Investigating the Structural and Functional Changes in the Optic Nerve in Patients with Early Glaucoma Using the Optical Coherence Tomography (OCT) and RETeval System
Abstract
1. Introduction
2. Materials and Methods
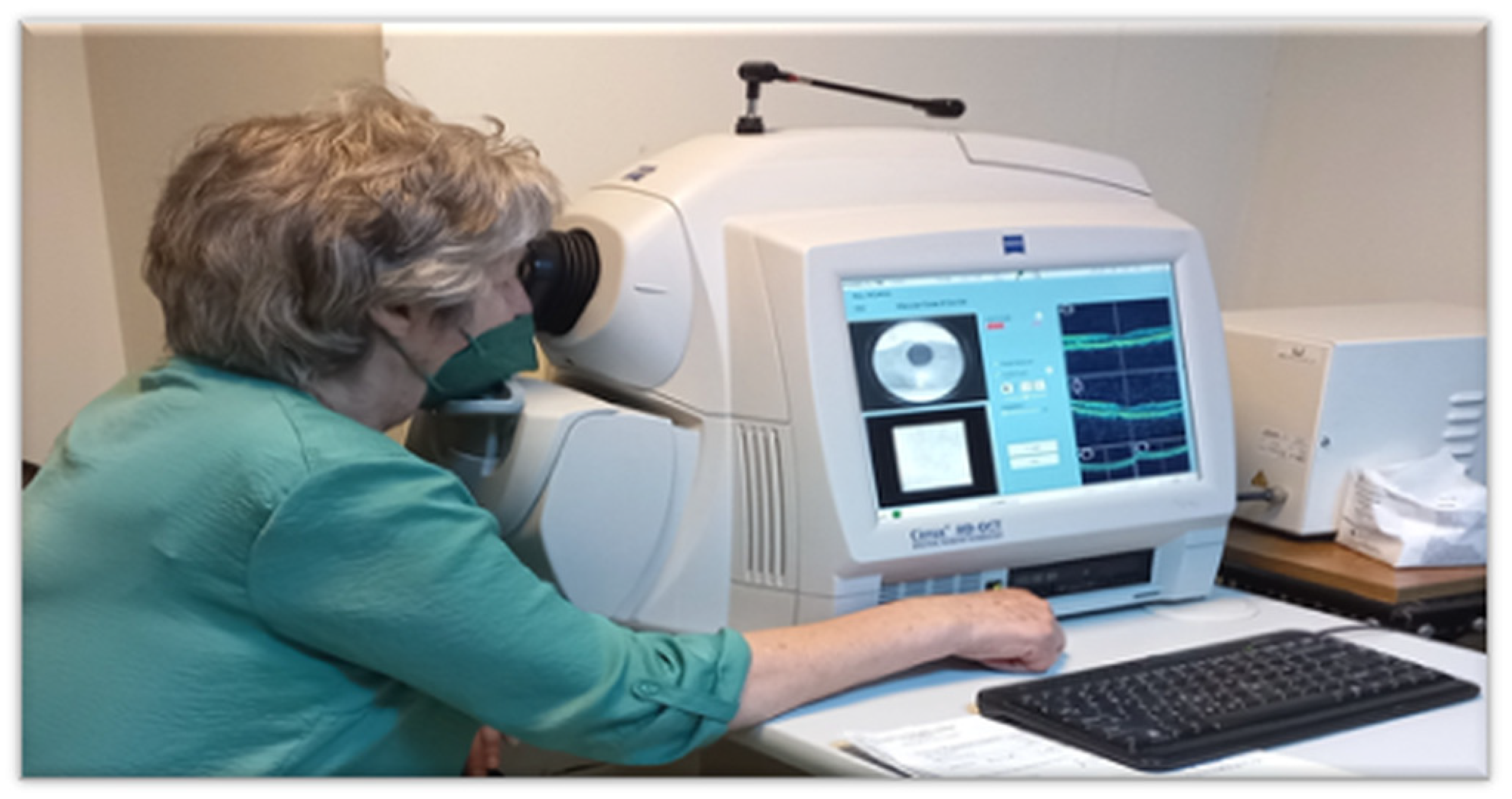
2.1. Spectral-Domain OCT Measurements
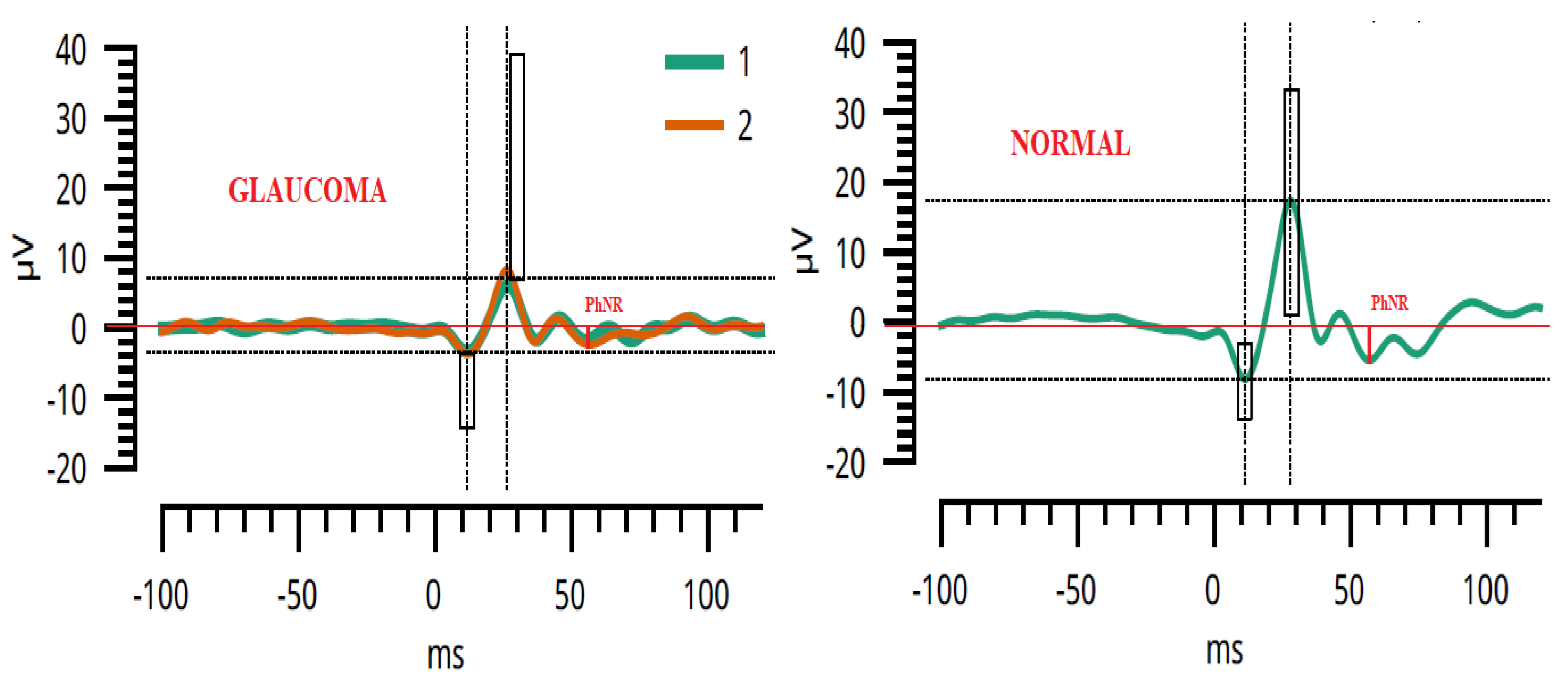
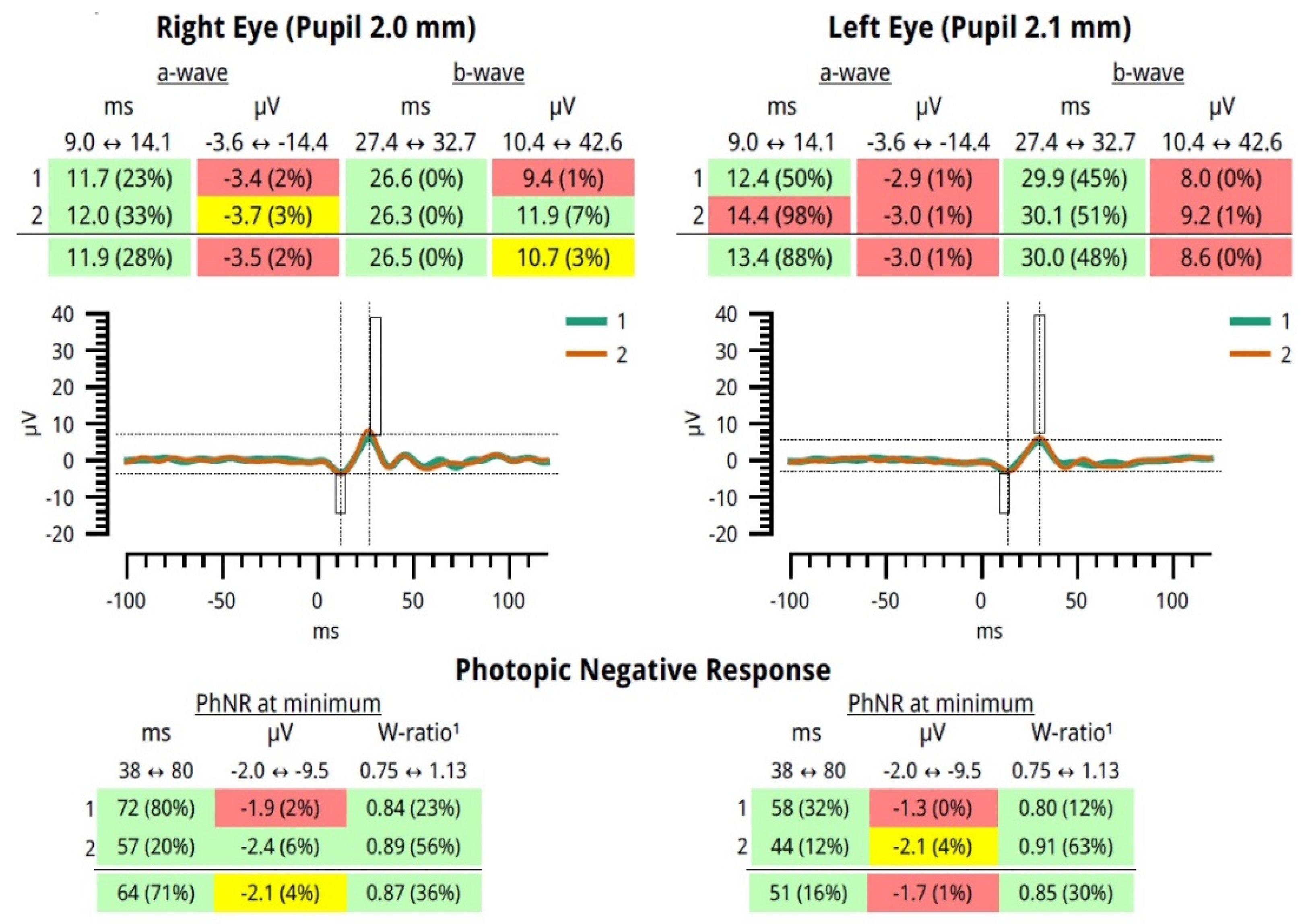
2.2. The ERG Protocol Specifications
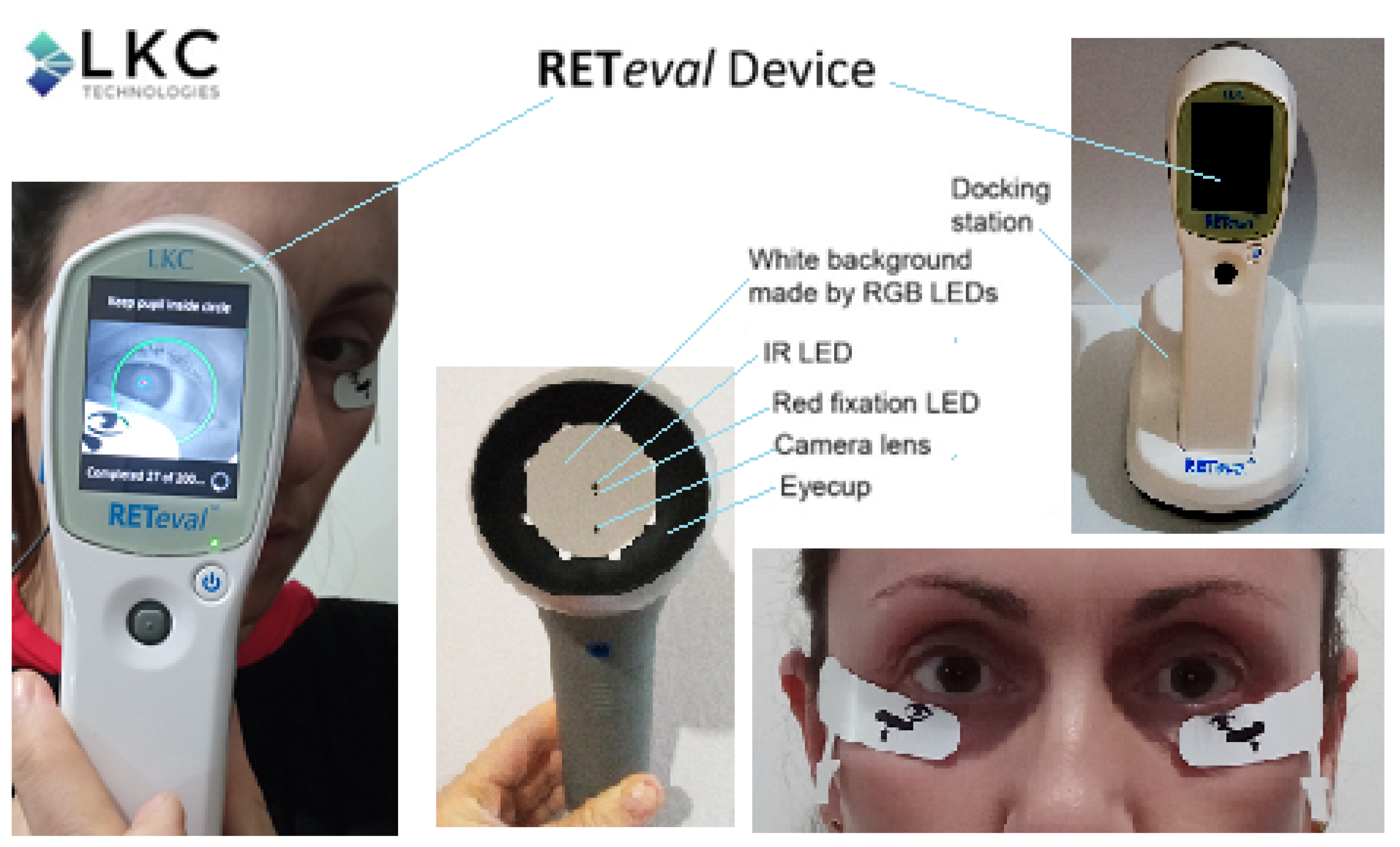
2.3. The Portable ERG Device—RETeval
2.4. Patients, Examination Procedure, and Evaluation
= Photopic flash luminance (cd × s/m2) × pupil area (mm2)
2.5. Parameter Assessment and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Assi, L.; Chamseddine, F.; Ibrahim, P.; Sabbagh, H.; Rosman, L.; Congdon, N.; Evans, J.; Ramke, J.; Kuper, H.; Burton, M.J.; et al. A global assessment of eye health and quality of life. JAMA Ophthalmol. 2021, 139, 526–541. [Google Scholar] [CrossRef]
- World Health Organization. World Report of Vision; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Braithwaite, T.; Calvert, M.; Gray, A.; Pesudovs, K.; Denniston, A.K. The use of patient-reported outcome research in modern ophthalmology: Impact on clinical trials and routine clinical practice. Patient Relat. Outcome Meas. 2019, 10, 9–24. [Google Scholar] [CrossRef]
- Camara, J.; Neto, A.; Pires, I.M.; Villasana, M.V.; Zdravevski, E.; Cunha, A. A Comprehensive Review of Methods and Equipment for Aiding Automatic Glaucoma Tracking. Diagnostics 2022, 12, 935. [Google Scholar] [CrossRef]
- Weinreb, R.; Aung, T.; Medeiros, F. The Pathophysiology and Treatment of Glaucoma: A Review. JAMA 2014, 311, 1901–1911. [Google Scholar] [CrossRef]
- Deemer, A.D.; Goldstein, J.E.; Ramulu, P.Y. Approaching rehabilitation in patients with advanced glaucoma. Eye 2022. [Google Scholar] [CrossRef]
- Deimantavicius, M.; Hamarat, Y.; Lucinskas, P.; Zakelis, R.; Bartusis, L.; Siaudvytyte, L.; Januleviciene, I.; Ragauskas, A. Prospective clinical study of non-invasive intracranial pressure measurements in open-angle glaucoma patients and healthy subjects. Medicina 2020, 56, 664. [Google Scholar] [CrossRef]
- Cvenkel, B.; Kolko, M. Devices and treatments to address low adherence in glaucoma patients: A narrative review. J. Clin. Med. 2023, 12, 151. [Google Scholar] [CrossRef] [PubMed]
- Quigley, H.; Addicks, E.; Green, W. Optic Nerve Damage in Human Glaucoma. Quantitative III Correlation of Nerve Fiber Loss and Visual Field Defect in Glaucoma, Ischemic Neuropathy, Papilledema, and Toxic Neuropathy. Arch. Ophthalmol. 1982, 100, 135–146. [Google Scholar] [CrossRef]
- Yaghoobi, G.; Heydari, B.; Heydari, S.R.; Poorabdolahi, F.; Sharifzadeh, G. Chronic Open-Angle Glaucoma and Its Association with The Cup Shape in Referral Ophthalmology Centre. Pharmacophores 2018, 9, 65–70. [Google Scholar]
- Sultan, M.; Mansberger, S.; Lee, P. Understanding the Importance of IOP Variables in Glaucoma: A Systematic Review. Surv. Ophthalmol. 2009, 54, 643–662. [Google Scholar] [CrossRef] [PubMed]
- Alsirhani, E.K.; Ayidh Alosaimi, S.M.; Ali Alkhawajah, S.A.; Alsaqer, S.K.; Alanazi, M.S.H.; Alanzi, H.O.H.; Alghamdi, L.S.A.; Alfaifi, A.S.; Almutairi, J.A. An Overview of Glaucoma Diagnosis & Management: A Literature Review. Arch. Pharma Pract. 2020, 11, 66–69. [Google Scholar]
- Noecker, R. The management of glaucoma and intraocular hypertension: Current approaches and recent advances. Ther. Clin. Risk Manag. 2006, 2, 193–206. [Google Scholar] [CrossRef]
- Sharma, P.; Sample, P.; Zangwill, L.; Schuman, J. Diagnostic Tools for Glaucoma Detection and Management. Surv. Ophthalmol. 2008, 53, S17–S32. [Google Scholar] [CrossRef] [PubMed]
- Tatham, A.J.; Medeiros, F.A. Detecting structural progression in glaucoma with optical coherence tomography. Ophthalmology 2017, 124, S57–S65. [Google Scholar] [CrossRef]
- Wilsey, L.J.; Fortune, B. Electroretinography in glaucoma diagnosis. Curr. Opin. Ophthalmol. 2016, 27, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Awwad, M.H.; Nada, O.; Hamdi, M.M.; El-Shazly, A.A.E.-F.; Elwan, S. Correlation between optical coherence tomography and photonic negative response of flash electroretinography in ganglion cell complex assessment in glaucoma patients. Clin. Ophthalmol. 2022, 16, 893–904. [Google Scholar] [CrossRef] [PubMed]
- Frishman, L.; Sustar, M.; Kremers, J.; McAnany, J.; Sarossy, M.; Tzekov, R.; Viswanathan, S. ISCEV extended protocol for the photopic negative response (PhNR) of the full-field electroretinogram. Doc. Ophthalmol. 2018, 136, 207–211. [Google Scholar] [CrossRef]
- Lee, S.Y.; Son, N.-H.; Bae, H.-W.; Seong, G.J.; Kim, C.Y. The role of pattern electroretinograms and optical coherence tomography angiography in the diagnosis of normal-tension glaucoma. Sci. Rep. 2021, 11, 12257. [Google Scholar] [CrossRef]
- Machida, S. Clinical Applications of the Photopic Negative Response to Optic Nerve and Retinal Diseases. J. Ophthalmol. 2012, 2012, 397178. [Google Scholar] [CrossRef]
- Kirkiewicz, M.; Lubinski, W.; Penkala, K. Photopic negative response of full-field electroretinography in patients with different stages of glaucomatous optic neuropathy. Doc. Ophthalmol. 2016, 132, 57–65. [Google Scholar] [CrossRef]
- Prencipe, M.; Perossini, T.; Brancoli, G.; Perossini, M. The photopic negative response (PhNR): Measurement approaches and utility in glaucoma. Int. Ophthalmol. 2020, 40, 3565–3576. [Google Scholar] [CrossRef]
- Hui, F.; Tang, J.; Hadoux, X.; Coote, M.; Crowston, J.G. Optimizing a portable ERG device for glaucoma clinic: The effect of interstimulus frequency on the photopic negative response. Trans. Vis. Sci. Technol. 2018, 7, 26. [Google Scholar] [CrossRef]
- Kita, Y.; Hollo, G.; Saito, T.; Momota, Y.; Kita, R.; Tsunoda, K.; Hirakata, A. RETeval portable electroretinogram parameters in different severity stages of glaucoma. J. Glaucoma 2020, 29, 572–580. [Google Scholar] [CrossRef]
- Kiszkielis, M.; Lubiński, W.; Penkala, K. The Photopic Negative Response as a promising diagnostic tool in glaucoma. A review. Klin. Ocz. 2012, 114, 138–142. [Google Scholar]
- Karanjia, R.; Berezovsky, A.; Sacai, P.; Cavascan, N.; Liu, H.; Nazarali, S.; Moraes-Filho, M.; Anderson, K.; Tran, J.; Watanabe, S.; et al. The Photopic Negative Response: An Objective Measure of Retinal Ganglion Cell Function in Patients With Leber’s Hereditary Optic Neuropathy. Investig. Ophthalmol. Vis. Sci. 2017, 58, BIO300–BIO306. [Google Scholar] [CrossRef]
- Wu, Z.; Hadoux, X.; Hui, F.; Sarossy, M.; Crowston, J.G. Photopic Negative Response Obtained Using a Handheld Electroretinogram Device: Determining the Optimal Measure and Repeatability. Trans. Vis. Sci. Technol. 2016, 5, 8. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, S.; Frishman, L.; Robson, J.; Walters, J. The Photopic Negative Response of the Flash Electroretinogram in Primary Open Angle Glaucoma. Investig. Ophthalmol. Vis. Sci. 2001, 42, 514–522. [Google Scholar]
- Al-Nosairy, K.; Hoffmann, M.; Bach, M. Non-invasive electrophysiology in glaucoma, structure and function—A review. Eye 2021, 35, 2374–2385. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Edwards, T.; Crowston, J.; Sarossy, M. The Test–Retest Reliability of the Photopic Negative Response (PhNR). Trans. Vis. Sci. Technol. 2014, 3, 1. [Google Scholar] [CrossRef]
- Mortlock, K.; Binns, A.; Aldebasi, Y.; North, R. Inter-subject, inter-ocular and inter-session repeatability of the photopic negative response of the electroretinogram recorded using DTL and skin electrodes. Doc. Ophthalmol. 2010, 121, 123–134. [Google Scholar] [CrossRef]
- Asakawa, K.; Amino, K.; Iwase, M.; Kusayanagi, Y.; Nakamura, A.; Suzuki, R.; Yuuki, T.; Ishikawa, H. New Mydriasis-Free Electroretinogram Recorded with Skin Electrodes in Healthy Subjects. BioMed Res. Int. 2017, 2017, 8539747. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Sugawara, A.; Nagashima, R.; Ikesugi, K.; Sugimoto, M.; Kondo, M. Factors Affecting Photopic Negative Response Recorded with Reteval System: Study of Young Healthy Subjects. Trans. Vis. Sci. Technol. 2020, 9, 19. [Google Scholar] [CrossRef]
- Raharja, A.; Leo, S.; Chow, I.; Indusegaran, M.; Hammond, C.; Mahroo, O.; Wong, S. Exploratory Study of the Association between the Severity of Idiopathic Intracranial Hypertension and Electroretinogram Photopic Negative Response Amplitude Obtained Using a Handheld Device. Life 2021, 11, 437. [Google Scholar] [CrossRef]
- Tang, J.; Hui, F.; Hadoux, X.; Sarossy, M.; Wijngaarden, P.; Coote, M.; Crowston, J.G. A comparison of the RETeval sensor strip and DTL electrode for recording the photopic negative response. Trans. Vis. Sci. Technol. 2018, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Kondo, M.; Sugimoto, M.; Ikesugi, K.; Matsubara, H. Effect of Pupil Size on Flicker ERGs Recorded With RETeval System: New Mydriasis-Free Full-Field ERG System. Investig. Ophthalmol. Vis. Sci. 2015, 56, 3684–3690. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Kraszewska, O.; Manning, C. Constant luminance (cd.s/m2) versus constant retinal illuminance (Td.s) stimulation in flicker ERGs. Doc. Ophthalmol. 2017, 134, 75–87. [Google Scholar] [CrossRef]
- Knight, O.J.; Girkin, C.A.; Budenz, D.L.; Durbin, M.K.; Feuer, W.J. Effect of race, age, and axial length on optic nerve head parameters and retinal nerve fiber layer thickness measured by Cirrus HD-OCT. Arch. Ophthalmol. 2012, 130, 312–318. [Google Scholar] [CrossRef]
- Aghaian, E.; Choe, J.E.; Lin, S.; Stamper, R.L. Central corneal thickness of caucasians, chinese, hispanics, filipinos, african, americans, and japanese in a glaucoma clinic. Ophthalmology 2004, 111, 2211–2219. [Google Scholar] [CrossRef]
- Machida, S.; Gotoh, Y.; Toba, Y.; Ohtaki, A.; Kaneko, M.; Kurosa, D. Correlation between photopic negative response and retinal nerve fiber layer thickness and optic disc topography in glaucomatous eyes. Investig. Ophthalmol. Vis. Sci. 2008, 49, 2201–2207. [Google Scholar] [CrossRef]




| Description of the Protocol PhNR 3.4 Hz Td Long | ||
|---|---|---|
| Flash Luminance Energy (Red LED, 621 nm) | Background Luminance (Blue LED, 470 nm) | Flashes |
| 38 Td . s @ 3.4 Hz | 380 Td | 200 |
| Mean Value ± Standard Deviation | ||||
|---|---|---|---|---|
| Variables | Case Group (n = 59) | Control Group (n = 63) | Control Group (Age 30–54) (n = 36) | Control Group (Age 55–80) (n = 27) |
| Age (y) | 67.7 ± 10.3 | 52.8 ± 12.0 | 44.1 ± 6.1 | 64.4 ± 6.8 |
| RNFL (μm) | 76.9 ± 12.9 | 91.4 ± 8.6 | 91.8 ± 8.9 | 90.9 ± 8.2 |
| a-wave (μV) | −7.4 ± 2.4 | −7.8 ± 2.6 | −7.5 ± 2.3 | −8.1 ± 3.0 |
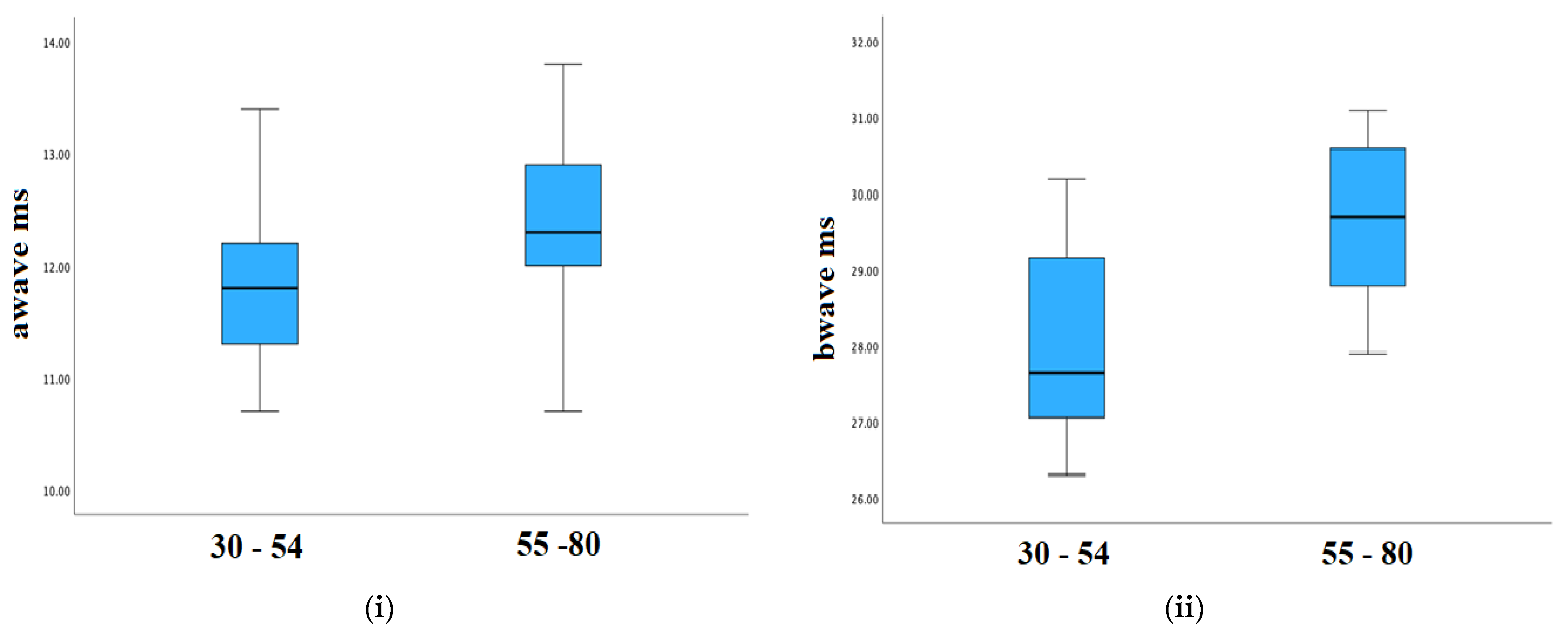
| a-wave (ms) | 12.8 ± 1.1 | 12.1 ± 0.8 | 11.8 ± 0.6 | 12.4 ± 0.8 |
| b-wave (μV) | 20.8 ± 6.0 | 23.3 ± 6.8 | 23.2 ± 6.6 | 23.4 ± 7.2 |
| b-wave (ms) | 30.5 ± 2.1 | 28.7 ± 1.4 | 28.0 ± 1.3 | 29.7 ± 1.0 |
| PhNrmin (μV) | −4.4 ± 1.3 | −5.2 ± 1.5 | −5.1 ± 1.4 | −5.4 ± 1.7 |
| PhNrmin (ms) | 60.9 ± 9.2 | 58.1 ± 9.7 | 56.3 ± 11.6 | 60.6 ± 5.7 |
| W-ratio | 0.86 ± 0.05 | 0.9 ± 0.1 | 0.9 ± 0.1 | 0.9 ± 0.1 |
| IOP (mm Hg) | 15.3 ± 2.7 | 15.6 ± 2.1 | 15.0 ± 2.1 | 16.4 ± 1.9 |
| Normality Test | ||
|---|---|---|
| Parameters | Case Group | Control Group |
| RNFL (μm) | 0.200 | 0.200 |
| a-wave (ms) | 0.200 | 0.200 |
| a-wave (μV) | 0.024 | 0.001 |
| b-wave (ms) | 0.200 | 0.200 |
| b-wave (μV) | 0.040 | 0.019 |
| PhNrmin (ms) | 0.005 | <0.001 |
| PhNrmin (μV) | 0.200 | 0.014 |
| W-ratio | 0.051 | 0.009 |
| p-Values | |||||
|---|---|---|---|---|---|
| Case Group | Control Group | Case Group/Control | |||
| Parameters | Left and Right Eye | Left and Right Eye | Age 30–54 and 55–80 | Age 30–80 | Age 55–80 |
| RNFL (μm) | 0.497 | 0.935 | 0.656 | <0.001 | <0.001 |
| a-wave (ms) | 0.987 | 0.019 | <0.001 | <0.001 | 0.05 |
| a-wave (μV) | 1 | 0.956 | 0.500 | 0.601 | 0.636 |
| b-wave (ms) | 0.431 | 0.816 | <0.001 | <0.001 | 0.01 |
| b-wave (μV) | 0.481 | 0.568 | 0.734 | 0.037 | 0.099 |
| PhNrmin (ms) | 0.291 | 0.842 | 0.067 | 0.022 | 0.072 |
| PhNrmin (μV) | 0.524 | 0.536 | 0.474 | 0.002 | 0.009 |
| W-ratio | 0.144 | 0.956 | 0.775 | <0.001 | 0.007 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bekollari, M.; Dettoraki, M.; Stavrou, V.; Skouroliakou, A.; Liaparinos, P. Investigating the Structural and Functional Changes in the Optic Nerve in Patients with Early Glaucoma Using the Optical Coherence Tomography (OCT) and RETeval System. Sensors 2023, 23, 4504. https://doi.org/10.3390/s23094504
Bekollari M, Dettoraki M, Stavrou V, Skouroliakou A, Liaparinos P. Investigating the Structural and Functional Changes in the Optic Nerve in Patients with Early Glaucoma Using the Optical Coherence Tomography (OCT) and RETeval System. Sensors. 2023; 23(9):4504. https://doi.org/10.3390/s23094504
Chicago/Turabian StyleBekollari, Marsida, Maria Dettoraki, Valentina Stavrou, Aikaterini Skouroliakou, and Panagiotis Liaparinos. 2023. "Investigating the Structural and Functional Changes in the Optic Nerve in Patients with Early Glaucoma Using the Optical Coherence Tomography (OCT) and RETeval System" Sensors 23, no. 9: 4504. https://doi.org/10.3390/s23094504
APA StyleBekollari, M., Dettoraki, M., Stavrou, V., Skouroliakou, A., & Liaparinos, P. (2023). Investigating the Structural and Functional Changes in the Optic Nerve in Patients with Early Glaucoma Using the Optical Coherence Tomography (OCT) and RETeval System. Sensors, 23(9), 4504. https://doi.org/10.3390/s23094504








