Stable Gastric Pentadecapeptide BPC 157—Possible Novel Therapy of Glaucoma and Other Ocular Conditions
Abstract
1. Introduction
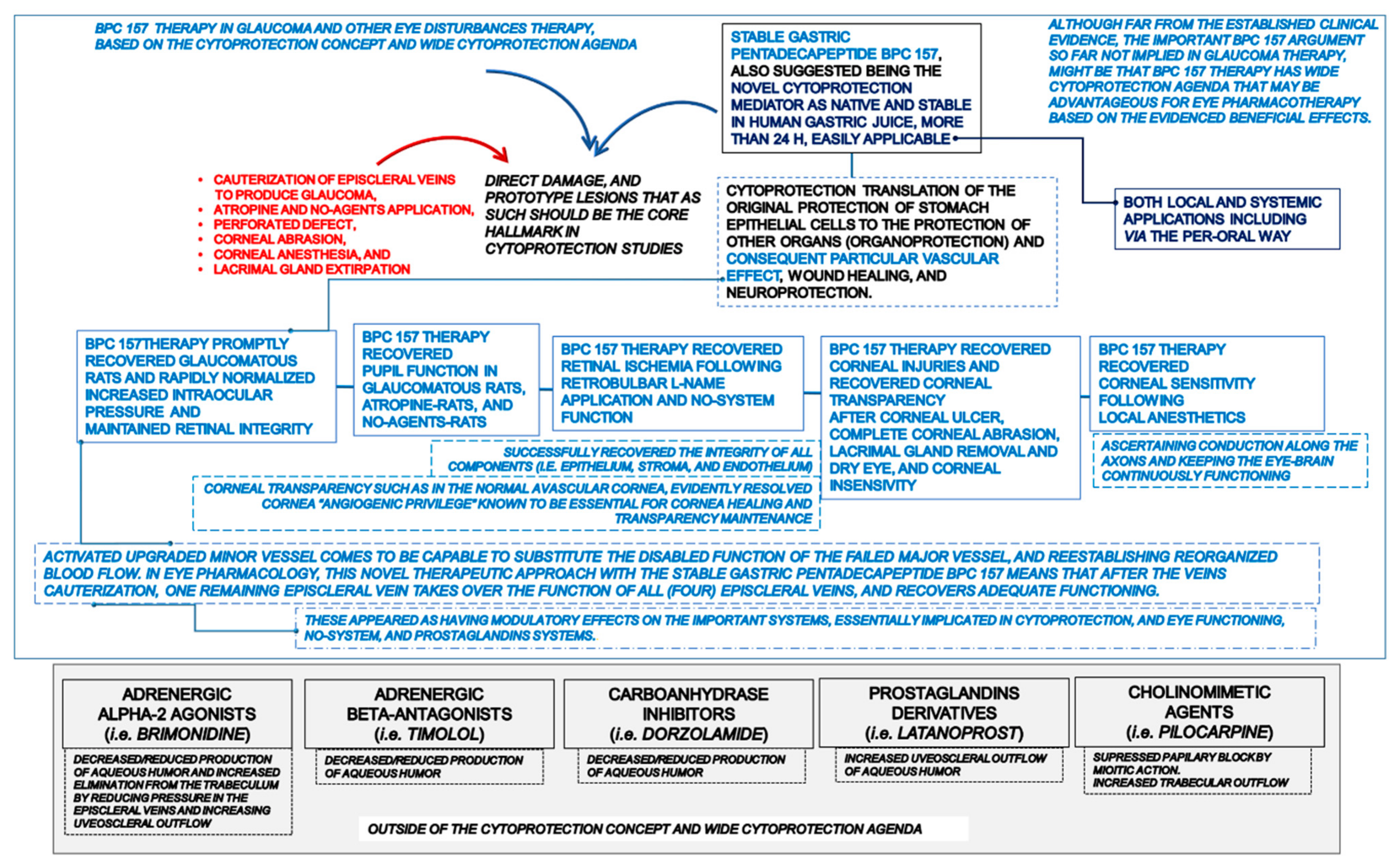
1.1. Particular Cytoprotective Aspects of BPC 157 Therapy in Glaucoma
1.2. The Proposed Cytoprotective Principle vs. Pitfalls of Standard Intraocular Pressure-Lowering Drugs
1.3. The Proposed BPC 157 Cytoprotective Principle
The Proposed BPC 157 Cytoprotective Principle as the Counteraction of the Occlusion/Occlusion-like Syndromes
1.4. Cytoprotection Agenda in Glaucoma Therapy Distinctive from the Focused Background of the Beta-Blockers, Alpha 2-Agonists, Inhibitors of Carbonic Anhydrase, or Parasympathomimetics, and Prostaglandin Derivatives
1.5. BPC 157 Therapy, Interaction with Essential Systems, i.e., Nitric Oxide (NO), Prostaglandins-System, Implicated in the Cytoprotection Concept and Glaucoma
1.6. BPC 157 and Glaucoma Therapy
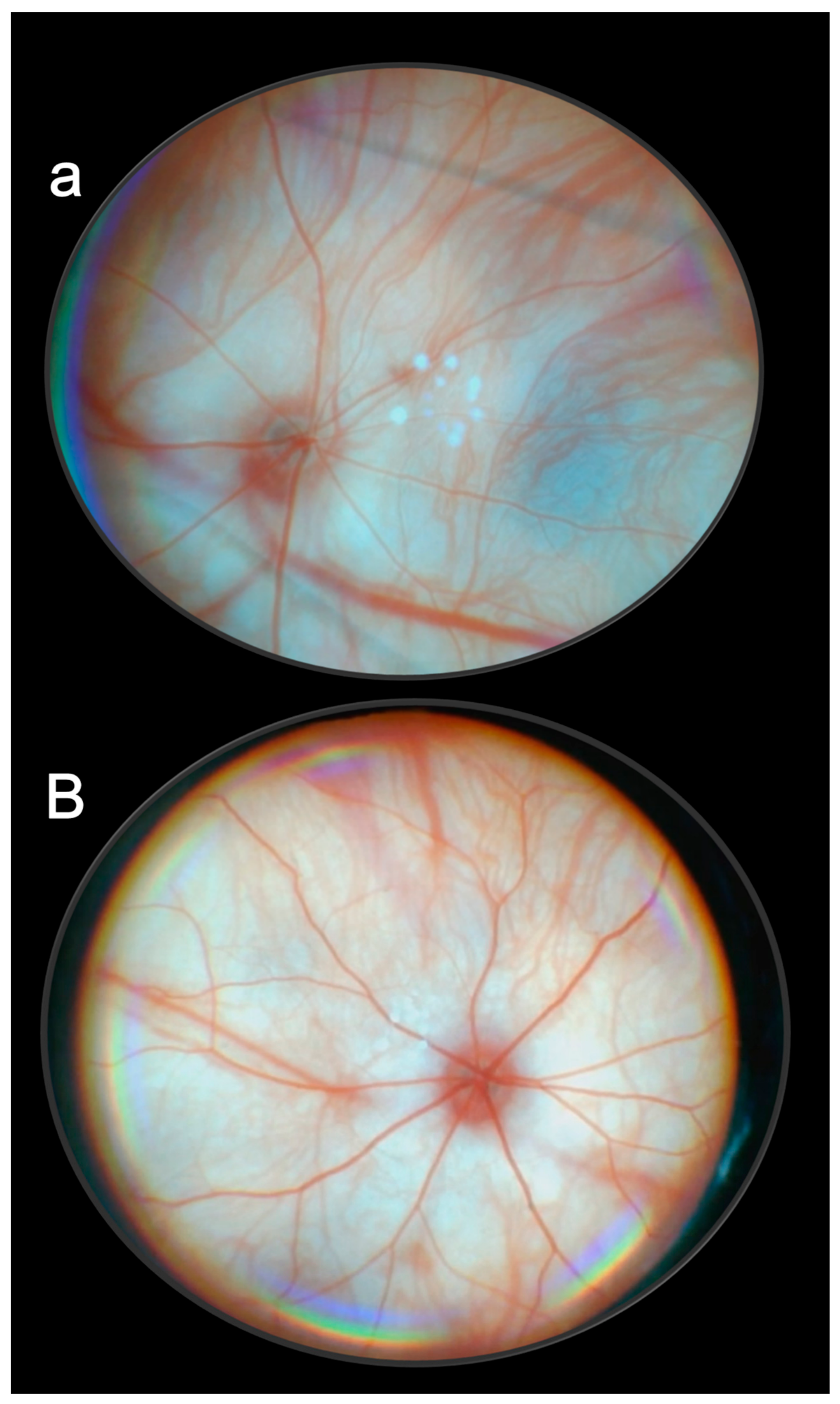
2. Glaucoma
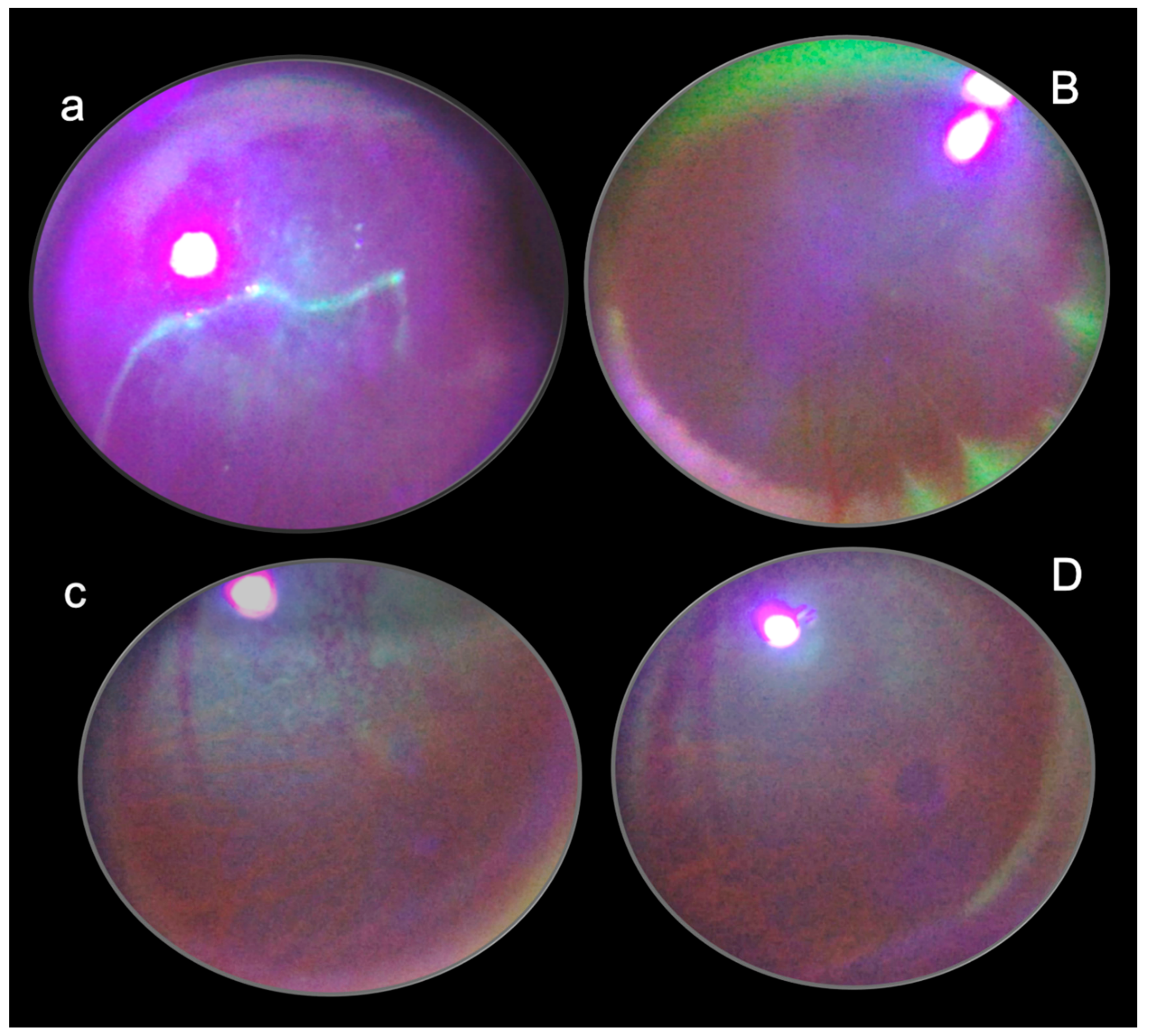
2.1. Model Consideration
2.2. BPC 157 Therapy May Rapidly Induce Normalization of Intraocular Pressure
2.3. BPC 157 Therapy Exhibited Immediate Normalization of Elevated Intraocular Pressure as a General Beneficial Effect
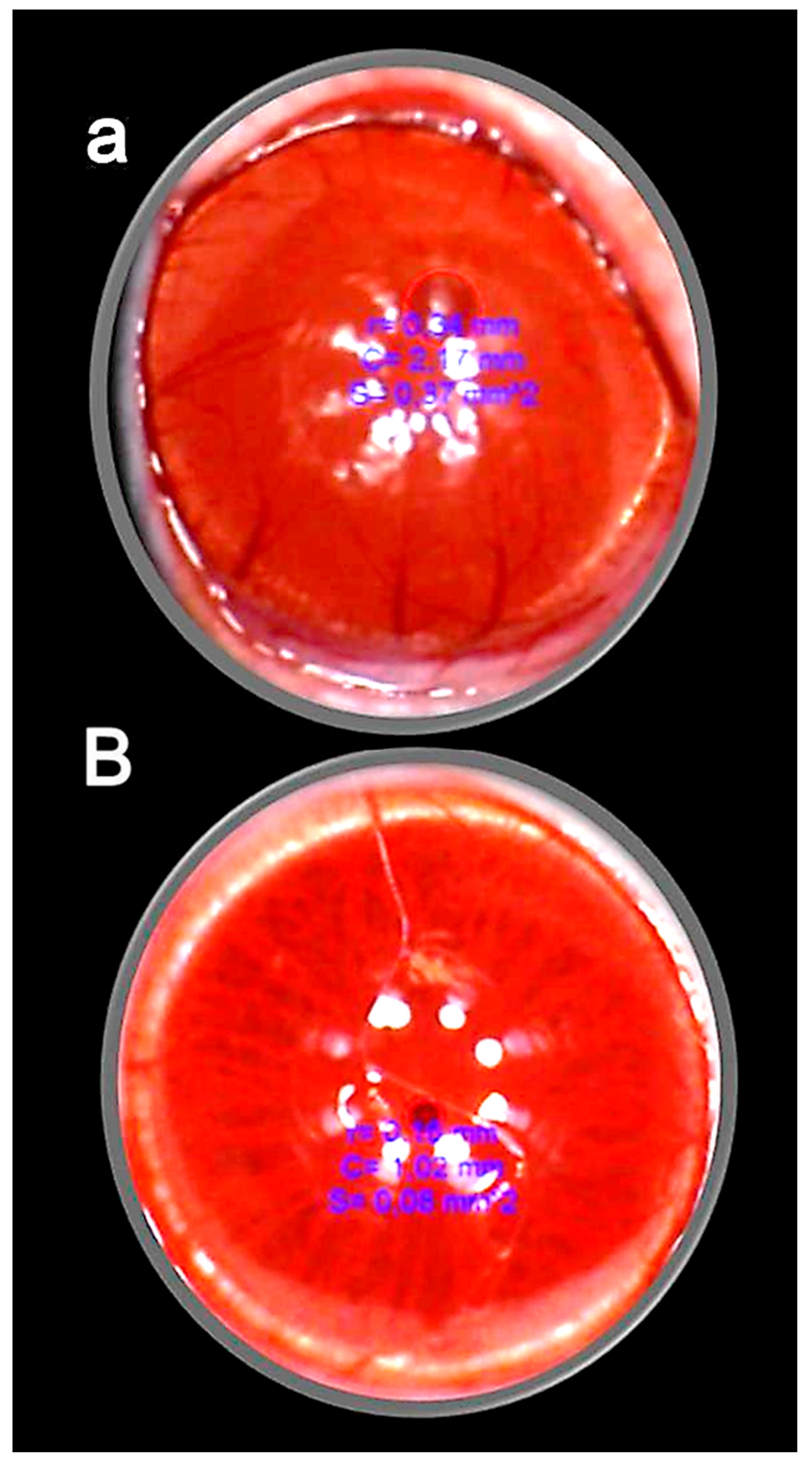
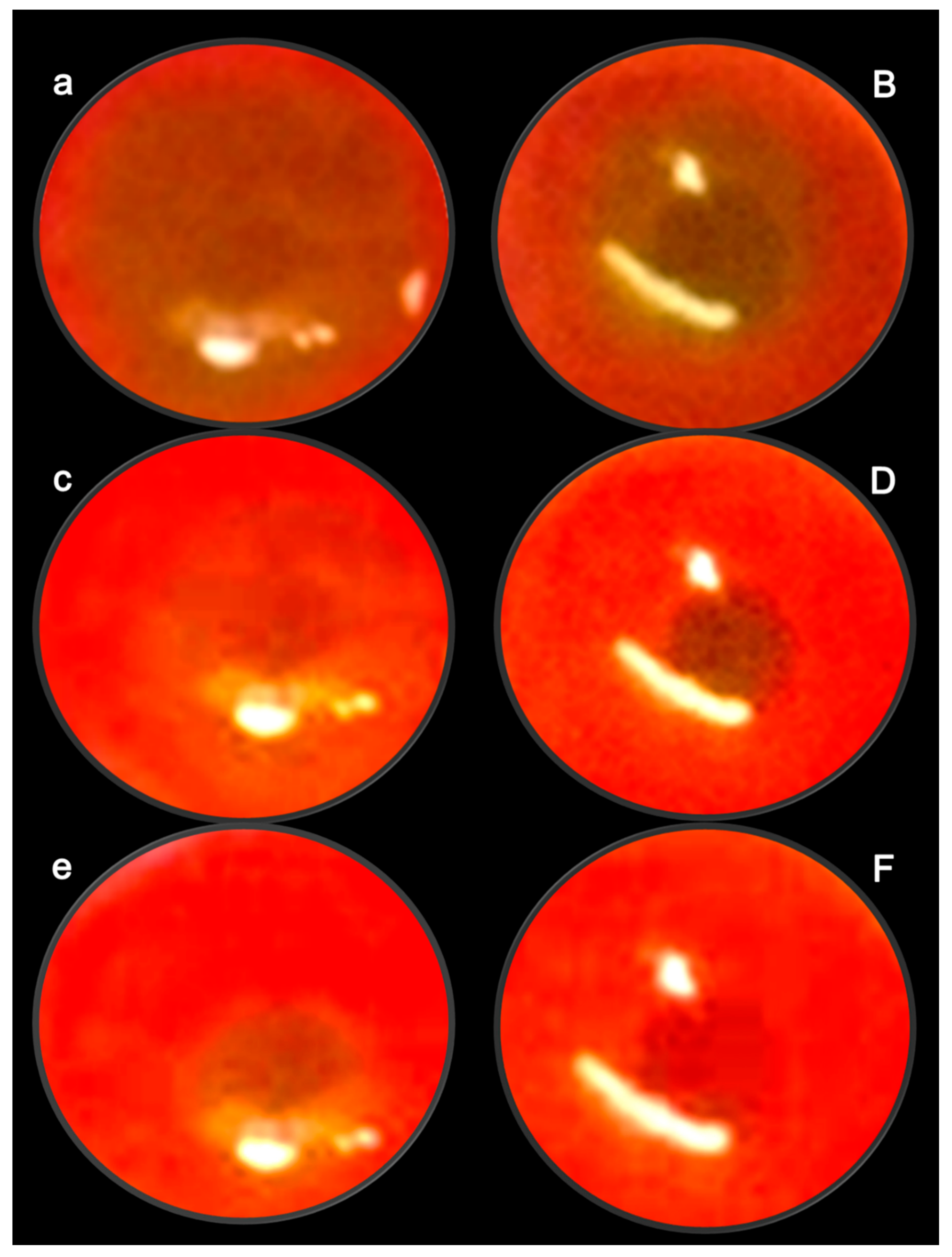
2.4. Retinal Ischemia
2.5. Retina–Brain Axis, Brain–Gut Axis, Gut–Brain Axis
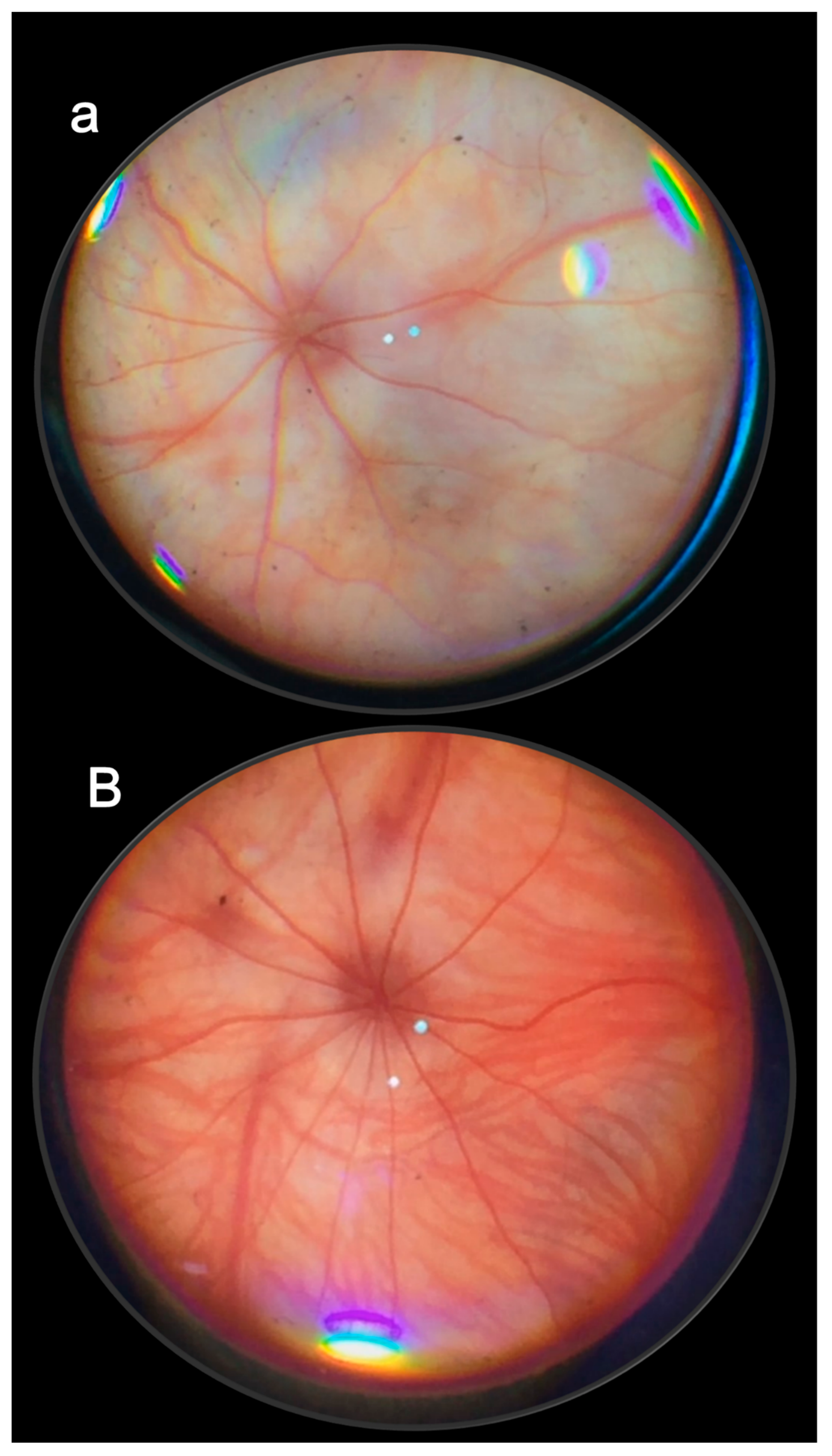
2.6. Mydriasis
2.7. Consistent Therapy Findings on Both Injured Eyes
3. Pupil Control
4. Retinal Ischemia
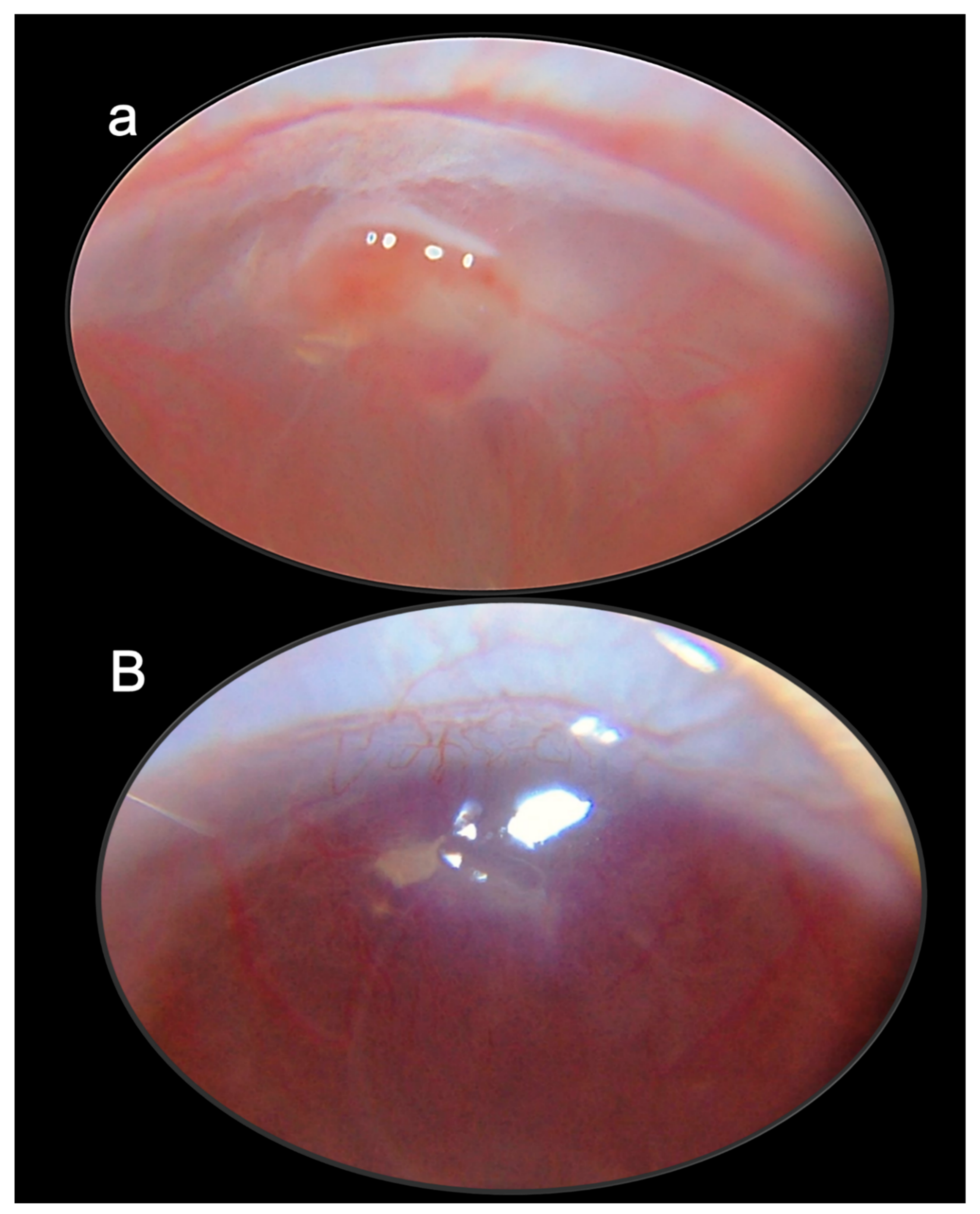
5. Cornea
6. Restoration of Corneal Sensitivity
7. Conclusions
7.1. Cytoprotection Concept in Eye Pharmacotherapy
7.2. Correlation between Glaucomatous Rats and Occlusion/Occlusion-like Syndromes Rats as Cytoprotection Implementation
7.3. Possible Regulatory Physiologic Role in Eye and Bodily Functions for Clinical Safety and Efficacy as Concluding Remarks
Funding
Acknowledgments
Conflicts of Interest
References
- Sikiric, P.; Gojkovic, S.; Knezevic, M.; Tepes, M.; Strbe, S.; Vukojevic, J.; Duzel, A.; Kralj, T.; Krezic, I.; Zizek, H.; et al. Stable gastric pentadecapeptide BPC 157: Prompt particular activation of the collateral pathways. Curr. Med. Chem. 2023, 30, 1568–1573. [Google Scholar] [CrossRef] [PubMed]
- Sikiric, P.; Udovicic, M.; Barisic, I.; Balenovic, D.; Zivanovic Posilovic, G.; Strinic, D.; Uzun, S.; Sikiric, S.; Krezic, I.; Zizek, H.; et al. Stable gastric pentadecapeptide BPC 157 as useful cytoprotective peptide therapy in the hearth disturbances, myocardial infarction, heart failure, pulmonary hypertension, arrhythmias, and thrombosis presentation. Biomedicines 2022, 10, 2696. [Google Scholar] [CrossRef] [PubMed]
- Sikiric, P.; Rucman, R.; Turkovic, B.; Sever, M.; Klicek, R.; Radic, B.; Drmic, D.; Stupnisek, M.; Misic, M.; Vuletic, L.B.; et al. Novel cytoprotective mediator, stable gastric pentadecapeptide BPC 157. Vascular recruitment and gastrointestinal tract healing. Curr. Pharm. Des. 2018, 24, 1990–2001. [Google Scholar] [CrossRef] [PubMed]
- Sikiric, P.; Seiwerth, S.; Rucman, R.; Drmic, D.; Stupnisek, M.; Kokot, A.; Sever, M.; Zoricic, I.; Zoricic, Z.; Batelja, L.; et al. Stress in gastrointestinal tract and stable gastric pentadecapeptide BPC 157. Finally, do we have a solution? Curr. Pharm. Des. 2017, 23, 4012–4028. [Google Scholar] [CrossRef]
- Sikiric, P.; Seiwerth, S.; Rucman, R.; Kolenc, D.; Vuletic, L.B.; Drmic, D.; Grgic, T.; Strbe, S.; Zukanovic, G.; Crvenkovic, D.; et al. Brain-gut axis and pentadecapeptide BPC 157: Theoretical and practical implications. Curr. Neuropharmacol. 2016, 14, 857–865. [Google Scholar] [CrossRef]
- Staresinic, M.; Japjec, M.; Vranes, H.; Prtoric, A.; Zizek, H.; Krezic, I.; Gojkovic, S.; Smoday, I.M.; Oroz, K.; Staresinic, E.; et al. Stable gastric pentadecapeptide BPC 157 and striated, smooth, and heart muscle. Biomedicines 2022, 10, 3221. [Google Scholar] [CrossRef]
- Sikiric, P.; Skrtic, A.; Gojkovic, S.; Krezic, I.; Zizek, H.; Lovric, E.; Sikiric, S.; Knezevic, M.; Strbe, S.; Milavic, M.; et al. Gastric pentadecapeptide BPC 157 in cytoprotection to resolve major vessel occlusion disturbances, ischemia-reperfusion injury following Pringle maneuver, and Budd-Chiari syndrome. World J. Gastroenterol. 2022, 28, 23–46. [Google Scholar] [CrossRef]
- Seiwerth, S.; Milavic, M.; Vukojevic, J.; Gojkovic, S.; Krezic, I.; Vuletic, L.B.; Pavlov, K.H.; Petrovic, A.; Sikiric, S.; Vranes, H.; et al. Stable gastric pentadecapeptide BPC 157 and wound healing. Front. Pharmacol. 2021, 12, 627533. [Google Scholar] [CrossRef]
- Vukojevic, J.; Milavic, M.; Perovic, D.; Ilic, S.; Cilic, A.Z.; Duran, N.; Strbe, S.; Zoricic, Z.; Filipcic, I.; Brecic, P.; et al. Pentadecapeptide BPC 157 and the central nervous system. Neural Regen. Res. 2022, 17, 482–487. [Google Scholar] [CrossRef]
- Sikiric, P.; Gojkovic, S.; Krezic, I.; Smoday, I.M.; Kalogjera, L.; Zizek, H.; Oroz, K.; Vranes, H.; Vukovic, V.; Labidi, M.; et al. Stable gastric pentadecapeptide BPC 157 may recover brain–gut axis and gut–brain axis function. Pharmaceuticals 2023, 16, 676. [Google Scholar] [CrossRef]
- Kralj, T.; Kokot, A.; Zlatar, M.; Masnec, S.; Kasnik Kovac, K.; Milkovic Perisa, M.; Batelja Vuletic, L.; Giljanovic, A.; Strbe, S.; Sikiric, S.; et al. Stable gastric pentadecapeptide BPC 157 therapy of rat glaucoma. Biomedicines 2021, 10, 89. [Google Scholar] [CrossRef]
- Kokot, A.; Zlatar, M.; Stupnisek, M.; Drmic, D.; Radic, R.; Vcev, A.; Seiwerth, S.; Sikiric, P. NO system dependence of atropine-induced mydriasis and L-NAME- and L-arginine-induced miosis: Reversal by the pentadecapeptide BPC 157 in rats and guinea pigs. Eur. J. Pharmacol. 2016, 771, 211–219. [Google Scholar] [CrossRef]
- Zlatar, M.; Kokot, A.; Vuletic, L.B.; Masnec, S.; Kralj, T.; Perisa, M.M.; Barisic, I.; Radic, B.; Milanovic, K.; Drmic, D.; et al. BPC 157 as a therapy for retinal ischemia induced by retrobulbar application of L-NAME in rats. Front. Pharmacol. 2021, 12, 632295. [Google Scholar] [CrossRef]
- Lazic, R.; Gabric, N.; Dekaris, I.; Bosnar, D.; Boban-Blagaic, A.; Sikiric, P. Gastric pentadecapeptide BPC 157 promotes corneal epithelial defects healing in rats. Coll. Antropol. 2005, 29, 321–325. [Google Scholar]
- Masnec, S.; Kokot, A.; Zlatar, M.; Kalauz, M.; Kunjko, K.; Radic, B.; Klicek, R.; Drmic, D.; Lazic, R.; Brcic, L.; et al. Perforating corneal injury in rat and pentadecapeptide BPC 157. Exp. Eye Res. 2015, 136, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Kralj, T.; Kokot, A.; Kasnik, K.; Drmic, D.; Zlatar, M.; Seiwerth, S.; Sikiric, P. Effects of pentadecapeptide BPC 157 on experimental rat model of dry eye. FASEB J. 2017, 31 (Suppl. 1), 993.3. [Google Scholar]
- Mirkovic, I.; Kralj, T.; Lozic, M.; Stambolija, V.; Kovacevic, J.; Vrdoljak, L.; Zlatar, M.; Milanovic, K.; Drmic, D.; Predovic, J.; et al. Pentadecapeptide BPC 157 shortens duration of tetracaine- and oxybuprocaine-induced corneal anesthesia in rats. Acta Clin. Croat. 2020, 59, 394–406. [Google Scholar] [CrossRef]
- Knezevic, M.; Gojkovic, S.; Krezic, I.; Zizek, H.; Malekinusic, D.; Vrdoljak, B.; Vranes, H.; Knezevic, T.; Barisic, I.; Horvat Pavlov, K.; et al. Occlusion of the superior mesenteric artery in rats reversed by collateral pathways activation: Gastric pentadecapeptide BPC 157 therapy counteracts multiple organ dysfunction syndrome; intracranial, portal and caval hypertension; and aortal hypotension. Biomedicines 2021, 9, 609. [Google Scholar] [CrossRef]
- Knezevic, M.; Gojkovic, S.; Krezic, I.; Zizek, H.; Malekinusic, D.; Vrdoljak, B.; Knezevic, T.; Vranes, H.; Drmic, D.; Staroveski, M.; et al. Occluded superior mesenteric artery and vein. Therapy with the stable gastric pentadecapeptide BPC 157. Biomedicines 2021, 9, 792. [Google Scholar] [CrossRef]
- Knezevic, M.; Gojkovic, S.; Krezic, I.; Zizek, H.; Vranes, H.; Malekinusic, D.; Vrdoljak, B.; Knezevic, T.; Pavlov, K.H.; Drmic, D.; et al. Complex syndrome of the complete occlusion of the end of the superior mesenteric vein, opposed with the stable gastric pentadecapeptide BPC 157 in rats. Biomedicines 2021, 9, 1029. [Google Scholar] [CrossRef]
- Kolovrat, M.; Gojkovic, S.; Krezic, I.; Malekinusic, D.; Vrdoljak, B.; Kasnik Kovac, K.; Kralj, T.; Drmic, D.; Barisic, I.; Horvat Pavlov, K.; et al. Pentadecapeptide BPC 157 resolves Pringle maneuver in rats, both ischemia and reperfusion. World J. Hepatol. 2020, 12, 184–206. [Google Scholar] [CrossRef] [PubMed]
- Gojkovic, S.; Krezic, I.; Vrdoljak, B.; Malekinusic, D.; Barisic, I.; Petrovic, A.; Horvat Pavlov, K.; Kolovrat, M.; Duzel, A.; Knezevic, M.; et al. Pentadecapeptide BPC 157 resolves suprahepatic occlusion of the inferior caval vein, Budd-Chiari syndrome model in rats. World J. Gastrointest. Pathophysiol. 2020, 11, 1–19. [Google Scholar] [CrossRef]
- Vukojevic, J.; Siroglavic, M.; Kasnik, K.; Kralj, T.; Stancic, D.; Kokot, A.; Kolaric, D.; Drmic, D.; Sever, A.Z.; Barisic, I.; et al. Rat inferior caval vein (ICV) ligature and particular new insights with the stable gastric pentadecapeptide BPC 157. Vascul. Pharmacol. 2018, 106, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Gojkovic, S.; Krezic, I.; Vranes, H.; Zizek, H.; Drmic, D.; Pavlov, K.H.; Petrovic, A.; Batelja, L.; Milavic, M.; Sikiric, S.; et al. BPC 157 therapy and the permanent occlusion of the superior sagittal sinus in rat. Vascular recruitment. Biomedicines 2021, 9, 744. [Google Scholar] [CrossRef]
- Vukojevic, J.; Vrdoljak, B.; Malekinusic, D.; Siroglavic, M.; Milavic, M.; Kolenc, D.; Boban Blagaic, A.; Bateljam, L.; Drmic, D.; Seiwerth, S.; et al. The effect of pentadecapeptide BPC 157 on hippocampal ischemia/reperfusion injuries in rats. Brain Behav. 2020, 10, e01726. [Google Scholar] [CrossRef]
- Strbe, S.; Gojkovic, S.; Krezic, I.; Zizek, H.; Vranes, H.; Barisic, I.; Strinic, D.; Orct, T.; Vukojevic, J.; Ilic, S.; et al. Over-dose lithium toxicity as an occlusive-like syndrome in rats and gastric pentadecapeptide BPC 157. Biomedicines 2021, 9, 1506. [Google Scholar] [CrossRef]
- Barisic, I.; Balenovic, D.; Udovicic, M.; Bardak, D.; Strinic, D.; Vlainic, J.; Vranes, H.; Smoday, I.M.; Krezic, I.; Milavic, M.; et al. Stable gastric pentadecapeptide BPC 157 may counteract myocardial infarction induced by isoprenaline in rats. Biomedicines 2022, 10, 265. [Google Scholar] [CrossRef]
- Gojkovic, S.; Krezic, I.; Vranes, H.; Zizek, H.; Drmic, D.; Batelja Vuletic, L.; Milavic, M.; Sikiric, S.; Stilinovic, I.; Simeon, P.; et al. Robert’s intragastric alcohol-induced gastric lesion model as an escalated general peripheral and central syndrome, counteracted by the stable gastric pentadecapeptide BPC 157. Biomedicines 2021, 9, 1300. [Google Scholar] [CrossRef]
- Tepes, M.; Gojkovic, S.; Krezic, I.; Zizek, H.; Madzar, Z.; Santak, G.; Batelja, L.; Milavic, M.; Sikiric, S.; Kocman, I.; et al. Stable gastric pentadecapeptide BPC 157 therapy for primary abdominal compartment syndrome in rats. Front. Pharmacol. 2021, 12, 718147. [Google Scholar] [CrossRef]
- Smoday, I.M.; Petrovic, I.; Kalogjera, L.; Vranes, H.; Zizek, H.; Krezic, I.; Gojkovic, S.; Skorak, I.; Hriberski, K.; Brizic, I.; et al. Therapy effect of the stable gastric pentadecapeptide BPC 157 on acute pancreatitis as vascular failure-induced severe peripheral and central syndrome in rats. Biomedicines 2022, 10, 1299. [Google Scholar] [CrossRef]
- Sharif, N.A. Degeneration of retina-brain components and connections in glaucoma: Disease causation and treatment options for eyesight preservation. Curr. Res. Neurobiol. 2022, 3, 100037. [Google Scholar] [CrossRef] [PubMed]
- Nathan, J. Hippocrates to Duke-Elder: An overview of the history of glaucoma. Clin. Exp. Optom. 2000, 83, 116–118. [Google Scholar] [CrossRef] [PubMed]
- Klimko, P.G.; Sharif, N.A. Discovery, characterization and clinical utility of prostaglandin agonists for the treatment of glaucoma. Br. J. Pharmacol. 2019, 176, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- Realini, T. A history of glaucoma pharmacology. Optom. Vis. Sci. 2011, 88, 36–38. [Google Scholar] [CrossRef] [PubMed]
- Civan, M.; Macknight, A.D. The ins and outs of aqueous humor secretion. Exp. Eye Res. 2004, 78, 625–631. [Google Scholar] [CrossRef]
- Brinchmann-Hansen, O.; Anmarkrud, N. Pilocarpine medication in open-angle glaucoma. A study using pilocarpine eyedrops and an ocular therapeutic system. Acta Ophthalmol. 1979, 57, 55–62. [Google Scholar] [CrossRef]
- Futakuchi, A.; Morimoto, T.; Ikeda, Y.; Tanihara, H.; Inoue, T.; ROCK-S study group collaborators 2020. Intraocular pressure-lowering effects of ripasudil in uveitic glaucoma, exfoliation glaucoma, and steroid-induced glaucoma patients: ROCK-S, a multicentre historical cohort study. Sci. Rep. 2020, 10, 10308. [Google Scholar] [CrossRef]
- Lin, C.W.; Sherman, B.; Moore, L.A.; Laethem, C.L.; Lu, D.W.; Pattabiraman, P.P.; Rao, P.V.; deLong, M.A.; Kopczynski, C.C. Discovery and preclinical development of Netarsudil, a novel ocular hypotensive agent for the treatment of glaucoma. J. Ocul. Pharmacol. Ther. 2018, 34, 40–51. [Google Scholar] [CrossRef]
- Asrani, S.; Bacharach, J.; Holland, E.; McKee, H.; Sheng, H.; Lewis, R.A.; Kopczynski, C.C.; Heah, T. Fixed-dose combination of netarsudil and latanoprost in ocular hypertension and open-angle glaucoma: Pooled efficacy/ safety analysis of phase 3 MERCURY-1 and -2. Adv. Ther. 2020, 37, 1620–1631. [Google Scholar] [CrossRef]
- Camras, C.B.; Bito, L.Z.; Toris, C.B. Prostaglandins and prostaglandin analogues. In Textbook of Ocular Pharmacology; Zimmerman, T.J., Kooner, K.S., Sharir, M., Fechtner, R.D., Eds.; Lippincott-Raven: Philadelphia, PA, USA, 1997; pp. 315–328. [Google Scholar]
- Robert, A. Cytoprotection by prostaglandins. Scand. J. Gastroenterol. 1981, 67, 223–227. [Google Scholar] [CrossRef]
- Robert, A. Cytoprotection by prostaglandins. Gastroenterology 1979, 77, 761–767. [Google Scholar] [CrossRef]
- Robert, A.; Lum, J.T.; Lancaster, C.; Olafsson, A.S.; Kolbasa, K.P.; Nezamis, J.E. Prevention by prostaglandins of caerulein-induced pancreatitis in rats. Lab. Investig. 1989, 60, 677–691. [Google Scholar]
- Elliott, G.; Whited, B.A.; Purmalis, A.; Davis, J.P.; Field, S.O.; Lancaster, C.; Robert, A. Effect of 16,16-dimethyl PGE2 on renal papillary necrosis and gastrointestinal ulcerations (gastric, duodenal, intestinal) produced in rats by mefenamic acid. Life Sci. 1986, 39, 423–432. [Google Scholar] [CrossRef]
- Szabo, S.; Usadel, K.H. Cytoprotection-organoprotection by somatostatin: Gastric and hepatic lesions. Experientia 1982, 38, 254–256. [Google Scholar] [CrossRef]
- Szabó, S. Role of sulfhydryls and early vascular lesions in gastric mucosal injury. Acta Physiol. Hung. 1984, 64, 203–214. [Google Scholar]
- Szabo, S. Experimental basis for a role for sulfhydryls and dopamine in ulcerogenesis: A primer for cytoprotection--organoprotection. Klin. Wochenschr. 1986, 64 (Suppl. 7), 116–122. [Google Scholar]
- Szabo, S.; Trier, J.S.; Brown, A.; Schnoor, J. Early vascular injury and increased vascular permeability in gastric mucosal injury caused by ethanol in the rat. Gastroenterology 1985, 88, 228–236. [Google Scholar] [CrossRef]
- Szabo, S. Mechanism of mucosal protection. In Gastric Cytoprotection: A Clinician’s Guide; Hollander, D., Tarnawski, A., Eds.; Plenum Medical Book Co.: New York, NY, USA, 1989; pp. 49–90. [Google Scholar]
- Pihan, G.; Majzoubi, D.; Haudenschild, C.; Trier, J.S.; Szabo, S. Early microcirculatory stasis in acute gastric mucosal injury in the rat and prevention by 16,16-dimethyl prostaglandin E2 or sodium thiosulfate. Gastroenterology 1986, 91, 1415–1426. [Google Scholar] [CrossRef] [PubMed]
- Eakins, K.E. Prostaglandin and non-prostaglandin mediated breeakdown of the blood-aqueous barrier. Exp. Eye Res. 1977, 25 (Suppl. 1), 483–498. [Google Scholar] [CrossRef]
- Starr, M.S. Further studies on the effect of prostaglandin on intraocular pressure in the rabbit. Exp. Eye Res. 1971, 11, 170–177. [Google Scholar] [CrossRef]
- Conquet, P.; Plazonnet, B.; Le Douarec, J.C. Arachidonic acid-induced elevation of intraocular pressure and anti-inflammatory agents. Investig. Ophthalmol. 1975, 14, 772–775. [Google Scholar]
- Camras, C.B.; Bito, L.Z. Reduction of intraocular pressure in normal and glaucomatous primate (Aotus trivirgatus) eyes by topically applied prostaglandin F2 alpha. Curr. Eye Res. 1981, 1, 205–209. [Google Scholar] [CrossRef]
- Bito, L.Z.; Draga, A.; Blanco, J.; Camras, C.B. Long-term maintenance of reduced intraocular pressure by daily or twice daily topical application of prostaglandins to cat or rhesus monkey eyes. Investig. Ophthalmol. Vis. Sci. 1983, 24, 312–319. [Google Scholar]
- Bito, L.Z.; Camras, C.B.; Gum, G.G.; Resul, B. The ocular hypotensive effects and side effects of prostaglandins on the eyes of experimental animals. Prog. Clin. Biol. Res. 1989, 312, 349–368. [Google Scholar]
- Zhou, L.; Zhan, W.; Wei, X. Clinical pharmacology and pharmacogenetics of prostaglandin analogues in glaucoma. Front. Pharmacol. 2022, 13, 1015338. [Google Scholar] [CrossRef]
- Aihara, M. Prostanoid receptor agonists for glaucoma treatment. Jpn. J. Ophthalmol. 2021, 65, 581–590. [Google Scholar] [CrossRef]
- MacIver, S.; Stout, N.; Ricci, O. New considerations for the clinical efficacy of old and new topical glaucoma medications. Clin. Exp. Optom. 2021, 104, 350–366. [Google Scholar] [CrossRef]
- Xalatan Patent Affirmed by Appeals Court. FDAnews Drug Daily Bulletin. 2005. Available online: http://www.fdanews.com/newsletter/article?articleId=75604&issueId=7953 (accessed on 24 April 2023).
- Laqueur, L. Ueber eine neue therapeutische Verwendung des Physostigmin. Cent. Fur Die Med. Wiss. 1876, 14, 421–422. [Google Scholar]
- Weber, A. Die Ursache des Glaucoms. Arch. Ophthalmol. 1877, 23, 1–91. [Google Scholar] [CrossRef][Green Version]
- Bleiman, B.S.; Schwartz, A.L. Paradoxical intraocular pressure response to pilocarpine. A proposed mechanism and treatment. Arch. Ophthalmol. 1979, 97, 1305–1306. [Google Scholar] [CrossRef]
- Katz, I.M. beta-blockers and the eye: An overview. Ann. Ophthalmol. 1978, 10, 847–850. [Google Scholar] [PubMed]
- Bartels, S.P.; Neufeld, A.H. Mechanisms of topical drugs used in the control of open angle glaucoma. Int. Ophthalmol. Clin. 1980, 20, 105–116. [Google Scholar] [CrossRef]
- Bartels, S.P.; Roth, H.O.; Jumblatt, M.M.; Neufeld, A.H. Pharmacological effects of topical timolol in the rabbit eye. Investig. Ophthalmol. Vis. Sci. 1980, 19, 1189–1197. [Google Scholar]
- Zimmerman, T.J.; Kaufman, H.E. Timolol, dose response and duration of action. Arch. Ophthalmol. 1977, 95, 605–607. [Google Scholar] [CrossRef]
- Becker, B. Decrease in intraocular pressure in man by a carbonic anhydrase inhibitor, diamox; a preliminary report. Am. J. Ophthalmol. 1954, 37, 13–15. [Google Scholar] [CrossRef]
- Grant, W.M.; Trotter, R.R. Diamox (acetazoleamide) in treatment of glaucoma. AMA Arch. Ophthalmol. 1954, 51, 735–739. [Google Scholar] [CrossRef]
- Zimmerman, T.J. Carbonic anhydrase inhibitors: From pills to drops. In 100 Years of Progress in Glaucoma; Van Buskirk, E.M., Shields, M.B., Eds.; Lippincott-Raven: Philadelphia, PA, USA, 1997; pp. 272–277. [Google Scholar]
- Le, H.H.; Chang, M.R.; Cheng, Q.; Lee, D.A.; Hartenbaum, D. The effectiveness and safety of dorzolamide 2% in addition to multiple topical antiglaucoma medications. J. Ocul. Pharmacol. Ther. 1999, 15, 305–312. [Google Scholar] [CrossRef]
- Conlon, R.; Saheb, H.; Ahmed, I.I.K. Glaucoma treatment trends: A review. Can. J. Ophthalmol. 2017, 52, 114–124. [Google Scholar] [CrossRef]
- Janson, B.J.; Alward, W.L.; Kwon, Y.H.; Bettis, D.I.; Fingert, J.H.; Provencher, L.M.; Goins, K.M.; Wagoner, M.D.; Greiner, M.A. Glaucoma-associated corneal endothelial cell damage: A review. Surv. Ophthalmol. 2018, 63, 500–506. [Google Scholar] [CrossRef]
- Kandarakis, S.A.; Togka, K.A.; Doumazos, L.; Mylona, I.; Katsimpris, A.; Petrou, P.; Kymionis, G. The multifarious effects of various glaucoma pharmacotherapy on corneal endothelium: A narrative review. Ophthalmol. Ther. 2023, 12, 1457–1478. [Google Scholar] [CrossRef]
- Baratz, K.H.; Nau, C.B.; Winter, E.J.; McLaren, J.W.; Hodge, D.O.; Herman, D.C.; Bourne, W.M. Effects of glaucoma medications on corneal endothelium, keratocytes, and subbasal nerves among participants in the ocular hypertension treatment study. Cornea 2006, 25, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.S.; Trope, G.E.; Basu, P.K. Beta adrenoceptors and regenerating corneal epithelium. J. Ocul. Pharmacol. 1990, 6, 101–112. [Google Scholar] [CrossRef]
- Trope, G.E.; Liu, G.S.; Basu, P.K. Toxic effects of topically administered betagan, betoptic, and timoptic on regenerating corneal epithelium. J. Ocul. Pharmacol. 1988, 4, 359–366. [Google Scholar] [CrossRef]
- Yuan, X.; Ma, X.; Yang, L.; Zhou, Q.; Li, Y. β-blocker eye drops affect ocular surface through β2 adrenoceptor of corneal limbal stem cells. BMC Ophthalmol. 2021, 21, 419. [Google Scholar] [CrossRef]
- Fan, D.; Fan, T.J. Clonidine induces apoptosis of human corneal epithelial cells through death receptors-mediated, mitochondria-dependent signaling pathway. Toxicol. Sci. 2017, 156, 252–260. [Google Scholar] [CrossRef]
- Tanimura, H.; Minamoto, A.; Narai, A.; Hirayama, T.; Suzuki, M.; Mishima, H.K. Corneal edema in glaucoma patients after the addition of brinzolamide 1% ophthalmic suspension. Jpn. J. Ophthalmol. 2005, 49, 332–333. [Google Scholar] [CrossRef]
- Zhao, J.C.; Chen, T. Brinzolamide induced reversible corneal decompensation. Br. J. Ophthalmol. 2005, 89, 389–390. [Google Scholar] [CrossRef]
- Konowal, A.; Morrison, J.C.; Brown, S.V.; Cooke, D.L.; Maguire, L.J.; Verdier, D.V.; Fraunfelder, F.T.; Dennis, R.F.; Epstein, R.J. Irreversible corneal decompensation in patients treated with topical dorzolamide. Am. J. Ophthalmol. 1999, 127, 403–406. [Google Scholar] [CrossRef]
- Egan, C.A.; Hodge, D.O.; McLaren, J.W.; Bourne, W.M. Effect of dorzolamide on corneal endothelial function in normal human eyes. Investig. Ophthalmol. Vis. Sci. 1998, 39, 23–29. [Google Scholar]
- Lass, J.H.; Khosrof, S.A.; Laurence, J.K.; Horwitz, B.; Ghosh, K.; Adamsons, I. A double-masked, randomized, 1-year study comparing the corneal effects of dorzolamide, timolol, and betaxolol. Dorzolamide Corneal Effects Study Group. Arch. Ophthalmol. 1998, 116, 1003–1010. [Google Scholar] [CrossRef][Green Version]
- Fischbarg, J.; Lim, J.J. Role of cations, anions and carbonic anhydrase in fluid transport across rabbit corneal endothelium. J. Physiol. 1974, 241, 647–675. [Google Scholar] [CrossRef] [PubMed]
- Jang, M.; Kang, K.E.; Cho, B.J. Effect of prostaglandin analogues on central corneal thickness: 3-Year follow-up results. Korean J. Ophthalmol. 2020, 34, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Eraslan, N.; Celikay, O. Effects of topical prostaglandin therapy on corneal layers thickness in primary open-angle glaucoma patients using anterior segment optical coherence tomography. Int. Ophthalmol. 2023, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Yim, H.W. Effect of topical prostaglandin analogue therapy on central corneal thickness. J. Clin. Med. 2022, 12, 44. [Google Scholar] [CrossRef]
- Kadri, R.; Shetty, A.; Parameshwar, D.; Kudva, A.A.; Achar, A.; Shetty, J. Effect of prostaglandin analogues on central corneal thickness in patients with glaucoma: A systematic review and meta-analysis with trial sequential analysis. Indian J. Ophthalmol. 2022, 70, 1502–1512. [Google Scholar] [CrossRef]
- Er, H. The effect of topical parasympathomimetics on corneal epithelial healing in rabbits. Doc. Ophthalmol. 1997, 93, 327–335. [Google Scholar]
- Chernyavsky, A.I.; Galitovskiy, V.; Shchepotin, I.B.; Jester, J.V.; Grando, S.A. The acetylcholine signaling network of corneal epithelium and its role in regulation of random and directional migration of corneal epithelial cells. Investig. Ophthalmol. Vis. Sci. 2014, 55, 6921–6933. [Google Scholar] [CrossRef][Green Version]
- Syed, Z.A.; Rapuano, C.J. Rho kinase (ROCK) inhibitors in the management of corneal endothelial disease. Curr. Opin. Ophthalmol. 2021, 32, 268–274. [Google Scholar] [CrossRef]
- Schlötzer-Schrehardt, U.; Zenkel, M.; Strunz, M.; Gießl, A.; Schondorf, H.; da Silva, H.; Schmidt, G.A.; Greiner, M.A.; Okumura, N.; Koizumi, N.; et al. Potential functional restoration of corneal endothelial cells in Fuchs endothelial corneal dystrophy by ROCK inhibitor (ripasudil). Am. J. Ophthalmol. 2021, 224, 185–199. [Google Scholar] [CrossRef]
- Reina-Torres, E.; De Ieso, M.D.; Pasquale, L.R.; Madekurozwa, M.; van Baternburg-Sherwood, J.; Overby, D.R.; Stamer, W.D. The vital role for nitric oxide in intraocular pressure homeostasis. Prog. Retin. Eye Res. 2021, 83, 100922. [Google Scholar] [CrossRef]
- Eraslan, N.; Ekici, E.; Celikay, O. The effect of topical bimatoprost on corneal clarity in primary open-angle glaucoma: A longitudinal prospective assessment. Int. Ophthalmol. 2022, 42, 731–738. [Google Scholar] [CrossRef]
- Sikiric, P.; Seiwerth, S.; Rucman, R.; Turkovic, B.; Rokotov, D.S.; Brcic, L.; Sever, M.; Klicek, R.; Radic, B.; Drmic, D.; et al. Stable gastric pentadecapeptide BPC 157-NO-system relation. Curr. Pharm. Des. 2014, 20, 1126–1135. [Google Scholar] [CrossRef]
- Sikiric, P.; Drmic, D.; Boban Blagaic, A.; Tvrdeic, A.; Krezic, I.; Gojkovic, S.; Zizek, H.; Sikiric, S.; Strbe, S.; Smoday, I.M.; et al. Stable gastric pentadecapeptide BPC 157 and NO-system. In Nitric Oxide: From Research to Therapeutics; Ray, A., Gulati, K., Eds.; Advances in Biochemistry in Health and Disease 22; Springer Nature Switzerland AG: Cham, Switzerland, 2023; pp. 349–376. [Google Scholar] [CrossRef]
- Sikiric, P.; Seiwerth, S.; Grabarevic, Z.; Rucman, R.; Petek, M.; Jagic, V.; Turkovic, B.; Rotkvic, I.; Mise, S.; Zoricic, I.; et al. The influence of a novel pentadecapeptide, BPC 157, on N(G)-nitro-L-arginine methylester and L-arginine effects on stomach mucosa integrity and blood pressure. Eur. J. Pharmacol. 1997, 332, 23–33. [Google Scholar] [CrossRef]
- Turkovic, B.; Sikiric, P.; Seiwerth, S.; Mise, S.; Anic, T.; Petek, M. Stable gastric pentadecapeptide BPC 157 studied for inflammatory bowel disease (PLD-116, PL14736, Pliva) induces nitric oxide synthesis. Gastroenterology 2004, 126, 287. [Google Scholar]
- Stupnisek, M.; Kokot, A.; Drmic, D.; Hrelec Patrlj, M.; Zenko Sever, A.; Kolenc, D.; Radic, B.; Suran, J.; Bojic, D.; Vcev, A.; et al. Pentadecapeptide BPC 157 reduces bleeding and thrombocytopenia after amputation in rats treated with heparin, warfarin, L-NAME and L-arginine. PLoS ONE 2015, 10, e0123454. [Google Scholar] [CrossRef]
- Stupnisek, M.; Franjic, S.; Drmic, D.; Hrelec, M.; Kolenc, D.; Radic, B.; Bojic, D.; Vcev, A.; Seiwerth, S.; Sikiric, P. Pentadecapeptide BPC 157 reduces bleeding time and thrombocytopenia after amputation in rats treated with heparin, warfarin or aspirin. Thromb. Res. 2012, 129, 652–659. [Google Scholar] [CrossRef]
- Konosic, S.; Petricevic, M.; Ivancan, V.; Konosic, L.; Goluza, E.; Krtalic, B.; Drmic, D.; Stupnisek, M.; Seiwerth, S.; Sikiric, P. Intragastric application of aspirin, clopidogrel, cilostazol, and BPC 157 in rats: Platelet aggregation and blood clot. Oxid. Med. Cell. Longev. 2019, 2019, 9084643. [Google Scholar] [CrossRef]
- Hsieh, M.J.; Lee, C.H.; Chueh, H.Y.; Chang, G.J.; Huang, H.Y.; Lin, Y.; Pang, J.S. Modulatory effects of BPC 157 on vasomotor tone and the activation of Src-Caveolin-1-endothelial nitric oxide synthase pathway. Sci. Rep. 2020, 10, 17078. [Google Scholar] [CrossRef]
- Hsieh, M.J.; Liu, H.T.; Wang, C.N.; Huang, H.Y.; Lin, Y.; Ko, Y.S.; Wang, J.S.; Chang, V.H.; Pang, J.S. Therapeutic potential of pro-angiogenic BPC157 is associated with VEGFR2 activation and up-regulation. J. Mol. Med. 2017, 95, 323–333. [Google Scholar] [CrossRef]
- Gamulin, O.; Oroz, K.; Coric, L.; Krajacic, M.; Skrabic, M.; Dretar, V.; Strbe, S.; Talapko, J.; Juzbasic, M.; Krezic, I.; et al. Fourier transform infrared spectroscopy reveals molecular changes in blood vessels of rats treated with pentadecapeptide BPC 157. Biomedicines 2022, 10, 3130. [Google Scholar] [CrossRef]
- Sikiric, P.; Seiwerth, S.; Rucman, R.; Turkovic, B.; Rokotov, D.S.; Brcic, L.; Sever, M.; Klicek, R.; Radic, B.; Drmic, D.; et al. Toxicity by NSAIDs. Counteraction by stable gastric pentadecapeptide BPC 157. Curr. Pharm. Des. 2013, 19, 76–83. [Google Scholar] [PubMed]
- Park, J.M.; Lee, H.J.; Sikiric, P.; Hahm, K.B. BPC 157 rescued NSAID-cytotoxicity via stabilizing intestinal permeability and enhancing cytoprotection. Curr. Pharm. Des. 2020, 26, 2971–2981. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.A.; Han, Y.M.; An, J.M.; Park, Y.J.; Sikiric, P.; Kim, D.H.; Kwon, K.A.; Kim, Y.J.; Yang, D.; Tchah, H.; et al. BPC157 as potential agent rescuing from cancer cachexia. Curr. Pharm. Des. 2018, 24, 1947–1956. [Google Scholar] [CrossRef]
- Chang, C.H.; Tsai, W.C.; Lin, M.S.; Hsu, Y.H.; Pang, J.H.S. The promoting effect of pentadecapeptide BPC 157 on tendon healing involves tendon outgrowth, cell survival, and cell migration. J. Appl. Physiol. 2011, 110, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.H.; Tsai, W.C.; Hsu, Y.H.; Pang, J.H.S. Pentadecapeptide BPC 157 enhances the growth hormone receptor expression in tendon fibroblasts. Molecules 2014, 19, 19066–19077. [Google Scholar] [CrossRef]
- Huang, T.; Zhang, K.; Sun, L.; Xue, X.; Zhang, C.; Shu, Z.; Mu, N.; Gu, J.; Zhang, W.; Wang, Y.; et al. Body protective compound-157 enhances alkali-burn wound healing in vivo and promotes proliferation, migration, and angiogenesis in vitro. Drug Des. Devel. Ther. 2015, 9, 2485–2499. [Google Scholar] [CrossRef]
- Tkalcevic, V.I.; Cuzic, S.; Brajsa, K.; Mildner, B.; Bokulic, A.; Situm, K.; Perovic, D.; Glojnaric, I.; Parnham, M.J. Enhancement by PL 14736 of granulation and collagen organization in healing wounds and the potential role of egr-1 expression. Eur. J. Pharmacol. 2007, 570, 212–221. [Google Scholar] [CrossRef]
- Wang, X.Y.; Qu, M.; Duan, R.; Shi, D.; Jin, L.; Gao, J.; Wood, J.D.; Li, J.; Wang, G.D. Cytoprotective mechanism of the novel gastric peptide BPC157 in gastrointestinal tract and cultured enteric neurons and glial cells. Neurosci. Bull. 2019, 35, 167–170. [Google Scholar] [CrossRef]
- Wu, H.; Wei, M.; Li, N.; Lu, Q.; Shrestha, S.M.; Tan, J.; Zhang, Z.; Wu, G.; Shi, R. Clopidogrel-induced gastric injury in rats is attenuated by stable gastric pentadecapeptide BPC 157. Drug Des. Devel. Ther. 2020, 14, 5599–5610. [Google Scholar] [CrossRef]
- Huang, B.S.; Huang, S.C.; Chen, F.H.; Chang, Y.; Mei, H.F.; Huang, H.Y.; Chen, W.Y.; Pang, J.S. Pentadecapeptide BPC 157 efficiently reduces radiation-induced liver injury and lipid accumulation through Kruppel-like factor 4 upregulation both in vivo and in vitro. Life Sci. 2022, 310, 121072. [Google Scholar] [CrossRef]
- Mittag, T.W.; Danias, J.; Pohorenec, G.; Yuan, H.M.; Burakgazi, E.; Chalmers-Redman, R.; Podos, S.M.; Tatton, W.G. Retinal damage after 3 to 4 months of elevated intraocular pressure in a rat glaucoma model. Investig. Ophthalmol. Vis. Sci. 2000, 41, 3451–3459. [Google Scholar]
- Goldblum, D.; Kontiola, A.I.; Mittag, T.; Chen, B.; Danias, J. Non-invasive determination of intraocular pressure in the rat eye. Comparison of an electronic tonometer (TonoPen), and a rebound (impact probe) tonometer. Graefes Arch. Clin. Exp. Ophthalmol. 2002, 240, 942–946. [Google Scholar] [CrossRef]
- Urcola, J.H.; Hernández, M.; Vecino, E. Three experimental glaucoma models in rats: Comparison of the effects of intraocular pressure elevation on retinal ganglion cell size and death. Exp. Eye Res. 2006, 83, 429–437. [Google Scholar] [CrossRef]
- Danias, J.; Shen, F.; Kavalarakis, M.; Chen, B.; Goldblum, D.; Lee, K.; Zamora, M.F.; Su, Y.; Brodie, S.E.; Podos, S.M.; et al. Characterization of retinal damage in the episcleral vein cauterization rat glaucoma model. Exp. Eye. Res. 2006, 82, 219–228. [Google Scholar] [CrossRef]
- Vidal-Sanz, M.; Salinas-Navarro, M.; Nadal-Nicolás, F.M.; Alarcón-Martínez, L.; Valiente-Soriano, F.J.; de Imperial, J.M.; Avilés-Trigueros, M.; Agudo-Barriuso, M.; Villegas-Pérez, M.P. Understanding glaucomatous damage: Anatomical and functional data from ocular hypertensive rodent retinas. Prog. Retin. Eye Res. 2012, 31, 1–27. [Google Scholar] [CrossRef]
- Biswas, S.; Wan, K.H. Review of rodent hypertensive glaucoma models. Acta Ophthalmol. 2019, 97, e331–e340. [Google Scholar] [CrossRef]
- McKinnon, S.J.; Schlamp, C.L.; Nickells, R.W. Mouse models of retinal ganglion cell death and glaucoma. Exp. Eye Res. 2009, 88, 816–824. [Google Scholar] [CrossRef]
- Pang, I.H.; Clark, A.F. Rodent models for glaucoma retinopathy and optic neuropathy. J. Glaucoma 2007, 16, 483–505. [Google Scholar] [CrossRef]
- Johnson, T.V.; Tomarev, S.I. Rodent models of glaucoma. Brain Res. Bull. 2010, 81, 349–358. [Google Scholar] [CrossRef]
- Ahmed, F.A.; Chaudhary, P.; Sharma, S.C. Effects of increased intraocular pressure on rat retinal ganglion cells. Int. J. Dev. Neurosci. 2001, 19, 209–218. [Google Scholar] [CrossRef]
- Naskar, R.; Wissing, M.; Thanos, S. Detection of early neuron degeneration and accompanying microglial responses in the retina of a rat model of glaucoma. Investig. Ophthalmol. Vis. Sci. 2002, 43, 2962–2968. [Google Scholar]
- Kanamori, A.; Nakamura, M.; Mukuno, H.; Maeda, H.; Negi, A. Diabetes has an additive effect on neural apoptosis in rat retina with chronically elevated intraocular pressure. Curr. Eye Res. 2004, 28, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Park, C.K. Retinal ganglion cell death is delayed by activation of retinal intrinsic cell survival program. Brain Res. 2005, 1057, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Kanamori, A.; Nakamura, M.; Nakanishi, Y.; Nagai, A.; Mukuno, H.; Yamada, Y.; Negi, A. Akt is activated via insulin/IGF-1 receptor in rat retina with episcleral vein cauterization. Brain Res. 2004, 1022, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, R.; Zhou, X.; Wu, J. Decreased d-serine levels prevent retinal ganglio cell apoptosis in glaucomatous animal model. Investig. Ophthalmol. Vis. Sci. 2018, 59, 5045–5052. [Google Scholar] [CrossRef]
- Ahmed, F.A.; Hegazy, K.; Chaudhary, P.; Sharma, S.C. Neuroprotective effect of alpha(2) agonist (brimonidine) on adult rat retinal ganglion cells after increased intraocular pressure. Brain Res. 2001, 913, 133–139. [Google Scholar] [CrossRef]
- Ashpole, N.E.; Overby, D.R.; Ethier, C.R.; Stamer, W.D. Shear stress-triggered nitric oxide release from Schlemm’s canal cells. Investig. Ophthalmol. Vis. Sci. 2014, 55, 8067–8076. [Google Scholar] [CrossRef]
- Lima, M.G.; Maximino, C.; Matos Oliveira, K.R.; Brasil, A.; Crespo-Lopez, M.E.; Batista Ede, J.; Rocha, F.A.; Picanço-Diniz, D.L.; Herculano, A.M. Nitric oxide as a regulatory molecule in the processing of the visual stimulus. Nitric Oxide 2014, 36, 44–50. [Google Scholar] [CrossRef]
- Cramer, K.S.; Leamey, C.A.; Sur, M. Nitric oxide as a signaling molecule in visual system development. Prog. Brain Res. 1998, 118, 101–114. [Google Scholar]
- Cudeiro, J.; Rivadulla, C. Sight and insight—On the physiological role of nitric oxide in the visual system. Trends Neurosci. 1999, 22, 389. [Google Scholar] [CrossRef]
- Toda, N.; Nakanishitoda, M. Nitric Oxide: Ocular Blood Flow, Glaucoma, Anddiabetic Retinopathy. Prog. Retin. Eye Res. 2007, 26, 205–238. [Google Scholar] [CrossRef]
- Lucas-Ruiz, F.; Galindo-Romero, C.; Albaladejo-García, V.; Vidal-Sanz, M.; Agudo-Barriuso, M. Mechanisms implicated in the contralateral effect in the central nervous system after unilateral injury: Focus on the visual system. Neural. Regen. Res. 2021, 16, 2125–2131. [Google Scholar] [CrossRef]
- Osborne, N.N.; Casson, R.J.; Wood, J.P.; Chidlow, G.; Graham, M.; Melena, J. Retinal ischemia: Mechanisms of damage and potential therapeutic strategies. Prog. Retin. Eye Res. 2004, 23, 91–147. [Google Scholar] [CrossRef]
- Belosic Halle, Z.; Vlainic, J.; Drmic, D.; Strinic, D.; Luetic, K.; Sucic, M.; Medvidovic-Grubisic, M.; Pavelic Turudic, T.; Petrovic, I.; Seiwerth, S.; et al. Class side effects: Decreased pressure in the lower oesophageal and the pyloric sphincters after the administration of dopamine antagonists, neuroleptics, anti-emetics, L-NAME, pentadecapeptide BPC 157 and L-arginine. Inflammopharmacology 2017, 25, 511–522. [Google Scholar] [CrossRef]
- Luetic, K.; Sucic, M.; Vlainic, J.; Halle, Z.B.; Strinic, D.; Vidovic, T.; Luetic, F.; Marusic, M.; Gulic, S.; Pavelic, T.T.; et al. Cyclophosphamide induced stomach and duodenal lesions as a NO-system disturbance in rats: L-NAME, L-arginine, stable gastric pentadecapeptide BPC 157. Inflammopharmacology 2017, 25, 255–264. [Google Scholar] [CrossRef]
- Sucic, M.; Luetic, K.; Jandric, I.; Drmic, D.; Sever, A.Z.; Vuletic, L.B.; Halle, Z.B.; Strinic, D.; Kokot, A.; Seiwerth, R.S.; et al. Therapy of the rat hemorrhagic cystitis induced by cyclophosphamide. Stable gastric pentadecapeptide BPC 157, L-arginine, L-NAME. Eur. J. Pharmacol. 2019, 861, 172593. [Google Scholar] [CrossRef] [PubMed]
- Sever, A.Z.; Sever, M.; Vidovic, T.; Lojo, N.; Kolenc, D.; Vuletic, L.B.; Drmic, D.; Kokot, A.; Zoricic, I.; Coric, M.; et al. Stable gastric pentadecapeptide BPC 157 in the therapy of the rats with bile duct ligation. Eur. J. Pharmacol. 2019, 847, 130–142. [Google Scholar] [CrossRef]
- Amic, F.; Drmic, D.; Bilic, Z.; Krezic, I.; Zizek, H.; Peklic, M.; Klicek, R.; Pajtak, A.; Amic, E.; Vidovic, T.; et al. Bypassing major venous occlusion and duodenal lesions in rats, and therapy with the stable gastric pentadecapeptide BPC 157, L-NAME and L-arginine. World J. Gastroenterol. 2018, 24, 5366–5378. [Google Scholar] [CrossRef]
- Duzel, A.; Vlainic, J.; Antunovic, M.; Malekinusic, D.; Vrdoljak, B.; Samara, M.; Gojkovic, S.; Krezic, I.; Vidovic, T.; Bilic, Z.; et al. Stable gastric pentadecapeptide BPC 157 in the treatment of colitis and ischemia and reperfusion in rats: New insights. World J. Gastroenterol. 2017, 23, 8465–8488. [Google Scholar] [CrossRef]
- Cesar, L.B.; Gojkovic, S.; Krezic, I.; Malekinusic, D.; Zizek, H.; Vuletic, L.B.; Petrovic, A.; Pavlov, K.H.; Drmic, D.; Kokot, A.; et al. Bowel adhesion and therapy with the stable gastric pentadecapeptide BPC 157, L-NAME and L-arginine in rats. World J. Gastrointest. Pharmacol. Ther. 2020, 11, 93–109. [Google Scholar] [CrossRef]
- Hirooka, K.; Yamamoto, T.; Kiuchi, Y. Dysfunction of axonal transport in normal-tension glaucoma: A biomarker of disease progression and a potential therapeutic target. Neural Regen. Res. 2021, 16, 506–507. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, P.C.; Thompson, H.S. Mydriasis and increased intraocular pressure. II. Iris fluorescein studies. Arch. Ophthalmol. 1972, 87, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, P.C.; Thompson, H.S. Mydriasis and increased intraocular pressure. I. Pupillographic studies. Arch. Ophthalmol. 1972, 87, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, H.M.G. Effect of pharmacological mydriasis on intraocular pressure in eyes with filtering blebs compared to normal eyes: A pilot study. Clin. Ophthalmol. 2022, 16, 231–237. [Google Scholar] [CrossRef]
- McDonald, J.E.; Kiland, J.A.; Kaufman, P.L.; Bentley, E.; Ellinwood, N.M.; McLellan, G.J. Effect of topical latanoprost 0.005% on intraocular pressure and pupil diameter in normal and glaucomatous cats. Vet. Ophthalmol. 2016, 19 (Suppl. 1), 13–23. [Google Scholar] [CrossRef]
- Kiland, J.A.; Voss, A.M.; McLellan, G.J. Effect of timolol maleate gel-forming solution on intraocular pressure, pupil diameter, and heart rate in normal and glaucomatous cats. Vet. Ophthalmol. 2016, 19 (Suppl. 1), 91–96. [Google Scholar] [CrossRef]
- Wilkie, D.A.; Latimer, C.A. Effects of topical administration of timolol maleate on intraocular pressure and pupil size in cats. Am. J. Vet. Res. 1991, 52, 436–440. [Google Scholar]
- Slenter, I.J.M.; Djajadiningrat-Laanen, S.C.; Elders, D.J.; de Gee, R.; Koele, L.E.; Vermeer, L.W.; Boevé, M.H. The effects of topical dorzolamide 2% and brinzolamide 1%, either alone or combined with timolol 0.5%, on intraocular pressure, pupil diameter, and heart rate in healthy cats. Vet. Ophthalmol. 2020, 23, 16–24. [Google Scholar] [CrossRef]
- Wilkie, D.A.; Latimer, C.A. Effects of topical administration of 2.0% pilocarpine on intraocular pressure and pupil size in cats. Am. J. Vet. Res. 1991, 52, 441–444. [Google Scholar]
- Pfeiffer, N.; Traverso, C.E.; Lorenz, K.; Saarela, V.; Liinamaa, J.; Uusitalo, H.; Astakhov, Y.; Boiko, E.; Ropo, A.; Preservative-free Tafluprost/Timolol Fixed Combination Study Group. A 6-month study comparing efficacy, safety, and tolerability of the preservative-free fixed combination of tafluprost 0.0015% and timolol 0.5% versus each of its individual preservative-free components. Adv. Ther. 2014, 31, 1228–1246. [Google Scholar] [CrossRef]
- Traverso, C.E.; Ropo, A.; Papadia, M.; Uusitalo, H. A phase II study on the duration and stability of the intraocular pressure-lowering effect and tolerability of Tafluprost compared with latanoprost. J. Ocul. Pharmacol. Ther. 2010, 26, 97–104. [Google Scholar] [CrossRef]
- Van der Valk, R.; Webers, C.A.; Schouten, J.S.; Zeegers, M.P.; Hendrikse, F. Intraocular pressure-lowering effects of all commonly used glaucoma drugs: A meta-analysis of randomized clinical trials. Ophthalmology 2005, 112, 1177–1185. [Google Scholar] [CrossRef]
- Webers, C.A.; Beckers, H.J.; Zeegers, M.P.; Nuijts, R.M.; Hendrikse, F. The intraocular pressure-lowering effect of prostaglandin analogs combined with topical ß-blocker therapy: A systematic review and meta-analysis. Ophthalmology 2010, 117, 2067–2074.e6. [Google Scholar] [CrossRef]
- Boyle, J.E.; Ghosh, K.; Gieser, D.K.; Adamsons, I.A. A randomized trial comparing the dorzolamide-timolol combination given twice daily to monotherapy with timolol and dorzolamide. Ophthalmology 1998, 105, 1945–1951. [Google Scholar] [CrossRef]
- Cheng, J.-W.; Cheng, S.-W.; Gao, L.-D.; Lu, G.-C.; Wei, R.-L. Intraocular pressure-lowering effects of commonly used fixed-combination drus with timolol. A systemic review and meta-analysis. PLoS ONE 2012, 7, e45079. [Google Scholar] [CrossRef]
- Lippa, E.A.; Carlson, L.E.; Ehinger, B.; Eriksson, L.O.; Finnström, K.; Holmin, C.; Nilsson, S.E.; Nyman, K.; Raitta, C.; Ringvold, A.; et al. Dose response and duration of action of dorzolamide, a topical carbonic anhydrase inhibitor. Arch. Ophthalmol. 1992, 110, 495–499. [Google Scholar] [CrossRef]
- Li, T.; Lindsley, K.; Rouse, B.; Hong, H.; Shi, Q.; Friedman, S.S.; Wormald, R.; Dickersin, K. Comparative effectiveness of first-line medications for primary open-angle glaucoma: A systematic review and network meta-analysis. Ophthalmology 2016, 123, 129–140. [Google Scholar] [CrossRef]
- Pang, I.H.; Wang, W.H.; Clark, A.F. Acute effects of glaucoma medications on rat intraocular pressure. Exp. Eye Res. 2005, 80, 207–214. [Google Scholar] [CrossRef]
- Husain, S.; Whitlock, N.A.; Rice, D.S.; Crosson, C.E. Effects of latanoprost on rodent intraocular pressure. Exp. Eye Res. 2006, 83, 1453–1458. [Google Scholar] [CrossRef]
- Bertaud, S.; Aragno, V.; Baudouin, C.; Labbé, A. Primary open-angle glaucoma. Rev. Med. Interne. 2019, 40, 445–452. [Google Scholar] [CrossRef]
- Agrawal, A.; Singh, A.; Mittal, S.K. Glaucoma in Asia- An epidemiological perspective. Nepal. J. Ophthalmol. 2017, 9, 208–211. [Google Scholar] [CrossRef]
- Minegishi, Y.; Nakayama, M.; Iejima, D.; Kawase, K.; Iwata, T. Significance of optineurin mutations in glaucoma and other diseases. Prog. Retin. Eye Res. 2016, 55, 149–181. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, A.I.; Salazar, J.J.; de Hoz, R.; Rojas, B.; Gallego, B.I.; Salobrar-García, E.; Valiente-Soriano, F.J.; Triviño, A.; Ramirez, J.M. Macro- and microglial responses in the fellow eyes contralateral to glaucomatous eyes. Prog. Brain Res. 2015, 220, 155–172. [Google Scholar] [PubMed]
- Gallego, B.I.; Salazar, J.J.; de Hoz, R.; Rojas, B.; Ramírez, A.I.; Salinas-Navarro, M.; Ortín-Martínez, A.; Valiente-Soriano, F.J.; Avilés-Trigueros, M.; Villegas-Perez, M.P.; et al. IOP induces upregulation of GFAP and MHC-II and microglia reactivity in mice retina contralateral to experimental glaucoma. J. Neuroinflamm. 2012, 9, 92. [Google Scholar] [CrossRef] [PubMed]
- Rojas, B.; Gallego, B.I.; Ramírez, A.I.; Salazar, J.J.; de Hoz, R.; Valiente-Soriano, F.J.; Avilés-Trigueros, M.; Villegas-Perez, M.P.; Vidal-Sanz, M.; Triviño, A.; et al. Microglia in mouse retina contralateral to experimental glaucoma exhibit multiple signs of activation in all retinal layers. J. Neuroinflamm. 2014, 11, 133. [Google Scholar] [CrossRef]
- Mac Nair, C.E.; Nickells, R.W. Neuroinflammation in glaucoma and optic nerve damage. Prog. Mol. Biol. Transl. Sci. 2015, 134, 343–363. [Google Scholar]
- Kanamori, A.; Nakamura, M.; Nakanishi, Y.; Yamada, Y.; Negi, A. Long-term glial reactivity in rat retinas ipsilateral and contralateral to experimental glaucoma. Exp. Eye Res. 2005, 81, 48–56. [Google Scholar] [CrossRef]
- Salinas-Navarro, M.; Alarcón-Martínez, L.; Valiente-Soriano, F.J.; Ortín-Martínez, A.; Jiménez-López, M.; Avilés-Trigueros, M.; Villegas-Pérez, M.P.; de la Villa, P.; Vidal-Sanz, M. Functional and morphological effects of laser-induced ocular hypertension in retinas of adult albino Swiss mice. Mol. Vis. 2009, 15, 2578–2598. [Google Scholar]
- Imai, N.; Tsuyama, Y.; Murayama, K.; Adachi-Usami, E. Protective effect of nitric oxide on ischemic retina. Nippon. Ganka Gakkai Zasshi 1997, 101, 639–643. [Google Scholar]
- Ostwald, P.; Goldstein, I.M.; Pachnanda, A.; Roth, S. Effect of nitric oxide synthase inhibition on blood flow after retinal ischemia in cats. Investig. Ophthalmol. Vis. Sci. 1995, 36, 2396–2403. [Google Scholar]
- Ostwald, P.; Park, S.S.; Toledano, A.Y.; Roth, S. Adenosine receptor blockade and nitric oxide synthase inhibition in the retina: Impact upon post-ischemic hyperemia and the electroretinogram. Vision Res. 1997, 37, 3453–3461. [Google Scholar] [CrossRef]
- Hangai, M.; Yoshimura, N.; Hiroi, K.; Mandai, M.; Honda, Y. Interleukin-1 gene expression in transient retinal ischemia in the rat. Investig. Ophthalmol. Vis. Sci. 1995, 36, 571–578. [Google Scholar]
- Sakamoto, K.; Yonoki, Y.; Kubota, Y.; Kuwagata, M.; Saito, M.; Nakahara, T.; Ishii, K. Inducible nitric oxide synthase inhibitors abolished histological protection by late ischemic preconditioning in rat retina. Exp. Eye Res. 2006, 82, 512–518. [Google Scholar] [CrossRef]
- Nagaoka, T.; Sakamoto, T.; Mori, F.; Sato, E.; Yoshida, A. The effect of nitric oxide on retinal blood flow during hypoxia in cats. Investig. Ophthalmol. Vis. Sci. 2002, 43, 3037–3044. [Google Scholar]
- Sridhar, M.S. Anatomy of cornea and ocular surface. Indian J. Ophthalmol. 2018, 66, 190–194. [Google Scholar] [CrossRef]
- Quazi, Y.; Wong, G.; Monson, B.; Stringham, J.; Ambati, B.K. Corneal transparency: Genesis, maintenance and dysfunction. Brain Res. Bull. 2010, 81, 198–210. [Google Scholar] [CrossRef]
- Edelhauser, H.F. The balance between corneal transparency and edema: The Proctor Lecture. Invest. Ophthalmol. Vis. Sci. 2006, 47, 1754–1767. [Google Scholar] [CrossRef]
- Donn, A.; Maurice, D.M.; Mills, N.L. Studies on the living cornea in vitro. II. The active transport of sodium across the epithelium. Arch. Ophthalmol. 1959, 62, 748–757. [Google Scholar] [CrossRef]
- Harris, J.E.; Nordquist, L.I. The hydration of the cornea: I. Transport of water from the cornea. Am. J. Ophthalmol. 1955, 42, 100–110. [Google Scholar] [CrossRef]
- Zadunaisky, J.A.; Lande, M.A.; Chalfie, M.; Neufeld, A.H. Ion pumps in the cornea and their stimulation by epinephrine and cyclic-AMP. Exp. Eye. Res. 1973, 15, 577–583. [Google Scholar] [CrossRef]
- Klyce, S.D.; Neufeld, A.N.; Zadunaisky, J.A. The activation of chloride transport by epinephrine and Db cyclic-AMP in the cornea of the rabbit. Investig. Ophthalmol. 1973, 12, 127–139. [Google Scholar]
- Schultz, G.; Cipolla, L.; Whitehouse, A.; Eiferman, R.; Woost, P.; Jumblatt, M. Growth factors and corneal endothelial cells: III. Stimulation of adult human corneal endothelial cell mitosis in vitro by defined mitogenic agents. Cornea 1992, 11, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Tshionyi, M.; Shay, E.; Lunde, E.; Lin, A.; Han, K.Y.; Jain, S.; Chang, J.H.; Azar, D.T. Hemangiogenesis and lymphangiogenesis in corneal pathology. Cornea 2012, 31, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Azar, D.T. Corneal angiogenic privilege: Angiogenic and antiangiogenic factors in corneal avascularity, vasculogenesis, and wound healing (an American Ophthalmological Society thesis). Trans. Am. Ophthalmol. Soc. 2006, 104, 264–302. [Google Scholar]
- Kaminska, G.M.; Niederkorn, J.Y. Spontaneous corneal neovascularization in nude mice. Local imbalance between angiogenic and anti-angiogenic factors. Investig. Ophthalmol. Vis. Sci. 1993, 34, 222–230. [Google Scholar]
- Maisonpierre, P.C.; Suri, C.; Jones, P.F.; Bartunkova, S.; Wiegand, S.J.; Radziejewski, C.; Compton, D.; McClain, J.; Aldrich, T.H.; Papadopoulos, N.; et al. Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science 1997, 277, 55–60. [Google Scholar] [CrossRef]
- Brcic, L.; Brcic, I.; Staresinic, M.; Novinscak, T.; Sikiric, P.; Seiwerth, S. Modulatory effect of gastric pentadecapeptide BPC 157 on angiogenesis in muscle and tendon healing. J. Physiol. Pharmacol. 2009, 60 (Suppl. 7), 191–196. [Google Scholar]
- Seiwerth, S.; Rucman, R.; Turkovic, B.; Sever, M.; Klicek, R.; Radic, B.; Drmic, D.; Stupnisek, M.; Misic, M.; Vuletic, L.B.; et al. BPC 157 and standard angiogenic growth factors. Gastrointestinal tract healing, lessons from tendon, ligament, muscle and bone healing. Curr. Pharm. Des. 2018, 24, 1972–1989. [Google Scholar] [CrossRef]
- Kozobolis, V.P.; Detorakis, E.T.; Maskaleris, G.; Koukoula, S.C.; Fountoulakis, N.; Chrysochoou, F.; Konstas, A.G. Corneal sensitivity changes following the instillation of latanoprost, bimatoprost, and travoprost eyedrops. Am. J. Ophthalmol. 2005, 139, 742–743. [Google Scholar] [CrossRef]
- Kohlhaas, M.; Mammen, A.; Richard, G. Change in corneal sensitivity after topical dorzolamide administration. A comparative study. Ophthalmologe 1997, 94, 424–427. [Google Scholar] [CrossRef]
- Romero-Díaz de León, L.; Morales-León, J.E.; Ledesma-Gil, J.; Navas, A. Conjunctival and corneal sensitivity in patients under topical antiglaucoma treatment. Int. Ophthalmol. 2016, 36, 299–303. [Google Scholar] [CrossRef]
- Terai, N.; Müller-Holz, M.; Spoerl, E.; Pillunat, L.E. Short-term effect of topical antiglaucoma medication on tear-film stability, tear secretion, and corneal sensitivity in healthy subjects. Clin. Ophthalmol. 2011, 5, 517–525. [Google Scholar] [CrossRef]
- Adachi, K.; Kashii, S.; Masai, H.; Ueda, M.; Morizane, C.; Kaneda, K.; Kume, T.; Akaike, A.; Honda, Y. Mechanism of the pathogenesis of glutamate neurotoxicity in retinal ischemia. Arch. Clin. Exp. Ophthalmol. 1998, 236, 766–774. [Google Scholar] [CrossRef]
- Adachi, K.; Fujita, Y.; Morizane, C.; Akaike, A.; Ueda, M.; Satoh, M.; Masai, H.; Kashii, S.; Honda, Y. Inhibition of NMDA receptors and nitric oxide synthase reduces ischemic injury of the retina. Eur. J. Pharmacol. 1998, 350, 53–57. [Google Scholar] [CrossRef]
- Ju, W.K.; Kim, K.Y.; Park, S.J.; Park, D.K.; Park, C.B.; Oh, S.J.; Chung, J.W.; Chun, M.H. Nitric oxide is involved in sustained and delayed cell death of rat retina following transient ischemia. Brain Res. 2000, 881, 231–236. [Google Scholar] [CrossRef]
- Lozic, M.; Stambolija, V.; Krezic, I.; Dugandzic, A.; Zivanovic-Posilovic, G.; Gojkovic, S.; Kovacevic, J.; Vrdoljak, L.; Mirkovic, I.; Kokot, A.; et al. In relation to NO-system, stable pentadecapeptide BPC 157 counteracts lidocaine-induced adverse effects in rats and depolarisation in vitro. Emerg. Med. Int. 2020, 2020, 6805354. [Google Scholar] [CrossRef]
- Zivanovic-Posilovic, G.; Balenovic, D.; Barisic, I.; Strinic, D.; Stambolija, V.; Udovicic, M.; Uzun, S.; Drmic, D.; Vlainic, J.; Bencic, M.L.; et al. Stable gastric pentadecapeptide BPC 157 and bupivacaine. Eur. J. Pharmacol. 2016, 793, 56–65. [Google Scholar] [CrossRef]
- Medvidovic-Grubisic, M.; Stambolija, V.; Kolenc, D.; Katancic, J.; Murselovic, T.; Plestina-Borjan, I.; Strbe, S.; Drmic, D.; Barisic, I.; Sindic, A.; et al. Hypermagnesemia disturbances in rats, NO-related: Pentadecapeptide BPC 157 abrogates, L-NAME and L-arginine worsen. Inflammopharmacology 2017, 25, 439–449. [Google Scholar] [CrossRef]
- Barisic, I.; Balenovic, D.; Klicek, R.; Radic, B.; Nikitovic, B.; Drmic, D.; Udovicic, M.; Strinic, D.; Bardak, D.; Berkopic, L.; et al. Mortal hyperkalemia disturbances in rats are NO-system related. The life saving effect of pentadecapeptide BPC 157. Regul. Pept. 2013, 181, 50–66. [Google Scholar] [CrossRef]
- Balenovic, D.; Barisic, I.; Prkacin, I.; Horvat, I.; Udovicic, M.; Uzun, S.; Strinic, D.; Pevec, D.; Drmic, D.; Radic, B.; et al. Mortal furosemide-hypokalemia-disturbances in rats NO-system related shorten survival by L-NAME. Therapy benefit with BPC 157 peptide more than with L-arginine. J. Clin. Exp. Cardiol. 2012, 3, 201. [Google Scholar] [CrossRef]
- McGee, H.T.; Fraunfelder, F.W. Toxicities of topical ophthalmic anesthetics. Expert Opin. Drug Saf. 2007, 6, 637–640. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, K.; Tashiro, A.; Thompson, R.; Nishida, Y.; Bereiter, D.A. Trigeminal interpolaris/caudalis transition neurons mediate reflex lacrimation evoked by bright light in the rat. Eur. J. Neurosci. 2012, 36, 3492–3499. [Google Scholar] [CrossRef] [PubMed]
- Grabarevic, Z.; Tisljar, M.; Artukovic, B.; Bratulic, M.; Dzaja, P.; Seiwerth, S.; Sikiric, P.; Peric, J.; Geres, D.; Kos, J. The influence of BPC 157 on nitric oxide agonist and antagonist induced lesions in broiler chicken. J. Physiol. Paris 1997, 91, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Tlak Gajger, I.; Ribaric, J.; Smodis Skerl, M.; Vlainic, J.; Sikiric, P. Stable gastric pentadecapeptide BPC 157 in honeybee (Apis mellifera) therapy, to control Nosema ceranae invasions in apiary conditions. J. Vet. Pharmacol. Ther. 2018, 41, 614–621. [Google Scholar] [CrossRef]
- Tlak Gajger, I.; Smodis Skerl, M.I.; Sostaric, P.; Suran, J.; Sikiric, P.; Vlainic, J. Physiological and immunological status of adult honeybees (Apis mellifera) fed sugar syrup supplemented with pentadecapeptide BPC 157. Biology 2021, 10, 891. [Google Scholar] [CrossRef]
- Xu, C.; Sun, L.; Ren, F.; Huang, P.; Tian, Z.; Cui, J.; Zhang, W.; Wang, S.; Zhang, K.; He, L.; et al. Preclinical safety evaluation of body protective compound-157, a potential drug for treating various wounds. Regul. Toxicol. Pharmacol. 2020, 114, 104665. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sikiric, P.; Kokot, A.; Kralj, T.; Zlatar, M.; Masnec, S.; Lazic, R.; Loncaric, K.; Oroz, K.; Sablic, M.; Boljesic, M.; et al. Stable Gastric Pentadecapeptide BPC 157—Possible Novel Therapy of Glaucoma and Other Ocular Conditions. Pharmaceuticals 2023, 16, 1052. https://doi.org/10.3390/ph16071052
Sikiric P, Kokot A, Kralj T, Zlatar M, Masnec S, Lazic R, Loncaric K, Oroz K, Sablic M, Boljesic M, et al. Stable Gastric Pentadecapeptide BPC 157—Possible Novel Therapy of Glaucoma and Other Ocular Conditions. Pharmaceuticals. 2023; 16(7):1052. https://doi.org/10.3390/ph16071052
Chicago/Turabian StyleSikiric, Predrag, Antonio Kokot, Tamara Kralj, Mirna Zlatar, Sanja Masnec, Ratimir Lazic, Kristina Loncaric, Katarina Oroz, Marko Sablic, Marta Boljesic, and et al. 2023. "Stable Gastric Pentadecapeptide BPC 157—Possible Novel Therapy of Glaucoma and Other Ocular Conditions" Pharmaceuticals 16, no. 7: 1052. https://doi.org/10.3390/ph16071052
APA StyleSikiric, P., Kokot, A., Kralj, T., Zlatar, M., Masnec, S., Lazic, R., Loncaric, K., Oroz, K., Sablic, M., Boljesic, M., Antunovic, M., Sikiric, S., Strbe, S., Stambolija, V., Beketic Oreskovic, L., Kavelj, I., Novosel, L., Zubcic, S., Krezic, I., ... Staresinic, M. (2023). Stable Gastric Pentadecapeptide BPC 157—Possible Novel Therapy of Glaucoma and Other Ocular Conditions. Pharmaceuticals, 16(7), 1052. https://doi.org/10.3390/ph16071052





