77 | 99.59 | 101.89 |
| N18 | 7.22 | 13.43 | 19.39 | 36.36 | 51.76 | 66.15 | 81.60 | 95.56 | 98.36 | 98.79 |
| N19 | 7.07 | 10.51 | 14.77 | 27.64 | 39.66 | 51.14 | 62.00 | 74.87 | 90.27 | 102.70 |
| N20 | 4.31 | 7.94 | 11.82 | 23.02 | 34.54 | 45.94 | 56.84 | 67.15 | 85.30 | 95.83 |
| N21 | 11.48 | 22.47 | 31.41 | 52.13 | 70.99 | 80.55 | 93.21 | 99.25 | 100.46 | 101.38 |
| N22 | 5.85 | 11.14 | 16.30 | 33.75 | 49.02 | 62.48 | 81.26 | 93.31 | 96.75 | 99.62 |
| N23 | 9.08 | 13.96 | 19.60 | 34.96 | 49.83 | 64.27 | 77.88 | 90.49 | 104.73 | 108.76 |
| N24 | 7.22 | 12.67 | 18.17 | 35.71 | 54.29 | 71.97 | 83.19 | 88.95 | 97.10 | 96.81 |
| N25 | 24.22 | 24.90 | 28.19 | 49.99 | 74.44 | 96.73 | 99.26 | 100.49 | 99.99 | 101.19 |
| N26 | 8.24 | 15.16 | 22.05 | 39.93 | 61.10 | 78.47 | 85.00 | 89.67 | 92.78 | 92.18 |
| N27 | 6.39 | 11.19 | 17.53 | 26.90 | 37.74 | 48.33 | 59.97 | 71.48 | 94.42 | 98.64 |
| N28 | 37.96 | 35.87 | 43.18 | 73.71 | 89.40 | 95.64 | 95.81 | 96.08 | 97.05 | 97.61 |
| N29 | 9.60 | 17.78 | 25.51 | 46.26 | 69.24 | 92.13 | 102.30 | 101.49 | 101.06 | 104.56 |
| N30 | 9.22 | 17.90 | 27.01 | 59.66 | 85.79 | 89.84 | 91.94 | 92.38 | 90.10 | 90.02 |
| N31 | 15.61 | 27.72 | 39.79 | 70.35 | 92.34 | 98.12 | 102.60 | 102.01 | 102.48 | 101.55 |
| N32 | 7.06 | 13.17 | 18.67 | 34.21 | 47.76 | 59.55 | 72.41 | 79.00 | 94.97 | 100.16 |
| Filament | Active Substance | Polymer Matrix | Plasticiser | Disintegrant | ||||
|---|---|---|---|---|---|---|---|---|
| Type | % | Type | % | Type | % | Type | % | |
| F1 | DS | 15 | PVA | 72 | MAN | 10 | CSSNa | 3 |
| F2 | DS | 15 | PVA | 72 | MAN | 10 | PVPP | 3 |
| F3 | DS | 15 | PVA | 67 | MAN | 15 | CSSNa | 3 |
| F4 | DS | 15 | PVA | 67 | MAN | 15 | PVPP | 3 |
| F5 | DS | 15 | PVA | 72 | ERY | 10 | CSSNa | 3 |
| F6 | DS | 15 | PVA | 72 | ERY | 10 | PVPP | 3 |
| F7 | DS | 15 | PVA | 67 | ERY | 15 | CSSNa | 3 |
| F8 | DS | 15 | PVA | 67 | ERY | 15 | PVPP | 3 |
| Factors | Design Level | Responses | |||||
|---|---|---|---|---|---|---|---|
| −1 | +1 | ||||||
| X1 | Superdisintegrant type [-] | CSSNa | PVPP | Y1 | % DS release at 5 min | Y6 | % DS release at 60 min |
| X2 | Plasticiser conc. [%, w/w] | 10 | 15 | Y2 | % DS release at 10 min | Y7 | % DS release at 75 min |
| X3 | Plasticiser type [-] | MAN | ERY | Y3 | % DS release at 15 min | Y8 | % DS release at 90 min |
| X4 | Layer height [mm] | 0.05 | 0.2 | Y4 | % DS release at 30 min | Y9 | % DS release at 120 min |
| X5 | Tablet geometry [-] | CYL | TUB | Y5 | % DS release at 45 min | Y10 | % DS release at 240 min |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Digkas, T.; Porfire, A.; Van Renterghem, J.; Samaro, A.; Borodi, G.; Vervaet, C.; Crișan, A.G.; Iurian, S.; De Beer, T.; Tomuta, I. Development of Diclofenac Sodium 3D Printed Cylindrical and Tubular-Shaped Tablets through Hot Melt Extrusion and Fused Deposition Modelling Techniques. Pharmaceuticals 2023, 16, 1062. https://doi.org/10.3390/ph16081062
Digkas T, Porfire A, Van Renterghem J, Samaro A, Borodi G, Vervaet C, Crișan AG, Iurian S, De Beer T, Tomuta I. Development of Diclofenac Sodium 3D Printed Cylindrical and Tubular-Shaped Tablets through Hot Melt Extrusion and Fused Deposition Modelling Techniques. Pharmaceuticals. 2023; 16(8):1062. https://doi.org/10.3390/ph16081062
Chicago/Turabian StyleDigkas, Tryfon, Alina Porfire, Jeroen Van Renterghem, Aseel Samaro, Gheorghe Borodi, Chris Vervaet, Andrea Gabriela Crișan, Sonia Iurian, Thomas De Beer, and Ioan Tomuta. 2023. "Development of Diclofenac Sodium 3D Printed Cylindrical and Tubular-Shaped Tablets through Hot Melt Extrusion and Fused Deposition Modelling Techniques" Pharmaceuticals 16, no. 8: 1062. https://doi.org/10.3390/ph16081062
APA StyleDigkas, T., Porfire, A., Van Renterghem, J., Samaro, A., Borodi, G., Vervaet, C., Crișan, A. G., Iurian, S., De Beer, T., & Tomuta, I. (2023). Development of Diclofenac Sodium 3D Printed Cylindrical and Tubular-Shaped Tablets through Hot Melt Extrusion and Fused Deposition Modelling Techniques. Pharmaceuticals, 16(8), 1062. https://doi.org/10.3390/ph16081062










