A Novel Signal Restoration Method of Noisy Photoplethysmograms for Uninterrupted Health Monitoring
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials and Preprocessing
- 1.
- ECG match database (ECGMDB): This database contains 30 clinical recordings from 16 patients within the BIDMC PPG and Respiration Dataset. Recordings consisted of a noisy PPG segment with a maximum duration of 20 s, alongside a corresponding clean ECG segment. The aim of this database was to evaluate whether HR analysis from reconstructed PPGs matched the HR analysis from the ECGs, determining the reliability of such reconstructed PPGs for continuous HR monitoring, especially in those cases where the ECG is unavailable.
- 2.
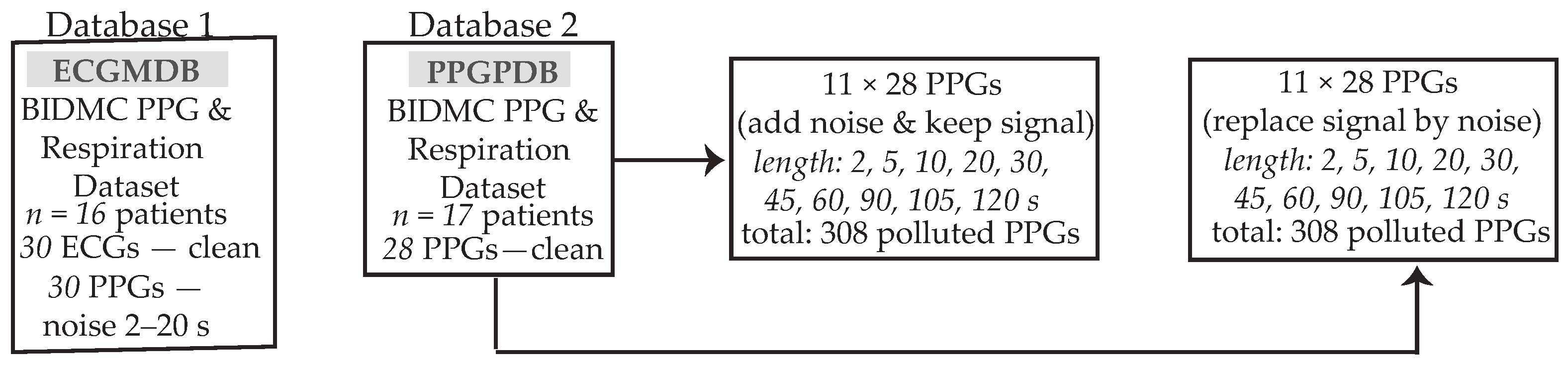
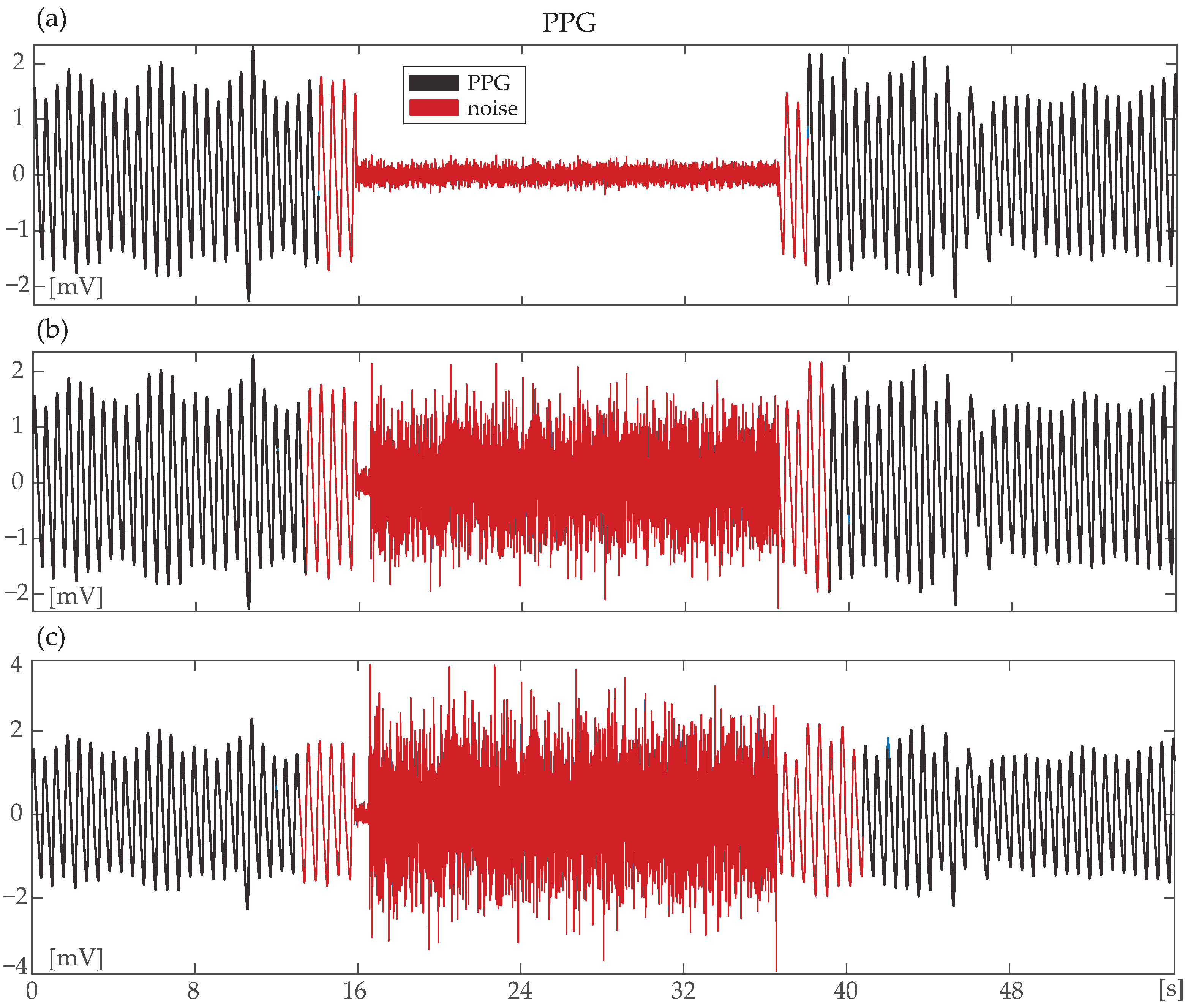
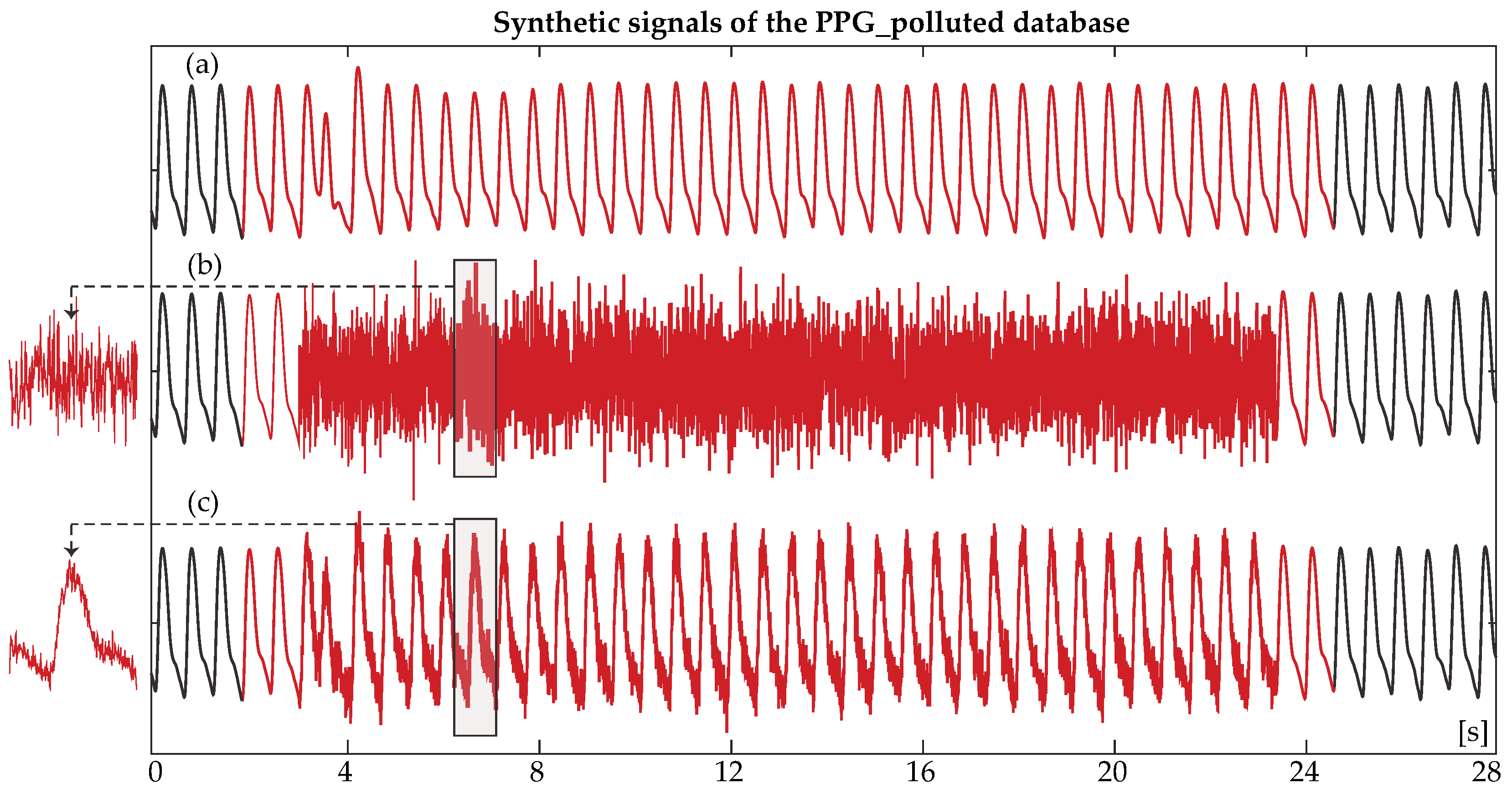
- PPG polluted database (PPGPDB): For this database, 28 real 8-min clean PPG recordings of 17 patients from the BIDMC PPG and Respiration Dataset were recruited. For each real PPG, 22 synthetic signals were created. Eleven of these signals were created from the addition of random noise with a varying duration of 2, 5, 10, 20, 30, 45, 60, 75, 90, 105, and 120 s in the real PPG and the remaining 11, with the addition of random noise with varying duration of the same length, following the complete cancellation of the respective clean PPG segment. A scheme of the utilized databases can be observed in Figure 1. The objective of the creation of two synthetic sub-databases out of the PPGPDB was to test the noise detection algorithm both in the case of deteriorated signal quality due to noise and in the case when the signal is completely lost due to loss of contact with the recording device.
2.2. Motion Artifact Detection
- Step 1: The first step of MA detection was signal segmentation into 8 s epochs with 75% overlapping. This allows for the detection of noise at a minimum length of 2 s.
- Step 2: Spectral analysis was performed in order to detect the dominant frequency (DF) of each epoch [31]. Given that normal HR rarely exceeds the 0.83–3.33 Hz limits, a first-level detection of artifacts was performed by verifying that DF belongs to the broadened 0.3–4 Hz range. Once this hypothesis was verified, the 2nd () and 3 () harmonics were defined as DF and DF, respectively, and the spectral power () of each 0.7 Hz band with DF, , and centered was calculated.
- Step 3: The cumulative spectral power (CSP) was defined as the sum of the spectral power at each of the three spectral windowsand compared with the total spectral power (TSP) of the segment. An artifact was detected when the condition was fulfilled.
- Step 4: In the case in which no artifact was detected, a last-round check was performed by verifying the existence of a spectral peak at each of the 3 spectral windows of DF, , and . In the opposite case, the segment was labelled as noise. The aim of this step is to detect any artifacts with a spectral peak close to the DF of a normal heart rate and a gradual spectral slope. Figure 4c illustrates the power spectral density of a clean segment, while Figure 4d shows the power spectral density of a noisy segment.Figure 4. Power spectrum of a clean (a) and a noisy photoplethysmography (PPG) signal segment (b) and their corresponding PPG signals. Shaded areas indicate the Hz spectral windows around dominant frequency (DF) and the harmonics. Even though cumulative spectral power (CSP) is relatively high in case (d), no peak is found in the window with centered. Spectral overlapping between two spectral windows is indicative of noisy segments.Figure 4. Power spectrum of a clean (a) and a noisy photoplethysmography (PPG) signal segment (b) and their corresponding PPG signals. Shaded areas indicate the Hz spectral windows around dominant frequency (DF) and the harmonics. Even though cumulative spectral power (CSP) is relatively high in case (d), no peak is found in the window with centered. Spectral overlapping between two spectral windows is indicative of noisy segments.
- Step 5: Each 8 s segment detected as noise was then stored into a matrix, and the actual noisy part of each segment was finally defined by checking whether sequential windows are detected or not as noise. Figure 5 shows the power spectral density of a segment that contains a clean and a noisy part. Originally, the entire 8 s segment is labelled as noise, but in the end, only the first four seconds are detected as actual noise, and the remaining four seconds are considered as a clean PPG signal.
- Step 6: A final optional amplitude control was performed in order to spot undetected noise of very low or very high amplitude. For the very low and the very high amplitude noise, the following thresholds were used, respectively, after trial and errorwhere is the normalized PPG according to the highest amplitude and

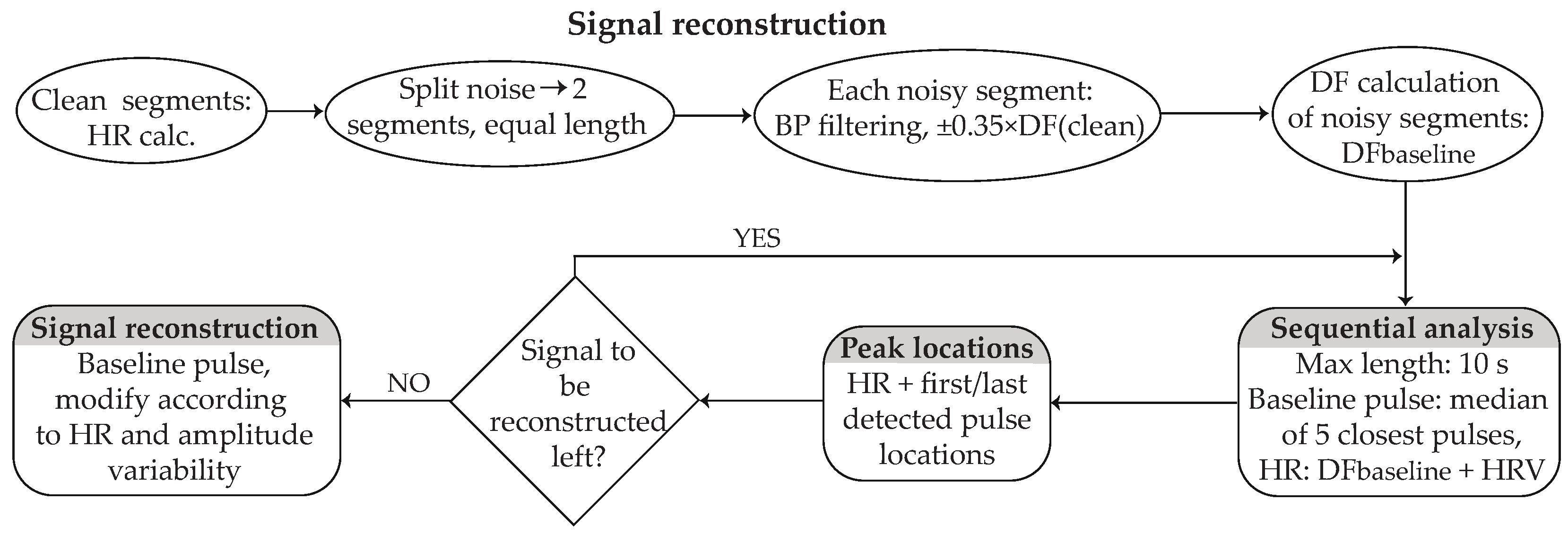
2.3. Signal Reconstruction
- Step 1—Calculating the reference parameters: Before reconstruction, a short preparation including the calculation of parameters that will serve as a reference for the signal reconstruction were computed. These include the following:
- -
- The HR of the clean segments surrounding noise. PPG pulse peaks were detected by 2nd-derivative analysis based on an adaptive amplitude threshold [32]. Each segment consisted of 10 pulses.
- -
- The noisy signal was divided into two segments of equal length, and each segment was band-pass filtered with a 2nd-order Butterworth filter with cut-off frequencies of the DF according to the HR of the closest detected pulse.
- -
- The DF of each segment was calculated and used as the baseline for the signal reconstruction (baseline DF). In order to avoid any distortion in the morphology of the signal between the clean-reconstructed signal transition, the first and last points of the noisy segments were appropriately relocated so that they correspond to the middle point of the valley between two successive zero-crossing points.
- -
- HRV and amplitude variability of the closest clean segments were calculated as the difference in HR and amplitude between two successive peaks, respectively.
- -
- The baseline pulse for each segment was calculated as the median pulse of the 5 closest pulses of the clean signal surrounding the noise. In order for the signal to be coherent, each baseline pulse started and ended in the middle point of the valley between two successive zero-crossing points.
- Step 2—Localizing the peaks of the segment under reconstruction: The reconstruction process was performed in segments of 10 s or less, starting from the edges and moving towards the center of the noisy part. For the HR calculation of each peak, the baseline DF of each segment along with the corresponding HRV was considered, so that the HRV of the closest peak was assigned to the first pulse, the HRV of the second closest peak was assigned to the second pulse, and this process continued until the HR of all peaks of this segment was calculated. For the peak locations, the HR distance from the last and first detected peaks of the clean segments surrounding the noise was calculated, and the remaining peak locations were defined from the distance to the last detected peak according to HR.
- Step 3—Localizing the peaks of the remaining signal: This step was performed only if the noise duration was longer than 20 s. The signal left to be reconstructed was calculated by considering PPG HR and the location of the last detected peaks of the already reconstructed segment. The next segment under reconstruction was then defined and an iterative peak location process started using the baseline DF as well the HRV of the closest pulses of the already reconstructed segment.
- Step 4—Fixing inconsistencies in peak localization: When no 10 s segment was left for reconstruction, a last-round control for the signal left for reconstruction was performed by calculating the distance between the two middle peaks of the reconstructed signal. If the distance was longer than 0 but shorter than the length of a pulse, each distance between two successive peaks was prolonged by one sample point, starting from the middle of the reconstructed segment and moving simultaneously forward and backwards, until no sample points were left. If the distance was longer than a pulse, the corresponding number of pulses was added in the middle of the reconstructed segment. This step was repeated until the distance of the two middle peaks was equal to the length of a pulse, with a margin of 2 sample points.
- Step 5—Signal replacement: The reconstruction was finalized by replacing the noisy signal with the baseline pulses, prolonged or shortened according to the peak-to-peak distance, so that each peak location corresponded to the peak of each pulse. Additionally, each pulse was stretched or shrunk in amplitude according to the corresponding amplitude variability.
2.4. Evaluation
2.4.1. Evaluation of the Noise Detection Method
- TP: 1 s of noise, correctly detected as noise;
- FP: 1 s of clean signal, wrongly labelled as noise;
- FN: 1 s of noise, wrongly labelled as clean signal;
- TN: 1 s of clean signal, correctly identified as clean signal.
2.4.2. Evaluation of the PPG Reconstruction Method
3. Results
3.1. MA Detection
3.2. PPG Reconstruction
3.2.1. ECG Match Database
3.2.2. PPG Polluted Database
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 2007, 28, R1–R39. [Google Scholar] [CrossRef] [PubMed]
- Labati, R.D.; Piuri, V.; Rundo, F.; Scotti, F. Photoplethysmographic biometrics: A comprehensive survey. Pattern Recognit. Lett. 2022, 156, 119–125. [Google Scholar] [CrossRef]
- Zhao, T.; Wang, Y.; Liu, J.; Cheng, J.; Chen, Y.; Yu, J. Robust Continuous Authentication Using Cardiac Biometrics from Wrist-Worn Wearables. IEEE Internet Things J. 2022, 9, 9542–9556. [Google Scholar] [CrossRef]
- Castaneda, D.; Esparza, A.; Ghamari, M.; Soltanpur, C.; Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int. J. Biosens. Bioelectron. 2018, 4, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Pang, B.; Liu, M.; Zhang, X.; Li, P.; Chen, H. A novel approach framework based on statistics for reconstruction and heartrate estimation from PPG with heavy motion artifacts. Sci. China Inf. Sci. 2018, 61, 022312. [Google Scholar] [CrossRef]
- Tang, Q.; Chen, Z.; Menon, C.; Ward, R.; Elgendi, M. PPGTempStitch: A MATLAB Toolbox for Augmenting Annotated Photoplethsmogram Signals. Sensors 2021, 21, 4007. [Google Scholar] [CrossRef]
- Maity, A.K.; Veeraraghavan, A.; Sabharwal, A. PPGMotion: Model-based detection of motion artifacts in photoplethysmography signals. Biomed. Signal Process. Control 2022, 75, 103632. [Google Scholar] [CrossRef]
- Bolanos, M.; Nazeran, H.; Haltiwanger, E. Comparison of heart rate variability signal features derived from electrocardiography and photoplethysmography in healthy individuals. In Proceedings of the 2006 International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 31 August 2006–3 September 2006; pp. 4289–4294. [Google Scholar] [CrossRef]
- Sun, S.; Bezemer, R.; Long, X.; Muehlsteff, J.; Aarts, R.M. Systolic blood pressure estimation using PPG and ECG during physical exercise. Physiol. Meas. 2016, 37, 2154. [Google Scholar] [CrossRef]
- Obi, A.I. An Overview of Wearable Photoplethysmographic Sensors and Various Algorithms for Tracking of Heart Rates. Eng. Proc. 2022, 10, 77. [Google Scholar] [CrossRef]
- Casalino, G.; Castellano, G.; Nisio, A.; Pasquadibisceglie, V.; Zaza, G. A mobile app for contactless measurement of vital signs through remote Photoplethysmography. In Proceedings of the 2022 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Prague, Czech Republic, 9–12 October 2022; pp. 2675–2680. [Google Scholar] [CrossRef]
- Polak, A.G.; Klich, B.; Saganowski, S.; Prucnal, M.A.; Kazienko, P. Processing Photoplethysmograms Recorded by Smartwatches to Improve the Quality of Derived Pulse Rate Variability. Sensors 2022, 22, 7047. [Google Scholar] [CrossRef]
- Wolling, F.; Wasala, S.M.; Van Laerhoven, K. Optimal Preprocessing of Raw Signals from Reflective Mode Photoplethysmography in Wearable Devices. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Virtual, 1–5 November 2021; pp. 1157–1163. [Google Scholar] [CrossRef]
- Shao, S.; Wang, T.; Wang, L.; Li, S.; Yao, C. A Photoplethysmograph Signal Preprocess Method Based on Wavelet Transform. In Proceedings of the 2021 36th Youth Academic Annual Conference of Chinese Association of Automation (YAC), Nanchang, China, 28–30 May 2021. [Google Scholar] [CrossRef]
- Pilt, K.; Meigas, K.; Karai, D.; Kaik, J. PPG Signal Processing for Pulse Delay Computing by Using Adaptive Comb Filter. In World Congress on Medical Physics and Biomedical Engineering, September 7–12, 2009, Munich, Germany: Vol. 25/4 Image Processing, Biosignal Processing, Modelling and Simulation, Biomechanics; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar] [CrossRef]
- Guo, J.; Chen, X.; Zhao, J.; Zhang, X.; Chen, X. An Effective Photoplethysmography Heart Rate Estimation Framework Integrating Two-Level Denoising Method and Heart Rate Tracking Algorithm Guided by Finite State Machine. IEEE J. Biomed. Health Inform. 2022, 26, 3731–3742. [Google Scholar] [CrossRef] [PubMed]
- Dao, D.; Salehizadeh, S.M.A.; Noh, Y.; Chong, J.W.; Cho, C.H.; McManus, D.; Darling, C.E.; Mendelson, Y.; Chon, K.H. A Robust Motion Artifact Detection Algorithm for Accurate Detection of Heart Rates From Photoplethysmographic Signals Using Time-Frequency Spectral Features. IEEE J. Biomed. Health Inform. 2017, 21, 1242–1253. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Song, S.; Vullings, R.; Biswas, D.; Simões-Capela, N.; van Helleputte, N.; van Hoof, C.; Groenendaal, W. Motion Artifact Reduction for Wrist-Worn Photoplethysmograph Sensors Based on Different Wavelengths. Sensors 2019, 19, 673. [Google Scholar] [CrossRef] [PubMed]
- Wan, C.; Chen, D.; Yang, J. Pulse rate estimation from forehead photoplethysmograph signal using RLS adaptive filtering with dynamical reference signal. Biomed. Signal Process. Control 2022, 71, 103189. [Google Scholar] [CrossRef]
- Lee, H.; Chung, H.; Ko, H.; Parisi, A.; Busacca, A.; Faes, L.; Pernice, R.; Lee, J. Adaptive scheduling of acceleration and gyroscope for motion artifact cancelation in photoplethysmography. Comput. Methods Programs Biomed. 2022, 226, 107126. [Google Scholar] [CrossRef] [PubMed]
- Waugh, W.; Allen, J.; Wightman, J.; Sims, A.J.; Beale, T.A.W. Novel Signal Noise Reduction Method through Cluster Analysis, Applied to Photoplethysmography. Comput. Math. Methods Med. 2018, 2018, 6812404. [Google Scholar] [CrossRef] [PubMed]
- Moscato, S.; Giudice, S.L.; Massaro, G.; Chiari, L. Wrist Photoplethysmography Signal Quality Assessment for Reliable Heart Rate Estimate and Morphological Analysis. Sensors 2022, 22, 5831. [Google Scholar] [CrossRef]
- Chong, J.W.; Dao, D.K.; Salehizadeh, S.M.A.; McManus, D.D.; Darling, C.E.; Chon, K.H.; Mendelson, Y. Photoplethysmograph signal reconstruction based on a novel hybrid motion artifact detection-reduction approach. Part I: Motion and noise artifact detection. Ann. Biomed. Eng. 2014, 42, 2238–2250. [Google Scholar] [CrossRef]
- Rodrigues, J.; Liu, H.; Folgado, D.; Belo, D.; Schultz, T.; Gamboa, H. Feature-Based Information Retrieval of Multimodal Biosignals with a Self-Similarity Matrix: Focus on Automatic Segmentation. Biosensors 2022, 12, 1182. [Google Scholar] [CrossRef]
- Pimentel, M.A.; Johnson, A.E.; Charlton, P.H.; Birrenkott, D.; Watkinson, P.J.; Tarassenko, L.; Clifton, D.A. Toward a robust estimation of respiratory rate from pulse oximeters. IEEE Trans. Biomed. Eng. 2016, 64, 1914–1923. [Google Scholar] [CrossRef]
- Saeed, M.; Villarroel, M.; Reisner, A.T.; Clifford, G.; Lehman, L.W.; Moody, G.; Heldt, T.; Kyaw, T.H.; Moody, B.; Mark, R.G. Multiparameter Intelligent Monitoring in Intensive Care II: A public-access intensive care unit database. Crit. Care Med. 2011, 39, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Goldberger, A.L.; Amaral, L.A.; Glass, L.; Hausdorff, J.M.; Ivanov, P.C.; Mark, R.G.; Mietus, J.E.; Moody, G.B.; Peng, C.-K.; Stanley, H.E. PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals. Circulation 2000, 101, E215–E220. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Iniesta, M.; Ródenas, J.; Rieta, J.J.; Alcaraz, R. The stationary wavelet transform as an efficient reductor of powerline interference for atrial bipolar electrograms in cardiac electrophysiology. Physiol. Meas. 2019, 40, 075003. [Google Scholar] [CrossRef] [PubMed]
- Sörnmo, L.; Laguna, P. Electrocardiogram (ECG) Signal Processing. In Wiley Encyclopedia of Biomedical Engineering; John Wiley and Sons: New York, NY, USA, 2006; Volume 2, pp. 1298–1313. [Google Scholar] [CrossRef]
- Martinez, A.; Alcaraz, R.; Rieta, J.J. A new method for automatic delineation of ECG fiducial points based on the Phasor Transform. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2010, 2010, 4586–4589. [Google Scholar] [CrossRef] [PubMed]
- Alcaraz, R.; Hornero, F.; Rieta, J.J. Electrocardiographic Spectral Features for Long-Term Outcome Prognosis of Atrial Fibrillation Catheter Ablation. Ann. Biomed. Eng. 2016, 44, 3307–3318. [Google Scholar] [CrossRef] [PubMed]
- Anisimov, A.; Alekseev, B.; Egorov, D. Comparison of Heart Rate Derived from ECG and Pulse Wave Signals during Controlled Breathing Test for Biofeedback Systems. In Proceedings of the 2021 IEEE Ural-Siberian Conference on Computational Technologies in Cognitive Science, Genomics and Biomedicine (CSGB), Novosibirsk, Russia, 26–28 May 2021; pp. 430–434. [Google Scholar] [CrossRef]
- Altman, D.G.; Bland, J.M. Measurement in Medicine: The Analysis of Method Comparison Studies. J. R. Stat. Soc. Ser. D (Stat.) 1983, 32, 307. [Google Scholar] [CrossRef]
- Giavarina, D. Understanding Bland Altman analysis. Biochem. Medica 2015, 25, 141–151. [Google Scholar] [CrossRef]
- Shi, W.; Zhou, C.; Zhang, Y.; Li, K.; Ren, X.; Liu, H.; Ye, X. Hybrid modeling on reconstitution of continuous arterial blood pressure using finger photoplethysmography. Biomed. Signal Process. Control 2023, 85, 104972. [Google Scholar] [CrossRef]
- Salehizadeh, S.M.A.; Dao, D.K.; Chong, J.W.; McManus, D.; Darling, C.; Mendelson, Y.; Chon, K.H. Photoplethysmograph signal reconstruction based on a novel motion artifact detection-reduction approach. Part II: Motion and noise artifact removal. Ann. Biomed. Eng. 2014, 42, 2251–2263. [Google Scholar] [CrossRef]









| Accuracy [%] | Sensitivity [%] | Specificity [%] | |
|---|---|---|---|
| ECGMDB | |||
| PPGPDB |
| Noise Addition | Accuracy [%] | Sensitivity [%] | Specificity [%] |
|---|---|---|---|
| 2 s | |||
| 5 s | |||
| 10 s | |||
| 20 s | |||
| 30 s | |||
| 45 s | |||
| 60 | |||
| 75 s | |||
| 90 s | |||
| 105 s | |||
| 120 s |
| HR | Correlation | MWU | BA | ||||
|---|---|---|---|---|---|---|---|
| Mean (std) | Median (iqr) | [%] | Value () | Value | CI [%] | CV [%] | |
| ECG | – | – | – | – | – | ||
| PPG | – | – | – | – | – | ||
| AE | – | – | – | – | – | ||
| ECG–PPG | – | – | |||||
| Median Values | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ref. | 2 s | 5 s | 10 s | 20 s | 30 s | 45 s | 60 s | 75 s | 90 s | 105 s | 120 s | |
| SD | ||||||||||||
| MAE | – | |||||||||||
| CI | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 s | 5 s | 10 s | 20 s | 30 s | 45 s | 60 s | 75 s | 90 s | 105 s | 120 s | |
| 0.97 | 0.86 | 0.97 | 0.93 | 0.97 | 0.97 | 0.93 | 0.97 | 0.97 | 0.97 | 0.97 | |
| 0.93 | 0.93 | 0.93 | 0.93 | 0.97 | 0.89 | 0.97 | 0.93 | 0.93 | 0.93 | 1.00 | |
| SD | 0.93 | 0.89 | 0.93 | 0.97 | 0.93 | 0.89 | 0.93 | 0.89 | 0.93 | 0.97 | 0.97 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vraka, A.; Zangróniz, R.; Quesada, A.; Hornero, F.; Alcaraz, R.; Rieta, J.J. A Novel Signal Restoration Method of Noisy Photoplethysmograms for Uninterrupted Health Monitoring. Sensors 2024, 24, 141. https://doi.org/10.3390/s24010141
Vraka A, Zangróniz R, Quesada A, Hornero F, Alcaraz R, Rieta JJ. A Novel Signal Restoration Method of Noisy Photoplethysmograms for Uninterrupted Health Monitoring. Sensors. 2024; 24(1):141. https://doi.org/10.3390/s24010141
Chicago/Turabian StyleVraka, Aikaterini, Roberto Zangróniz, Aurelio Quesada, Fernando Hornero, Raúl Alcaraz, and José J. Rieta. 2024. "A Novel Signal Restoration Method of Noisy Photoplethysmograms for Uninterrupted Health Monitoring" Sensors 24, no. 1: 141. https://doi.org/10.3390/s24010141
APA StyleVraka, A., Zangróniz, R., Quesada, A., Hornero, F., Alcaraz, R., & Rieta, J. J. (2024). A Novel Signal Restoration Method of Noisy Photoplethysmograms for Uninterrupted Health Monitoring. Sensors, 24(1), 141. https://doi.org/10.3390/s24010141








