Abstract
Bacterial resistance mechanisms are continuously and rapidly evolving. This is particularly true for Gram-negative bacteria. Over the last decade, the strategy to develop new β-lactam/β-lactamase inhibitors (BLs/BLIs) combinations has paid off and results from phase 3 and real-world studies are becoming available for several compounds. Cefiderocol warrants a separate discussion for its peculiar mechanism of action. Considering the complexity of summarizing and integrating the emerging literature data of clinical outcomes, microbiological mechanisms, and pharmacokinetic/pharmacodynamic properties of the new BL/BLI and cefiderocol, we aimed to provide an overview of data on the following compounds: aztreonam/avibactam, cefepime/enmetazobactam, cefepime/taniborbactam, cefepime/zidebactam, cefiderocol, ceftaroline/avibactam, ceftolozane/tazobactam, ceftazidime/avibactam, imipenem/relebactam, meropenem/nacubactam and meropenem/vaborbactam. Each compound is described in a dedicated section by experts in infectious diseases, microbiology, and pharmacology, with tables providing at-a-glance information.
1. Introduction
The epidemiology of infections sustained by multidrug-resistant Gram-negative bacteria is rapidly evolving. New drugs are available or are on the horizon. Most are combinations of a β-lactam and a β-lactamase inhibitor. One part is the antibiotic cefiderocol that has a peculiar antibacterial mechanism of action. Dispensing of such an armamentarium requires in-depth knowledge of their microbiological spectrum of activity, pharmacokinetic/pharmacodynamic (PK/PD) properties, and clinical study results. Herein, we aimed to summarize the new antibacterial molecules in order to help clinicians in choosing the most appropriate drug according to the type of patient (e.g., obese, critically ill, nephropathic), the type of bacterium (e.g., non-fermenting Gram-negative), and the site of infection (e.g., pneumonia, skin and soft tissue, bloodstream infections). The following molecules are described: aztreonam/avibactam, cefepime/enmetazobactam, cefepime/taniborbactam, cefepime/zidebactam, cefiderocol, ceftaroline-fosamil/avibactam, ceftolozane/tazobactam, ceftazidime/avibactam, imipenem/relebactam, meropenem/nacubactam, and meropenem/vaborbactam (Figure 1).
2. Aztreonam/Avibactam
Aztreonam is an old antibiotic approved by the Food and Drug Administration (FDA) and the European regulatory authorities in 1986. Its clinical use was strongly limited by the spread of extended-spectrum β-lactamase (ESBL) and AmpC-type determinants. Of note, metallo-β-lactamases (MBLs) are able to hydrolyze all β-lactams except for the monobactam aztreonam. However, due to the frequent co-production of class A β-lactamases or AmpC-type determinants within MBL-producing Gram-negatives, aztreonam remains active only in one-third of cases [1]. For this reason, combining aztreonam with avibactam could represent a good antimicrobial strategy. A single product formulation of aztreonam/avibactam is currently under development in phase 3 studies for the treatment of MBL-sustained infections. Aztreonam/avibactam has antimicrobial activity against carbapenemase-producing Enterobacterales, P. aeruginosa (including isolates producing Klebsiella pneumoniae carbapenemase, KPC; Verona integron-encoded metallo-β-lactamase, VIM; imipenemase, IMP; New Delhi metallo-β-lactamase, NDM; and oxacillinase, OXA-48), and Stenotrophomonas maltophilia [2,3]. No antimicrobial activity has been reported against A. baumannii (no inhibition of A. baumannii OXA-type enzymes). Resistance in P. aeruginosa has been associated with impermeability (porin loss), the production of AmpC-type (Pseudomonas-derived cephalosporinase 1; PDC) variants, OXA enzymes (other than OXA-48), or hyperexpression of efflux systems, while resistance in Enterobacterales could be associated with a specific amino acid insertion (12 bp duplications) in PBP3 determinants causing a reduction in affinity for aztreonam [2] (Table 1). For antimicrobial susceptibility testing purpose, the concentration of avibactam is fixed at 4 mg/L [4]. No clinical breakpoint (CLSI, EUCAST, or FDA) has been approved for this combination. An EUCAST epidemiological cut-off (ECOFF) value has not been assigned.

Table 1.
Microbiological targets.
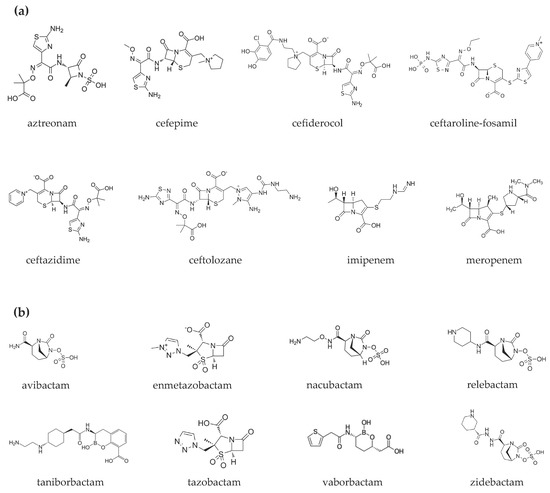
Figure 1.
Chemical structures of (a) β-lactams and (b) β-lactamase inhibitors.
Currently, seven clinical trials on aztreonam/avibactam are registered: five are completed and two are recruiting. The efficacy of the combination is being tested in patients with bloodstream infections (BSIs), complicated intra-abdominal infections (cIAIs), complicated urinary tract infections (cUTIs), hospital-acquired pneumonia (HAP), and ventilator-associated pneumonia (VAP). In contrast, aztreonam/avibactam safety is more generally being evaluated in patients with serious or complicated bacterial infections [5]. Recently, a phase 2 trial was published: 34 patients with cIAIs were treated for 5–14 days with aztreonam/avibactam + metronidazole. No patients had either ESBL or MBL-positive isolates. Patients were divided into three cohorts: (1) 500/137 mg, followed by 1500/410 mg every 6 h; (2) 500/167 mg, followed by 1500/500 mg every 6 h; and (3) extension of exposure at the higher dose regimen. The most common adverse events were hepatic enzyme increases (26%) and diarrhea (15%). Clinical cure rates at the test-of-cure visit were 59% overall [6]. Data from this study supported the regimen selected for the phase 3 trial (500/167 mg, followed by 1500/500 mg every 6 h) (Table 2).

Table 2.
Clinical settings investigated or under investigation for each compound.
In the recently published phase 2 clinical trial, aztreonam showed, in the first cohort, a geometric mean volume of distribution (Vd) of 20.0 L, 16.9% (geometric coefficient of variance) and a clearance (Cl) of 6.4 L/h (35.4%), while for avibactam, a Vd of 26.0 L (22.0%) and a Cl of 10.1 L/h (42.6%) was described. Similar data were obtained in the other two cohorts [6]. In patients with cIAI, avibactam’s Cl was lower, while avibactam and aztreonam Vd were higher than in healthy volunteers, as expected in critical patients, due to changes in protein levels, extracellular fluids, and blood volume [6], as already described for avibactam Vd in critical patients with comorbidities and burns [7]. Further PK studies on the combination have not yet been conducted, despite clinical experiences in various infections [2]. Studies on avibactam show that the drug diffuses into epithelial lung fluid (ELF) with concentrations around 30% of those in plasma [8,9]. Instead, the blood–brain barrier represents an obstacle to the diffusion [10] (Table 3 and Table 4).

Table 3.
Pharmacokinetic parameters of β-lactams/β-lactamase inhibitors and cefiderocol. The concentrations of β-lactams and β-lactamase inhibitors were determined using liquid chromatography–tandem mass spectrometry.

Table 4.
Recommended dosages and dose adjustment in renal insufficiency.
3. Cefepime/Enmetazobactam
Enmetazobactam is a new β-lactamase inhibitor similar in structure to tazobactam, with increased bacterial cell penetration and potency. Similar to tazobactam, enmetazobactam inhibits CTX-M, TEM, SHV, and other class A β-lactamases (except for KPC), but does not inhibit class B and D β-lactamases and carbapenemases. Enmetazobactam alone does not exhibit inhibitory activity against Gram-negative bacteria. The cefepime/enmetazobactam combination is active in vitro against ESBL- and AmpC-producing Enterobacterales and P. aeruginosa [51]. The in vivo efficacy of cefepime/enmetazobactam was demonstrated using a mouse model of septicemia, indicating the ability of enmetazobactam to significantly enhance the therapeutic efficacy of cefepime in vivo. This new combination represents a potential treatment alternative, contributing to “carbapenem sparing” strategies for infections caused by ESBL-producing Enterobacterales [52]. No antimicrobial activity was reported against A. baumannii and S. maltophilia [53] (Table 1). For antimicrobial susceptibility testing purpose, the concentration of enmetazobactam is fixed at 8 mg/L. No clinical breakpoint (CLSI, EUCAST, or FDA) has been approved for this combination. An EUCAST epidemiological cut-off (ECOFF) value has not been assigned [4].
From a clinical point of view, cefepime/enmetazobactam has been evaluated in two phase 1 (NCT03680352 and NCT03685084), one phase 2 (NCT03680612), and one phase 3 trial (NCT03687255) [54,55,56,57]. The recent ALLIUM trial compared cefepime/enmetazobactam (2/0.5 g every 8 h intravenously (i.v.)) to piperacillin-tazobactam (4.5 g every 8 h, i.v.) in patients with cUTIs, including acute pyelonephritis [56]. The baseline participants numbered 1034 (516 in the cefepime/enmetazobactam group and 518 in the piperacillin/tazobactam group). The proportion of patients in the microbiological modified intention-to-treat (m-MITT) population that achieved overall treatment success was 79% (n = 273) and 59% (n = 196) in the cefepime/enmetazobactam and piperacillin-tazobactam groups, respectively [55]. In addition, cefepime/enmetazobactam displayed a higher proportion of patients in the m-MITT population with clinical cure compared with piperacillin/tazobactam (92% vs. 89%), alongside a tolerable safety profile [56]. Of note, a higher rate of Clostridioides difficile infections was reported in the cefepime/enmetazobactam group (13% vs. 0%) [56] (Table 1).
The PK profile of enmetazobactam together with cefepime has been evaluated in a mouse septicemia model; in this model, the profile of enmetazobactam mirrors that of cefepime, and an fT > MIC of 40–60% for cefepime and the time above a free threshold drug concentration of 20% (fT > Ct) for enmetazobactam remain the PK/PD indices predictive of efficacy [14]. A clinical trial on the PK in ELF and tissue penetration has recently been completed. Healthy volunteers were treated with 2 g cefepime/1 g enmetazobactam every 8 h. At steady state, the area under the curve (AUC)(0–24) plasma/AUC(0–24) ELF ratio was 61% (± 29) for cefepime and 53% (±21) for enmetazobactam. The study shows that both drugs diffuse similarly in ELF, providing evidence for the potential role of the association with nosocomial pneumonia [15]. Two other studies on healthy volunteers [55] and on patients with renal insufficiency are ongoing [55,56] (Table 3 and Table 4).
4. Cefepime/Taniborbactam
Taniborbactam is a highly potent broad-spectrum boronate derivative β-lactamase inhibitor that acts as an irreversible, covalent inhibitor of serine β-lactamases and as a competitive inhibitor of MBLs. For this reason, taniborbactam presents a broad spectrum of activity, including all four Ambler classes of β-lactamase enzymes, especially the more clinically relevant B1 subclass of MBL (VIM- and NDM-type enzymes). It has excellent penetration of the outer membrane of Gram-negatives [58]. Taniborbactam combined with the cephalosporin cefepime lowered the MIC of cefepime against ESBL-, AmpC-, and carbapenemase-producing isolates. In contrast, isolates of blaNDM-5-producing E. coli were reported, presenting MIC values > 8 mg/L for cefepime/taniborbactam. In addition, penicillin-binding protein (PBP)3 mutations may be the main reason for higher MICs of the combination among NDM-producing E. coli [59]. The combination showed antimicrobial activity against S. maltophilia, but not against A. baumannii [60] (Table 1). For antimicrobial susceptibility testing purposes, the concentration of taniborbactam is fixed at 4 mg/L [4]. No clinical breakpoint (CLSI, EUCAST, or FDA) has been approved for this combination. An EUCAST epidemiological cut-off (ECOFF) value has not been assigned.
Currently no human studies on cefepime/taniborbactam have been published. However, in a recent study, Lasko et al. assessed the efficacy of the combination in a neutropenic murine cUTI model. The authors used dosing regimens resembling human exposure to 2/0.5 g every 8 h. Eighteen cefepime-resistant clinical isolates (ESBL, AmpC, KPC, OXA-48) were tested. Cefepime/taniborbactam exhibited robust killing of kidney bacteria (until MIC of 32 mg/l) [60]. Two trials are being conducted in humans: one is a study assessing safety in healthy subjects and the other is a phase 3, randomized, double-blind noninferiority study (currently recruiting) aimed at evaluating cefepime/taniborbactam vs. meropenem for the treatment of cUTI. The primary outcome is a composite of microbiological eradication and symptomatic clinical success at test-of-cure [61]. Results are not yet available (Table 2).
As mentioned above, preclinical studies show that cefepime and cefepime/taniborbactam concentration–time profiles are comparable in the murine model and in humans. In the neutropenic murine thigh infection model, Abdelraouf et al. showed that the best PK/PD index remains fT > MIC of 50% for the cephalosporin and the fAUC24/MIC for the β-lactamase inhibitor [17]. No human studies on the PKs of the combination cefepime/taniborbactam have been published and the results of the two trials currently ongoing have not been reported yet [61]. Dowell et al. have evaluated the safety and PKs of single and multiple doses of taniborbactam in human volunteers. The study shows that multiple doses (750 mg every 8 h) result in an AUC of 139.5 (±21.6) h * ng/mL, a Vd of 37.4 (±19.9) L, a half-life (t ½) of 4.7 (±15.4) h, and a renal Cl of 5.6 (±2.1) L/h [18]. The mean fraction of the drug excreted unchanged in urine was 92.4% (±10.2). Cefepime is also excreted unchanged in the urine [16], and the combination is being studied in cUTIs (Table 3 and Table 4).
5. Cefepime/Zidebactam
Zidebactam is a new-generation diazobicyclooctane-derived inhibitor (DBO), non-β-lactam antibiotic, with a dual mode of action involving selective, high-affinity binding of the PBP2 of Gram-negative bacteria and inhibition of β-lactamases. Due to PBP2 binding, zidebactam alone demonstrates antibacterial activity against various isolates of Enterobacterales and P. aeruginosa. It has been shown that the combination of cefepime/zidebactam results in increased inhibitory activity and stability against the hydrolysis of a wide range of β-lactamases [62]. Zidebactam combined with cefepime in a 1:1 combination is in clinical development for the treatment of Gram-negative bacterial infections. Studies have evaluated the in vitro activity of cefepime combined with zidebactam against a large worldwide collection of contemporary clinical isolates of Gram-negative organisms [63], demonstrating potent in vitro activity against Enterobacterales and P. aeruginosa, including isolates producing all classes of clinically relevant β-lactamases (classes A, C, and D), except for MBLs. Zidebactam was shown to cause potentiation in vitro of cefepime against S. maltophilia, but modest potentiation occurred against A. baumannii, with elevated MIC values (≥16 mg/L) [64,65] (Table 1). For antimicrobial susceptibility testing purpose, zidebactam should be tested at a 1:1 concentration with cefepime [4]. No clinical breakpoint (CLSI, EUCAST, or FDA) has been approved for this combination. An EUCAST epidemiological cut-off (ECOFF) value has not been assigned.
Three phase 1 trials (NCT02707107, NCT02942810 and NCT03630094) [66,67,68] and one phase 3 trial (NCT04979806) [69] have defined the value of this molecule. The efficacy, safety, and tolerability of cefepime/zidebactam (2 g of cefepime plus 1 g of zidebactam, every 8 h) in comparison to meropenem (1 g every 8 h) in the treatment of hospitalized patients with cUTIs or acute pyelonephritis are being examined as part of a phase 3 randomized, double-blind, multicenter, non-inferiority study (NCT04979806) [69]. A total of 504 hospitalized adults (≥18 years of age) with cUTIs or acute pyelonephritis will participate in the research project. A combination of clinical symptoms and signs and the presence of pyuria will be used to diagnose cUTIs or acute pyelonephritis. The research drugs’ treatment period lasts between seven and ten days [69]. No study results are posted on ClinicalTrials.gov for this study at this time, but are expected after August 2022 (Table 2).
The PKs of the two compounds are similar: in healthy volunteers, cefepime has a Vd of 15.4 ± 2.9 L and a PB of 20% while zidebactam has a Vd of 17.4 ± 3.2 L and a PB of <15% [69]. Data regarding the tissue penetration are available only for the respiratory tract: the ELF to total plasma penetration ratio, after multiple doses of cefepime 2 g plus 1 g zidebactam every 8 h, is 39% and 38%, respectively, while alveolar macrophage to total plasma ratios are 27% and 10%. The penetration ratio is based on total plasma concentration, as both agents have low plasma PB [20]. In healthy volunteers, cefepime has a mean t½ of 2.0 (±0.2) h and a Cl of 6.36 (±1.35) L/h, whereas zidebactam has a t½ of 1.9 (±0.3) and a Cl of 7.44 (±1.54) [20]. Both compounds are renally eliminated and dosage adjustments are required in patients with renal failure [70] (Table 3 and Table 4).
6. Cefiderocol
Cefiderocol is a combination of a catechol-type siderophore and a cephalosporin core with side chains similar to cefepime and ceftazidime. A catechol moiety on the 3-position of the R2 side chain allows cefiderocol to function as a siderophore molecule, chelating extracellular iron. Following the chelation of iron, cefiderocol is transported to the periplasmic space through ferric iron transport systems located on the outer membrane of Gram-negatives. Once within the periplasmic space, cefiderocol dissociates from the iron and binds to PBPs, inhibiting peptidoglycan cell wall synthesis [71]. Its unique structure and mechanism of action confer enhanced stability against hydrolysis by many β-lactamases, such as CTX-M, and carbapenemases KPC, NDM, VIM, IMP, OXA-23, OXA-48-like, OXA-51-like, and OXA-58 [72]. Cefiderocol has a broad antibacterial spectrum against a variety of aerobic bacteria, including Enterobacterales, Acinetobacter spp., Pseudomonas spp., Burkholderia spp., and S. maltophilia. Isolates of A. baumannii producing PER-like β-lactamases and NDM-like β-lactamases showed reduced susceptibility to cefiderocol. Malik et al. reported that reduced expression of the siderophore receptor gene pirA is correlated with resistance to cefiderocol in A. baumannii. Moreover, mutations involving the PBP3 may also contribute to cefiderocol resistance [73]. Interestingly, cefiderocol in combination with avibactam exhibited excellent activity against all OXA-23 and PER-like β-lactamase coproducing isolates [74] (Table 1). Cefiderocol formulation is commercially available (1 g vials). EUCAST provided a clinical breakpoint of ≤2 mg/L for Enterobacterales and Pseudomonas spp., while CLSI provided a clinical breakpoint of ≤4 mg/L for Enterobacterales, P. aeruginosa, Acinetobacter spp., and S. maltophilia [4].
A randomized, open-label, prospective, phase 3 clinical trial for cefiderocol was conducted in patients with carbapenem-resistant Gram-negative bacterial infections, regardless of species or source of infection, including sepsis and BSIs (ClinicalTrials.gov registration: NCT02714595) [38]. As defined by the best available therapy, clinical cure rates in nosocomial pneumonia (NP; 50%) and BSI (53%) were comparable between cefiderocol and the comparator (43 vs. 43%) [38]. In CREDIBLE-CR, cefiderocol was associated with favorable microbiological outcomes vs. the best available therapy when it came to cUTIs (53 vs. 20%) [38]. Moreover, cefiderocol caused a higher number of deaths, particularly in the Acinetobacter spp. subgroup, a finding for which no clear explanation was offered [38]. APEKS-NP is a randomized, double-blind, phase 3, non-inferiority investigation published recently by Wunderink et al. [75]. This study included 148 participants who were given cefiderocol and 152 subjects who were given meropenem. Cefiderocol was found to be non-inferior to high-dose extended-infusion meropenem in patients with Gram-negative NP, and mortality on day 14 was similar in all groups (12.4 vs. 11.6%) [75]. Moreover, Hsueh et al. examined the cefiderocol, ceftolozane/tazobactam, and ceftazidime/avibactam microbiological profiles in vitro for P. aeruginosa, S. maltophilia and A. baumannii bloodstream isolates [76] (Table 2). P. aeruginosa isolates resistant to colistin and imipenem were more susceptible to cefiderocol in vitro than those resistant to ceftolozane/tazobactam and ceftazidime/avibactam [76].
Specific tissue penetration data are available for the respiratory system: in healthy volunteers after a single 2 g i.v. dose, the drug penetrates into ELF with geometric mean concentration ratios, over 6 h, ranging from 0.0927 to 0.116 mg/L for ELF and total plasma [77]. In patients with VAP, the geometric mean ELF concentration of cefiderocol was 7.63 mg/L at the end of infusion, and 10.40 mg/L 2 h later. The ELF/unbound plasma concentration ratio was 0.212 (21.2%) at the end of infusion and 0.547 after 2 h, suggesting delayed lung distribution, with concentrations sufficient to treat Gram-negative bacteria [77].
Due to its hydrophilicity, cefiderocol shows urinary excretion with a negligible hepatic metabolism. After administration of multiple doses in healthy volunteers, the total drug Cl is 5.4 (±14.0) L/h, the t½ is 2.7 (±21.6) h [21] and the Vd 18 L (±3.36) [78]. Changes in renal function are the first cause of dose adjustment [79]; interestingly, this is true also for patients with CrCl >120 mL/min for which the administration interval should be reduced [80].
7. Ceftaroline/Avibactam
Ceftaroline-avibactam combines a fifth-generation broad-spectrum cephalosporin, with bactericidal activity against Gram-positive (including methicillin-resistant S. aureus) and Gram-negative pathogens, with avibactam, a diazabicyclooctane-derived molecule that can reversibly inhibit several β-lactamases, including Ambler class A, class C, and certain class D enzymes [82]. This association significantly extended the spectrum of action to ESBL-, AmpC-, KPC-, and OXA-48-producing Enterobacterales. More recently, it was demonstrated that ceftaroline-avibactam might increase the activity spectrum on K. pneumoniae-producing carbapenemases and multiple β-lactamases and modifications in OmpK35 and OmpK36 porins [83]. No activity was reported against MBL producers. Ceftaroline-avibactam demonstrated limited activity against A. baumannii and P. aeruginosa [84] (Table 1). For antimicrobial susceptibility testing purposes, the concentration of avibactam is fixed at 4 mg/L [4]. No clinical breakpoint (CLSI, EUCAST, or FDA) has been approved for this combination. An EUCAST epidemiological cut-off (ECOFF) value has not been assigned.
From a clinical point of view, ceftaroline-avibactam has been studied in a phase 2 trial (NCT01281462) in adults with cUTIs [85]. This study compared treatment with i.v.-co-administered ceftaroline fosamil, the prodrug of ceftaroline, and avibactam with different schedules, every 8 or 12 h; these arms were compared with doripenem or placebo. The study involved 217 patients and ended in 2012, and no results were posted or published elsewhere up to date. The chosen outcome measures were microbiological response to a test-of-cure and the safety profiles of the combined molecules. Secondary outcomes were the clinical response to the test of cure. Other completed works on that compound are mostly preclinical [NCT01624246, NCT01789528, NCT01290900] and results are not available [86,87,88]. Due to the interesting compound association, it would be of great interest not only to receive updates on this study, but also to observe from such a combination a potential development in the setting of HAP, VAP, ventilated hospital-acquired pneumonia (vHAP), and other complicated infections. No further conclusions can be extrapolated from the current available data on clinical use (Table 2).
In healthy volunteers, the PK parameters relative to the distribution of ceftaroline-fosamil/avibactam in the fixed-dose combination (600 mg/600 mg) are a Vd of 19.8 (±2.9) L when administered in a single dose and of 16.9 (±2.4) L when administered in multiple doses [23]. Ceftaroline-fosamil was approved in 2010 for the treatment of adults and children with community-acquired bacterial pneumonia and acute bacterial skin and skin structure infections [89]. In addition, the combination has been used off-label in serious infections such as nosocomial pneumonia, osteoarticular infections, meningitis, and endocarditis. In these tissues, ceftaroline-fosamil diffuses when administered at high doses (from 200 mg every 12 h to 800 mg every 8 h) [90] and has a good antibacterial effect. More studies are however needed to study the PK of the combination in more detail. Ceftaroline-fosamil/avibactam is primarily renally excreted; adjustment is therefore necessary for CrCL ≤ 50 mL/min [91] (Table 3 and Table 4).
8. Ceftolozane/Tazobactam
Ceftolozane/tazobactam is a new β-lactam/β-lactamase inhibitor combination consisting of a fixed (2:1) combination of an antipseudomonal cephalosporin, ceftolozane, and a well-established β-lactamase inhibitor, tazobactam, approved by the FDA in 2014. The chemical structure of ceftolozane is based on oxyimino-aminothiazolyl cephalosporin with a pyrazole substituent at the 3-position side chain, instead of the lighter pyridium, typical of ceftazidime. This heavier side chain has the ability to penetrate through porin channels and provides a steric obstacle to hydrolysis mediated by ESBL and AmpC determinants [92]. Ceftolozane/tazobactam presents antimicrobial activity against Enterobacterales and P. aeruginosa by the inhibition of common class A β-lactamases (TEM, SHV, CTX-M) or of class C enzymes [93]. Ceftolozane/tazobactam antimicrobial activity is less affected by P. aeruginosa AmpC enzymes than ceftazidime/avibactam, and, for this reason, ceftolozane/tazobactam is commonly considered an antipseudomonal drug. According to the Italian survey on P. aeruginosa, ceftolozane/tazobactam was the most active anti-Pseudomonas agent; moreover, it was active against approximately half the isolates that are resistant to all other β-lactams or resistant to all other agents except colistin [94]. High levels of resistance to ceftolozane/tazobactam in P. aeruginosa were associated with the overexpression and structural modification of AmpC [95]. No antimicrobial activity has been reported against A. baumannii and S. maltophilia, as well as against carbapenemase-producing microorganisms [96]. Ceftolozane/tazobactam is commercially available in a 2:1 formulation (Table 1). For antimicrobial susceptibility testing purposes, the concentration of tazobactam is fixed at 4 mg/L [4]. EUCAST and CLSI provided a susceptibility clinical breakpoint of ≤2 mg/L for Enterobacterales and of ≤4 mg/L for P. aeruginosa [4].
For cUTIs and cIAIs, the FDA and EMA approved 1.5 g (ratio of 1.0 ceftolozane to 0.5 tazobactam) every 8 h, with a double dosage (3 g; 2:1 ratio of ceftolozane to tazobactam) approved for the phase 3 trial ASPECT-NP for nosocomial pneumonia [40,41,97]. Bassetti et al. described one of the largest clinical trials using ceftolozane/tazobactam in a multicenter cohort of 101 patients with documented P. aeruginosa infection [98]. The only independent predictor of clinical failure was sepsis for patients with clinical success in comparison to those who suffered clinical failure, according to multivariate analyses (OR = 3.02, 95% CI: 1.01–9.2; p = 0.05) [98]. CEFTABUSE-registered results showed a non-significant trend towards more favorable 14-day clinical cure rates in ceftolozane/tazobactam-treated patients than aminoglycoside or colistin-treated patients (81.3% vs. 56.3%; p = 0.11%) [99]. In addition, a systematic study concluded that ceftolozane/tazobactam therapy could be useful, even outside of an accepted setting of indication, for difficult-to-treat P. aeruginosa infections [100] (Table 2).
Lung penetration in healthy volunteers was 61% for ceftolozane and 63% for taniborbactam, assuming, respectively, a PB of 21% and 30% [101]. Similarly, in critically ill, mechanically ventilated patients, lung penetration was 50% and 62%, respectively [102]. Ceftolozane Vd is about 13.5 L, while tazobactam is 18.2 L; these parameters are increased in patients with pneumonia compared with healthy subjects [103] and in neonates, consistent with age-related physiologic changes [104,105]. The combination has been employed off-label in skin and soft-tissue, bone and joint, bloodstream and multiple infections, suggesting good tissue penetration also in these tissues [100]. However, the combination does not provide adequate exposure in cerebral spinal fluid [106]. Both compounds are renally eliminated and dosage adjustment is required in renal impairment (Table 3 and Table 4).
9. Ceftazidime/Avibactam
Ceftazidime/avibactam is a β-lactam/β-lactamase inhibitor combination available since 2015. Avibactam is structurally different from the other clinically used β-lactamase inhibitors since it does not contain a β-lactam core. The inhibitory mechanism proceeds by opening of the avibactam ring, but the reaction is reversible, because the deacylation leads to the regeneration of the compound and not to hydrolysis and turnover [107]. Compounding avibactam with ceftazidime resulted in overcoming resistance due to Ambler class A, class C, and some class D β-lactamases [11]. For this reason, ceftazidime/avibactam has become a first-line option against KPC- or OXA-48-producing Enterobacterales, and represents an alternative option against ESBL- or AmpC-producing Enterobacterales and against P. aeruginosa. Episodes of colonization or infection due to ceftazidime/avibactam resistant strains have rapidly been reported in the literature [108]. Resistance to ceftazidime/avibactam is commonly due to the presence of MBLs as their activity is not restored by avibactam. Other mechanisms include increased expression of the blaKPC gene, specific mutations of genes coding for carbapenemases, changes in cell permeability (i.e., loss of porins), expression of efflux pumps, and, in the case of P. aeruginosa, by hyperexpression of PDC enzymes variants [109,110,111]. Ceftazidime/avibactam has no antimicrobial activity against Acinetobacter baumannii (no inhibition of A. baumannii OXA-type enzymes). Ceftazidime/avibactam is commercially available in a 4:1 formulation. For susceptibility testing purposes, the concentration of avibactam is fixed at 4 mg/L [112] (Table 1). EUCAST and CLSI provided a susceptibility clinical breakpoint of ≤8 mg/L for Enterobacterales and P. aeruginosa [4].
Ceftazidime/avibactam is approved for use in cIAIs, cUTIs, and HAP/VAP therapy, as well as in infections with microorganisms resistant to ceftazidime (RECLAIM, RECAPTURE 1&2, REPROVE, and REPRISE studies, respectively) [113,114,115,116]. Real-world data from patients with carbapenemases KPC and OXA-48 confirmed the clinical effectiveness of ceftazidime/avibactam [117,118,119,120]. Moreover, Fiore et al. found no differences in mortality rates between ceftazidime/avibactam monotherapy and combination therapy (N = 503 patients; direct evidence OR: 0.96; 95% CI: 0.65–1.41), and Onorato et al. found similar results in an unpublished systematic review [121,122]. A retrospective longitudinal investigation of 138 patients with KPC-producing K. pneumoniae bacteremia, whose mortality was considerably lower than that of a matched cohort of patients treated with medications other than ceftazidime/avibactam (36.5% against 55.8%, p = 0.005), was addressed by Tumbarello et al. [118]. Moreover, Shields et al. found that treatment with ceftazidime/avibactam had a significantly greater rate of clinical success (85 vs. 48/40/37%, p = 0.02) and survival at 90 days (92 vs. 69/55%, p =0.01) than other regimens, as well as higher renal safety compared to aminoglycoside- and colistin-based regimens [120] (Table 2).
PK studies have shown that the approved dosage (2/0.5 g every 8 h) provides adequate plasma levels [8] and sufficient drugs’ distribution in all approved indications [123]. In particular, the ELF:plasma penetration ratios are 52% for ceftazidime and 42% for avibactam. Cefepime-avibactam has been successfully used in the treatment of serious infections with limited treatment options and in tissues with difficult drug penetration [124], such in bone and joint infections [125,126], endocarditis [127], mediastinitis [128], abscesses [28], and post-transplant renal necrosis [129]. Ceftazidime PB is approximately 10% and the Vd is 14.3 L [130]. Avibactam PB is also low (5.7–8.2%) and the Vd is approximately 15–25 L [29]. Both drugs have a t½ of approximately 2 h [11] and dose adjustment is required in patients with moderate and severe renal impairment [124]. In patients on hemodialysis, the dose has to be administered after hemodialysis (Table 3 and Table 4).
10. Imipenem/Relebactam
Relebactam is a non-β-lactam, bicyclic diazabicyclooctane, β-lactamase inhibitor, structurally related to avibactam, but differing by the addition of a piperidine ring to the 2-position carbonyl group. Both inhibitors display activity against Ambler class A and class C β-lactamases [108,131,132]. Imipenem/relebactam has improved activity against P. aeruginosa with decreased expression of OprD and overproduction of AmpC β-lactamases, thanks to relebactam AmpC inhibition. Imipenem/relebactam maintains a limited activity against blaOXA-48-expressing carbapenem-resistant Enterobacterales, and has no activity against MBLs (including IMP, VIM, and NDM)-producing isolates. Relebactam has no activity against OXA class D β-lactamases of A. baumannii. Based on the data available, the addition of relebactam does not improve the activity of imipenem against A. baumannii and S. maltophilia [133,134]. Imipenem/relebactam is now commercially available in a 1:1 formulation (plus cilastatin). For susceptibility testing purposes, the concentration of relebactam is fixed at 4 mg/L [112] (Table 1). EUCAST provided a susceptibility clinical breakpoint of ≤2 mg/L for Enterobacterales, P. aeruginosa, and Acinetobacter spp., while CLSI provided a susceptibility clinical breakpoint of ≤1 mg/L for Enterobacterales and ≤2 mg/L for P. aeruginosa [4,112].
Two randomized, controlled, comparative, phase 3 clinical trials on imipenem/relebactam, RESTORE-IMI 1 and RESTORE-IMI 2, were conducted. In the first, the efficacy and safety of imipenem/relebactam was comparable to colistin plus imipenem for the treatment of imipenem-non-susceptible bacterial infections (including cIAIs, cUTIs, HAP and VAP in 47 patients with 16% K. pneumoniae and 16% KPC), with a 70% favorable overall response. A significantly lower incidence of nephrotoxicity was reported for imipenem/relebactam (10% vs. 56%, p = 0.002) [135]. In the second study, imipenem/relebactam was found to be non-inferior to piperacillin/tazobactam for the treatment of HAP/VAP. A sample of 537 patients was enrolled, and empiric linezolid administered in both arms. Overall, the data showed a favorable profile for imipenem/relebactam for critically ill and high-risk patients. Reported adverse events in both studies warned of the potential gastrointestinal disturbances, electrolyte imbalances, phlebitis and/or infusion-site reactions, fever, headache, and hypertension [136]. A phase 3 non-randomized, not controlled, open-label clinical study investigated the safety and efficacy of imipenem/relebactam in 81 Japanese subjects with cIAIs or cUTIs (14 bacteremic, 7 septic). Microorganisms were mostly non-MDR, and the results were in line with registration studies, showing comparable favorable efficacy and safety [137]. The microbiological features of the study may not add informative data for MDR pathogens. Finally, a phase 4 investigator-initiated, open-label, randomized, single-center trial is recruiting participants to study the clinical response of imipenem/relebactam in febrile neutropenia (NCT04983901) [45] (Table 2).
Because of their hydrophilic structures, the distribution of imipenem/relebactam is prevalent in the interstitial spaces; PB is about 20% for imipenem, 20% for cilastatin and 22% for relebactam; Vd is 24.3 L for imipenem and cilastatin and 19 L for relebactam [138]. The two drugs achieve relatively high concentrations in the respiratory system: the exposure in ELF, relative to that of unbound concentrations in plasma, is 55% for imipenem and 54% for relebactam [31]. As expected, imipenem was not detected in alveolar cells, providing further confirmation that its concentrations in the extracellular compartment are relevant for treating pneumonia [31]. Both imipenem and relebactam have renal Cl and a t½ of approximately 1 h [[138]; dose adjustment should be performed in renal impairment [139]. In hemodialyzed patients, the dose has to be administered after hemodialysis (Table 3 and Table 4).
11. Meropenem/Nacubactam
Similarly to zidebactam, nacubactam belongs to a new generation of DBO inhibitor. The meropenem/nacubactam combination exerts a potentiated spectrum of activity against class A, C, and some class D β-lactamases (a weak interaction with subclass 2 d enzymes), and promotes a further affinity for PBP2. This combination may potentially overcome ceftazidime/avibactam-resistant isolates among KPC-producing Enterobacterales due to mutation in the Ω-loop, with MIC values ≤ 8 mg/L [132,140]. The enhanced activity of the meropenem/nacubactam combination was demonstrated against class A serine carbapenemase-producing Enterobacterales [141], and against meropenem-resistant P. aeruginosa clinical isolates [142]. No data are available for activity against OXA-48-producing Enterobacterales. This combination showed no enhanced activity in comparison to meropenem alone, against A. baumannii [143]. Meropenem/nacubactam is currently in phase 2 trial (Table 1). For antimicrobial susceptibility testing purpose, nacubactam should be tested at a 1:1 concentration with meropenem [4]. No clinical breakpoint (CLSI, EUCAST, or FDA) has been approved for this combination. An EUCAST epidemiological cut-off (ECOFF) value has not been assigned.
To date, no clinical studies have explored the real-life use of the combination of meropenem/nacubactam in either phase 2 or 3 trials. The only study that explored the topic deeply is a non-randomized, open-label, one-treatment, one-group study in participants with cUTIs, including pyelonephritis, to characterize the PK of nacubactam co-administered with meropenem (NCT03174795) [144]. The study involved 20 patients and ended in 2017. The results were not displayed, and the primary outcomes were mainly pharmacokinetically directed. In preclinical studies, the chosen dosage for meropenem was similar to that for meropenem/vaborbactam, for which superposable considerations could be extrapolated. The addition of nacubactam may lead to wider microorganism coverage, as discussed in the previous section. We shall await clinical studies to broaden these considerations before making more inferences into the clinical use of this promising molecule (Table 2).
Two phase 1 studies show that the coadministration of 2000 mg of meropenem and 2000 mg of nacubactam does not significantly alter the PKs of either drugs [33]; the two compounds show similar PK after a single i.v. administration: meropenem shows a Vd of 15–20 L, a t½ of 1 h and a low PB of 2%, while for nacubactam, a Vd of 21.9 L, a t½ of 2.66 h, and a PB of 2% have been demonstrated [33].
A clinical study to investigate the intrapulmonary lung penetration of the combination in healthy volunteers has been completed, but results have not been posted yet [145]. Pre-clinical studies have been conducted in neutropenic murine models: after administering a dose mimicking the combination dosage of 2000/2000 mg every 8 h in humans, the %t > ELF at different drug concentrations and AUC0–24 were comparable in humans and mice, validating the animal model to assess the efficacy of the combination [142] (Table 3 and Table 4).
12. Meropenem/Vaborbactam
Meropenem/vaborbactam is a novel carbapenem-boronic acid β-lactamase inhibitor formulation approved by the FDA in 2017 [146,147]. Vaborbactam was designed to improve the performance of meropenem against carbapenemase-producing organisms. The boronic structure of vaborbactam forms a reversible covalent bond with the catalytic serine site of the β-lactamases [148]. Meropenem/vaborbactam presents antimicrobial activity against class A and class C β-lactamase-producing Enterobacterales, especially those producing ESBL, KPC, and AmpC determinants; hence, it represents a first-line choice for the treatment of KPC-producing Enterobacterales. Meropenem/vaborbactam was also shown to be active against strains of Enterobacterales producing other types of class A serine carbapenemases, such as SME and NMC-A enzymes [147]. Resistance to meropenem/vaborbactam in KPC-producing Enterobacterales is currently very rare and mostly due to porin inactivation (OmpK35/36) [149,150,151,152]. Interestingly, meropenem/vaborbactam retains activity also against strains producing KPC mutants that confer resistance to ceftazidime/avibactam (e.g., KPC-8, KPC-31) [153]. Accordingly, meropenem/vaborbactam is more specific than ceftazidime/avibactam against KPC-producing Enterobacterales. The activity of meropenem/vaborbactam against P. aeruginosa and A. baumannii was found to be similar to that of meropenem alone. In fact, in these species, meropenem resistance is largely mediated by mechanisms that are not antagonized by vaborbactam (e.g., outer-membrane impermeability, upregulation of efflux systems, and production of class B or class D β-lactamases) [154]. No antimicrobial activity has been reported for MBL-producing Gram-negatives and OXA-48-producing Enterobacterales. Meropenem/vaborbactam is commercially available in a 1:1 formulation. For susceptibility testing purposes, the concentration of vaborbactam is fixed at 8 mg/L [112] (Table 1). EUCAST provided a susceptibility clinical breakpoint of ≤8 mg/L for Enterobacterales and P. aeruginosa, while CLSI provided a susceptibility clinical breakpoint of ≤4 mg/L only for Enterobacterales [112].
The efficacy, tolerability, and safety of meropenem/vaborbactam for the treatment of cUTIs and acute pyelonephritis have been investigated in a phase 3 non-inferiority trial (TANGO I) [47]. In this study, 59.1% of patients were diagnosed with acute pyelonephritis and 40.9% with cUTIs. The most common pathogens were Enterobacteriaceae (29% ESBL) and P. aeruginosa. Per-pathogen clinical outcomes and microbiological eradication rates were similar among treatment groups. Meropenem/vaborbactam was found to be non-inferior to piperacillin/tazobactam for the primary outcome. Thereafter, a randomized, open-label trial investigated patients with cUTIs, HAP/VAP, bacteremia or cIAIs due to known or suspected carbapenem-resistant Enterobacteriaceae, of whom 63% were KPC-producing (TANGO II) [155]. The comparator was the “best available therapy” (including a variety of molecules, 67% in combination), and the results showed the superiority of meropenem/vaborbactam, especially in immunocompromised patients. The trial was terminated prematurely after an interim analysis demonstrating higher cure rates and lower mortality and nephrotoxicity rates with meropenem/vaborbactam. Lastly, NCT03006679, a phase 3b, double-blind, multicenter study, was launched to compare meropenem/vaborbactam with piperacillin/tazobactam for the treatment of HAP/VAP. The study was withdrawn due to the sponsor’s decision [156]. Preliminary real-world experiences have been published and have shown good results and confirmed data from trials, specifically with regard to carbapenem-resistant Enterobacteriaceae and KPC-producing bacteria and in isolates resistant to ceftazidime/avibactam [157,158,159,160]. Caution should be used in patients treated with valproic acid for potential interactions (Table 2).
The association is approved only for the treatment of cUTIs [34,161], at the combination ratio 2000/2000 mg q 8 h [[162]; however, Wenzler et al. found that its intrapulmonary penetration, based on the AUC (0–8) ratio of ELF and unbound plasma concentration, was 65% for meropenem and 79% for vaborbactam [35], suggesting a potential role on HAP and VAP [163]. Adequate penetration into cerebrospinal fluid, interstitial space, and tissue compartments has been demonstrated for meropenem; however, no data are currently available on vaborbactam or the association of the two drugs in these districts. Meropenem PB is approximately 2% and the Vd is 20.2 L, vaborbactam PB is instead 33% and the Vd is 18.6 L. The plasma Cl of meropenem and vaborbactam are similar. The t½ is 1.3 and 1.9 h, respectively; both drugs are renally eliminated and dosage adjustments are needed in patients with renal impairment [35,162]. In hemodialyzed patients, the dose has to be administered after hemodialysis [34] (Table 3 and Table 4).
13. Conclusions
Infections sustained by MDR or extensively drug-resistant (XDR) Gram-negatives represent a serious cause of concern. A “standard of care” for these infections is lacking, therefore familiarity with clinical, microbiological, and PK/PD data of new molecules/compounds is fundamental to achieve better clinical outcomes. In this review, we provided microbiological, clinical and pharmacological data for the new BL/BLIs and cefiderocol, to be used as an “all-inclusive” guide for clinicians to counsel the proper antibiotic therapy against infections sustained by MDR or XDR pathogens. It is of note that some less well-represented pathogens, such as Burkholderia spp., Pandorea spp., Elizabethkingia spp., Chryseobacterium spp. and Myroides spp. that usually have MDR or XDR phenotypes, may not be susceptible to most antibiotics here presented. This aspect did not reflect the aims of this review and was not included, but does warrant more specific studies.
Considering microbiological targets, most new antibiotics are active against ESBL, AmpC, and OXA-48-like determinants, while only a few showed antimicrobial activity against MBL producers (including S. maltophilia) and A. baumannii, thereby still representing an important challenge for the treatment of infectious diseases. Notably, for P. aeruginosa, good therapeutic options are currently or potentially available. Cefiderocol presents a broader spectrum of antimicrobial activity, being active against all investigated targets. Conversely, ceftolozane/tazobactam presents the most restricted antimicrobial activity, being active only against ESBL, AmpC, and P. aeruginosa. In addition, aztreonam/avibactam, cefepime/taniborbactam, and cefepime/zidebactam present wider antimicrobial activity, being active against six or seven investigated targets; hence, they are deserving of high expectations for their future introduction in clinical therapy.
In-depth knowledge of PK and PD properties of these antibiotics or antibiotic combinations is warranted to optimize prescribing and to preserve their antibacterial activity. From a PK point of view, all the mentioned agents are hydrophilic drugs and their relative solubility impacts on their volume of distribution, which mostly corresponds to extracellular fluids. The degree of plasma PB is also important, since only unbound drugs are able to exert antimicrobial activity; with the exception of cefiderocol with a PB of 40–60%, all other compounds are usually characterized by a low-to-moderate plasma PB. On the basis of these characteristics, these antibiotics diffuse easily in tissues and reach antibacterial levels in the ELF, therefore being useful in pulmonary infections. Finally, the hydrophilic nature of β-lactams is responsible for the route of elimination; for these agents, it is almost always renal. Efficacy in cICUs has been demonstrated; however, dose adjustment in patients with renal insufficiency is required.
β-Lactams exhibit time-dependent antibacterial effects, and maintaining the unbound drug concentration above the MIC (ft > MIC) for a significant part of the dosing interval predicts microbiological efficacy. This is particularly important in critically ill subjects [164,165] and in infections caused by multidrug-resistant bacteria [166]. Indeed, the inability to attain fT > MIC > 50% has been associated, in a large study in critically ill patients, with a 32% decreased likelihood of a positive clinical outcome [167] and, to attain this target, continuous infusion regimens have been proposed [168,169,170]. For most compounds described in the present review, maintenance of fT >MIC of 40–50% or more has been suggested, with longer values described only for cefiderocol (Table 3) and continuous infusion is therefore employed; however, for certain drugs, including the carbapenems and some of the newest cephalosporins such as ceftaroline, stability at room temperature is limited to 3–4 h and therefore these agents are better administered as a prolonged infusion to enhance pharmacodynamic exposure while retaining stability requirements.
From a clinical point of view, most studies were performed in patients with cICUs and fewer in patients with BSIs. Cefiderocol, ceftazidime/avibactam, and meropenem/vaborbactam are the compounds with broader clinical indications, although the microbiology spectrum is different with cefiderocol having the broadest one, followed by ceftazidime/avibactam and meropenem/vaborbactam. The “pro and cons” of the different new antibiotic compounds are shown in Table 5.

Table 5.
Pro and cons of new antibiotic compounds.
Belonging to the class of β-lactams, which inhibit the synthesis of the bacterial peptidoglycan cell wall, a bacterial target absent in eukaryotic cells, these agents have low direct toxicity. Hypersensitivity reactions are the most common adverse effect and, because of the common β-lactam ring, cross reactivity can occur. In addition, allergic reactions can be directed against the side chain; for instance, the R1 side chain is identical in cefotaxime, cefiderocol, and aztreonam, and cross reactivity between these agents has been described [171]. Central nervous system dysfunctions with headache, confusion, and seizure risk have been also described for all the compounds and associations, particularly in patients treated with high doses or with renal dysfunction. Finally, all these agents can change the composition of the microflora of the gastrointestinal tract, and Clostridioides difficile infections are a possible risk.
In conclusion, in consideration of their spectrum of activity, PK/PD characteristics, and relative low toxicity, these compounds represent an interesting possibility in the treatment of MDR or XDR Gram-negative bacteria. However, despite the recent introduction of these antibiotics, resistance has already been reported (especially for ceftazidime/avibactam). Known potential resistance mechanisms to the described antibiotic compounds are summarized in Table 6.

Table 6.
Resistance mechanisms in target organisms.
This review suggests that a cautious and optimal antimicrobial stewardship, also considering combination therapy including old and new molecules, is strongly advisable, in order to preserve last-resort antibiotics.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tan, X.; Kim, H.S.; Baugh, K.; Huang, Y.; Kadiyala, N.; Wences, M.; Singh, N.; Wenzler, E.; Bulman, Z.P. Therapeutic Options for Metallo-β-Lactamase-Producing Enterobacterales. Infect. Drug Resist. 2021, 14, 125–142. [Google Scholar] [CrossRef] [PubMed]
- Mauri, C.; Maraolo, A.E.; Di Bella, S.; Luzzaro, F.; Principe, L. The Revival of Aztreonam in Combination with Avibactam against Metallo-β-Lactamase-Producing Gram-Negatives: A Systematic Review of In Vitro Studies and Clinical Cases. Antibiotics 2021, 10, 1012. [Google Scholar] [CrossRef] [PubMed]
- Sader, H.S.; Carvalhaes, C.G.; Arends, S.J.R.; Castanheira, M.; Mendes, R.E. Aztreonam/avibactam Activity against Clinical Isolates of Enterobacterales Collected in Europe, Asia and Latin America in 2019. J. Antimicrob. Chemother. 2021, 76, 659–666. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 31st ed.; CLSI Supplement M100; Clinical Laboratory Standards Institute: Malvern, PA, USA, 2021. [Google Scholar]
- Aztreonam/Avibactam—List Results. ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/results?cond=aztreonam%2Favibactam&term=&cntry=&state=&city=&dist= (accessed on 5 February 2022).
- Cornely, O.A.; Cisneros, J.M.; Torre-Cisneros, J.; Rodríguez-Hernández, M.J.; Tallón-Aguilar, L.; Calbo, E.; Horcajada, J.P.; Queckenberg, C.; Zettelmeyer, U.; Arenz, D.; et al. Pharmacokinetics and Safety of Aztreonam/avibactam for the Treatment of Complicated Intra-Abdominal Infections in Hospitalized Adults: Results from the REJUVENATE Study. J. Antimicrob. Chemother. 2020, 75, 618–627. [Google Scholar] [CrossRef]
- Falcone, M.; Menichetti, F.; Cattaneo, D.; Tiseo, G.; Baldelli, S.; Galfo, V.; Leonildi, A.; Tagliaferri, E.; Di Paolo, A.; Pai, M.P. Pragmatic Options for Dose Optimization of Ceftazidime/avibactam with Aztreonam in Complex Patients. J. Antimicrob. Chemother. 2021, 76, 1025–1031. [Google Scholar] [CrossRef]
- Dimelow, R.; Wright, J.G.; MacPherson, M.; Newell, P.; Das, S. Population Pharmacokinetic Modelling of Ceftazidime and Avibactam in the Plasma and Epithelial Lining Fluid of Healthy Volunteers. Drugs R&D 2018, 18, 221–230. [Google Scholar]
- Karaiskos, I.; Lagou, S.; Pontikis, K.; Rapti, V.; Poulakou, G. The “Old” and the “New” Antibiotics for MDR Gram-Negative Pathogens: For Whom, When, and How. Front. Public Health 2019, 7, 151. [Google Scholar] [CrossRef]
- Di Paolo, A.; Gori, G.; Tascini, C.; Danesi, R.; Del Tacca, M. Clinical Pharmacokinetics of Antibacterials in Cerebrospinal Fluid. Clin. Pharmacokinet. 2013, 52, 511–542. [Google Scholar] [CrossRef]
- Nichols, W.W.; Newell, P.; Critchley, I.A.; Riccobene, T.; Das, S. Avibactam Pharmacokinetic/Pharmacodynamic Targets. Antimicrob. Agents Chemother. 2018, 62, 02446-17. [Google Scholar] [CrossRef]
- Luci, G.; Mattioli, F.; Falcone, M.; Di Paolo, A. Pharmacokinetics of Non-β-Lactam β-Lactamase Inhibitors. Antibiotics 2021, 10, 769. [Google Scholar] [CrossRef]
- Ramsey, C.; MacGowan, A.P. A Review of the Pharmacokinetics and Pharmacodynamics of Aztreonam. J. Antimicrob. Chemother. 2016, 71, 2704–2712. [Google Scholar] [CrossRef] [PubMed]
- Bernhard, F.; Odedra, R.; Sordello, S.; Cardin, R.; Franzoni, S.; Charrier, C.; Belley, A.; Warn, P.; Machacek, M.; Knechtle, P. Pharmacokinetics-Pharmacodynamics of Enmetazobactam Combined with Cefepime in a Neutropenic Murine Thigh Infection Model. Antimicrob. Agents Chemother. 2020, 64, e00078-20. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Fitzgerald, R.; Ullah, A.; Bula, M.; Collins, A.M.; Mitsi, E.; Reine, J.; Hill, H.; Rylance, J.; Ferreira, D.M.; et al. Intrapulmonary Pharmacokinetics of Cefepime and Enmetazobactam in Healthy Volunteers: Towards New Treatments for Nosocomial Pneumonia. Antimicrob. Agents Chemother. 2020, 65, e01468-20. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, M.P.; Nakahiro, R.K.; Chin, A.; Bedikian, A. Cefepime Clinical Pharmacokinetics. Clin. Pharmacokinet. 1993, 25, 88–102. [Google Scholar] [CrossRef]
- Abdelraouf, K.; Almarzoky Abuhussain, S.; Nicolau, D.P. In Vivo Pharmacodynamics of New-Generation β-Lactamase Inhibitor Taniborbactam (formerly VNRX-5133) in Combination with Cefepime against Serine-β-Lactamase-Producing Gram-Negative Bacteria. J. Antimicrob. Chemother. 2020, 75, 3601–3610. [Google Scholar] [CrossRef]
- Dowell, J.A.; Dickerson, D.; Henkel, T. Safety and Pharmacokinetics in Human Volunteers of Taniborbactam (VNRX-5133), a Novel Intravenous β-Lactamase Inhibitor. Antimicrob. Agents Chemother. 2021, 65, e0105321. [Google Scholar] [CrossRef]
- Lepak, A.J.; Zhao, M.; Andes, D.R. WCK 5222 (Cefepime/Zidebactam) Pharmacodynamic Target Analysis against Metallo-β-Lactamase Producing in the Neutropenic Mouse Pneumonia Model. Antimicrob. Agents Chemother. 2019, 63, e01648-19. [Google Scholar] [CrossRef]
- Rodvold, K.A.; Gotfried, M.H.; Chugh, R.; Gupta, M.; Patel, A.; Chavan, R.; Yeole, R.; Friedland, H.D.; Bhatia, A. Plasma and Intrapulmonary Concentrations of Cefepime and Zidebactam Following Intravenous Administration of WCK 5222 to Healthy Adult Subjects. Antimicrob. Agents Chemother. 2018, 62, e00682-18. [Google Scholar] [CrossRef]
- Saisho, Y.; Katsube, T.; White, S.; Fukase, H.; Shimada, J. Pharmacokinetics, Safety, and Tolerability of Cefiderocol, a Novel Siderophore Cephalosporin for Gram-Negative Bacteria, in Healthy Subjects. Antimicrob. Agents Chemother. 2018, 62, e02163-17. [Google Scholar] [CrossRef]
- Katsube, T.; Echols, R.; Wajima, T. Pharmacokinetic and Pharmacodynamic Profiles of Cefiderocol, a Novel Siderophore Cephalosporin. Clin. Infect. Dis. 2019, 69, S552–S558. [Google Scholar] [CrossRef]
- Riccobene, T.A.; Su, S.F.; Rank, D. Single- and Multiple-Dose Study to Determine the Safety, Tolerability, and Pharmacokinetics of Ceftaroline Fosamil in Combination with Avibactam in Healthy Subjects. Antimicrob. Agents Chemother. 2013, 57, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Riccobene, T.A.; Pushkin, R.; Jandourek, A.; Knebel, W.; Khariton, T. Penetration of Ceftaroline into the Epithelial Lining Fluid of Healthy Adult Subjects. Antimicrob. Agents Chemother. 2016, 60, 5849–5857. [Google Scholar] [CrossRef] [PubMed]
- Lepak, A.J.; Reda, A.; Marchillo, K.; Van Hecker, J.; Craig, W.A.; Andes, D. Impact of MIC Range for Pseudomonas Aeruginosa and Streptococcus Pneumoniae on the Ceftolozane in Vivo Pharmacokinetic/pharmacodynamic Target. Antimicrob. Agents Chemother. 2014, 58, 6311–6314. [Google Scholar] [CrossRef] [PubMed]
- Xiao, A.J.; Caro, L.; Popejoy, M.W.; Huntington, J.A.; Kullar, R. PK/PD Target Attainment with Ceftolozane/Tazobactam Using Monte Carlo Simulation in Patients with Various Degrees of Renal Function, Including Augmented Renal Clearance and End-Stage Renal Disease. Infect. Dis. Ther. 2017, 6, 137–148. [Google Scholar] [CrossRef]
- Nicolau, D.P.; De Waele, J.; Kuti, J.L.; Caro, L.; Larson, K.B.; Yu, B.; Gadzicki, E.; Zeng, Z.; Rhee, E.G.; Rizk, M.L. Pharmacokinetics and Pharmacodynamics of Ceftolozane/Tazobactam in Critically Ill Patients With Augmented Renal Clearance. Int. J. Antimicrob. Agents 2021, 57, 106299. [Google Scholar] [CrossRef]
- Davido, B.; Fellous, L.; Lawrence, C.; Maxime, V.; Rottman, M.; Dinh, A. Ceftazidime-Avibactam and Aztreonam, an Interesting Strategy to Overcome β-Lactam Resistance Conferred by Metallo-β-Lactamases in Enterobacteriaceae and Pseudomonas Aeruginosa. Antimicrob. Agents Chemother. 2017, 61, e01008-17. [Google Scholar] [CrossRef]
- Merdjan, H.; Rangaraju, M.; Tarral, A. Safety and Pharmacokinetics of Single and Multiple Ascending Doses of Avibactam Alone and in Combination with Ceftazidime in Healthy Male Volunteers: Results of Two Randomized, Placebo-Controlled Studies. Clin. Drug Investig. 2015, 35, 307–317. [Google Scholar] [CrossRef]
- Van Duin, D.; Bonomo, R.A. Ceftazidime/Avibactam and Ceftolozane/Tazobactam: Second-Generation β-Lactam/β-Lactamase Inhibitor Combinations. Clin. Infect. Dis. 2016, 63, 234–241. [Google Scholar] [CrossRef]
- Rizk, M.L.; Rhee, E.G.; Jumes, P.A.; Gotfried, M.H.; Zhao, T.; Mangin, E.; Bi, S.; Chavez-Eng, C.M.; Zhang, Z.; Butterton, J.R. Intrapulmonary Pharmacokinetics of Relebactam, a Novel β-Lactamase Inhibitor, Dosed in Combination with Imipenem-Cilastatin in Healthy Subjects. Antimicrob. Agents Chemother. 2018, 62, e01411-17. [Google Scholar] [CrossRef]
- Heo, Y.-A. Imipenem/Cilastatin/Relebactam: A Review in Gram-Negative Bacterial Infections. Drugs 2021, 81, 377–388. [Google Scholar] [CrossRef]
- Mallalieu, N.L.; Winter, E.; Fettner, S.; Patel, K.; Zwanziger, E.; Attley, G.; Rodriguez, I.; Kano, A.; Salama, S.M.; Bentley, D.; et al. Safety and Pharmacokinetic Characterization of Nacubactam, a Novel β-Lactamase Inhibitor, Alone and in Combination with Meropenem, in Healthy Volunteers. Antimicrob. Agents Chemother. 2020, 64, e02229-19. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, S. Meropenem/Vaborbactam: A Review in Complicated Urinary Tract Infections. Drugs 2018, 78, 1259–1270. [Google Scholar] [CrossRef] [PubMed]
- Wenzler, E.; Scoble, P.J. An Appraisal of the Pharmacokinetic and Pharmacodynamic Properties of Meropenem-Vaborbactam. Infect. Dis. Ther. 2020, 9, 769–784. [Google Scholar] [CrossRef] [PubMed]
- Wenzler, E.; Gotfried, M.H.; Loutit, J.S.; Durso, S.; Griffith, D.C.; Dudley, M.N.; Rodvold, K.A. Meropenem-RPX7009 Concentrations in Plasma, Epithelial Lining Fluid, and Alveolar Macrophages of Healthy Adult Subjects. Antimicrob. Agents Chemother. 2015, 59, 7232–7239. [Google Scholar] [CrossRef]
- Zhuang, L.; Yu, Y.; Wei, X.; Florian, J.; Jang, S.H.; Reynolds, K.S.; Wang, Y. Evaluation of Hemodialysis Effect on Pharmacokinetics of Meropenem/Vaborbactam in End-Stage Renal Disease Patients Using Modeling and Simulation. J. Clin. Pharmacol. 2020, 60, 1011–1021. [Google Scholar] [CrossRef]
- Bassetti, M.; Echols, R.; Matsunaga, Y.; Ariyasu, M.; Doi, Y.; Ferrer, R.; Lodise, T.P.; Naas, T.; Niki, Y.; Paterson, D.L.; et al. Efficacy and Safety of Cefiderocol or Best Available Therapy for the Treatment of Serious Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria (CREDIBLE-CR): A Randomised, Open-Label, Multicentre, Pathogen-Focused, Descriptive, Phase 3 Trial. Lancet Infect. Dis. 2021, 21, 226–240. [Google Scholar] [CrossRef]
- Portsmouth, S.; Van Veenhuyzen, D.; Echols, R.; Machida, M.; Ferreira, J.C.A.; Ariyasu, M.; Tenke, P.; Nagata, T.D. Cefiderocol versus Imipenem-Cilastatin for the Treatment of Complicated Urinary Tract Infections Caused by Gram-Negative Uropathogens: A Phase 2, Randomised, Double-Blind, Non-Inferiority Trial. Lancet Infect. Dis. 2018, 18, 1319–1328. [Google Scholar] [CrossRef]
- Wagenlehner, F.M.; Umeh, O.; Steenbergen, J.; Yuan, G.; Darouiche, R.O. Ceftolozane-Tazobactam Compared with Levofloxacin in the Treatment of Complicated Urinary-Tract Infections, Including Pyelonephritis: A Randomised, Double-Blind, Phase 3 Trial (ASPECT-cUTI). Lancet 2015, 385, 1949–1956. [Google Scholar] [CrossRef]
- Kollef, M.H.; Nováček, M.; Kivistik, Ü.; Réa-Neto, Á.; Shime, N.; Martin-Loeches, I.; Timsit, J.-F.; Wunderink, R.G.; Bruno, C.J.; Huntington, J.A.; et al. Ceftolozane-Tazobactam versus Meropenem for Treatment of Nosocomial Pneumonia (ASPECT-NP): A Randomised, Controlled, Double-Blind, Phase 3, Non-Inferiority Trial. Lancet Infect. Dis. 2019, 19, 1299–1311. [Google Scholar] [CrossRef]
- Dietch, Z.C.; Shah, P.M.; Sawyer, R.G. Advances in Intra-Abdominal Sepsis: What Is New? Curr. Infect. Dis. Rep. 2015, 17, 497. [Google Scholar] [CrossRef]
- Hernández-Tejedor, A.; Merino-Vega, C.D.; Martín-Vivas, A.; Ruiz de Luna-González, R.; Delgado-Iribarren, A.; Gabán-Díez, Á.; Temprano-Gómez, I.; De la Calle-Pedrosa, N.; González-Jiménez, A.I.; Algora-Weber, A. Successful Treatment of Multidrug-Resistant Pseudomonas Aeruginosa Breakthrough Bacteremia with Ceftolozane/tazobactam. Infection 2017, 45, 115–117. [Google Scholar] [CrossRef] [PubMed]
- Sousa Dominguez, A.; Perez-Rodríguez, M.T.; Nodar, A.; Martinez-Lamas, L.; Perez-Landeiro, A.; Crespo Casal, M. Successful Treatment of MDR Pseudomonas Aeruginosa Skin and Soft-Tissue Infection with Ceftolozane/tazobactam. J. Antimicrob. Chemother. 2017, 72, 1262–1263. [Google Scholar] [PubMed]
- Imipenem, Cilastatin Sodium, and Relebactam Monohydrate for the Treatment of Cancer Patients with Febrile Neutropenia. Available online: https://clinicaltrials.gov/ct2/show/NCT04983901 (accessed on 5 February 2022).
- Sims, M.; Mariyanovski, V.; McLeroth, P.; Akers, W.; Lee, Y.-C.; Brown, M.L.; Du, J.; Pedley, A.; Kartsonis, N.A.; Paschke, A. Prospective, Randomized, Double-Blind, Phase 2 Dose-Ranging Study Comparing Efficacy and Safety of Imipenem/cilastatin plus Relebactam with Imipenem/cilastatin Alone in Patients with Complicated Urinary Tract Infections. J. Antimicrob. Chemother. 2017, 72, 2616–2626. [Google Scholar] [CrossRef] [PubMed]
- Kaye, K.S.; Bhowmick, T.; Metallidis, S.; Bleasdale, S.C.; Sagan, O.S.; Stus, V.; Vazquez, J.; Zaitsev, V.; Bidair, M.; Chorvat, E.; et al. Effect of Meropenem-Vaborbactam vs Piperacillin-Tazobactam on Clinical Cure or Improvement and Microbial Eradication in Complicated Urinary Tract Infection: The TANGO I Randomized Clinical Trial. JAMA 2018, 319, 788–799. [Google Scholar] [CrossRef]
- Buckman, S.A.; Krekel, T.; Muller, A.E.; Mazuski, J.E. Ceftazidime-Avibactam for the Treatment of Complicated Intra-Abdominal Infections. Expert Opin. Pharmacother. 2016, 17, 2341–2349. [Google Scholar] [CrossRef]
- Torres, A.; Zhong, N.; Pachl, J.; Timsit, J.-F.; Kollef, M.; Chen, Z.; Song, J.; Taylor, D.; Laud, P.J.; Stone, G.G.; et al. Ceftazidime-Avibactam versus Meropenem in Nosocomial Pneumonia, Including Ventilator-Associated Pneumonia (REPROVE): A Randomised, Double-Blind, Phase 3 Non-Inferiority Trial. Lancet Infect. Dis. 2018, 18, 285–295. [Google Scholar] [CrossRef]
- Wagenlehner, F.M.; Sobel, J.D.; Newell, P.; Armstrong, J.; Huang, X.; Stone, G.G.; Yates, K.; Gasink, L.B. Ceftazidime-Avibactam Versus Doripenem for the Treatment of Complicated Urinary Tract Infections, Including Acute Pyelonephritis: RECAPTURE, a Phase 3 Randomized Trial Program. Clin. Infect. Dis. 2016, 63, 754–762. [Google Scholar] [CrossRef]
- Isler, B.; Harris, P.; Stewart, A.G.; Paterson, D.L. An Update on Cefepime and Its Future Role in Combination with Novel β-Lactamase Inhibitors for MDR Enterobacterales and Pseudomonas Aeruginosa. J. Antimicrob. Chemother. 2021, 76, 550–560. [Google Scholar] [CrossRef]
- Papp-Wallace, K.M.; Bethel, C.R.; Caillon, J.; Barnes, M.D.; Potel, G.; Bajaksouzian, S.; Rutter, J.D.; Reghal, A.; Shapiro, S.; Taracila, M.A.; et al. Beyond Piperacillin-Tazobactam: Cefepime and AAI101 as a Potent β-Lactam-β-Lactamase Inhibitor Combination. Antimicrob. Agents Chemother. 2019, 63, e00105-19. [Google Scholar] [CrossRef]
- Liu, P.-Y.; Ko, W.-C.; Lee, W.-S.; Lu, P.-L.; Chen, Y.-H.; Cheng, S.-H.; Lu, M.-C.; Lin, C.-Y.; Wu, T.-S.; Yen, M.-Y.; et al. In Vitro Activity of Cefiderocol, Cefepime/enmetazobactam, Cefepime/zidebactam, Eravacycline, Omadacycline, and Other Comparative Agents against Carbapenem-Non-Susceptible Pseudomonas Aeruginosa and Acinetobacter baumannii Isolates Associated from Bloodstream Infection in Taiwan between 2018–2020. J. Microbiol. Immunol. Infect. 2021, in press. [Google Scholar] [CrossRef]
- Cefepime/AAI101 Phase 2 Study in Hospitalized Adults With cUTI. Available online: https://clinicaltrials.gov/ct2/show/NCT03680612 (accessed on 5 February 2022).
- Pharmacokinetics of Cefepime and AAI101 in Subjects with Renal Insufficiency and Healthy Subjects. Available online: https://clinicaltrials.gov/ct2/show/NCT03680352 (accessed on 5 February 2022).
- Safety and Efficacy Study of Cefepime-AAI101 in the Treatment of Complicated Urinary Tract Infections. Available online: https://clinicaltrials.gov/ct2/show/NCT03687255 (accessed on 5 February 2022).
- Investigation of AAI101 Safety, Tolerability & PK in Healthy Volunteers. Available online: https://clinicaltrials.gov/ct2/show/NCT03685084 (accessed on 5 February 2022).
- Liu, B.; Trout, R.E.L.; Chu, G.-H.; McGarry, D.; Jackson, R.W.; Hamrick, J.C.; Daigle, D.M.; Cusick, S.M.; Pozzi, C.; De Luca, F.; et al. Discovery of Taniborbactam (VNRX-5133): A Broad-Spectrum Serine- and Metallo-β-Lactamase Inhibitor for Carbapenem-Resistant Bacterial Infections. J. Med. Chem. 2020, 63, 2789–2801. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhao, C.; Wang, Q.; Wang, Z.; Liang, X.; Zhang, F.; Zhang, Y.; Meng, H.; Chen, H.; Li, S.; et al. In Vitro Activity of the Novel β-Lactamase Inhibitor Taniborbactam (VNRX-5133), in Combination with Cefepime or Meropenem, against MDR Gram-Negative Bacterial Isolates from China. J. Antimicrob. Chemother. 2020, 75, 1850–1858. [Google Scholar] [CrossRef] [PubMed]
- Lasko, M.J.; Nicolau, D.P.; Asempa, T.E. Clinical Exposure-Response Relationship of Cefepime/taniborbactam against Gram-Negative Organisms in the Murine Complicated Urinary Tract Infection Model. J. Antimicrob. Chemother. 2022, 77, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Safety and Efficacy Study of Cefepime/VNRX-5133 in Patients with Complicated Urinary Tract Infections—Full Text View. ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT03840148 (accessed on 5 February 2022).
- Karaiskos, I.; Galani, I.; Papoutsaki, V.; Galani, L.; Giamarellou, H. Carbapenemase Producing: Implication on Future Therapeutic Strategies. Expert Rev. Anti-Infect. Ther. 2022, 20, 53–69. [Google Scholar] [CrossRef]
- Sader, H.S.; Castanheira, M.; Huband, M.; Jones, R.N.; Flamm, R.K. WCK 5222 (Cefepime-Zidebactam) Antimicrobial Activity against Clinical Isolates of Gram-Negative Bacteria Collected Worldwide in 2015. Antimicrob. Agents Chemother. 2017, 61, e00072-17. [Google Scholar] [CrossRef]
- Lasko, M.J.; Abdelraouf, K.; Nicolau, D.P. Comparative in Vivo Activity of Human-Simulated Plasma and Epithelial Lining Fluid Exposures of WCK 5222 (cefepime/zidebactam) against KPC- and OXA-48-like-Producing Klebsiella Pneumoniae in the Neutropenic Murine Pneumonia Model. J. Antimicrob. Chemother. 2021, 76, 2310–2316. [Google Scholar] [CrossRef]
- Livermore, D.M.; Mushtaq, S.; Warner, M.; Vickers, A.; Woodford, N. In Vitro Activity of Cefepime/zidebactam (WCK 5222) against Gram-Negative Bacteria. J. Antimicrob. Chemother. 2017, 72, 1373–1385. [Google Scholar] [CrossRef]
- MED Study to Evaluate the Safety, Tolerability and Pharmacokinetics of Intravenous WCK 5222 (Zidebactam and Cefepime) in Healthy Volunteers. Available online: https://clinicaltrials.gov/ct2/show/NCT02707107 (accessed on 8 February 2022).
- To Investigate the Pharmacokinetics of Intravenous WCK 5222 (FEP-ZID) in Patients with Renal Impairment. Available online: https://clinicaltrials.gov/ct2/show/NCT02942810 (accessed on 8 February 2022).
- Plasma and Intrapulmonary Concentrations Study of WCK 5222. Available online: https://clinicaltrials.gov/ct2/show/NCT03630094 (accessed on 8 February 2022).
- Study of Cefepime-Zidebactam (FEP-ZID) in Complicated Urinary Tract Infection (cUTI) or Acute Pyelonephritis (AP). Available online: https://clinicaltrials.gov/ct2/show/NCT04979806 (accessed on 5 February 2022).
- Preston, R.A.; Mamikonyan, G.; DeGraff, S.; Chiou, J.; Kemper, C.J.; Xu, A.; Mastim, M.; Yeole, R.; Chavan, R.; Patel, A.; et al. Single-Center Evaluation of the Pharmacokinetics of WCK 5222 (Cefepime-Zidebactam Combination) in Subjects with Renal Impairment. Antimicrob. Agents Chemother. 2019, 63, e01484-18. [Google Scholar] [CrossRef]
- El-Lababidi, R.M.; Rizk, J.G. Cefiderocol: A Siderophore Cephalosporin. Ann. Pharmacother. 2020, 54, 1215–1231. [Google Scholar] [CrossRef]
- Wu, J.Y.; Srinivas, P.; Pogue, J.M. Cefiderocol: A Novel Agent for the Management of Multidrug-Resistant Gram-Negative Organisms. Infect. Dis. Ther. 2020, 9, 17–40. [Google Scholar] [CrossRef]
- Malik, S.; Kaminski, M.; Landman, D.; Quale, J. Cefiderocol Resistance in Acinetobacter baumannii: Roles of β-Lactamases, Siderophore Receptors, and Penicillin Binding Protein 3. Antimicrob. Agents Chemother. 2020, 64, e01221-20. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Sadek, M.; Nordmann, P. Contribution of PER-Type and NDM-Type β-Lactamases to Cefiderocol Resistance in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2021, 65, e0087721. [Google Scholar] [CrossRef] [PubMed]
- Wunderink, R.G.; Matsunaga, Y.; Ariyasu, M.; Clevenbergh, P.; Echols, R.; Kaye, K.S.; Kollef, M.; Menon, A.; Pogue, J.M.; Shorr, A.F.; et al. Cefiderocol versus High-Dose, Extended-Infusion Meropenem for the Treatment of Gram-Negative Nosocomial Pneumonia (APEKS-NP): A Randomised, Double-Blind, Phase 3, Non-Inferiority Trial. Lancet Infect. Dis. 2021, 21, 213–225. [Google Scholar] [CrossRef]
- Hsueh, S.-C.; Lee, Y.-J.; Huang, Y.-T.; Liao, C.-H.; Tsuji, M.; Hsueh, P.-R. In Vitro Activities of Cefiderocol, Ceftolozane/tazobactam, Ceftazidime/avibactam and other Comparative Drugs against Imipenem-Resistant Pseudomonas Aeruginosa and Acinetobacter baumannii, and Stenotrophomonas Maltophilia, All Associated with Bloodstream Infections in Taiwan. J. Antimicrob. Chemother. 2019, 74, 380–386. [Google Scholar] [PubMed]
- Katsube, T.; Nicolau, D.P.; Rodvold, K.A.; Wunderink, R.G.; Echols, R.; Matsunaga, Y.; Menon, A.; Portsmouth, S.; Wajima, T. Intrapulmonary Pharmacokinetic Profile of Cefiderocol in Mechanically Ventilated Patients with Pneumonia. J. Antimicrob. Chemother. 2021, 76, 2902–2905. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, S.; Singley, C.M.; Hoover, J.; Nakamura, R.; Echols, R.; Rittenhouse, S.; Tsuji, M.; Yamano, Y. Efficacy of Cefiderocol against Carbapenem-Resistant Gram-Negative Bacilli in Immunocompetent-Rat Respiratory Tract Infection Models Recreating Human Plasma Pharmacokinetics. Antimicrob. Agents Chemother. 2017, 61, e00700-17. [Google Scholar] [CrossRef]
- Katsube, T.; Saisho, Y.; Shimada, J.; Furuie, H. Intrapulmonary Pharmacokinetics of Cefiderocol, a Novel Siderophore Cephalosporin, in Healthy Adult Subjects. J. Antimicrob. Chemother. 2019, 74, 1971–1974. [Google Scholar] [CrossRef]
- Bilbao-Meseguer, I.; Rodríguez-Gascón, A.; Barrasa, H.; Isla, A.; Solinís, M.Á. Augmented Renal Clearance in Critically Ill Patients: A Systematic Review. Clin. Pharmacokinet. 2018, 57, 1107–1121. [Google Scholar] [CrossRef]
- Kawaguchi, N.; Katsube, T.; Echols, R.; Wajima, T. Population Pharmacokinetic Analysis of Cefiderocol, a Parenteral Siderophore Cephalosporin, in Healthy Subjects, Subjects with Various Degrees of Renal Function, and Patients with Complicated Urinary Tract Infection or Acute Uncomplicated Pyelonephritis. Antimicrob. Agents Chemother. 2018, 62, 01391-17. [Google Scholar] [CrossRef]
- Vrancianu, C.O.; Dobre, E.G.; Gheorghe, I.; Barbu, I.; Cristian, R.E.; Chifiriuc, M.C. Present and Future Perspectives on Therapeutic Options for Carbapenemase-Producing Infections. Microorganisms 2021, 9, 730. [Google Scholar] [CrossRef]
- Khalid, A.; Lubián, A.F.; Ma, L.; Lin, R.C.Y.; Iredell, J.R. Characterizing the Role of Porin Mutations in Susceptibility of Beta Lactamase Producing Klebsiella Pneumoniae Isolates to Ceftaroline and Ceftaroline-Avibactam. Int. J. Infect. Dis. 2020, 93, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Castanheira, M.; Sader, H.S.; Farrell, D.J.; Mendes, R.E.; Jones, R.N. Activity of Ceftaroline-Avibactam Tested against Gram-Negative Organism Populations, Including Strains Expressing One or More β-Lactamases and Methicillin-Resistant Staphylococcus Aureus Carrying Various Staphylococcal Cassette Chromosome Mec Types. Antimicrob. Agents Chemother. 2012, 56, 4779–4785. [Google Scholar] [CrossRef] [PubMed]
- Comparative Study of Coadministered Ceftaroline Fosamil and NXL104 vs. Intravenous Doripenem in Adult Subjects with Complicated Urinary Tract Infections. Available online: https://clinicaltrials.gov/ct2/show/NCT01281462 (accessed on 5 February 2022).
- Pharmacokinetic Study of Ceftaroline Fosamil/Avibactam in Adults with Augmented Renal Clearance. Available online: https://clinicaltrials.gov/ct2/show/NCT01624246 (accessed on 5 February 2022).
- A Study to Investigate the Effect of Administration of Ceftazidime-Avibactam (CAZ-AVI) and Ceftaroline Fosamil-Avibactam (CXL) on the Intestinal Flora of Healthy Volunteers. Available online: https://clinicaltrials.gov/ct2/show/NCT01789528 (accessed on 5 February 2022).
- A Single-Centre, Randomised, Double-Blind, Placebo-Controlled, Four Way Crossover Phase I Study to Investigate the Effect on QT/QTc Interval of Ceftazidime NXL104 or Ceftaroline Fosamil NXL104, Compared with Placebo, Using Moxifloxacin (Avelox®) as a Positive Control, in Healthy Male Volunteers. Available online: https://clinicaltrials.gov/ct2/show/NCT01290900 (accessed on 5 February 2022).
- Esposito, S.; Carrothers, T.J.; Riccobene, T.; Stone, G.G.; Kantecki, M. Ceftaroline Fosamil for Treatment of Pediatric Complicated Skin and Soft Tissue Infections and Community-Acquired Pneumonia. Paediatr. Drugs 2021, 23, 549–563. [Google Scholar] [CrossRef] [PubMed]
- Pani, A.; Colombo, F.; Agnelli, F.; Frantellizzi, V.; Baratta, F.; Pastori, D.; Scaglione, F. Off-Label Use of Ceftaroline Fosamil: A Systematic Review. Int. J. Antimicrob. Agents 2019, 54, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Kalaria, S.; Williford, S.; Guo, D.; Shu, Y.; Medlin, C.; Li, M.; Yeung, S.Y.A.; Ali, F.; Jean, W.; Gopalakrishnan, M.; et al. Optimizing Ceftaroline Dosing in Critically Ill Patients Undergoing Continuous Renal Replacement Therapy. Pharmacotherapy 2021, 41, 205–211. [Google Scholar] [CrossRef]
- Murano, K.; Yamanaka, T.; Toda, A.; Ohki, H.; Okuda, S.; Kawabata, K.; Hatano, K.; Takeda, S.; Akamatsu, H.; Itoh, K.; et al. Structural Requirements for the Stability of Novel Cephalosporins to AmpC Beta-Lactamase Based on 3D-Structure. Bioorg. Med. Chem. 2008, 16, 2261–2275. [Google Scholar] [CrossRef]
- Sader, H.S.; Rhomberg, P.R.; Farrell, D.J.; Jones, R.N. Antimicrobial Activity of CXA-101, a Novel Cephalosporin Tested in Combination with Tazobactam against Enterobacteriaceae, Pseudomonas Aeruginosa, and Bacteroides Fragilis Strains Having Various Resistance Phenotypes. Antimicrob. Agents Chemother. 2011, 55, 2390–2394. [Google Scholar] [CrossRef]
- Giani, T.; Arena, F.; Pollini, S.; Di Pilato, V.; D’Andrea, M.M.; Henrici De Angelis, L.; Bassetti, M.; Rossolini, G.M. Pseudomonas Aeruginosa Working Group Italian Nationwide Survey on Pseudomonas Aeruginosa from Invasive Infections: Activity of Ceftolozane/tazobactam and Comparators, and Molecular Epidemiology of Carbapenemase Producers. J. Antimicrob. Chemother. 2018, 73, 664–671. [Google Scholar] [CrossRef]
- Cabot, G.; Bruchmann, S.; Mulet, X.; Zamorano, L.; Moyà, B.; Juan, C.; Haussler, S.; Oliver, A. Pseudomonas Aeruginosa Ceftolozane-Tazobactam Resistance Development Requires Multiple Mutations Leading to Overexpression and Structural Modification of AmpC. Antimicrob. Agents Chemother. 2014, 58, 3091–3099. [Google Scholar] [CrossRef]
- Sader, H.S.; Farrell, D.J.; Flamm, R.K.; Jones, R.N. Ceftolozane/tazobactam Activity Tested against Aerobic Gram-Negative Organisms Isolated from Intra-Abdominal and Urinary Tract Infections in European and United States Hospitals (2012). J. Infect. 2014, 69, 266–277. [Google Scholar] [CrossRef]
- Solomkin, J.; Hershberger, E.; Miller, B.; Popejoy, M.; Friedland, I.; Steenbergen, J.; Yoon, M.; Collins, S.; Yuan, G.; Barie, P.S.; et al. Ceftolozane/Tazobactam Plus Metronidazole for Complicated Intra-Abdominal Infections in an Era of Multidrug Resistance: Results from a Randomized, Double-Blind, Phase 3 Trial (ASPECT-cIAI). Clin. Infect. Dis. 2015, 60, 1462–1471. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Castaldo, N.; Cattelan, A.; Mussini, C.; Righi, E.; Tascini, C.; Menichetti, F.; Mastroianni, C.M.; Tumbarello, M.; Grossi, P.; et al. Ceftolozane/tazobactam for the Treatment of Serious Pseudomonas Aeruginosa Infections: A Multicentre Nationwide Clinical Experience. Int. J. Antimicrob. Agents 2019, 53, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Vena, A.; Giacobbe, D.R.; Mussini, C.; Cattelan, A.; Bassetti, M. Ceftabuse Study Group Clinical Efficacy of Ceftolozane-Tazobactam Versus Other Active Agents for the Treatment of Bacteremia and Nosocomial Pneumonia due to Drug-Resistant Pseudomonas Aeruginosa. Clin. Infect. Dis. 2020, 71, 1799–1801. [Google Scholar] [CrossRef] [PubMed]
- Maraolo, A.E.; Mazzitelli, M.; Trecarichi, E.M.; Buonomo, A.R.; Torti, C.; Gentile, I. Ceftolozane/tazobactam for Difficult-to-Treat Pseudomonas Aeruginosa Infections: A Systematic Review of Its Efficacy and Safety for off-Label Indications. Int. J. Antimicrob. Agents 2020, 55, 105891. [Google Scholar] [CrossRef]
- Chandorkar, G.; Huntington, J.A.; Gotfried, M.H.; Rodvold, K.A.; Umeh, O. Intrapulmonary Penetration of Ceftolozane/tazobactam and Piperacillin/tazobactam in Healthy Adult Subjects. J. Antimicrob. Chemother. 2012, 67, 2463–2469. [Google Scholar] [CrossRef] [PubMed]
- Caro, L.; Nicolau, D.P.; De Waele, J.J.; Kuti, J.L.; Larson, K.B.; Gadzicki, E.; Yu, B.; Zeng, Z.; Adedoyin, A.; Rhee, E.G. Lung Penetration, Bronchopulmonary Pharmacokinetic/pharmacodynamic Profile and Safety of 3 G of Ceftolozane/tazobactam Administered to Ventilated, Critically Ill Patients with Pneumonia. J. Antimicrob. Chemother. 2020, 75, 1546–1553. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Patel, Y.T.; Fiedler-Kelly, J.; Feng, H.-P.; Bruno, C.J.; Gao, W. Population Pharmacokinetic Analysis for Plasma and Epithelial Lining Fluid Ceftolozane/Tazobactam Concentrations in Patients with Ventilated Nosocomial Pneumonia. J. Clin. Pharmacol. 2021, 61, 254–268. [Google Scholar] [CrossRef]
- Ang, J.Y.; Arrieta, A.; Bradley, J.S.; Zhang, Z.; Yu, B.; Rizk, M.L.; Johnson, M.G.; Rhee, E.G. Ceftolozane/Tazobactam in Neonates and Young Infants: The Challenges of Collecting Pharmacokinetics and Safety Data in This Vulnerable Patient Population. Am. J. Perinatol. 2021, 38, 804–809. [Google Scholar] [CrossRef]
- Bradley, J.S.; Ang, J.Y.; Arrieta, A.C.; Larson, K.B.; Rizk, M.L.; Caro, L.; Yang, S.; Yu, B.; Johnson, M.G.; Rhee, E.G. Pharmacokinetics and Safety of Single Intravenous Doses of Ceftolozane/Tazobactam in Children with Proven or Suspected Gram-Negative Infection. Pediatr. Infect. Dis. J. 2018, 37, 1130–1136. [Google Scholar] [CrossRef]
- Sime, F.B.; Lassig-Smith, M.; Starr, T.; Stuart, J.; Pandey, S.; Parker, S.L.; Wallis, S.C.; Lipman, J.; Roberts, J.A. Population Pharmacokinetics of Unbound Ceftolozane and Tazobactam in Critically Ill Patients without Renal Dysfunction. Antimicrob. Agents Chemother. 2019, 63, e01265-19. [Google Scholar] [CrossRef]
- Tooke, C.L.; Hinchliffe, P.; Bragginton, E.C.; Colenso, C.K.; Hirvonen, V.H.A.; Takebayashi, Y.; Spencer, J. β-Lactamases and β-Lactamase Inhibitors in the 21st Century. J. Mol. Biol. 2019, 431, 3472–3500. [Google Scholar] [CrossRef] [PubMed]
- Di Bella, S.; Giacobbe, D.R.; Maraolo, A.E.; Viaggi, V.; Luzzati, R.; Bassetti, M.; Luzzaro, F.; Principe, L. Resistance to Ceftazidime/avibactam in Infections and Colonisations by KPC-Producing Enterobacterales: A Systematic Review of Observational Clinical Studies. J. Glob. Antimicrob. Resist. 2021, 25, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Humphries, R.M.; Hindler, J.A.; Wong-Beringer, A.; Miller, S.A. Activity of Ceftolozane-Tazobactam and Ceftazidime-Avibactam against Beta-Lactam-Resistant Pseudomonas Aeruginosa Isolates. Antimicrob. Agents Chemother. 2017, 61, e01858-17. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.; Hemarajata, P.; Sun, D.; Rubio-Aparicio, D.; Tsivkovski, R.; Yang, S.; Sebra, R.; Kasarskis, A.; Nguyen, H.; Hanson, B.M.; et al. Resistance to Ceftazidime-Avibactam Is Due to Transposition of KPC in a Porin-Deficient Strain of Klebsiella Pneumoniae with Increased Efflux Activity. Antimicrob. Agents Chemother. 2017, 61, e00989-17. [Google Scholar] [CrossRef]
- Lee, M.; Abbey, T.; Biagi, M.; Wenzler, E. Activity of Aztreonam in Combination with Ceftazidime-Avibactam against Serine- and Metallo-β-Lactamase-Producing Pseudomonas Aeruginosa. Diagn. Microbiol. Infect. Dis. 2021, 99, 115227. [Google Scholar] [CrossRef]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 10.0. 2020. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_12.0_Breakpoint_Tables.pdf (accessed on 6 February 2022).
- Mazuski, J.E.; Gasink, L.B.; Armstrong, J.; Broadhurst, H.; Stone, G.G.; Rank, D.; Llorens, L.; Newell, P.; Pachl, J. Efficacy and Safety of Ceftazidime-Avibactam Plus Metronidazole Versus Meropenem in the Treatment of Complicated Intra-Abdominal Infection: Results from a Randomized, Controlled, Double-Blind, Phase 3 Program. Clin. Infect. Dis. 2016, 62, 1380–1389. [Google Scholar]
- Carmeli, Y.; Armstrong, J.; Laud, P.J.; Newell, P.; Stone, G.; Wardman, A.; Gasink, L.B. Ceftazidime-Avibactam or Best Available Therapy in Patients with Ceftazidime-Resistant Enterobacteriaceae and Pseudomonas Aeruginosa Complicated Urinary Tract Infections or Complicated Intra-Abdominal Infections (REPRISE): A Randomised, Pathogen-Directed, Phase 3 Study. Lancet Infect. Dis. 2016, 16, 661–673. [Google Scholar]
- Torres, A.; Rank, D.; Melnick, D.; Rekeda, L.; Chen, X.; Riccobene, T.; Critchley, I.A.; Lakkis, H.D.; Taylor, D.; Talley, A.K. Randomized Trial of Ceftazidime-Avibactam vs Meropenem for Treatment of Hospital-Acquired and Ventilator-Associated Bacterial Pneumonia (REPROVE): Analyses per US FDA-Specified End Points. Open Forum Infect. Dis. 2019, 6, ofz149. [Google Scholar] [CrossRef]
- Mendes, R.E.; Castanheira, M.; Woosley, L.N.; Stone, G.G.; Bradford, P.A.; Flamm, R.K. Molecular β-Lactamase Characterization of Gram-Negative Pathogens Recovered from Patients Enrolled in the Ceftazidime-Avibactam Phase 3 Trials (RECAPTURE 1 and 2) for Complicated Urinary Tract Infections: Efficacies Analysed against Susceptible and Resistant Subsets. Int. J. Antimicrob. Agents 2018, 52, 287–292. [Google Scholar]
- Sousa, A.; Pérez-Rodríguez, M.T.; Soto, A.; Rodríguez, L.; Pérez-Landeiro, A.; Martínez-Lamas, L.; Nodar, A.; Crespo, M. Effectiveness of Ceftazidime/avibactam as Salvage Therapy for Treatment of Infections due to OXA-48 Carbapenemase-Producing Enterobacteriaceae. J. Antimicrob. Chemother. 2018, 73, 3170–3175. [Google Scholar] [CrossRef]
- Tumbarello, M.; Trecarichi, E.M.; Corona, A.; De Rosa, F.G.; Bassetti, M.; Mussini, C.; Menichetti, F.; Viscoli, C.; Campoli, C.; Venditti, M.; et al. Efficacy of Ceftazidime-Avibactam Salvage Therapy in Patients with Infections Caused by Klebsiella Pneumoniae Carbapenemase-Producing K. Pneumoniae. Clin. Infect. Dis. 2019, 68, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Tumbarello, M.; Raffaelli, F.; Giannella, M.; Mantengoli, E.; Mularoni, A.; Venditti, M.; De Rosa, F.G.; Sarmati, L.; Bassetti, M.; Brindicci, G.; et al. Ceftazidime-Avibactam Use for Klebsiella Pneumoniae Carbapenemase-Producing K. Pneumoniae Infections: A Retrospective Observational Multicenter Study. Clin. Infect. Dis. 2021, 73, 1664–1676. [Google Scholar] [CrossRef] [PubMed]
- Shields, R.K.; Nguyen, M.H.; Chen, L.; Press, E.G.; Potoski, B.A.; Marini, R.V.; Doi, Y.; Kreiswirth, B.N.; Clancy, C.J. Ceftazidime-Avibactam Is Superior to Other Treatment Regimens against Carbapenem-Resistant Klebsiella Pneumoniae Bacteremia. Antimicrob. Agents Chemother. 2017, 61, e00883-17. [Google Scholar] [CrossRef] [PubMed]
- Fiore, M.; Alfieri, A.; Di Franco, S.; Pace, M.C.; Simeon, V.; Ingoglia, G.; Cortegiani, A. Ceftazidime-Avibactam Combination Therapy Compared to Ceftazidime-Avibactam Monotherapy for the Treatment of Severe Infections Due to Carbapenem-Resistant Pathogens: A Systematic Review and Network Meta-Analysis. Antibiotics 2020, 9, 388. [Google Scholar] [CrossRef]
- Onorato, L.; Di Caprio, G.; Signoriello, S.; Coppola, N. Efficacy of Ceftazidime/avibactam in Monotherapy or Combination Therapy against Carbapenem-Resistant Gram-Negative Bacteria: A Meta-Analysis. Int. J. Antimicrob. Agents 2019, 54, 735–740. [Google Scholar] [CrossRef]
- Li, J.; Lovern, M.; Green, M.L.; Chiu, J.; Zhou, D.; Comisar, C.; Xiong, Y.; Hing, J.; MacPherson, M.; Wright, J.G.; et al. Ceftazidime-Avibactam Population Pharmacokinetic Modeling and Pharmacodynamic Target Attainment Across Adult Indications and Patient Subgroups. Clin. Transl. Sci. 2019, 12, 151–163. [Google Scholar] [CrossRef]
- Soriano, A.; Carmeli, Y.; Omrani, A.S.; Moore, L.S.P.; Tawadrous, M.; Irani, P. Ceftazidime-Avibactam for the Treatment of Serious Gram-Negative Infections with Limited Treatment Options: A Systematic Literature Review. Infect. Dis. Ther. 2021, 10, 1989–2034. [Google Scholar] [CrossRef]
- Mittal, J.; Szymczak, W.A.; Guo, Y.; Levi, M.H.; Chen, L.; Kreiswirth, B.N.; Riska, P.F.; Nori, P. Two for the Price of One: Emerging Carbapenemases in a Returning Traveller to New York City. BMJ Case Rep. 2018, 2018, bcr2018225440. [Google Scholar] [CrossRef]
- Cairns, K.A.; Hall, V.; Martin, G.E.; Griffin, D.W.J.; Stewart, J.D.; Khan, S.F.; Abbott, I.J.; Meher-Homji, Z.; Morrissey, C.O.; Sia, C.; et al. Treatment of Invasive IMP-4 Enterobacter Cloacae Infection in Transplant Recipients Using Ceftazidime/avibactam with Aztreonam: A Case Series and Literature Review. Transpl. Infect. Dis. 2021, 23, e13510. [Google Scholar] [CrossRef]
- Alghoribi, M.F.; Alqurashi, M.; Okdah, L.; Alalwan, B.; AlHebaishi, Y.S.; Almalki, A.; Alzayer, M.A.; Alswaji, A.A.; Doumith, M.; Barry, M. Successful Treatment of Infective Endocarditis due to Pandrug-Resistant Klebsiella Pneumoniae with Ceftazidime-Avibactam and Aztreonam. Sci. Rep. 2021, 11, 9684. [Google Scholar] [CrossRef]
- Shaw, E.; Rombauts, A.; Tubau, F.; Padullés, A.; Càmara, J.; Lozano, T.; Cobo-Sacristán, S.; Sabe, N.; Grau, I.; Rigo-Bonnin, R.; et al. Clinical Outcomes after Combination Treatment with Ceftazidime/avibactam and Aztreonam for NDM-1/OXA-48/CTX-M-15-Producing Klebsiella Pneumoniae Infection. J. Antimicrob. Chemother. 2018, 73, 1104–1106. [Google Scholar] [CrossRef] [PubMed]
- Stewart, J.; Snoeyenbos Newman, G.; Jain, R.; Bryan, A.; Berger, H.; Montenovo, M.; Bakthavatsalam, R.; Kling, C.E.; Sibulesky, L.; Shalhub, S.; et al. Transplant Tourism Complicated by Life-Threatening New Delhi Metallo-β-Lactamase-1 Infection. Am. J. Transplant. 2019, 19, 1224–1228. [Google Scholar] [CrossRef]
- Bulitta, J.B.; Landersdorfer, C.B.; Hüttner, S.J.; Drusano, G.L.; Kinzig, M.; Holzgrabe, U.; Stephan, U.; Sörgel, F. Population Pharmacokinetic Comparison and Pharmacodynamic Breakpoints of Ceftazidime in Cystic Fibrosis Patients and Healthy Volunteers. Antimicrob. Agents Chemother. 2010, 54, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Zhanel, G.G.; Lawrence, C.K.; Adam, H.; Schweizer, F.; Zelenitsky, S.; Zhanel, M.; Lagacé-Wiens, P.R.S.; Walkty, A.; Denisuik, A.; Golden, A.; et al. Imipenem-Relebactam and Meropenem-Vaborbactam: Two Novel Carbapenem-β-Lactamase Inhibitor Combinations. Drugs 2018, 78, 65–98. [Google Scholar] [CrossRef] [PubMed]
- Yahav, D.; Giske, C.G.; Grāmatniece, A.; Abodakpi, H.; Tam, V.H.; Leibovici, L. New β-Lactam-β-Lactamase Inhibitor Combinations. Clin. Microbiol. Rev. 2020, 34, e00115-20. [Google Scholar] [CrossRef] [PubMed]
- Lob, S.H.; Hackel, M.A.; Kazmierczak, K.M.; Young, K.; Motyl, M.R.; Karlowsky, J.A.; Sahm, D.F. In Vitro Activity of Imipenem-Relebactam against Gram-Negative ESKAPE Pathogens Isolated by Clinical Laboratories in the United States in 2015 (Results from the SMART Global Surveillance Program). Antimicrob. Agents Chemother. 2017, 61, e02209-16. [Google Scholar] [CrossRef]
- Tooke, C.L.; Hinchliffe, P.; Lang, P.A.; Mulholland, A.J.; Brem, J.; Schofield, C.J.; Spencer, J. Molecular Basis of Class A β-Lactamase Inhibition by Relebactam. Antimicrob. Agents Chemother. 2019, 63, e00564-19. [Google Scholar] [CrossRef]
- Motsch, J.; Murta de Oliveira, C.; Stus, V.; Köksal, I.; Lyulko, O.; Boucher, H.W.; Kaye, K.S.; File, T.M.; Brown, M.L.; Khan, I.; et al. RESTORE-IMI 1: A Multicenter, Randomized, Double-Blind Trial Comparing Efficacy and Safety of Imipenem/Relebactam vs Colistin Plus Imipenem in Patients with Imipenem-Nonsusceptible Bacterial Infections. Clin. Infect. Dis. 2020, 70, 1799–1808. [Google Scholar] [CrossRef]
- Titov, I.; Wunderink, R.G.; Roquilly, A.; Rodríguez Gonzalez, D.; David-Wang, A.; Boucher, H.W.; Kaye, K.S.; Losada, M.C.; Du, J.; Tipping, R.; et al. A Randomized, Double-Blind, Multicenter Trial Comparing Efficacy and Safety of Imipenem/Cilastatin/Relebactam Versus Piperacillin/Tazobactam in Adults with Hospital-Acquired or Ventilator-Associated Bacterial Pneumonia (RESTORE-IMI 2 Study). Clin. Infect. Dis. 2021, 73, e4539–e4548. [Google Scholar] [CrossRef]
- Kohno, S.; Bando, H.; Yoneyama, F.; Kikukawa, H.; Kawahara, K.; Shirakawa, M.; Aoyama, N.; Brown, M.; Paschke, A.; Takase, A. The Safety and Efficacy of Relebactam/imipenem/cilastatin in Japanese Patients with Complicated Intra-Abdominal Infection or Complicated Urinary Tract Infection: A Multicenter, Open-Label, Noncomparative Phase 3 Study. J. Infect. Chemother. 2021, 27, 262–270. [Google Scholar] [CrossRef]
- Bhagunde, P.; Patel, P.; Lala, M.; Watson, K.; Copalu, W.; Xu, M.; Kulkarni, P.; Young, K.; Rizk, M.L. Population Pharmacokinetic Analysis for Imipenem-Relebactam in Healthy Volunteers and Patients with Bacterial Infections. CPT Pharmacomet. Syst. Pharmacol. 2019, 8, 748–758. [Google Scholar] [CrossRef] [PubMed]
- Bhagunde, P.; Colon-Gonzalez, F.; Liu, Y.; Wu, J.; Xu, S.S.; Garrett, G.; Jumes, P.; Lasseter, K.; Marbury, T.; Rizk, M.L.; et al. Impact of Renal Impairment and Human Organic Anion Transporter Inhibition on Pharmacokinetics, Safety and Tolerability of Relebactam Combined with Imipenem and Cilastatin. Br. J. Clin. Pharmacol. 2020, 86, 944–957. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.D.; Taracila, M.A.; Good, C.E.; Bajaksouzian, S.; Rojas, L.J.; Van Duin, D.; Kreiswirth, B.N.; Jacobs, M.R.; Haldimann, A.; Papp-Wallace, K.M.; et al. Nacubactam Enhances Meropenem Activity against Carbapenem-Resistant Klebsiella Pneumoniae Producing KPC. Antimicrob. Agents Chemother. 2019, 63, e00432-19. [Google Scholar] [CrossRef] [PubMed]
- Monogue, M.L.; Giovagnoli, S.; Bissantz, C.; Zampaloni, C.; Nicolau, D.P. Efficacy of Meropenem with a Novel Non-β-Lactam-β-Lactamase Inhibitor, Nacubactam, against Gram-Negative Organisms Exhibiting Various Resistance Mechanisms in a Murine Complicated Urinary Tract Infection Model. Antimicrob. Agents Chemother. 2018, 62, e025996-17. [Google Scholar] [CrossRef]
- Asempa, T.E.; Motos, A.; Abdelraouf, K.; Bissantz, C.; Zampaloni, C.; Nicolau, D.P. Meropenem–nacubactam Activity against AmpC-Overproducing and KPC-Expressing Pseudomonas Aeruginosa in a Neutropenic Murine Lung Infection Model. Int. J. Antimicrob. Agents 2020, 55, 105838. [Google Scholar] [CrossRef] [PubMed]
- Davies, D.T.; Leiris, S.; Zalacain, M.; Sprynski, N.; Castandet, J.; Bousquet, J.; Lozano, C.; Llanos, A.; Alibaud, L.; Vasa, S.; et al. Discovery of ANT3310, a Novel Broad-Spectrum Serine β-Lactamase Inhibitor of the Diazabicyclooctane Class, Which Strongly Potentiates Meropenem Activity against Carbapenem-Resistant Enterobacterales and Acinetobacter baumannii. J. Med. Chem. 2020, 63, 15802–15820. [Google Scholar] [CrossRef]
- A Study to Investigate the Pharmacokinetics of RO7079901 and Meropenem in Participants with a Complicated Urinary Tract Infection. Available online: https://clinicaltrials.gov/ct2/show/NCT03174795 (accessed on 5 February 2022).
- A Study to Investigate the Intrapulmonary Lung Penetration of Nacubactam in Healthy Participants. Available online: https://clinicaltrials.gov/ct2/show/NCT03182504 (accessed on 24 February 2022).
- Shoulders, B.R.; Casapao, A.M.; Venugopalan, V. An Update on Existing and Emerging Data for Meropenem-Vaborbactam. Clin. Ther. 2020, 42, 692–702. [Google Scholar] [CrossRef]
- Lomovskaya, O.; Sun, D.; Rubio-Aparicio, D.; Nelson, K.; Tsivkovski, R.; Griffith, D.C.; Dudley, M.N. Vaborbactam: Spectrum of Beta-Lactamase Inhibition and Impact of Resistance Mechanisms on Activity in Enterobacteriaceae. Antimicrob. Agents Chemother. 2017, 61, e01443-17. [Google Scholar] [CrossRef]
- Hecker, S.J.; Reddy, K.R.; Totrov, M.; Hirst, G.C.; Lomovskaya, O.; Griffith, D.C.; King, P.; Tsivkovski, R.; Sun, D.; Sabet, M.; et al. Discovery of a Cyclic Boronic Acid β-Lactamase Inhibitor (RPX7009) with Utility vs Class A Serine Carbapenemases. J. Med. Chem. 2015, 58, 3682–3692. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Huband, M.D.; Mendes, R.E.; Flamm, R.K.; Castanheira, M. In Vitro Activity of Meropenem/vaborbactam and Characterisation of Carbapenem Resistance Mechanisms among Carbapenem-Resistant Enterobacteriaceae from the 2015 Meropenem/vaborbactam Surveillance Programme. Int. J. Antimicrob. Agents 2018, 52, 144–150. [Google Scholar] [CrossRef]
- Dulyayangkul, P.; Douglas, E.J.A.; Lastovka, F.; Avison, M.B. Resistance to Ceftazidime/Avibactam plus Meropenem/Vaborbactam When Both Are Used Together Is Achieved in Four Steps in Metallo-β-Lactamase-Negative Klebsiella Pneumoniae. Antimicrob. Agents Chemother. 2020, 64, 00409-20. [Google Scholar] [CrossRef]
- Gaibani, P.; Lombardo, D.; Bussini, L.; Bovo, F.; Munari, B.; Giannella, M.; Bartoletti, M.; Viale, P.; Lazzarotto, T.; Ambretti, S. Epidemiology of Meropenem/Vaborbactam Resistance in KPC-Producing Causing Bloodstream Infections in Northern Italy, 2018. Antibiotics 2021, 10, 536. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Rubio-Aparicio, D.; Nelson, K.; Dudley, M.N.; Lomovskaya, O. Meropenem-Vaborbactam Resistance Selection, Resistance Prevention, and Molecular Mechanisms in Mutants of KPC-Producing Klebsiella Pneumoniae. Antimicrob. Agents Chemother. 2017, 61, e01694-17. [Google Scholar] [CrossRef] [PubMed]
- Wilson, W.R.; Kline, E.G.; Jones, C.E.; Morder, K.T.; Mettus, R.T.; Doi, Y.; Nguyen, M.H.; Clancy, C.J.; Shields, R.K. Effects of KPC Variant and Porin Genotype on the Activity of Meropenem-Vaborbactam against Carbapenem-Resistant. Antimicrob. Agents Chemother. 2019, 63, e02048-18. [Google Scholar] [CrossRef]
- Novelli, A.; Del Giacomo, P.; Rossolini, G.M.; Tumbarello, M. Meropenem/vaborbactam: A next Generation β-Lactam β-Lactamase Inhibitor Combination. Expert Rev. Anti. Infect. Ther. 2020, 18, 643–655. [Google Scholar] [CrossRef] [PubMed]
- Wunderink, R.G.; Giamarellos-Bourboulis, E.J.; Rahav, G.; Mathers, A.J.; Bassetti, M.; Vazquez, J.; Cornely, O.A.; Solomkin, J.; Bhowmick, T.; Bishara, J.; et al. Effect and Safety of Meropenem-Vaborbactam versus Best-Available Therapy in Patients with Carbapenem-Resistant Enterobacteriaceae Infections: The TANGO II Randomized Clinical Trial. Infect. Dis. Ther. 2018, 7, 439–455. [Google Scholar] [CrossRef] [PubMed]
- A Study of Meropenem-Vaborbactam Versus Piperacillin/Tazobactam in Participants with Hospital-Acquired and Ventilator-Associated Bacterial Pneumonia—Full Text View. ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT03006679 (accessed on 6 February 2022).
- Shields, R.K.; McCreary, E.K.; Marini, R.V.; Kline, E.G.; Jones, C.E.; Hao, B.; Chen, L.; Kreiswirth, B.N.; Doi, Y.; Clancy, C.J.; et al. Early Experience with Meropenem-Vaborbactam for Treatment of Carbapenem-Resistant Enterobacteriaceae Infections. Clin. Infect. Dis. 2020, 71, 667–671. [Google Scholar] [CrossRef] [PubMed]
- Alosaimy, S.; Jorgensen, S.C.J.; Lagnf, A.M.; Melvin, S.; Mynatt, R.P.; Carlson, T.J.; Garey, K.W.; Allen, D.; Venugopalan, V.; Veve, M.; et al. Real-World Multicenter Analysis of Clinical Outcomes and Safety of Meropenem-Vaborbactam in Patients Treated for Serious Gram-Negative Bacterial Infections. Open Forum Infect. Dis. 2020, 7, ofaa051. [Google Scholar] [CrossRef]
- Ackley, R.; Roshdy, D.; Meredith, J.; Minor, S.; Anderson, W.E.; Capraro, G.A.; Polk, C. Meropenem-Vaborbactam versus Ceftazidime-Avibactam for Treatment of Carbapenem-Resistant Infections. Antimicrob. Agents Chemother. 2020, 64, e02313-19. [Google Scholar] [CrossRef]
- Athans, V.; Neuner, E.A.; Hassouna, H.; Richter, S.S.; Keller, G.; Castanheira, M.; Brizendine, K.D.; Mathers, A.J. Meropenem-Vaborbactam as Salvage Therapy for Ceftazidime-Avibactam-Resistant Bacteremia and Abscess in a Liver Transplant Recipient. Antimicrob. Agents Chemother. 2019, 63, e01551-18. [Google Scholar] [CrossRef]
- Lee, Y.R.; Baker, N.T. Meropenem-Vaborbactam: A Carbapenem and Beta-Lactamase Inhibitor with Activity against Carbapenem-Resistant Enterobacteriaceae. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1411–1419. [Google Scholar] [CrossRef] [PubMed]
- Griffith, D.C.; Sabet, M.; Tarazi, Z.; Lomovskaya, O.; Dudley, M.N. Pharmacokinetics/Pharmacodynamics of Vaborbactam, a Novel Beta-Lactamase Inhibitor, in Combination with Meropenem. Antimicrob. Agents Chemother. 2019, 63, e01659-18. [Google Scholar] [CrossRef]
- Honeybourne, D. Antibiotic Penetration into Lung Tissues. Thorax 1994, 49, 104–106. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Taccone, F.S.; Laterre, P.-F.; Dugernier, T.; Spapen, H.; Delattre, I.; Wittebole, X.; De Backer, D.; Layeux, B.; Wallemacq, P.; Vincent, J.-L.; et al. Insufficient β-Lactam Concentrations in the Early Phase of Severe Sepsis and Septic Shock. Crit. Care 2010, 14, R126. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.A.; Kirkpatrick, C.M.J.; Lipman, J. Monte Carlo Simulations: Maximizing Antibiotic Pharmacokinetic Data to Optimize Clinical Practice for Critically Ill Patients. J. Antimicrob. Chemother. 2011, 66, 227–231. [Google Scholar] [CrossRef]
- Turnidge, J.D. The Pharmacodynamics of Beta-Lactams. Clin. Infect. Dis. 1998, 27, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.A.; Paul, S.K.; Akova, M.; Bassetti, M.; De Waele, J.J.; Dimopoulos, G.; Kaukonen, K.-M.; Koulenti, D.; Martin, C.; Montravers, P.; et al. DALI: Defining Antibiotic Levels in Intensive Care Unit Patients: Are Current β-Lactam Antibiotic Doses Sufficient for Critically Ill Patients? Clin. Infect. Dis. 2014, 58, 1072–1083. [Google Scholar] [CrossRef]
- Bauer, K.A.; West, J.E.; O’Brien, J.M.; Goff, D.A. Extended-Infusion Cefepime Reduces Mortality in Patients with Pseudomonas Aeruginosa Infections. Antimicrob. Agents Chemother. 2013, 57, 2907–2912. [Google Scholar] [CrossRef]
- Dulhunty, J.M.; Roberts, J.A.; Davis, J.S.; Webb, S.A.R.; Bellomo, R.; Gomersall, C.; Shirwadkar, C.; Eastwood, G.M.; Myburgh, J.; Paterson, D.L.; et al. Continuous Infusion of Beta-Lactam Antibiotics in Severe Sepsis: A Multicenter Double-Blind, Randomized Controlled Trial. Clin. Infect. Dis. 2013, 56, 236–244. [Google Scholar] [CrossRef]
- Falagas, M.E.; Tansarli, G.S.; Ikawa, K.; Vardakas, K.Z. Clinical Outcomes with Extended or Continuous versus Short-Term Intravenous Infusion of Carbapenems and Piperacillin/tazobactam: A Systematic Review and Meta-Analysis. Clin. Infect. Dis. 2013, 56, 272–282. [Google Scholar]
- Chaudhry, S.B.; Veve, M.P.; Wagner, J.L. Cephalosporins: A Focus on Side Chains and β-Lactam Cross-Reactivity. Pharmacy 2019, 7, 103. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).