Peptide LCGA-17 Attenuates Behavioral and Neurochemical Deficits in Rodent Models of PTSD and Depression
Abstract
:1. Introduction
2. Results
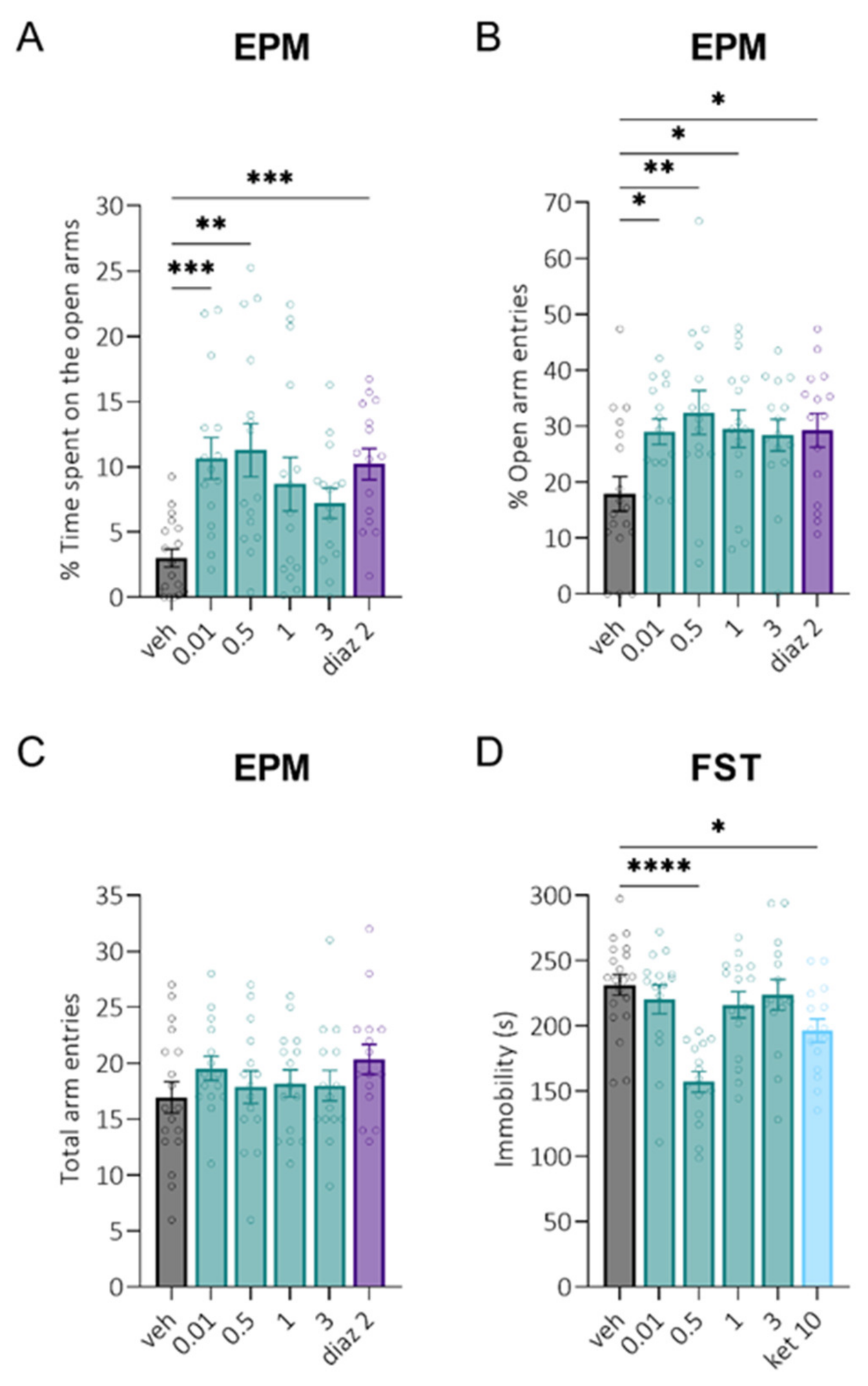
2.1. Dose-Finding Studies in Naïve Rats after Intranasal Administration
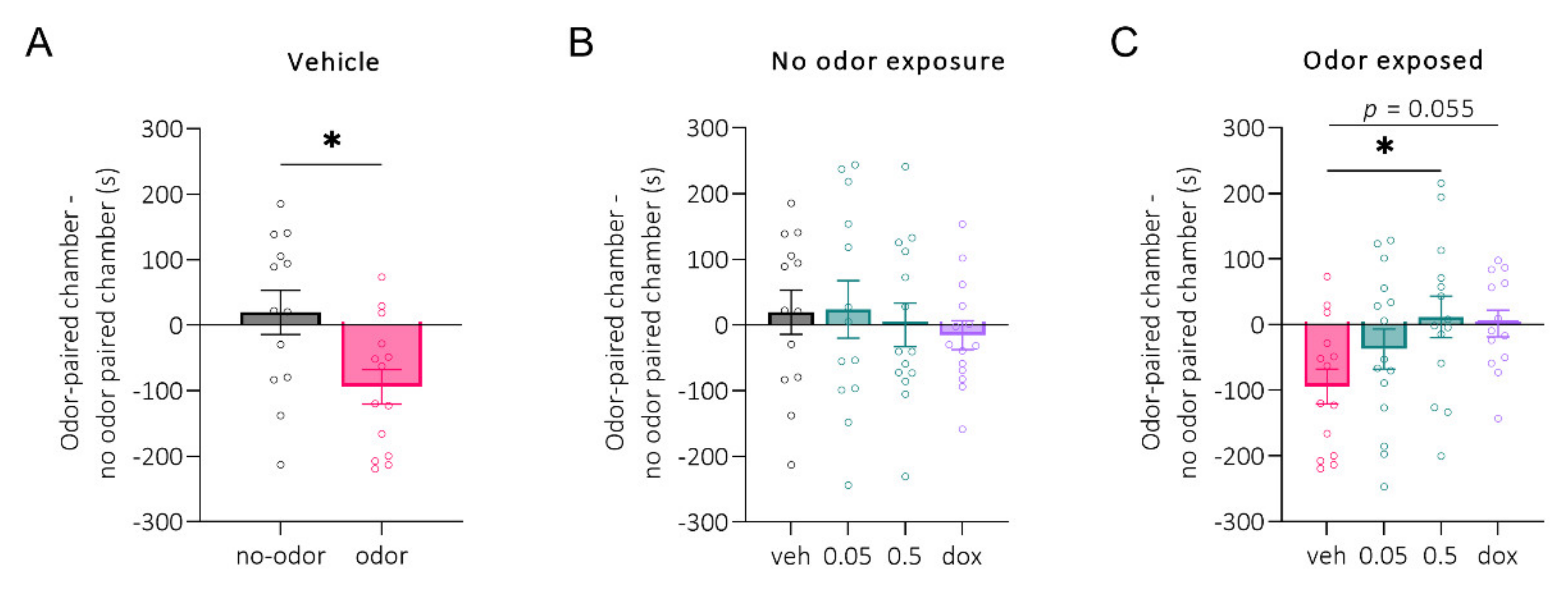
2.2. POCPA Study
2.3. CUS Study
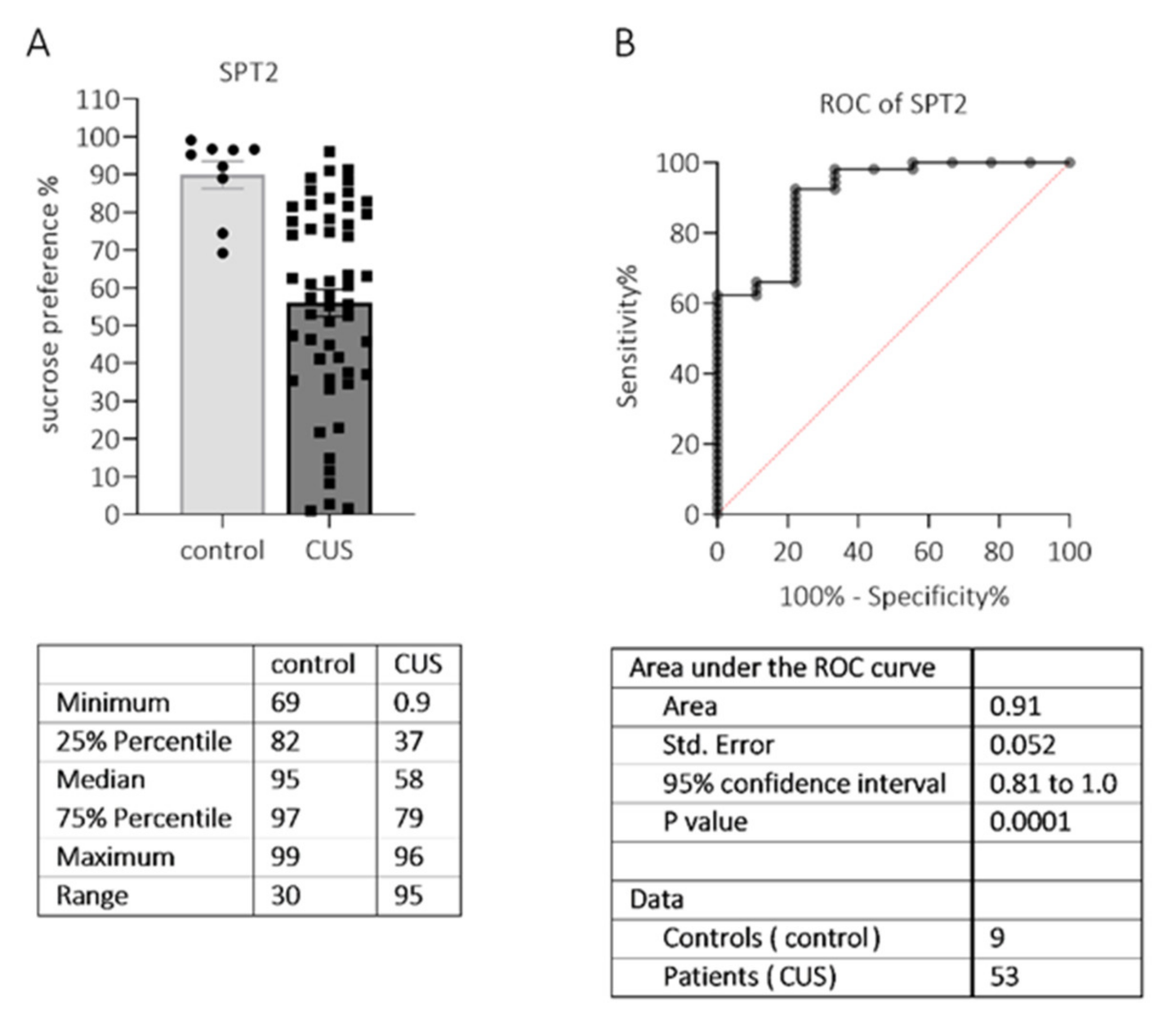
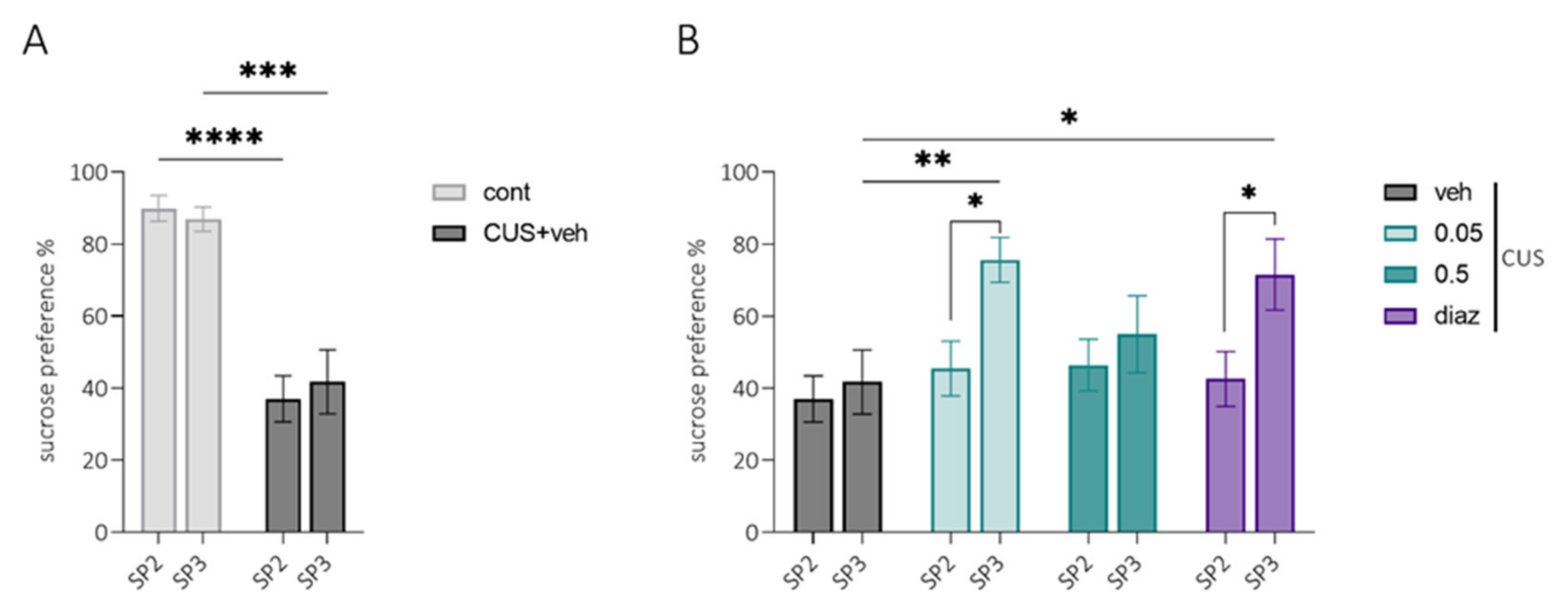
2.3.1. SPT2 (Sucrose Preference Test)
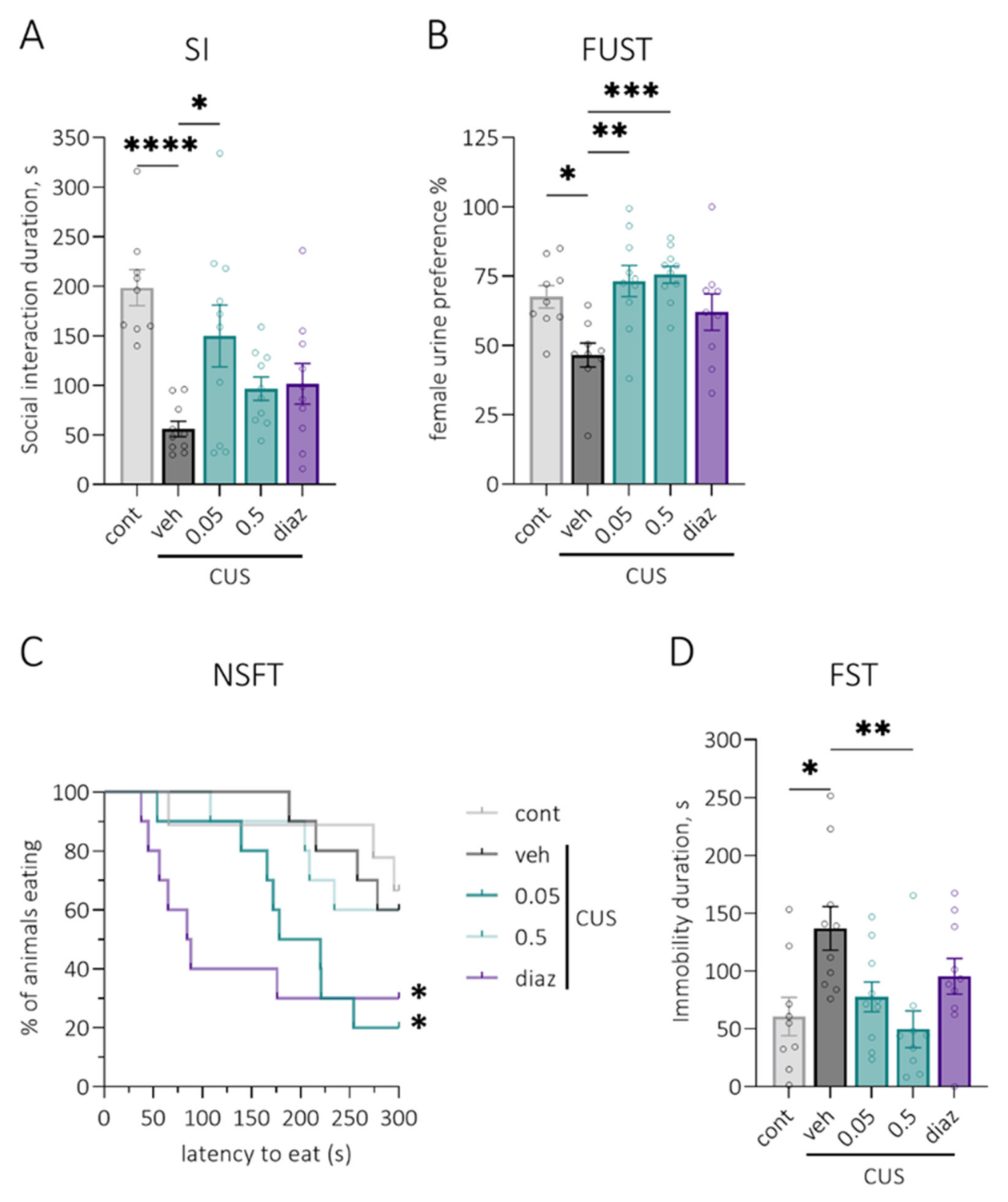
2.3.2. SI (Social Interaction Test)
2.3.3. FUST (Female Urine Sniffing Test)
2.3.4. NSFT (Novelty-Suppressed Feeding Test)
2.3.5. SPT3 (Sucrose Preference Test)
2.3.6. FST (Forced Swim Test)
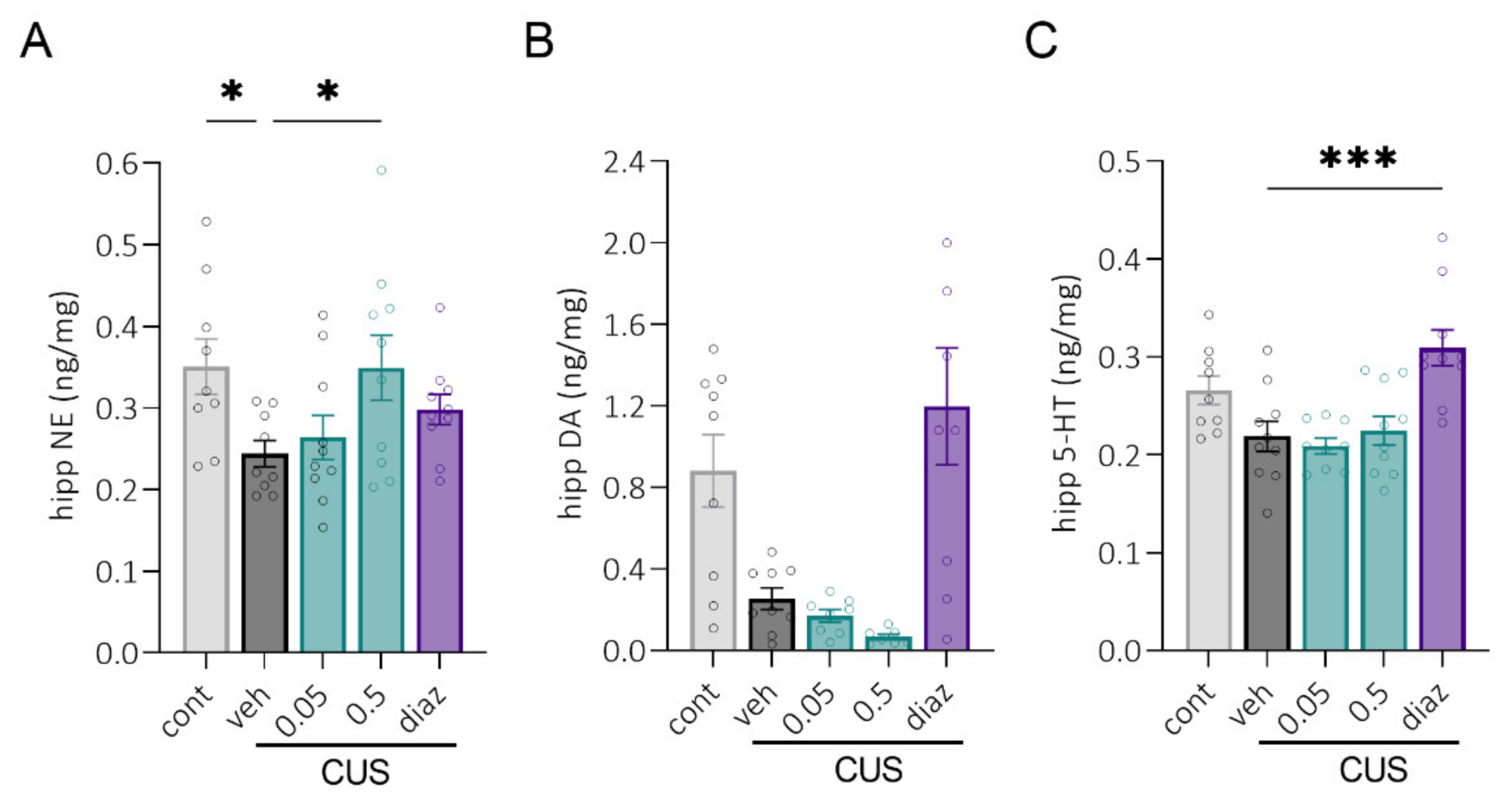
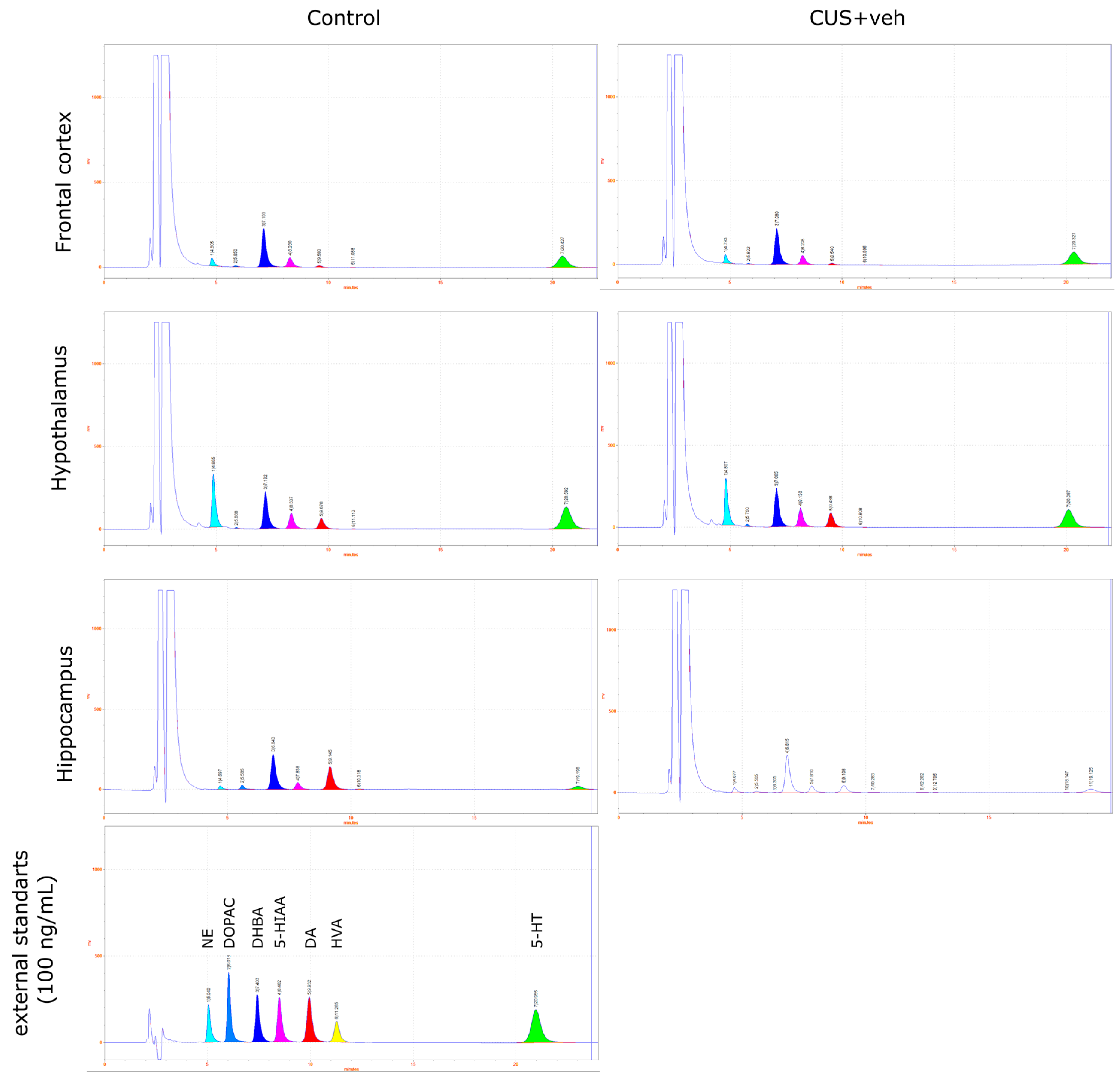
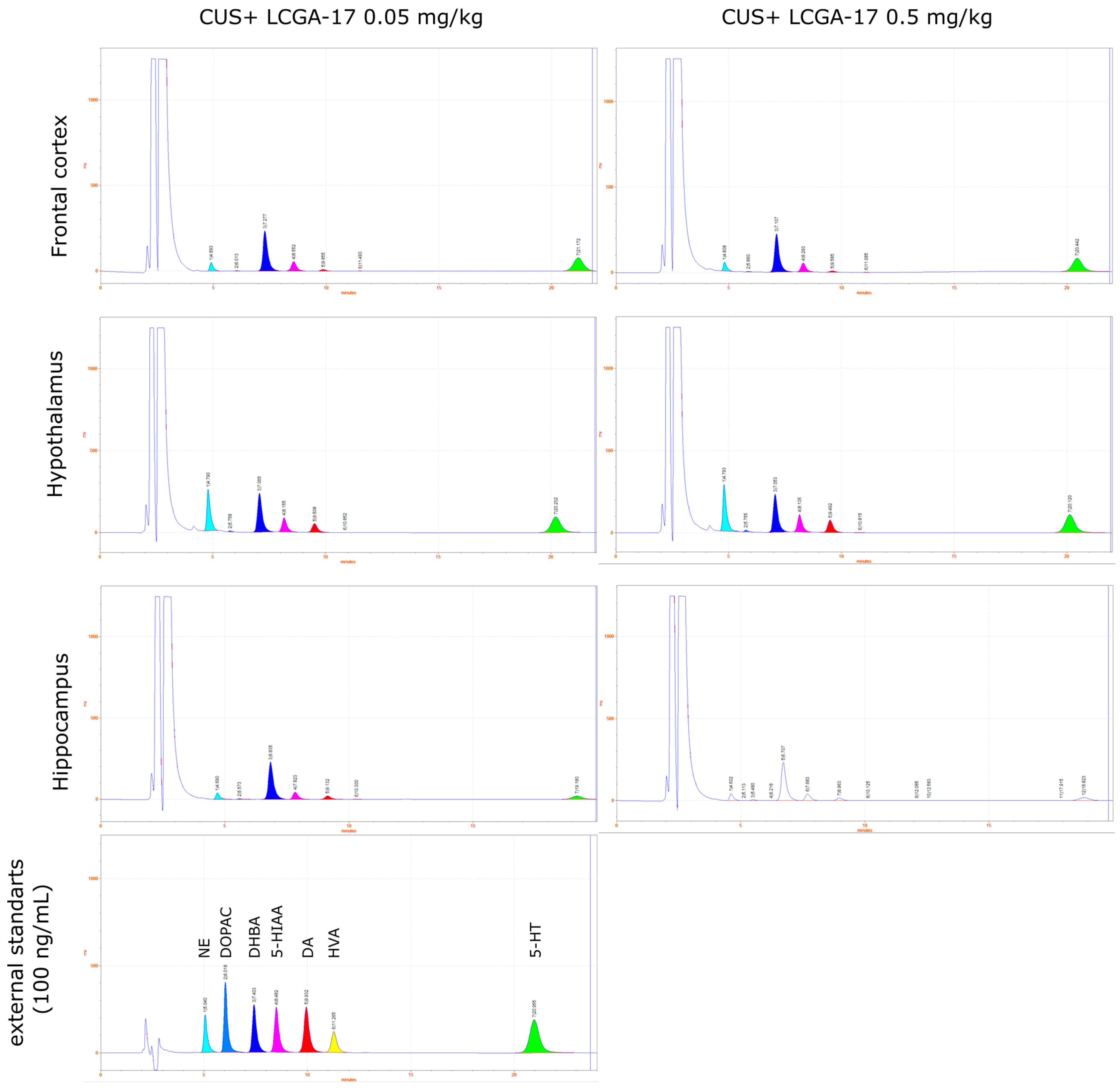
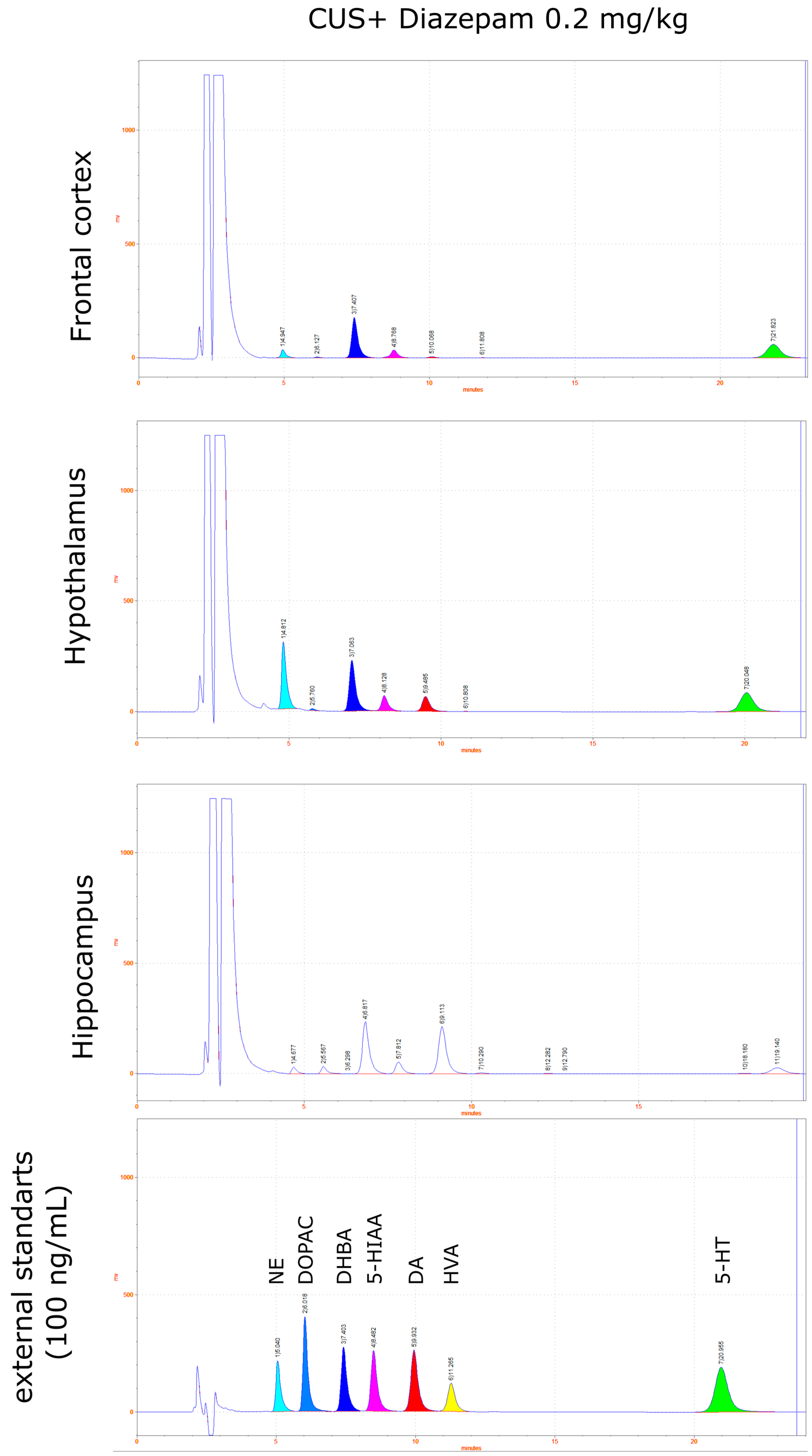
2.4. Biogenic Amines Concentrations after CUS
3. Discussion
4. Materials and Methods
4.1. Animals and Housing
4.2. Drug Treatment
4.2.1. Dose-Finding Study
4.2.2. POCPA Study
4.2.3. CUS Study
4.3. Behavioral Testing
4.4. Predator Odor Conditioned Place Aversion (POCPA) Model
4.5. Chronic Unpredictable Stress (CUS) Model
4.6. Biogenic Amines Assay
4.6.1. Brain Samples Preparation
4.6.2. HPLC Analysis
4.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Christiansen, D.M.; Berke, E.T. Gender- and Sex-Based Contributors to Sex Differences in PTSD. Curr. Psychiatry Rep. 2020, 22, 19. [Google Scholar] [CrossRef] [PubMed]
- Hoge, C.W.; Riviere, L.A.; Wilk, J.E.; Herrell, R.K.; Weathers, F.W. The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: A head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. Lancet Psychiatry 2014, 1, 269–277. [Google Scholar] [CrossRef]
- Sareen, J. Posttraumatic Stress Disorder in Adults: Impact, Comorbidity, Risk Factors, and Treatment. Can. J. Psychiatry 2014, 59, 460–467. [Google Scholar] [CrossRef] [Green Version]
- Shalev, A.; Liberzon, I.; Marmar, C. Post-Traumatic Stress Disorder. N. Engl. J. Med. 2017, 376, 2459–2469. [Google Scholar] [CrossRef] [PubMed]
- Flory, J.D.; Yehuda, R. Comorbidity between post-traumatic stress disorder and major depressive disorder: Alternative explanations and treatment considerations. Dialogues Clin. Neurosci. 2015, 17, 141–150. [Google Scholar] [CrossRef]
- Radell, M.L.; Hamza, E.A.; Moustafa, A.A. Depression in post-traumatic stress disorder. Rev. Neurosci. 2020, 31, 703–722. [Google Scholar] [CrossRef] [PubMed]
- Gisquet-Verrier, P.; Le Dorze, C. Post Traumatic Stress Disorder and Substance Use Disorder as Two Pathologies Affecting Memory Reactivation: Implications for New Therapeutic Approaches. Front. Behav. Neurosci. 2019, 13, 26. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.D.L.; Cottler, L.B. The Epidemiology of Post-Traumatic Stress Disorder and Alcohol Use Disorder. Alcohol Res. 2018, 39, 113–120. [Google Scholar] [PubMed]
- American Psychological Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults: (501872017-001); American Psychological Association: Washington, DC, USA, 2017. [Google Scholar]
- Wright, L.A.; Sijbrandij, M.; Sinnerton, R.; Lewis, C.; Roberts, N.P.; Bisson, J.I. Pharmacological prevention and early treatment of post-traumatic stress disorder and acute stress disorder: A systematic review and meta-analysis. Transl. Psychiatry 2019, 9, 334. [Google Scholar] [CrossRef]
- Hoskins, M.; Pearce, J.; Bethell, A.; Dankova, L.; Barbui, C.; Tol, W.A.; Van Ommeren, M.; De Jong, J.; Seedat, S.; Chen, H.; et al. Pharmacotherapy for post-traumatic stress disorder: Systematic review and meta-analysis. Br. J. Psychiatry 2015, 206, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.J.; Ipser, J.C.; Seedat, S.; Sager, C.; Amos, T. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database Syst. Rev. 2006, 2006, CD002795. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.L.; Dunn, M.K. Therapeutic peptides: Historical perspectives, current development trends, and future directions. Bioorg. Med. Chem. 2018, 26, 2700–2707. [Google Scholar] [CrossRef] [PubMed]
- Malyshev, A.V.; Sukhanova, I.A.; Zlobin, A.S.; Gedzun, V.R.; Pavshintsev, V.V.; Vasileva, E.V.; Zalevsky, A.O.; Doronin, I.I.; Mitkin, N.A.; Golovin, A.V.; et al. In silico Screening and Behavioral Validation of a Novel Peptide, LCGA-17, With Anxiolytic-Like Properties. Front. Neurosci. 2021, 15, 705590. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Bachu, R.; Kotapati, P.; Adnan, M.; Ahmed, R.; Farooq, U.; Saeed, H.; Khan, A.M.; Zubair, A.; Qamar, I.; et al. Use of Gabapentin in the Treatment of Substance Use and Psychiatric Disorders: A Systematic Review. Front. Psychiatry 2019, 10, 228. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, D.S.; Waldman, S.; Allgulander, C. Evidence-based pharmacological treatment of generalized anxiety disorder. Int. J. Neuropsychopharmacol. 2011, 14, 697–710. [Google Scholar] [CrossRef] [PubMed]
- Bandelow, B.; Zohar, J.; Hollander, E.; Kasper, S.; Möller, H.J.; Zohar, J.; Hollander, E.; Kasper, S.; Möller, H.J.; Bandelow, B.; et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Pharmacological Treatment of Anxiety, Obsessive-Compulsive and Post-Traumatic Stress Disorders—First Revision. World J. Biol. Psychiatry 2008, 9, 248–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lüscher, B.; Möhler, H. Brexanolone, a neurosteroid antidepressant, vindicates the GABAergic deficit hypothesis of depression and may foster resilience. F1000Research 2019, 8, 751. [Google Scholar] [CrossRef] [Green Version]
- Möhler, H. The GABA system in anxiety and depression and its therapeutic potential. Neuropharmacology 2012, 62, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Wang, D.-S.; Bonin, R.P.; Penna, A.; Alavian-Ghavanini, A.; Zurek, A.A.; Rauw, G.; Baker, G.B.; Orser, B.A. Gabapentin increases expression of δ subunit-containing GABAA receptors. EBioMedicine 2019, 42, 203–213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albrechet-Souza, L.; Gilpin, N.W. The predator odor avoidance model of post-traumatic stress disorder in rats. Behav. Pharmacol. 2019, 30, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, A.M.; Gilpin, N.W. Blunted hypothalamo-pituitary adrenal axis response to predator odor predicts high stress reactivity. Physiol. Behav. 2015, 147, 16–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willner, P. The chronic mild stress (CMS) model of depression: History, evaluation and usage. Neurobiol. Stress 2017, 6, 78–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papp, M.; Gruca, P.; Lason-Tyburkiewicz, M.; Willner, P. Antidepressant, anxiolytic and procognitive effects of subacute and chronic ketamine in the chronic mild stress model of depression. Behav. Pharmacol. 2017, 28, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Papp, M.; Moryl, E.; Willner, P. Pharmacological validation of the chronic mild stress model of depression. Eur. J. Pharmacol. 1996, 296, 129–136. [Google Scholar] [CrossRef]
- Willner, P.; Gruca, P.; Lason, M.; Tota-Glowczyk, K.; Litwa, E.; Niemczyk, M.; Papp, M. Validation of chronic mild stress in the Wistar-Kyoto rat as an animal model of treatment-resistant depression. Behav. Pharmacol. 2019, 30, 239–250. [Google Scholar] [CrossRef]
- Lochhead, J.; Thorne, R.G. Intranasal delivery of biologics to the central nervous system. Adv. Drug Deliv. Rev. 2012, 64, 614–628. [Google Scholar] [CrossRef] [PubMed]
- Pires, A.; Fortuna, A.; Alves, G.; Falcão, A. Intranasal Drug Delivery: How, Why and What for? J. Pharm. Pharm. Sci. 2009, 12, 288–311. [Google Scholar] [CrossRef] [Green Version]
- Meredith, M.E.; Salameh, T.S.; Banks, W.A. Intranasal Delivery of Proteins and Peptides in the Treatment of Neurodegenerative Diseases. AAPS J. 2015, 17, 780–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strekalova, T.; Spanagel, R.; Bartsch, D.A.; Henn, F.A.; Gass, P. Stress-Induced Anhedonia in Mice is Associated with Deficits in Forced Swimming and Exploration. Neuropsychopharmacology 2004, 29, 2007–2017. [Google Scholar] [CrossRef] [PubMed]
- Strekalova, T.; Couch, Y.; Kholod, N.; Boyks, M.; Malin, D.; Leprince, P.; Steinbusch, H.M. Update in the methodology of the chronic stress paradigm: Internal control matters. Behav. Brain Funct. 2011, 7, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Statistics. Available online: https://www.nimh.nih.gov/health/statistics (accessed on 22 March 2022).
- Herbst, L.; Gaigher, T.; Siqueira, A.; Joca, S.; Sampaio, K.; Beijamini, V. New evidence for refinement of anesthetic choice in procedures preceding the forced swimming test and the elevated plus-maze. Behav. Brain Res. 2019, 368, 111897. [Google Scholar] [CrossRef]
- Clarke, M.; Razmjou, S.; Prowse, N.; Dwyer, Z.; Litteljohn, D.; Pentz, R.; Anisman, H.; Hayley, S. Ketamine modulates hippocampal neurogenesis and pro-inflammatory cytokines but not stressor induced neurochemical changes. Neuropharmacology 2016, 112, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Kara, N.; Agam, G.; Anderson, G.; Zitron, N.; Einat, H. Lack of effect of chronic ketamine administration on depression-like behavior and frontal cortex autophagy in female and male ICR mice. Behav. Brain Res. 2017, 317, 576–580. [Google Scholar] [CrossRef] [PubMed]
- Krimmel, S.R.; Zanos, P.; Georgiou, P.; Colloca, L.; Gould, T.D. Classical conditioning of antidepressant placebo effects in mice. Psychopharmacology 2019, 237, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Tizabi, Y.; Bhatti, B.; Manaye, K.; Das, J.; Akinfiresoye, L. Antidepressant-like effects of low ketamine dose is associated with increased hippocampal AMPA/NMDA receptor density ratio in female Wistar–Kyoto rats. Neuroscience 2012, 213, 72–80. [Google Scholar] [CrossRef] [Green Version]
- Richards, A.; Inslicht, S.; Ruoff, L.M.; Metzler, T.J.; Goldstein, L.A.; Chapman, C.M.; Hubachek, S.Q.; Neylan, T.C. An Open-Label Study of Doxazosin Extended-Release for PTSD: Findings and Recommendations for Future Research on Doxazosin. FOCUS 2018, 16, 67–73. [Google Scholar] [CrossRef]
- Rodgman, C.; Verrico, C.D.; Holst, M.; Thompson-Lake, D.; Haile, C.N.; De La Garza, R.; Raskind, M.A.; Newton, T.F. Doxazosin XL Reduces Symptoms of Posttraumatic Stress Disorder in Veterans With PTSD. J. Clin. Psychiatry 2016, 77, e561–e565. [Google Scholar] [CrossRef] [PubMed]
- McKinney, B.C.; Murphy, G.G. The L-Type voltage-gated calcium channel Cav1.3 mediates consolidation, but not extinction, of contextually conditioned fear in mice. Learn. Mem. 2006, 13, 584–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, E.P.; Schafe, G.E.; LeDoux, J.E. NMDA Receptors and L-Type Voltage-Gated Calcium Channels Contribute to Long-Term Potentiation and Different Components of Fear Memory Formation in the Lateral Amygdala. J. Neurosci. 2002, 22, 5239–5249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abramova, O.; Zorkina, Y.; Syunyakov, T.; Zubkov, E.; Ushakova, V.; Silantyev, A.; Soloveva, K.; Gurina, O.; Majouga, A.; Morozova, A.; et al. Brain Metabolic Profile after Intranasal vs. Intraperitoneal Clomipramine Treatment in Rats with Ultrasound Model of Depression. Int. J. Mol. Sci. 2021, 22, 9598. [Google Scholar] [CrossRef]
- Rincón-Cortés, M.; Grace, A.A. Antidepressant effects of ketamine on depression-related phenotypes and dopamine dysfunction in rodent models of stress. Behav. Brain Res. 2019, 379, 112367. [Google Scholar] [CrossRef]
- Surget, A.; Saxe, M.; Leman, S.; Ibarguen-Vargas, Y.; Chalon, S.; Griebel, G.; Hen, R.; Belzung, C. Drug-Dependent Requirement of Hippocampal Neurogenesis in a Model of Depression and of Antidepressant Reversal. Biol. Psychiatry 2008, 64, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.-L.; Luo, L.; Mu, R.-H.; Liu, B.-B.; Geng, D.; Liu, Q.; Yi, L.-T. Fluoxetine regulates mTOR signalling in a region-dependent manner in depression-like mice. Sci. Rep. 2015, 5, 16024. [Google Scholar] [CrossRef]
- Bollinger, J.L.; Horchar, M.J.; Wohleb, E.S. Diazepam limits microglia-mediated neuronal remodeling in the prefrontal cortex and associated behavioral consequences following chronic unpredictable stress. Neuropsychopharmacology 2020, 45, 1766–1776. [Google Scholar] [CrossRef]
- Amiresmaeili, A.; Roohollahi, S.; Mostafavi, A.; Askari, N. Effects of oregano essential oil on brain TLR4 and TLR2 gene expression and depressive-like behavior in a rat model. Res. Pharm. Sci. 2018, 13, 130–141. [Google Scholar] [CrossRef]
- Aricioğlu, F.; Yalcinkaya, C.; Ozkartal, C.S.; Tuzun, E.; Sirvanci, S.; Kucukali, C.I.; Utkan, T. NLRP1-Mediated Antidepressant Effect of Ketamine in Chronic Unpredictable Mild Stress Model in Rats. Psychiatry Investig. 2020, 17, 283–291. [Google Scholar] [CrossRef] [Green Version]
- Benasi, G.; Guidi, J.; Offidani, E.; Balon, R.; Rickels, K.; Fava, G.A. Benzodiazepines as a Monotherapy in Depressive Disorders: A Systematic Review. Psychother. Psychosom. 2018, 87, 65–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stancheva, S.; Petkov, V.V. Effects of chronic diazepam and medazepam treatment on the level of biogenic monoamines in different rat brain areas. Acta Physiol. Pharmacol. Bulg. 1988, 14, 26–31. [Google Scholar]
- Wingenfeld, K.; Wolf, O.T. Stress, Memory, and the Hippocampus. Hippocampus Clin. Neurosci. 2014, 34, 109–120. [Google Scholar] [CrossRef]
- Valente, M.M.; Bortolotto, V.; Cuccurazzu, B.; Ubezio, F.; Meneghini, V.; Francese, M.T.; Canonico, P.L.; Grilli, M. α2δ Ligands Act as Positive Modulators of Adult Hippocampal Neurogenesis and Prevent Depression-Like Behavior Induced by Chronic Restraint Stress. Mol. Pharmacol. 2012, 82, 271–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaby, L.E.; Sadik, N.; Burson, N.A.; Lloyd, S.; O’Donnel, K.; Winters, J.; Conti, A.C.; Liberzon, I.; Perrine, S.A. Repeated stress exposure in mid-adolescence attenuates behavioral, noradrenergic, and epigenetic effects of trauma-like stress in early adult male rats. Sci. Rep. 2020, 10, 17935. [Google Scholar] [CrossRef] [PubMed]
- Ushakova, V.M.; Morozova, A.Y.; Reznik, A.M.; Kostyuk, G.P.; Chekhonin, V.P. Molecular Biological Aspects of Depressive Disorders: A Modern View. Mol. Biol. 2020, 54, 639–660. [Google Scholar] [CrossRef]
- Hayashida, K.-I.; Eisenach, J.C. Descending Noradrenergic Inhibition: An Important Mechanism of Gabapentin Analgesia in Neuropathic Pain. Adv. Exp. Med. Biol. 2018, 1099, 93–100. [Google Scholar] [CrossRef]
- Pellow, S.; Chopin, P.; File, S.E.; Briley, M. Validation of open: Closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J. Neurosci. Methods 1985, 14, 149–167. [Google Scholar] [CrossRef]
- Colelli, V.; Campus, P.; Conversi, D.; Orsini, C.; Cabib, S. Either the dorsal hippocampus or the dorsolateral striatum is selectively involved in consolidation of forced swim-induced immobility depending on genetic background. Neurobiol. Learn. Mem. 2014, 111, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Morozova, A.; Zubkov, E.; Strekalova, T.; Kekelidze, Z.; Storozeva, Z.; Schroeter, C.A.; Bazhenova, N.; Lesch, K.-P.; Cline, B.H.; Chekhonin, V. Ultrasound of alternating frequencies and variable emotional impact evokes depressive syndrome in mice and rats. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2016, 68, 52–63. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Association Publishing: Washington, DC, USA, 2013; ISBN 0-89042-557-4. [Google Scholar]
- Zorkina, Y.A.; Zubkov, E.; Morozova, A.Y.; Ushakova, V.; Chekhonin, V.P. The Comparison of a New Ultrasound-Induced Depression Model to the Chronic Mild Stress Paradigm. Front. Behav. Neurosci. 2019, 13, 146. [Google Scholar] [CrossRef]
- File, S.E.; Seth, P. A review of 25 years of the social interaction test. Eur. J. Pharmacol. 2003, 463, 35–53. [Google Scholar] [CrossRef]
- Jiao, H.; Yan, Z.; Ma, Q.; Li, X.; Jiang, Y.; Liu, Y.; Chen, J. Influence of Xiaoyaosan on depressive-like behaviors in chronic stress-depressed rats through regulating tryptophan metabolism in hippocampus. Neuropsychiatr. Dis. Treat. 2018, 15, 21–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dulawa, S.C.; Hen, R. Recent advances in animal models of chronic antidepressant effects: The novelty-induced hypophagia test. Neurosci. Biobehav. Rev. 2005, 29, 771–783. [Google Scholar] [CrossRef] [PubMed]
- Malkesman, O.; Scattoni, M.L.; Paredes, D.; Tragon, T.; Pearson, B.; Shaltiel, G.; Chen, G.; Crawley, J.N.; Manji, H.K. The Female Urine Sniffing Test: A Novel Approach for Assessing Reward-Seeking Behavior in Rodents. Biol. Psychiatry 2010, 67, 864–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edwards, S.; Baynes, B.B.; Carmichael, C.Y.; Zamora-Martinez, E.R.; Barrus, M.; Koob, G.F.; Gilpin, N.W. Traumatic stress reactivity promotes excessive alcohol drinking and alters the balance of prefrontal cortex-amygdala activity. Transl. Psychiatry 2013, 3, e296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roltsch, E.A.; Baynes, B.B.; Mayeux, J.P.; Whitaker, A.M.; Baiamonte, B.A.; Gilpin, N.W. Predator odor stress alters corticotropin-releasing factor-1 receptor (CRF1R)-dependent behaviors in rats. Neuropharmacology 2013, 79, 83–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belov, D.R.; Efimova, E.V.; Fesenko, Z.S.; Antonova, K.A.; Kolodyazhny, S.F.; Lakstygal, A.M.; Gainetdinov, R.R. Putative Trace-Amine Associated Receptor 5 (TAAR5) Agonist α-NETA Increases Electrocorticogram Gamma-Rhythm in Freely Moving Rats. Cell. Mol. Neurobiol. 2019, 40, 203–213. [Google Scholar] [CrossRef] [PubMed]

| Procedures | Day of Experiment | Days of Treatment |
|---|---|---|
| Adaptation | 1–14 | - |
| SPT1 | 15–21 | - |
| The division into “stressed” and “unstressed” groups | ||
| CUS | 22–48 | - |
| SPT2 | 49–55 | - |
| The division into treatment groups | ||
| SI | 61–62 | 4 |
| FUST | 65–66 | 8 |
| NSFT | 67–69 | 11 |
| SPT3 | 72–75 | 16 |
| FST | 75–76 | 18 |
| sacrifice | 79–80 | 22 |
| Day of Stress | 10 a.m.–6 p.m. | 6 p.m.–10 a.m. |
|---|---|---|
| 1, 8, 15, 22 | Cold room (1 h) | Intermittent lightning (on/off every 2 h) |
| 2, 9, 16, 23 | Cage tilt (45°) | Water deprivation |
| 3, 10, 17, 24 | Stroboscopic light | Light overnight |
| 4, 11, 18, 25 | Wet bedding | Mouse cage |
| 5, 12, 19, 26 | No bedding | Intermittent lighting (on/off every 2 h) |
| 6, 13, 20 | 6-month-old new rat | Light overnight |
| 7, 14, 21 | White noise | Stroboscopic light |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malyshev, A.V.; Sukhanova, I.A.; Ushakova, V.M.; Zorkina, Y.A.; Abramova, O.V.; Morozova, A.Y.; Zubkov, E.A.; Mitkin, N.A.; Pavshintsev, V.V.; Doronin, I.I.; et al. Peptide LCGA-17 Attenuates Behavioral and Neurochemical Deficits in Rodent Models of PTSD and Depression. Pharmaceuticals 2022, 15, 462. https://doi.org/10.3390/ph15040462
Malyshev AV, Sukhanova IA, Ushakova VM, Zorkina YA, Abramova OV, Morozova AY, Zubkov EA, Mitkin NA, Pavshintsev VV, Doronin II, et al. Peptide LCGA-17 Attenuates Behavioral and Neurochemical Deficits in Rodent Models of PTSD and Depression. Pharmaceuticals. 2022; 15(4):462. https://doi.org/10.3390/ph15040462
Chicago/Turabian StyleMalyshev, Anton V., Iuliia A. Sukhanova, Valeria M. Ushakova, Yana A. Zorkina, Olga V. Abramova, Anna Y. Morozova, Eugene A. Zubkov, Nikita A. Mitkin, Vsevolod V. Pavshintsev, Igor I. Doronin, and et al. 2022. "Peptide LCGA-17 Attenuates Behavioral and Neurochemical Deficits in Rodent Models of PTSD and Depression" Pharmaceuticals 15, no. 4: 462. https://doi.org/10.3390/ph15040462
APA StyleMalyshev, A. V., Sukhanova, I. A., Ushakova, V. M., Zorkina, Y. A., Abramova, O. V., Morozova, A. Y., Zubkov, E. A., Mitkin, N. A., Pavshintsev, V. V., Doronin, I. I., Gedzun, V. R., Babkin, G. A., Sanchez, S. A., Baker, M. D., & Haile, C. N. (2022). Peptide LCGA-17 Attenuates Behavioral and Neurochemical Deficits in Rodent Models of PTSD and Depression. Pharmaceuticals, 15(4), 462. https://doi.org/10.3390/ph15040462







