Motion Cancellation Technique of Vital Signal Detectors Based on Continuous-Wave Radar Technology
Abstract
1. Introduction
- Radar architecture and design modifications;
- Signal processing algorithms for motion artifact suppression;
- Studies on propagation characteristics and environmental impact mitigation.
2. Continuous-Wave Radars for Vital Sign Detection
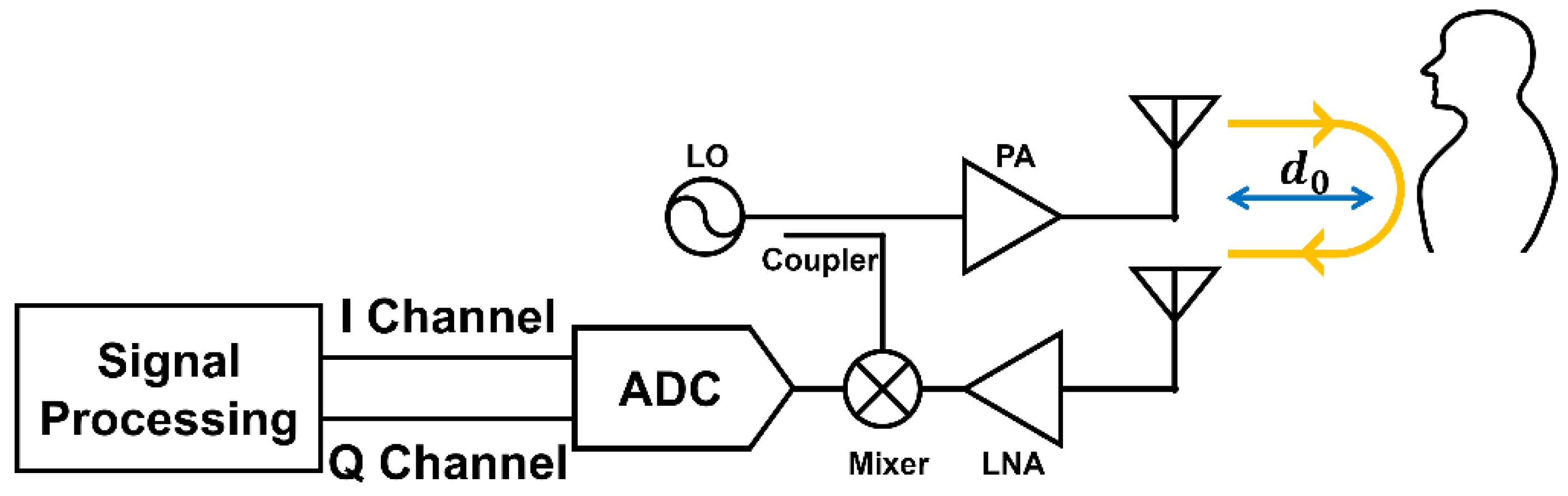
2.1. Principle of CW Radar for Vital Sign Detection
2.2. Challenges in Vital Sign Detection
2.2.1. Body Motion Artifacts
- Reduced SNR: Large-amplitude motion artifacts overshadow weaker signals from respiration or heartbeat.
- Distorted phase: Rapid or erratic movements affect the received phase information, complicating vital signal extraction.
- Unexpected frequency shifts: Body motion can generate frequency components similar to those of respiration and heartbeat signals, making it challenging to distinguish genuine vital sign data.
2.2.2. Environmental Disturbances
- Multipath interference: Radar signals may reflect off walls, furniture, and other objects, thereby creating multiple propagation paths. These multipath reflections introduce phase and amplitude distortions that hinder accurate signal interpretation, particularly in dense indoor settings.
- Electromagnetic interference (EMI): Radar sensors operate in specific frequency bands; therefore, interference from Wi-Fi, Bluetooth, 5G base stations, or medical equipment can lower the SNR, rendering vital sign detection unstable or unreliable.
- Multi-subject detection: When multiple individuals are present, accurately separating each subject’s vital signals becomes challenging. Techniques such as multiple-input multiple-output (MIMO) radar may be required to isolate individual respiration and heartbeat signals.
2.2.3. Sensor Sensitivity and Placement
- Importance of optimal placement: Improper sensor placement may lead to reduced SNR and phase detection errors. Direct alignment with the thoracic or cardiac regions is typically recommended for accurate measurements.
- Body posture and signal attenuation: Different postures, such as sitting, standing, or lying down, alter the reflection patterns. Changes in subject-to-sensor distance can further attenuate signals, leading to reduced detection accuracy.
- Weak signal strength: Because respiration and heartbeat movements inherently generate low-amplitude signals, advanced techniques (e.g., signal amplification, high-resolution fast Fourier transform (FFT)) are required to improve system sensitivity.
3. Motion Cancellation Techniques
3.1. Radar Architecture Enhancements
3.1.1. Multi-Antenna and MIMO Systems
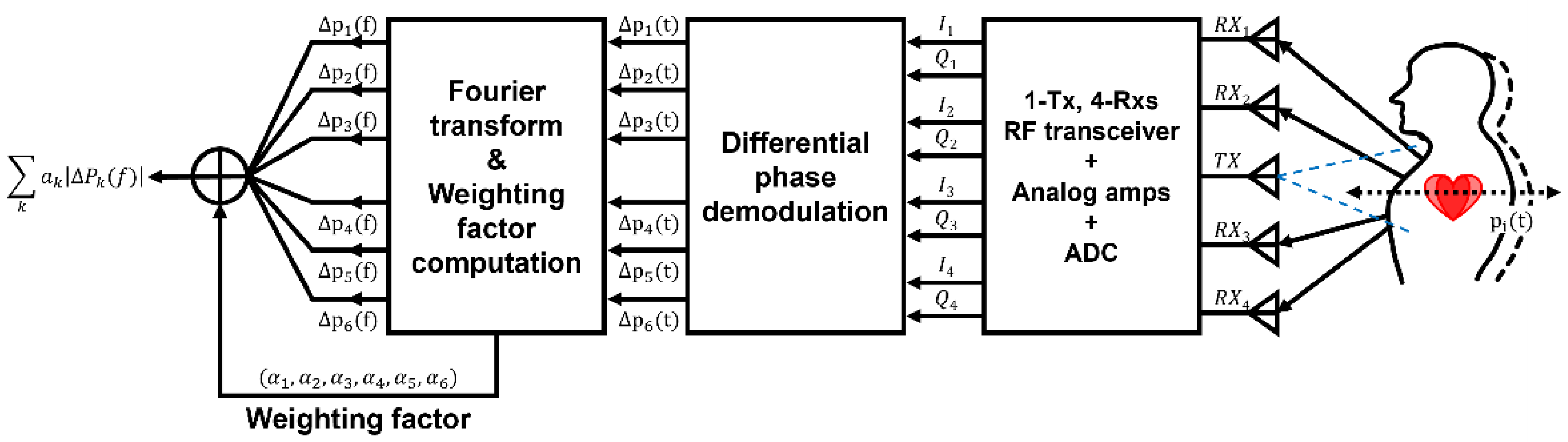
- A differential phase Doppler radar system using a collocated multiple-receiver array effectively removes common motion components by analyzing the phase differences among the receiver channels [12]. This approach demonstrated an improvement of over 20 dB in noise suppression relative to the single-antenna setup.
- A virtual array-based radar system uses Pearson correlation coefficients to identify highly correlated regions among multiple measurement points on the chest [13]. A Kalman filter tracked these regions to suppress artifacts, achieving heartbeat and respiration detection errors within 5 bpm under dynamic conditions (motion speeds of up to 0.5 m/s).
- Null-point beamforming with a 60 GHz FMCW MIMO radar successfully reduced common body motion artifacts by 18 dB, enabling simultaneous vital sign detection in two individuals [14]. Independent signals are allocated to each target to facilitate motion compensation under random conditions.
- In an LFMCW radar with multiple receivers, a four-receiver array combines multi-channel Kalman smoothing with local hidden Markov models to improve the SNR by up to 7.5 dB [15]. This approach maintained respiration and heartbeat detection errors below 2 bpm in RBM.
- MIMO-based radar has also proven effective in in-vehicle environments, where driver motion and vehicle vibration degrade performance [16]. Digital beamforming effectively isolated the driver’s vital signals from extraneous reflections, yielding a heart rate detection error of 0.82 bpm and a respiration rate error of 0.16 rpm.
3.1.2. Distributed Radar Sensor
- Two 5.8 GHz radars placed at different angles (e.g., 30°, 45°, and 60°) significantly enhanced the SNR, boosting detection accuracy to approximately 97.8% that of single-radar configurations [17].
- A front-and-rear dual-radar setup was tested during treadmill walking with deep learning-based signal restoration (CNN and LSTM), which effectively isolated the respiration signals [18]. This approach maintained high accuracy even under moderate subject motion.
- A 60 GHz FMCW radar that fuses multi-range-bin data for driver monitoring [19] by integrating a Kalman filter with multi-signal fusion achieved a 1.9 bpm lower error than the single-radar approach, reliably detecting breath-hold events.
3.1.3. Multi-View Beamforming Radar
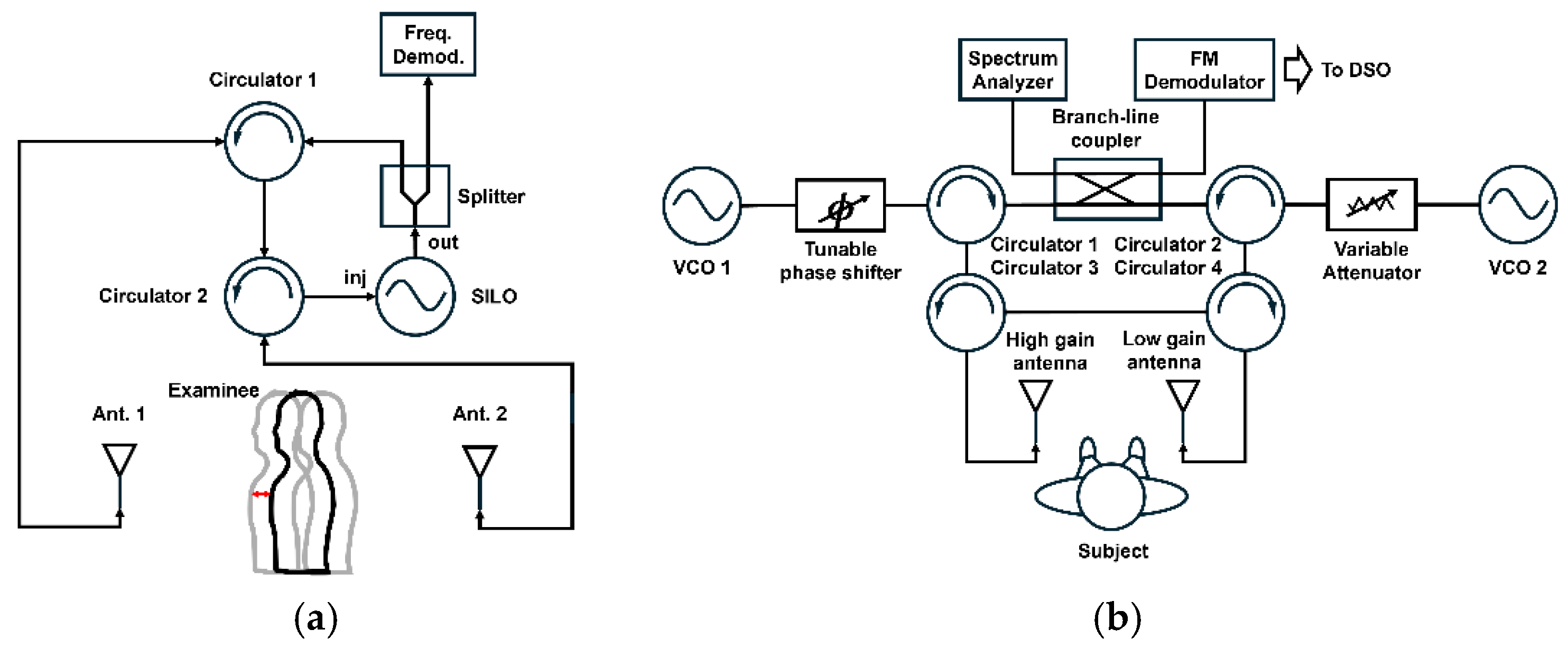
3.1.4. Single-Chip Single-Antenna Radar
3.1.5. Multi-Channel Radar Systems Resilient to RBM
3.1.6. Accurate Heartbeat Measurement Across Various Body Postures
3.2. Signal Processing Approaches
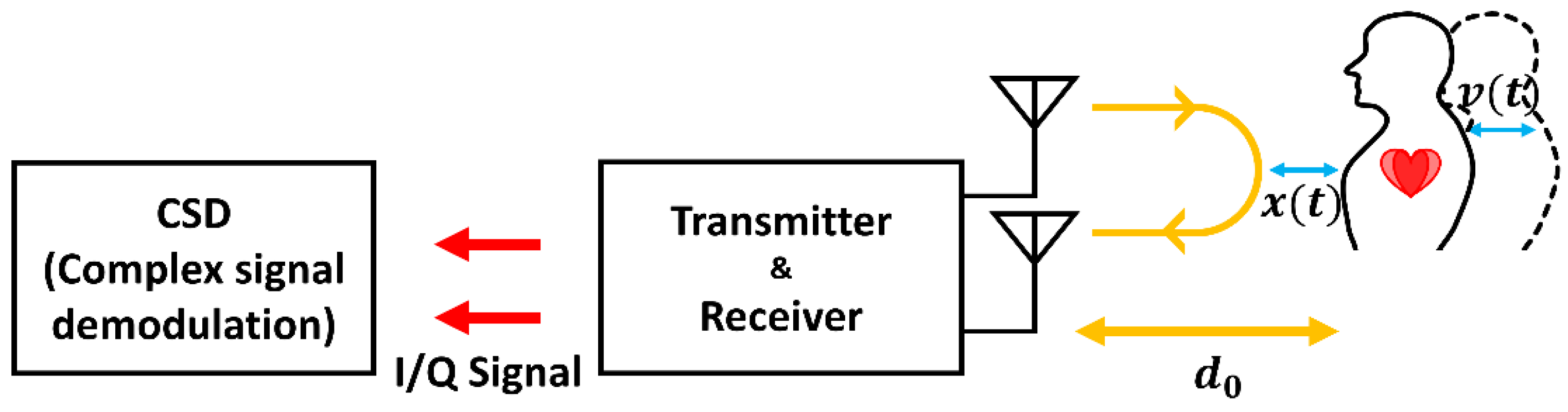
3.2.1. Complex Signal Demodulation
3.2.2. Polynomial Fitting and Adaptive Filter Approaches
- Matched filter-assisted polynomial fitting. Lv et al. [32] combined matched filtering with third-order polynomial fitting to remove RBM components at speeds of up to 15 mm/s. Although the matched filter increases the SNR by emphasizing known signal patterns, higher motion speeds (>50 mm/s) still pose challenges because of template mismatch.
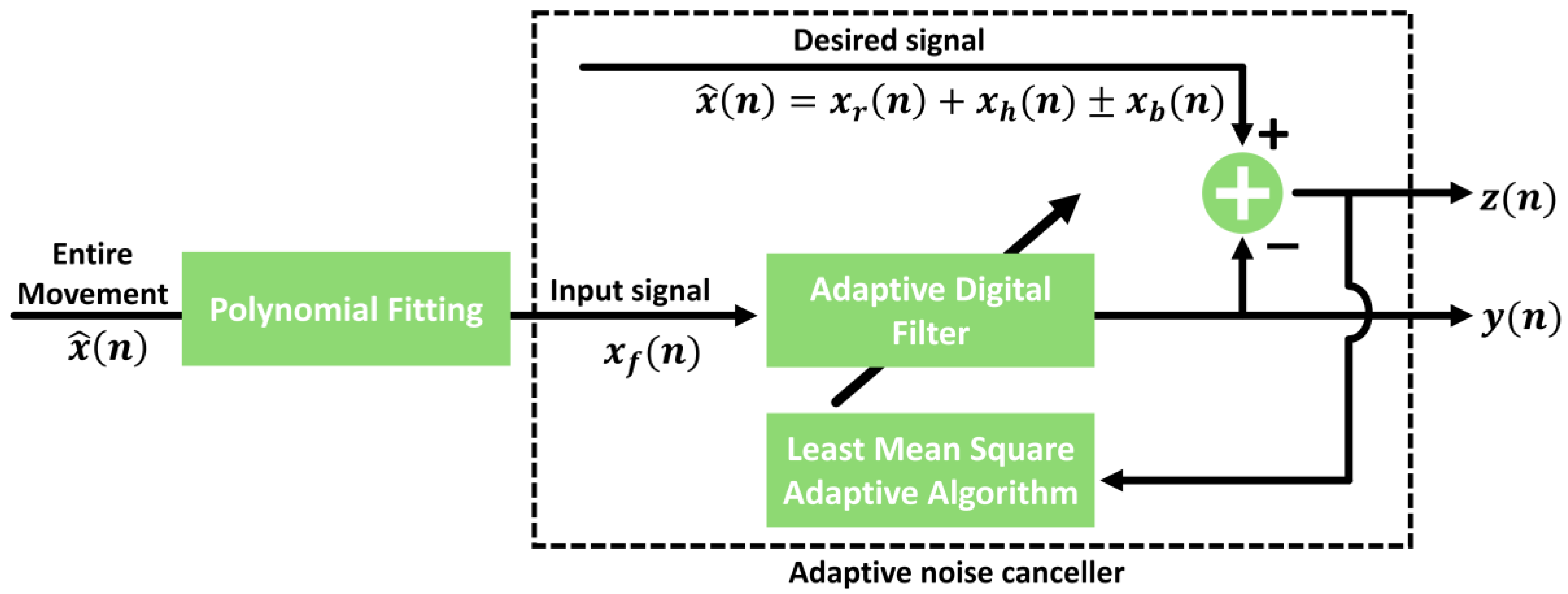
- Adaptive noise cancellation (ANC) and N-DCT. As shown in Figure 8, Yang et al. [33] used ANC, polynomial fitting, and N-DCT to enhance signal quality in the presence of RBM by up to 47.6 mm/s. However, an initial ANC learning phase is required, and multi-interference environments can degrade performance.
- Sekak et al. [34] utilized cyclostationary signal processing, which exhibits periodic changes over time, to extract cyclic characteristics in the frequency domain. They introduced several techniques, such as cyclic moments, cyclic autocorrelation, and cyclic cumulants, to differentiate between the first and second order of cycle signals. By analyzing the cyclostationary signal, they obtained vital signal detection with a maximum error of 0.102 Hz for respiration and 0.038 Hz for heartbeat. Measurement results demonstrate that cyclostationary signal analysis can enhance vital sign detection even in the presence of noise and movement, particularly when combined with a bi-static radar system operating at 2.5 GHz.
3.2.3. External Interference Removal Using the Least Squares Method
3.2.4. FMCW Radar Integration with Adaptive Filters
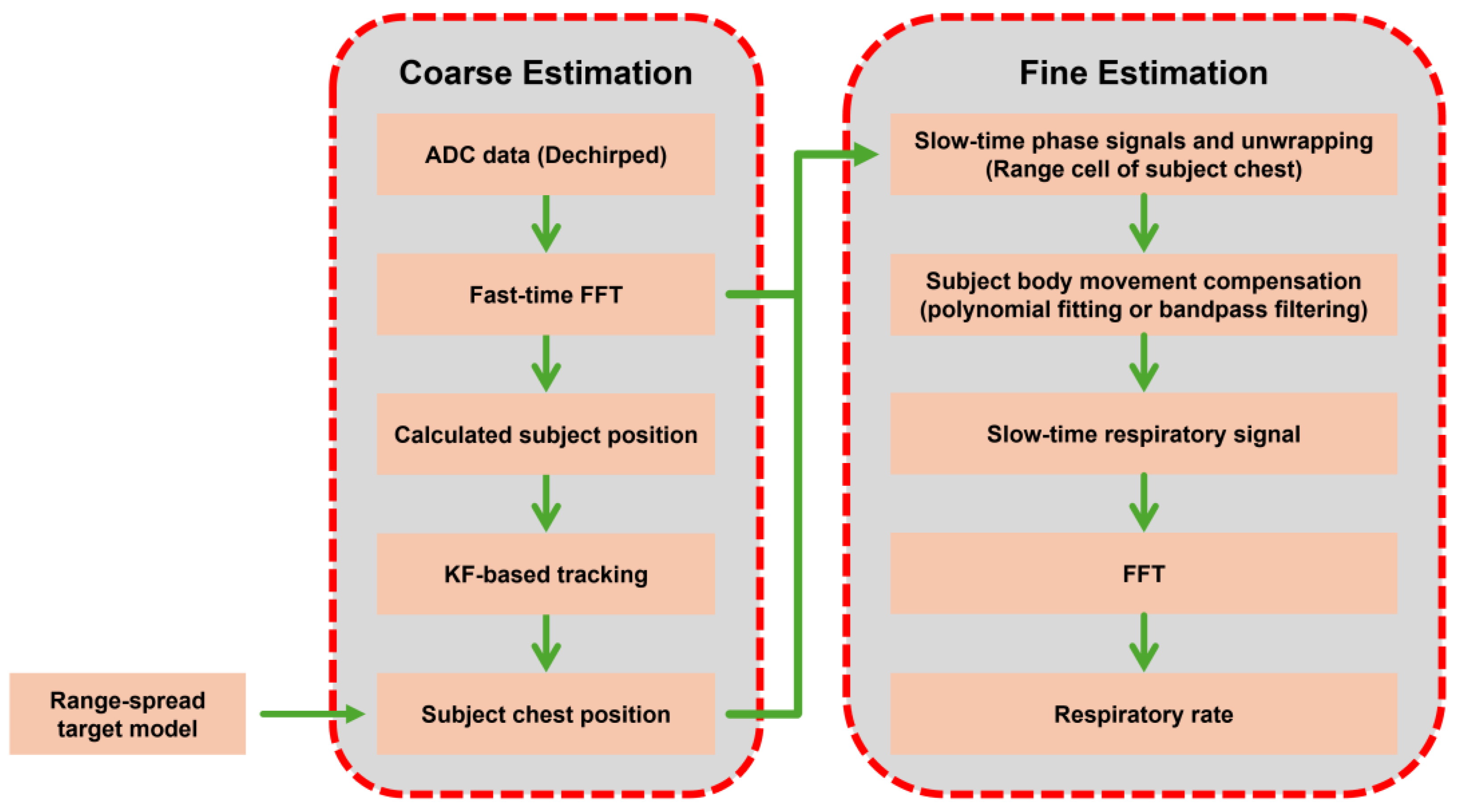
3.2.5. Mode Decomposition Techniques
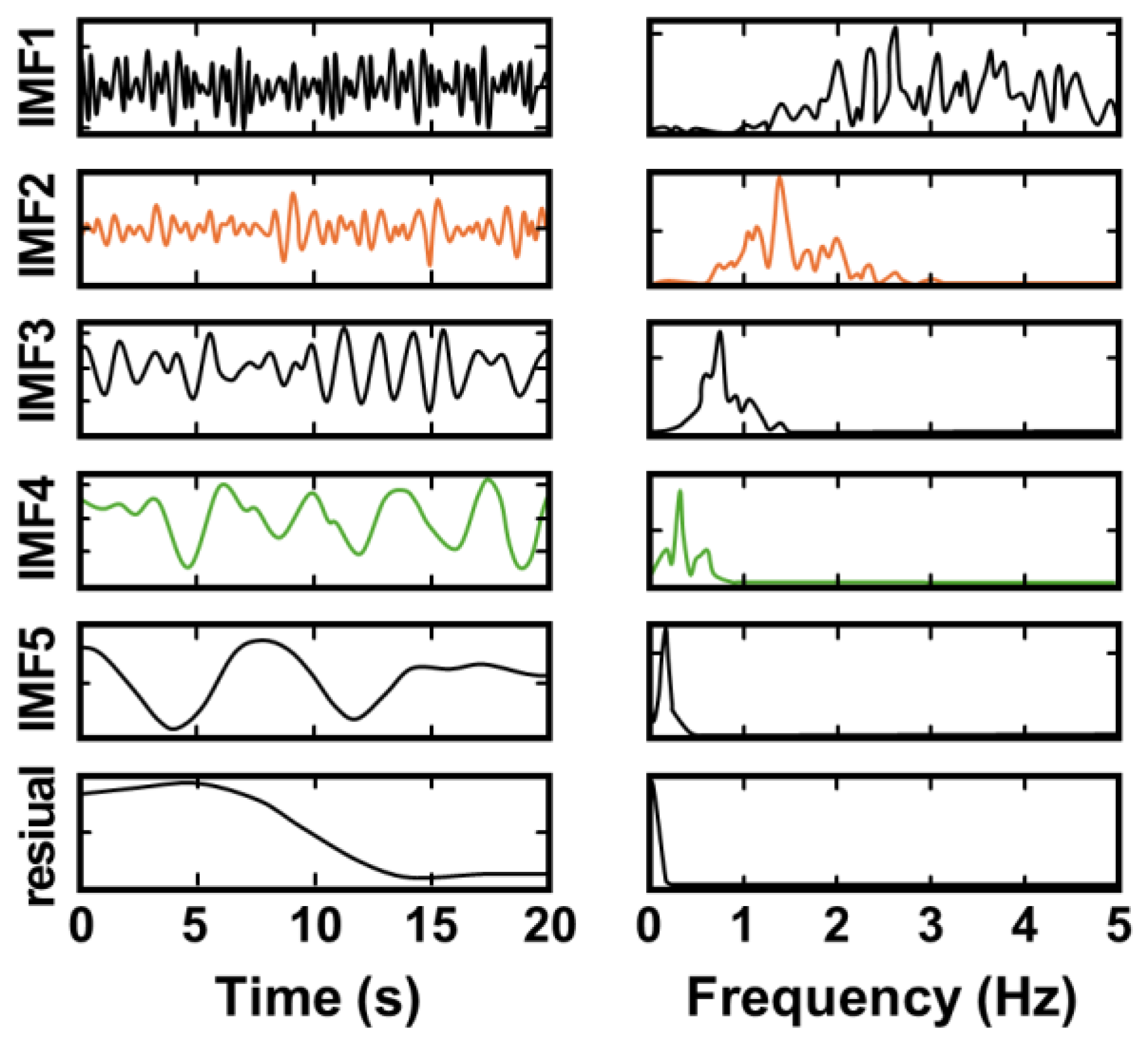
- Hu et al. [43] combined ICEEMDAN with the improvised adaptive range bin selection technique to track targets and effectively extract vital signals, even when moving in indoor environments at a walking speed of 1 m/s. The range profile matrix (RPM) and Doppler-range matrix (DRM) were combined to track the movement of the target and dynamically update the position where the signal most strongly reflects the signal, thereby enabling adaptive detection of target location and stable signal detection. Figure 12 shows that the vital information of a moving subject was successfully extracted using the ICEEMDAN method, with significant results that were confirmed through the frequency spectrum.
- Range-Doppler matrix (RDM) of FMCW radar data and a Gaussian interpolation algorithm (GIA) were presented in [44]. RDM is derived from the two-dimensional 2D-FFT of FMCW radar data. A Gaussian interpolation algorithm (GIA) was applied in the Doppler dimension to estimate the target velocity signals. To mitigate large-scale body motion, a robust enhanced trend filtering (RETF) algorithm was employed. To extract respiratory and heartbeat frequencies, the time-varying filter-based empirical mode decomposition (TVF-EMD) algorithm was used. Evaluations with data from seven volunteers using Texas Instrument’s AWR1642 radar achieved accuracies of 93% for respiration and 95% for heart rate detection, effectively handling random body movements without relying on range bin selection, thus avoiding phase wrap issues.
- VMD-based methods improve frequency-band precision. However, optimal parameter tuning (e.g., number of modes, penalty factors) and high computational costs remain barriers to real-time applications. Various studies have explored approaches to optimizing parameter tuning in the VMD method. Qu et al. [46] proposed an improved adaptive parameter variational mode decomposition (IAPVMD) method that integrates the energy loss rate evaluation with the mode discrimination criterion to determine the optimal parameter that would eliminate the RBM. A metaheuristic whale optimization algorithm (WOA)-based parameter tuning method was proposed in [47] to mitigate RBM interference and improve the stability of cardiac component extraction. Variational mode extraction (VME) further refines the VMD by targeting specific frequencies, reducing the complexity of multi-mode decompositions [48,49]. Despite their sophistication, these methods still face challenges in the presence of rapid or unpredictable motions.
3.3. Propagation and Environmental Studies
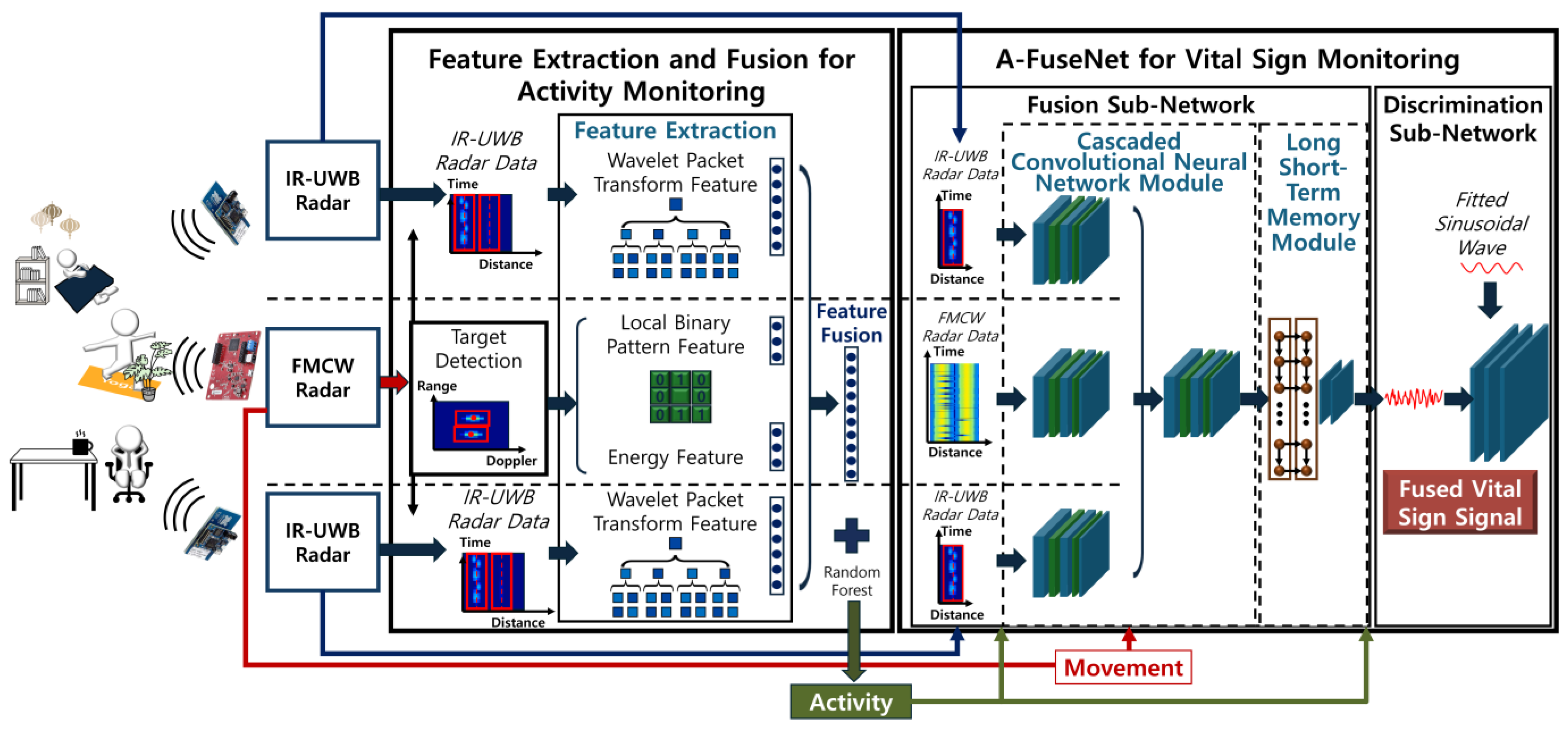
3.3.1. Multi-Radar Data Fusion
3.3.2. Hybrid Radar Systems for Motion Robust Monitoring
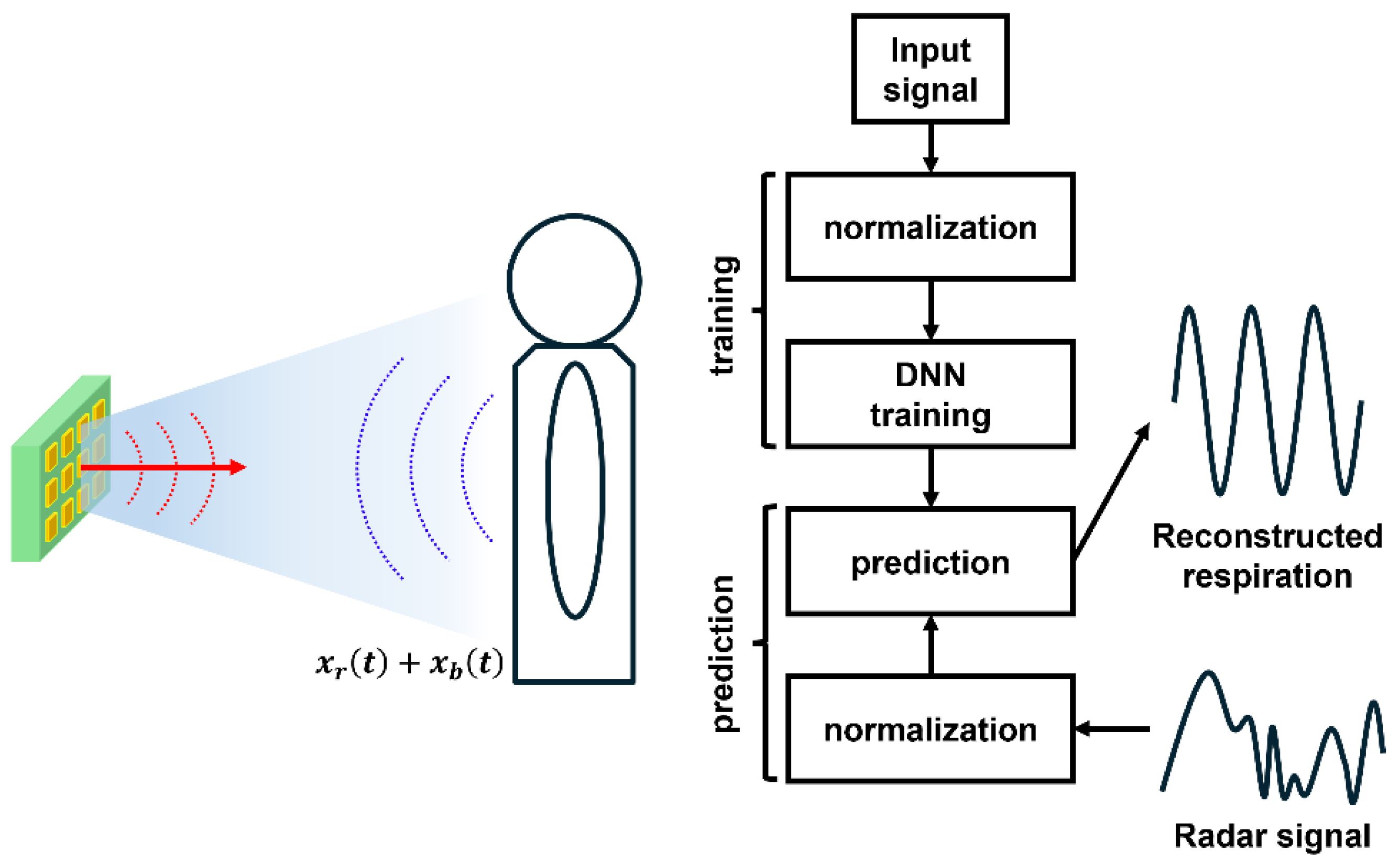
3.3.3. Integrated Neural Networks
4. Discussion
- Multi-modal sensor fusion systems
- 2.
- AI-driven signal processing
- 3.
- Low-power and miniaturized radar systems
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADC | Analog-to-Digital Converter |
| AI | Artificial Intelligence |
| ANC | Adaptive Noise Cancellation |
| CNN | Convolutional Neural Network |
| CW | Continuous Wave |
| DNN | Deep Neural Network |
| DRM | Doppler Range Matrix |
| EM | Electromagnetic |
| EMI | Electromagnetic Interference |
| EMD | Empirical Mode Decomposition |
| FFT | Fast Fourier Transform |
| FMCW | Frequency-Modulated CW |
| GAN | Generative Adversarial Network |
| HVD | Hilbert Vibration Decomposition |
| CEEMDAN | Complete Ensemble Empirical Mode Decomposition with Adaptive Noise |
| ICEEMDAN | Improved Complete Ensemble Empirical Mode Decomposition with Adaptive Noise |
| IMF | Intrinsic Mode Function |
| I/Q | In-Phase/Quadrature |
| IR-UWB | Impulse Radio Ultra-Wideband |
| LCVCO | LC-Based Voltage-Controlled Oscillator |
| LFMCW | Linear Frequency-Modulated CW |
| LNA | Low Noise Amplifier |
| LO | Local Oscillator |
| LSM | Least Squares Method |
| LSTM | Long Short-Term Memory |
| MIMO | Multi-Input Multi-Output |
| N-DCT | N-Dimensional Discrete Cosine Transform |
| PA | Power Amplifier |
| PMCW | Pulse-Modulated CW |
| RBM | Random Body Motion |
| RPM | Range Profile Matrix |
| RVCO | Ring-Based Voltage-Controlled Oscillator |
| SIL | Self-Injection Locking |
| SMIL | Self/Mutually Injection-Locked |
| SNR | Signal-to-Noise Ratio |
| TA-RS | Tracking-Aided Range-Spread |
| TVF-EMD | Time-Varying Filter Empirical Mode Decomposition |
| VaR-VSM | Vision-Assisted Radar with Variational Variance Stabilizing Mapping |
| VCO | Voltage-Controlled Oscillator |
| VMD | Variational Mode Decomposition |
| VME | Variational Mode Extraction |
| WMC-VMD | Weighted Multi-Channel Variational Mode Decomposition |
References
- Bourdoux, A.; Parashar, K.; Bauduin, M. Phenomenology of mutual interference of FMCW and PMCW automotive radars. In Proceedings of the 2017 IEEE Radar Conference, Seattle, WA, USA, 8–12 May 2017; pp. 1709–1714. [Google Scholar]
- Kim, J.; Park, J.; Jang, S.; Yang, J. Peak detection algorithm for vital sign detection using Doppler radar sensors. Sensors 2019, 19, 1575. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.; Park, J.; Yang, J. Detrending technique for denoising in CW radar. Sensors 2021, 21, 6376. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Lee, G.; Lee, I.; Yang, J. Heart rate extraction technique with mitigation of respiration harmonic for bio-radar sensors. IEEE Sens. J. 2025, 25, 929–939. [Google Scholar] [CrossRef]
- Jang, A.; Lee, I.; Yang, J. Remote vital signal detection using ambient noise cancellation based on beam-switching Doppler radar. IEEE Trans. Instrum. Meas. 2024, 73, 1–15. [Google Scholar] [CrossRef]
- Park, J.; Jeong, Y.; Lee, G.; Oh, J.; Yang, J. 915-MHz continuous-wave Doppler radar sensor for detection of vital signs. Electronics 2019, 8, 561. [Google Scholar] [CrossRef]
- Zhang, Y.; Kurata, M.; Sanada, H.; Kajiwara, A. FMCW radar for small displacement detection of vital signal using projection matrix method. Int. J. Antennas Propag. 2013, 2013, 571986. [Google Scholar] [CrossRef][Green Version]
- Lee, I.; Yang, J. Signal preprocessing for heartbeat detection using continuous-wave Doppler radar. IEEE Microw. Wireless Technol. Lett. 2023, 33, 479–482. [Google Scholar] [CrossRef]
- Iyer, S.; Zhao, L.; Mohan, M.P.; Jimeno, J.; Siyal, M.Y.; Alphones, A.; Karim, M.F. mm-Wave radar-based vital signs monitoring and arrhythmia detection using machine learning. Sensors 2022, 22, 3106. [Google Scholar] [CrossRef]
- Wiesner, A. A multifrequency interferometric CW radar for vital signs detection. In Proceedings of the 2009 IEEE Radar Conference, Pasadena, CA, USA, 4–8 May 2009; pp. 1–4. [Google Scholar] [CrossRef]
- Williams, C.; Uddin, S.D.; Li, C. Target isolation and enhancement through coherent multi-view vital-Doppler detection. In Proceedings of the 2024 IEEE SENSORS Conference, Kobe, Japan, 20–23 October 2024; pp. 1–4. [Google Scholar] [CrossRef]
- Han, K.; Hong, S. Differential phase Doppler radar with collocated multiple receivers for noncontact vital signal detection. IEEE Trans. Microw. Theory Tech. 2019, 67, 1233–1243. [Google Scholar] [CrossRef]
- Xu, D.; Yu, W.; Wang, Y.; Chen, M.-L. Vital signs detection in the presence of nonperiodic body movements. IEEE Trans. Instrum. Meas. 2024, 73, 12345–12354. [Google Scholar] [CrossRef]
- Han, K.; Hong, S. MIMO differential radar using null point beams for vital sign detection in the presence of body motions. In Proceedings of the 19th European Radar Conference (EuRAD 2022), Milan, Italy, 28–30 September 2022; pp. 177–180. [Google Scholar] [CrossRef]
- Wu, Q.; Mei, Z.; Lai, Z.; Li, D.; Zhao, D. A non-contact vital signs detection in a multi-channel 77 GHz LFMCW radar system. IEEE Access 2021, 9, 106120–106128. [Google Scholar] [CrossRef]
- Wang, F.; Zeng, X.; Wu, C.; Wang, B.; Liu, K.J.R. Driver vital signs monitoring using millimeter wave radio. IEEE Internet Things J. 2022, 9, 11283–11298. [Google Scholar] [CrossRef]
- Jang, A.-J.; Lee, I.-S.; Yang, J.-R. Vital signal detection using multi-radar for reductions in body movement effects. Sensors 2021, 21, 7398. [Google Scholar] [CrossRef]
- Gomes, G.; Gouveia, C.; Albuquerque, D.; Brás, S.; Pinho, P. Dual-radar integration for vital signs acquisition under heavy body movement using machine learning. In Proceedings of the 22nd Mediterranean Electrotechnical Conference (MELECON 2024), Porto, Portugal, 25–27 June 2024; pp. 367–371. [Google Scholar] [CrossRef]
- Gharamohammadi, A.; Pirani, M.; Khajepour, A.; Shaker, G. Multi-bin breathing pattern estimation by radar fusion for enhanced driver monitoring. IEEE Trans. Instrum. Meas. 2023, 72, 1–10. [Google Scholar] [CrossRef]
- Uddin, S.D.; Li, C. Multi-view beamforming radar for random body motion cancellation. In Proceedings of the 2024 IEEE International Symposium on Antennas and Propagation and USNC-URSI Radio Science Meeting (AP-S/URSI 2024), Florence, Italy, 14–19 July 2024; pp. 1–4. [Google Scholar] [CrossRef]
- Reggad, H.; Jiang, X.; Wu, X.; Amirtharajah, R.; Matthews, D.; Liu, X. A single-chip single-antenna radar for remote vital sign monitoring. IEEE Trans. Microw. Theory Tech. 2023, 71, 4519–4532. [Google Scholar] [CrossRef]
- Tang, M.-C.; Wang, F.-K.; Horng, T.-S. Single self-injection-locked radar with two antennas for monitoring vital signs with large body movement cancellation. IEEE Trans. Microw. Theory Tech. 2017, 65, 5324–5333. [Google Scholar] [CrossRef]
- Tang, M.-C.; Kuo, C.-Y.; Wun, D.-C.; Wang, F.-K.; Horng, T.-S. A self- and mutually injection-locked radar system for monitoring vital signs in real time with random body movement cancellation. IEEE Trans. Microw. Theory Tech. 2016, 64, 4812–4822. [Google Scholar] [CrossRef]
- Tang, M.-C.; Kuo, C.-Y.; Wun, D.-C.; Wang, F.-K.; Horng, T.-S. Same side dual SIL-radar system for real-time vital sign monitoring with random body movement cancellation. In Proceedings of the 2016 IEEE MTT-S International Microwave Symposium (IMS 2016), San Francisco, CA, USA, 22–27 May 2016; pp. 1–4. [Google Scholar] [CrossRef]
- Batchu, S.; Narasimhachar, H.; Mayeda, J.C.; Hall, T.; Lopez, J.; Nguyen, T.; Banister, R.E.; Lie, D.Y.C. Overnight non-contact continuous vital signs monitoring using an intelligent automatic beam-steering Doppler sensor at 2.4 GHz. In Proceedings of the 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC 2017), Jeju, Republic of Korea, 11–15 July 2017; pp. 763–766. [Google Scholar] [CrossRef]
- Ni, C.; Pan, J.; Du, D.; Yang, X.; Shi, C.; Chen, S.; Yang, D.; Liu, S. Accurate heart rate measurement across various body postures using FMCW radar. IEEE Trans. Instrum. Meas. 2024, 73, 4006013. [Google Scholar] [CrossRef]
- Li, C.; Lubecke, V.M.; Boric-Lubecke, O.; Lin, J. A review on recent advances in Doppler radar sensors for noncontact healthcare monitoring. IEEE Trans. Microw. Theory Tech. 2013, 61, 2046–2060. [Google Scholar] [CrossRef]
- Gharamohammadi, A.; Khajepour, A.; Shaker, G. In-vehicle monitoring by radar: A review. IEEE Sensors J. 2023, 23, 25650–25672. [Google Scholar] [CrossRef]
- Paterniani, G.; Sgreccia, D.; Davoli, A.; Guerzoni, G.; Di Viestri, P.; Valenti, A.C. Radar-based monitoring of vital signs: A tutorial overview. Proc. IEEE 2023, 111, 277–317. [Google Scholar] [CrossRef]
- Li, C.; Lin, J. Random body movement cancellation in Doppler radar vital sign detection. IEEE Trans. Microw. Theory Tech. 2008, 56, 3143–3152. [Google Scholar] [CrossRef]
- Tu, J.; Hwang, T.; Lin, J. Respiration rate measurement under 1-D body motion using single continuous-wave Doppler radar vital sign detection system. IEEE Trans. Microw. Theory Tech. 2016, 64, 1937–1946. [Google Scholar] [CrossRef]
- Lv, Q.; Chen, L.; An, K.; Wang, J.; Li, H.; Ye, D.; Huangfu, J.; Li, C.; Ran, L. Doppler vital signs detection in the presence of large-scale random body movements. IEEE Trans. Microw. Theory Tech. 2018, 66, 4261–4270. [Google Scholar] [CrossRef]
- Yang, Z.-K.; Shi, H.; Zhao, S.; Huang, X.-D. Vital sign detection during large-scale and fast body movements based on an adaptive noise cancellation algorithm using a single Doppler radar sensor. Sensors 2020, 20, 4183. [Google Scholar] [CrossRef]
- Sekak, F.; Zerhouni, K.; Elbahhar, F.; Haddad, M.; Loyez, C.; Haddadi, K. Cyclostationary-based vital signs detection using microwave radar at 2.5 GHz. Sensors 2020, 20, 3396. [Google Scholar] [CrossRef]
- Min, L.; Zhang, Y.; Wang, H.; Liu, J.; Chen, X.; Yang, Y. Anti-interference heartbeat measurement based on a miniaturized Doppler radar sensor. Adv. Math. Phys. 2021, 2021, 1620938. [Google Scholar] [CrossRef]
- Ren, W.; Han, H.; Chang, S.; Liu, Q. Tracking-aided respiration detection using radar during large-scale body movements. IEEE Sens. J. 2023, 23, 17187–17199. [Google Scholar] [CrossRef]
- Dai, X.; Zhang, Y.; Wang, L.; Chen, H.; Li, J.; Liu, M. Vital signs detection of moving targets using FMCW radar. Meas. Sci. Technol. 2024, 36, 017002. [Google Scholar] [CrossRef]
- Huang, N.E.; Shen, Z.; Long, S.R.; Wu, M.C.; Shih, H.H.; Zheng, Q.; Yen, N.C.; Tung, C.C.; Liu, H.H. The empirical mode decomposition and the Hilbert spectrum for nonlinear and non-stationary time series analysis. Proc. R. Soc. Lond. A Math. Phys. Eng. Sci. 1998, 454, 903–995. [Google Scholar] [CrossRef]
- Dragomiretskiy, K.; Zosso, D. Variational mode decomposition. IEEE Trans. Signal Process. 2014, 62, 531–544. [Google Scholar] [CrossRef]
- Mostafanezhad, I.; Yavari, E.; Boric-Lubecke, O.; Lubecke, V.M.; Mandic, D.P. Cancellation of unwanted Doppler radar sensor motion using empirical mode decomposition. IEEE Sens. J. 2013, 13, 1897–1904. [Google Scholar] [CrossRef]
- Hernandez-Aguila, M.; Olvera-Cervantes, J.-L.; Perez-Ramos, A.-E.; Corona-Chavez, A. Methodology for the determination of human respiration rate by using Doppler radar and empirical modal decomposition. Sci. Rep. 2022, 12, 8675. [Google Scholar] [CrossRef]
- Cheng, P.-L.; Yang, C.-L. Heart rate detection with Hilbert vibration decomposition in random body movements based on FMCW radars. IEEE Microw. Wireless Technol. Lett. 2023, 33, 935–938. [Google Scholar] [CrossRef]
- Hu, Y.; Toda, T. Remote vital signs measurement of indoor walking persons using mm-wave FMCW radar. IEEE Access 2022, 10, 78219–78230. [Google Scholar] [CrossRef]
- Fu, S.; Ling, M.; Li, Z.; Pan, L. A new method for vital sign detection using FMCW radar based on random body motion cancellation. Biomed. Eng. Biomed. Tech. 2023, 68, 617–632. [Google Scholar] [CrossRef]
- Li, H.; Li, Z.; Mo, W. A time varying filter approach for empirical mode decomposition. Signal Process. 2017, 138, 146–158. [Google Scholar] [CrossRef]
- Qu, L.; Liu, C.; Yang, T.; Sun, Y. Vital sign detection of FMCW radar based on improved adaptive parameter variational mode decomposition. IEEE Sensors J. 2023, 23, 25048–25060. [Google Scholar]
- Hao, Z.; Gao, Y.; Tang, Y.; Wang, Y.; Fan, K.; Li, F. FMCW-Based contactless heart rate monitoring. Sci. Rep. 2025, 15, 2616. [Google Scholar] [CrossRef]
- Nazari, M.; Sakhaei, S.M. Variational mode extraction: A new efficient method to derive respiratory signals from ECG. IEEE J. Biomed. Health Inform. 2018, 22, 1059–1067. [Google Scholar] [CrossRef]
- Zhou, M.; Liu, Y.; Wu, S.; Wang, C.; Chen, Z.; Li, H. A novel scheme of high-precision heart rate detection with a mm-wave FMCW radar. IEEE Access 2023, 11, 85118–85136. [Google Scholar] [CrossRef]
- Yang, X.; Zhang, X.; Ding, Y.; Zhang, L. Indoor activity and vital sign monitoring for moving people with multiple radar data fusion. Remote Sens. 2021, 13, 3791. [Google Scholar] [CrossRef]
- Gu, C.; Wang, G.; Li, Y.; Inoue, T.; Li, C. A hybrid radar-camera sensing system with phase compensation for random body movement cancellation in Doppler vital sign detection. IEEE Trans. Microw. Theory Tech. 2013, 61, 4678–4688. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, Z.; Zhang, J.A.; Zhang, H.; Xu, M. Vital sign monitoring in dynamic environment via mmWave radar and camera fusion. IEEE Trans. Mob. Comput. 2024, 23, 4163–4180. [Google Scholar] [CrossRef]
- Arsalan, M.; Janjua, M.G.; Santra, A.; Issakov, V. Radar-based vital signal classification: Detecting random body movement and inter-modulation products with temporal convolutional networks. In Proceedings of the 21st European Radar Conference (EuRAD 2024), Paris, France, 25–27 September 2024; pp. 164–167. [Google Scholar] [CrossRef]
- Gu, C.; Wang, J.; Lien, J. Deep neural network based body movement cancellation for Doppler radar vital sign detection. In Proceedings of the 2019 IEEE MTT-S International Wireless Symposium (IWS), Guangzhou, China, 19–22 May 2019; pp. 1–3. [Google Scholar] [CrossRef]
- Gong, J.; Zhang, X.; Lin, K.; Ren, J.; Zhang, Y.; Qiu, W. RF vital sign sensing under free body movement. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 101. [Google Scholar] [CrossRef]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, M.-S.; Park, Y.; Park, J.-E.; Lee, G.-H.; Jeon, S.-H.; Lee, J.-H.; Yoon, J.-H.; Yang, J.-R. Motion Cancellation Technique of Vital Signal Detectors Based on Continuous-Wave Radar Technology. Sensors 2025, 25, 2156. https://doi.org/10.3390/s25072156
Kwon M-S, Park Y, Park J-E, Lee G-H, Jeon S-H, Lee J-H, Yoon J-H, Yang J-R. Motion Cancellation Technique of Vital Signal Detectors Based on Continuous-Wave Radar Technology. Sensors. 2025; 25(7):2156. https://doi.org/10.3390/s25072156
Chicago/Turabian StyleKwon, Min-Seok, Yuna Park, Joo-Eun Park, Geon-Haeng Lee, Sang-Hoon Jeon, Jae-Hyun Lee, Joon-Hyuk Yoon, and Jong-Ryul Yang. 2025. "Motion Cancellation Technique of Vital Signal Detectors Based on Continuous-Wave Radar Technology" Sensors 25, no. 7: 2156. https://doi.org/10.3390/s25072156
APA StyleKwon, M.-S., Park, Y., Park, J.-E., Lee, G.-H., Jeon, S.-H., Lee, J.-H., Yoon, J.-H., & Yang, J.-R. (2025). Motion Cancellation Technique of Vital Signal Detectors Based on Continuous-Wave Radar Technology. Sensors, 25(7), 2156. https://doi.org/10.3390/s25072156





