Unicompartmental Knee Arthroplasty for Osteoarthritis Eliminates Lateral Thrust: Associations between Lateral Thrust Detected by Inertial Measurement Units and Clinical Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Gait Analysis
2.3. Radiographic Analysis and Clinical Outcome Assessment
2.4. Statistical Analysis
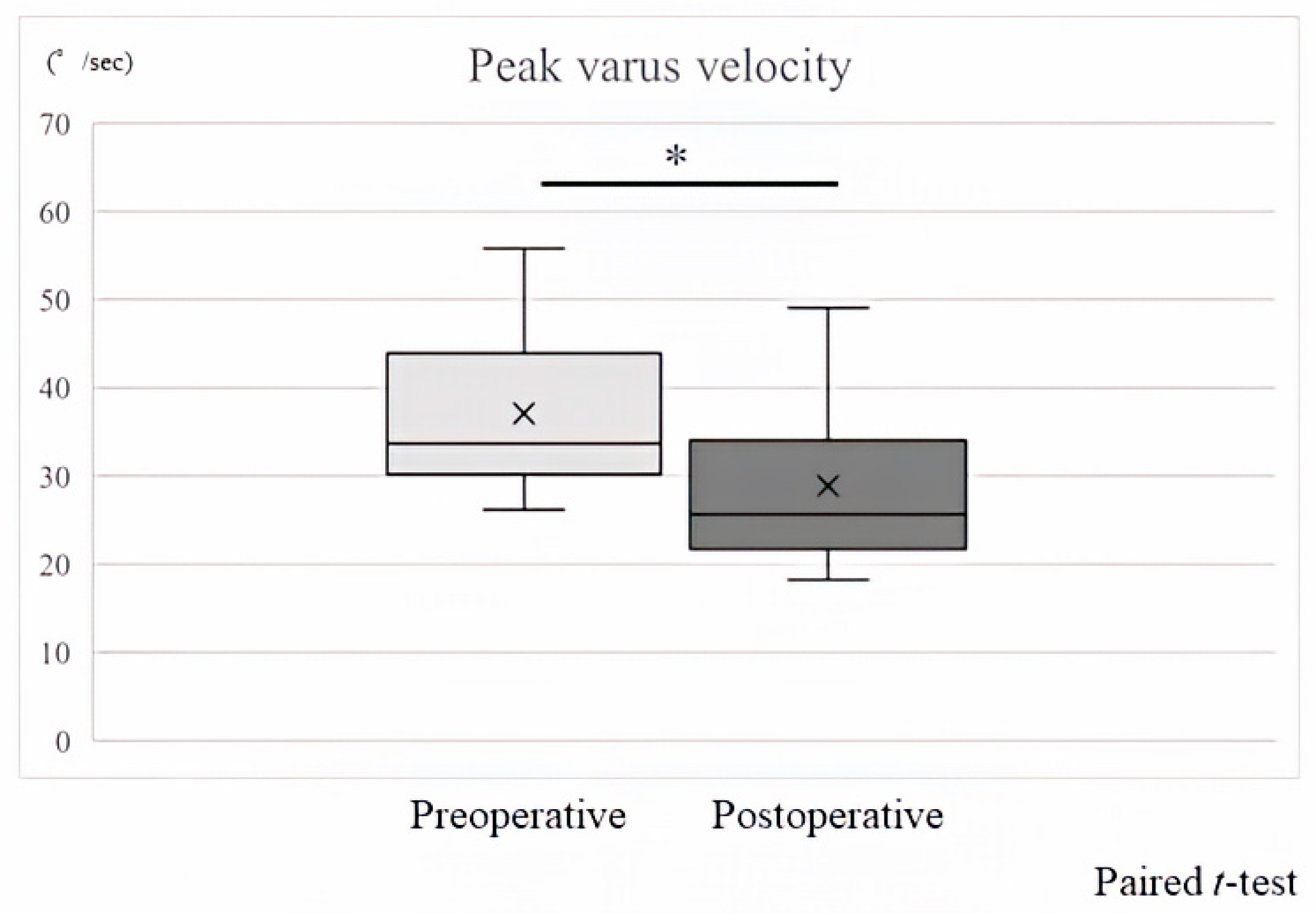
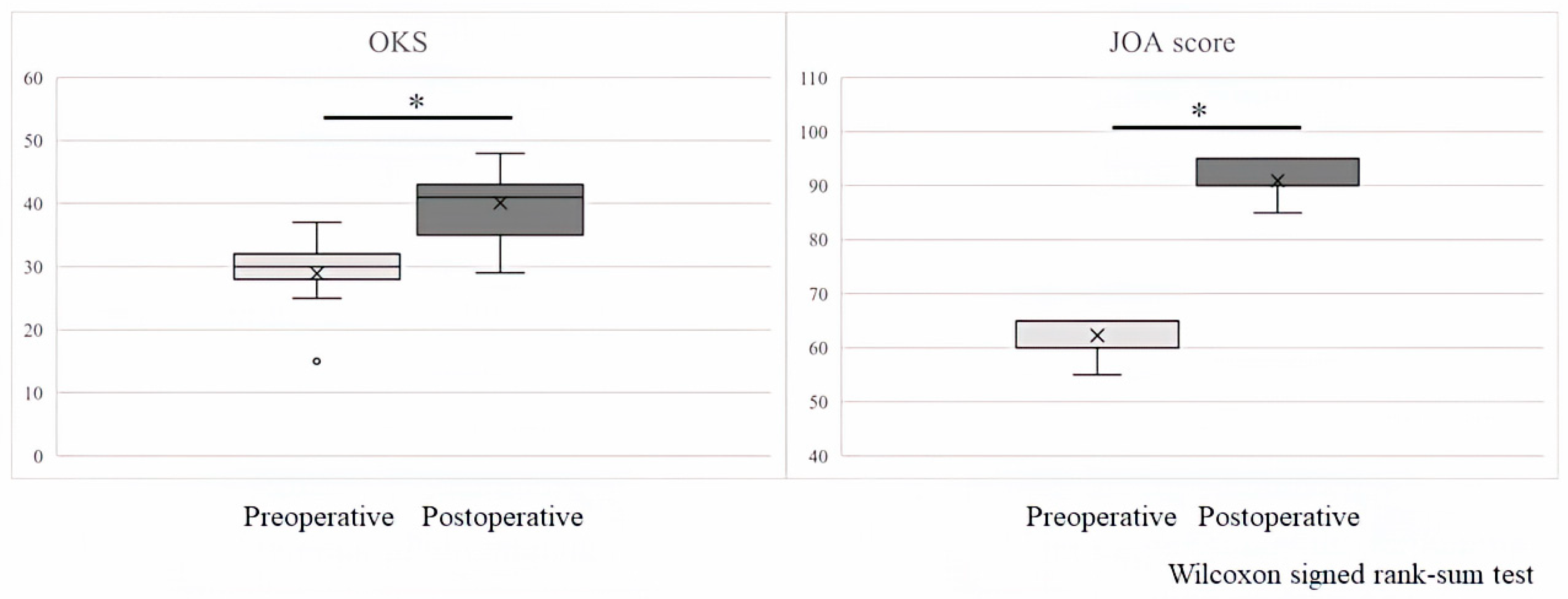
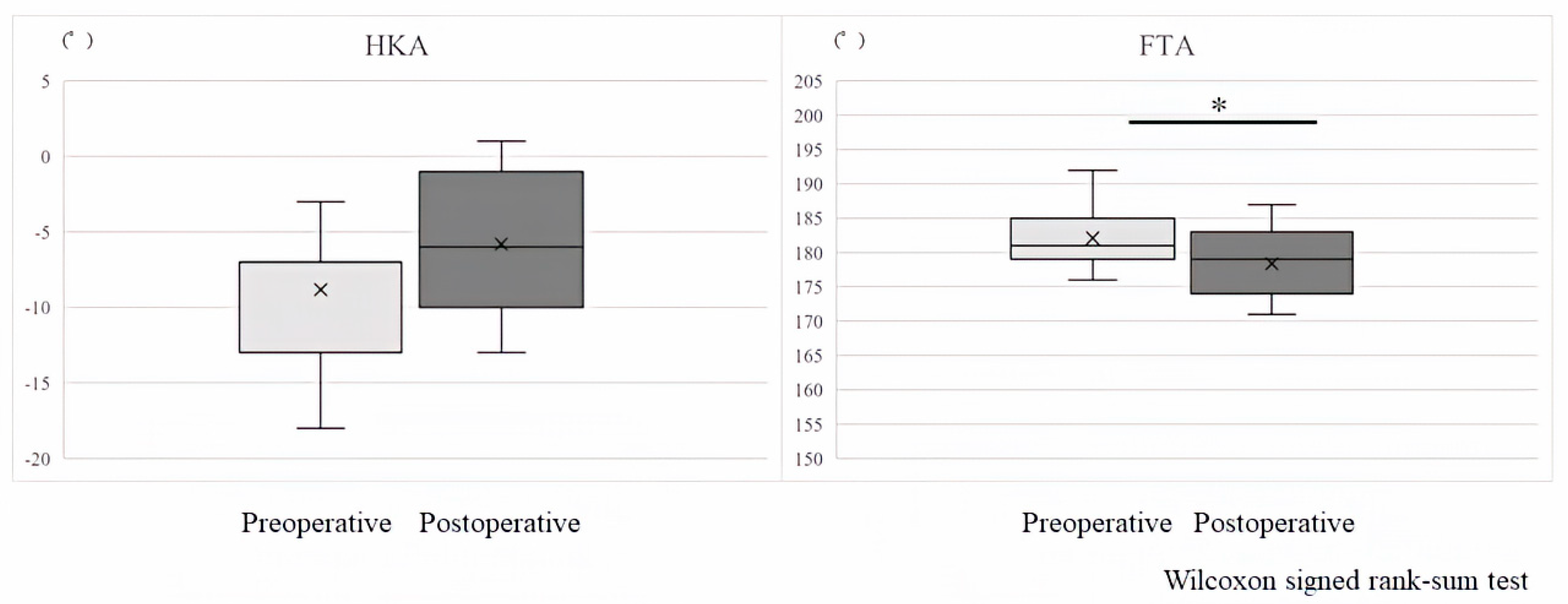
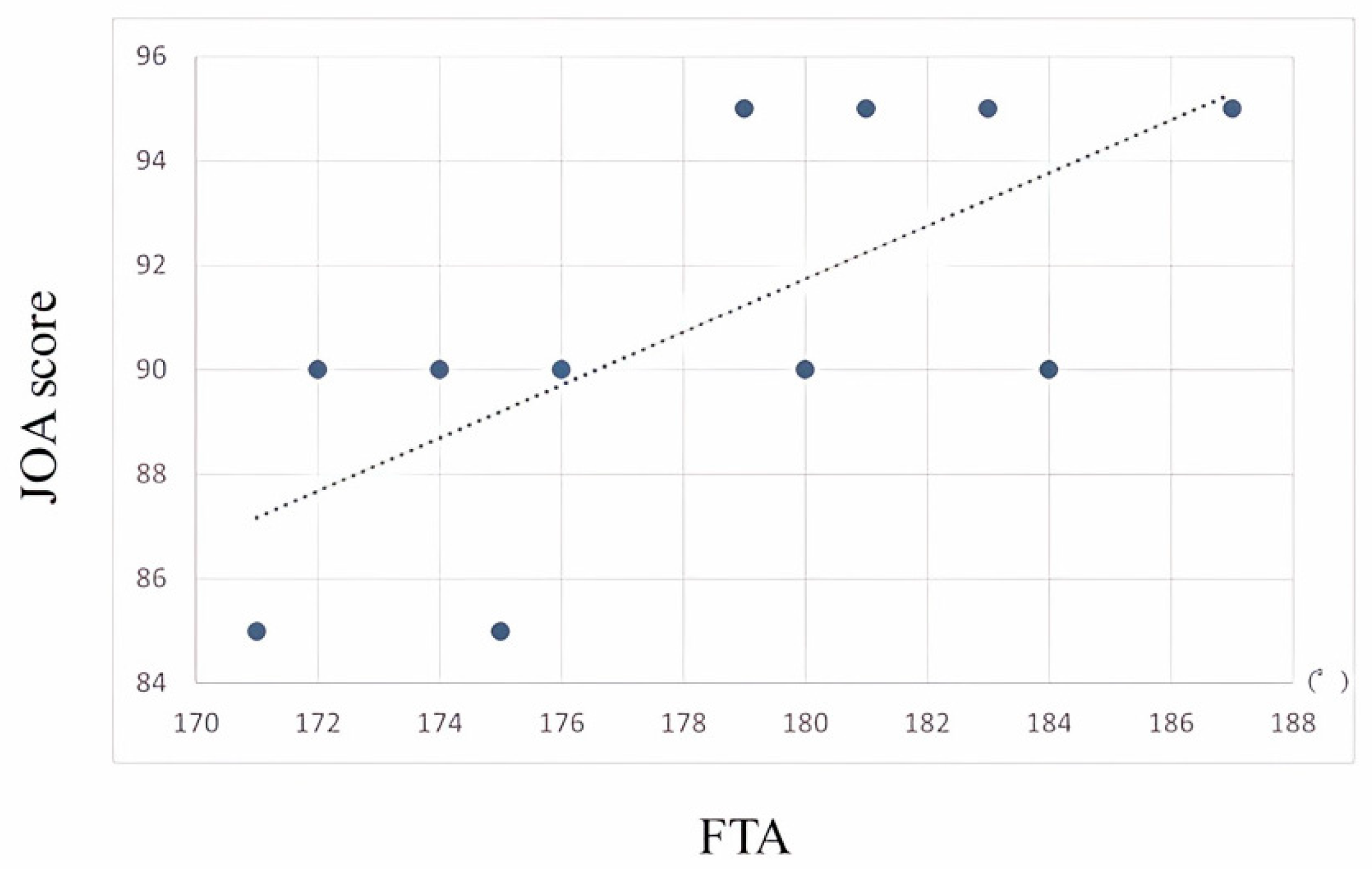
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Muraki, S.; Oka, H.; Akune, T.; Mabuchi, A.; En-yo, Y.; Yoshida, M.; Saika, A.; Suzuki, T.; Yoshida, H.; Ishibashi, H.; et al. Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: The ROAD study. Osteoarthr. Cartilage. 2009, 17, 1137–1143. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; Bierma-Zeinstra, S. Osteoarthritis. Lancet 2019, 393, 1745–1759. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, N.; Muraki, S.; Oka, H.; Kawaguchi, H.; Nakamura, K.; Akune, T. Cohort profile: Research on Osteoarthritis/osteoporosis Against Disability (ROAD) Study. Int. J. Epidemiol. 2010, 39, 988–995. [Google Scholar] [CrossRef]
- Di Martino, A.; Bordini, B.; Barile, F.; Ancarani, C.; Digennaro, V.; Faldini, C. Unicompartmental knee arthroplasty has higher revisions than total knee arthroplasty at long term follow-up: A registry study on 6453 prostheses. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3323–3329. [Google Scholar] [CrossRef] [PubMed]
- van der List, J.P.; Zuiderbaan, H.A.; Pearle, A.D. Why do medial unicompartmental knee arthroplasties fail today? J. Arthroplast. 2016, 31, 1016–1021. [Google Scholar] [CrossRef] [PubMed]
- Leiss, F.; Götz, J.S.; Maderbacher, G.; Zeman, F.; Meissner, W.; Grifka, J.; Benditz, A.; Greimel, F. Pain management of unicompartmental (UKA) vs. total knee arthroplasty (TKA) based on a matched pair analysis of 4144 cases. Sci. Rep. 2020, 10, 17660. [Google Scholar] [CrossRef] [PubMed]
- Hopper, G.P.; Leach, W.J. Participation in sporting activities following knee replacement: Total versus unicompartmental. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 973–979. [Google Scholar] [CrossRef]
- Burn, E.; Sanchez-Santos, M.T.; Pandit, H.G.; Hamilton, T.W.; Liddle, A.D.; Murray, D.W.; Pinedo-Villanueva, R. Ten-year patient-reported outcomes following total and minimally invasive unicompartmental knee arthroplasty: A propensity score-matched cohort analysis. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1455–1464. [Google Scholar] [CrossRef]
- Emerson, R.H., Jr.; Hansborough, T.; Reitman, R.D.; Rosenfeldt, W.; Higgins, L.L. Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin. Orthop. 2002, 404, 62–70. [Google Scholar] [CrossRef]
- Xu, D.; Zhou, H.; Quan, W.; Jiang, X.; Liang, M.; Li, S.; Ugbolue, U.C.; Baker, J.S.; Gusztav, F.; Ma, X.; et al. A new method proposed for realizing human gait pattern recognition: Inspirations for the application of sports and clinical gait analysis. Gait Posture 2024, 107, 293–305. [Google Scholar] [CrossRef]
- Xu, D.; Quan, W.; Zhou, H.; Sun, D.; Baker, J.S.; Gu, Y. Explaining the differences of gait patterns between high and low-mileage runners with machine learning. Sci. Rep. 2022, 12, 2981. [Google Scholar] [CrossRef] [PubMed]
- Hreljac, A.; Marshall, R.N.; Hume, P.A. Evaluation of lower extremity overuse injury potential in runners. Med. Sci. Sports Exerc. 2000, 32, 1635–1641. [Google Scholar] [CrossRef] [PubMed]
- Andriacchi, T.P.; Mündermann, A.; Smith, R.L.; Alexander, E.J.; Dyrby, C.O.; Koo, S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann. Biomed. Eng. 2004, 32, 447–457. [Google Scholar] [CrossRef] [PubMed]
- Lo, G.H.; Harvey, W.F.; McAlindon, T.E. Associations of varus thrust and alignment with pain in knee osteoarthritis. Arthritis Rheum. 2012, 64, 2252–2259. [Google Scholar] [CrossRef] [PubMed]
- Tsukamoto, H.; Saito, K.; Matsunaga, T.; Iwami, T.; Saito, H.; Kijima, H.; Akagawa, M.; Komatsu, A.; Miyakoshi, N.; Shimada, Y. Diagnostic accuracy of the mobile assessment of varus thrust using nine-axis inertial measurement units. Prog. Rehabil. Med. 2021, 6, 20210009. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, Y.; Komatsu, A.; Iwami, T.; Tsukamoto, H.; Shimada, Y. Comparison of MARG sensor results for different mounting positions and physiques for accurate knee joint motion measurement. In Proceedings of the 2019 4th Asia-Pacific Conference on Intelligent Robot Systems (ACIRS), Nagoya, Japan, 13–15 July 2019. [Google Scholar]
- Koshino, T.; Morii, T.; Wada, J.; Saito, H.; Ozawa, N.; Noyori, K. High tibial osteotomy with fixation by a blade plate for medial compartment osteoarthritis of the knee. Orthop. Clin. N. Am. 1989, 20, 227–243. [Google Scholar]
- Brouwer, G.M.; van Tol, A.W.; Bergink, A.P.; Belo, J.N.; Bernsen, R.M.; Reijman, M.; Pols, H.A.; Bierma-Zeinstra, S.M. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007, 56, 1204–1211. [Google Scholar] [CrossRef] [PubMed]
- Cooke, T.D.; Scudamore, R.A.; Bryant, J.T.; Sorbie, C.; Siu, D.; Fisher, B. A quantitative approach to radiography of the lower limb. Principles and applications. J. Bone Jt. Surg. Br. 1991, 73, 715–720. [Google Scholar] [CrossRef]
- Choudhury, A.K.; Bansal, S.; Pranav, J.; Raja, B.S.; Gupta, T.; Paul, S.; Gupta, K.; Kalia, R.B. Increased medial talar tilt may incite ankle pain and predispose ankle osteoarthritis after correction of severity of knee varus deformity among patients undergoing bilateral total knee arthroplasty: A prospective observation. Knee Surg. Relat. Res. 2024, 36, 7. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Sharma, L.; Chang, A.H.; Jackson, R.D.; Nevitt, M.; Moisio, K.C.; Hochberg, M.; Eaton, C.; Kwoh, C.K.; Almagor, O.; Cauley, J.; et al. Varus thrust and incident and progressive knee osteoarthritis. Arthritis Rhematol. 2017, 69, 2136–2143. [Google Scholar] [CrossRef]
- Fukutani, N.; Iijima, H.; Fukumoto, T.; Uritani, D.; Kaneda, E.; Ota, K.; Aoyama, T.; Tsuboyama, T.; Matsuda, S. Association of varus thrust with pain and stiffness and activities of daily living in patients with medial knee osteoarthritis. Phys. Ther. 2016, 96, 165–175. [Google Scholar] [CrossRef]
- Chang, A.H.; Chmiel, J.S.; Moisio, K.C.; Almagor, O.; Zhang, Y.; Cahue, S.; Sharma, L. Varus thrust and knee frontal plane dynamic motion in persons with knee osteoarthritis. Osteoarthr. Cartil. 2013, 21, 1668–1673. [Google Scholar] [CrossRef]
- Tsukamoto, H.; Saito, K.; Saito, H.; Kijima, H.; Akagawa, M.; Komatsu, A.; Iwami, T.; Miyakoshi, N. A Novel Classification of Coronal Plane Knee Joint Instability Using Nine-Axis Inertial Measurement Units in Patients with Medial Knee Osteoarthritis. Sensors 2023, 23, 2797. [Google Scholar] [CrossRef]

| Patient No. | Age (Years) | Sex | Gait Speed (m/s) Preoperative/Postoperative | Height (cm) | Body Weight (kg) Preoperative/Postoperative |
|---|---|---|---|---|---|
| 1 | 75 | Female | 0.76/0.77 | 146.0 | 65.5/71.0 |
| 2 | 70 | Female | 1.09/1.14 | 154.8 | 56.1/54.0 |
| 3 | 80 | Male | 0.70/0.73 | 159.2 | 58.7/57.4 |
| 4 | 75 | Female | 0.80/1.23 | 154.0 | 50.8/51.0 |
| 5 | 82 | Male | 0.68/0.86 | 161.7 | 61.9/62.5 |
| 6 | 64 | Male | 0.94/1.11 | 158.1 | 79.3/81.1 |
| 7 | 74 | Male | 0.68/0.80 | 171.3 | 63.5/64.0 |
| 8 | 75 | Female | 0.77/1.03 | 155.4 | 65.3/60.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sato, H.; Kijima, H.; Iwami, T.; Tsukamoto, H.; Saito, H.; Kudo, D.; Kimura, R.; Kasukawa, Y.; Miyakoshi, N. Unicompartmental Knee Arthroplasty for Osteoarthritis Eliminates Lateral Thrust: Associations between Lateral Thrust Detected by Inertial Measurement Units and Clinical Outcomes. Sensors 2024, 24, 2019. https://doi.org/10.3390/s24072019
Sato H, Kijima H, Iwami T, Tsukamoto H, Saito H, Kudo D, Kimura R, Kasukawa Y, Miyakoshi N. Unicompartmental Knee Arthroplasty for Osteoarthritis Eliminates Lateral Thrust: Associations between Lateral Thrust Detected by Inertial Measurement Units and Clinical Outcomes. Sensors. 2024; 24(7):2019. https://doi.org/10.3390/s24072019
Chicago/Turabian StyleSato, Hikaru, Hiroaki Kijima, Takehiro Iwami, Hiroaki Tsukamoto, Hidetomo Saito, Daisuke Kudo, Ryota Kimura, Yuji Kasukawa, and Naohisa Miyakoshi. 2024. "Unicompartmental Knee Arthroplasty for Osteoarthritis Eliminates Lateral Thrust: Associations between Lateral Thrust Detected by Inertial Measurement Units and Clinical Outcomes" Sensors 24, no. 7: 2019. https://doi.org/10.3390/s24072019
APA StyleSato, H., Kijima, H., Iwami, T., Tsukamoto, H., Saito, H., Kudo, D., Kimura, R., Kasukawa, Y., & Miyakoshi, N. (2024). Unicompartmental Knee Arthroplasty for Osteoarthritis Eliminates Lateral Thrust: Associations between Lateral Thrust Detected by Inertial Measurement Units and Clinical Outcomes. Sensors, 24(7), 2019. https://doi.org/10.3390/s24072019





