Medicines Reconciliation in the Emergency Department: Important Prescribing Discrepancies between the Shared Medication Record and Patients’ Actual Use of Medication
Abstract
:1. Introduction
2. Results
2.1. Patient Characteristics
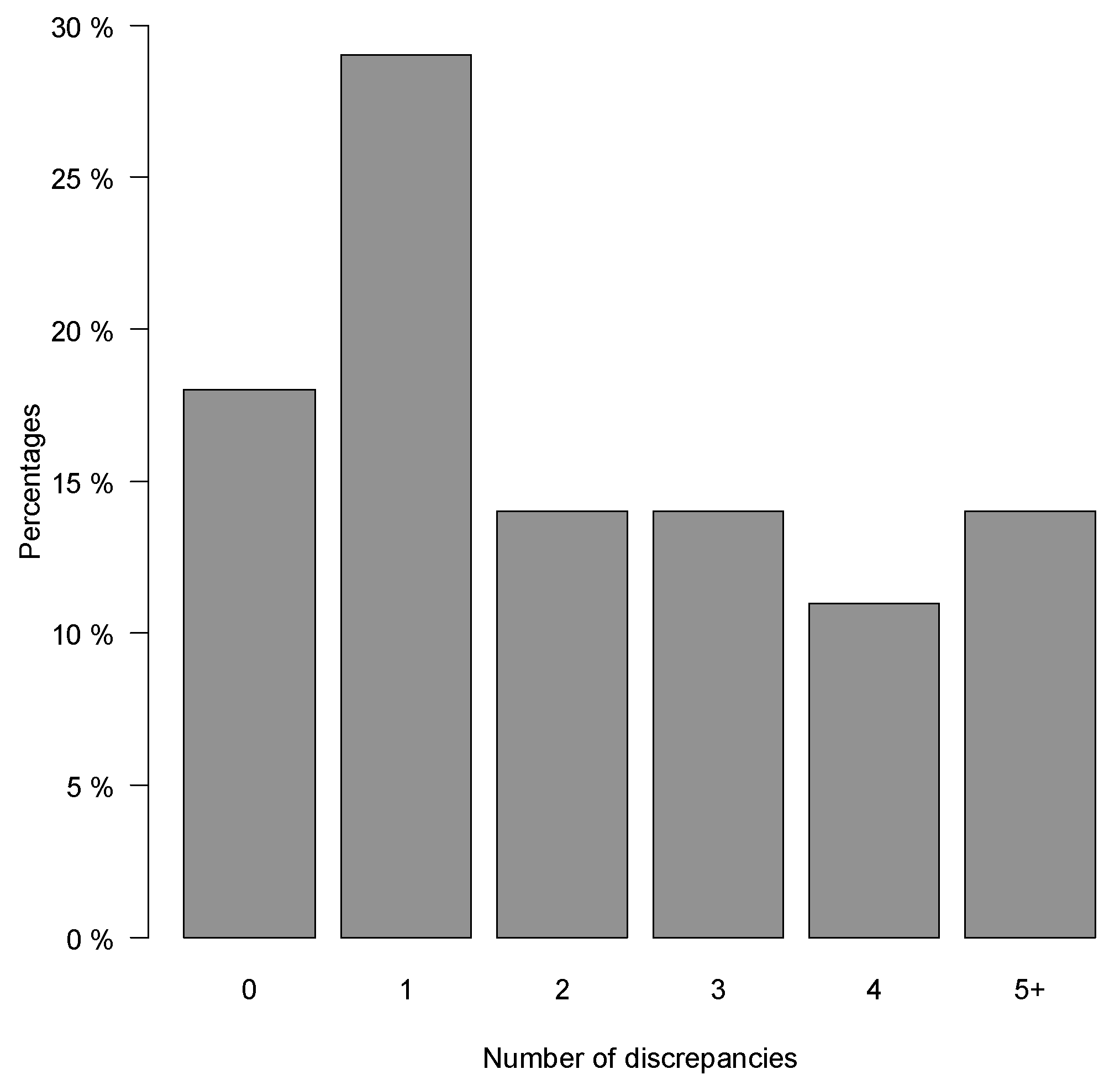
2.2. Number of Prescribing Discrepancies
2.3. Types of Prescribing Discrepancies
2.4. Factors Associated with the Rate of Prescribing Discrepancies
2.5. Medicines Reconciliations Completed during Normal Working Hours
3. Discussion
3.1. Main Findings
3.2. Results in Context of Other Studies
3.3. Updating the SMR: Possible Solutions and Reflections
3.4. Strengths and Limitations
4. Materials and Methods
4.1. Ethics Approval
4.2. Setting
4.3. Design and Patients
4.4. Data Collection and the Best Possible Medication History
4.5. Outcomes
4.6. Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| ATC-Drug Group (Level 2) | Description | Number of Discrepancies, n (%) |
|---|---|---|
| A02 | Drugs for acid related disorders | 25 (22.7) |
| N02 | Analgesics | 13 (11.8) |
| C09 | Agents acting on the renin-angiotensin system | 11 (10.0) |
| A06 | Drugs for constipation | 5 (4.5) |
| B01 | Antithrombotic agents | 5 (4.5) |
| A12 | Mineral supplements | 5 (4.5) |
| C10 | Lipid modifying agents | 5 (4.5) |
| C01 | Cardiac therapy | 5 (4.5) |
| R03 | Drugs for obstructive airway diseases | 4 (3.6) |
| B03 | Antianemic preparations | 4 (3.6) |
| J01 | Antibacterials for systemic use | 4 (3.6) |
| N03 | Antiepileptics | 4 (3.6) |
| N05 | Psycholeptics | 3 (2.7) |
| A11 | Vitamins | 3 (2.7) |
| N06 | Psychoanaleptics | 2 (1.8) |
| A10 | Drugs used in diabetes | 2 (1.8) |
| M01 | Anti-inflammatory and antirheumatic products | 2 (1.8) |
| H02 | Corticosteroids for systemic use | 2 (1.8) |
| R01 | Nasal preparations | 1 (0.9) |
| C03 | Diuretics | 1 (0.9) |
| M03 | Muscle relaxants | 1 (0.9) |
| S01 | Ophthalmologicals | 1 (0.9) |
| L01 | Antineoplastic agents | 1 (0.9) |
| D01 | Antifungals for dermatological use | 1 (0.9) |
| Covariate (Number of Patients) | Incidence Rate Ratio | Confidence Interval | p-Value |
|---|---|---|---|
| Age, years | |||
| <65 (44) 65–79 (years) (30) ≥80 (years) (26) | Ref 0.67 0.53 | Ref 0.45–0.99 0.33–0.86 | Ref 0.514 0.119 |
| Female Male 65–79 (52) | Ref 0.98 | Ref 0.68–1.43 | Ref 1.00 |
| All models are adjusted for age and sex | |||
| Days since the last SMR update * | |||
| First tertile: 0–27 (33) Second tertile: 28–114 (28) Third tertile: ≥115 (29) | Ref 1.27 1.14 | Ref 0.85–1.89 0.76–1.73 | Ref 1.00 1.00 |
| Who updated the SMR last * | |||
| Hospital (37) Outpatients clinic (29) GP (24) | Ref 1.03 1.22 | Ref 0.69–1.54 0.82–1.81 | Ref 1.00 1.00 |
| Time of admission to the ED | |||
| During normal working hours (48) Outside normal working hours (52) | Ref 2.59 | Ref 1.84–3.63 | Ref <0.001 |
| Help with medication dispensing | |||
| No (71) Yes (29) | Ref 0.18 | Ref 0.10–0.33 | Ref <0.001 |
| Triage level | |||
| 1 or 2 (23) 3 (51) 4 (26) | Ref 0.97 0.79 | Ref 0.62–1.53 0.45–1.37 | Ref 1.00 1.00 |
References
- Lau, H.S.; Florax, C.; Porsius, A.J.; De Boer, A. The Completeness of Medication Histories in Hospital Medical Records of Patients Admitted to General Internal Medicine Wards. Br. J. Clin. Pharmacol. 2000, 49, 597–603. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.E.; Pedersen, A.B.; Bach, K.F. Medication History on Internal Medicine Wards: Assessment of Extra Information Collected from Second Drug Interviews and GP Lists. Pharmacoepidemiol. Drug Saf. 2003, 12, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Knez, L.; Suskovic, S.; Rezonja, R.; Laaksonen, R.; Mrhar, A. The Need for Medication Reconciliation: A Cross-Sectional Observational Study in Adult Patients. Respir. Med. 2011, 105 (Suppl. 1), S60–S66. [Google Scholar] [CrossRef] [Green Version]
- Beers, M.H.; Munekata, M.; Storrie, M. The Accuracy of Medication Histories in the Hospital Medical Records of Elderly Persons. J. Am. Geriatr. Soc. 1990, 38, 1183–1187. [Google Scholar] [CrossRef] [PubMed]
- Shaw, J.; Seal, R.; Pilling, M. Room for Review a Guide to Medication Review: The Agenda for Patients, Practitioners and Managers; Medicines Partnership: London, UK, 2002. [Google Scholar]
- Ministry of Health. Fælles Medicinkort (FMK)—Sundhedsdatastyrelsen. Available online: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-faelles-medicinkort (accessed on 28 November 2021). (In Danish)
- The Danish Health Data Authority. Shared Medicine Card. Available online: https://www.danishhealthdata.com/find-health-data/,-w- (accessed on 28 November 2021).
- The Danish Health Data Authority. Best Practice på FMK. Available online: https://sundhedsdatastyrelsen.dk/-/media/sds/filer/registre-og-services/faelles-medicinkort/fmk-sundhedsprofesionelle/best_practice_fmk.pdf (accessed on 30 November 2021). (In Danish).
- Munck, L.K.; Hansen, K.R.; Mølbak, A.G.; Balle, H.; Kongsgren, S. The Use of Shared Medication Record as Part of Medication Reconciliation at Hospital Admission Is Feasible. Dan. Med. J. 2014, 61, A4817. [Google Scholar]
- Mueller, S.K.; Sponsler, K.C.; Kripalani, S.; Schnipper, J.L. Hospital-Based Medication Reconciliation Practices: A Systematic Review. Arch. Intern. Med. 2012, 172, 1057–1069. [Google Scholar] [CrossRef]
- Cornu, P.; Steurbaut, S.; Leysen, T.; De Baere, E.; Ligneel, C.; Mets, T.; Dupont, A.G. Effect of Medication Reconciliation at Hospital Admission on Medication Discrepancies during Hospitalization and at Discharge for Geriatric Patients. Ann. Pharmacother. 2012, 46, 484–494. [Google Scholar] [CrossRef]
- DeAntonio, J.H.; Leichtle, S.W.; Hobgood, S.; Boomer, L.; Aboutanos, M.; Mangino, M.J.; Wijesinghe, D.S.; Jayaraman, S. Medication Reconciliation and Patient Safety in Trauma: Applicability of Existing Strategies. J. Surg. Res. 2020, 246, 482–489. [Google Scholar] [CrossRef]
- Moore, P.; Armitage, G.; Wright, J.; Dobrzanski, S.; Ansari, N.; Hammond, I.; Scally, A. Medicines Reconciliation Using a Shared Electronic Health Care Record. J. Patient Saf. 2011, 7, 148–154. [Google Scholar] [CrossRef]
- Region Hovedstaden. Lægemiddelkomitéer i Region Hovedstaden og Region Sjælland Lægemiddelordination. Available online: https://vip.regionh.dk/VIP/Admin/GUI.nsf/Desktop.html?open&openlink=https://vip.regionh.dk/VIP/Slutbruger/Portal.nsf/Main.html?open&unid=XDCFC8C0A263E4AB3C12578AA002C8412&level=159716&dbpath=/VIP/Redaktoer/RH.nsf/&windowwidth=1100&windowheight=600&windowtitle=S%F8g (accessed on 24 January 2022). (In Danish)
- Bülow, C.; Noergaard, J.D.S.V.; Faerch, K.U.; Pontoppidan, C.; Unkerskov, J.; Johansson, K.S.; Kornholt, J.; Christensen, M.B. Causes of Discrepancies between Medications Listed in the National Electronic Prescribing System and Patients’ Actual Use of Medications. Basic Clin. Pharmacol. Toxicol. 2021, 129, 221–231. [Google Scholar] [CrossRef]
- Bülow, C.; Flagstad Bech, C.; Ullitz Faerch, K.; Trærup Andersen, J.; Byg Armandi, H.; Treldal, C. Discrepancies Between the Medication List in Electronic Prescribing Systems and Patients’ Actual Use of Medicines. Sr. Care Pharm. 2019, 34, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Christensen, S.; Jensen, L.D.; Kaae, S.; Vinding, K.L.; Petersen, J. Implementation of the shared medication record is difficult. Ugeskr. Laeg. 2014, 176, 1389–1391. [Google Scholar] [PubMed]
- Buck, T.C.; Gronkjaer, L.S.; Duckert, M.-L.; Rosholm, J.-U.; Aagaard, L. Medication Reconciliation and Prescribing Reviews by Pharmacy Technicians in a Geriatric Ward. J. Res. Pharm. Pract. 2013, 2, 145–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michaelsen, M.H.; McCague, P.; Bradley, C.P.; Sahm, L.J. Medication Reconciliation at Discharge from Hospital: A Systematic Review of the Quantitative Literature. Pharmacy 2015, 3, 53–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belda-Rustarazo, S.; Cantero-Hinojosa, J.; Salmeron-García, A.; González-García, L.; Cabeza-Barrera, J.; Galvez, J. Medication Reconciliation at Admission and Discharge: An Analysis of Prevalence and Associated Risk Factors. Int. J. Clin. Pract. 2015, 69, 1268–1274. [Google Scholar] [CrossRef]
- Bjeldbak-Olesen, M.; Danielsen, A.G.; Tomsen, D.V.; Jakobsen, T.J. Medication Reconciliation Is a Prerequisite for Obtaining a Valid Medication Review. Dan. Med. J. 2013, 60, A4605. [Google Scholar]
- Urban, R.; Armitage, G.; Morgan, J.; Marshall, K.; Blenkinsopp, A.; Scally, A. Custom and Practice: A Multi-Center Study of Medicines Reconciliation Following Admission in Four Acute Hospitals in the UK. Res. Soc. Adm. Pharm. RSAP 2014, 10, 355–368. [Google Scholar] [CrossRef]
- Pippins, J.R.; Gandhi, T.K.; Hamann, C.; Ndumele, C.D.; Labonville, S.A.; Diedrichsen, E.K.; Carty, M.G.; Karson, A.S.; Bhan, I.; Coley, C.M.; et al. Classifying and Predicting Errors of Inpatient Medication Reconciliation. J. Gen. Intern. Med. 2008, 23, 1414–1422. [Google Scholar] [CrossRef] [Green Version]
- Cornish, P.L.; Knowles, S.R.; Marchesano, R.; Tam, V.; Shadowitz, S.; Juurlink, D.N.; Etchells, E.E. Unintended Medication Discrepancies at the Time of Hospital Admission. Arch. Intern. Med. 2005, 165, 424–429. [Google Scholar] [CrossRef]
- Houlind, M.B.; Andersen, A.L.; Treldal, C.; Jørgensen, L.M.; Kannegaard, P.N.; Castillo, L.S.; Christensen, L.D.; Tavenier, J.; Rasmussen, L.J.H.; Ankarfeldt, M.Z.; et al. A Collaborative Medication Review Including Deprescribing for Older Patients in an Emergency Department: A Longitudinal Feasibility Study. J. Clin. Med. 2020, 9, 348. [Google Scholar] [CrossRef] [Green Version]
- Schytte-Hansen, S.; Karkov, L.L.; Balslev-Clausen, A.P. The personal electronic medicine profile contributes to the avoidance of wrong medication at transfer from primary to secondary sector. Ugeskr. Laeg. 2011, 173, 2793–2797. [Google Scholar] [PubMed]
- Tamblyn, R.; Abrahamowicz, M.; Buckeridge, D.L.; Bustillo, M.; Forster, A.J.; Girard, N.; Habib, B.; Hanley, J.; Huang, A.; Kurteva, S.; et al. Effect of an Electronic Medication Reconciliation Intervention on Adverse Drug Events: A Cluster Randomized Trial. JAMA Netw. Open 2019, 2, e1910756. [Google Scholar] [CrossRef] [PubMed]
- Jurado, C.; Calmels, V.; Lobinet, E.; Divol, E.; Hanaire, H.; Metsu, D.; Sallerin, B. The Electronic Pharmaceutical Record: A New Method for Medication Reconciliation. J. Eval. Clin. Pract. 2018, 24, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Meguerditchian, A.N.; Krotneva, S.; Reidel, K.; Huang, A.; Tamblyn, R. Medication Reconciliation at Admission and Discharge: A Time and Motion Study. BMC Health Serv. Res. 2013, 13, 485. [Google Scholar] [CrossRef] [Green Version]
- Bracey, G.; Miller, G.; Franklin, B.D.; Jacklin, A.; Gaskin, G. The Contribution of a Pharmacy Admissions Service to Patient Care. Clin. Med. 2008, 8, 53–57. [Google Scholar] [CrossRef]
- Rose, A.J.; Fischer, S.H.; Paasche-Orlow, M.K. Beyond Medication Reconciliation: The Correct Medication List. JAMA 2017, 317, 2057–2058. [Google Scholar] [CrossRef]
- Mekonnen, A.B.; Abebe, T.B.; McLachlan, A.J.; Brien, J.-A.E. Impact of Electronic Medication Reconciliation Interventions on Medication Discrepancies at Hospital Transitions: A Systematic Review and Meta-Analysis. BMC Med. Inform. Decis. Mak. 2016, 16, 112. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Medication Safety in Transitions of Care: Technical Report; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. Available online: https://www.r-project.org/ (accessed on 30 November 2021).
| Demographic Data | Median (IQR) or n (%) |
|---|---|
| Sex (men) | 52 (52) |
| Age (years) | 66.5 (53–80) |
| Admitted during normal working hours 8:00 a.m.–3:00 p.m. | 48 (48) |
| Admitted outside normal working hours 3:01 p.m.–07:59 a.m. | 52 (52) |
| Referred to the ED by a GP or Outpatient clinic | 37 (37) |
| Referred to the ED by an emergency or out-of-hours service healthcare professional | 55 (55) |
| Self-referral to the ED | 8 (8) |
| Triage level ≥ 3 | 78 (78) |
| Length of hospital stay | 2 (1–4) |
| Patients with a hospital interaction within 90 days before index admission | 66 (66) |
| eGFR mL/min/1.73 m2 | 83 (56–90) |
| <60 mL/min/1.73 m2 | 29 (29) |
| Medication listed in the SMR | 10 (7–13) |
| Medication used (regularly scheduled and PRN) | 8 (5–11) |
| Medication used (regularly scheduled) | 6 (3–9) |
| Patients using ≥1 regular medications | 93 (93) |
| Patients using ≥5 regular medications | 63 (63) |
| Days since the last SMR update * | 59 (14–154) |
| <30 days since the last SMR update | 35 (35) |
| <31–89 days since the last SMR update | 16 (16) |
| ≥90 days since the last SMR update | 39 (39) |
| GP completed last update of the SMR * | 24 (26) |
| Help with medication dispensing | 29 (29) |
| Types of Discrepancies | Discrepancies, n (%) | Patients, % |
|---|---|---|
| Order not in use | 157 (65) | 61 |
| Incorrect dose frequency | 37 (16) | 24 |
| Omission of order | 29 (12) | 15 |
| Duplicate order | 9 (4) | 9 |
| Incorrect dosage | 8 (3) | 6 |
| Covariate (Number of Patients) | Incidence Rate Ratio | Confidence Interval | p-Value |
|---|---|---|---|
| Age, years | |||
| <65 (44) 65–79 (30) ≥80 (26) | Ref 0.58 0.49 | Ref 0.48–0.71 0.38–0.92 | Ref <0.001 <0.001 |
| Female Male 65–79 (52) | Ref 0.96 | Ref 0.80–1.15 | Ref 1.00 |
| All models are adjusted for age and sex | |||
| Days since the last SMR update * | |||
| First tertile: 0–27 (33) Second tertile: 28–114 (28) Third tertile: ≥115 (29) | Ref 1.16 1.53 | Ref 0.96–1.40 1.29–1.82 | Ref 1.00 <0.001 |
| Who updated the SMR last * | |||
| Hospital (37) Outpatients clinic (29) GP (24) | Ref 1.02 1.19 | Ref 0.84–1.23 0.98–1.43 | Ref 1.00 0.836 |
| Time of admission to the ED | |||
| During normal working hours (48) Outside normal working hours (52) | Ref 1.04 | Ref 0.87–1.24 | Ref 1.00 |
| Help with medication dispensing | |||
| No (71) Yes (29) | Ref 0.31 | Ref 0.24–0.39 | Ref <0.001 |
| Triage level | |||
| 1 or 2 (23) 3 (51) 4 (26) | Ref 0.95 1.16 | Ref 0.75–1.19 0.90–1.49 | Ref 1.00 1.005 |
| Time | Number of Patients | Patients with ≥1 Prescribing Discrepancy, n (%) |
|---|---|---|
| Admitted during normal working hours (8.00 a.m.–3.00 p.m.) | 49 | 37 (76) |
| Admitted outside normal working hours (3.01 p.m.–7.59 a.m.), but still admitted the following morning (until at least 9.30 a.m.) | 35 | 27 (77) |
| Admitted and discharged outside normal working hours (3.01 p.m.–7.59 a.m.) | 16 | 15 (94) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andersen, T.S.; Gemmer, M.N.; Sejberg, H.R.C.; Jørgensen, L.M.; Kallemose, T.; Andersen, O.; Iversen, E.; Houlind, M.B. Medicines Reconciliation in the Emergency Department: Important Prescribing Discrepancies between the Shared Medication Record and Patients’ Actual Use of Medication. Pharmaceuticals 2022, 15, 142. https://doi.org/10.3390/ph15020142
Andersen TS, Gemmer MN, Sejberg HRC, Jørgensen LM, Kallemose T, Andersen O, Iversen E, Houlind MB. Medicines Reconciliation in the Emergency Department: Important Prescribing Discrepancies between the Shared Medication Record and Patients’ Actual Use of Medication. Pharmaceuticals. 2022; 15(2):142. https://doi.org/10.3390/ph15020142
Chicago/Turabian StyleAndersen, Tanja Stenholdt, Mia Nimb Gemmer, Hayley Rose Constance Sejberg, Lillian Mørch Jørgensen, Thomas Kallemose, Ove Andersen, Esben Iversen, and Morten Baltzer Houlind. 2022. "Medicines Reconciliation in the Emergency Department: Important Prescribing Discrepancies between the Shared Medication Record and Patients’ Actual Use of Medication" Pharmaceuticals 15, no. 2: 142. https://doi.org/10.3390/ph15020142
APA StyleAndersen, T. S., Gemmer, M. N., Sejberg, H. R. C., Jørgensen, L. M., Kallemose, T., Andersen, O., Iversen, E., & Houlind, M. B. (2022). Medicines Reconciliation in the Emergency Department: Important Prescribing Discrepancies between the Shared Medication Record and Patients’ Actual Use of Medication. Pharmaceuticals, 15(2), 142. https://doi.org/10.3390/ph15020142







