A Smartwatch or Just a Watch? A Validation Study of the Smartwatch KC08 for Measuring Blood Pressure
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Measurements
2.2.1. Primary Outcome: Blood Pressure Measurement
2.2.2. Secondary Outcomes: Heart Rate and Blood Oxygen Saturation Measurement
2.3. Statistical Analyses
3. Results
3.1. Participants
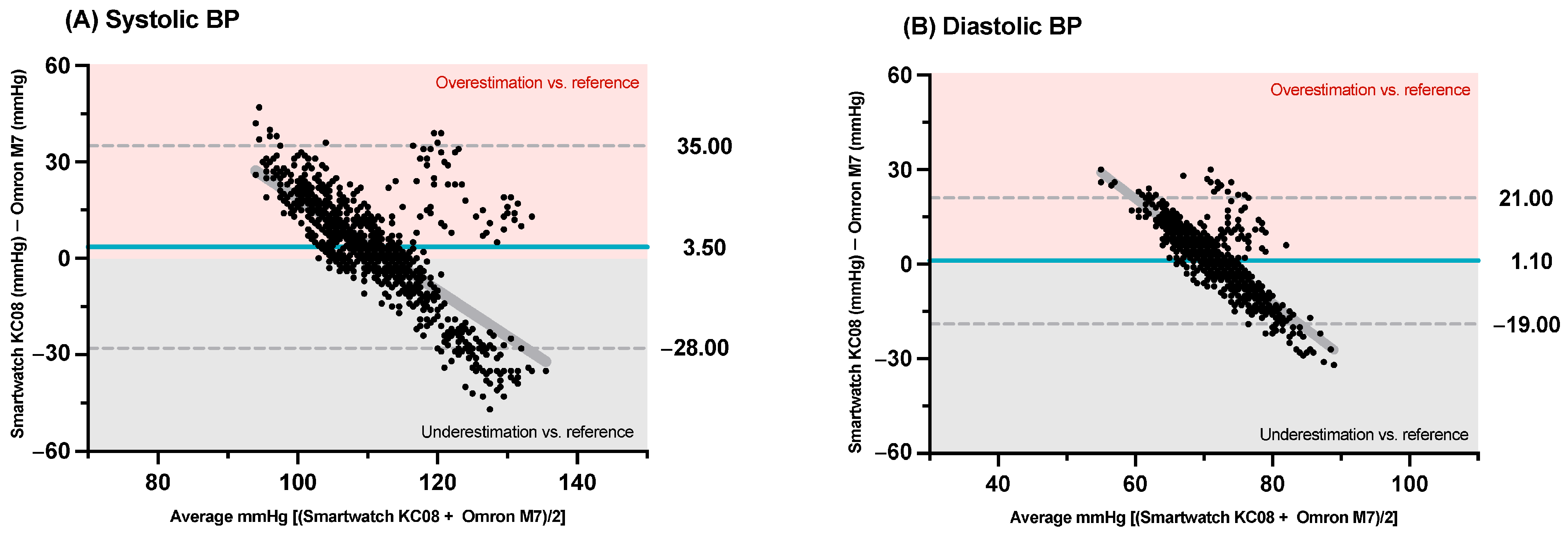
3.2. Primary Outcome: Blood Pressure
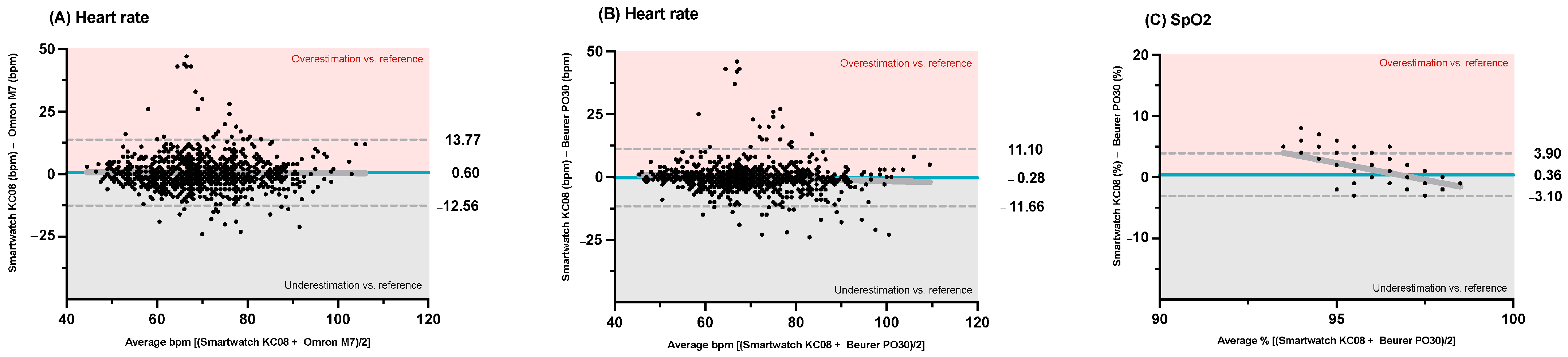
3.3. Secondary Outcomes: Heart Rate and SpO2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACC | American College of Cardiology |
| AHA | American Heart Association |
| BP | Blood pressure |
| bpm | Beats per minute |
| CI | Confidence interval |
| CV | Coefficient of variation |
| ESC | European Society of Cardiology |
| ISO | International Organization for Standardization |
| LoA | Limits of agreement |
| mmHg | Millimeters of mercury |
| SD | Standard deviation |
| SpO2 | Blood oxygen saturation |
| PPG | Photoplethysmography |
| PPT | Pulse transit time |
| PWV | Pulse wave velocity |
References
- Jose, A.P.; Awasthi, A.; Kondal, D.; Kapoor, M.; Roy, A.; Prabhakaran, D. Impact of repeated blood pressure measurement on blood pressure categorization in a population-based study from India. J. Hum. Hypertens. 2019, 33, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Boateng, E.B.; Ampofo, A.G. A glimpse into the future: Modelling global prevalence of hypertension. BMC Public Health 2023, 23, 1906. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar]
- Konstantinidis, D.; Iliakis, P.; Tatakis, F.; Thomopoulos, K.; Dimitriadis, K.; Tousoulis, D.; Tsioufis, K. Wearable blood pressure measurement devices and new approaches in hypertension management: The digital era. J. Hum. Hypertens. 2022, 36, 945–951. [Google Scholar] [CrossRef]
- Margolis, K.L.; Asche, S.E.; Bergdall, A.R.; Dehmer, S.P.; Groen, S.E.; Kadrmas, H.M.; Kerby, T.J.; Klotzle, K.J.; Maciosek, M.V.; Michels, R.D.; et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: A cluster randomized clinical trial. JAMA 2013, 310, 46–56. [Google Scholar] [CrossRef]
- McManus, R.J.; Little, P.; Stuart, B.; Morton, K.; Raftery, J.; Kelly, J.; Bradbury, K.; Zhang, J.; Zhu, S.; Murray, E.; et al. Home and Online Management and Evaluation of Blood Pressure (HOME BP) using a digital intervention in poorly controlled hypertension: Randomised controlled trial. BMJ 2021, 372, m4858. [Google Scholar] [CrossRef]
- Bradley, C.K.; Shimbo, D.; Colburn, D.A.; Pugliese, D.N.; Padwal, R.; Sia, S.K.; Anstey, D.E. Cuffless Blood Pressure Devices. Am. J. Hypertens. 2022, 35, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Piwek, L.; Ellis, D.A.; Andrews, S.; Joinson, A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016, 13, e1001953. [Google Scholar] [CrossRef]
- Falter, M.; Scherrenberg, M.; Driesen, K.; Pieters, Z.; Kaihara, T.; Xu, L.; Caiani, E.G.; Castiglioni, P.; Faini, A.; Parati, G.; et al. Smartwatch-Based Blood Pressure Measurement Demonstrates Insufficient Accuracy. Front. Cardiovasc. Med. 2022, 9, 958212. [Google Scholar] [CrossRef]
- Islam, S.M.S.; Chow, C.K.; Daryabeygikhotbehsara, R.; Subedi, N.; Rawstorn, J.; Tegegne, T.; Karmakar, C.; Siddiqui, M.U.; Lambert, G.; Maddison, R. Wearable cuffless blood pressure monitoring devices: A systematic review and meta-analysis. Eur. Heart J. Digit. Health 2022, 3, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.H.; Kang, M.K.; Choi, C.E.; Min, J.; Lee, H.Y.; Lim, S. Validation of a wearable cuff-less wristwatch-type blood pressure monitoring device. Sci. Rep. 2020, 10, 19015. [Google Scholar] [CrossRef]
- Man, P.K.; Cheung, K.L.; Sangsiri, N.; Shek, W.J.; Wong, K.L.; Chin, J.W.; Chan, T.T.; So, R.H. Blood Pressure Measurement: From Cuff-Based to Contactless Monitoring. Healthcare 2022, 10, 2113. [Google Scholar] [CrossRef] [PubMed]
- Stergiou, G.S.; Alpert, B.; Mieke, S.; Asmar, R.; Atkins, N.; Eckert, S.; Frick, G.; Friedman, B.; Grassl, T.; Ichikawa, T.; et al. A universal standard for the validation of blood pressure measuring devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. J. Hypertens. 2018, 36, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Hajj-Boutros, G.; Landry-Duval, M.A.; Comtois, A.S.; Gouspillou, G.; Karelis, A.D. Wrist-worn devices for the measurement of heart rate and energy expenditure: A validation study for the Apple Watch 6, Polar Vantage V and Fitbit Sense. Eur. J. Sport Sci. 2023, 23, 165–177. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- McEvoy, J.W.; McCarthy, C.P.; Bruno, R.M.; Brouwers, S.; Canavan, M.D.; Ceconi, C.; Christodorescu, R.M.; Daskalopoulou, S.S.; Ferro, C.J.; Gerdts, E.; et al. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur. Heart J. 2024, 45, 3912–4018. [Google Scholar]
- Stergiou, G.S.; Mukkamala, R.; Avolio, A.; Kyriakoulis, K.G.; Mieke, S.; Murray, A.; Parati, G.; Schutte, A.E.; Sharman, J.E.; Asmar, R.; et al. Cuffless blood pressure measuring devices: Review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J. Hypertens. 2022, 40, 1449–1460. [Google Scholar] [CrossRef]
- Hahnen, C.; Freeman, C.G.; Haldar, N.; Hamati, J.N.; Bard, D.M.; Murali, V.; Merli, G.J.; Joseph, J.I.; van Helmond, N. Accuracy of Vital Signs Measurements by a Smartwatch and a Portable Health Device: Validation Study. JMIR Mhealth Uhealth 2020, 8, e16811. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Zhou, Y.N.; Zhou, Y.; Wang, J.G. Validation of the watch-type HUAWEI WATCH D oscillometric wrist blood pressure monitor in adult Chinese. Blood Press. Monit. 2022, 27, 353–356. [Google Scholar] [CrossRef]
- Yi, L.; Lv, Z.H.; Hu, S.Y.; Liu, Y.Q.; Yan, J.B.; Zhang, H.; Li, H.B.; Chen, Q.; Li, Y.Y.; Jiang, Y.F.; et al. Validating the accuracy of a multifunctional smartwatch sphygmomanometer to monitor blood pressure. J. Geriatr. Cardiol. 2022, 19, 843–852. [Google Scholar]
- Kuwabara, M.; Harada, K.; Hishiki, Y.; Kario, K. Validation of two watch-type wearable blood pressure monitors according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J. Clin. Hypertens. 2019, 21, 853–858. [Google Scholar] [CrossRef]
- Montalvo, S.; Martinez, A.; Arias, S.; Lozano, A.; Gonzalez, M.P.; Dietze-Hermosa, M.S.; Boyea, B.L.; Dorgo, S. Commercial Smart Watches and Heart Rate Monitors: A Concurrent Validity Analysis. J. Strength Cond. Res. 2023, 37, 1802–1808. [Google Scholar] [CrossRef] [PubMed]
- Duking, P.; Giessing, L.; Frenkel, M.O.; Koehler, K.; Holmberg, H.C.; Sperlich, B. Wrist-Worn Wearables for Monitoring Heart Rate and Energy Expenditure While Sitting or Performing Light-to-Vigorous Physical Activity: Validation Study. JMIR Mhealth Uhealth 2020, 8, e16716. [Google Scholar] [CrossRef]
- Zeng, Z.; Li, L.; Hu, L.; Wang, K.; Li, L. Smartwatch measurement of blood oxygen saturation for predicting acute mountain sickness: Diagnostic accuracy and reliability. Digit. Health 2024, 10, 20552076241284910. [Google Scholar] [CrossRef] [PubMed]
- Lauterbach, C.J.; Romano, P.A.; Greisler, L.A.; Brindle, R.A.; Ford, K.R.; Kuennen, M.R. Accuracy and Reliability of Commercial Wrist-Worn Pulse Oximeter During Normobaric Hypoxia Exposure Under Resting Conditions. Res. Q. Exerc. Sport 2021, 92, 549–558. [Google Scholar] [CrossRef]
- Pipek, L.Z.; Nascimento, R.F.V.; Acencio, M.M.P.; Teixeira, L.R. Comparison of SpO(2) and heart rate values on Apple Watch and conventional commercial oximeters devices in patients with lung disease. Sci. Rep. 2021, 11, 18901. [Google Scholar] [CrossRef]

| Participants (n = 100) | |
|---|---|
| Gender—n (% women) | 62 (62%) |
| Caucasian—n (%) | 100 (100%) |
| Age—years | 40.94 ± 17.54 |
| Weight—kg | 69.46 ± 12.42 |
| Height—m | 1.68 ± 0.09 |
| BMI—kg/m2 | 24.12 ± 4.37 |
| Current smoking—n (%) | 17 (17%) |
| Current pharmacological treatment—n (%) | 37 (37%) |
| Outcome | Smartwatch KC08 | Omron M7 | Beurer PO30 | p-Value |
|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 112.33 ± 5.93 (103–140) | 108.79 ± 15.17 (71–153) | - | <0.001 |
| 111.00 [109.00–114.00] | 107.00 [98.25–116.00] | - | ||
| Diastolic blood pressure (mmHg) | 72.45 ± 3.08 (66–87) | 71.35 ± 9.70 (40–105) | - | 0.032 |
| 72.00 [71.00–73.00] | 71.00 [65.00–78.00] | - | ||
| Heart rate (bpm) | 69.89 ± 11.00 (46–112) | 69.28 ± 11.07 (43–103) | 70.16 ± 11.46 (43–112) | <0.001 |
| 69.00 [62.00–77.00] | 69.00 [62.00–76.00] | 69.00 [63.00–77.00] | ||
| Blood oxygen saturation (%) | 96.96 ± 0.84 (94–99) | - | 96.60 ± 1.60 (90–99) | <0.001 |
| 97.00 [96.00–98.00] | - | 97.00 [96.00–98.00] |
| Outcome | Smartwatch KC08 CV (%) | Omron M7 CV (%) | Beurer PO30 CV (%) | ICC (95% CI) | p-Value |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 1.63 | 4.07 | - | 0.054 (−0.071–0.164) | 0.192 |
| Diastolic blood pressure (mmHg) | 1.85 | 4.87 | - | −0.027 (−0.163–0.093) | 0.663 |
| Heart rate (bpm) | 6.26 | 4.65 | 4.95 | 0.947 (0.941–0.953) | <0.001 |
| Blood oxygen saturation (%) | 0.86 | - | 0.70 | 0.059 (−0.060–0.166) | 0.158 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Ortiz, S.; García-Chico, C.; Musso-Daury, L.; González-Ustio, S.; Peñín-Grandes, S.; Pinto-Fraga, J.; Maroto-Izquierdo, S.; Santos-Lozano, A. A Smartwatch or Just a Watch? A Validation Study of the Smartwatch KC08 for Measuring Blood Pressure. Sensors 2025, 25, 3793. https://doi.org/10.3390/s25123793
López-Ortiz S, García-Chico C, Musso-Daury L, González-Ustio S, Peñín-Grandes S, Pinto-Fraga J, Maroto-Izquierdo S, Santos-Lozano A. A Smartwatch or Just a Watch? A Validation Study of the Smartwatch KC08 for Measuring Blood Pressure. Sensors. 2025; 25(12):3793. https://doi.org/10.3390/s25123793
Chicago/Turabian StyleLópez-Ortiz, Susana, Celia García-Chico, Lisa Musso-Daury, Sara González-Ustio, Saúl Peñín-Grandes, José Pinto-Fraga, Sergio Maroto-Izquierdo, and Alejandro Santos-Lozano. 2025. "A Smartwatch or Just a Watch? A Validation Study of the Smartwatch KC08 for Measuring Blood Pressure" Sensors 25, no. 12: 3793. https://doi.org/10.3390/s25123793
APA StyleLópez-Ortiz, S., García-Chico, C., Musso-Daury, L., González-Ustio, S., Peñín-Grandes, S., Pinto-Fraga, J., Maroto-Izquierdo, S., & Santos-Lozano, A. (2025). A Smartwatch or Just a Watch? A Validation Study of the Smartwatch KC08 for Measuring Blood Pressure. Sensors, 25(12), 3793. https://doi.org/10.3390/s25123793










