Experimental In Vitro Microfluidic Calorimetric Chip Data towards the Early Detection of Infection on Implant Surfaces
Abstract
1. Introduction
2. Materials and Methods
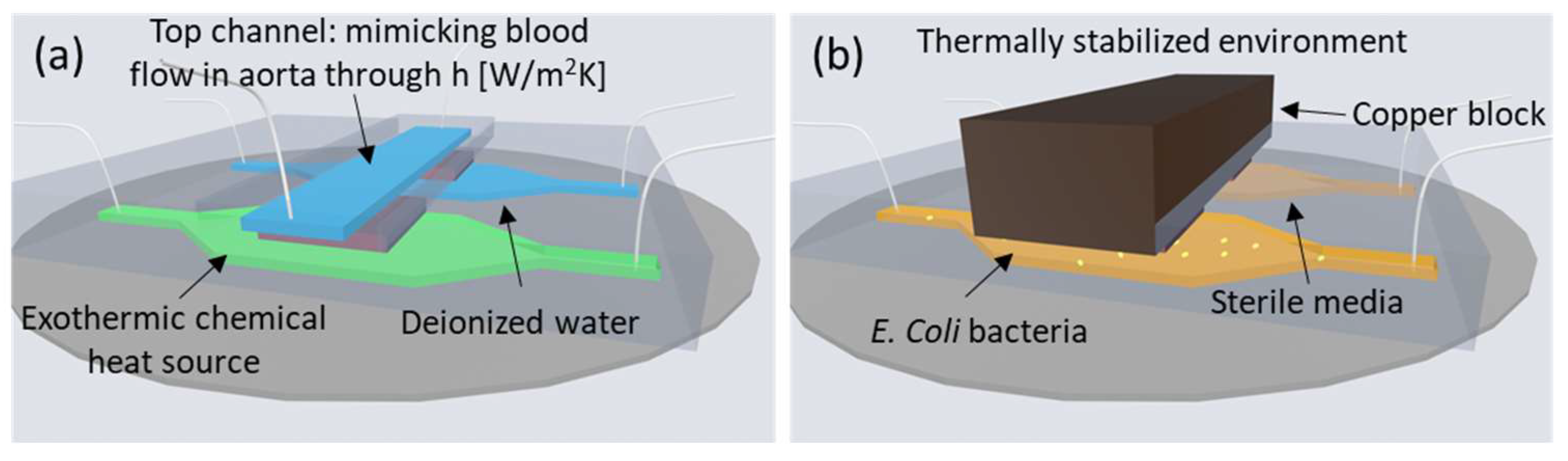
2.1. Experimental System and Setup
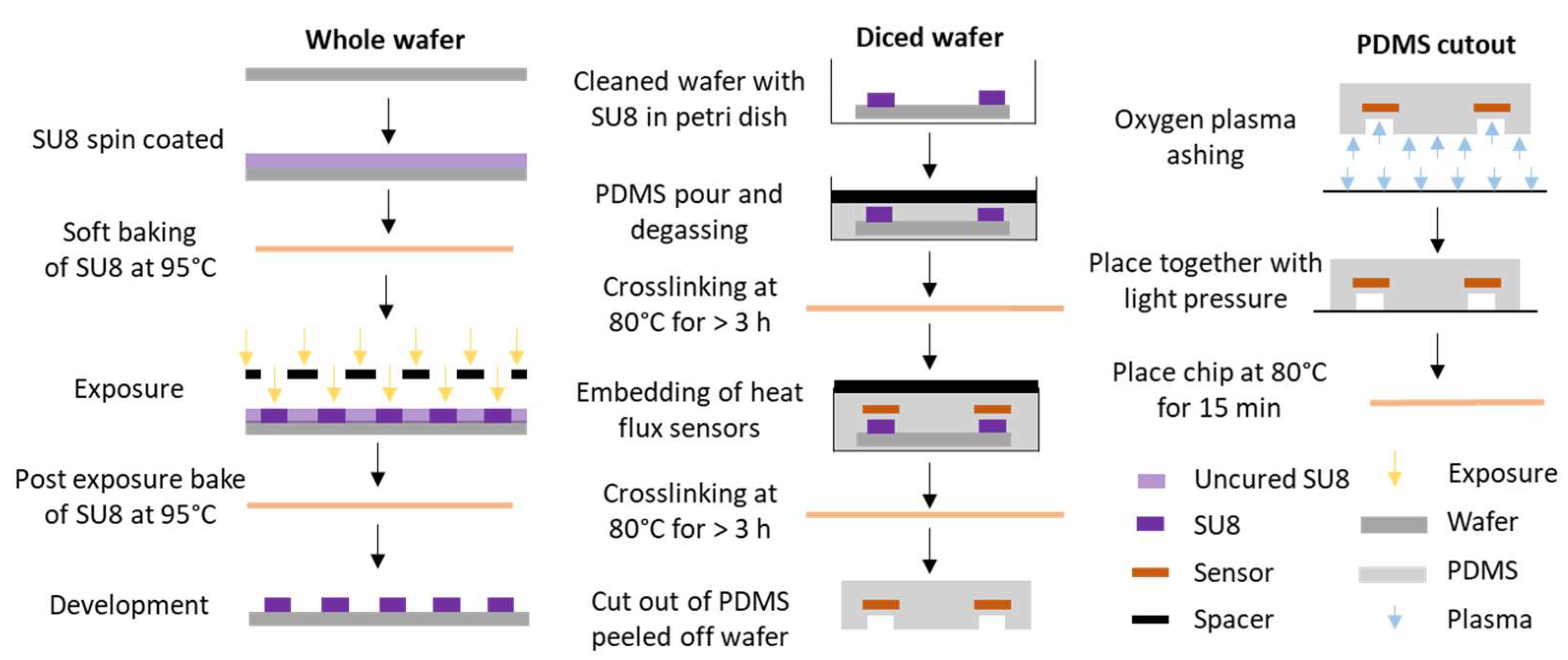
2.2. Microfluidic Chip Fabrication Steps
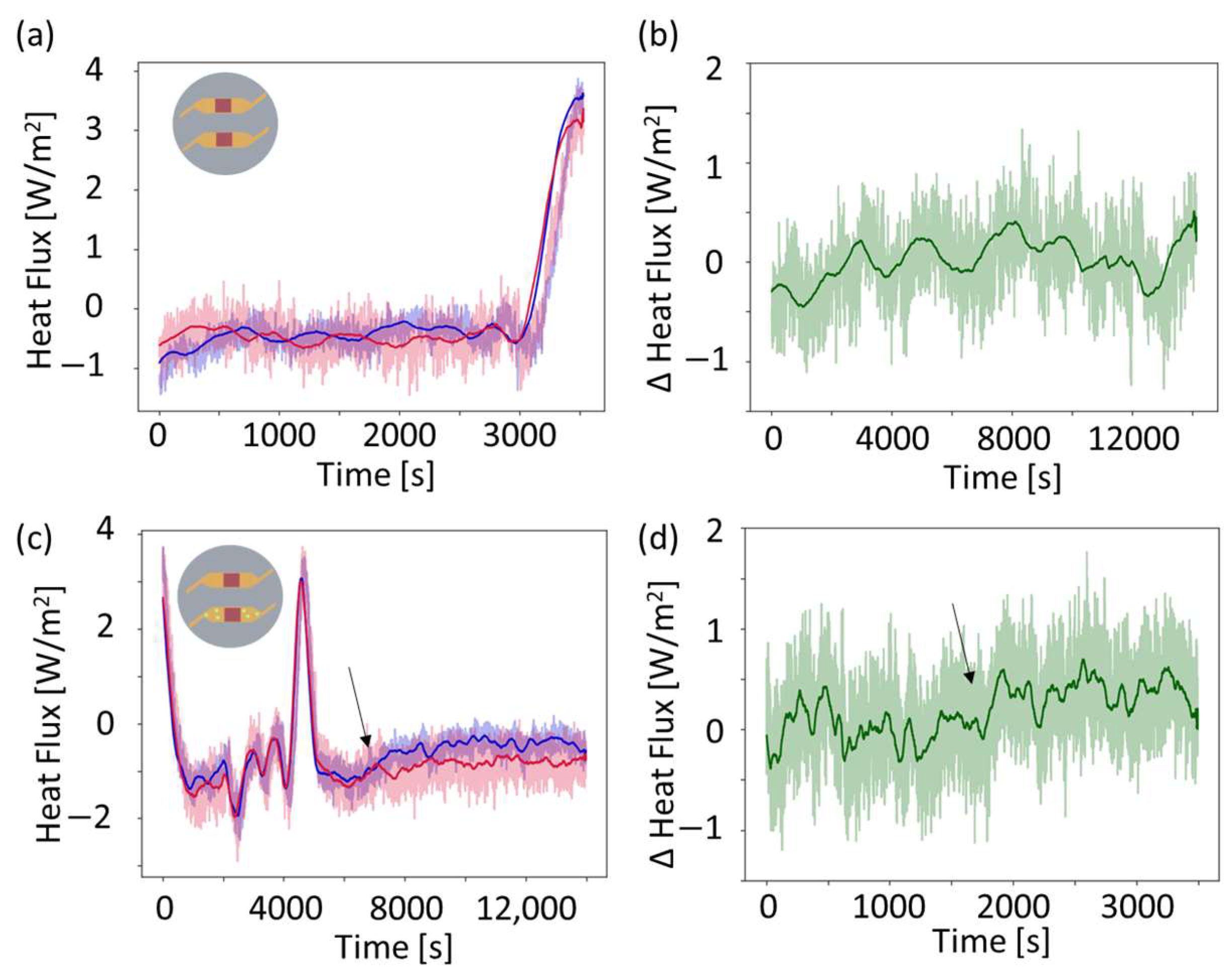
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vehusheia, S.L.K.; Roman, C.; Braissant, O.; Arnoldini, M.; Hierold, C. Enabling direct microcalorimetric measurement of metabolic activity and exothermic reactions onto microfluidic platforms via heat flux sensor integration. Microsystems Nanoeng. 2023, 9, 56. [Google Scholar] [CrossRef]
- Al-Hallak, M.H.D.K.; Sarfraz, M.K.; Azarmi, S.; Kohan, M.H.G.; Roa, W.H.; Löbenberg, R. Microcalorimetric method to assess phagocytosis: Macrophage-nanoparticle interactions. AAPS J. 2011, 13, 1. [Google Scholar] [CrossRef]
- Hansen, L.D.; Macfarlane, C.; McKinnon, N.; Smith, B.N.; Criddle, R.S. Use of calorespirometric ratios, heat per CO2 and heat per O2, to quantify metabolic paths and energetics of growing cells. Thermochim. Acta 2004, 422, 55–61. [Google Scholar] [CrossRef]
- Trampuz, A.; Salzmann, S.; Antheaume, J.; Daniels, A.U. Microcalorimetry: A novel method for detection of microbial contamination in platelet products. Transfusion 2007, 47, 1643–1650. [Google Scholar] [CrossRef]
- Braissant, O.; Wirz, D.; Göpfert, B.; Daniels, A.U. Use of isothermal microcalorimetry to monitor microbial activities. BMC Microbiol. 2010, 13, 171. [Google Scholar] [CrossRef]
- Butini, M.E.; Abbandonato, G.; Di Rienzo, C.; Trampuz, A.; Di Luca, M. Isothermal microcalorimetry detects the presence of persister cells in a Staphylococcus aureus biofilm after vancomycin treatment. Front. Microbiol. 2019, 10, 332. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, H.; Feng, J.; Neuzil, P. Recent advances of microcalorimetry for studying cellular metabolic heat. TrAC Trends Anal. Chem. 2021, 143, 115353. [Google Scholar] [CrossRef]
- Maskow, T.; Lerchner, J.; Peitzsch, M.; Harms, H.; Wolf, G. Chip calorimetry for the monitoring of whole cell biotransformation. J. Biotechnol. 2006, 122, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Sha, X.; Yu, S.; Zhao, Y. Nanocalorimeters for biomolecular analysis and cell metabolism monitoring. Biomicrofluidics 2020, 14, 011503. [Google Scholar] [CrossRef]
- Xu, J.; Reiserer, R.; Tellinghuisen, J.; Wikswo, J.P.; Baudenbacher, F.J. A microfabricated nanocalorimeter: Design, characterization, and chemical calibration. Anal. Chem. 2008, 80, 2728–2733. [Google Scholar] [CrossRef]
- Johannessen, E.A.; Weaver, J.M.R.; Cobbold, P.H.; Cooper, J.M. Heat conduction nanocalorimeter for pl-scale single cell measurements. Appl. Phys. Lett. 2002, 80, 2029–2031. [Google Scholar] [CrossRef]
- Bae, J.; Zheng, J.; Zhang, H.; Foster, P.J.; Needleman, D.J.; Vlassak, J.J. A micromachined picocalorimeter sensor for liquid samples with application to chemical reactions and biochemistry. Adv. Sci. 2021, 8, 1–11. [Google Scholar] [CrossRef]
- Yang, Y.; Chen, Y.; Tang, H.; Zong, N.; Jiang, X. Microfluidics for Biomedical Analysis. Small Methods 2020, 4, 1900451. [Google Scholar] [CrossRef]
- Soleimany, A.P.; Bhatia, S.N. Activity-Based Diagnostics: An Emerging Paradigm for Disease Detection and Monitoring. Trends Mol. Med. 2020, 26, 450–468. [Google Scholar] [CrossRef] [PubMed]
- Zelenin, S.; Hansson, J.; Ardabili, S.; Ramachandraiah, H.; Brismar, H.; Russom, A. Microfluidic-based isolation of bacteria from whole blood for sepsis diagnostics. Biotechnol. Lett. 2015, 37, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Jang, K.-J.; Mehr, A.P.; Hamilton, G.A.; McPartlin, L.A.; Chung, S.; Suh, K.-Y.; Ingber, D.E. Human kidney proximal tubule-on-a-chip for drug transport and nephrotoxicity assessment. Integr. Biol. 2013, 5, 1119–1129. [Google Scholar] [CrossRef] [PubMed]
- Postek, W.; Garstecki, P. Droplet Microfluidics for High-Throughput Analysis of Antibiotic Susceptibility in Bacterial Cells and Populations. Acc. Chem. Res. 2021, 55, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Shirure, V.S.; Bi, Y.; Curtis, M.B.; Lezia, A.; Goedegebuure, M.M.; Goedegebuure, S.P.; Aft, R.; Fields, R.C.; George, S.C. Tumor-on-a-chip platform to investigate progression and drug sensitivity in cell lines and patient-derived organoids. Lab Chip 2018, 18, 3687–3702. [Google Scholar] [CrossRef] [PubMed]
- Vehusheia, S.L.K.; Roman, C.; Cesarovic, N.; Hierold, C. Microfluidic thermal model for early detection of infection on aortic grafts. In Proceedings of the Technical Digest of 22nd International Conference on Solid State Sensors, Actuators and Microsystems (Transducers), Kyoto, Japan, 25–29 June 2023; pp. 951–954. [Google Scholar]
- Vehusheia, S.L.K.; Roman, C.; Sonderegger, R.; Cesarovic, N.; Hierold, C. Finite element-based feasibility study on utilizing heat flux sensors for early detection of vascular graft infections. Sci. Rep. 2023, 13, 16198. [Google Scholar] [CrossRef]
- Nagpal, V.; Sohail, M.R. Prosthetic Vascular Graft Infections: A Contemporary Approach to Diagnosis and Management. Curr. Infect. Dis. Rep. 2011, 13, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, J.S.; Ward, R.E.; Lacroix, J.; Hébert, P.C.; Barnes, M.A.; Bohn, D.J.; Dirks, P.B.; Doucette, S.; Fergusson, D.; Gottesman, R.; et al. Hypothermia Therapy after Traumatic Brain Injury in Children. N. Engl. J. Med. 2008, 358, 2447–2456. [Google Scholar] [CrossRef] [PubMed]
- Higuera-Guisset, J.; Rodríguez-Viejo, J.; Chacón, M.; Muñoz, F.; Vigués, N.; Mas, J. Calorimetry of microbial growth using a thermopile based microreactor. Thermochim. Acta 2005, 427, 187–191. [Google Scholar] [CrossRef]
- Arens, S.; Kraft, C.; Schlegel, U.; Printzen, G.; Perren, S.M.; Hansis, M. Susceptibility to local infection in biological internal fixation. Arch. Orthop. Trauma Surg. 1999, 119, 82–85. [Google Scholar] [CrossRef]
- Harrasser, N.; Gorkotte, J.; Obermeier, A.; Feihl, S.; Straub, M.; Slotta-Huspenina, J.; von Eisenhart-Rothe, R.; Moser, W.; Gruner, P.; de Wild, M.; et al. A new model of implant-related osteomyelitis in the metaphysis of rat tibiae. BMC Musculoskelet. Disord. 2016, 17, 152. [Google Scholar] [CrossRef]
- Monzon, M.; García-Álvare, F.; Lacleriga, A.; Gracia, E.; Leiva, J.; Oteiza, C.; Amorena, B. A simple infection model using pre-colonized implants to reproduce rat chronic Staphylococcus aureus osteomyelitis and study antibiotic treatment. J. Orthop. Res. 2001, 19, 820–826. [Google Scholar] [CrossRef] [PubMed]
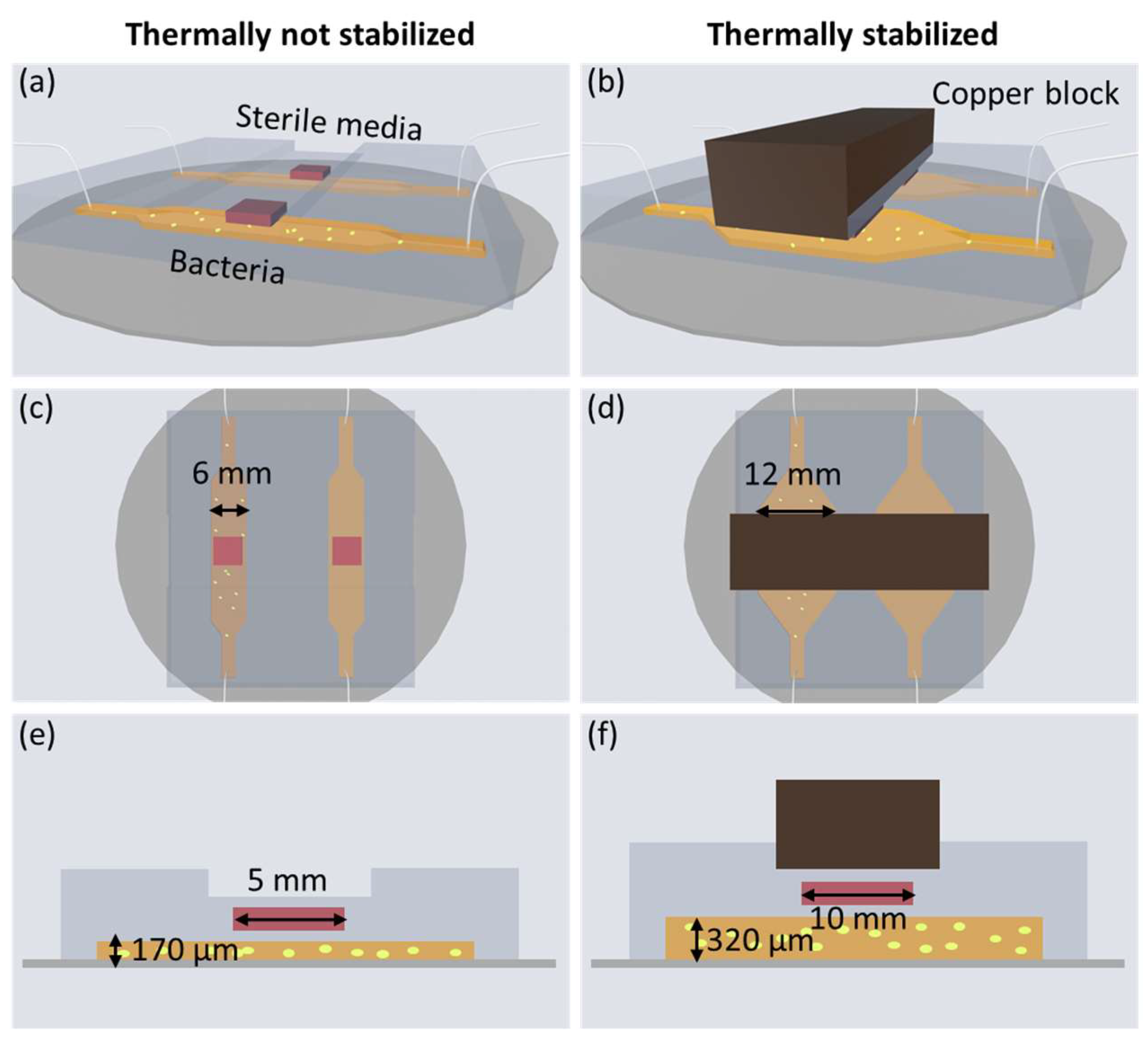



| Property | Thermally Not-Stabilized | Thermally Stabilized [1] |
|---|---|---|
| Growth detection | Yes | Yes |
| Channel size (underneath sensor) | 6 mm × 6 mm × 170 μm | 12 mm × 12 mm × 320 μm |
| Channel volume | 6 μL | 46 μL |
| Sensor | gSKIN XM | gSKIN XP |
| Sensor resolution | 0.41 W/m2 | 0.06 W/m2 |
| Temperature fluctuation | 1 K | 0.3 K |
| Standard deviation heat flux | 0.32 W/m2 | 0.05 W/m2 |
| Standard deviation averaged heat flux | 0.20 W/m2 | 0.02 W/m2 |
| OD limit of detection * | 3 × 108 cells/mL | 2 × 107 cells/mL |
| Cell population limit of detection * | 1.8 × 106 cells | 9.2 × 105 cells |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vehusheia, S.L.K.; Roman, C.I.; Arnoldini, M.; Hierold, C. Experimental In Vitro Microfluidic Calorimetric Chip Data towards the Early Detection of Infection on Implant Surfaces. Sensors 2024, 24, 1019. https://doi.org/10.3390/s24031019
Vehusheia SLK, Roman CI, Arnoldini M, Hierold C. Experimental In Vitro Microfluidic Calorimetric Chip Data towards the Early Detection of Infection on Implant Surfaces. Sensors. 2024; 24(3):1019. https://doi.org/10.3390/s24031019
Chicago/Turabian StyleVehusheia, Signe L. K., Cosmin I. Roman, Markus Arnoldini, and Christofer Hierold. 2024. "Experimental In Vitro Microfluidic Calorimetric Chip Data towards the Early Detection of Infection on Implant Surfaces" Sensors 24, no. 3: 1019. https://doi.org/10.3390/s24031019
APA StyleVehusheia, S. L. K., Roman, C. I., Arnoldini, M., & Hierold, C. (2024). Experimental In Vitro Microfluidic Calorimetric Chip Data towards the Early Detection of Infection on Implant Surfaces. Sensors, 24(3), 1019. https://doi.org/10.3390/s24031019







