A Role for Neuropeptide S in Alcohol and Cocaine Seeking
Abstract
1. Introduction
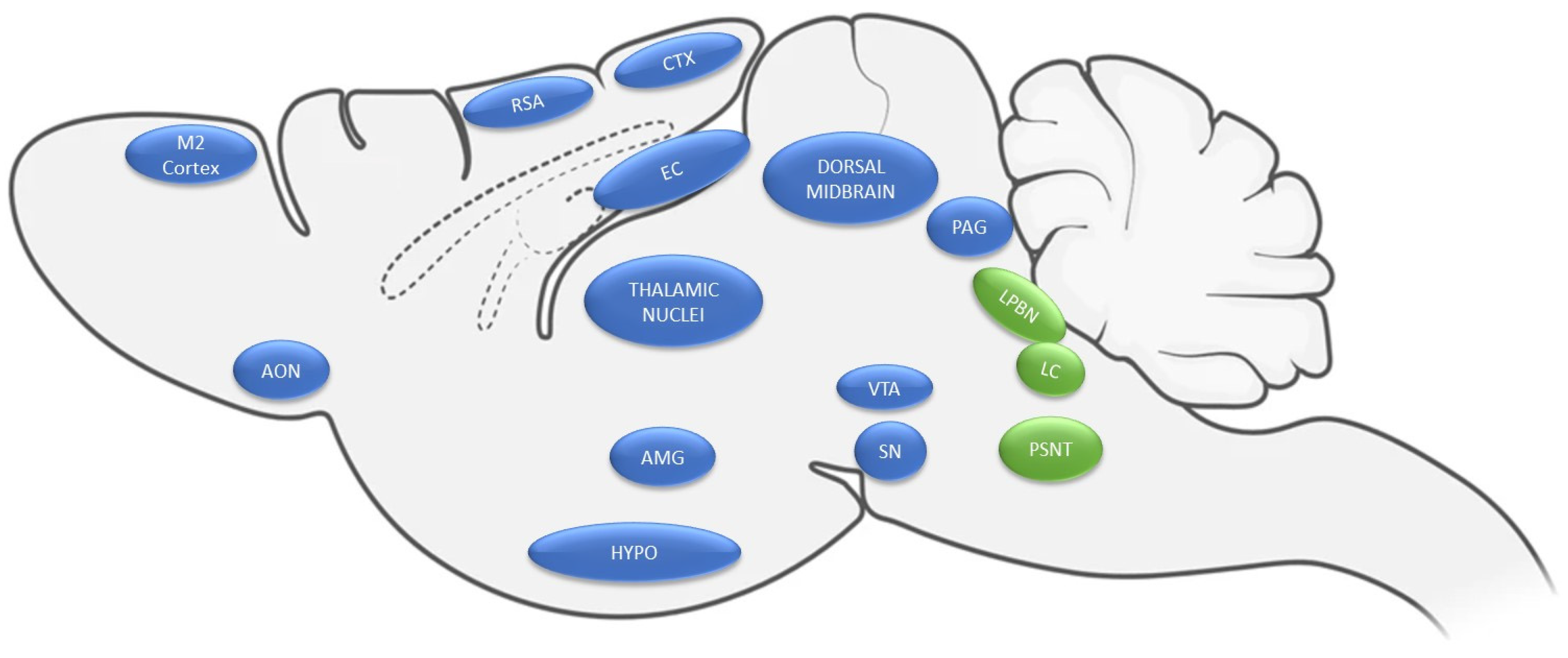
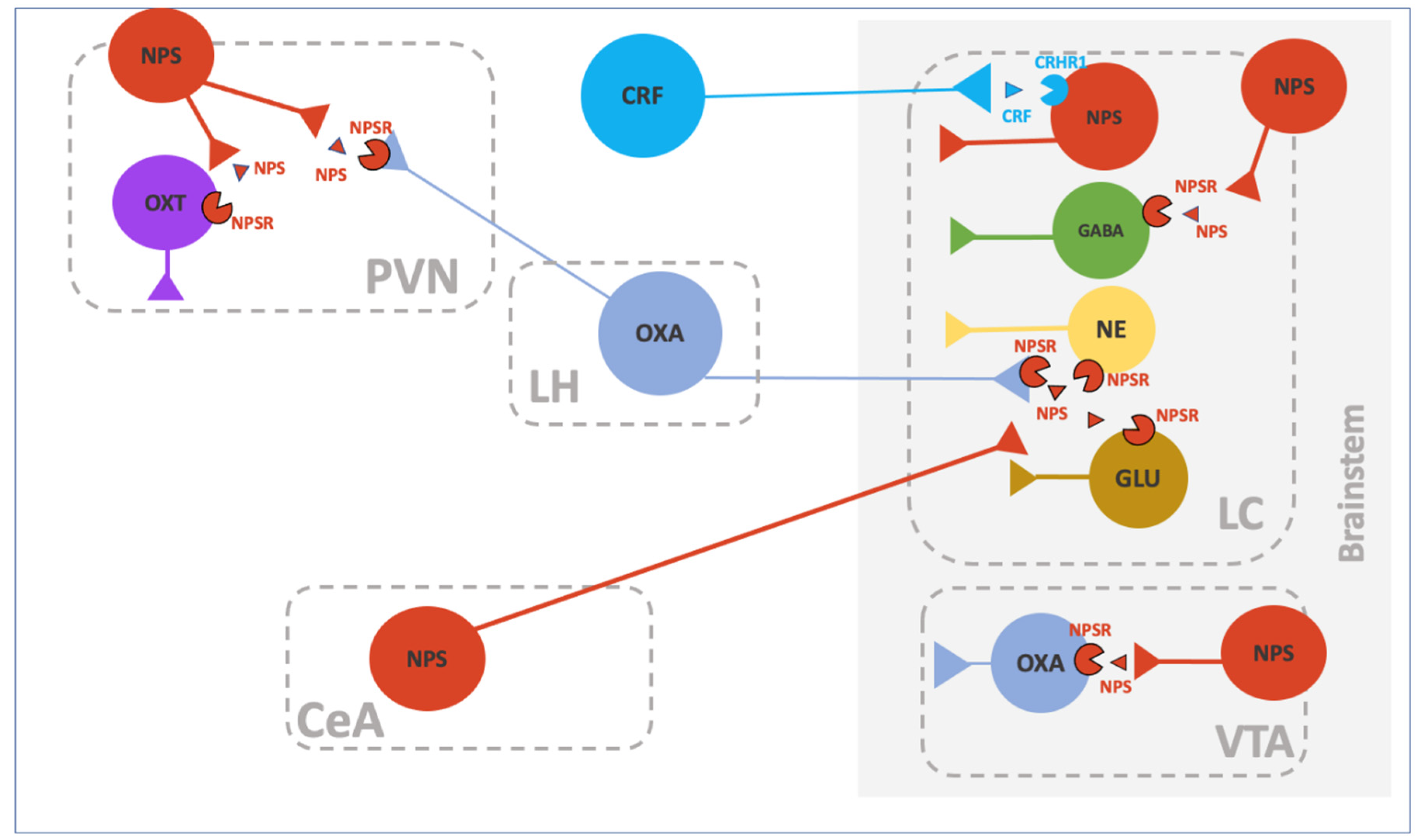
2. Neurobiology of NPS
3. Role of NPS in AUD
3.1. NPS on Alcohol Drinking and Operant Self-Administration
3.2. NPS on Reinstatement of Alcohol Seeking
4. NPS and Reward
5. Role of NPS in Cocaine Seeking
5.1. Role of the NPS System in Cocaine-Induced Reward
5.2. Role of the NPS System in the Reinstatement of Cocaine Seeking
6. Conclusive Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, X.; Zeng, J.; Zhou, A.; Theodorsson, E.; Fahrenkrug, J.; Reinscheid, R.K. Molecular fingerprint of neuropeptide S-producing neurons in the mouse brain. J. Comp. Neurol. 2011, 519, 1847–1866. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.L.; Gall, C.M.; Jackson, V.R.; Civelli, O.; Reinscheid, R.K. Distribution of neuropeptide S receptor mRNA and neurochemical characteristics of neuropeptide S-expressing neurons in the rat brain. J. Comp. Neurol. 2007, 500, 84–102. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.L.; Reinscheid, R.K.; Huitron-Resendiz, S.; Clark, S.D.; Wang, Z.; Lin, S.H.; Brucher, F.A.; Zeng, J.; Ly, N.K.; Henriksen, S.J.; et al. Neuropeptide S: A neuropeptide promoting arousal and anxiolytic-like effects. Neuron 2004, 43, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Rizzi, A.; Vergura, R.; Marzola, G.; Ruzza, C.; Guerrini, R.; Salvadori, S.; Regoli, D.; Calo, G. Neuropeptide S is a stimulatory anxiolytic agent: A behavioural study in mice. Br. J. Pharmacol. 2008, 154, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Donner, J.; Haapakoski, R.; Ezer, S.; Melen, E.; Pirkola, S.; Gratacos, M.; Zucchelli, M.; Anedda, F.; Johansson, L.E.; Soderhall, C.; et al. Assessment of the neuropeptide S system in anxiety disorders. Biol. Psychiatry 2010, 68, 474–483. [Google Scholar] [CrossRef]
- Zoicas, I.; Menon, R.; Neumann, I.D. Neuropeptide S reduces fear and avoidance of con-specifics induced by social fear conditioning and social defeat, respectively. Neuropharmacology 2016, 108, 284–291. [Google Scholar] [CrossRef]
- Jungling, K.; Seidenbecher, T.; Sosulina, L.; Lesting, J.; Sangha, S.; Clark, S.D.; Okamura, N.; Duangdao, D.M.; Xu, Y.L.; Reinscheid, R.K.; et al. Neuropeptide S-mediated control of fear expression and extinction: Role of intercalated GABAergic neurons in the amygdala. Neuron 2008, 59, 298–310. [Google Scholar] [CrossRef]
- Meis, S.; Bergado-Acosta, J.R.; Yanagawa, Y.; Obata, K.; Stork, O.; Munsch, T. Identification of a neuropeptide S responsive circuitry shaping amygdala activity via the endopiriform nucleus. PLoS ONE 2008, 3, e2695. [Google Scholar] [CrossRef]
- Reinscheid, R.K.; Xu, Y.L.; Okamura, N.; Zeng, J.; Chung, S.; Pai, R.; Wang, Z.; Civelli, O. Pharmacological characterization of human and murine neuropeptide s receptor variants. J. Pharmacol. Exp. Ther. 2005, 315, 1338–1345. [Google Scholar] [CrossRef]
- Raczka, K.A.; Gartmann, N.; Mechias, M.L.; Reif, A.; Buchel, C.; Deckert, J.; Kalisch, R. A neuropeptide S receptor variant associated with overinterpretation of fear reactions: A potential neurogenetic basis for catastrophizing. Mol. Psychiatry 2010, 15, 1067–1074. [Google Scholar] [CrossRef][Green Version]
- Okamura, N.; Hashimoto, K.; Iyo, M.; Shimizu, E.; Dempfle, A.; Friedel, S.; Reinscheid, R.K. Gender-specific association of a functional coding polymorphism in the Neuropeptide S receptor gene with panic disorder but not with schizophrenia or attention-deficit/hyperactivity disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry 2007, 31, 1444–1448. [Google Scholar] [CrossRef] [PubMed]
- Dannlowski, U.; Kugel, H.; Franke, F.; Stuhrmann, A.; Hohoff, C.; Zwanzger, P.; Lenzen, T.; Grotegerd, D.; Suslow, T.; Arolt, V.; et al. Neuropeptide-S (NPS) receptor genotype modulates basolateral amygdala responsiveness to aversive stimuli. Neuropsychopharmacology 2011, 36, 1879–1885. [Google Scholar] [CrossRef] [PubMed]
- Gechter, J.; Liebscher, C.; Geiger, M.J.; Wittmann, A.; Schlagenhauf, F.; Lueken, U.; Wittchen, H.U.; Pfleiderer, B.; Arolt, V.; Kircher, T.; et al. Association of NPSR1 gene variation and neural activity in patients with panic disorder and agoraphobia and healthy controls. Neuroimage Clin. 2019, 24, 102029. [Google Scholar] [CrossRef] [PubMed]
- Domschke, K.; Reif, A.; Weber, H.; Richter, J.; Hohoff, C.; Ohrmann, P.; Pedersen, A.; Bauer, J.; Suslow, T.; Kugel, H.; et al. Neuropeptide S receptor gene—converging evidence for a role in panic disorder. Mol. Psychiatry 2011, 16, 938–948. [Google Scholar] [CrossRef] [PubMed]
- Fedeli, A.; Braconi, S.; Economidou, D.; Cannella, N.; Kallupi, M.; Guerrini, R.; Calo, G.; Cifani, C.; Massi, M.; Ciccocioppo, R. The paraventricular nucleus of the hypothalamus is a neuroanatomical substrate for the inhibition of palatable food intake by neuropeptide S. Eur. J. Neurosci. 2009, 30, 1594–1602. [Google Scholar] [CrossRef]
- Botticelli, L.; Micioni Di Bonaventura, E.; Ubaldi, M.; Ciccocioppo, R.; Cifani, C.; Micioni Di Bonaventura, M.V. The Neural Network of Neuropeptide S (NPS): Implications in Food Intake and Gastrointestinal Functions. Pharmaceuticals 2021, 14, 293. [Google Scholar] [CrossRef]
- Smith, K.L.; Patterson, M.; Dhillo, W.S.; Patel, S.R.; Semjonous, N.M.; Gardiner, J.V.; Ghatei, M.A.; Bloom, S.R. Neuropeptide S stimulates the hypothalamo-pituitary-adrenal axis and inhibits food intake. Endocrinology 2006, 147, 3510–3518. [Google Scholar] [CrossRef]
- Ubaldi, M.; Giordano, A.; Severi, I.; Li, H.; Kallupi, M.; de Guglielmo, G.; Ruggeri, B.; Stopponi, S.; Ciccocioppo, R.; Cannella, N. Activation of Hypocretin-1/Orexin-A Neurons Projecting to the Bed Nucleus of the Stria Terminalis and Paraventricular Nucleus Is Critical for Reinstatement of Alcohol Seeking by Neuropeptide S. Biol. Psychiatry 2016, 79, 452–462. [Google Scholar] [CrossRef]
- Cannella, N.; Economidou, D.; Kallupi, M.; Stopponi, S.; Heilig, M.; Massi, M.; Ciccocioppo, R. Persistent increase of alcohol-seeking evoked by neuropeptide S: An effect mediated by the hypothalamic hypocretin system. Neuropsychopharmacology 2009, 34, 2125–2134. [Google Scholar] [CrossRef]
- Kallupi, M.; Cannella, N.; Economidou, D.; Ubaldi, M.; Ruggeri, B.; Weiss, F.; Massi, M.; Marugan, J.; Heilig, M.; Bonnavion, P.; et al. Neuropeptide S facilitates cue-induced relapse to cocaine seeking through activation of the hypothalamic hypocretin system. Proc. Natl. Acad. Sci. USA 2010, 107, 19567–19572. [Google Scholar] [CrossRef]
- Zhao, P.; Shao, Y.F.; Zhang, M.; Fan, K.; Kong, X.P.; Wang, R.; Hou, Y.P. Neuropeptide S promotes wakefulness through activation of the posterior hypothalamic histaminergic and orexinergic neurons. Neuroscience 2012, 207, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Paneda, C.; Huitron-Resendiz, S.; Frago, L.M.; Chowen, J.A.; Picetti, R.; de Lecea, L.; Roberts, A.J. Neuropeptide S reinstates cocaine-seeking behavior and increases locomotor activity through corticotropin-releasing factor receptor 1 in mice. J. Neurosci. 2009, 29, 4155–4161. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jungling, K.; Liu, X.; Lesting, J.; Coulon, P.; Sosulina, L.; Reinscheid, R.K.; Pape, H.C. Activation of neuropeptide S-expressing neurons in the locus coeruleus by corticotropin-releasing factor. J. Physiol. 2012, 590, 3701–3717. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.T.; Chiu, Y.T.; Chiu, Y.C.; Hor, C.C.; Lee, H.J.; Guerrini, R.; Calo, G.; Chiou, L.C. Neuropeptide S-initiated sequential cascade mediated by OX1, NK1, mGlu5 and CB1 receptors: A pivotal role in stress-induced analgesia. J. Biomed. Sci. 2020, 27, 7. [Google Scholar] [CrossRef] [PubMed]
- Jungling, K.; Lange, M.D.; Szkudlarek, H.J.; Lesting, J.; Erdmann, F.S.; Doengi, M.; Kugler, S.; Pape, H.C. Increased GABAergic Efficacy of Central Amygdala Projections to Neuropeptide S Neurons in the Brainstem During Fear Memory Retrieval. Neuropsychopharmacology 2015, 40, 2753–2763. [Google Scholar] [CrossRef]
- Domi, E.; Xu, L.; Toivainen, S.; Nordeman, A.; Gobbo, F.; Venniro, M.; Shaham, Y.; Messing, R.O.; Visser, E.; van den Oever, M.C.; et al. A neural substrate of compulsive alcohol use. Sci. Adv. 2021, 7, eabg9045. [Google Scholar] [CrossRef]
- Haubensak, W.; Kunwar, P.S.; Cai, H.; Ciocchi, S.; Wall, N.R.; Ponnusamy, R.; Biag, J.; Dong, H.W.; Deisseroth, K.; Callaway, E.M.; et al. Genetic dissection of an amygdala microcircuit that gates conditioned fear. Nature 2010, 468, 270–276. [Google Scholar] [CrossRef]
- Zhang, S.; Jin, X.; You, Z.; Wang, S.; Lim, G.; Yang, J.; McCabe, M.; Li, N.; Marota, J.; Chen, L.; et al. Persistent nociception induces anxiety-like behavior in rodents: Role of endogenous neuropeptide S. Pain 2014, 155, 1504–1515. [Google Scholar] [CrossRef]
- Jiang, J.H.; Peng, Y.L.; Zhang, P.J.; Xue, H.X.; He, Z.; Liang, X.Y.; Chang, M. The ventromedial hypothalamic nucleus plays an important role in anxiolytic-like effect of neuropeptide S. Neuropeptides 2018, 67, 36–44. [Google Scholar] [CrossRef]
- Chauveau, F.; Claverie, D.; Lardant, E.; Varin, C.; Hardy, E.; Walter, A.; Canini, F.; Rouach, N.; Rancillac, A. Neuropeptide S promotes wakefulness through the inhibition of sleep-promoting ventrolateral preoptic nucleus neurons. Sleep 2020, 43, zsz189. [Google Scholar] [CrossRef]
- Barchiesi, R.; Chanthongdee, K.; Domi, E.; Gobbo, F.; Coppola, A.; Asratian, A.; Toivainen, S.; Holm, L.; Augier, G.; Xu, L.; et al. Stress-induced escalation of alcohol self-administration, anxiety-like behavior, and elevated amygdala Avp expression in a susceptible subpopulation of rats. Addict. Biol. 2021, 26, e13009. [Google Scholar] [CrossRef] [PubMed]
- Grund, T.; Goyon, S.; Li, Y.; Eliava, M.; Liu, H.; Charlet, A.; Grinevich, V.; Neumann, I.D. Neuropeptide S Activates Paraventricular Oxytocin Neurons to Induce Anxiolysis. J. Neurosci. 2017, 37, 12214–12225. [Google Scholar] [CrossRef] [PubMed]
- Leonard, S.K.; Dwyer, J.M.; Sukoff Rizzo, S.J.; Platt, B.; Logue, S.F.; Neal, S.J.; Malberg, J.E.; Beyer, C.E.; Schechter, L.E.; Rosenzweig-Lipson, S.; et al. Pharmacology of neuropeptide S in mice: Therapeutic relevance to anxiety disorders. Psychopharmacology 2008, 197, 601–611. [Google Scholar] [CrossRef] [PubMed]
- Han, R.W.; Yin, X.Q.; Chang, M.; Peng, Y.L.; Li, W.; Wang, R. Neuropeptide S facilitates spatial memory and mitigates spatial memory impairment induced by N-methyl-D-aspartate receptor antagonist in mice. Neurosci. Lett. 2009, 455, 74–77. [Google Scholar] [CrossRef]
- Liu, X.; Si, W.; Garau, C.; Jungling, K.; Pape, H.C.; Schulz, S.; Reinscheid, R.K. Neuropeptide S precursor knockout mice display memory and arousal deficits. Eur. J. Neurosci. 2017, 46, 1689–1700. [Google Scholar] [CrossRef]
- Reinscheid, R.K. Phylogenetic appearance of neuropeptide S precursor proteins in tetrapods. Peptides 2007, 28, 830–837. [Google Scholar] [CrossRef]
- Laas, K.; Reif, A.; Akkermann, K.; Kiive, E.; Domschke, K.; Lesch, K.P.; Veidebaum, T.; Harro, J. Neuropeptide S receptor gene variant and environment: Contribution to alcohol use disorders and alcohol consumption. Addict. Biol. 2015, 20, 605–616. [Google Scholar] [CrossRef]
- Laas, K.; Reif, A.; Kiive, E.; Domschke, K.; Lesch, K.P.; Veidebaum, T.; Harro, J. A functional NPSR1 gene variant and environment shape personality and impulsive action: A longitudinal study. J. Psychopharmacol. 2014, 28, 227–236. [Google Scholar] [CrossRef]
- Fontenelle, L.F.; Oostermeijer, S.; Harrison, B.J.; Pantelis, C.; Yucel, M. Obsessive-compulsive disorder, impulse control disorders and drug addiction: Common features and potential treatments. Drugs 2011, 71, 827–840. [Google Scholar] [CrossRef]
- Laas, K.; Reif, A.; Akkermann, K.; Kiive, E.; Domschke, K.; Lesch, K.P.; Veidebaum, T.; Harro, J. Interaction of the neuropeptide S receptor gene Asn(1)(0)(7)Ile variant and environment: Contribution to affective and anxiety disorders, and suicidal behaviour. Int. J. Neuropsychopharmacol. Off. Sci. J. Coll. Int. Neuropsychopharmacol. 2014, 17, 541–552. [Google Scholar] [CrossRef]
- Clark, S.D.; Duangdao, D.M.; Schulz, S.; Zhang, L.; Liu, X.; Xu, Y.L.; Reinscheid, R.K. Anatomical characterization of the neuropeptide S system in the mouse brain by in situ hybridization and immunohistochemistry. J. Comp. Neurol. 2011, 519, 1867–1893. [Google Scholar] [CrossRef] [PubMed]
- Adori, C.; Barde, S.; Bogdanovic, N.; Uhlen, M.; Reinscheid, R.R.; Kovacs, G.G.; Hokfelt, T. Neuropeptide S- and Neuropeptide S receptor-expressing neuron populations in the human pons. Front. Neuroanat. 2015, 9, 126. [Google Scholar] [CrossRef] [PubMed]
- Leonard, S.K.; Ring, R.H. Immunohistochemical localization of the neuropeptide S receptor in the rat central nervous system. Neuroscience 2011, 172, 153–163. [Google Scholar] [CrossRef]
- Meis, S.; Stork, O.; Munsch, T. Neuropeptide S-mediated facilitation of synaptic transmission enforces subthreshold theta oscillations within the lateral amygdala. PLoS ONE 2011, 6, e18020. [Google Scholar] [CrossRef] [PubMed]
- Ren, W.; Kiritoshi, T.; Gregoire, S.; Ji, G.; Guerrini, R.; Calo, G.; Neugebauer, V. Neuropeptide S: A novel regulator of pain-related amygdala plasticity and behaviors. J. Neurophysiol. 2013, 110, 1765–1781. [Google Scholar] [CrossRef][Green Version]
- Ionescu, I.A.; Dine, J.; Yen, Y.C.; Buell, D.R.; Herrmann, L.; Holsboer, F.; Eder, M.; Landgraf, R.; Schmidt, U. Intranasally administered neuropeptide S (NPS) exerts anxiolytic effects following internalization into NPS receptor-expressing neurons. Neuropsychopharmacology 2012, 37, 1323–1337. [Google Scholar] [CrossRef][Green Version]
- Dine, J.; Ionescu, I.A.; Stepan, J.; Yen, Y.C.; Holsboer, F.; Landgraf, R.; Eder, M.; Schmidt, U. Identification of a role for the ventral hippocampus in neuropeptide S-elicited anxiolysis. PLoS ONE 2013, 8, e60219. [Google Scholar] [CrossRef]
- Bulbul, M.; Sinen, O.; Ozkan, A.; Aslan, M.A.; Agar, A. Central neuropeptide-S treatment improves neurofunctions of 6-OHDA-induced Parkinsonian rats. Exp. Neurol. 2019, 317, 78–86. [Google Scholar] [CrossRef]
- Mochizuki, T.; Kim, J.; Sasaki, K. Microinjection of neuropeptide S into the rat ventral tegmental area induces hyperactivity and increases extracellular levels of dopamine metabolites in the nucleus accumbens shell. Peptides 2010, 31, 926–931. [Google Scholar] [CrossRef]
- Si, W.; Aluisio, L.; Okamura, N.; Clark, S.D.; Fraser, I.; Sutton, S.W.; Bonaventure, P.; Reinscheid, R.K. Neuropeptide S stimulates dopaminergic neurotransmission in the medial prefrontal cortex. J. Neurochem. 2010, 115, 475–482. [Google Scholar] [CrossRef]
- Raiteri, L.; Luccini, E.; Romei, C.; Salvadori, S.; Calo, G. Neuropeptide S selectively inhibits the release of 5-HT and noradrenaline from mouse frontal cortex nerve endings. Br. J. Pharmacol. 2009, 157, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Li, M.S.; Peng, Y.L.; Jiang, J.H.; Xue, H.X.; Wang, P.; Zhang, P.J.; Han, R.W.; Chang, M.; Wang, R. Neuropeptide S Increases locomotion activity through corticotropin-releasing factor receptor 1 in substantia nigra of mice. Peptides 2015, 71, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Didonet, J.J.; Cavalcante, J.C.; Souza, L.d.S.; Costa, M.S.; Andre, E.; Soares-Rachetti, V.d.P.; Guerrini, R.; Calo, G.; Gavioli, E.C. Neuropeptide S counteracts 6-OHDA-induced motor deficits in mice. Behav. Brain Res. 2014, 266, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Gao, Y.H.; Chang, M.; Peng, Y.L.; Yao, J.; Han, R.W.; Wang, R. Neuropeptide S inhibits the acquisition and the expression of conditioned place preference to morphine in mice. Peptides 2009, 30, 234–240. [Google Scholar] [CrossRef]
- Enquist, J.; Ferwerda, M.; Madhavan, A.; Hok, D.; Whistler, J.L. Chronic ethanol potentiates the effect of neuropeptide s in the basolateral amygdala and shows increased anxiolytic and anti-depressive effects. Neuropsychopharmacology 2012, 37, 2436–2445. [Google Scholar] [CrossRef]
- Cannella, N.; Kallupi, M.; Ruggeri, B.; Ciccocioppo, R.; Ubaldi, M. The role of the neuropeptide S system in addiction: Focus on its interaction with the CRF and hypocretin/orexin neurotransmission. Prog. Neurobiol. 2013, 100, 48–59. [Google Scholar] [CrossRef]
- Cao, J.; de Lecea, L.; Ikemoto, S. Intraventricular administration of neuropeptide S has reward-like effects. Eur. J. Pharmacol. 2011, 658, 16–21. [Google Scholar] [CrossRef]
- Han, R.W.; Zhang, R.S.; Xu, H.J.; Chang, M.; Peng, Y.L.; Wang, R. Neuropeptide S enhances memory and mitigates memory impairment induced by MK801, scopolamine or Abeta(1)(-)(4)(2) in mice novel object and object location recognition tasks. Neuropharmacology 2013, 70, 261–267. [Google Scholar] [CrossRef]
- Gardella, E.; Romei, C.; Cavallero, A.; Trapella, C.; Fedele, E.; Raiteri, L. Neuropeptide S inhibits release of 5-HT and glycine in mouse amygdala and frontal/prefrontal cortex through activation of the neuropeptide S receptor. Neurochem. Int. 2013, 62, 360–366. [Google Scholar] [CrossRef]
- Okamura, N.; Garau, C.; Duangdao, D.M.; Clark, S.D.; Jungling, K.; Pape, H.C.; Reinscheid, R.K. Neuropeptide S enhances memory during the consolidation phase and interacts with noradrenergic systems in the brain. Neuropsychopharmacology 2011, 36, 744–752. [Google Scholar] [CrossRef]
- Han, R.W.; Xu, H.J.; Zhang, R.S.; Wang, P.; Chang, M.; Peng, Y.L.; Deng, K.Y.; Wang, R. Neuropeptide S interacts with the basolateral amygdala noradrenergic system in facilitating object recognition memory consolidation. Neurobiol. Learn. Mem. 2014, 107, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Ensho, T.; Nakahara, K.; Suzuki, Y.; Murakami, N. Neuropeptide S increases motor activity and thermogenesis in the rat through sympathetic activation. Neuropeptides 2017, 65, 21–27. [Google Scholar] [CrossRef]
- Niimi, M. Centrally administered neuropeptide S activates orexin-containing neurons in the hypothalamus and stimulates feeding in rats. Endocrine 2006, 30, 75–79. [Google Scholar] [CrossRef]
- Grant, B.F.; Stinson, F.S.; Dawson, D.A.; Chou, S.P.; Dufour, M.C.; Compton, W.; Pickering, R.P.; Kaplan, K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry 2004, 61, 807–816. [Google Scholar] [CrossRef]
- Ersche, K.D.; Turton, A.J.; Pradhan, S.; Bullmore, E.T.; Robbins, T.W. Drug addiction endophenotypes: Impulsive versus sensation-seeking personality traits. Biol. Psychiatry 2010, 68, 770–773. [Google Scholar] [CrossRef] [PubMed]
- von Diemen, L.; Bassani, D.G.; Fuchs, S.C.; Szobot, C.M.; Pechansky, F. Impulsivity, age of first alcohol use and substance use disorders among male adolescents: A population based case-control study. Addiction 2008, 103, 1198–1205. [Google Scholar] [CrossRef]
- Badia-Elder, N.E.; Henderson, A.N.; Bertholomey, M.L.; Dodge, N.C.; Stewart, R.B. The effects of neuropeptide S on ethanol drinking and other related behaviors in alcohol-preferring and -nonpreferring rats. Alcohol Clin. Exp. Res. 2008, 32, 1380–1387. [Google Scholar] [CrossRef]
- Cannella, N.; Kallupi, M.; Li, H.W.; Stopponi, S.; Cifani, C.; Ciccocioppo, R.; Ubaldi, M. Neuropeptide S differently modulates alcohol-related behaviors in alcohol-preferring and non-preferring rats. Psychopharmacology 2016, 233, 2915–2924. [Google Scholar] [CrossRef]
- Cifani, C.; Micioni Di Bonaventura, M.V.; Cannella, N.; Fedeli, A.; Guerrini, R.; Calo, G.; Ciccocioppo, R.; Ubaldi, M. Effect of neuropeptide S receptor antagonists and partial agonists on palatable food consumption in the rat. Peptides 2011, 32, 44–50. [Google Scholar] [CrossRef]
- Beck, B.; Fernette, B.; Stricker-Krongrad, A. Peptide S is a novel potent inhibitor of voluntary and fast-induced food intake in rats. Biochem. Biophys. Res. Commun. 2005, 332, 859–865. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; Economidou, D.; Cippitelli, A.; Cucculelli, M.; Ubaldi, M.; Soverchia, L.; Lourdusamy, A.; Massi, M. Genetically selected Marchigian Sardinian alcohol-preferring (msP) rats: An animal model to study the neurobiology of alcoholism. Addict. Biol. 2006, 11, 339–355. [Google Scholar] [CrossRef] [PubMed]
- Dine, J.; Ionescu, I.A.; Avrabos, C.; Yen, Y.C.; Holsboer, F.; Landgraf, R.; Schmidt, U.; Eder, M. Intranasally applied neuropeptide S shifts a high-anxiety electrophysiological endophenotype in the ventral hippocampus towards a “normal”-anxiety one. PLoS ONE 2015, 10, e0120272. [Google Scholar] [CrossRef] [PubMed]
- Lukas, M.; Neumann, I.D. Nasal application of neuropeptide S reduces anxiety and prolongs memory in rats: Social versus non-social effects. Neuropharmacology 2012, 62, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Vitale, G.; Filaferro, M.; Ruggieri, V.; Pennella, S.; Frigeri, C.; Rizzi, A.; Guerrini, R.; Calo, G. Anxiolytic-like effect of neuropeptide S in the rat defensive burying. Peptides 2008, 29, 2286–2291. [Google Scholar] [CrossRef]
- Wegener, G.; Finger, B.C.; Elfving, B.; Keller, K.; Liebenberg, N.; Fischer, C.W.; Singewald, N.; Slattery, D.A.; Neumann, I.D.; Mathe, A.A. Neuropeptide S alters anxiety, but not depression-like behaviour in Flinders Sensitive Line rats: A genetic animal model of depression. Int. J. Neuropsychopharmacol. Off. Sci. J. Coll. Int. Neuropsychopharmacol. 2012, 15, 375–387. [Google Scholar] [CrossRef]
- Borruto, A.M.; Stopponi, S.; Li, H.; Weiss, F.; Roberto, M.; Ciccocioppo, R. Genetically selected alcohol-preferring msP rats to study alcohol use disorder: Anything lost in translation? Neuropharmacology 2021, 186, 108446. [Google Scholar] [CrossRef]
- Stewart, R.B.; Gatto, G.J.; Lumeng, L.; Li, T.K.; Murphy, J.M. Comparison of alcohol-preferring (P) and nonpreferring (NP) rats on tests of anxiety and for the anxiolytic effects of ethanol. Alcohol 1993, 10, 1–10. [Google Scholar] [CrossRef]
- Domi, A.; Stopponi, S.; Domi, E.; Ciccocioppo, R.; Cannella, N. Sub-dimensions of Alcohol Use Disorder in Alcohol Preferring and Non-preferring Rats, a Comparative Study. Front. Behav. Neurosci. 2019, 13, 3. [Google Scholar] [CrossRef]
- Bokstrom, K.; Balldin, J.; Langstrom, G. Individual mood profiles in alcohol withdrawal. Alcohol Clin. Exp. Res. 1991, 15, 508–513. [Google Scholar] [CrossRef]
- Roelofs, S.M. Hyperventilation, anxiety, craving for alcohol: A subacute alcohol withdrawal syndrome. Alcohol 1985, 2, 501–505. [Google Scholar] [CrossRef]
- Ruggeri, B.; Braconi, S.; Cannella, N.; Kallupi, M.; Soverchia, L.; Ciccocioppo, R.; Ubaldi, M. Neuropeptide S receptor gene expression in alcohol withdrawal and protracted abstinence in postdependent rats. Alcohol Clin. Exp. Res. 2010, 34, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Gehlert, D.R.; Cippitelli, A.; Thorsell, A.; Le, A.D.; Hipskind, P.A.; Hamdouchi, C.; Lu, J.; Hembre, E.J.; Cramer, J.; Song, M.; et al. 3-(4-Chloro-2-morpholin-4-yl-thiazol-5-yl)-8-(1-ethylpropyl)-2,6-dimethyl-imidazo [1,2-b]pyridazine: A novel brain-penetrant, orally available corticotropin-releasing factor receptor 1 antagonist with efficacy in animal models of alcoholism. J. Neurosci. 2007, 27, 2718–2726. [Google Scholar] [CrossRef] [PubMed]
- Economidou, D.; Hansson, A.C.; Weiss, F.; Terasmaa, A.; Sommer, W.H.; Cippitelli, A.; Fedeli, A.; Martin-Fardon, R.; Massi, M.; Ciccocioppo, R.; et al. Dysregulation of nociceptin/orphanin FQ activity in the amygdala is linked to excessive alcohol drinking in the rat. Biol. Psychiatry 2008, 64, 211–218. [Google Scholar] [CrossRef][Green Version]
- de Guglielmo, G.; Martin-Fardon, R.; Teshima, K.; Ciccocioppo, R.; Weiss, F. MT-7716, a potent NOP receptor agonist, preferentially reduces ethanol seeking and reinforcement in post-dependent rats. Addict. Biol. 2015, 20, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Bifone, A.; Gozzi, A.; Cippitelli, A.; Matzeu, A.; Domi, E.; Li, H.; Scuppa, G.; Cannella, N.; Ubaldi, M.; Weiss, F.; et al. phMRI, neurochemical and behavioral responses to psychostimulants distinguishing genetically selected alcohol-preferring from genetically heterogenous rats. Addict. Biol. 2019, 24, 981–993. [Google Scholar] [CrossRef] [PubMed]
- Slattery, D.A.; Naik, R.R.; Grund, T.; Yen, Y.C.; Sartori, S.B.; Fuchsl, A.; Finger, B.C.; Elfving, B.; Nordemann, U.; Guerrini, R.; et al. Selective breeding for high anxiety introduces a synonymous SNP that increases neuropeptide S receptor activity. J. Neurosci. 2015, 35, 4599–4613. [Google Scholar] [CrossRef]
- Thorsell, A.; Tapocik, J.D.; Liu, K.; Zook, M.; Bell, L.; Flanigan, M.; Patnaik, S.; Marugan, J.; Damadzic, R.; Dehdashti, S.J.; et al. A novel brain penetrant NPS receptor antagonist, NCGC00185684, blocks alcohol-induced ERK-phosphorylation in the central amygdala and decreases operant alcohol self-administration in rats. J. Neurosci. 2013, 33, 10132–10142. [Google Scholar] [CrossRef]
- O’Brien, C.P.; Childress, A.R.; Ehrman, R.; Robbins, S.J. Conditioning factors in drug abuse: Can they explain compulsion? J. Psychopharmacol. 1998, 12, 15–22. [Google Scholar] [CrossRef]
- Domi, E.; Domi, A.; Adermark, L.; Heilig, M.; Augier, E. Neurobiology of alcohol seeking behavior. J. Neurochem. 2021, 157, 1585–1614. [Google Scholar] [CrossRef]
- Moorman, D.E.; James, M.H.; Kilroy, E.A.; Aston-Jones, G. Orexin/hypocretin-1 receptor antagonism reduces ethanol self-administration and reinstatement selectively in highly-motivated rats. Brain Res. 2017, 1654, 34–42. [Google Scholar] [CrossRef]
- Lawrence, A.J.; Cowen, M.S.; Yang, H.J.; Chen, F.; Oldfield, B. The orexin system regulates alcohol-seeking in rats. Br. J. Pharmacol. 2006, 148, 752–759. [Google Scholar] [CrossRef] [PubMed]
- Schneider, E.R.; Rada, P.; Darby, R.D.; Leibowitz, S.F.; Hoebel, B.G. Orexigenic peptides and alcohol intake: Differential effects of orexin, galanin, and ghrelin. Alcohol Clin. Exp. Res. 2007, 31, 1858–1865. [Google Scholar] [CrossRef]
- Srinivasan, S.; Simms, J.A.; Nielsen, C.K.; Lieske, S.P.; Bito-Onon, J.J.; Yi, H.; Hopf, F.W.; Bonci, A.; Bartlett, S.E. The dual orexin/hypocretin receptor antagonist, almorexant, in the ventral tegmental area attenuates ethanol self-administration. PLoS ONE 2012, 7, e44726. [Google Scholar] [CrossRef]
- Domi, E.; Xu, L.; Patz, M.; Nordeman, A.; Augier, G.; Holm, L.; Toivainen, S.; Augier, E.; Hansson, A.C.; Heilig, M. Nicotine increases alcohol self-administration in male rats via a mu-opioid mechanism within the mesolimbic pathway. Br. J. Pharmacol. 2020, 177, 4516–4531. [Google Scholar] [CrossRef] [PubMed]
- Domi, A.; Barbier, E.; Adermark, L.; Domi, E. Targeting the Opioid Receptors: A Promising Therapeutic Avenue for Treatment in “Heavy Drinking Smokers”. Alcohol Alcohol. 2021, 56, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Okamura, N.; Habay, S.A.; Zeng, J.; Chamberlin, A.R.; Reinscheid, R.K. Synthesis and pharmacological in vitro and in vivo profile of 3-oxo-1,1-diphenyl-tetrahydro-oxazolo[3,4-a]pyrazine-7-carboxylic acid 4-fluoro-benzylamide (SHA 68), a selective antagonist of the neuropeptide S receptor. J. Pharmacol. Exp. Ther. 2008, 325, 893–901. [Google Scholar] [CrossRef]
- Kallupi, M.; de Guglielmo, G.; Cannella, N.; Li, H.W.; Calo, G.; Guerrini, R.; Ubaldi, M.; Renger, J.J.; Uebele, V.N.; Ciccocioppo, R. Hypothalamic neuropeptide S receptor blockade decreases discriminative cue-induced reinstatement of cocaine seeking in the rat. Psychopharmacology 2013, 226, 347–355. [Google Scholar] [CrossRef]
- Melamed, J.Y.; Zartman, A.E.; Kett, N.R.; Gotter, A.L.; Uebele, V.N.; Reiss, D.R.; Condra, C.L.; Fandozzi, C.; Lubbers, L.S.; Rowe, B.A.; et al. Synthesis and evaluation of a new series of Neuropeptide S receptor antagonists. Bioorg. Med. Chem. Lett. 2010, 20, 4700–4703. [Google Scholar] [CrossRef]
- Zhang, Y.; Gilmour, B.P.; Navarro, H.A.; Runyon, S.P. Identifying structural features on 1,1-diphenyl-hexahydro-oxazolo[3,4-a]pyrazin-3-ones critical for Neuropeptide S antagonist activity. Bioorg. Med. Chem. Lett. 2008, 18, 4064–4067. [Google Scholar] [CrossRef][Green Version]
- Schmoutz, C.D.; Zhang, Y.; Runyon, S.P.; Goeders, N.E. Antagonism of the neuropeptide S receptor with RTI-118 decreases cocaine self-administration and cocaine-seeking behavior in rats. Pharmacol. Biochem. Behav. 2012, 103, 332–337. [Google Scholar] [CrossRef]
- Bonano, J.S.; Runyon, S.P.; Hassler, C.; Glennon, R.A.; Stevens Negus, S. Effects of the neuropeptide S receptor antagonist RTI-118 on abuse-related facilitation of intracranial self-stimulation produced by cocaine and methylenedioxypyrovalerone (MDPV) in rats. Eur. J. Pharmacol. 2014, 743, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Chou, Y.H.; Hor, C.C.; Lee, M.T.; Lee, H.J.; Guerrini, R.; Calo, G.; Chiou, L.C. Stress induces reinstatement of extinguished cocaine conditioned place preference by a sequential signaling via neuropeptide S, orexin, and endocannabinoid. Addict. Biol. 2021, 26, e12971. [Google Scholar] [CrossRef] [PubMed]
- Tung, L.W.; Lu, G.L.; Lee, Y.H.; Yu, L.; Lee, H.J.; Leishman, E.; Bradshaw, H.; Hwang, L.L.; Hung, M.S.; Mackie, K.; et al. Orexins contribute to restraint stress-induced cocaine relapse by endocannabinoid-mediated disinhibition of dopaminergic neurons. Nat. Commun. 2016, 7, 12199. [Google Scholar] [CrossRef]
- Borgland, S.L.; Ungless, M.A.; Bonci, A. Convergent actions of orexin/hypocretin and CRF on dopamine neurons: Emerging players in addiction. Brain Res. 2010, 1314, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Winsky-Sommerer, R.; Yamanaka, A.; Diano, S.; Borok, E.; Roberts, A.J.; Sakurai, T.; Kilduff, T.S.; Horvath, T.L.; de Lecea, L. Interaction between the corticotropin-releasing factor system and hypocretins (orexins): A novel circuit mediating stress response. J. Neurosci. 2004, 24, 11439–11448. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, F.; Yamada, S.; Ueta, Y. Centrally administered orexin-A activates corticotropin-releasing factor-containing neurons in the hypothalamic paraventricular nucleus and central amygdaloid nucleus of rats: Possible involvement of central orexins on stress-activated central CRF neurons. Regul. Pept. 2004, 118, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Al-Barazanji, K.A.; Wilson, S.; Baker, J.; Jessop, D.S.; Harbuz, M.S. Central orexin-A activates hypothalamic-pituitary-adrenal axis and stimulates hypothalamic corticotropin releasing factor and arginine vasopressin neurones in conscious rats. J. Neuroendocrinol. 2001, 13, 421–424. [Google Scholar] [CrossRef]
- Korotkova, T.M.; Sergeeva, O.A.; Eriksson, K.S.; Haas, H.L.; Brown, R.E. Excitation of ventral tegmental area dopaminergic and nondopaminergic neurons by orexins/hypocretins. J. Neurosci. 2003, 23, 7–11. [Google Scholar] [CrossRef]
- Borgland, S.L.; Taha, S.A.; Sarti, F.; Fields, H.L.; Bonci, A. Orexin A in the VTA is critical for the induction of synaptic plasticity and behavioral sensitization to cocaine. Neuron 2006, 49, 589–601. [Google Scholar] [CrossRef]
- Korotkova, T.M.; Brown, R.E.; Sergeeva, O.A.; Ponomarenko, A.A.; Haas, H.L. Effects of arousal- and feeding-related neuropeptides on dopaminergic and GABAergic neurons in the ventral tegmental area of the rat. Eur. J. Neurosci. 2006, 23, 2677–2685. [Google Scholar] [CrossRef]
- Wang, B.; Shaham, Y.; Zitzman, D.; Azari, S.; Wise, R.A.; You, Z.B. Cocaine experience establishes control of midbrain glutamate and dopamine by corticotropin-releasing factor: A role in stress-induced relapse to drug seeking. J. Neurosci. 2005, 25, 5389–5396. [Google Scholar] [CrossRef] [PubMed]
- Narita, M.; Nagumo, Y.; Hashimoto, S.; Narita, M.; Khotib, J.; Miyatake, M.; Sakurai, T.; Yanagisawa, M.; Nakamachi, T.; Shioda, S.; et al. Direct involvement of orexinergic systems in the activation of the mesolimbic dopamine pathway and related behaviors induced by morphine. J. Neurosci. 2006, 26, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Narita, M.; Nagumo, Y.; Miyatake, M.; Ikegami, D.; Kurahashi, K.; Suzuki, T. Implication of protein kinase C in the orexin-induced elevation of extracellular dopamine levels and its rewarding effect. Eur. J. Neurosci. 2007, 25, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; You, Z.B.; Wise, R.A. Reinstatement of cocaine seeking by hypocretin (orexin) in the ventral tegmental area: Independence from the local corticotropin-releasing factor network. Biol. Psychiatry 2009, 65, 857–862. [Google Scholar] [CrossRef]
- Clark, S.D.; Kenakin, T.P.; Gertz, S.; Hassler, C.; Gay, E.A.; Langston, T.L.; Reinscheid, R.K.; Runyon, S.P. Identification of the first biased NPS receptor agonist that retains anxiolytic and memory promoting effects with reduced levels of locomotor stimulation. Neuropharmacology 2017, 118, 69–78. [Google Scholar] [CrossRef]
| Brain System | Animal | Sex | Route of Administration | Experimental Procedure | Effect | Ref. |
|---|---|---|---|---|---|---|
| DA system | Wistar rats | Male | Intra-VTA injection | In vivo microdyalisis | ↑ DA release in the Nac | [55] |
| Sprague Dawley rats | Male | Central injection (i.c.v.) | In vivo microdyalisis | ↑ DA release in the mPFC | [56] | |
| Swiss mice | N/A | Bath perfusion | Ex vivo synaptosomes | Little ↑ effects on evoked DA release in cortical synaptosomes | [57] | |
| Wistar rats/Swiss mice | Male | Central injection (i.c.v.) | cFOS immunodetection | ↑ cFOS expression in SNC DA neurons | [54,58] | |
| Wistar rats | Male | Central injection (i.c.v.) | In vivo microdyalisis | ↑ DA local release in the SNC of 6-OHDA treated rats | [54] | |
| 5-HT system | Swiss mice | N/A | Bath perfusion | Ex vivo synaptosomes | ↓ evoked 5-HT release in cortical and amygdaloidal synaptosomes | [57] |
| Sprague Dawley rats | Male | Central injection (i.c.v.) | In vivo microdyalisis | No effects on 5-HT in the mPFC | [56] | |
| NA system | Swiss mice | N/A | Bath perfusion | Ex vivo synaptosomes | Little effects on evoked DA release in cortical synaptosomes | [57] |
| Limbic system | C57BL/6J mice | N/A | Bath perfusion | Ex vivo patch-clamp recordings | ↑ glutamate release on mITC neurons and ↑ feedforward inhibition on CeA neurons | [15] |
| GAD67-GFP mice | N/A | Bath perfusion | Ex vivo patch-clamp recordings | ↑ feedforward inhibition on BLA principal neurons and ↑ excitation of EPN principal neurons | [16] | |
| Sprague Dawley rats | Male | Bath perfusion | Ex vivo patch-clamp recordings | No effects on evoked glutamate release and feedforward inhibition the CeA of control animals | [51] | |
| ↓ evoked glutamate release and ↑ feedforward inhibition in the CeA in a neuropathic pain model | ||||||
| C57BL/6N mice | Male | Bath perfusion/intranasal | Ex vivo field potential recordings | ↓ Paired pulse ratio and impaired LTP in CA3-CA1 synapses of the ventral hippocampus | [52,53] | |
| Hypothalamus and HPA axis | Long Evans, Sprague Dawley, Wistar rats | Male | Central injection (i.c.v.) | cFOS immunodetection | ↑ cFOS expression in LH, DMH and PeF Hcrt-1/Ox-A neurons | [25,27,28] |
| Sprague Dawley rats | Male | Central injection (i.c.v.) | cFOS immunodetection | ↑ cFOS expression in TMN histaminergic neurons | [28] | |
| C57BL/6J mice | Male | Bath perfusion | Ex vivo patch-clamp recordings | ↑ neuronal activity of non-galanin VLPO neurons | [37] | |
| ↓ neuronal activity of galanin VLPO neurons by ↑ GABA release | ||||||
| Wistar rats | Male | Bath perfusion | Ex vivo GCamp6 calcium signaling | ↑ OXT neuronal activity | [39] | |
| Central injection (i.c.v.) | In vivo microdyalisis | ↑ OXT local release | ||||
| Wistar rats | Male | Central injection (i.c.v.) | Plasma concentration | ↑ concentration ACTH and corticosterone | [24] | |
| Bath perfusion | Hypothalamic explants | ↑ CRF and vasopressin release from anterior pituitary segments, no effects on ACTH and NPY |
| Drug of Abuse | Strain | Drug | Route | Paradigm | Result | Ref. |
|---|---|---|---|---|---|---|
| Alcohol | P rats | NPS | i.c.v. | TBC | Reduced alcohol intake | [66] |
| Alcohol | Wistar rats | NPS | i.c.v. and LH | Cued reinstatement | Exacerbated seeking | [18] |
| Alcohol | Wistar rats | NPS | i.c.v. | Post-dependent alcohol withdrawal | Alleviated symptoms | [80] |
| Alcohol | Mice | NPS | i.c.v. | TBC | Reduced alcohol intake | [54] |
| Alcohol | Wistar rats | NPSR antagonist NCGC00185684 | i.p. | Fixed ratio self-administration | Decreased self-administration | [86] |
| Alcohol | Wistar rats | NPS | LH | Cued reinstatement | Exacerbated seeking | [17] |
| Alcohol | Wistar and msP rats | NPS | i.c.v. | Reinstatement of seeking and self-administration | Reinstated seeking in Wistars and reduced self-administration in msP | [67] |
| Cocaine | Wild-type and CRF1 KO mice | NPS | i.c.v. | Reinstatement of seeking | Reinstated seeking in wild-type but not CRF1KO mice | [21] |
| Cocaine | Long Evans rats | NPS | i.c.v. and LH | Cued reinstatement | Exacerbated seeking | [19] |
| Cocaine | Wistar rats | NPSR antagonist RTI118 | i.p. | Cued reinstatement of seeking and self-administration | Decreased both | [99] |
| Cocaine | Long Evans rats | NPSR antagonist NPSR-QA1 | i.p. | Cued reinstatement of seeking | Reduced seeking | [96] |
| NCT Number | Disease | Treatment | Phase |
|---|---|---|---|
| NCT03897062 | Alcohol Use Disorder | Suvorexant | 2 |
| NCT04229095 | Alcohol Use Disorder | Suvorexant | 2 |
| NCT04287062 | Opioid Use Disorder | Suvorexant | 2 |
| NCT04262193 | Opioid Use Disorder | Suvorexant | 2 |
| NCT03789214 | Opioid Use Disorder | Suvorexant | 2 |
| NCT05145764 | Opioid Use Disorder | Suvorexant | 2 |
| NCT04818086 | Opioid Use Disorder | Lemborexant | 1 and 2 |
| NCT02785406 | Cocaine Use Disorder | Suvorexant | 2 |
| NCT03937986 | Cocaine Use Disorder | Suvorexant | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannella, N.; Borruto, A.M.; Petrella, M.; Micioni Di Bonaventura, M.V.; Soverchia, L.; Cifani, C.; De Carlo, S.; Domi, E.; Ubaldi, M. A Role for Neuropeptide S in Alcohol and Cocaine Seeking. Pharmaceuticals 2022, 15, 800. https://doi.org/10.3390/ph15070800
Cannella N, Borruto AM, Petrella M, Micioni Di Bonaventura MV, Soverchia L, Cifani C, De Carlo S, Domi E, Ubaldi M. A Role for Neuropeptide S in Alcohol and Cocaine Seeking. Pharmaceuticals. 2022; 15(7):800. https://doi.org/10.3390/ph15070800
Chicago/Turabian StyleCannella, Nazzareno, Anna Maria Borruto, Michele Petrella, Maria Vittoria Micioni Di Bonaventura, Laura Soverchia, Carlo Cifani, Sara De Carlo, Esi Domi, and Massimo Ubaldi. 2022. "A Role for Neuropeptide S in Alcohol and Cocaine Seeking" Pharmaceuticals 15, no. 7: 800. https://doi.org/10.3390/ph15070800
APA StyleCannella, N., Borruto, A. M., Petrella, M., Micioni Di Bonaventura, M. V., Soverchia, L., Cifani, C., De Carlo, S., Domi, E., & Ubaldi, M. (2022). A Role for Neuropeptide S in Alcohol and Cocaine Seeking. Pharmaceuticals, 15(7), 800. https://doi.org/10.3390/ph15070800







