A Longitudinal Study of Physical Function Factors Related to Lower Limb Circumduction During Gait in Acute Stroke Patients with Hemiparesis
Highlights
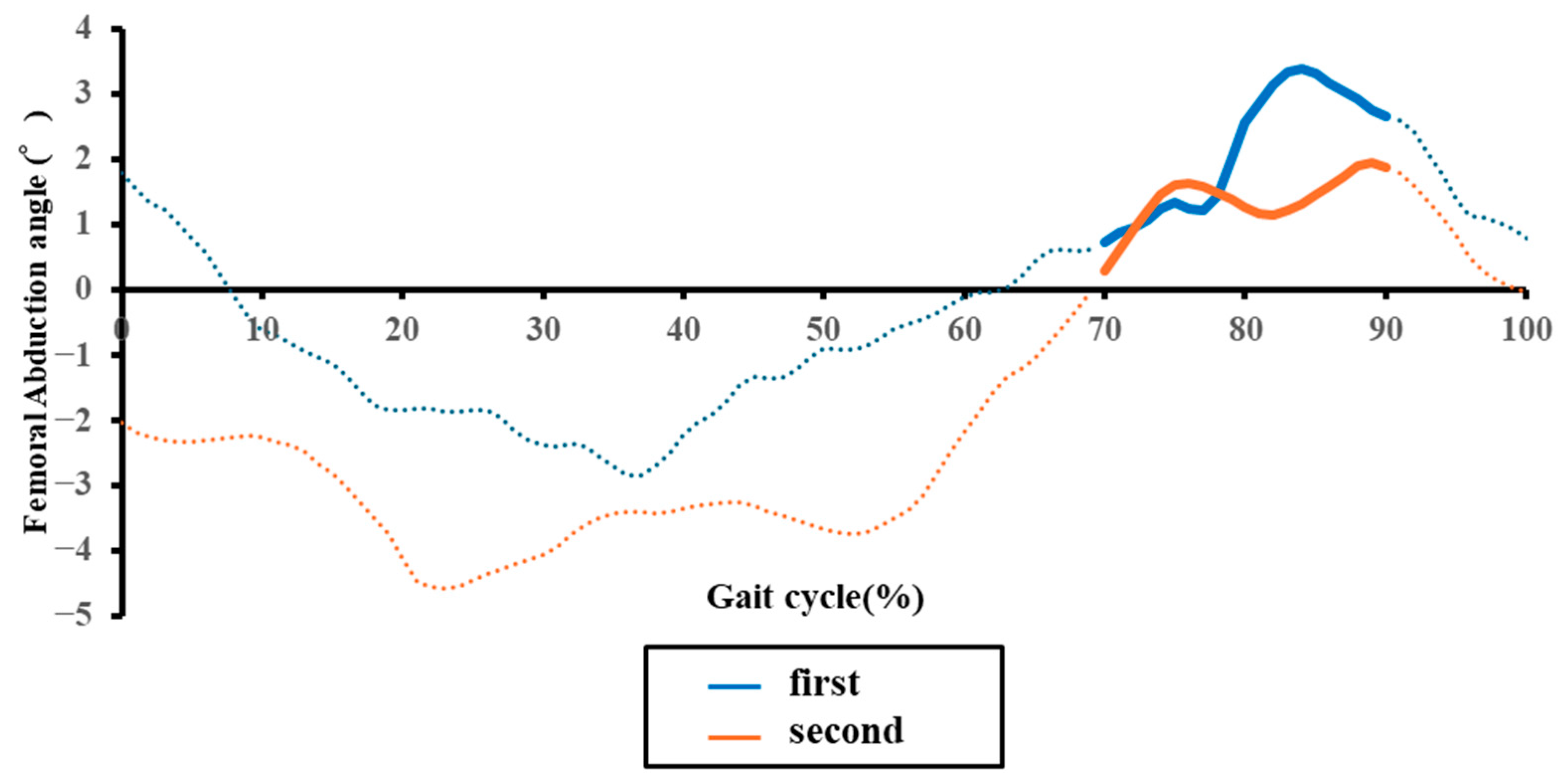
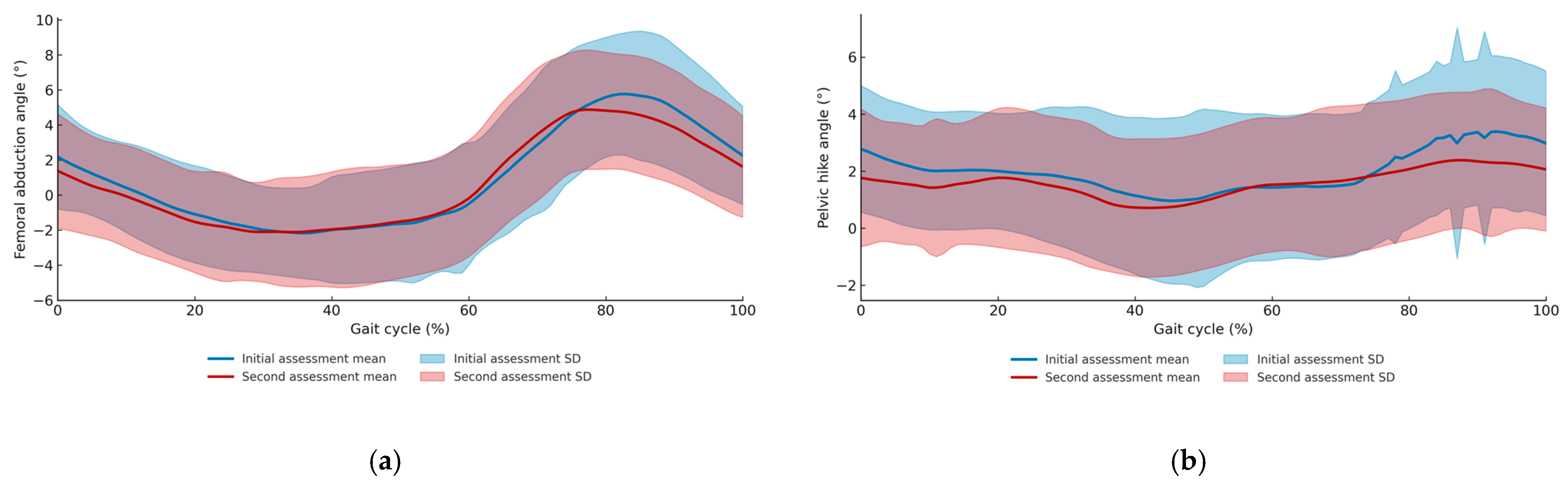
- Paretic femoral abduction and pelvic hike angles significantly decreased over time in acute stroke patients.
- Reduced femoral abduction correlated with paretic ankle motor recovery, while reduced pelvic hike correlated with paretic knee motor recovery.
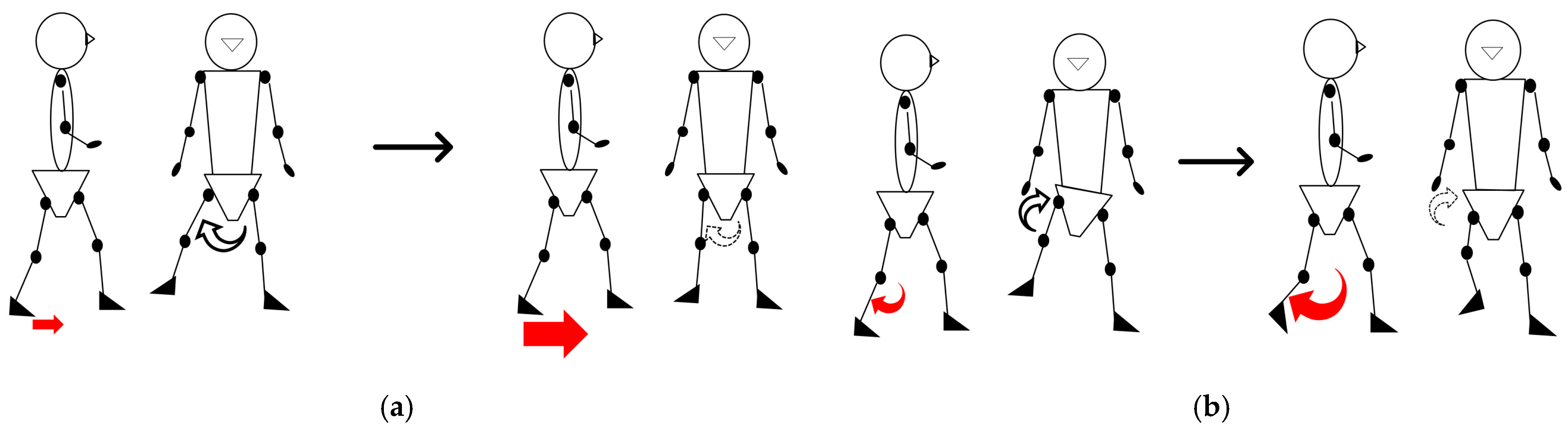
- Femoral abduction and pelvic hike are distinct adaptive strategies, not a single “circumduction” pattern as often assumed.
- Compensatory movements in acute stroke should be re-evaluated as adaptive phenomena during recovery, not merely as abnormal movements.
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
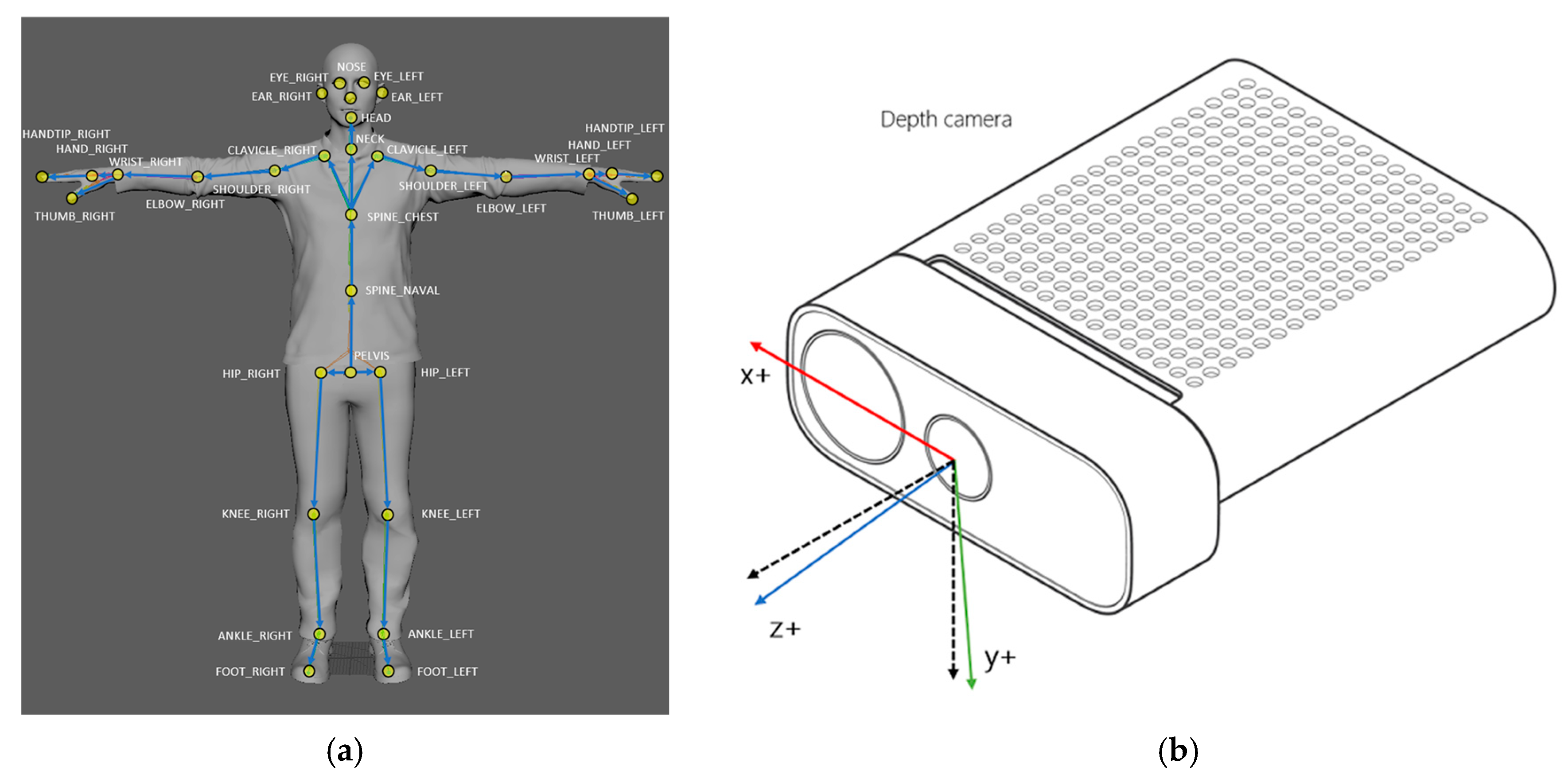
2.2. Measuring Equipment
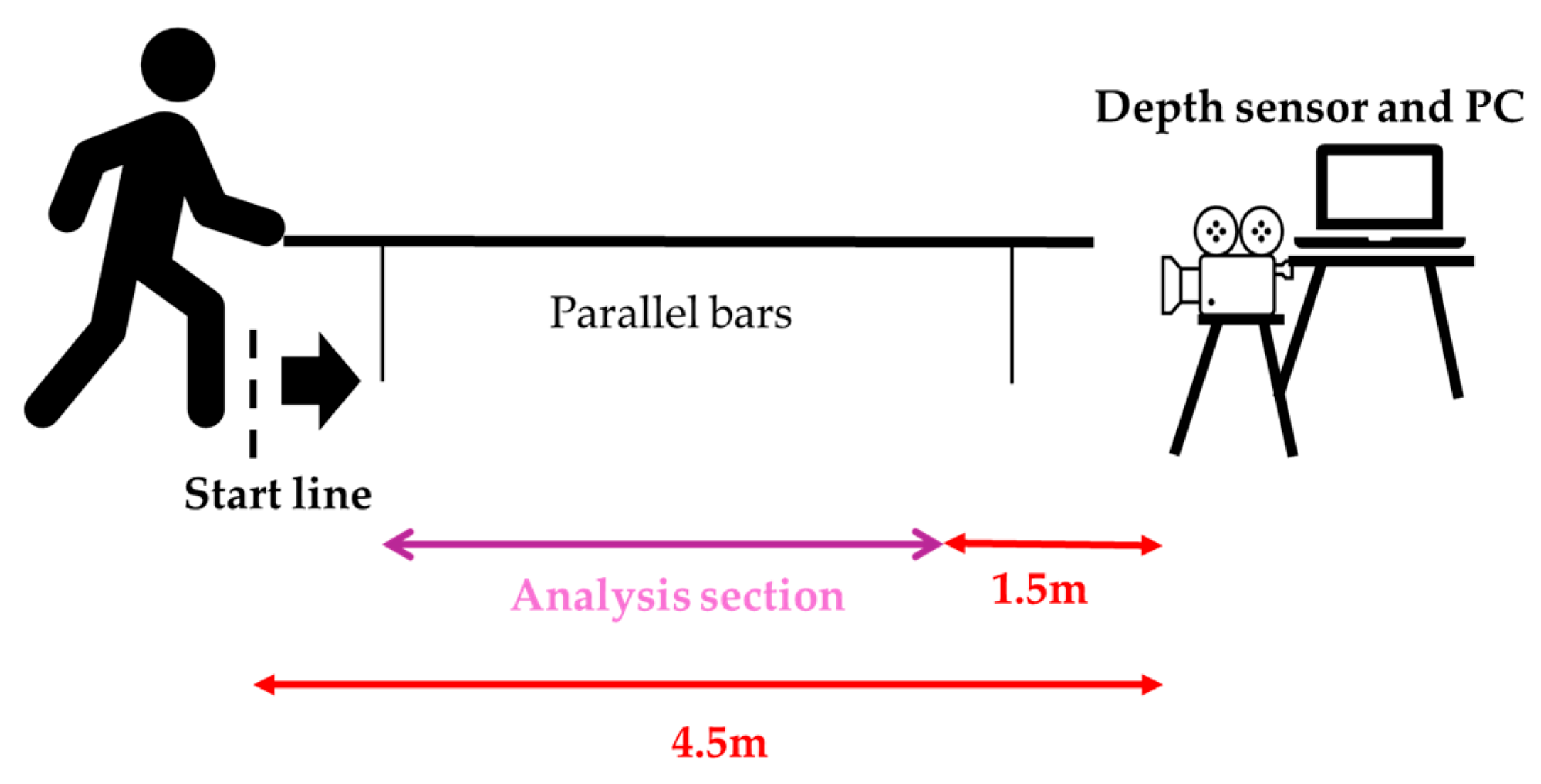
2.3. Gait Assessment
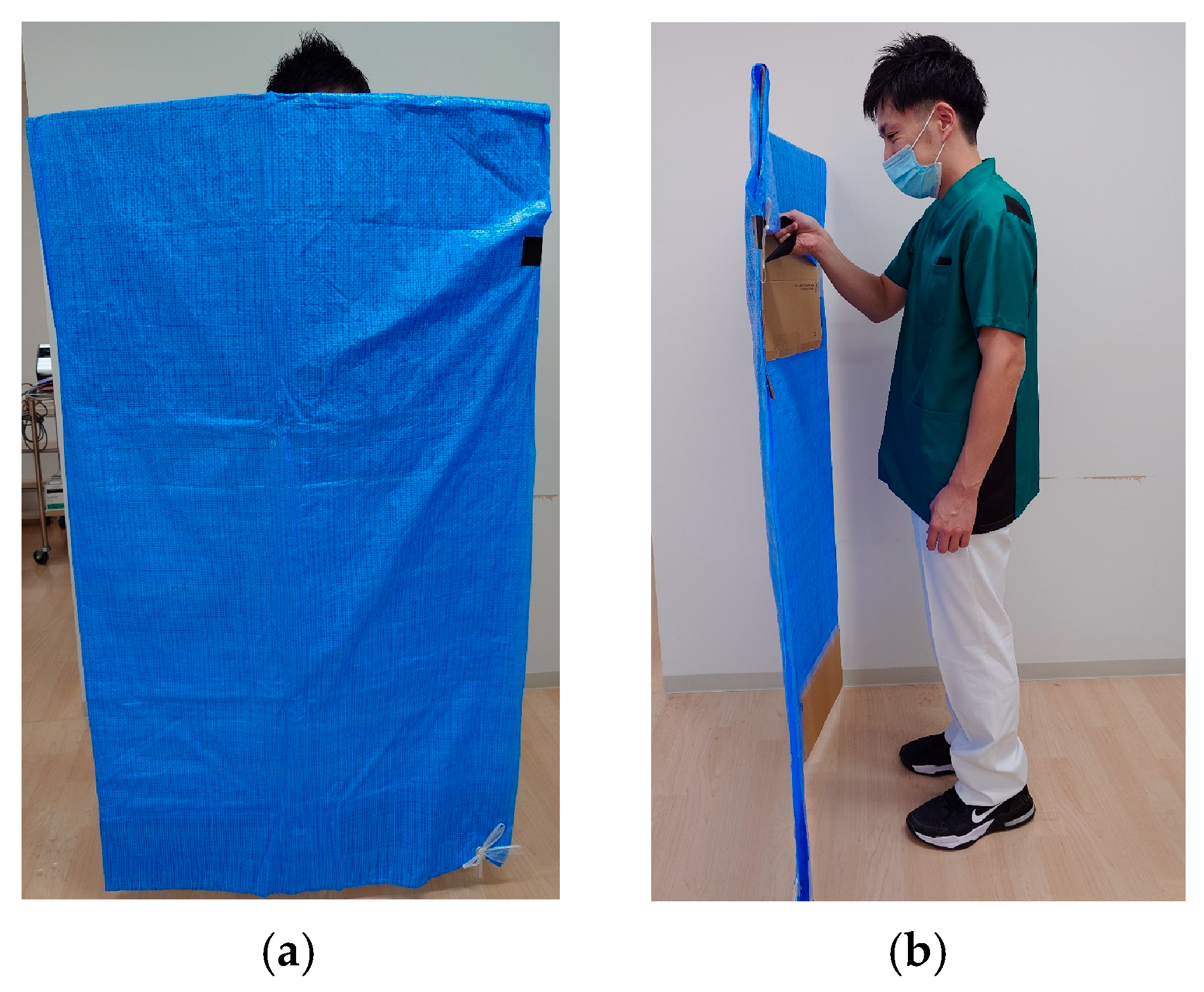
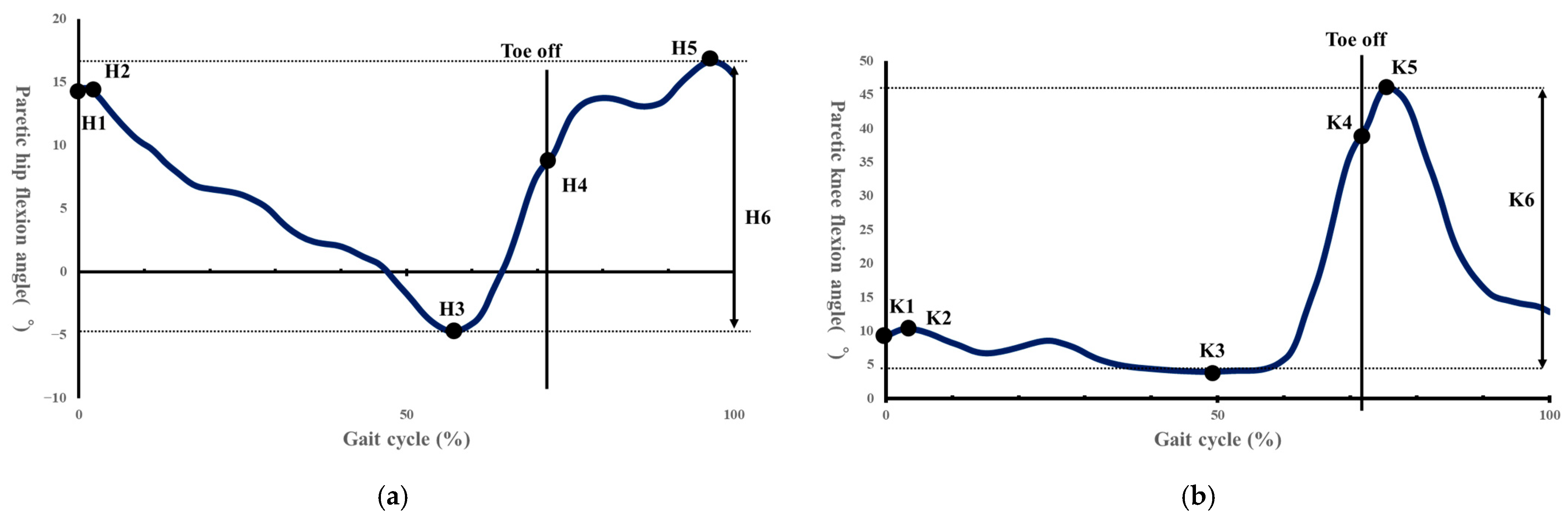
2.4. Data Processing
2.5. Statical Analysis
3. Results
3.1. Participant Characteristics
3.2. Longitudinal Changes in Gait Parameters
3.3. Longitudinal Changes in Measures of Physical Function
3.4. Associations Between Changes in Compensatory Movements and Motor Function
4. Discussion
4.1. Relationship Between Compensatory Movements and Gait/Physical Function at Initial Assessment
4.2. Longitudinal Changes in Gait: Context for Compensation Attenuation
4.3. Temporal Changes in Paretic Femoral Abduction Angle and Its Relationship with Physical Function
4.4. Temporal Changes in Paretic Pelvic Hike and Its Relationship with Physical Function
4.5. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Imanawanto, K.; Andriana, M.; Satyawati, R. Correlation Between Joint Position Sense, Threshold to Detection of Passive Motion of the Knee Joint and Walking Speed of Post-Stroke Patient. Int. J. Res. Publ. 2021, 83, 110–118. [Google Scholar] [CrossRef]
- Mizuta, N.; Hasui, N.; Nakatani, T.; Takamura, Y.; Fujii, S.; Tsutsumi, M.; Taguchi, J.; Morioka, S. Walking characteristics including mild motor paralysis and slow walking speed in post-stroke patients. Sci. Rep. 2020, 10, 11819. [Google Scholar] [CrossRef]
- Odetunde, M.O.; Makinde, A.F.; Jimoh, O.M.; Mbada, C.E.; Niyi-Odumosu, F.; Fatoye, F. Physical activity, fatigue severity, and health-related quality of life of community-dwelling stroke survivors: A cross-sectional study. Bull. Fac. Phys. Ther. 2025, 30, 9. [Google Scholar] [CrossRef]
- Balbinot, G.; Schuch, C.P.; Oliveira, H.B.; Peyré-Tartaruga, L.A. Mechanical and energetic determinants of impaired gait following stroke: Segmental work and pendular energy transduction during treadmill walking. Biol. Open 2020, 9, bio051581. [Google Scholar] [CrossRef]
- Fulk, G.D.; He, Y.; Boyne, P.; Dunning, K. Predicting Home and Community Walking Activity Poststroke. Stroke 2017, 48, 406–411. [Google Scholar] [CrossRef]
- Ribeiro, J.A.M.; Oliveira, S.G.; di Thommazo-Luporini, L.; Phillips, S.A.; Catai, A.M.; Borghi-Silva, A.; Ribeiro, J.A.M.; Oliveira, S.G.; di Thommazo-Luporini, L.; Monteiro, C.I.; et al. Energy Cost During the 6-Min Walk Test and Its Relationship to Real-World Walking After Stroke: A Correlational, Cross-Sectional Pilot Study. Phys. Ther. 2019, 99, 1656–1666. Available online: https://academic.oup.com/ptj (accessed on 5 May 2024). [CrossRef]
- Ardestani, M.M.; Kinnaird, C.R.; Henderson, C.E.; Hornby, T.G. Compensation or Recovery? Altered Kinetics and Neuromuscular Synergies Following High-Intensity Stepping Training Poststroke. Neurorehabilit. Neural Repair 2019, 33, 47–58. [Google Scholar] [CrossRef]
- Kerrigan, D.C.; Frates, E.P.; Rogan, S.; Riley, P.O. Hip Hiking and Circumduction Quantitative Definitions. Am. J. Phys. Med. Rehabil. 2000, 79, 247–252. [Google Scholar] [CrossRef]
- Awad, L.N.; Bae, J.; Kudzia, P.; Long, A.; Hendron, K.; Holt, K.G.; O’ Donnell, K.; Ellis, T.D.; Walsh, C.J. Reducing Circumduction and Hip Hiking During Hemiparetic Walking Through Targeted Assistance of the Paretic Limb Using a Soft Robotic Exosuit. Am. J. Phys. Med. Rehabil. 2017, 96, S157–S164. [Google Scholar] [CrossRef] [PubMed]
- Mahtani, G.B.; Kinnaird, C.R.; Connolly, M.; Holleran, C.L.; Hennessy, P.W.; Woodward, J.; Brazg, G.; Roth, E.J.; Hornby, T.G. Altered Sagittal-and Frontal-Plane Kinematics Following High-Intensity Stepping Training Versus Conventional Interventions in Subacute Stroke Background. Common locomotor deficits observed in people poststroke include. Orig. Res. 2017, 97, 320–329. [Google Scholar]
- Zissimopoulos, A.; Fatone, S.; Gard, S. Effects of ankle-foot orthoses on mediolateral foot-placement ability during post-stroke gait. Prosthet. Orthot. Int. 2015, 39, 372–379. [Google Scholar] [CrossRef]
- Akbas, T.; Neptune, R.R.; Sulzer, J. Neuromusculoskeletal simulation reveals abnormal rectus femoris-gluteus medius coupling in post-stroke gait. Front. Neurol. 2019, 10, 301. [Google Scholar] [CrossRef]
- Stanhope, V.A.; Knarr, B.A.; Reisman, D.S.; Higginson, J.S. Frontal plane compensatory strategies associated with self-selected walking speed in individuals post-stroke. Clin. Biomech. 2014, 29, 518–522. [Google Scholar] [CrossRef]
- Akbas, T.; Prajapati, S.; Ziemnicki, D.; Tamma, P.; Gross, S.; Sulzer, J. Hip circumduction is not a compensation for reduced knee flexion angle during gait. J. Biomech. 2019, 87, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Tamaya, V.C.; Wim, S.; Herssens, N.; van de Walle, P.; Willem, D.H.; Steven, T.; Ann, H. Trunk biomechanics during walking after sub-acute stroke and its relation to lower limb impairments. Clin. Biomech. 2020, 75, 105013. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Seamon, B.A.; Lee, R.K.; Kautz, S.A.; Neptune, R.R.; Sulzer, J.S. Post-stroke Stiff-Knee gait: Are there different types or different severity levels? J. Neuroeng. Rehabil. 2025, 22, 36. [Google Scholar] [CrossRef]
- Akbas, T.; Kim, K.; Doyle, K.; Manella, K.; Lee, R.; Spicer, P.; Knikou, M.; Sulzer, J. Rectus femoris hyperreflexia contributes to Stiff-Knee gait after stroke. J. Neuroeng. Rehabil. 2020, 17, 117. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.Y.; Lee, R.K.; Spicer, P.; Sulzer, J. Does kinematic gait quality improve with functional gait recovery? A longitudinal pilot study on early post-stroke individuals. J. Biomech. 2020, 105, 109761. [Google Scholar] [CrossRef]
- Cavaggioni, L.; Trecroci, A.; Formenti, D.; Hogarth, L.; Tosin, M.; Alberti, G. Seasonal changes in breathing pattern, trunk stabilization, and muscular power in paralympic swimmers. Adapt. Phys. Act. Q. 2021, 38, 215–231. [Google Scholar] [CrossRef]
- Han, X.; Guffanti, D.; Brunete, A. A Comprehensive Review of Vision-Based Sensor Systems for Human Gait Analysis. Sensors 2025, 25, 498. [Google Scholar] [CrossRef] [PubMed]
- Microsoft. Azure Kinect Body Tracking Joints. Available online: https://learn.microsoft.com/ja-jp/previous-versions/azure/kinect-dk/body-joints (accessed on 7 November 2025).
- Microsoft. Azure Kinect DK Coordinate System. Available online: https://learn.microsoft.com/ja-jp/previous-versions/azure/kinect-dk/coordinate-systems (accessed on 19 November 2025).
- Bawa, A.; Banitsas, K.; Abbod, M. A Review on the Use of Microsoft Kinect for Gait Abnormality and Postural Disorder Assessment. J. Healthc. Eng. 2021, 2021, 4360122. [Google Scholar] [CrossRef]
- Sugai, R.; Maeda, S.; Shibuya, R.; Sekiguchi, Y.; Izumi, S.I.; Hayashibe, M.; Owaki, D. LSTM Network-Based Estimation of Ground Reaction Forces During Walking in Stroke Patients Using Markerless Motion Capture System. IEEE Trans. Med. Robot. Bionics 2023, 5, 1016–1024. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Eltoukhy, M.; Oh, J.; Kuenze, C.; Signorile, J. Improved kinect-based spatiotemporal and kinematic treadmill gait assessment. Gait Posture 2017, 51, 77–83. [Google Scholar] [CrossRef]
- Eltoukhy, M.; Kuenze, C.; Oh, J.; Jacopetti, M.; Wooten, S.; Signorile, J. Microsoft Kinect can distinguish differences in over-ground gait between older persons with and without Parkinson’s disease. Med. Eng. Phys. 2017, 44, 1–7. [Google Scholar] [CrossRef]
- Shibuya, R. Verification of the Reliability of Gait Data for Patients with Hemiparesis Measured by a Depth Sensor. Master’s Thesis, Department of Disability Science, Graduate School of Medicine, Tohoku University, Sendai, Japan. Unpublished.
- Kazuhisa, D. Consistency and validity of the Stroke Impairment Assessment Set (SIAS) in hemiplegic stroke patients (1)—Motor function, muscle tone, tendon reflexes, and healthy side function on the paretic side. Rehabil. Med. 1995, 32, 113–122. [Google Scholar]
- Sonoda, S. Consistency and validity of the Stroke Impairment Assessment Set (SIAS) for functional assessment of hemiplegic stroke patients (2)—Trunk, higher brain function, sensory items and outcome prediction. Rehabil. Med. 1995, 32, 123–132. [Google Scholar]
- Yeh, T.T.; Chang, K.C.; Wu, C.Y. The Active Ingredient of Cognitive Restoration: A Multicenter Randomized Controlled Trial of Sequential Combination of Aerobic Exercise and Computer-Based Cognitive Training in Stroke Survivors with Cognitive Decline. Arch. Phys. Med. Rehabil. 2019, 100, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Tölgyessy, M.; Dekan, M.; Chovanec, Ľ.; Hubinský, P. Evaluation of the azure kinect and its comparison to kinect v1 and kinect v2. Sensors 2021, 21, 413. [Google Scholar] [CrossRef]
- Kharazi, M.R.; Memari, A.H.; Shahrokhi, A.; Nabavi, H.; Khorami, S.; Rasooli, A.H.; Barnamei, H.R.; Jamshidian, A.R.; Mirbagheri, M.M. Validity of microsoft kinectTM for measuring gait parameters. In Proceedings of the 2015 22nd Iranian Conference on Biomedical Engineering, ICBME 2015, Online, 25–27 November 2015; pp. 375–379. [Google Scholar] [CrossRef]
- Springer, S.; Seligmann, G.Y. Validity of the kinect for gait assessment: A focused review. Sensors 2016, 16, 194. [Google Scholar] [CrossRef]
- Zeni, J.A., Jr.; Richards, J.G.; Higginson, J. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture 2008, 27, 710–714. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.; Gamble, J.G. Human Walking; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006; pp. 33–51. [Google Scholar]
- Kinsella, S.; Moran, K. Gait pattern categorization of stroke participants with equinus deformity of the foot. Gait Posture 2008, 27, 144–151. [Google Scholar] [CrossRef]
- Chan, Y.H. Biostatistics 104: Correlational analysis. Singap. Med. J. 2003, 44, 614–619. [Google Scholar]
- Dean, J.C.; Embry, A.E.; Stimpson, K.H.; Perry, L.A.; Kautz, S.A. Effects of hip abduction and adduction accuracy on post-stroke gait. Clin. Biomech. 2017, 44, 14–20. [Google Scholar] [CrossRef]
- Wang, Y.; Mukaino, M.; Ohtsuka, K.; Otaka, Y.; Tanikawa, H.; Matsuda, F.; Tsuchiyama, K.; Yamada, J.; Saitoh, E. Gait characteristics of post-stroke hemiparetic patients with different walking speeds. Int. J. Rehabil. Res. 2020, 43, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Haruyama, K.; Kawakami, M.; Okada, K.; Okuyama, K.; Tsuzuki, K.; Liu, M. Pelvis-toe distance: 3-dimensional gait characteristics of functional limb shortening in hemiparetic stroke. Sensors 2021, 21, 5417. [Google Scholar] [CrossRef] [PubMed]
- Little, V.L.; McGuirk, T.E.; Perry, L.A.; Patten, C. Pelvic excursion during walking post-stroke: A novel classification system. Gait Posture 2018, 62, 395–404. [Google Scholar] [CrossRef]
- Kwakkel, G.; van Peppen, R.; Wagenaar, R.C.; Dauphinee, S.W.; Richards, C.; Ashburn, A.; Miller, K.; Lincoln, N.; Partridge, C.; Wellwood, I.; et al. Effects of augmented exercise therapy time after stroke: A meta-analysis. Stroke 2004, 35, 2529–2536. [Google Scholar] [CrossRef]
- Patterson, K.K.; Parafianowicz, I.; Danells, C.J.; Closson, V.; Verrier, M.C.; Staines, W.R.; Black, S.E.; McIlroy, W.E. Gait Asymmetry in Community-Ambulating Stroke Survivors. Arch. Phys. Med. Rehabil. 2008, 89, 304–310. [Google Scholar] [CrossRef]
- Mizuike, C.; Ohgi, S.; Morita, S. Analysis of stroke patient walking dynamics using a tri-axial accelerometer. Gait Posture 2009, 30, 60–64. [Google Scholar] [CrossRef]
- Kettlety, S.A.; Finley, J.M.; Reisman, D.S.; Schweighofer, N.; Leech, K.A. Speed-dependent biomechanical changes vary across individual gait metrics post-stroke relative to neurotypical adults. J. Neuroeng. Rehabil. 2023, 20, 14. [Google Scholar] [CrossRef]
- Awad, L.N.; Palmer, J.A.; Pohlig, R.T.; Binder-Macleod, S.A.; Reisman, D.S. Walking speed and step length asymmetry modify the energy cost of walking after stroke. Neurorehabilit. Neural Repair 2015, 29, 416–423. [Google Scholar] [CrossRef]
- Balasubramanian, C.K.; Bowden, M.G.; Neptune, R.R.; Kautz, S.A. Relationship Between Step Length Asymmetry and Walking Performance in Subjects with Chronic Hemiparesis. Arch. Phys. Med. Rehabil. 2007, 88, 43–49. [Google Scholar] [CrossRef]
- Sánchez, N.; Acosta, A.M.; López-Rosado, R.; Dewald, J.P.A. Neural constraints affect the ability to generate hip abduction torques when combined with hip extension or ankle plantarflexion in chronic hemiparetic stroke. Front. Neurol. 2018, 9, 564. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.B.; Kim, J.S.; Hong, B.Y.; Sul, B.; Song, S.; Sung, W.J.; Hwang, B.Y.; Lim, S.H. Brain lesions affecting gait recovery in stroke patients. Brain Behav. 2017, 7, e00868. [Google Scholar] [CrossRef] [PubMed]
- Wren, T.A.L.; Tucker, C.A.; Rethlefsen, S.A.; Gorton, G.E.; Õunpuu, S. Clinical efficacy of instrumented gait analysis: Systematic review 2020 update. Gait Posture 2020, 80, 274–279. [Google Scholar] [CrossRef] [PubMed]
| Stroke Patients | ||
|---|---|---|
| Gender (male/female) a | 17/5 | |
| Age (year) b | 66.05 | (15.44) |
| Height (m) b | 1.65 | (0.08) |
| Weight (kg) b | 68.43 | (15.43) |
| Diagnosis (Hemorrhage/Infarction) a | 5/17 | |
| Paretic side (left/right) a | 14/8 | |
| Time since onset (days) b | 8.77 | (5.27) |
| Longitudinal study period | 12.95 | (1.15) |
| Physical therapy time during longitudinal period (minutes) | 25.72 | (7.68) |
| Spatiotemporal Parameters | Initial Assessment | Second Assessment | Effect Size | p-Value |
|---|---|---|---|---|
| Gait speed (m/s) a | 0.38 (0.16) | 0.53 (0.18) | −1.18 | <0.001 |
| Double stance time (s) b | 0.49 (0.23) | 0.35 (0.18) | 0.88 | <0.001 |
| Paretic stance time (s) a | 1.44 (0.54) | 1.10 (0.34) | −0.79 | <0.001 |
| Paretic swing time (s) b | 0.53 (0.16) | 0.48 (0.11) | −0.42 | 0.051 |
| Stride length on the paretic side (m) a | 0.66 (0.15) | 0.78 (0.14) | −1.08 | <0.001 |
| Step length on the paretic side (m) a | 0.31 (0.08) | 0.36 (0.07) | −0.72 | 0.003 |
| Step width (m) a | 0.13 (0.03) | 0.12 (0.04) | 0.30 | 0.174 |
| Paretic femoral abduction angle (°) a | 6.71 (3.78) | 5.79 (3.47) | 0.51 | 0.049 |
| Paretic pelvic hike angle (°) a | 3.82 (2.34) | 2.90 (2.35) | 0.51 | 0.025 |
| H1 (°) b | 23.18 (5.67) | 23.93 (4.30) | −0.17 | 0.424 |
| H2 (°) a | 23.20 (5.40) | 24.02 (4.29) | −0.20 | 0.367 |
| H3 (°) a | −3.89 (6.17) | −5.91 (5.13) | 0.42 | 0.064 |
| H4 (°) a | 5.52 (7.12) | 4.69 (5.76) | 0.14 | 0.521 |
| H5 (°) a | 24.28 (6.79) | 25.55 (5.49) | −0.25 | 0.263 |
| H6 (°) a | 29.59 (5.42) | 32.32 (5.43) | −0.47 | 0.039 |
| K1 (°) a | 9.93 (5.16) | 8.58 (5.23) | 0.34 | 0.124 |
| K2 (°) a | 15.15 (4.80) | 15.09 (6.20) | 0.01 | 0.963 |
| K3 (°) a | 5.65 (3.16) | 5.96 (4.40) | −0.13 | 0.543 |
| K4 (°) a | 35.24 (10.95) | 37.74 (8.89) | −0.36 | 0.108 |
| K5 (°) a | 46.65 (11.67) | 50.87 (10.82) | −0.51 | 0.026 |
| K6 (°) a | 41.82 (10.73) | 45.84 (9.77) | −0.48 | 0.036 |
| SIAS Evaluation Items | First Assessment | Second Assessment | Effect Size | p-Value |
|---|---|---|---|---|
| Hip joint (0/1/2/3/4/5) a | 3 (4-2) | 4 (5-3) | −0.82 | <0.001 |
| Knee joint (0/1/2/3/4/5) a | 4 (4-3) | 4 (5-3) | −0.58 | 0.006 |
| Ankle joint (0/1/2/3/4/5) a | 3 (4-2) | 4 (5-3) | −0.74 | <0.001 |
| L/E Deep tendon reflex (0/1/2/3) a | 1 (2-1) | 2 (2-1) | −0.30 | 0.153 |
| L/E muscle tone (0/1/2/3) a | 2 (3-2) | 3 (3-2) | −0.30 | 0.160 |
| Superficial sensation (0/1/2/3) a | 3 (3-3) | 3 (3-3) | −0.37 | 0.083 |
| Deep sensation (0/1/2/3) a | 3 (3-3) | 3 (3-3) | −0.42 | 0.046 |
| Abdominal strength (0/1/2/3) a | 1 (2-0) | 2 (3-2) | −0.66 | 0.002 |
| Spatiotemporal and Kinematic Variables | Mean (SD) | Paretic Side Femoral Abduction Angle | Paretic Side Pelvic Hike Angle | ||||
|---|---|---|---|---|---|---|---|
| Correlation | p-Value | 1 − β | Correlation | p-Value | 1 − β | ||
| Gait speed Δ (m/s) a | 0.15 (0.13) | 0.09 | 0.701 | 0.94 | 0.03 | 0.886 | 0.97 |
| Double stance time Δ (s) a | −0.14 (0.16) | −0.24 | 0.290 | 0.81 | 0.12 | 0.609 | 0.92 |
| Paretic stance time Δ (s) b | −0.34 (0.34) | −0.19 | 0.393 | 0.87 | 0.10 | 0.661 | 0.94 |
| Paretic swing time Δ (s) b | −0.05 (0.13) | 0.32 | 0.148 | 0.70 | 0.41 | 0.058 | 0.52 |
| Paretic stride length Δ (m) a | 0.12 (0.11) | 0.03 | 0.881 | 0.97 | 0.00 | 0.996 | 0.98 |
| Paretic step length Δ (m) a | 0.04 (0.06) | −0.03 | 0.892 | 0.97 | 0.15 | 0.517 | 0.90 |
| Step width Δ (m) a | −0.01 (0.03) | −0.22 | 0.332 | 0.84 | 0.12 | 0.604 | 0.92 |
| Paretic pelvic hike Δ (°) a | −0.91 (1.74) | 0.55 | 0.008 | 0.23 | - | - | |
| H1Δ (°) b | 0.75 (4.33) | −0.31 | 0.154 | 0.71 | −0.32 | 0.148 | 0.70 |
| H2Δ (°) a | 0.83 (4.20) | −0.34 | 0.118 | 0.66 | −0.27 | 0.221 | 0.77 |
| H3Δ (°) a | −2.02 (4.84) | −0.03 | 0.886 | 0.97 | −0.14 | 0.545 | 0.91 |
| H4Δ (°) a | −0.83 (5.99) | 0.02 | 0.938 | 0.97 | −0.14 | 0.540 | 0.91 |
| H5Δ (°) a | 1.27 (5.19) | −0.13 | 0.557 | 0.92 | −0.13 | 0.557 | 0.92 |
| H6Δ (°) a | 2.73 (5.82) | −0.09 | 0.679 | 0.94 | 0.02 | 0.936 | 0.97 |
| K1Δ (°) a | −1.35 (3.94) | −0.09 | 0.690 | 0.94 | −0.25 | 0.271 | 0.80 |
| K2Δ (°) a | −0.06 (5.98) | −0.23 | 0.311 | 0.83 | −0.13 | 0.569 | 0.92 |
| K3Δ (°) a | 0.31 (2.38) | −0.36 | 0.096 | 0.62 | −0.22 | 0.324 | 0.84 |
| K4Δ (°) a | 2.49 (6.96) | 0.26 | 0.247 | 0.79 | 0.03 | 0.894 | 0.97 |
| K5Δ (°) a | 4.22 (8.24) | 0.1 | 0.660 | 0.94 | 0.09 | 0.700 | 0.94 |
| K6Δ (°) a | 4.02 (8.40) | 0.19 | 0.388 | 0.87 | 0.13 | 0.573 | 0.92 |
| SIAS Evaluation Items | Median (IQR) | Paretic Side Femoral Abduction Angle | Paretic Side Pelvic Hike Angle | ||||
|---|---|---|---|---|---|---|---|
| Correlation | p-Value | 1 − β | Correlation | p-Value | 1 − β | ||
| Hip joint Δ b | 1 (1-1) | 0.42 | 0.050 | 0.50 | −0.20 | 0.371 | 0.86 |
| Knee joint Δ b | 0 (1-0) | −0.28 | 0.203 | 0.76 | −0.43 | 0.046 | 0.48 |
| Ankle joint Δ b | 1 (1-0) | −0.49 | 0.021 | 0.35 | −0.01 | 0.962 | 0.97 |
| L/E deep tendon reflex Δ b | 0 (1-0) | −0.34 | 0.121 | 0.66 | −0.13 | 0.566 | 0.92 |
| L/E muscle tone Δ b | 0 (0) | 0.01 | 0.969 | 0.66 | −0.31 | 0.161 | 0.71 |
| L/E superficial sensation Δ b | 0 (0) | −0.16 | 0.487 | 0.97 | −0.03 | 0.888 | 0.97 |
| L/E deep sensation Δ b | 0 (0) | 0.02 | 0.935 | 0.90 | 0.13 | 0.559 | 0.92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shibuya, R.; Sekiguchi, Y.; Honda, K.; Miyagi, M.; Owaki, D.; Hayashibe, M.; Ebihara, S. A Longitudinal Study of Physical Function Factors Related to Lower Limb Circumduction During Gait in Acute Stroke Patients with Hemiparesis. Sensors 2025, 25, 7309. https://doi.org/10.3390/s25237309
Shibuya R, Sekiguchi Y, Honda K, Miyagi M, Owaki D, Hayashibe M, Ebihara S. A Longitudinal Study of Physical Function Factors Related to Lower Limb Circumduction During Gait in Acute Stroke Patients with Hemiparesis. Sensors. 2025; 25(23):7309. https://doi.org/10.3390/s25237309
Chicago/Turabian StyleShibuya, Ryosuke, Yusuke Sekiguchi, Keita Honda, Midori Miyagi, Dai Owaki, Mitsuhiro Hayashibe, and Satoru Ebihara. 2025. "A Longitudinal Study of Physical Function Factors Related to Lower Limb Circumduction During Gait in Acute Stroke Patients with Hemiparesis" Sensors 25, no. 23: 7309. https://doi.org/10.3390/s25237309
APA StyleShibuya, R., Sekiguchi, Y., Honda, K., Miyagi, M., Owaki, D., Hayashibe, M., & Ebihara, S. (2025). A Longitudinal Study of Physical Function Factors Related to Lower Limb Circumduction During Gait in Acute Stroke Patients with Hemiparesis. Sensors, 25(23), 7309. https://doi.org/10.3390/s25237309







