Evaluating Sex Differences in Efficacy, Safety and Pharmacokinetics in Patients Treated with Cannabis by a Metered-Dose Inhaler
Abstract
:1. Introduction
2. Results
2.1. Real-World Evidence Data
2.1.1. Sample
Patient Characteristics
2.1.2. Inhaler Treatment Characteristics
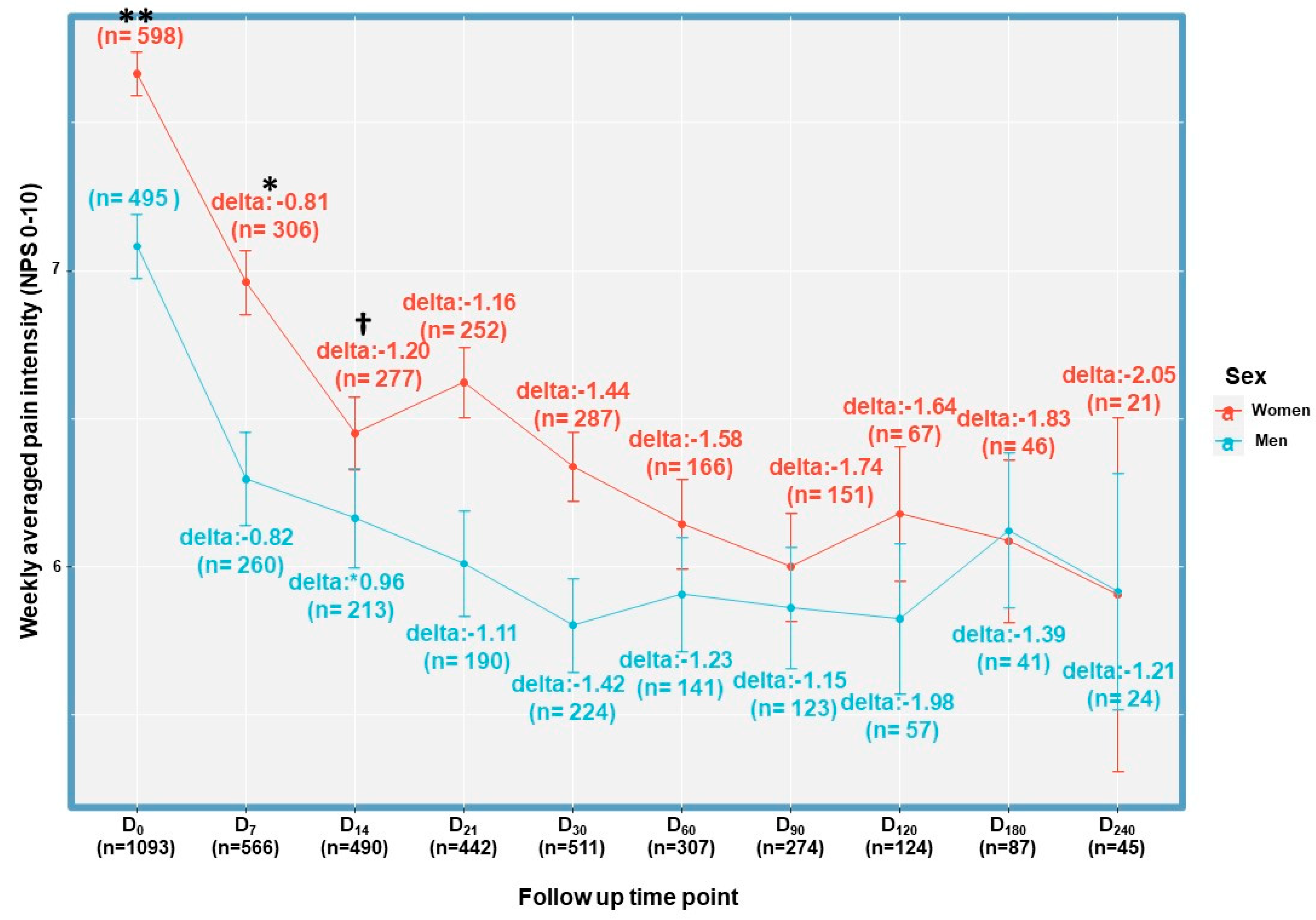
2.1.3. Treatment Effectiveness
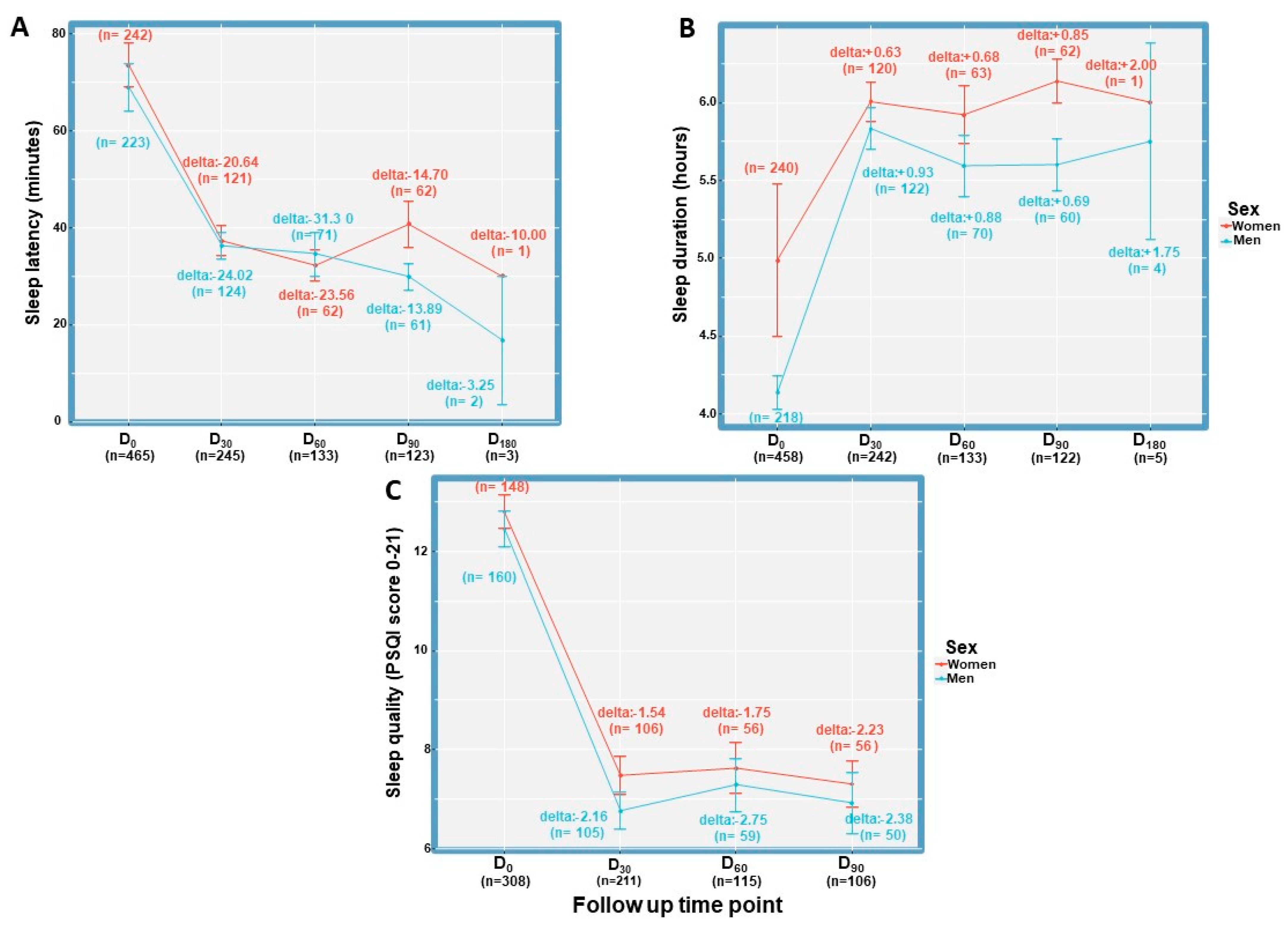
Evaluation of Sleep Latency, Duration and Quality
2.1.4. Treatment Safety
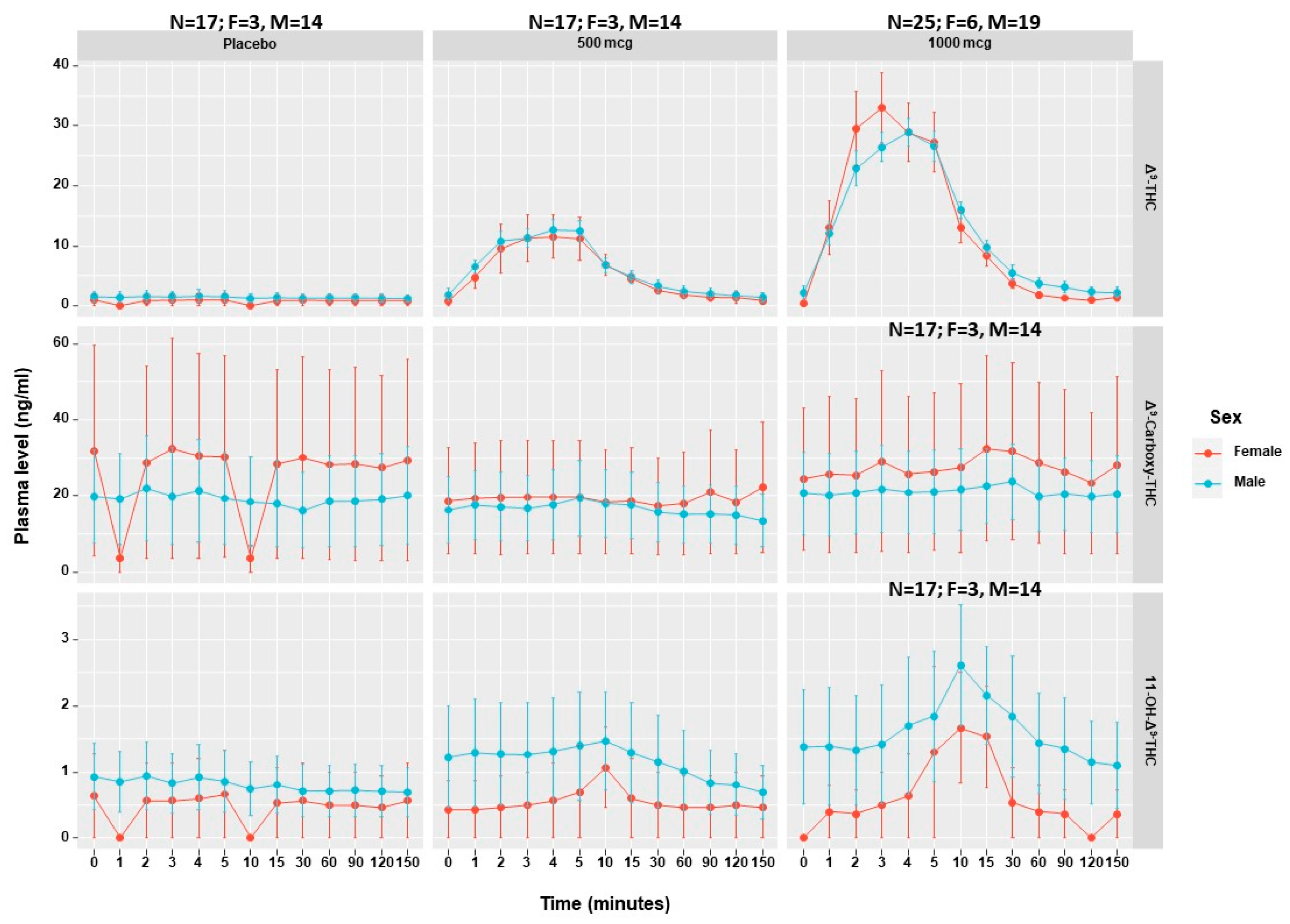
2.2. PK Studies
2.2.1. Description
2.2.2. Sample
2.2.3. PK Characteristics
2.2.4. Cardiovascular Measurements
2.2.5. Treatment Safety
3. Discussion
Limitations
4. Materials and Methods
4.1. General Considerations
4.2. Device
4.3. Cohort Study
4.3.1. Outcome Measures
4.3.2. Data Collection
4.4. PK Studies Design and Setting
4.5. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mauvais-Jarvis, F.; Berthold, H.K.; Campesi, I.; Carrero, J.J.; Dakal, S.; Franconi, F.; Gouni-Berthold, I.; Heiman, M.L.; Kautzky-Willer, A.; Klein, S.L.; et al. Sex-and gender-based pharmacological response to drugss. Pharmacol. Rev. 2021, 73, 730–762. [Google Scholar] [CrossRef] [PubMed]
- Gayà, T.F.; Ferrer, C.B.; Mas, A.J.; Seoane-Mato, D.; Reyes, F.Á.; Sánchez, M.D.; Dubois, C.M.; Sánchez-Fernández, S.A.; Vargas, L.M.R.; García Morales, P.V.; et al. Prevalence of fibromyalgia and associated factors in Spain. Clin. Exp. Rheumatol. 2020, 38, S47–S52. [Google Scholar]
- Sznitman, S.R. Trends in medical cannabis licensure, Israel, 2013–2018. Drug Alcohol Rev. 2020, 39, 763–767. [Google Scholar] [CrossRef] [PubMed]
- Landshaft, Y.; Albo, B.; Mechoulam, R.; Afek, A. The Updated Green Book (May 2019): The Official Guide to Clinical Care in Medical Cannabis (IMCP-GCP). Available online: https://www.health.gov.il/hozer/mmk154_2016.pdf (accessed on 8 June 2020).
- Tseng, A.H.; Harding, J.W.; Craft, R.M. Pharmacokinetic factors in sex differences in -tetrahydrocannabinol-induced behavioral effects in rats. Behav. Brain Res. 2004, 154, 77–83. [Google Scholar] [CrossRef]
- Aviram, J.; Lewitus, G.; Vysotski, Y.; Berman, P.; Shapira, A.; Procaccia, S.; Meiri, D. Sex Differences in Medical Cannabis Related Adverse effects. Pain 2021, 163, 975–983. [Google Scholar] [CrossRef]
- Di Marzo, V.; Piscitelli, F. The Endocannabinoid System and its Modulation by Phytocannabinoids. Neurotherapeutics 2015, 12, 692–698. [Google Scholar] [CrossRef]
- Bisogno, T.; Wenger, T.; Manzanares, J.; Milone, A.; Berrendero, F.; Di Marzo, V.; Ramos, J.A.; Ferna, J.J. Sex Steroid Influence on Cannabinoid CB 1 Receptor mRNA and Endocannabinoid Levels in the Anterior Pituitary Gland. Biochem. Biophys. Res. Commun. 2000, 270, 260–266. [Google Scholar] [CrossRef]
- Craft, R.M.; Haas, A.E.; Wiley, J.L.; Yu, Z.; Clowers, B.H.; Biochem, P.; Author, B. Gonadal hormone modulation of Δ-9-tetrahydrocannabinol-induced antinociception and metabolism in female versus male rats. Pharmacol. Biochem. Behav. 2017, 152, 36–43. [Google Scholar] [CrossRef]
- Farquhar, C.E.; Breivogel, C.S.; Gamage, T.F.; Gay, E.A.; Thomas, B.F.; Craft, R.M.; Wiley, J.L. Sex, THC, and hormones: Effects on density and sensitivity of CB1 cannabinoid receptors in rats. Drug Alcohol Depend. 2019, 194, 20–27. [Google Scholar] [CrossRef]
- Cooper, Z.D.; Haney, M. Sex-dependent effects of cannabis-induced analgesia. Drug Alcohol Depend. 2016, 167, 112–120. [Google Scholar] [CrossRef]
- Fogel, J.S.; Kelly, T.H.; Westgate, P.M.; Lile, J.A. Pharmacology, Biochemistry and Behavior Sex differences in the subjective effects of oral Δ-9-THC in cannabis users. Pharmacol. Biochem. Behav. 2017, 152, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Rademaker, M. Do Women Have More Adverse Drug Reactions? Am. J. Clin. Dermatol. 2001, 2, 349–351. [Google Scholar] [CrossRef] [PubMed]
- Bruni, N.; Della Pepa, C.; Oliaro-Bosso, S.; Pessione, E.; Gastaldi, D.; Dosio, F. Cannabinoid delivery systems for pain and inflammation treatment. Molecules 2018, 23, 2478. [Google Scholar] [CrossRef] [PubMed]
- Hodsoll, J.; Fusar-poli, P.; Strang, J.; Murray, R.M.; Freeman, T.P.; Mcguire, P. Does cannabidiol make cannabis safer? A randomised, double-blind, cross-over trial of cannabis with four different CBD:THC ratios. Neuropsychopharmacology 2022, 48, 869–876. [Google Scholar] [CrossRef]
- Almog, S.; Aharon-Peretz, J.; Vulfsons, S.; Ogintz, M.; Abalia, H.; Lupo, T.; Hayon, Y.; Eisenberg, E. The Pharmacokinetics, Efficacy, and Safety of a Novel Selective-Dose Cannabis Inhaler in Patients with Chronic Pain: A Randomized, Double-Blinded, Placebo-Controlled Trial. Eur. J. Pain. 2020, 24, 1505–1516. [Google Scholar] [CrossRef]
- Aviram, J.; Pud, D.; Gershoni, T.; Schiff Keren, B.; Ogintz, M.; Vulfsons, S.; Yashar, T.; Haim Moshe, A.; Brill, S.; Amital, H.; et al. Medical Cannabis Treatment for Chronic Pain: Outcomes and Prediction of Response. Eur. J. Pain. 2020, 25, 359–374. [Google Scholar] [CrossRef]
- Aviram, J.; Atzmony, D.; Eisenberg, E. Long-term effectiveness and safety of medical cannabis administered through the metered-dose Syqe Inhaler. Pain Rep. 2022, 7, e1011. [Google Scholar] [CrossRef]
- Eisenberg, E.; Ogintz, M.; Almog, S. The Pharmacokinetics, Efficacy, Safety, and Ease of Use of a Novel Portable Metered-Dose Cannabis Inhaler in Patients With Chronic Neuropathic Pain: A Phase 1a Study. J. Pain. Palliat. Care Pharmacother. 2014, 28, 216–225. [Google Scholar] [CrossRef]
- Mogil, J.S. Qualitative sex differences in pain processing: Emerging evidence of a biased literature. Nat. Rev. Neurosci. 2020, 21, 353–365. [Google Scholar] [CrossRef]
- Casale, R.; Atzeni, F.; Bazzichi, L.; Beretta, G.; Costantini, E.; Sacerdote, P.; Tassorelli, C. Pain in Women: A Perspective Review on a Relevant Clinical Issue that Deserves Prioritization. Pain Ther. 2021, 10, 287–314. [Google Scholar] [CrossRef]
- Sorge, R.E.; Mapplebeck, J.C.; Rosen, S.; Beggs, S.; Taves, S.; Alexander, J.K.; Martin, L.J.; Austin, J.-S.; Sotocinal, S.G.; Chen, D.; et al. Different immune cells mediate mechanical pain hypersensitivity in male and female mice. Nat. Neurosci. 2015, 18, 1081–1083. [Google Scholar] [CrossRef] [PubMed]
- Sorge, R.E.; Totsch, S.K. Sex Differences in Pain. J. Neurosci. Res. 2017, 95, 1271–1281. [Google Scholar] [CrossRef]
- Blanton, H.L.; Barnes, R.C.; McHann, M.C.; Bilbrey, J.A.; Wilkerson, J.L.; Guindon, J. Sex differences and the endocannabinoid system in pain. Pharmacol. Biochem. Behav. 2021, 202, 173107. [Google Scholar] [CrossRef]
- Ujváry, I.; Grotenhermen, F. 11-Nor-9-carboxy-∆9-tetrahydrocannabinol—A ubiquitous yet underresearched cannabinoid. A review of the literature. Cannabinoids 2014, 9, 1–8. [Google Scholar]
- Wall, M.E.; Pepez-Reyes, M. The Metabolism of Δ9-Tetrahydrocannabinol and Related Cannabinoids in Man. J. Clin. Pharmacol. 1981, 21, 178S–189S. [Google Scholar] [CrossRef]
- Huestis, M.A. Human Cannabinoid Pharmacokinetics. Chem. Biodivers. 2009, 4, 1770–1804. [Google Scholar] [CrossRef]
- Abuhasira, R.; Schleider, L.B.-L.; Mechoulam, R.; Novack, V. Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. Eur. J. Intern. Med. 2018, 49, 44–50. [Google Scholar] [CrossRef]
- Wallace, M.S.; Marcotte, T.D.; Atkinson, J.H.; Padovano, H.T.; Bonn-Miller, M. A Secondary Analysis from a Randomized Trial on the Effect of Plasma Tetrahydrocannabinol Levels on Pain Reduction in Painful Diabetic Peripheral Neuropathy. J. Pain 2020, 21, 1175–1186. [Google Scholar] [CrossRef]
- Gershoni, T.; Pud, D.; Aviram, J.; Eisenberg, E. Wellness of patients with chronic pain is not only about pain intensity. Pain Pract. 2022, 23, 145–154. [Google Scholar] [CrossRef]
- Aviram, J.; Procaccia, S.; Vysotski, Y.; Meiri, D. Reply to Montmeat et al. Pain 2022, 163, e1217–e1221. [Google Scholar] [CrossRef]
- Olsson, F.; Erridge, S.; Tait, J.; Holvey, C.; Coomber, R.; Hoare, J.; Khan, S.; Weatherall, M.W.; Platt, M.; Rucker, J.J.; et al. An observational study of safety and clinical outcome measures across patient groups in the United Kingdom Medical Cannabis Registry. Expert Rev. Clin. Pharmacol. 2023, 16, 257–266. [Google Scholar] [CrossRef]
- Cuttler, C.; Mischley, L.; Sexton, M. Sex Differences in Cannabis Use and Effects: A Cross-Sectional Survey of Cannabis Users. Cannabis Cannabinoid Res. 2016, 1, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Landshaft, Y.; Albo, B.; Mechoulam, R.; Afek, A. The Green Book (2021 Edition), 3rd ed.; Israeli Medical Cannabis Agency: Jerusalem, Israel, 2021. [Google Scholar]
- Vulfsons, S.; Ognitz, M.; Bar Sela, G.; Raz Pasteur, A.; Eisenberg, E. Cannabis treatment in hospitalized patients using the SYQE inhaler: Results of a pilot open-label study. Palliat. Support. Care 2020, 18, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Aviram, J.; Atzmony, D.; Frenklakh, A.; Kroll, A.; Zaks, I.; Hazekamp, A. THC degradation does not impair the accuracy of THC doses aerosolized by the metered—Dose SyqeAir inhaler: A 24-month stability trial. J. Cannabis Res. 2022, 4, 55. [Google Scholar] [CrossRef] [PubMed]
- Shochat, T.; Tzischinsky, O.; Oksenberg, A.; Peled, R. Validation of the Pittsburgh Sleep Quality Index Hebrew translation (PSQI-H) in a sleep clinic sample. Isr. Med. Assoc. J. 2007, 9, 853–856. [Google Scholar]
- Heinzen, E.; Sinnwell, J.; Atkinson, E.; Gunderson, T.; Dougherty, G. Arsenal: An Arsenal of “R” Functions for Large-Scale Statistical Summaries, Version 3.3.0; CRAN: Vienna, Austria, 2019.
- Ströbel, A.; Haynes, A. R Package Atable: Create Tables for Reporting Clinical Trials, Version 0.1.5; Comprehensive R Archive Network (CRAN): Vienna, Austria, 2019.
- Wickham, H. Tidyverse: Easily Install and Load “Tidyverse” Packages, Version 1.3.0; Comprehensive R Archive Network (CRAN): Vienna, Austria, 2019.
- Bates, D.; Maechler, M.; Bolker, B.; Walker, S. lme4: Linear Mixed-Effects Models Using Eigen and S4, R Package Version 1.7; CRAN: Vienna, Austria, 2014; pp. 1–23.



| Women N = 607 | Men N = 513 | Overall N = 1120 | Statistic (p-Value) | |
|---|---|---|---|---|
| Mean ± SD | ||||
| BMI | 27.0 ± 10.5 | 27.0 ± 4.72 | 27.0 ± 8.3 | 0 (0.98) † |
| Age | 59.5 ± 19.2 | 60.7 ± 16.2 | 60.1 ± 17.9 | 1.14 (0.28) † |
| Previous cannabis use | ||||
| N (%) | ||||
| Completely cannabis naïve | 111 (18) | 97 (19) | 208 (19) | 1.39 (0.3) †† |
| Previous recreational use | 8 (1) | 3 (<1) | 11 (<1) | |
| Previous MC use | 317 (52) | 287 (56) | 604 (54) | |
| Previous use of inflorescence | 116 (19) | 144 (28) | 260 (23) | 12.52 (<0.001) †† |
| Previous use of oil | 271 (44) | 219 (43) | 490 (44) | 0.43 (0.51) †† |
| Previous edibles | 2 (<1) | 1 (<1) | 3 (<1) | NA |
| Previous RSO | 1 (<1) | 0 (<1) | 1 (<1) | NA |
| Previous Sativex | 2 (<1) | 4 (<1) | 6 (<1) | NA |
| Previous other | 3 (<1) | 3 (<1) | 6 (<1) | NA |
| Intention of using MC concomitantly with the MDI (Yes) | 92 (16) | 94 (20) | 186 (18) | 3.26 (0.2) †† |
| MDI and MC concomitant use whilst having previous MC experience (n = 604) | 83 (28) | 86 (32) | 169 (30) | 1.68 (0.43) †† |
| Mean ± SD | ||||
| MC dose gr/month | 19.6 ± 10.8 | 23.0 ± 13.1 | 21.2 ± 12.1 | 9.9 (<0.005) † |
| Previous MC use duration (months) | 17.13 ± 22.03 | 27.76 ± 34.44 | 22.3 ± 29.19 | 15.87 (<0.001) † |
| Adverse Events by SOC | Proportion of Women (CI 95%) N = 666 | Proportion of Men (CI 95%) N = 582 | Overall Proportion (CI 95%) N = 1248 | Wilson’s χ2 Test (p-Value) |
|---|---|---|---|---|
| Any (at least 1 AE) | 9.76 (7.73–12.25) | 10.31 (8.09–13.05) | 10.02 (8.47–11.81) | 0.05 (0.82) |
| Nervous System Disorders | 5.26 (3.8–7.22) | 6.01 (4.36–8.25) | 5.61 (4.46–7.03) | 0.21 (0.65) |
| Gastrointestinal Disorders | 3.15 (2.07–4.77) | 2.23 (1.31–3.78) | 2.72 (1.96–3.78) | 0.67 (0.41) |
| Psychiatric Disorders | 1.2 (0.61–2.35) | 2.06 (1.18–3.57) | 1.6 (1.04–2.46) | 0.96 (0.33) |
| Respiratory, Thoracic and Mediastinal Disorders | 1.95 (1.14–3.31) | 1.55 (0.82–2.91) | 1.76 (1.17–2.65) | 2.43 (0.12) |
| General Disorders and Administration Site Conditions | 2.1 (1.26–3.5) | 0.86 (0.37–2) | 1.52 (0.98–2.37) | 0.11 (0.74) |
| Cardiac Disorders | 0.45 (0.15–1.32) | 0.86 (0.37–2) | 0.64 (0.33–1.26) | 0.3 (0.58) |
| Musculoskeletal and Connective Tissue Disorders | 0 (0–0.57) | 0.17 (0.03–0.97) | 0.08 (0.01–0.45) | 0 (0.95) |
| Skin and Subcutaneous Tissue Disorders | 0 (0–0.57) | 0.17 (0.03–0.97) | 0.08 (0.01–0.45) | 0 (0.95) |
| Vascular Disorders | 0 (0–0.57) | 0.17 (0.03–0.97) | 0.08 (0.01–0.45) | 0 (0.95) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aviram, J.; Glezerman, M.; Hayam, E.; Belobrov, R.; Procaccia, S.; Meiri, D.; Eisenberg, E. Evaluating Sex Differences in Efficacy, Safety and Pharmacokinetics in Patients Treated with Cannabis by a Metered-Dose Inhaler. Pharmaceuticals 2023, 16, 1426. https://doi.org/10.3390/ph16101426
Aviram J, Glezerman M, Hayam E, Belobrov R, Procaccia S, Meiri D, Eisenberg E. Evaluating Sex Differences in Efficacy, Safety and Pharmacokinetics in Patients Treated with Cannabis by a Metered-Dose Inhaler. Pharmaceuticals. 2023; 16(10):1426. https://doi.org/10.3390/ph16101426
Chicago/Turabian StyleAviram, Joshua, Marek Glezerman, Eytan Hayam, Rostislav Belobrov, Shiri Procaccia, David Meiri, and Elon Eisenberg. 2023. "Evaluating Sex Differences in Efficacy, Safety and Pharmacokinetics in Patients Treated with Cannabis by a Metered-Dose Inhaler" Pharmaceuticals 16, no. 10: 1426. https://doi.org/10.3390/ph16101426
APA StyleAviram, J., Glezerman, M., Hayam, E., Belobrov, R., Procaccia, S., Meiri, D., & Eisenberg, E. (2023). Evaluating Sex Differences in Efficacy, Safety and Pharmacokinetics in Patients Treated with Cannabis by a Metered-Dose Inhaler. Pharmaceuticals, 16(10), 1426. https://doi.org/10.3390/ph16101426







