The Growing Skyline of Advanced Hepatocellular Carcinoma Treatment: A Review
Abstract
1. Introduction
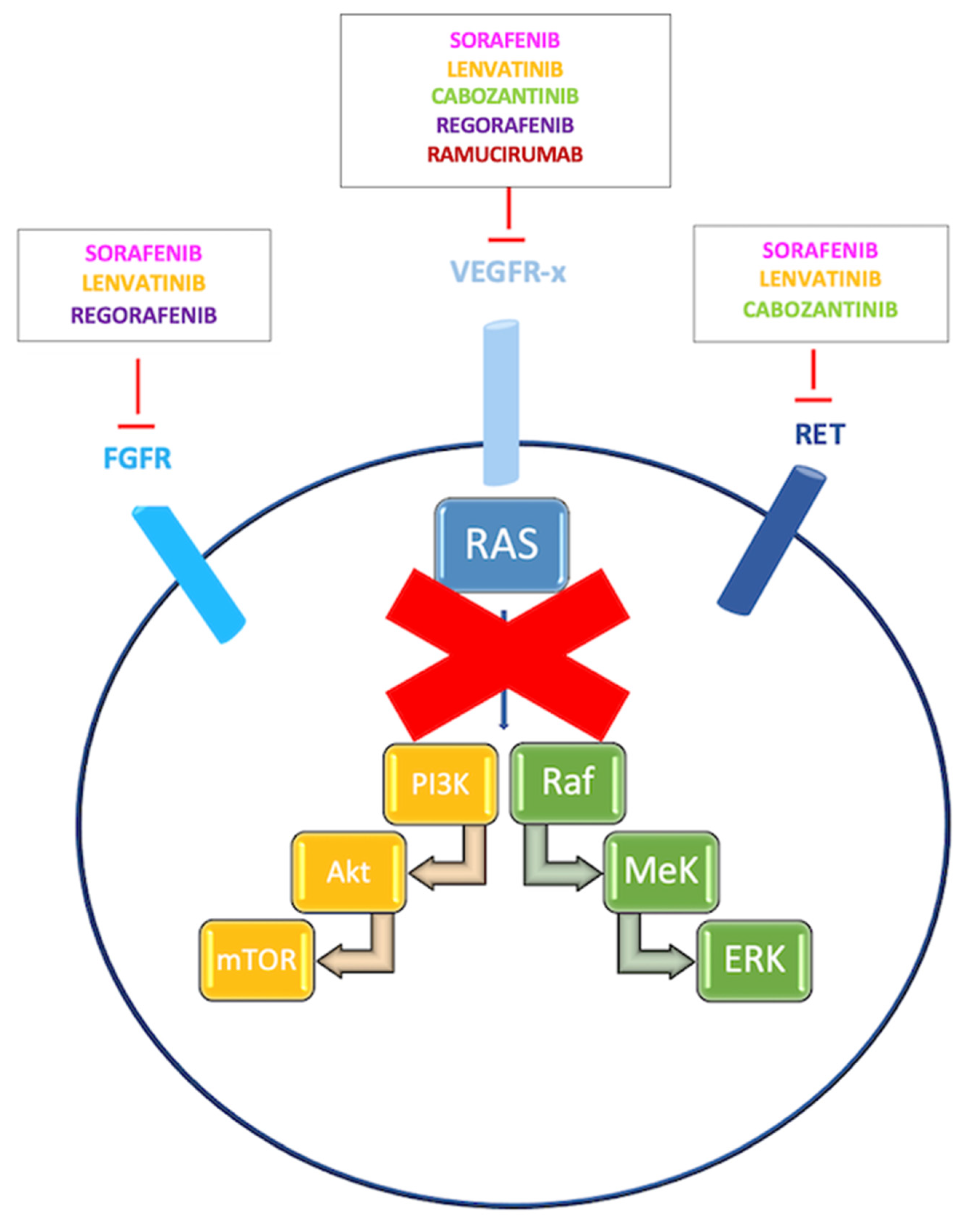
2. Target Therapies
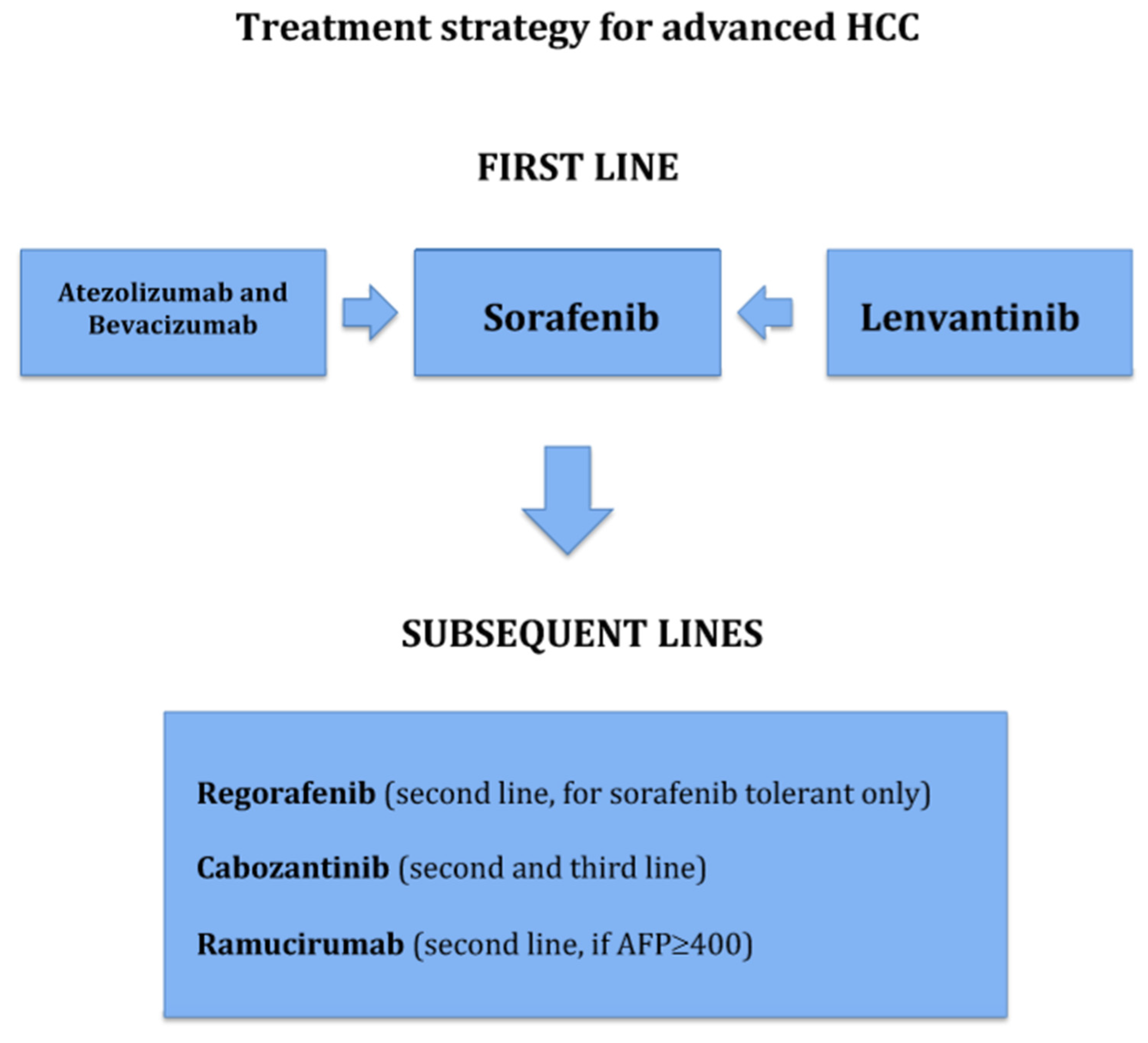
2.1. First-Line of Treatment
2.1.1. Sorafenib
2.1.2. Lenvantinib
2.2. Subsequent Lines of Treatment
2.2.1. Regorafenib
2.2.2. Cabozantinib
2.2.3. Ramucirumab
3. Immune Checkpoint Inhibitor (ICI) Monotherapy
3.1. Anti-PD-1
3.1.1. First-Line of Treatment
3.1.2. Second-Line of treatment
3.2. Anti-PD-L1
4. Chemotherapy
5. Combination Therapies
5.1. ICIs + ICIs
5.2. ICIs + Target Therapies
5.3. ICIs + anti-VEGF
5.4. ICIs + TKI
6. Defining the Best Sequencing Strategy
7. Unmet Needs and Future Perspectives
7.1. Neoadjuvant/Adjuvant Setting
7.2. Timely Transitioning from Loco-Regional to Systemic Treatments
7.3. Predictive Biomarkers
7.4. Radiomics
8. Impact of COVID-19 Pandemic at a Glance
9. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Villanueva, A. Hepatocellular carcinoma. N. Engl. J. Med. 2019, 380, 1450–1462. [Google Scholar] [CrossRef]
- Center, M.M.; Jemal, A. International trends in liver cancer incidence rates. Cancer Epidemiol. Biomark. Prev. 2011. [Google Scholar] [CrossRef]
- Midorikawa, Y.; Yamamoto, S.; Tatsuno, K.; Renard-Guillet, C.; Tsuji, S.; Hayashi, A.; Ueda, H.; Fukuda, S.; Fujita, T.; Katoh, H.; et al. Accumulation of Molecular Aberrations Distinctive to Hepatocellular Carcinoma Progression. Cancer Res. 2020, 80, 3810–3819. [Google Scholar] [CrossRef]
- Ghouri, Y.A.; Mian, I.; Rowe, J.H. Review of hepatocellular carcinoma: Epidemiology, etiology, and carcinogenesis. J. Carcinog. 2017. [Google Scholar] [CrossRef]
- Morse, M.A.; Sun, W.; Kim, R.; He, A.R.; Abada, P.B.; Mynderse, M.; Finn, R.S. The role of angiogenesis in hepatocellular carcinoma. Clin. Cancer Res. 2019. [Google Scholar] [CrossRef] [PubMed]
- Nigussie Mekuria, A.; Degaga Abdi, A. Potential Molecular Targets and Drugs for Treatment of Hepatocellular Carcinoma. J. Cancer Sci. Ther. 2017. [Google Scholar] [CrossRef]
- Hernandez-Gea, V.; Toffanin, S.; Friedman, S.L.; Llovet, J.M. Role of the microenvironment in the pathogenesis and treatment of hepatocellular carcinoma. Gastroenterology 2013. [Google Scholar] [CrossRef]
- Wu, S.D.; Ma, Y.S.; Fang, Y.; Liu, L.L.; Fu, D.; Shen, X.Z. Role of the microenvironment in hepatocellular carcinoma development and progression. Cancer Treat. Rev. 2012. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.X.; Qiu, X.Y.; Hu, D.X.; Chen, X.Q. Advances in hypoxia-mediated mechanisms in hepatocellular Carcinoma. Mol. Pharmacol. 2017. [Google Scholar] [CrossRef]
- Boland, P.; Wu, J. Systemic therapy for hepatocellular carcinoma: Beyond sorafenib. Chin. Clin. Oncol. 2018. [Google Scholar] [CrossRef]
- A new prognostic system for hepatocellular carcinoma: A retrospective study of 435 patients: The Cancer of the Liver Italian Program (CLIP) investigators. Hepatology 1998, 28, 751–755. [CrossRef] [PubMed]
- Granito, A.; Bolondi, L. Non-transplant therapies for patients with hepatocellular carcinoma and Child-Pugh-Turcotte class B cirrhosis. Lancet Oncol. 2017, 18, e101–e112. [Google Scholar] [CrossRef]
- Johnson, P.J.; Berhane, S.; Kagebayashi, C.; Satomura, S.; Teng, M.; Reeves, H.; O’Beirne, J.; Fox, R.; Skowronska, A.; Palmer, D.; et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based Approach-The ALBI grade. J. Clin. Oncol. 2015, 33, 550–558. [Google Scholar] [CrossRef]
- Kim, J.E.; Ryoo, B.Y.; Ryu, M.H.; Chang, H.M.; Suh, D.J.; Lee, H.C.; Lim, Y.S.; Kim, K.M.; Kang, Y.K. Sorafenib for hepatocellular carcinoma according to Child-Pugh class of liver function. Cancer Chemother. Pharmacol. 2011, 68, 1285–1290. [Google Scholar] [CrossRef]
- McNamarra, M.G.; Slagter, A.E.; Nuttall, C.; Frizziero, M.; Pihlak, R.; Lamarca, A.; Tariq, N.; Valle, J.W.; Hubner, R.A.; Knox, J.J.; et al. Sorafenib as first-line therapy in patients with Child-Pugh B hepatocellular carcinoma- a meta-analysis. Eur. J. Cancer 2018, 105, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bruix, J.; Gores, G.G.; Mazzaferro, V. Hepatocellular carcinoma: Clinical frontiers and perspectives. NIH Public Access 2014, 63, 844–855. [Google Scholar] [CrossRef] [PubMed]
- Dimri, M.; Satyanarayana, A. Molecular signaling pathways and therapeutic targets in hepatocellular carcinoma. Cancers 2020, 12, 491. [Google Scholar] [CrossRef] [PubMed]
- Faivre, S.; Rimassa, L.; Finn, R.S. Molecular therapies for HCC: Looking outside the box. J. Hepatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M. Targeted and immune therapies for hepatocellular carcinoma: Predictions for 2019 and beyond. World J. Gastroenterol. 2019. [Google Scholar] [CrossRef]
- Chen, J.; Jin, R.; Zhao, J.; Liu, J.; Ying, H.; Yan, H.; Zhou, S.; Liang, Y.; Huang, D.; Liang, X.; et al. Potential molecular, cellular and microenvironmental mechanism of sorafenib resistance in hepatocellular carcinoma. Cancer Lett. 2015. [Google Scholar] [CrossRef]
- Kohga, K.; Takehara, T.; Tatsumi, T.; Ishida, H.; Miyagi, T.; Hosui, A.; Hayashi, N. Sorafenib inhibits the shedding of major histocompatibility complex class i-related chain a on hepatocellular carcinoma cells by down-regulating a disintegrin and metalloproteinase. Hepatology 2010. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Cao, Q.; Wen, W.; Wang, H. Targeted therapy for hepatocellular carcinoma: Challenges and opportunities. Cancer Lett. 2019. [Google Scholar] [CrossRef] [PubMed]
- Kane, R.C.; Farrell, A.T.; Madabushi, R.; Booth, B.; Chattopadhyay, S.; Sridhara, R.; Justice, R.; Pazdur, R. Sorafenib for the Treatment of Unresectable Hepatocellular Carcinoma. Oncologist 2009. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.L.; Kang, Y.K.; Lin, D.Y.; Park, J.W.; Kudo, M.; Qin, S.; Chung, H.C.; Song, X.; Xu, J.; Poggi, G.; et al. Sunitinib versus sorafenib in advanced hepatocellular cancer: Results of a randomized phase III trial. J. Clin. Oncol. 2013. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.J.; Qin, S.; Park, J.W.; Poon, R.T.; Raoul, J.L.; Philip, P.A.; Hsu, C.H.; Hu, T.H.; Heo, J.; Xu, J.; et al. Brivanib versus sorafenib as first-line therapy in patients with unresectable, advanced hepatocellular carcinoma: Results from the randomized phase III BRISK-FL study. J. Clin. Oncol. 2013. [Google Scholar] [CrossRef]
- Zhu, A.X.; Rosmorduc, O.; Evans, T.R.; Ross, P.J.; Santoro, A.; Carrilho, F.J.; Bruix, J.; Qin, S.; Thuluvath, P.J.; Llovet, J.M.; et al. Search: A phase III, randomized, double-blind, placebo-controlled trial of sorafenib plus erlotinib in patients with advanced hepatocellular carcinoma. J. Clin. Oncol. 2015. [Google Scholar] [CrossRef]
- Cainap, C.; Qin, S.; Huang, W.T.; Chung, I.J.; Pan, H.; Cheng, Y.; Kudo, M.; Kang, Y.K.; Chen, P.J.; Toh, H.C.; et al. Linifanib versus sorafenib in patients with advanced hepatocellular carcinoma: Results of a randomized phase III trial. J. Clin. Oncol. 2015. [Google Scholar] [CrossRef]
- Zhu, A.X.; Ancukiewicz, M.; Supko, J.G.; Sahani, D.V.; Blaszkowsky, L.S.; Meyerhardt, J.A.; Abrams, T.A.; McCleary, N.J.; Bhargava, P.; Muzikansky, A.; et al. Efficacy, safety, pharmacokinetics, and biomarkers of cediranib monotherapy in advanced hepatocellular carcinoma: A phase II study. Clin. Cancer Res. 2013. [Google Scholar] [CrossRef]
- Cheng, A.L.; Thongprasert, S.; Lim, H.Y.; Sukeepaisarnjaroen, W.; Yang, T.S.; Wu, C.C.; Chao, Y.; Chan, S.L.; Kudo, M.; Ikeda, M.; et al. Randomized, open-label phase 2 study comparing frontline dovitinib versus sorafenib in patients with advanced hepatocellular carcinoma. Hepatology 2016. [Google Scholar] [CrossRef]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.W.; Han, G.; Jassem, J.; et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A d phase 3 non-inferiority trial. Lancet 2018. [Google Scholar] [CrossRef]
- Capozzi, M.; De Divitiis, C.; Ottaiano, A.; Von Arx, C.; Scala, S.; Tatangelo, F.; Delrio, P.; Tafuto, S. Lenvatinib, a molecule with versatile application: From preclinical evidence to future development in anti-cancer treatment. Cancer Manag. Res. 2019. [Google Scholar] [CrossRef]
- Liu, Z.; Lin, Y.; Zhang, J.; Zhang, Y.; Li, Y.; Liu, Z.; Li, Q.; Luo, M.; Liang, R.; Ye, J. Molecular targeted and immune checkpoint therapy for advanced hepatocellular carcinoma. J. Exp. Clin. Cancer Res. 2019. [Google Scholar] [CrossRef] [PubMed]
- Bruix, J.; Qin, S.; Merle, P.; Granito, A.; Huang, Y.H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Breder, V.; et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017. [Google Scholar] [CrossRef]
- Finn, R.S.; Merle, P.; Granito, A.; Huang, Y.H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Gerolami, R.; Caparello, C.; et al. Outcomes of sequential treatment with sorafenib followed by regorafenib for HCC: Additional analyses from the phase III RESORCE trial. J. Hepatol. 2018. [Google Scholar] [CrossRef]
- Yoo, C.; Park, J.W.; Kim, Y.J.; Kim, D.Y.; Yu, S.J.; Lim, T.S.; Lee, S.J.; Ryoo, B.Y.; Lim, H.Y. Multicenter retrospective analysis of the safety and efficacy of regorafenib after progression on sorafenib in Korean patients with hepatocellular carcinoma. Investig. New Drugs 2019. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.; Yang, X.R.; Chung, W.Y.; Dennison, A.R.; Zhou, J. Targeted therapy for hepatocellular carcinoma. Signal Transduct. Target. Ther. 2020. [Google Scholar] [CrossRef] [PubMed]
- Abou-Alfa, G.K.; Meyer, T.; Cheng, A.-L.; El-Khoueiry, A.B.; Rimassa, L.; Ryoo, B.-Y.; Cicin, I.; Merle, P.; Chen, Y.H.; Park, J.-W.; et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N. Engl. J. Med. 2018. [Google Scholar] [CrossRef]
- Chau, I.; Peck-Radosavljevic, M.; Borg, C.; Malfertheiner, P.; Seitz, J.F.; Park, J.O.; Ryoo, B.Y.; Yen, C.J.; Kudo, M.; Poon, R.; et al. Ramucirumab as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib: Patient-focused outcome results from the randomised phase III REACH study. Eur. J. Cancer 2017. [Google Scholar] [CrossRef]
- Zhu, A.X.; Park, J.O.; Ryoo, B.Y.; Yen, C.J.; Poon, R.; Pastorelli, D.; Blanc, J.F.; Chung, H.C.; Baron, A.D.; Pfiffer, T.E.; et al. Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): A randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2015. [Google Scholar] [CrossRef]
- Kudo, M.; Hatano, E.; Ohkawa, S.; Fujii, H.; Masumoto, A.; Furuse, J.; Wada, Y.; Ishii, H.; Obi, S.; Kaneko, S.; et al. Ramucirumab as second-line treatment in patients with advanced hepatocellular carcinoma: Japanese subgroup analysis of the REACH trial. J. Gastroenterol. 2017. [Google Scholar] [CrossRef]
- Zhu, A.X.; Kang, Y.K.; Yen, C.J.; Finn, R.S.; Galle, P.R.; Llovet, J.M.; Assenat, E.; Brandi, G.; Pracht, M.; Lim, H.Y.; et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019. [Google Scholar] [CrossRef]
- Kruger, S.; Ilmer, M.; Kobold, S.; Cadilha, B.L.; Endres, S.; Ormanns, S.; Schuebbe, G.; Renz, B.W.; D’Haese, J.G.; Schloesser, H.; et al. Advances in cancer immunotherapy 2019—Latest trends. J. Exp. Clin. Cancer Res. 2019, 38, 268. [Google Scholar] [CrossRef] [PubMed]
- Iñarrairaegui, M.; Melero, I.; Sangro, B. Immunotherapy of Hepatocellular Carcinoma: Facts and Hopes. Clin. Cancer Res. 2018, 24, 1518–1524. [Google Scholar] [CrossRef]
- Yarchoan, M.; Xing, D.; Luan, L.; Xu, H.; Sharma, R.B.; Popovic, A.; Pawlik, T.M.; Kim, A.K.; Zhu, Q.; Jaffee, E.M. Characterization of the Immune Microenvironment in Hepatocellular Carcinoma. Clin Cancer Res. 2017, 23, 7333–7339. [Google Scholar] [CrossRef] [PubMed]
- Salmaninejad, A.; Valilou, S.F.; Shabgah, A.G.; Alimardani, M.; Pasdar, A.; Sahebkar, A. PD-1/PD-L1 pathway: Basic biology and role in cancer immunotherapy. J. Cell Physiol. 2019, 234, 16824–16837. [Google Scholar] [CrossRef]
- Buchbinder, E.I.; Desai, A. CTLA-4 and PD-1 Pathways: Similarities, Differences, and Implications of Their Inhibition. Am. J. Clin. Oncol. 2016, 39, 98–106. [Google Scholar] [CrossRef]
- Ko, K.; Mak, L.-Y.; Cheung, K.-S.; Yuen, M.-F. Hepatocellular carcinoma: Recent advances and emerging medical therapies. F1000Research 2020, 9, 620. [Google Scholar] [CrossRef]
- El-Khoueiry, A.B.; Sangro, B.; Yau, T.; Crocenzi, T.S.; Kudo, M.; Hsu, C.; Kim, T.Y.; Choo, S.P.; Trojan, J.; Welling THRd Meyer, T.; et al. Nivolumab in patients with advanced hepatocellular carcinoma (checkMate 040): An open label, non-comparative phase ½ dose escalation and expansion trial. Lancet. 2017, 389, 2492–2502. [Google Scholar] [CrossRef]
- FDA Grants Accelerated Approval to Nivolumab for HCC Previously Treated with Sorafenib. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-nivolumab-hcc-previously-treated-sorafenib (accessed on 10 October 2020).
- Yau, T.; Park, J.W.; Finn, R.S.; Cheng, A.; Mathurin, P.; Edeline, J.; Kudo, M.; Han, K.; Harding, J.J.; Merle, P.; et al. LBA38_PR CheckMate 459: A randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first- line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann. Oncol. 2019, 30 (Suppl. 5), v851–v934. [Google Scholar] [CrossRef]
- Sangro, B.; Park, J.; Finn, R.; Cheng, A.; Mathurin, P.; Edeline, J.; Kudo, M.; Han, K.; Harding, J.; Merle, P.; et al. LBA-3 CheckMate 459: Long-term (minimum follow-up 33.6 months) survival outcomes with nivolumab versus sorafenib as first-line treatment in patients with advanced hepatocellular carcinoma. Ann. Oncol. 2020, 31 (Suppl. 3), S241–S242. [Google Scholar] [CrossRef]
- Dahan, R.; Sega, E.; Engelhardt, J.; Selby, M.; Korman, A.J.; Ravetch, J.V. FcγRs modulate the anti-tumor activity of antibodies targeting thePD-1/PD-L1 axis. Cancer Cell. 2015, 28, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Deva, S.; Lee, J.-S.; Lin, C.-C.; Yen, C.-J.; Millward, M.; Chao, Y.; Keam, B.; Jameson, M.; Hou, M.-M.; Kang, Y.-K.; et al. A PhaseIA/IB trial of tislelizumab, an anti-PD-1 antibody, in patients with advanced solid tumors. Ann. Oncol. 2018, 29 (Suppl. 8), 700. [Google Scholar] [CrossRef]
- Qin, S.; Finn, R.S.; Kudo, M.; Meyer, T.; Vogel, A.; Ducreux, M.; Macarulla, T.M.; Tomasello, G.; Boisserie, F.; Hou, J.; et al. RATIONALE 301 study: Tislelizumab versus sorafenib as first-line treatment for unresectable hepatocellular carcinoma. Future Oncol. 2019, 15, 1811–1822. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.X.; Finn, R.S.; Edeline, J.; Cattan, S.; Ogasawara, S.; Palmer, D.; Verslype, C.; Zagonel, V.; Fartoux, L.; Vogel, A.; et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): A non-randomised, open-label phase 2 trial. Lancet Oncol. 2018, 19, 940–952. [Google Scholar] [CrossRef]
- FDA Grants Accelerated Approval to Pembrolizumab for Hepatocellular Carcinoma. Available online: https://www.fda.gov/drugs/fda-grants-accelerated-approval-pembrolizumab-hepatocellular-carcinoma (accessed on 10 October 2020).
- Finn, R.S.; Ryoo, B.Y.; Merle, P.; Kudo, M.; Bouattour, M.; Lim, H.Y.; Breder, V.; Edeline, J.; Chao, Y.; Ogasawara, S.; et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: A ran- domized, double-blind, phase III trial. J. Clin. Oncol. 2020, 38, 193–202. [Google Scholar] [CrossRef]
- Wainberg, Z.A.; Segal, N.H.; Jaeger, D.; Lee, K.-H.; Marshall, J.; Antonia, S.J.; Butler, M.; Sanborn, R.E.; Nemunaitis, J.; Carlson, C.A.; et al. Safety and clinical activity of durvalumab monotherapy in patients with hepatocellular carcinoma (HCC). J. Clin. Oncol. 2017, 35, 4071. [Google Scholar] [CrossRef]
- Phase II Study of Avelumab in Patients with Advanced Hepatocellular Carcinoma After Prior Sorafenib Treatment (Avelumab HCC). Available online: https://clinicaltrials.gov/ct2/show/NCT03389126 (accessed on 10 October 2020). [CrossRef]
- Pinato, D.J.; Guerra, N.; Fessas, P.; Murphy, R.; Mineo, T.; Mauri, F.A.; Mukherjee, S.K.; Thursz, M.; Wong, C.N.; Sharma, R.; et al. Immune-based therapies for hepatocellular carcinoma. Oncogene 2020, 39, 3620–3637. [Google Scholar] [CrossRef] [PubMed]
- Casadei Gardini, A.; Foca, F.; Scartozzi, M.; Silvestris, N.; Tamburini, E.; Faloppi, L.; Brunetti, O.; Rudnas, B.; Pisconti, S.; Valgiusti, M.; et al. Metronomic capecitabine versus best supportive care as second line treatmentm in hepatocellular carcinoma: A retrospective study. Sci. Rep. 2017, 7, 42499. [Google Scholar] [CrossRef]
- Trevisani, F.; Brandi, G.; Garuti, F.; Barbera, M.A.; Tortora, R.; Casadei Gardini, A.; Granito, A.; Tovoli, F.; De Lorenzon, S.; Inghilesi, A.L.; et al. Metronomic capecitabine as second-line treatment dor hepatocellular carcinoma after sorafenib discontinuation. J. Cancer Res. Clin. Oncol. 2018, 144, 403–414. [Google Scholar] [CrossRef]
- Buchbinder, E.I.; Desai, A. CTLA-4 and PD-1 pathways. Annu. Clin. Oncol. 2016, 39, 98–106. [Google Scholar] [CrossRef]
- Chen, D.S.; Mellman, I. Oncology meets immunology: The cancer-immunity cycle. Immunity 2013, 29, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wolchok, J.D.; Chiarion-Sileni, V.; Gonzalez, R.; Rutkowski, P.; Grob, J.J.; Cowey, C.L.; Lao, C.D.; Wagstaff, J.; Schadendorf, D.; Ferrucci, P.F.; et al. Overall Survival with Combined Nivolumab and Ipilimumab in advanced melanoma. N. Engl. J. Med. 2017, 377, 1345–1356. [Google Scholar] [CrossRef] [PubMed]
- Yau, T.; Kang, Y.K.; Kim, T.Y.; El-Khoueiry, A.B.; Santoro, A.; Sangro, B.; Melero, I.; Kudo, M.; Hou, M.M.; Matilla, A.; et al. Nivolumab + ipilimumab combination therapy in patients with advanced hepatocellular carcinoma: Results from CheckMate 040. J. Clin. Oncol. 2019, 37. [Google Scholar] [CrossRef]
- Kelley, R.K.; Abou-Alfa, G.K.; Bendell, J.C.; Kim, T.Y.; Borad, M.J.; Yong, W.P.; Morse, M.; Kang, Y.K.; Rebelatto, M.; Makowsky, M.; et al. Phase I/II study of durmalumab and tremelimumab in patients with unresectable hepatocellular carcinoma: Phase I safety and efficacy analises. J. Clin. Oncol. 2017, 35. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Chan, S.L.; Furuse, J.; Galle, P.R.; Kelley, R.K.; Qin, S.; Armstrong, J.; Darilay, A.; Vlahovic, G.; Negro, A.; et al. A randomized, multicenter phase 3 study of durvalumab and tremelimumab as first-line treatment in patients with unresectable HCC: HIMALAYA study. J. Clin. Oncol. 2018, 36. [Google Scholar] [CrossRef]
- Noman, M.Z.; Desantis, G.; Janji, B.; Hasmim, M.; Karray, S.; Dessen, P.; Bronte, V.; Chouaib, S. PD-L1 is a novel direct target of HIF-1α, and its blockade under hypoxia enhanced MDSC-mediated T cell activation. J. Exp. Med. 2014, 211, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Hato, T.; Zhu, A.X.; Duda, D.G. Rationally combining anti-VEGF therapy with checkpoint inhibitors in hepatocellular carcinoma. Immunotherapy 2016, 8, 299–313. [Google Scholar] [CrossRef]
- Pishvaian, M.J.; Lee, M.S.; Ryoo, B.Y.; Stein, S.; Lee, K.H.; Liu, B. Phase Ib study of atezolizumab + bevacizumab in HCC. Ann. Oncol. 2018, 29–35. [Google Scholar] [CrossRef]
- Cheng, A.L.; Qin, S.; Ikeda, M.; Galle, P.; Zhu, A.; Kim, T.Y.; Kudo, M.; Breder, V.; Kaseb, A.; Li, D.; et al. LBA3—IMbrave150: Efficacy and safety results from a ph III study evaluating atezolizumab (atezo) + bevacizumab (bev) vs sorafenib (Sor) as first treatment (tx) for patients (pts) with unresectable hepatocellular carcinoma (HCC). Ann. Oncol. 2019, 30, ix186–ix187. [Google Scholar] [CrossRef]
- Pal, S.K.; Vaishampayan, U.N.; Castellano, D.E.; Necchi, A.; Van Herpen, C.M.; Ramsingh, G.; Loriot, Y.; Agarwal, N. Phase Ib (COSMIC-021) trial of cabozantinib (C) in urothelial carcinoma (UC) or C in combination with atezolizumab (A) in patients (pts) with UC, castrate resistant prostate cancer (CRPC) or renal cell carcinoma (RCC). J. Clin. Oncol. 2019, 37 (Suppl. 7), TPS683. [Google Scholar] [CrossRef]
- Study of Cabozantinib in Combination with Atezolizumab versus Sorafenib in Subjects with Adavnced HCC Who Have Not Received Previous Systemic Anticancer Therapy (COSMIC-312). Available online: https://clinicaltrials.gov/ct2/show/NCT03755791 (accessed on 10 October 2020).
- Lu, X.; Horner, J.W.; Paul, E.; Shang, X.; Troncoso, P.; Deng, P.; Jiang, S.; Chang, Q.; Spring, D.J.; Sharma, P.; et al. Effective combinatorial immunotherapy for castration resistant prostate cancer. Nature 2017, 543, 728–732. [Google Scholar] [CrossRef] [PubMed]
- Nadal, R.M.; Mortazavi, A.; Stein, M.; Pal, S.K.; Davarpanah, N.N.; Parnes, H.L.; Ning, Y.M.; Cordes, L.M.; Bagheri, M.H.; Lindenberg, L.; et al. Results of phase I plus expansion cohorts of cabozantinib plus nivolumab and cabonivo plus ipilimumab in patients with metastatic urothelial carcinoma and other genitourinary malignancies. J. Clin. Oncol. 2018, 36, 515. [Google Scholar] [CrossRef]
- Kato, Y.; Tabata, K.; Kimura, T.; Yachie-Kinoshita, A.; Ozawa, Y.; Yamada, K.; Ito, J.; Tachino, S.; Hori, Y.; Matsuki, M.; et al. Lenvatinib plus anti-PDL-1 antibody combination treatment activates CD8+ T cells through reduction of tumor-associated macrophage and activation of the interferon pathway. PLoS ONE 2019, 14, e0212513. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Ikeda, M.; Zhu, A.X.; Sung, M.W.; Baron, A.D.; Kudo, M.; Okusaka, T.; Kobayashi, M.; Kumada, H.; Kaneko, S.; et al. Phase Ib study of Lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J. Clin. Oncol. 2020, 38. [Google Scholar] [CrossRef] [PubMed]
- Safety and Efficacy of Lenvatinib (E7080/MK-7902) in Combination with Pembrolizumab (MK-3475) versus Lenvatinib as First-Line Therapy in Partecipants with Advanced Hepatocellular Carcinoma (MK-7902-002/E7080-G000-311/LEAP-002). Available online: https://clinicaltrials.gov/ct2/show/NCT03713593 (accessed on 10 October 2020). [CrossRef]
- Akateh, C.; MBlack, S.; Conteh, L.; Miller, E.D.; Noonan, A.; Elliot, E.; Pawlik, T.M.; Tsung, A.; Cloyd, J. Neoadjuvant and adjuvant treatment strategies for hepatocellular carcinoma. World J. Gastroenterol. 2019, 25, 3704–3721. [Google Scholar] [CrossRef]
- Barbier, L.; Muscari, F.; Le Guellec, S.; Pariente, A.; Otal, P.; Suc, B. Liver resection after downstaging hepatocellular carcinoma with Sorafenib. Intern. J. Hepatol. 2011, 2011, 791013. [Google Scholar] [CrossRef]
- Irtan, S.; Chopin-Laly, X.; Ronot, M.; Faivre, S.; Paradis, V.; Belghiti, J. Complete regression of locally advanced hepatocellular carcinoma induced by sorafenib allowing curative resection. Liver Int. 2011, 31, 740–743. [Google Scholar] [CrossRef]
- Bouattour, M.; Fartoux, L.; Rosmorduc, O.; Scatton, O.; Vibert, E.; Costentin, C.; Soubrane, O.; Ronot, M.; Granier, M.M.; De Gramont, A.; et al. BIOSHARE multicenter neoadjuvant phase 2 study: Results of pre-operative sorafenib in patients with resectable hepatocellular carcinoma (HCC)—From GERCOR IRC. J. Clin. Oncol. 2016, 34, 252. [Google Scholar] [CrossRef]
- Zhang, Z.; Liu, Q.; He, J.; Yang, J.; Yang, G.; Wu, M. The effect of preoperative transcatheter hepatic arterial chemoembolization on disease-free survival after hepatectomy for hepatocellular carcinoma. Cancer 2000, 89, 2606–2612. [Google Scholar] [CrossRef]
- Li, C.; Wang, M.-D.; Lu, L.; Wu, H.; Yu, J.-J.; Zhang, W.-G.; Pawlik, T.M.; Zhang, Y.-M.; Zhou, Y.-H.; Gu, W.-M.; et al. Preoperative transcatheter arterial chemoembolization for surgical resection of huge hepatocellular carcinoma (≥10 cm): A multicenter propensity matching analysis. Hepatol. Int. 2019, 13, 736–747. [Google Scholar] [CrossRef]
- Sasaki, A.; Iwashita, Y.; Shibata, K.; Ohta, M.; Kitano, S.; Mori, M. Preoperative transcatheter arterial chemoembolization reduces long-term survival rate after hepatic resection for resectable hepatocellular carcinoma. Eur. J. Surg. Oncol. (EJSO) 2006, 32, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Zhu, G.Q.; Shi, K.Q.; Yu, H.J.; He, S.Y.; Braddock, M.; Zhou, M.T.; Chen, Y.P.; Zheng, M.H. Optimal adjuvant therapy for resected hepatocellular carcinoma: A systematic review with network meta-analysis. Oncotarget 2015, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; He, X.D.; Yao, N.; Liang, W.J.; Zhang, Y.C. A meta-analysis of adjuvant therapy after potentially curative treatment for hepatocellular carcinoma. Cancer J. Gastroenterol. 2013, 27, 351–363. [Google Scholar] [CrossRef]
- Bruix, J.; Takayama, T.; Mazzaferro, V.; Chau, G.-Y.; Yang, J.; Kudo, M.; Cai, J.; Poon, R.T.; Han, K.-H.; Tak, W.Y.; et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): A phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2015, 16, 1344–1354. [Google Scholar] [CrossRef]
- Takayama, T.; Sekine, T.; Makuuchi, M.; Yamasaki, S.; Kosuge, T.; Yamamoto, J.; Shimada, K.; Sakamoto, M.; Hirohashi, S.; Ohashi, Y.; et al. Adoptive immunotherapy to lower postsurgical recurrence rates of hepatocellular carcinoma: A randomised trial. Lancet 2000, 356, 802–807. [Google Scholar] [CrossRef]
- Dong, H.; Li, Q.; Wang, J.; Zhang, T.; Kong, D.L. A randomized, controlled trial of postoperative adjuvant cytokine-induced killer cells immunotherapy after radical resection of hepatocellular carcinoma. Dig. Liver Dis. 2009, 41, 36–41. [Google Scholar]
- Brown, Z.J.; Greten, T.F.; Heinrich, B. Adjuvant Treatment of Hepatocellular Carcinoma: Prospect of Immunotherapy. Hepatology 2019, 70, 1437–1442. [Google Scholar] [CrossRef]
- Safety and Efficacy of Pembrolizumab (MK-3475) versus Placebo as Adjuvant Therapy in Partecipants with Hepatocellular Carcinoma (HCC) and Complete Radiological Response after Surgical Resection or Local Ablation (MK-3475-937/KEYNOTE-937). Available online: https://clinicaltrials.gov/ct2/show/NCT03867084 (accessed on 6 January 2021).
- A study of Nivolumab in Partecipants with Hepatocellular Carcinoma Who Are At Risk of Recurrence after Curative Hepatic Resection or Ablation (CheckMate 9DX). Available online: https://clinicaltrials.gov/ct2/show/NCT03383458 (accessed on 6 January 2021).
- Kudo, M.; Izumi, N.; Kokudo, N.; Matsui, O.; Sakamoto, M.; Nakashima, O.; Kojiro, M.; Makuuchi, M. Management of hepatocellular carcinoma in Japan: Consensus-Based Clinical Practice Guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Dig. Dis. 2011, 29, 339–364. [Google Scholar] [CrossRef]
- Arizumi, T.; Ueshima, K.; Chishina, H.; Kono, M.; Takita, M.; Kitai, S.; Inoue, T.; Yada, N.; Hagiwara, S.; Minami, Y.; et al. Validation of the criteria of transcatheter arterial chemoembolization failure or refractoriness in patients with advanced epatocellular carcinoma proposed by the LCSG. Oncology 2014, 87, 32–36. [Google Scholar] [CrossRef]
- Ogasawara, S.; Chiba, T.; Ooka, Y.; Kanogawa, N.; Motoyama, T.; Suzuki, E.; Tawada, A.; Kanai, F.; Yoshikawa, M.; Yokosuka, O. Efficacy of sorafenib in intermediate-stage hepatocellular carcinoma patients refractory to transarterial chemoembolization. Oncology 2014, 87, 330–334. [Google Scholar] [CrossRef]
- Arizumi, T.; Ueshima, K.; Minami, T.; Kono, M.; Chishina, H.; Takita, M.; Kitai, S.; Inoue, T.; Yada, N.; Hagiwara, S.; et al. Effectiveness of sorafenib in patients with transcatheter arterial chemoembolization (TACE) refractory and intermediate-stage hepatocellular carcinoma. Liver Cancer 2015, 4, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M. Regorafenib as second-line systemic therapy may change the treatment strategy and management paradigm for hepatocellular carcinoma. Liver Cancer 2016, 5, 235–244. [Google Scholar]
- Feng, J.; Lu, P.; Zhu, G.; Hooi, S.C.; Wu, Y.; Huang, X.; Dai, H.; Chen, P.; Li, Z.; Su, W.; et al. ACSL4 is a predictive biomarker of sorafenib sensitivity in hepatocellular carcinoma. Acta Pharmacol. Sin. 2020. [Google Scholar] [CrossRef] [PubMed]
- Louandre, C.; Marcq, I.; Bouhlal, H.; Lachaier, E.; Godin, C.; Saidak, Z.; Francois, C.; Chatelain, D.; Debuysscher, V.; Barbare, C.; et al. The retinoblastoma protein regulates ferroptosis induced by sorafenib in human hepatocellular carcinoma cells. Lancet 2015, 356, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Ou, Z.; Chen, R.; Niu, X.; Chen, D.; Kang, R.; Tang, D. Activation of the p62-Keap1-NRF2 pathway protects aganist ferroptosis in hepatocellular carcinoma cells. Hepatology 2016, 63, 173–184. [Google Scholar] [CrossRef]
- Abou-Alpha, G.K.; Ricci, S.; Amadori, D.; Santoro, A.; Figer, A.; De Greve, J.; Douillard, J.Y.; Lathia, C.; Schwartz, B.; Taylor, I.; et al. Phase II study of Sorafenib in patients with advanced hepatocellular carcinoma. J. Clin. Oncol. 2006, 24, 4293–4300. [Google Scholar] [CrossRef] [PubMed]
- Personeni, N.; Rimassa, L.; Pressiani, T.; Destro, A.; Ligorio, C.; Tronconi, M.C.; Bozzarelli, S.; Carnaghi, C.; Di Tommaso, L.; Giordano, L.; et al. Molecular determinants of outcome in sorafenib-treated patients with hepatocellular carcinoma. J. Cancer Res. Clin. Oncol. 2013, 139, 1179–1187. [Google Scholar] [CrossRef]
- Wang, P.; Jiang, Z.; Liu, X.; Yu, K.; Wang, C.; Li, H.; Zhong, L. PI16 attenuates response to Sorafenib and represents a predictive biomarker in hepatocellular carcinoma. Cancer Med. 2020, 9, 6972–6983. [Google Scholar] [CrossRef]
- Nishida, N.; Arizumi, T.; Hagiwara, S.; Ida, H.; Sakurai, T.; Kudo, M. MicroRNA for the prediction of early response to sorafenib treatment in human hepatocellular carcinoma. Liver Cancer 2017, 6, 113–125. [Google Scholar] [CrossRef]
- Kohno, T.; Morishita, A.; Iwama, H.; Fujita, K.; Tani, J.; Takuma, K.; Nakahara, M.; Oura, K.; Tadokoro, T.; Nomura, T.; et al. Comprehensive analysis of circulating microRNAs as predictive biomarkers for sorafenib therapy outcome in hepatocellular carcinoma. Oncol. Lett. 2020, 20, 1727–1733. [Google Scholar] [CrossRef]
- Marisi, G.; Petracci, E.; Raimondi, F.; Faloppi, L.; Foschi, F.G.; Lauletta, G.; Iavarone, M.; Canale, M.; Valgiusti, M.; Neri, L.M.; et al. ANGPT2 and NOS3 Polymorphisms and Clinical Outcome in Advanced Hepatocellular Carcinoma Patients Receiving Sorafenib. Cancers 2019, 11, 1023. [Google Scholar] [CrossRef]
- Marisi, G.; Cucchetti, A.; Ulivi, P.; Canale, M.; Cabibbo, G.; Solaini Foschi, F.G.; De Matteis, S.; Ercolani, G.; Valgiusti, M.; Frassineti, G.L.; et al. Ten years of Sorafenib in hepatocellular carcinoma: Are there any predictive and/or prognostic markers? World J. Gastroenterol. 2018, 24, 4152–4163. [Google Scholar] [CrossRef] [PubMed]
- Chuma, M.; Uojima, H.; Numata, K.; Hidaka, H.; Toyoda, H.; Hiraoka, A.; Tada, T.; Hirose, S.; Atsukawa, M.; Itokawa, N.; et al. Early changes in circulating FGF19 and Ang-2 levels as possible predictive biomarkers of clinical response to lenvatinib therapy in hepatocellular carcinoma. Cancers 2020, 12, 293. [Google Scholar] [CrossRef] [PubMed]
- Gilles, R.J.; Kinhan, P.E.; Hricak, H. Radiomics: Images are more than pictures, they re data. Radiology 2016, 278, 563–577. [Google Scholar] [CrossRef] [PubMed]
- Miranda Magalhaes Santos, J.M.; Clemente Oliveira, B.; Araujo-Filho, J.A.B.; Assuncao, A.N., Jr.; de MMachado, F.A.; Carlos Tavares Rocha, C.; Horvat, J.V.; Menezes, M.R.; Horvat, N. State-of-the-art in radiomics of hepatocellular carcinoma: A review of basic principles, applications, and limitations. Abdom. Radiol. 2020, 45, 342–353. [Google Scholar] [CrossRef] [PubMed]
- Wakabayashi, T.; Ouhmich, F.; Gonzalez-Cabrera, C.; Felli, E.; Saviano, A.; Agnus, V.; Savadjiev, P.; Baumert, T.F.; Pessaux, P.; Marescaux, J.; et al. Radiomics in hepatocellular carcinoma: A quantitative review. Hepatol. Int. 2019, 13, 546–559. [Google Scholar] [CrossRef]
- Lewis, S.; Hectors, S.; Taouli, B. Radiomics of hepatocellular carcinoma. Abdom. Radiol. 2020. [Google Scholar] [CrossRef]
- Panzuto, F.; Maccauro, M.; Campana, D.; Faggiano, A.; Massironi, S.; Pusceddu, S.; Spada, F.; Ferone, D.; Modica, R.; Grana, C.M.; et al. Impact of the SARS-CoV2 pandemic dissemination on the management of neuroendocrine neoplasia in Italy: A report from the Italian Association for Neuroendocrine Tumors (Itanet). J. Endocrinol. Investig. 2020. [Google Scholar] [CrossRef]
- Pellino, G.; Spinelli, A. How COVID-19 outbreak is impact- ing colorectal cancer patients in Italy: A long shadow beyond infection. Dis. Colon Rectum 2020, 63, 720–722. [Google Scholar] [CrossRef]
- Xu, Y.; Hu, K.; Wang, M. Clinical recommendations on lung cancer management during the COVID-19 pandemic. Thorac. Cancer 2020, 11, 2067–2074. [Google Scholar] [CrossRef]
- Lam Chan, S.; Masatoshi, K. Impacts of COVID-19 on Liver Cancers: During and after the pandemic. Liver Cancer 2020, 9, 491–502. [Google Scholar] [CrossRef] [PubMed]
| Status | Clinical Trial | Phase | Treatment Setting | |
|---|---|---|---|---|
| NCT04102098 | Recruiting | A study of atezolizumab plus bevacizumab versus active surveillance as adjuvant therapy in patients with hepatocellular carcinoma at high risk of recurrence after surgical resection or ablation | Phase III | Adjuvant |
| NCT03867084 | Recruiting | Safety and efficacy of pembrolizumab (MK-3475) versus placebo as adjuvant therapy in participants with hepatocellular carcinoma (HCC) and complete radiological response after surgical resection or local ablation (MK-3475-937/KEYNOTE-937) | Phase III | Adjuvant |
| NCT03859128 | Recruiting | Toripalimab or placebo as adjuvant therapy in hepatocellular carcinoma after curative hepatic resection | Phase II/ III | Adjuvant |
| NCT03847428 | Recruiting | Assessment of efficacy and safety of durvalumab alone or combined with bevacizumab in high-risk-of-recurrence HCC patients after curative treatment | Phase III | Adjuvant |
| NCT03383458 | Recruiting | A study of nivolumab in participants with hepatocellular carcinoma who are at high risk of recurrence after curative hepatic resection or ablation | Phase III | Adjuvant |
| NCT02738697 | Recruiting | Adjuvant chemotherapy with FOLFOX in HCC patients after resection | Phase III | Adjuvant |
| NCT03778957 | Recruiting | A global study to evaluate transarterial chemoembolization (TACE) in combination with durvalumab and bevacizumab therapy in patients with locoregional hepatocellular carcinoma | Phase III | Locoregional disease |
| NCT04523493 | Recruiting | Phase III study of toripalimab (JS001) combined with lenvatinib for advanced HCC | Phase III | Palliative |
| NCT04246177 | Recruiting | Evaluation of safety and efficacy of lenvatinib (E7080/MK-7902) with pembrolizumab (MK-3475) in combination with transarterial chemoembolization (TACE) in participants with incurable/non-metastatic hepatocellular carcinoma (MK-7902-012/ E7080-G000-318/LEAP-012) | Phase III | Palliative |
| NCT04039607 | Recruiting | A study of nivolumab in combination with ipilimumab in participants with advanced hepatocellular carcinoma | Phase III | Palliative |
| NCT03794440 | Recruiting | A study to evaluate the efficacy and safety of sintilimab in combination with IBI305 (anti-VEGF monoclonal antibody) compared to sorafenib as the first-line treatment for advanced hepatocellular carcinoma. | Phase II/III | Palliative |
| NCT03764293 | Recruiting | A study to evaluate SHR-1210 in combination with apatinib as first-line therapy in patients with advanced HCC | Phase III | Palliative |
| NCT03755791 | Recruiting | A study of cabozantinib in combination with atezolizumab versus sorafenib in subjects with advanced HCC who have not received previous systemic anticancer therapy | Phase III | Palliative |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schipilliti, F.M.; Garajová, I.; Rovesti, G.; Balsano, R.; Piacentini, F.; Dominici, M.; Gelsomino, F. The Growing Skyline of Advanced Hepatocellular Carcinoma Treatment: A Review. Pharmaceuticals 2021, 14, 43. https://doi.org/10.3390/ph14010043
Schipilliti FM, Garajová I, Rovesti G, Balsano R, Piacentini F, Dominici M, Gelsomino F. The Growing Skyline of Advanced Hepatocellular Carcinoma Treatment: A Review. Pharmaceuticals. 2021; 14(1):43. https://doi.org/10.3390/ph14010043
Chicago/Turabian StyleSchipilliti, Francesca Matilde, Ingrid Garajová, Giulia Rovesti, Rita Balsano, Federico Piacentini, Massimo Dominici, and Fabio Gelsomino. 2021. "The Growing Skyline of Advanced Hepatocellular Carcinoma Treatment: A Review" Pharmaceuticals 14, no. 1: 43. https://doi.org/10.3390/ph14010043
APA StyleSchipilliti, F. M., Garajová, I., Rovesti, G., Balsano, R., Piacentini, F., Dominici, M., & Gelsomino, F. (2021). The Growing Skyline of Advanced Hepatocellular Carcinoma Treatment: A Review. Pharmaceuticals, 14(1), 43. https://doi.org/10.3390/ph14010043





