SIGLEC-1 in Systemic Sclerosis: A Useful Biomarker for Differential Diagnosis
Abstract
1. Introduction
2. Results
2.1. Patients
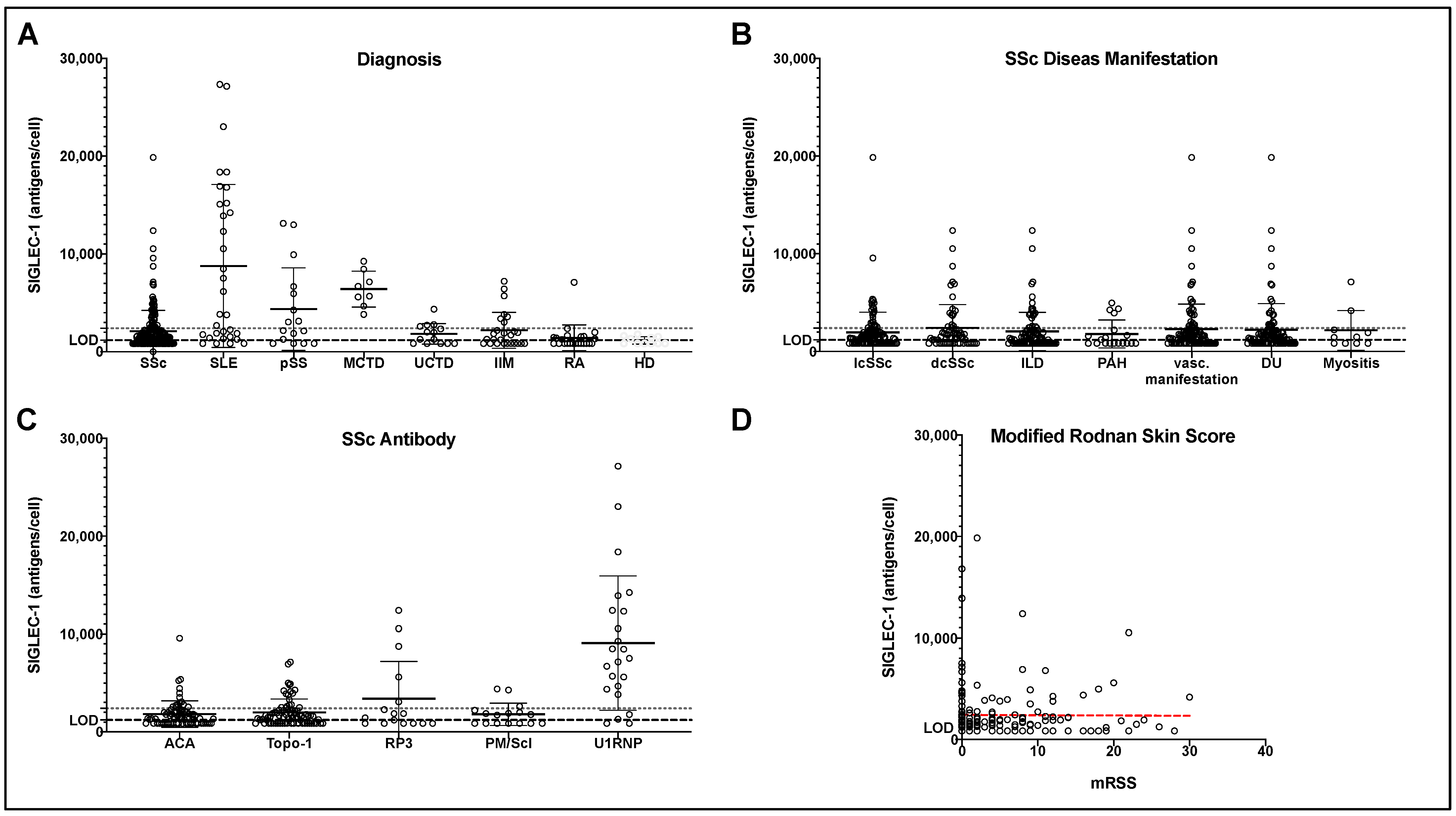
2.2. SIGLEC-1 Expression in SSc and Control Groups
2.3. SIGLEC-1 Expression and SSc Manifestations
2.4. SIGLEC-1 Expression and SSc-Specific Autoantibodies
2.5. Association of SIGLEC-1 Expression and mRSS
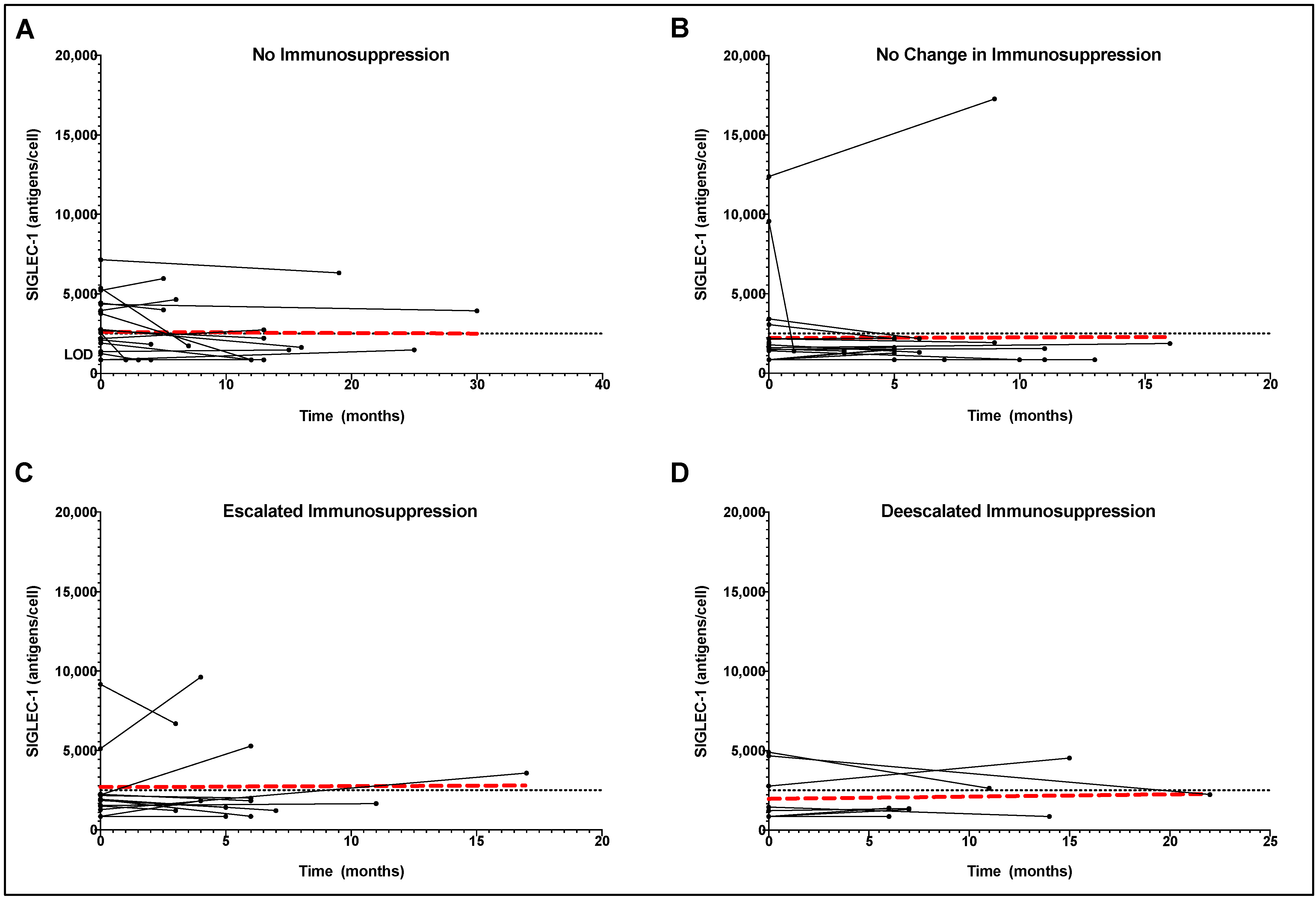
2.6. Longitudinal SIGLEC-1 Expression in Treated and Untreated SSc Patients
2.7. SIGLEC-1 as Biomarker in Differential Diagnosis of SSc
3. Discussion
4. Material and Methods
4.1. Study Design
4.2. Patients
4.3. Multi-Color Flow Cytometry for SIGLEC-1 Validation
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Denton, C.P.; Khanna, D. Systemic sclerosis. Lancet 2017, 390, 1685–1699. [Google Scholar] [CrossRef]
- Gabrielli, A.; Avvedimento, E.V.; Krieg, T. Scleroderma. N. Engl. J. Med. 2009, 360, 1989–2003. [Google Scholar] [CrossRef] [PubMed]
- Allanore, Y.; Simms, R.; Distler, O.; Trojanowska, M.; Pope, J.; Denton, C.P.; Varga, J. Systemic sclerosis. Nat. Rev. Dis. Prim. 2015, 1, 15002. [Google Scholar] [CrossRef] [PubMed]
- Assassi, S.; Mayes, M.D.; Arnett, F.C.; Gourh, P.; Agarwal, S.K.; McNearney, T.A.; Chaussabel, D.; Oommen, N.; Fischbach, M.; Shah, K.R.; et al. Systemic sclerosis and lupus: Points in an interferon-mediated continuum. Arthritis Care Res. 2010, 62, 589–598. [Google Scholar] [CrossRef]
- Psarras, A.; Emery, P.; Vital, E. Type I interferon-mediated autoimmune diseases: Pathogenesis, diagnosis and targeted therapy. Rheumatology 2017, 56, 1662–1675. [Google Scholar] [CrossRef]
- Skaug, B.; Assassi, S. Type I interferon dysregulation in Systemic Sclerosis. Cytokine 2019, 132, 154635. [Google Scholar] [CrossRef]
- Ewu, M.; Eassassi, S. The Role of Type 1 Interferon in Systemic Sclerosis. Front. Immunol. 2013, 4, 266. [Google Scholar] [CrossRef]
- Duan, H.; Fleming, J.; Pritchard, D.K.; Amon, L.M.; Xue, J.; Arnett, H.A.; Chen, G.; Breen, P.; Buckner, J.H.; Molitor, J.A.; et al. Combined analysis of monocyte and lymphocyte messenger RNA expression with serum protein profiles in patients with scleroderma. Arthritis Care Res. 2008, 58, 1465–1474. [Google Scholar] [CrossRef]
- Brkic, Z.; van Bon, L.; Cossu, M.; van Helden-Meeuwsen, C.G.; Vonk, M.C.; Knaapen, H.; Berg, W.V.D.; A Dalm, V.; Van Daele, P.L.; Severino, A.; et al. The interferon type I signature is present in systemic sclerosis before overt fibrosis and might contribute to its pathogenesis through high BAFF gene expression and high collagen synthesis. Ann. Rheum. Dis. 2015, 75, 1567–1573. [Google Scholar] [CrossRef]
- York, M.R.; Nagai, T.; Mangini, A.J.; Lemaire, R.; van Seventer, J.M.; Lafyatis, R. A macrophage marker, siglec-1, is increased on circulating monocytes in patients with systemic sclerosis and induced by type i interferons and toll-like receptor agonists. Arthritis Care Res. 2007, 56, 1010–1020. [Google Scholar] [CrossRef]
- Tan, F.K.; Zhou, X.; Mayes, M.D.; Gourh, P.; Guo, X.; Marcum, C.; Jin, L.; Arnett, F.C. Signatures of differentially regulated interferon gene expression and vasculotrophism in the peripheral blood cells of systemic sclerosis patients. Rheumatology 2006, 45, 694–702. [Google Scholar] [CrossRef]
- Mondini, M.; Vidali, M.; De Andrea, M.; Azzimonti, B.; Airò, P.; D’Ambrosio, R.; Riboldi, P.; Meroni, P.L.; Albano, E.; Shoenfeld, Y.; et al. A novel autoantigen to differentiate limited cutaneous systemic sclerosis from diffuse cutaneous systemic sclerosis: The interferon-inducible gene IFI16. Arthritis Care Res. 2006, 54, 3939–3944. [Google Scholar] [CrossRef]
- Oliveira, J.J.; Karrar, S.; Rainbow, D.B.; Pinder, C.L.; Clarke, P.; García, A.R.; Al-Assar, O.; Burling, K.; Morris, S.; Stratton, R.; et al. The plasma biomarker soluble SIGLEC-1 is associated with the type I interferon transcriptional signature, ethnic background and renal disease in systemic lupus erythematosus. Arthritis Res. Ther. 2018, 20, 152. [Google Scholar] [CrossRef]
- Pillai, S.; Netravali, I.A.; Cariappa, A.; Mattoo, H. Siglecs and Immune Regulation. Annu. Rev. Immunol. 2012, 30, 357–392. [Google Scholar] [CrossRef]
- Rose, T.; Szelinski, F.; Lisney, A.; Reiter, K.; Fleischer, S.J.; Burmester, G.R.; Radbruch, A.; Hiepe, F.; Grützkau, A.; Biesen, R.; et al. SIGLEC1 is a biomarker of disease activity and indicates extraglandular manifestation in primary Sjögren’s syndrome. RMD Open 2016, 2, e000292. [Google Scholar] [CrossRef]
- Graf, M.; von Stuckrad, S.L.; Uruha, A.; Klotsche, J.; Zorn-Pauly, L.; Unterwalder, N.; Buttgereit, T.; Krusche, M.; Meisel, C.; Burmester, G.R.; et al. SIGLEC1 enables straightforward assessment of type I interferon activity in idiopathic inflammatory myopathies. RMD Open 2022, 8, e001934. [Google Scholar] [CrossRef]
- Lerkvaleekul, B.; Veldkamp, S.R.; van der Wal, M.M.; Schatorjé, E.J.H.; Kamphuis, S.S.M.; Berg, J.M.V.D.; Muller, P.C.E.H.; Armbrust, W.; Vastert, S.J.; Wienke, J.; et al. Siglec-1 expression on monocytes is associated with the interferon signature in juvenile dermatomyositis and can predict treatment response. Rheumatology 2021, 61, 2144–2155. [Google Scholar] [CrossRef]
- Xiong, Y.-S.; Cheng, Y.; Lin, Q.-S.; Wu, A.-L.; Yu, J.; Li, C.; Sun, Y.; Zhong, R.-Q.; Wu, L.-J. Increased expression of Siglec-1 on peripheral blood monocytes and its role in mononuclear cell reactivity to autoantigen in rheumatoid arthritis. Rheumatology 2013, 53, 250–259. [Google Scholar] [CrossRef]
- Wu, Y.; Guo, Q.; Gong, X.; Sun, W.; Zhang, W.; Zhao, W.; Yang, Y.; Fan, C.; Li, Y.; Teng, W.; et al. Increased expression of Siglec-1 on peripheral blood monocytes and its relationship with inflammatory reaction in autoimmune thyroiditis. Chin. J. Endocrinol. Metab. 2019, 12, 99–104. [Google Scholar]
- Bao, G.; Han, Z.; Yan, Z.; Wang, Q.; Zhou, Y.; Yao, D.; Gu, M.; Chen, B.; Chen, S.; Deng, A.; et al. Increased Siglec-1 Expression in Monocytes of Patients with Primary Biliary Cirrhosis. Immunol. Investig. 2010, 39, 645–660. [Google Scholar] [CrossRef]
- Rose, T.; Grützkau, A.; Klotsche, J.; Enghard, P.; Flechsig, A.; Keller, J.; Riemekasten, G.; Radbruch, A.; Burmester, G.-R.; Dörner, T.; et al. Are interferon-related biomarkers advantageous for monitoring disease activity in systemic lupus erythematosus? A longitudinal benchmark study. Rheumatology 2017, 56, 1618–1626. [Google Scholar] [CrossRef]
- Biesen, R.; Demir, C.; Barkhudarova, F.; Grün, J.R.; Steinbrich-Zöllner, M.; Backhaus, M.; Häupl, T.; Rudwaleit, M.; Riemekasten, G.; Radbruch, A.; et al. Sialic acid-binding Ig-like lectin 1 expression in inflammatory and resident monocytes is a potential biomarker for monitoring disease activity and success of therapy in systemic lupus erythematosus. Arthritis Care Res. 2008, 58, 1136–1145. [Google Scholar] [CrossRef]
- Von Stuckrad, S.L.; Klotsche, J.; Biesen, R.; Lieber, M.; Thumfart, J.; Meisel, C.; Unterwalder, N.; Kallinich, T. SIGLEC1 (CD169) is a sensitive biomarker for the deterioration of the clinical course in childhood systemic lupus erythematosus. Lupus 2020, 29, 1914–1925. [Google Scholar] [CrossRef]
- Farina, G.; Lafyatis, D.; Lemaire, R. A four-gene biomarker predicts skin disease in patients with diffuse cutaneous systemic sclerosis. Arthritis Care Res. 2010, 62, 580–588. [Google Scholar] [CrossRef]
- Eloranta, M.-L.; Franck-Larsson, K.; Lövgren, T.; Kalamajski, S.; Rönnblom, A.; Rubin, K.; Alm, G.V.; Rönnblom, L. Type I interferon system activation and association with disease manifestations in systemic sclerosis. Ann. Rheum. Dis. 2010, 69, 1396–1402. [Google Scholar] [CrossRef]
- Christmann, R.B.; Hayes, E.; Pendergrass, S.; Padilla, C.; Farina, G.; Affandi, A.J.; Whitfield, M.L.; Farber, H.; Lafyatis, R. Interferon and alternative activation of monocyte/macrophages in systemic sclerosis-associated pulmonary arterial hypertension. Arthritis Care Res. 2011, 63, 1718–1728. [Google Scholar] [CrossRef]
- Melsens, K.; De Keyser, F.; Decuman, S.; Piette, Y.; Vandecasteele, E.; Smith, V. Disease activity indices in systemic sclerosis: A systematic literature review. Clin. Exp. Rheumatol. 2016, 34, 186–192. [Google Scholar]
- Mierau, R.; Moinzadeh, P.; Riemekasten, G.; Melchers, I.; Meurer, M.; Reichenberger, F.; Buslau, M.; Worm, M.; Blank, N.; Hein, R.; et al. Frequency of disease-associated and other nuclear autoantibodies in patients of the German network for systemic scleroderma: Correlation with characteristic clinical features. Arthritis Res. Ther. 2011, 13, R172. [Google Scholar] [CrossRef]
- Ciechomska, M.; Skalska, U. Targeting interferons as a strategy for systemic sclerosis treatment. Immunol. Lett. 2018, 195, 45–54. [Google Scholar] [CrossRef]
- Ciechomska, M.; Cant, R.; Finnigan, J.; van Laar, J.M.; O’Reilly, S. Role of toll-like receptors in systemic sclerosis. Expert Rev. Mol. Med. 2013, 15, e9. [Google Scholar] [CrossRef]
- Muskardin, T.L.W.; Niewold, T.B. Type I interferon in rheumatic diseases. Nat. Rev. Rheumatol. 2018, 14, 214–228. [Google Scholar] [CrossRef] [PubMed]
- Theofilopoulos, A.N.; Baccala, R.; Beutler, B.; Kono, D.H. Type I interferons (α/β) in immunity and autoimmunity. Annu. Rev. Immunol. 2005, 23, 307–336. [Google Scholar] [CrossRef] [PubMed]
- Siegert, E.; Uruha, A.; Goebel, H.-H.; Preuße, C.; Casteleyn, V.; Kleefeld, F.; Alten, R.; Burmester, G.R.; Schneider, U.; Höppner, J.; et al. Systemic sclerosis-associated myositis features minimal inflammation and characteristic capillary pathology. Acta Neuropathol. 2021, 141, 917–927. [Google Scholar] [CrossRef] [PubMed]
- Sacre, K.; A Criswell, L.; McCune, J.M. Hydroxychloroquine is associated with impaired interferon-alpha and tumor necrosis factor-alpha production by plasmacytoid dendritic cells in systemic lupus erythematosus. Arthritis Res. Ther. 2012, 14, R155. [Google Scholar] [CrossRef]
- Christmann, R.B.; Sampaio-Barros, P.; Stifano, G.; Borges, C.L.; Carvalho, C.; Kairalla, R.; Parra, E.R.; Spira, A.; Simms, R.; Capellozzi, V.L.; et al. Association of Interferon- and Transforming Growth Factor β-Regulated Genes and Macrophage Activation With Systemic Sclerosis-Related Progressive Lung Fibrosis. Arthritis Rheumatol. 2013, 66, 714–725. [Google Scholar] [CrossRef]
- Furie, R.; Khamashta, M.; Merrill, J.T.; Werth, V.P.; Kalunian, K.; Brohawn, P.; Illei, G.G.; Drappa, J.; Wang, L.; Yoo, S. Anifrolumab, an Anti-Interferon-α Receptor Monoclonal Antibody, in Moderate-to-Severe Systemic Lupus Erythematosus. Arthritis Rheumatol. 2017, 69, 376–386. [Google Scholar] [CrossRef]
- Morand, E.F.; Furie, R.; Tanaka, Y.; Bruce, I.N.; Askanase, A.D.; Richez, C.; Bae, S.-C.; Brohawn, P.Z.; Pineda, L.; Berglind, A.; et al. Trial of Anifrolumab in Active Systemic Lupus Erythematosus. N. Engl. J. Med. 2020, 382, 211–221. [Google Scholar] [CrossRef]
- Kubo, S.; Nakayamada, S.; Sakata, K.; Kitanaga, Y.; Ma, X.; Lee, S.; Ishii, A.; Yamagata, K.; Nakano, K.; Tanaka, Y. Janus Kinase Inhibitor Baricitinib Modulates Human Innate and Adaptive Immune System. Front. Immunol. 2018, 9, 1510. [Google Scholar] [CrossRef]
- Burmester, G.R.; Blanco, R.; Charles-Schoeman, C.; Wollenhaupt, J.; Zerbini, C.; Benda, B.; Gruben, D.; Wallenstein, G.; Krishnaswami, S.; Zwillich, S.H.; et al. Tofacitinib (CP-690,550) in combination with methotrexate in patients with active rheumatoid arthritis with an inadequate response to tumour necrosis factor inhibitors: A randomised phase 3 trial. Lancet 2013, 381, 451–460. [Google Scholar] [CrossRef]
- Guo, X.; Higgs, B.; Bay-Jensen, A.C.; Karsdal, M.A.; Yao, Y.; Roskos, L.K.; White, W.I. Suppression of T Cell Activation and Collagen Accumulation by an Anti-IFNAR1 mAb, Anifrolumab, in Adult Patients with Systemic Sclerosis. J. Investig. Dermatol. 2015, 135, 2402–2409. [Google Scholar] [CrossRef]
- Karalilova, R.V.; Batalov, Z.A.; Sapundzhieva, T.L.; Matucci-Cerinic, M.; Batalov, A.Z. Tofacitinib in the treatment of skin and musculoskeletal involvement in patients with systemic sclerosis, evaluated by ultrasound. Rheumatol. Int. 2021, 41, 1743–1753. [Google Scholar] [CrossRef]
- You, H.; Xu, D.; Hou, Y.; Zhou, J.; Wang, Q.; Li, M.; Zeng, X. Tofacitinib as a possible treatment for skin thickening in diffuse cutaneous systemic sclerosis. Rheumatology 2020, 60, 2472–2477. [Google Scholar] [CrossRef]
- Hesselstrand, R.; Distler, J.H.W.; Riemekasten, G.; Wuttge, D.M.; Törngren, M.; Nyhlén, H.C.; Andersson, F.; Eriksson, H.; Sparre, B.; Tuvesson, H.; et al. An open-label study to evaluate biomarkers and safety in systemic sclerosis patients treated with paquinimod. Arthritis Res. Ther. 2021, 23, 204. [Google Scholar] [CrossRef]
- Calderon, L.M.; Pope, J.E. Precursors to Systemic Sclerosis and Systemic Lupus Erythematosus: From Undifferentiated Connective Tissue Disease to the Development of Identifiable Connective Tissue Diseases. Front. Immunol. 2022, 13, 869172. [Google Scholar] [CrossRef]
- Ortega-Hernandez, O.-D.; Shoenfeld, Y. Mixed connective tissue disease: An overview of clinical manifestations, diagnosis and treatment. Best Pract. Res. Clin. Rheumatol. 2012, 26, 61–72. [Google Scholar] [CrossRef]
- Zorn-Pauly, L.; von Stuckrad, A.S.L.; Klotsche, J.; Rose, T.; Kallinich, T.; Enghard, P.; Ostendorf, L.; Burns, M.; Doerner, T.; Meisel, C.; et al. Evaluation of SIGLEC1 in the diagnosis of suspected systemic lupus erythematosus. Rheumatology 2021, 61, 3396–3400. [Google Scholar] [CrossRef]
- Van den Hoogen, F.; Khanna, D.; Fransen, J.; Johnson, S.R.; Baron, M.; Tyndall, A.; Matucci-Cerinic, M.; Naden, R.P.; Medsger, T.A., Jr.; Carreira, P.E.; et al. 2013 classification criteria for systemic sclerosis: An American college of rheumatology/European league against rheumatism collaborative initiative. Ann. Rheum. Dis. 2013, 72, 1747–1755. [Google Scholar] [CrossRef]
- Aringer, M.; Costenbader, K.; Daikh, D.; Brinks, R.; Mosca, M.; Ramsey-Goldman, R.; Smolen, J.S.; Wofsy, D.; Boumpas, D.T.; Kamen, D.L.; et al. 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol. 2019, 71, 1400–1412. [Google Scholar] [CrossRef]
- Shiboski, C.H.; Shiboski, S.C.; Seror, R.; Criswell, L.A.; Labetoulle, M.; Lietman, T.M.; Rasmussen, A.; Scofield, H.; Vitali, C.; Bowman, S.J.; et al. 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjögren’s syndrome: A consensus and data-driven methodology involving three international patient cohorts. Ann. Rheum. Dis. 2017, 69, 35–45. [Google Scholar] [CrossRef]
- Alarcon-Segovia, D.; Villarreal, M.; Kasukawa, R.; Sharp, G.C. Classification and diagnostic criteria for mixed connective tissue disease. In Mixed Connective Tissue Disease and Anti-Nuclear Antibodies; Elsvier Science Publishers B.V. (Biomedical Division): Amsterdam, The Netherlands, 1987; pp. 33–40. [Google Scholar]
- Lundberg, I.E.; Tjärnlund, A.; Bottai, M.; Werth, V.P.; Pilkington, C.; De Visser, M.; Alfredsson, L.; A Amato, A.; Barohn, R.J.; Liang, M.H.; et al. 2017 European League Against Rheumatism/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Ann. Rheum. Dis. 2017, 76, 1955–1964. [Google Scholar] [CrossRef]
- Kay, J.; Upchurch, K.S. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatology 2012, 51 (Suppl. 6), vi5–vi9. [Google Scholar] [CrossRef] [PubMed]

| SSc | SLE | pSS | MCTD | UCTD | IIM | RA | HC | ||
|---|---|---|---|---|---|---|---|---|---|
| n = 203 | n = 32 | n = 16 | n = 8 | n = 14 | n = 26 | n = 23 | n = 13 | ||
| Sex | |||||||||
| No. (%) female | 171 (84.2) | 28 (87.5) | 15 (93.8) | 8 (100.0) | 9 (64.3) | 16 (61.5) | 17 (73.9) | 10 (76.9) | |
| No. (%) male | 32 (15.8) | 4 (12.5) | 1 (6.2) | 0 (0.0) | 5 (35.7) | 10 (38.5) | 6 (26.1) | 3 (23.1) | |
| Age (mean ± SD; yrs) | 57.84 ± 14.31 | 41.45 ± 12.70 | 66.00 ± 9.69 | 56.63 ± 19.15 | 58.93 ± 11.57 | 61.85 ± 14.42 | 62.44 ± 14.69 | 55.95 ± 15.49 | |
| At diagnosis | 46.67 ± 14.80 | 31.56 ± 12.31 | 56.75 ± 11.96 | 41.60 ± 23.36 | 58.00 ± 8.91 | 59.14 ± 15.29 | 51.83 ± 17.33 | N/A | |
| Disease duration (mean ± SD; yrs) | 10.15 ± 8.81 | 8.83 ± 8.58 | 8.17 ± 6.45 | 9.80 ± 9.42 | 0.50 ± 0.58 | 3.00 ± 2.77 | 10.72 ± 12.02 | N/A | |
| Antinuclear antibody positive, no. (%) | 186 (92.1%) | 31 (96.9%) | 15 (93.7) | 8 (100%) | 12 (85.5) | 15 (57.7) | 8 (34.8%) | 2 (15.3) | |
| All SSc Patients (n = 203) | Negative SIGELC-1 Signature (n = 158) | Positive SIGLEC-1 Signature (n = 45) | p Value | ||
|---|---|---|---|---|---|
| Cutaneous subset—n (%) | |||||
| diffuse (dcSSc) | 64 (31.5) | 47 (29.7) | 17 (37.8) | 0.306 | |
| limited (lcSSc) | 122 (60.1) | 99 (62.7) | 23 (51.1) | 0.163 | |
| sine scleroderma (ssSSc) | 17 (8.4) | 12 (7.6) | 5 (11.1) | 0.453 | |
| Immunological findings | |||||
| ANA | 186 (94.4) | 147 (93.0) | 39 (86.7) | 0.825 | |
| ACA | 71 (35.0) | 58 (36.7) | 13 (18.3) | 0.332 | |
| Topo-1 | 76 (37.4) | 58 (36.7) | 18 (28.9) | 0.687 | |
| RP3 | 16 (7.9) | 11 (7.0) | 5 (11.1) | 0.339 | |
| SSc organ manifestations, n (%) | |||||
| Raynaud’s phenomenon | 181 (89.2) | 144 (91.1) | 37 (82.2) | 0.090 | |
| ILD | 91 (44.8) | 70 (44.3) | 21 (46.7) | 0.779 | |
| PAH | 19 (9.4) | 15 (9.5) | 4 (8.9) | 0.902 | |
| DU | 97 (47.8) | 76 (48.1) | 21 (46.7) | 0.865 | |
| Cardiac involvement | 12 (5.9) | 7 (4.4) | 5 (11.1) | 0.094 | |
| SRC | 8 (3.9) | 5 (3.2) | 3 (6.7) | 0.287 | |
| Myositis | 10 (4.9) | 8 (5.1) | 2 (4.4) | 0.866 | |
| Laboratory values (mean ± SD) | |||||
| NT-pro-BNP—ng/L | 451.09 ± 1174.33 | 392.14 ± 947.07 | 646.29 ± 1726.65 | 0.204 | |
| CRP—mg/dl | 4.36 ± 9.70 | 4.00 ± 9.72 | 5.78 ± 9.60 | 0.279 | |
| Hb—mg/dl | 13.10 ± 1.62 | 13.10 ± 1.62 | 13.15 ± 166 | 0.815 | |
| Neutrophil granulocytes | 5.54 ± 2.63 | 5.66 ± 2.67 | 5.15 ± 2.46 | 0.275 | |
| Cardiopulmonary parameters (mean ± SD) | |||||
| FVC—%/exp. | 89.27 ± 20.16 | 91.34 ± 20.10 | 81.40 ± 18.70 | 0.007 | |
| FEV1—%/exp. | 86.30 ± 20.78 | 87.20 ± 21.53 | 83.00 ± 17.66 | 0.283 | |
| DLCO—%/exp. | 57.29 ± 18.91 | 58.29 ± 19.49 | 53.49 ± 16.19 | 0.195 | |
| LVEF—%/exp. | 62.27 ± 9.63 | 63.03 ± 9.08 | 59.44 ± 11.22 | 0.098 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Höppner, J.; Casteleyn, V.; Biesen, R.; Rose, T.; Windisch, W.; Burmester, G.R.; Siegert, E. SIGLEC-1 in Systemic Sclerosis: A Useful Biomarker for Differential Diagnosis. Pharmaceuticals 2022, 15, 1198. https://doi.org/10.3390/ph15101198
Höppner J, Casteleyn V, Biesen R, Rose T, Windisch W, Burmester GR, Siegert E. SIGLEC-1 in Systemic Sclerosis: A Useful Biomarker for Differential Diagnosis. Pharmaceuticals. 2022; 15(10):1198. https://doi.org/10.3390/ph15101198
Chicago/Turabian StyleHöppner, Jakob, Vincent Casteleyn, Robert Biesen, Thomas Rose, Wolfram Windisch, Gerd Rüdiger Burmester, and Elise Siegert. 2022. "SIGLEC-1 in Systemic Sclerosis: A Useful Biomarker for Differential Diagnosis" Pharmaceuticals 15, no. 10: 1198. https://doi.org/10.3390/ph15101198
APA StyleHöppner, J., Casteleyn, V., Biesen, R., Rose, T., Windisch, W., Burmester, G. R., & Siegert, E. (2022). SIGLEC-1 in Systemic Sclerosis: A Useful Biomarker for Differential Diagnosis. Pharmaceuticals, 15(10), 1198. https://doi.org/10.3390/ph15101198









