Validation of the Kinematic Assessment Protocol Used in the Technology-Supported Neurorehabilitation System, Rehabilitation Technologies for Hand and Arm (R3THA™), in Children and Teenagers with Cerebral Palsy
Abstract
:1. Introduction
1.1. Cerebral Palsy (CP) Background
1.2. Telerehabilitation in CP
1.3. Challenges in Remote Assessment in Children and Teenagers with CP
1.4. Study Objectives
2. Study One: Exploring the Relationship between R3HTA-AP Measurement Data and Children’s Ages and Upper Extremity Sizes
2.1. Materials and Methods
2.1.1. Study Participants
2.1.2. Study Protocol
2.1.3. Data Collection
Demographic Data
R3THA Assessment
2.1.4. Statistical Analysis
2.2. Results
2.2.1. Participants
2.2.2. Data Validation Analysis
3. Study Two: Evaluating the Validity of the R3HTA-AP by Correlating Its Kinematic Measurements with Clinical Assessments
3.1. Materials and Methods
3.1.1. Study Participants
3.1.2. Study Protocol
3.1.3. Data Collection
Demographic Data
Clinical Assessments
3.1.4. R3THA Assessment
3.2. Statistical Analysis
3.3. Results
3.3.1. Participants
3.3.2. Correlation Analysis
Correlation between Box and Blocks Test and R3THA-AP
Correlation between MA2-ROM and R3THA-AP
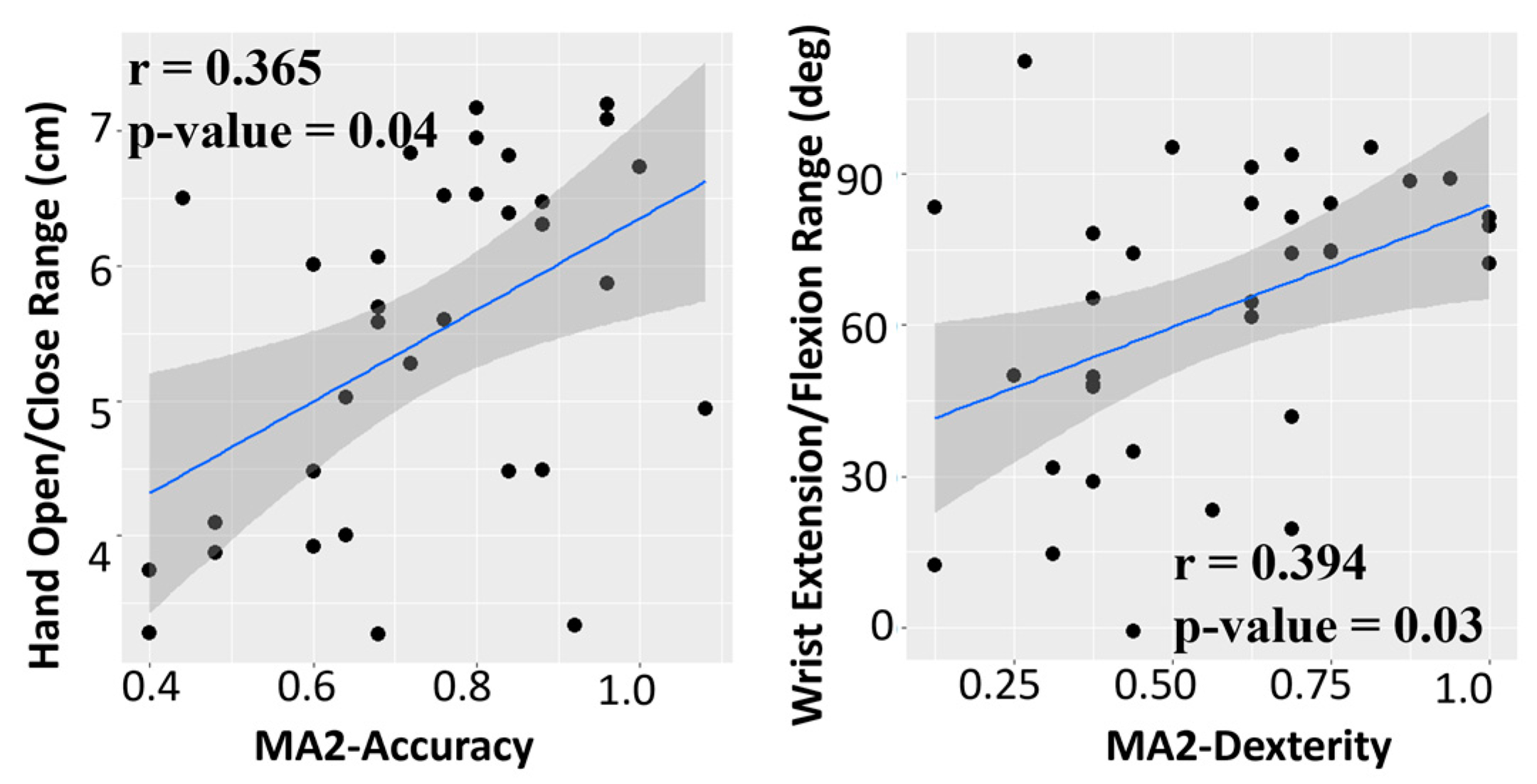
Correlation of R3THA-AP with MA2-Accuracy and MA2-Dexterity
4. Discussion
5. Conclusions
6. Patent
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Accardo, P.J.; Shapiro, B.K. Neurodevelopmental disabilities in pediatrics and child neurology: Child development training for the future. J. Pediatr. Rehabil. Med. 2008, 1, 113–114. [Google Scholar] [PubMed]
- Plasschaert, V.F.P.; Vriezekolk, J.E.; Aarts, P.B.M.; Geurts, A.C.H.; Van den Ende, C.H.M. Interventions to improve upper limb function for children with bilateral cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2019, 61, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Jackman, M.; Lannin, N.; Galea, C.; Sakzewski, L.; Miller, L.; Novak, I. What is the threshold dose of upper limb training for children with cerebral palsy to improve function? A systematic review. Aust. Occup. Ther. J. 2020, 67, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Pagaki-Skaliora, M.; Morrow, E.; Theologis, T. Telehealth and remote interventions for children with cerebral palsy: Scoping review. JMIR Rehabil. Assist. Technol. 2022, 9, e36842. [Google Scholar] [CrossRef]
- Tigrini, A.; Ranaldi, S.; Verdini, F.; Mobarak, R.; Scattolini, M.; Conforto, S.; Schmid, M.; Burattini, L.; Gambi, E.; Fioretti, S.; et al. Intelligent Human–Computer Interaction: Combined Wrist and Forearm Myoelectric Signals for Handwriting Recognition. Bioengineering 2024, 11, 458. [Google Scholar] [CrossRef]
- Tigrini, A.; Verdini, F.; Scattolini, M.; Barbarossa, F.; Burattini, L.; Morettini, M.; Fioretti, S.; Mengarelli, A. Handwritten digits recognition from sEMG: Electrodes location and feature selection. IEEE Access 2023, 11, 58006–58015. [Google Scholar] [CrossRef]
- Qiu, Q.; Cronce, A.; Patel, J.; Fluet, G.G.; Mont, A.J.; Merians, A.S.; Adamovich, S.V. Development of the Home based Virtual Rehabilitation System (HoVRS) to remotely deliver an intense and customized upper extremity training. J. Neuroeng. Rehabil. 2020, 17, 155. [Google Scholar] [CrossRef] [PubMed]
- Dostie, R.; Gaboury, I.; Cinar, E.; Camden, C. Acceptability of pediatric telerehabilitation interventions provided by physical therapists and occupational therapists—A scoping review. Phys. Occup. Ther. Pediatr. 2022, 42, 615–634. [Google Scholar] [CrossRef] [PubMed]
- Meyns, P.; Roman de Mettelinge, T.; van der Spank, J.; Coussens, M.; Van Waelvelde, H. Motivation in pediatric motor rehabilitation: A systematic search of the literature using the self-determination theory as a conceptual framework. Dev. Neurorehabilit. 2018, 21, 371–390. [Google Scholar] [CrossRef]
- Tarakci, E.; Arman, N.; Tarakci, D.; Kasapcopur, O. Leap Motion Controller-based training for upper extremity rehabilitation in children and adolescents with physical disabilities: A randomized controlled trial. J. Hand Ther. 2020, 33, 220–228.e221. [Google Scholar] [CrossRef]
- Avcil, E.; Tarakci, D.; Arman, N.; Tarakci, E. Upper extremity rehabilitation using video games in cerebral palsy: A randomized clinical trial. Acta Neurol. Belg. 2021, 121, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, J.M.; Fernandes, R.C.; Pinto, C.S.; Pinheiro, P.R.; Ribeiro, S.; de Albuquerque, V.H. Novel Virtual Environment for Alternative Treatment of Children with Cerebral Palsy. Comput. Intell. Neurosci. 2016, 2016, 8984379. [Google Scholar] [CrossRef] [PubMed]
- Laufer, Y.; Weiss, P.T.L. Virtual reality in the assessment and treatment of children with motor impairment: A systematic review. J. Phys. Ther. Educ. 2011, 25, 59–71. [Google Scholar] [CrossRef]
- Abtahi, P.; Hough, S.Q.; Landay, J.A.; Follmer, S. Beyond being real: A sensorimotor control perspective on interactions in virtual reality. In Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems, New Orleans, LA, USA, 29 April–5 May 2022; pp. 1–17. [Google Scholar]
- Okazaki, S.; Muraoka, Y.; Suzuki, R. Validity and reliability of leap motion controller for assessing grasping and releasing finger movements. J. Ergon. Technol. 2017, 17, 32–42. [Google Scholar]
- Butt, A.H.; Rovini, E.; Dolciotti, C.; Bongioanni, P.; De Petris, G.; Cavallo, F. Leap motion evaluation for assessment of upper limb motor skills in Parkinson’s disease. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 116–121. [Google Scholar]
- MontJohnson, A.; Cronce, A.; Qiu, Q.; Patel, J.; Eriksson, M.; Merians, A.; Adamovich, S.; Fluet, G. Laboratory-Based Examination of the Reliability and Validity of Kinematic Measures of Wrist and Finger Function Collected by a Telerehabilitation System in Persons with Chronic Stroke. Sensors 2023, 23, 2656. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, P.H. Critical values for Spearman’s rank order correlation. J. Educ. Stat. 1989, 14, 245–253. [Google Scholar]
- Bourke-Taylor, H. Melbourne Assessment of Unilateral Upper Limb Function: Construct validity and correlation with the Pediatric Evaluation of Disability Inventory. Dev. Med. Child Neurol. 2003, 45, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Jongbloed-Pereboom, M.; Nijhuis-van der Sanden, M.W.; Steenbergen, B. Norm scores of the box and block test for children ages 3-10 years. Am. J. Occup. Ther. 2013, 67, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Mathiowetz, V.; Volland, G.; Kashman, N.; Weber, K. Adult norms for the Box and Block Test of manual dexterity. Am. J. Occup. Ther. 1985, 39, 386–391. [Google Scholar] [CrossRef]
- Chan, A.; Halevi, T.; Memon, N. Leap Motion Controller for Authentication via Hand Geometry and Gestures. In Human Aspects of Information Security, Privacy, and Trust; Tryfonas, T., Askoxylakis, I., Eds.; Springer International Publishing: Cham, Switzerland, 2015; pp. 13–22. [Google Scholar]
- Martinie, O.; Mercier, C.; Gordon, A.M.; Robert, M.T. Upper Limb Motor Planning in Individuals with Cerebral Palsy Aged between 3 and 21 Years Old: A Systematic Review. Brain Sci. 2021, 11, 920. [Google Scholar] [CrossRef]
- National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention. Middle Childhood (6–8 Years of Age). 2021. Available online: https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle.html (accessed on 30 May 2024).
- Smeragliuolo, A.H.; Hill, N.J.; Disla, L.; Putrino, D. Validation of the Leap Motion Controller using markered motion capture technology. J. Biomech. 2016, 49, 1742–1750. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Rha, D.W.; Kim, S.A.; Park, E.S. The Dynamic Thumb-in-Palm Pattern in Children with Spastic Cerebral Palsy and Its Effects on Upper Limb Function. Children 2020, 8, 17. [Google Scholar] [CrossRef] [PubMed]
- Srikesavan, C.S.; Shay, B.; Szturm, T. Test-retest reliability and convergent validity of a computer based hand function test protocol in people with arthritis. Open Orthop. J. 2015, 9, 57. [Google Scholar] [CrossRef] [PubMed]
- Mollà-Casanova, S.; Llorens, R.; Borrego, A.; Salinas-Martínez, B.; Serra-Añó, P. Validity, reliability, and sensitivity to motor impairment severity of a multi-touch app designed to assess hand mobility, coordination, and function after stroke. J. NeuroEng. Rehabil. 2021, 18, 70. [Google Scholar] [CrossRef]





| R3THA-AP Subtest Items | Descriptions | Equation |
|---|---|---|
| Hand Open/Close Range (cm) | The participant fully opens and then fully closes their hand. The Hand Open/Close Range value is calculated by measuring the difference in the average distance between the fingertips and the center of the palm across all four fingers in these two positions. A larger value indicates a greater hand opening range. | where is the distance between the nth fingertips and the center of the palm when the hand is open; is the distance between the nth fingertips and the center of the palm when the hand is closed. |
| Hand Open/Close Trace Error Rate (%) | The participant controls a cursor that moves up and down by opening and closing their hand. The participant attempts to trace an irregular wave which moves on the screen from left to right at a constant speed. The trace error rate is calculated as the root mean square error (RMSE) between the cursor position and the corresponding target point on the wave normalized by Hand Open/Close Range. The smaller the value, the better the control of hand opening. | where n is the number of observations; is the cursor position; is the corresponding target point on the wave; is the Hand Open/Close Range. |
| Wrist Extension/Flexion Range (deg) | The participant extends and flexes their wrist against gravity with their forearm in a fixed position. The angular difference between these two positions is reported as the wrist pitch range. | Wrist Extension/Flexion Range = Max Wrist Extension angle + Max Wrist Flexion angle |
| Wrist Extension/Flexion Trace Error Rate (%) | The participant controls a cursor that moves up and down by extending and flexing their wrist. They use the cursor to trace a sine wave on the screen. The trace error rate is calculated as the root mean square error (RMSE) between the cursor position and the corresponding target point on the wave. | where n is the number of observations; is the cursor position; is the corresponding target point on the wave; is the wrist extension/flexion range. |
| Pronation/Supination Range (deg) | The participant moves and holds their hand in pronation and supination with their elbow fixed. The range is then calculated. | Pronation/Supination Range = Max Pronation angle + Max Supination angle |
| Pronation/Supination Trace Error Rate (%) | The participant controls a cursor that moves up and down by pronating and supinating their hand. They use the cursor to trace a sine wave on the screen. The trace error rate is calculated as the root mean square error (RMSE) between the cursor position and the corresponding target point on the wave. | where n is the number of observations; is the cursor position; is the corresponding target point on the wave; is the forearm pronation/supination range. |
| Mean (SD) | |
|---|---|
| Age | 9.28 (4.4) |
| Gender | 15 females/21 males |
| Hemiplegia side | 17 left/19 right |
| Upper extremity size (inches) | 13.22 (2.53) |
| Mean (SD) | |
|---|---|
| Age | 11.89 (2.5) |
| Gender | 7 females/14 males |
| Hemiplegia side | 11 left/9 right |
| Initial Box and Block Test | 13.15 (10.13) |
| Initial MA2-ROM | 0.71 (0.18) |
| Initial MA2-Accuracy | 0.57 (0.24) |
| Initial MA2-Dexterity | 0.74 (0.24) |
| Initial MA2-Fluency | 0.62 (0.16) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qiu, Q.; Mont, A.J.; Gross, A.; Fluet, G.; Adamovich, S.; Eriksson, M. Validation of the Kinematic Assessment Protocol Used in the Technology-Supported Neurorehabilitation System, Rehabilitation Technologies for Hand and Arm (R3THA™), in Children and Teenagers with Cerebral Palsy. Sensors 2024, 24, 5013. https://doi.org/10.3390/s24155013
Qiu Q, Mont AJ, Gross A, Fluet G, Adamovich S, Eriksson M. Validation of the Kinematic Assessment Protocol Used in the Technology-Supported Neurorehabilitation System, Rehabilitation Technologies for Hand and Arm (R3THA™), in Children and Teenagers with Cerebral Palsy. Sensors. 2024; 24(15):5013. https://doi.org/10.3390/s24155013
Chicago/Turabian StyleQiu, Qinyin, Ashley J. Mont, Amanda Gross, Gerard Fluet, Sergei Adamovich, and Mee Eriksson. 2024. "Validation of the Kinematic Assessment Protocol Used in the Technology-Supported Neurorehabilitation System, Rehabilitation Technologies for Hand and Arm (R3THA™), in Children and Teenagers with Cerebral Palsy" Sensors 24, no. 15: 5013. https://doi.org/10.3390/s24155013
APA StyleQiu, Q., Mont, A. J., Gross, A., Fluet, G., Adamovich, S., & Eriksson, M. (2024). Validation of the Kinematic Assessment Protocol Used in the Technology-Supported Neurorehabilitation System, Rehabilitation Technologies for Hand and Arm (R3THA™), in Children and Teenagers with Cerebral Palsy. Sensors, 24(15), 5013. https://doi.org/10.3390/s24155013








