Implications of Aperiodic and Periodic EEG Components in Classification of Major Depressive Disorder from Source and Electrode Perspectives
Abstract
1. Introduction
- Novel Investigation: This study is the first to investigate the impact of excluding the aperiodic component of resting-state EEG in different brain regions and in both electrode- and source-level EEGs for individuals with MDD vs. HC.
- Improved Classification: By utilizing periodic and aperiodic components separately, we aim to enhance the accuracy of distinguishing between MDD and HC individuals.
- Exploratory Analysis: We calculate the correlation between EEG features and the BDI and its subscales, providing additional insights into the neural correlates of depression.
2. Materials and Methods
2.1. Participants
2.2. EEG Data Recording and Processing
2.3. Statistical Analysis
- Combination by frequency band: we paired features from the same frequency band to form the feature sets.
- Combination by analysis type: we paired features from the same analysis type to form the feature sets.
- Dual-component combination: we combined features from different components of our analysis (periodic + aperiodic) to form the feature sets.
3. Results
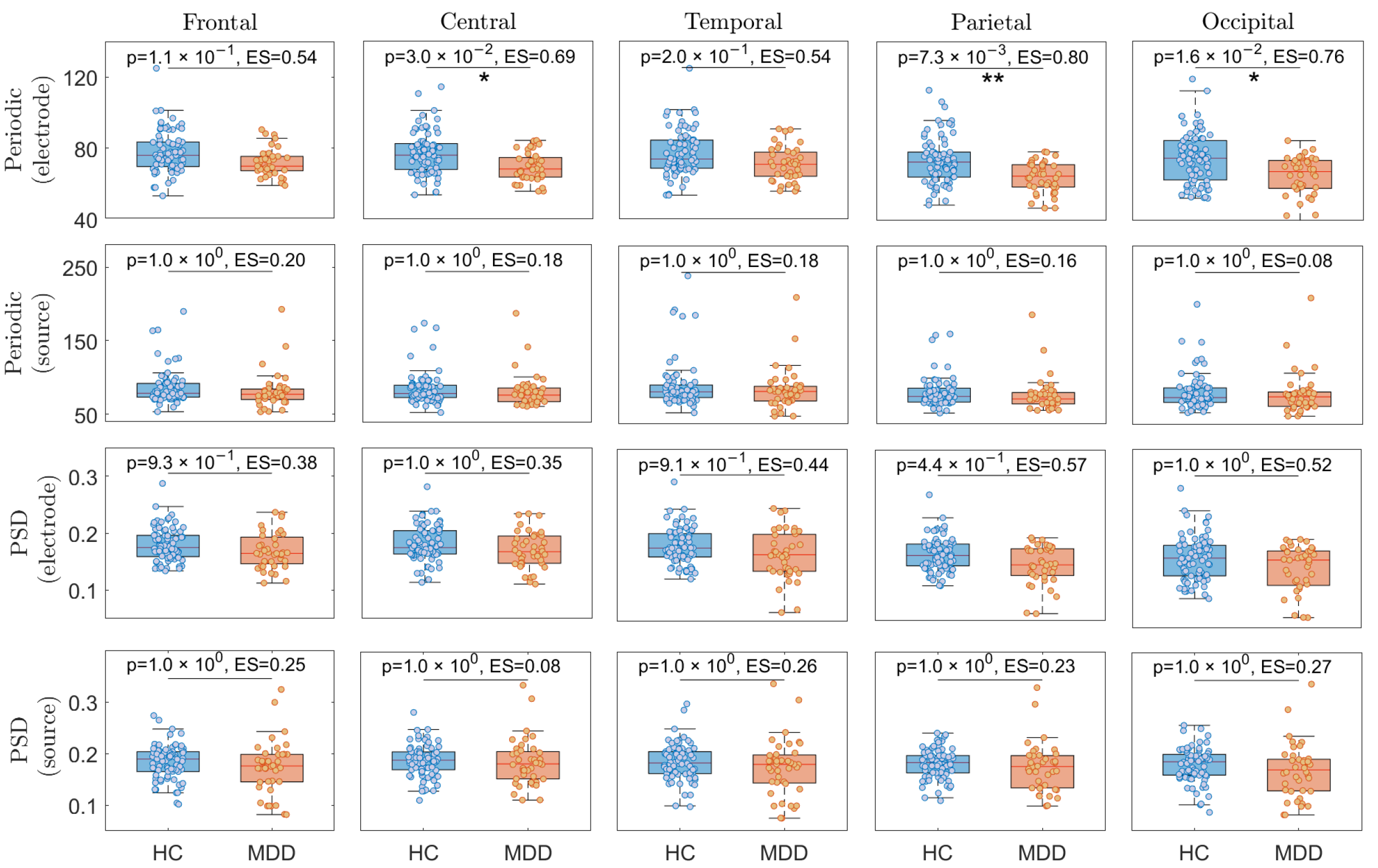
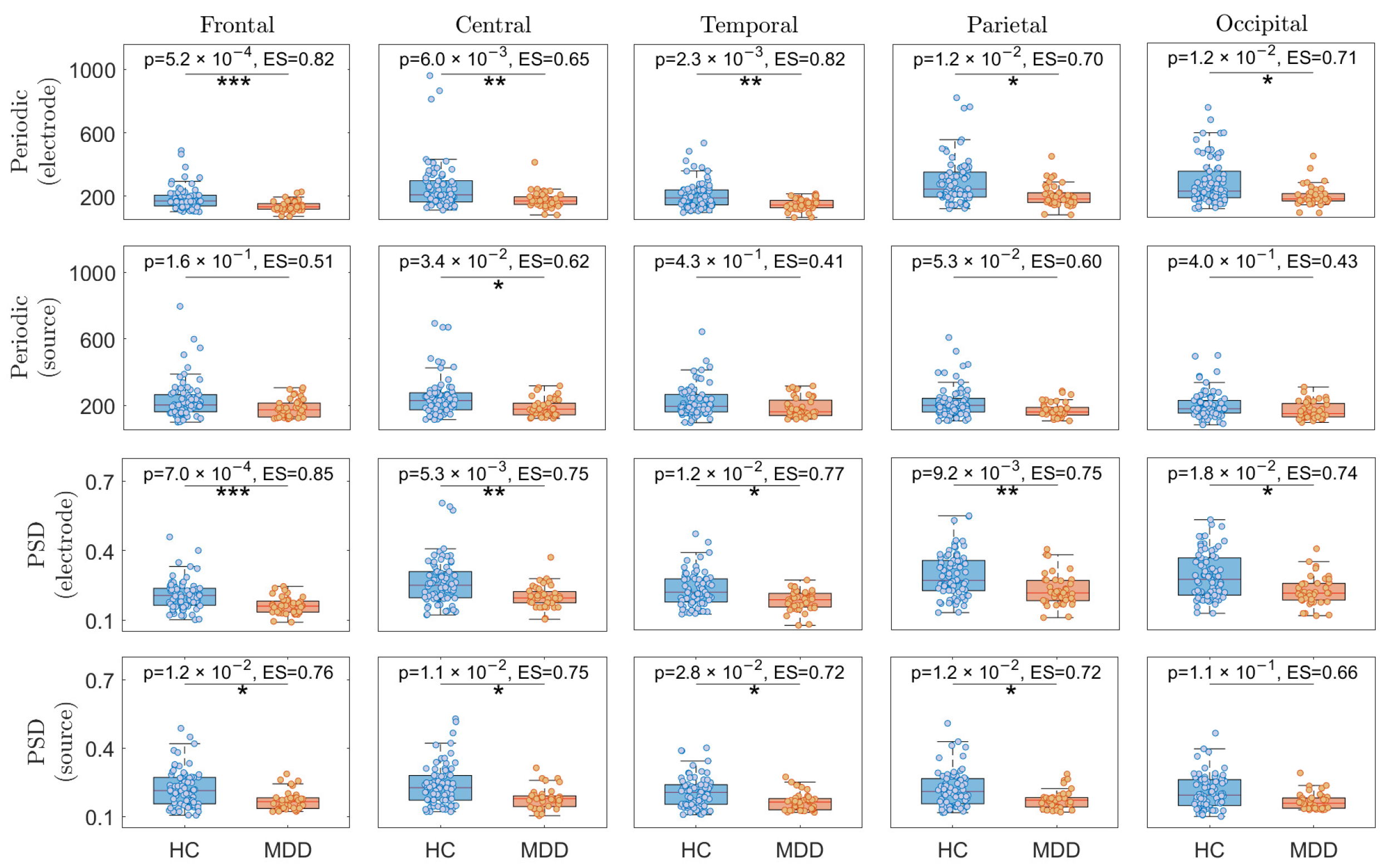
3.1. EEG Power Comparisons in Different Brain Regions
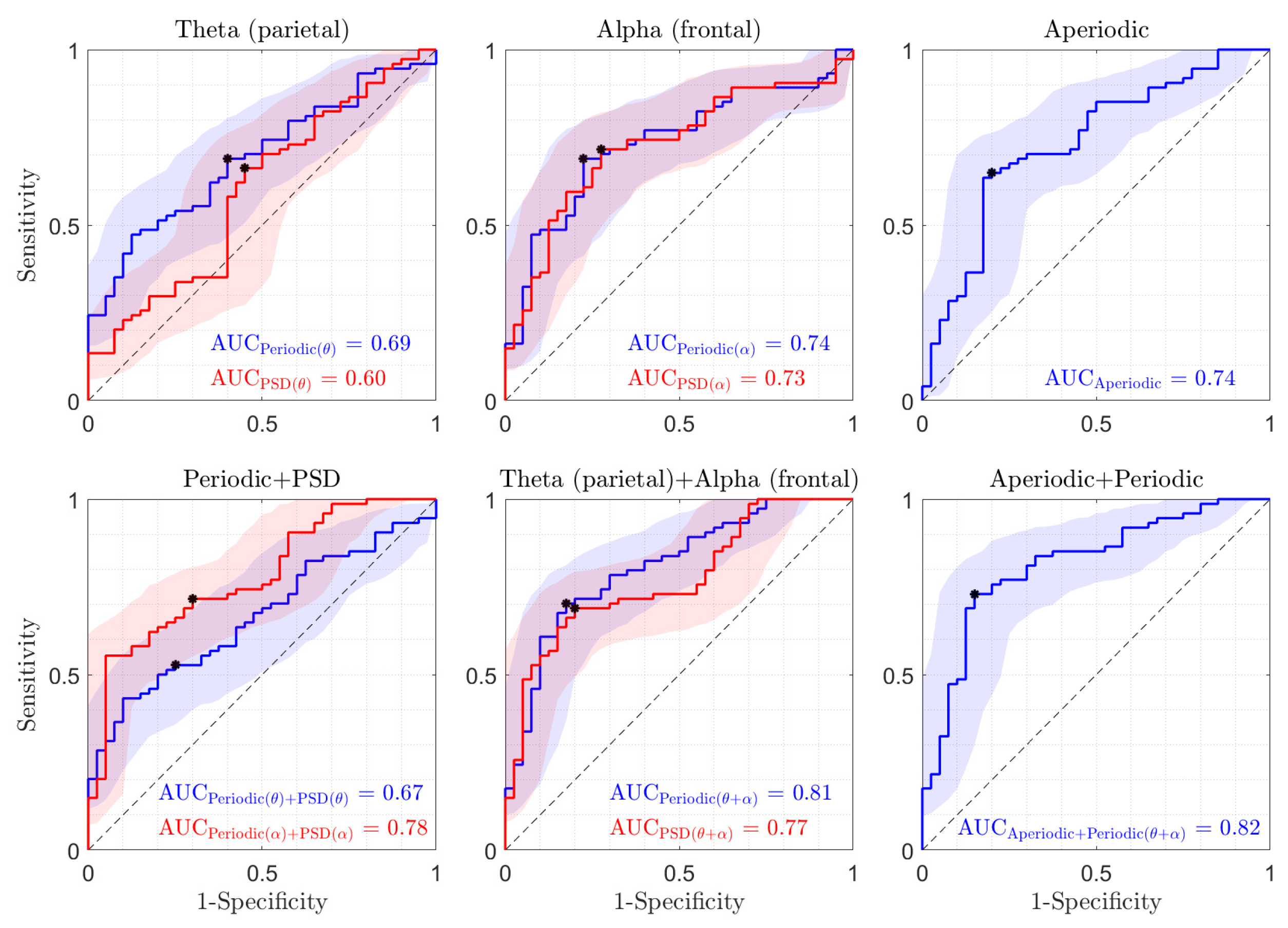
3.2. Classification
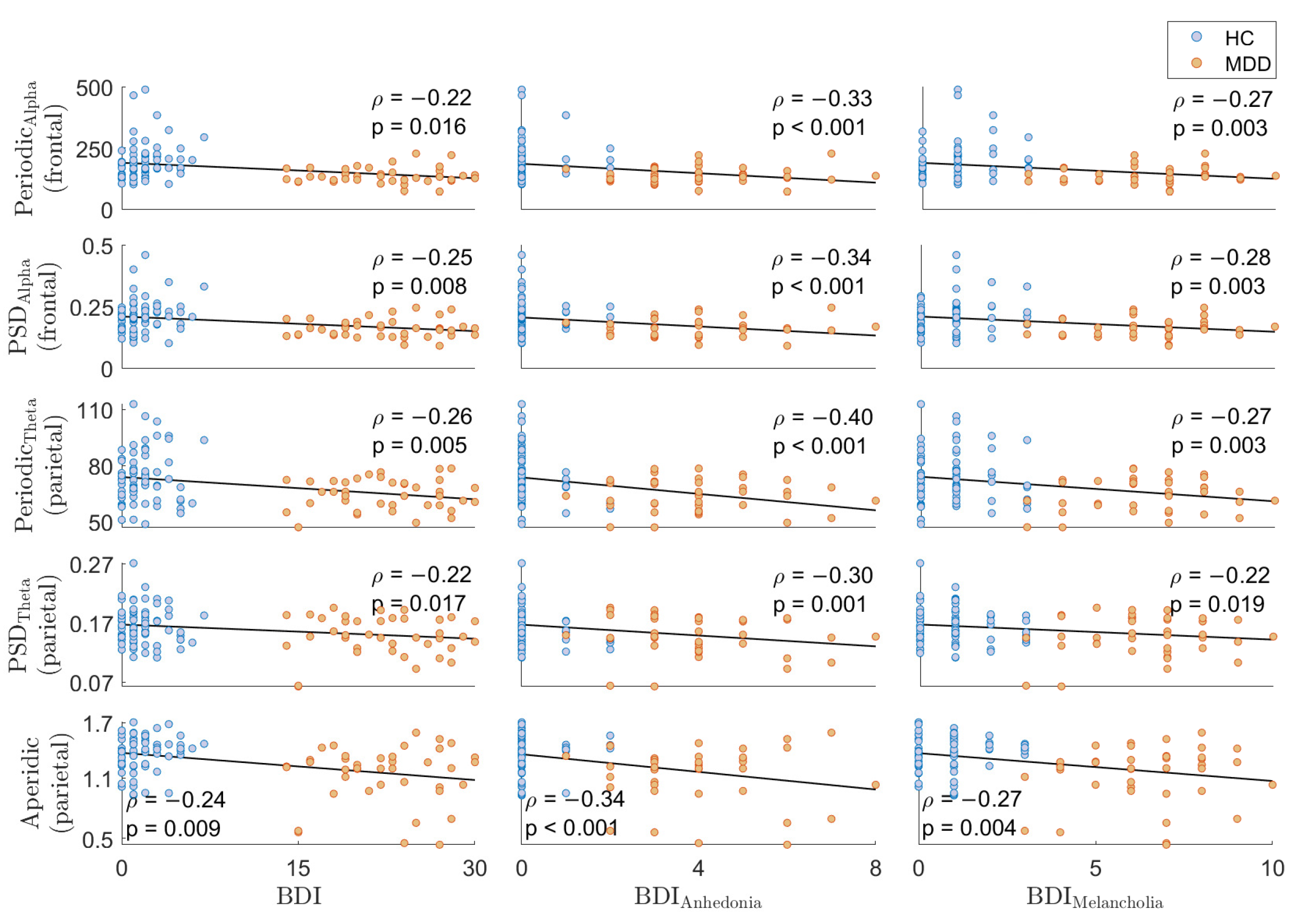
3.3. Correlation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACC | Anterior cingulate cortex |
| ANOVA | One-way analysis of variance |
| AUC | Area Under the Curve |
| BDI | Beck Depression Inventory |
| BDNF | Brain-derived neurotrophic factor |
| DUI | Duration of untreated illness |
| EEG | Electroencephalography |
| eLORETA | exact Low-Resolution Electric Tomography |
| ES | Effect size |
| GABA | Gamma-aminobutyric acid |
| HAPPE | Harvard Automated Preprocessing Pipeline |
| HC | Healthy control |
| LOSO | Leave-One-Subject-Out |
| MARA | Multiple Artifact Rejection Algorithm |
| MEG | Magnetoencephalography |
| MDD | Major depressive disorder |
| MNE | Minimum norm estimation |
| PSD | Power spectral density |
| ROIs | Regions of Interest |
| sLORETA | standardized Low-Resolution Electric Tomography |
| SSRIs | Selective Serotonin Reuptake Inhibitors |
| TAI | Trait Anxiety Inventory |
| W-ICA | Wavelet-enhanced independent component analysis |
References
- Otte, C.; Gold, S.M.; Penninx, B.W.; Pariante, C.M.; Etkin, A.; Fava, M.; Mohr, D.C.; Schatzberg, A.F. Major depressive disorder. Nat. Rev. Dis. Prim. 2016, 2, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Marx, W.; Penninx, B.W.; Solmi, M.; Furukawa, T.A.; Firth, J.; Carvalho, A.F.; Berk, M. Major depressive disorder. Nat. Rev. Dis. Prim. 2023, 9, 44. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; Technical Report; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- de Aguiar Neto, F.S.; Rosa, J.L.G. Depression biomarkers using non-invasive EEG: A review. Neurosci. Biobehav. Rev. 2019, 105, 83–93. [Google Scholar] [CrossRef]
- Mumtaz, W.; Malik, A.S.; Yasin, M.A.M.; Xia, L. Review on EEG and ERP predictive biomarkers for major depressive disorder. Biomed. Signal Process. Control 2015, 22, 85–98. [Google Scholar] [CrossRef]
- Yun, S.; Jeong, B. Aberrant EEG signal variability at a specific temporal scale in major depressive disorder. Clin. Neurophysiol. 2021, 132, 1866–1877. [Google Scholar] [CrossRef]
- Malik, A.S.; Mumtaz, W. EEG-Based Experiment Design for Major Depressive Disorder: Machine Learning and Psychiatric Diagnosis; Academic Press: Cambridge, MA, USA, 2019. [Google Scholar]
- Sanei, S.; Chambers, J.A. EEG Signal Processing and Machine Learning; John Wiley & Sons: Hoboken, NJ, USA, 2021. [Google Scholar]
- Simmatis, L.; Russo, E.E.; Geraci, J.; Harmsen, I.E.; Samuel, N. Technical and clinical considerations for electroencephalography-based biomarkers for major depressive disorder. Npj Ment. Health Res. 2023, 2, 18. [Google Scholar] [CrossRef]
- Fernández-Palleiro, P.; Rivera-Baltanás, T.; Rodrigues-Amorim, D.; Fernández-Gil, S.; del Carmen Vallejo-Curto, M.; Álvarez-Ariza, M.; López, M.; Rodriguez-Jamardo, C.; Luis Benavente, J.; de Las Heras, E.; et al. Brainwaves oscillations as a potential biomarker for major depression disorder risk. Clin. EEG Neurosci. 2020, 51, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Paré, D. Role of the basolateral amygdala in memory consolidation. Prog. Neurobiol. 2003, 70, 409–420. [Google Scholar] [CrossRef]
- Pare, D.; Collins, D.R. Neuronal correlates of fear in the lateral amygdala: Multiple extracellular recordings in conscious cats. J. Neurosci. 2000, 20, 2701–2710. [Google Scholar] [CrossRef]
- Knyazev, G.G. Motivation, emotion, and their inhibitory control mirrored in brain oscillations. Neurosci. Biobehav. Rev. 2007, 31, 377–395. [Google Scholar] [CrossRef]
- Joormann, J.; Gotlib, I.H. Emotion regulation in depression: Relation to cognitive inhibition. Cogn. Emot. 2010, 24, 281–298. [Google Scholar] [CrossRef] [PubMed]
- Aftanas, L.I.; Golocheikine, S.A. Human anterior and frontal midline theta and lower alpha reflect emotionally positive state and internalized attention: High-resolution EEG investigation of meditation. Neurosci. Lett. 2001, 310, 57–60. [Google Scholar] [CrossRef]
- Aftanas, L.I.; Varlamov, A.A.; Pavlov, S.V.; Makhnev, V.P.; Reva, N.V. Time-dependent cortical asymmetries induced by emotional arousal: EEG analysis of event-related synchronization and desynchronization in individually defined frequency bands. Int. J. Psychophysiol. 2002, 44, 67–82. [Google Scholar] [CrossRef] [PubMed]
- Başar, E. A review of alpha activity in integrative brain function: Fundamental physiology, sensory coding, cognition and pathology. Int. J. Psychophysiol. 2012, 86, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Voineskos, D.; Blumberger, D.M.; Zomorrodi, R.; Rogasch, N.C.; Farzan, F.; Foussias, G.; Rajji, T.K.; Daskalakis, Z.J. Altered transcranial magnetic stimulation–electroencephalographic markers of inhibition and excitation in the dorsolateral prefrontal cortex in major depressive disorder. Biol. Psychiatry 2019, 85, 477–486. [Google Scholar] [CrossRef]
- Luscher, B.; Shen, Q.; Sahir, N. The GABAergic deficit hypothesis of major depressive disorder. Mol. Psychiatry 2011, 16, 383–406. [Google Scholar] [CrossRef]
- Kito, S.; Hasegawa, T.; Takamiya, A.; Noda, T.; Nakagome, K.; Higuchi, T.; Koga, Y. Transcranial magnetic stimulation modulates resting EEG functional connectivity between the left dorsolateral prefrontal cortex and limbic regions in medicated patients with treatment-resistant depression. J. Neuropsychiatry Clin. Neurosci. 2017, 29, 155–159. [Google Scholar] [CrossRef]
- Nuss, P. Anxiety disorders and GABA neurotransmission: A disturbance of modulation. Neuropsychiatr. Dis. Treat. 2015, 11, 165–175. [Google Scholar]
- Lozano-Soldevilla, D. On the physiological modulation and potential mechanisms underlying parieto-occipital alpha oscillations. Front. Comput. Neurosci. 2018, 12, 23. [Google Scholar] [CrossRef]
- Hosseinifard, B.; Moradi, M.H.; Rostami, R. Classifying depression patients and normal subjects using machine learning techniques and nonlinear features from EEG signal. Comput. Methods Programs Biomed. 2013, 109, 339–345. [Google Scholar] [CrossRef]
- Mohammadi, M.; Al-Azab, F.; Raahemi, B.; Richards, G.; Jaworska, N.; Smith, D.; De La Salle, S.; Blier, P.; Knott, V. Data mining EEG signals in depression for their diagnostic value. BMC Med. Inform. Decis. Mak. 2015, 15, 108. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.F.; Kan, D.P.X.; Croarkin, P.; Phang, C.K.; Doruk, D. Neurophysiological correlates of depressive symptoms in young adults: A quantitative EEG study. J. Clin. Neurosci. 2018, 47, 315–322. [Google Scholar] [CrossRef]
- Dolsen, E.A.; Cheng, P.; Arnedt, J.T.; Swanson, L.; Casement, M.D.; Kim, H.S.; Goldschmied, J.R.; Hoffmann, R.F.; Armitage, R.; Deldin, P.J. Neurophysiological correlates of suicidal ideation in major depressive disorder: Hyperarousal during sleep. J. Affect. Disord. 2017, 212, 160–166. [Google Scholar] [CrossRef]
- Jaworska, N.; Blier, P.; Fusee, W.; Knott, V. Alpha power, alpha asymmetry and anterior cingulate cortex activity in depressed males and females. J. Psychiatr. Res. 2012, 46, 1483–1491. [Google Scholar] [CrossRef] [PubMed]
- Kemp, A.; Griffiths, K.; Felmingham, K.; Shankman, S.A.; Drinkenburg, W.; Arns, M.; Clark, C.R.; Bryant, R. Disorder specificity despite comorbidity: Resting EEG alpha asymmetry in major depressive disorder and post-traumatic stress disorder. Biol. Psychol. 2010, 85, 350–354. [Google Scholar] [CrossRef]
- Grin-Yatsenko, V.A.; Baas, I.; Ponomarev, V.A.; Kropotov, J.D. EEG power spectra at early stages of depressive disorders. J. Clin. Neurophysiol. 2009, 26, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Grin-Yatsenko, V.A.; Baas, I.; Ponomarev, V.A.; Kropotov, J.D. Independent component approach to the analysis of EEG recordings at early stages of depressive disorders. Clin. Neurophysiol. 2010, 121, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Kan, D.P.X.; Lee, P.F. Decrease alpha waves in depression: An electroencephalogram (EEG) study. In Proceedings of the 2015 International Conference on BioSignal Analysis, Processing and Systems (ICBAPS), Kuala Lumpur, Malaysia, 26–28 May 2015; IEEE: New York, NY, USA, 2015; pp. 156–161. [Google Scholar]
- Knott, V.J.; Telner, J.I.; Lapierre, Y.D.; Browne, M.; Horn, E.R. Quantitative EEG in the prediction of antidepressant response to imipramine. J. Affect. Disord. 1996, 39, 175–184. [Google Scholar] [CrossRef]
- Leuchter, A.F.; Cook, I.A.; Marangell, L.B.; Gilmer, W.S.; Burgoyne, K.S.; Howland, R.H.; Trivedi, M.H.; Zisook, S.; Jain, R.; McCracken, J.T.; et al. Comparative effectiveness of biomarkers and clinical indicators for predicting outcomes of SSRI treatment in major depressive disorder: Results of the BRITE-MD study. Psychiatry Res. 2009, 169, 124–131. [Google Scholar] [CrossRef]
- Knott, V.; Mahoney, C.; Kennedy, S.; Evans, K. Pre-treatment EEG and it’s relationship to depression severity and paroxetine treatment outcome. Pharmacopsychiatry 2000, 33, 201–205. [Google Scholar] [CrossRef]
- Donoghue, T.; Haller, M.; Peterson, E.J.; Varma, P.; Sebastian, P.; Gao, R.; Noto, T.; Lara, A.H.; Wallis, J.D.; Knight, R.T.; et al. Parameterizing neural power spectra into periodic and aperiodic components. Nat. Neurosci. 2020, 23, 1655–1665. [Google Scholar] [CrossRef] [PubMed]
- Gerster, M.; Waterstraat, G.; Litvak, V.; Lehnertz, K.; Schnitzler, A.; Florin, E.; Curio, G.; Nikulin, V. Separating neural oscillations from aperiodic 1/f activity: Challenges and recommendations. Neuroinformatics 2022, 20, 991–1012. [Google Scholar] [CrossRef] [PubMed]
- Merkin, A.; Sghirripa, S.; Graetz, L.; Smith, A.E.; Hordacre, B.; Harris, R.; Pitcher, J.; Semmler, J.; Rogasch, N.C.; Goldsworthy, M. Do age-related differences in aperiodic neural activity explain differences in resting EEG alpha? Neurobiol. Aging 2023, 121, 78–87. [Google Scholar] [CrossRef]
- Voytek, B.; Kayser, A.S.; Badre, D.; Fegen, D.; Chang, E.F.; Crone, N.E.; Parvizi, J.; Knight, R.T.; D’esposito, M. Oscillatory dynamics coordinating human frontal networks in support of goal maintenance. Nat. Neurosci. 2015, 18, 1318–1324. [Google Scholar] [CrossRef] [PubMed]
- Buzsaki, G.; Draguhn, A. Neuronal oscillations in cortical networks. Science 2004, 304, 1926–1929. [Google Scholar] [CrossRef]
- Cohen, M.X. Analyzing Neural Time Series Data: Theory and Practice; MIT Press: Cambridge, MA, USA, 2014. [Google Scholar]
- Cavanagh, J.F.; Napolitano, A.; Wu, C.; Mueen, A. The patient repository for EEG data+ computational tools (PRED+ CT). Front. Neuroinform. 2017, 11, 67. [Google Scholar] [CrossRef]
- Cavanagh, J.F.; Bismark, A.W.; Frank, M.J.; Allen, J.J. Multiple dissociations between comorbid depression and anxiety on reward and punishment processing: Evidence from computationally informed EEG. Comput. Psychiatry 2019, 3, 1. [Google Scholar] [CrossRef]
- Gabard-Durnam, L.J.; Mendez Leal, A.S.; Wilkinson, C.L.; Levin, A.R. The Harvard Automated Processing Pipeline for Electroencephalography (HAPPE): Standardized processing software for developmental and high-artifact data. Front. Neurosci. 2018, 12, 316496. [Google Scholar] [CrossRef]
- Delorme, A.; Makeig, S. EEGLAB: An open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods 2004, 134, 9–21. [Google Scholar] [CrossRef]
- Winkler, I.; Haufe, S.; Tangermann, M. Automatic classification of artifactual ICA-components for artifact removal in EEG signals. Behav. Brain Funct. 2011, 7, 1–15. [Google Scholar]
- Welch, P. The use of fast Fourier transform for the estimation of power spectra: A method based on time averaging over short, modified periodograms. IEEE Trans. Audio Electroacoust. 1967, 15, 70–73. [Google Scholar] [CrossRef]
- Pascual-Marqui, R.D.; Lehmann, D.; Koukkou, M.; Kochi, K.; Anderer, P.; Saletu, B.; Tanaka, H.; Hirata, K.; John, E.R.; Prichep, L.; et al. Assessing interactions in the brain with exact low-resolution electromagnetic tomography. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2011, 369, 3768–3784. [Google Scholar] [CrossRef] [PubMed]
- Varastegan, S.; Kazemi, R.; Rostami, R.; Khomami, S.; Zandbagleh, A.; Hadipour, A.L. Remember NIBS? tACS improves memory performance in elders with subjective memory complaints. GeroScience 2023, 45, 851–869. [Google Scholar] [CrossRef] [PubMed]
- Halder, T.; Talwar, S.; Jaiswal, A.K.; Banerjee, A. Quantitative evaluation in estimating sources underlying brain oscillations using current source density methods and beamformer approaches. Eneuro 2019, 6, ENEURO.0170-19.2019. [Google Scholar] [CrossRef] [PubMed]
- Hauk, O.; Stenroos, M.; Treder, M.S. Towards an objective evaluation of EEG/MEG source estimation methods–The linear approach. Neuroimage 2022, 255, 119177. [Google Scholar] [CrossRef]
- Evans, A.C.; Janke, A.L.; Collins, D.L.; Baillet, S. Brain templates and atlases. Neuroimage 2012, 62, 911–922. [Google Scholar] [CrossRef]
- Leventhal, A.M.; Rehm, L.P. The empirical status of melancholia: Implications for psychology. Clin. Psychol. Rev. 2005, 25, 25–44. [Google Scholar] [CrossRef]
- Mazza, F.; Guet-McCreight, A.; Valiante, T.A.; Griffiths, J.D.; Hay, E. In-silico EEG biomarkers of reduced inhibition in human cortical microcircuits in depression. PLoS Comput. Biol. 2023, 19, e1010986. [Google Scholar] [CrossRef]
- Coutin-Churchman, P.; Moreno, R. Intracranial current density (LORETA) differences in QEEG frequency bands between depressed and non-depressed alcoholic patients. Clin. Neurophysiol. 2008, 119, 948–958. [Google Scholar] [CrossRef]
- Pizzagalli, D.A.; Oakes, T.R.; Davidson, R.J. Coupling of theta activity and glucose metabolism in the human rostral anterior cingulate cortex: An EEG/PET study of normal and depressed subjects. Psychophysiology 2003, 40, 939–949. [Google Scholar] [CrossRef]
- Pizzagalli, D.A. Frontocingulate dysfunction in depression: Toward biomarkers of treatment response. Neuropsychopharmacology 2011, 36, 183–206. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Wang, Q.; Zhang, S.; Chen, Z.; Dai, Z.; Zhang, W.; Yao, Z.; Lu, Q. Local and large-scale resting-state oscillatory dysfunctions for early antidepressant response prediction in major depressive disorder. J. Affect. Disord. 2023, 340, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Cantisani, A.; Koenig, T.; Horn, H.; Müller, T.; Strik, W.; Walther, S. Psychomotor retardation is linked to frontal alpha asymmetry in major depression. J. Affect. Disord. 2015, 188, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Cantisani, A.; Koenig, T.; Stegmayer, K.; Federspiel, A.; Horn, H.; Müller, T.; Wiest, R.; Strik, W.; Walther, S. EEG marker of inhibitory brain activity correlates with resting-state cerebral blood flow in the reward system in major depression. Eur. Arch. Psychiatry Clin. Neurosci. 2016, 266, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Bolton, M.M.; Pittman, A.J.; Lo, D.C. Brain-derived neurotrophic factor differentially regulates excitatory and inhibitory synaptic transmission in hippocampal cultures. J. Neurosci. 2000, 20, 3221–3232. [Google Scholar] [CrossRef]
- Başar, E.; Güntekin, B.; Atagün, I.; Turp Gölbaşı, B.; Tülay, E.; Özerdem, A. Brain’s alpha activity is highly reduced in euthymic bipolar disorder patients. Cogn. Neurodynamics 2012, 6, 11–20. [Google Scholar] [CrossRef]
- Nguyen, T.D.; Ha, T.T.H. Bipolar disorder traits: An electroencephalogram systematic review. Vietnam J. Sci. Technol. Eng. 2022, 64, 84–90. [Google Scholar] [CrossRef]
- Nierenberg, A.A.; Agustini, B.; Köhler-Forsberg, O.; Cusin, C.; Katz, D.; Sylvia, L.G.; Peters, A.; Berk, M. Diagnosis and treatment of bipolar disorder: A review. JAMA 2023, 330, 1370–1380. [Google Scholar] [CrossRef]
- Bisley, J.W.; Goldberg, M.E. Attention, intention, and priority in the parietal lobe. Annu. Rev. Neurosci. 2010, 33, 1–21. [Google Scholar] [CrossRef]
- Stuss, D.T.; Knight, R.T. Principles of Frontal Lobe Function; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Zandbagleh, A.; Miltiadous, A.; Sanei, S.; Azami, H. Beta-to-Theta Entropy Ratio of EEG in Aging, Frontotemporal Dementia, and Alzheimer’s Dementia. Am. J. Geriatr. Psychiatry 2024, in press. [Google Scholar] [CrossRef]
- Rizvi, S.J.; Pizzagalli, D.A.; Sproule, B.A.; Kennedy, S.H. Assessing anhedonia in depression: Potentials and pitfalls. Neurosci. Biobehav. Rev. 2016, 65, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Moderie, C.; Nuñez, N.; Comai, S.; Saint-Laurent, M.; Fielding, A.; Low, N.; Gobbi, G. Distinct effects of antidepressants in association with mood stabilizers and/or antipsychotics in unipolar and bipolar depression. J. Clin. Psychopharmacol. 2022, 42, 118–124. [Google Scholar] [CrossRef] [PubMed]


| HC (n = 74) | MDD (n = 40) | F/(df) | p-Value | |
|---|---|---|---|---|
| Age in years (SD) | 18.98 (1.21) * | 18.70 (1.15) | 1.47 (1, 111) | 0.22 |
| Gender (male/female) | 35/39 | 10/30 | 5.40 (1) | 0.02 |
| BDI | 1.71 (1.65) | 22.27 (4.69) | 1.15e3 (1, 112) | <0.001 |
| BDI_Anh | 0.16 (0.46) | 4 (1.58) | 3.75e2 (1, 112) | <0.001 |
| BDI_Mel | 0.83 (0.90) | 6.42 (1.72) | 5.16e2 (1, 112) | <0.001 |
| TAI | 31.12 (5.49) | 56.15 (6.81) | 4.53e2 (1, 112) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zandbagleh, A.; Sanei, S.; Azami, H. Implications of Aperiodic and Periodic EEG Components in Classification of Major Depressive Disorder from Source and Electrode Perspectives. Sensors 2024, 24, 6103. https://doi.org/10.3390/s24186103
Zandbagleh A, Sanei S, Azami H. Implications of Aperiodic and Periodic EEG Components in Classification of Major Depressive Disorder from Source and Electrode Perspectives. Sensors. 2024; 24(18):6103. https://doi.org/10.3390/s24186103
Chicago/Turabian StyleZandbagleh, Ahmad, Saeid Sanei, and Hamed Azami. 2024. "Implications of Aperiodic and Periodic EEG Components in Classification of Major Depressive Disorder from Source and Electrode Perspectives" Sensors 24, no. 18: 6103. https://doi.org/10.3390/s24186103
APA StyleZandbagleh, A., Sanei, S., & Azami, H. (2024). Implications of Aperiodic and Periodic EEG Components in Classification of Major Depressive Disorder from Source and Electrode Perspectives. Sensors, 24(18), 6103. https://doi.org/10.3390/s24186103








